Abstract
Background
Revisional surgery is an important component of addressing weight regain and complications following primary bariatric surgery. Owing to provincial need and the complexity of this patient population, a specialized multidisciplinary revision clinic was developed. We sought to characterize patients who undergo revision surgery and compare their outcomes with primary bariatric surgery clinic data.
Methods
We completed a retrospective chart review of bariatric revision clinic patients compared with primary bariatric surgery patients from December 2009 to June 2014.
Results
We reviewed the charts of 2769 primary bariatric clinic patients, 886 of whom had bariatric surgery, and 534 revision bariatric clinic patients, 83 of whom had revision surgery. Fewer revision clinic patients underwent surgery than primary clinic patients (22% v. 32%). The mean preoperative body mass index (BMI) was 44.7 ± 9.5 in revision patients compared with 45.7 ± 7.6 in primary bariatric surgery patients. Most revision patients had a prior vertical banded gastroplasty (VBG; 48%) or a laparoscopic adjustable gastric band (LAGB; 24%). Bands were removed in 36% of all LAGB patients presenting to clinic. Of the 134 procedures performed in the revision clinic, 83 were bariatric weight loss surgeries, and 51 were band removals. Revision clinic patients experienced a significant decrease in BMI (from 44.7 ± 9.5 to 33.8 ± 7.5, p < 0.001); their BMI at 12-month follow-up was similar to that of primary clinic patients (34.5 ± 7.0, p = 0.7). Complications were significantly more frequent in revision patients than primary patients (41% v. 15%, p < 0.001).
Conclusion
A bariatric revision clinic manages a wide variety of complex patients distinct from those seen in a primary clinic. Operative candidates at the revision clinic are chosen based on favourable medical, anatomic and psychosocial factors, keeping in mind the resource constraints of a public health care system.
Abstract
Contexte
La chirurgie de révision est une intervention importante lors d’une reprise de poids ou lors de complications à la suite d’une chirurgie bariatrique primaire. Compte tenu des besoins provinciaux et de la complexité de cette population de patients, une clinique de révision multidisciplinaire spécialisée a été créée. Nous avons voulu caractériser les patients qui subissent une chirurgie de révision et comparer leurs résultats aux données de la clinique de chirurgie bariatrique primaire.
Méthodes
Nous avons procédé à un examen rétrospectif des dossiers des patients de la clinique de révision bariatrique par rapport aux patients ayant subi une chirurgie bariatrique primaire entre décembre 2009 et juin 2014.
Résultats
Nous avons examiné les dossiers de 2769 patients de la clinique bariatrique primaire, dont 886 avaient subi une chirurgie bariatrique, et 534 patients de la clinique de révision, dont 83 avaient subi une chirurgie de révision. Un moins grand nombre de patients de la clinique de révision ont subi une chirurgie comparativement aux patients de la clinique primaire (22 % c. 32 %). L’indice de masse corporelle (IMC) préopératoire moyen était de 44,7 ± 9,5 chez les patients de la clinique de révision, contre 45,7 ± 7,6 chez les patients ayant subi la chirurgie bariatrique primaire. La plupart des patients de la clinique de révision avaient déjà subi une gastroplastie verticale (48 %) ou une pose d’anneau gastrique ajustable par voie laparoscopique (24 %). Les anneaux gastriques ont été retirés chez 36 % de tous les patients de ce dernier groupe s’étant présentés à la clinique. Parmi les 134 interventions effectuées à la clinique de révision, 83 étaient des chirurgies bariatriques (pour perte de poids) et 51 concernaient des retraits d’anneaux. Les patients de la clinique de révision ont obtenu une diminution significative de leur IMC (de 44,7 ± 9,5 à 33,8 ± 7,5, p < 0,001), qui, au moment du suivi après 12 mois, était semblable à celui des patients de la clinique primaire (34,5 ± 7,0, p = 0,7). Les complications ont été considérablement plus fréquentes chez les patients soumis à une chirurgie de révision que chez les patients soumis à une chirurgie primaire (41 % c. 15 %, p < 0,001).
Conclusion
Une clinique de révision bariatrique gère une grande diversité de patients complexes, qui sont différents de la population suivie dans une clinique d’intervention primaire. À la clinique de révision, les candidats à l’opération sont choisis en fonction de facteurs médicaux, anatomiques et psychosociaux favorables, en gardant à l’esprit les ressources limitées du système de santé public.
Bariatric surgery is the only evidence-based sustainable solution for the management of severe obesity. 1,2 Without bariatric surgery only 5% of adults with established obesity can maintain a healthy body weight.1,3 In addition to weight loss, surgery can also improve comorbidities, such as diabetes, hypertension, dyslipidemia and sleep apnea.2 However, on average 20% of patients will either fail to lose adequate weight (< 50% excess weight loss) or will regain weight after surgery.4 Similar to hip replacements and cardiac surgery, revisional surgery is one aspect of treatment necessary to manage refractory symptoms or surgical complications. More bariatric surgeons are adding revisional bariatric procedures to their existing practices.5 This is a complex patient group that requires case-by-case medical and surgical management.6 A dedicated revision clinic was created to accommodate private and medical tourists who have little or no aftercare for the management of their nutrition and complications.7
A multidisciplinary approach is modelled after the primary clinic, which includes nurses, dieticians, psychologists and physicians. A specific “red flag” system is used by each discipline to screen out patients who would be unlikely to succeed with revision surgery. Red flag criteria include uncontrolled mental health issues, substance abuse, poor social supports, poor compliance and unrealistic goals.7 The objective of this study was to review all 5 years of patients since the inception of the clinic and compare the outcomes, patient populations and complications between the revision clinic and the primary clinic.
Methods
A retrospective review was conducted of patients who entered the Adult Bariatric Surgery Revision Clinic between its inception in December 2009 and June 2014. We retrieved information on demographics, body mass index (BMI), comorbidities, clinic visits, previous surgeries and complications. We also reviewed the charts of patients in the primary Edmonton Adult Bariatric Specialty Clinic over the same time period. This study was completed with full approval from our institutional ethics review board.
To enter the revision clinic, patients were required to have a history of bariatric surgery and imaging (at minimum upper gastrointestinal swallow study and esophagogastroduodenoscopy) to delineate anatomy before their first clinic appointment. Patients were evaluated by a multidisciplinary team, including a nurse, dietician and psychologist, for red flags.7 Surgical candidates were chosen based on the specific red flag system designed to identify patients who would be unlikely to benefit from further surgery. This conservative operating strategy mirrors that of the Centre of Excellence–accredited primary bariatric clinic. Surgical candidates also had to have anatomy amenable to operative correction. In our experience, patients who have anatomic abnormalities seen on imaging and have undergone several surgical procedures are likely to have adhesions or a more difficult operation, which may reduce the benefit:risk ratio of revisional surgery.
All surgeries in the revision clinic were carried out by a single revisional surgeon (C.d.G.). Details regarding the surgical techniques for both primary and revision surgeries have been published previously.8 Primarily open Roux-en-Y gastric bypass (ORYGB) was performed in our patient population. Differences between the laparoscopic and open techniques were subtle. A fundic resection was carried out to avoid the risk of ischemia, and the Roux limb was made retrocolic. Follow-up postoperatively occurred at 1, 3, 6 and 12 months.
Statistical analysis
All data were analyzed using STATA statistical software (Statacorp). Continuous variables (e.g., BMI and age) are presented as means ± standard deviations and were analyzed for statistical significance using Kruskal–Wallis and Wilcoxon signed-rank tests. Categorical variables were analyzed using χ2 and Fisher exact tests. Graphs were created using GraphPad Prism software version 5.0.
Results
We reviewed 534 charts from the revision clinic and 2769 from the primary bariatric clinic for the same time period. Of the 534 revision clinic patients, 18 patients were incomplete referrals, 130 patients were lost to follow-up after only 1 visit and 250 patients were treated medically. The remaining 136 patients were surgical candidates; 117 of them had surgery, whereas the others refused surgery and their symptoms were managed in other ways. Patients lost to follow-up were contacted by the clinic by phone, and these patients declined to return for more than 1 appointment. A large number of patients left the clinic after being considered inappropriate for surgery based on the red flag system (126 of 250, 50%) and did not want to pursue medical management. The primary clinic no longer follows patients who are not surgical candidates. Of the 2769 patients seen in the primary clinic, 886 patients had surgery, and the remaining 1883 patients were lost to follow-up or were not surgical candidates and were discharged.
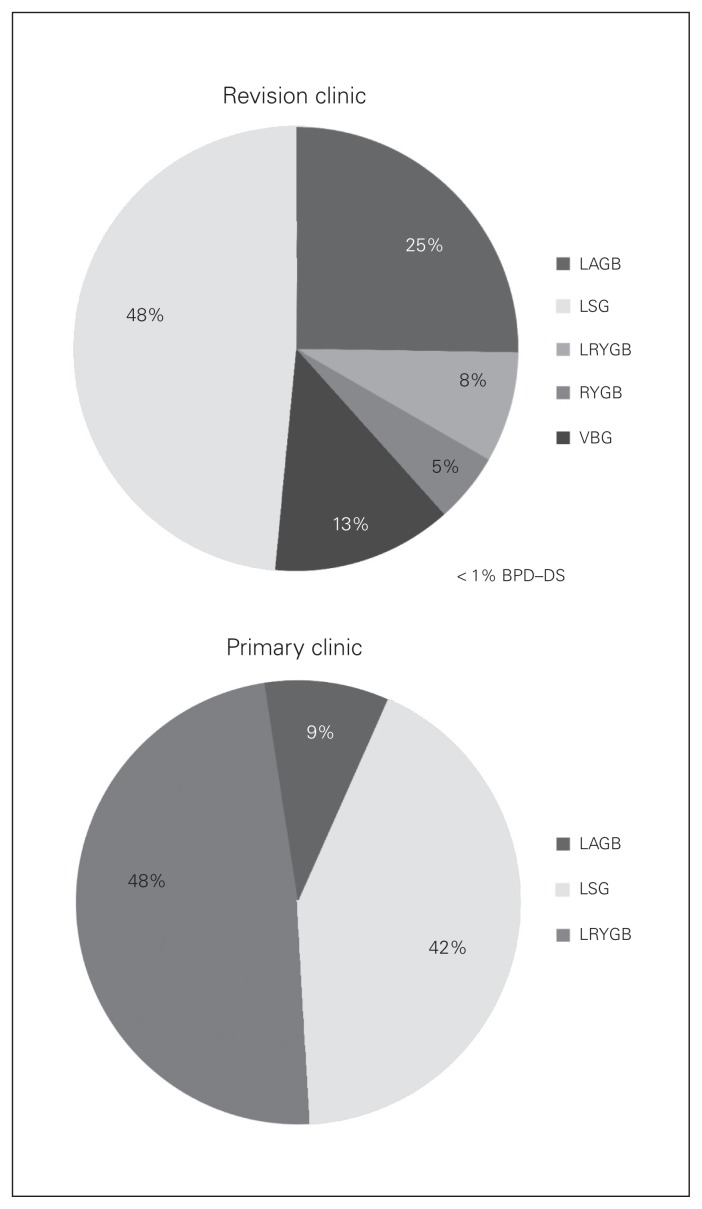
Demographic comparisons between the primary and revision clinic are shown in Table 1. Patients were significantly older in the revision group than in the primary group (p < 0.001). Significantly more patients in the primary clinic than the revision clinic had diabetes, hypertension and dyslipidemia, whereas more patients in the revision clinic than the primary clinic had reflux. Figure 1 compares the proportion of primary procedures of revision clinic patients and primary clinic patients. A larger proportion of patients in the revision clinic than in the primary clinic underwent laparoscopic adjustable gastric band (LAGB) procedures. Only 4% of patients in the revision clinic were referred from the primary clinic; they were referred if they had been previously discharged from the primary clinic. Many revision patients had their original surgeries performed in Alberta but outside of the primary clinic (52%), and 43% of patients were bariatric medical tourists — individuals who travel outside of the province in search of private medical care.8
Table 1.
Demographic and clinical characteristics of the study sample
| Characteristic | Group; mean ± SD or % | p value | |
|---|---|---|---|
| Primary (n = 2769) | Revision (n = 534) | ||
| Age, yr | 44.0 ± 9.1 | 48 ± 10 | < 0.001 |
| Female sex | 83 | 90 | < 0.001 |
| Initial BMI | 49.9 ± 8.6 | 42.7 ± 10.8 | < 0.001 |
| Comorbidity | |||
| Diabetes | 30 | 19 | < 0.001 |
| Hypertension | 41.3 | 27.4 | < 0.001 |
| Dyslipidemia | 26.9 | 13 | < 0.001 |
| Reflux | 24 | 42.1 | < 0.001 |
BMI = body mass index; SD = standard deviation.
Fig. 1.
Frequency of bariatric procedures in patients presenting to the revision clinic (top) and the primary bariatric clinic (bottom). BPD/DS = biliopancreatic diversion with duodenal switch; LAGB = laparoscopic adjustable gastric band; LRYGB = laparoscopic Rouxen-Y gastric bypass; LSG = laparoscopic sleeve gastrectomy; ORYGB = open Roux-en-Y gastric bypass; VBG = vertical banded gastroplasty.
The majority of patients in the revision clinic were referred owing to weight regain (64%). This was true for all previous surgeries except biliopancreatic diversion with duodenal switch (BPD/DS); 75% of those who underwent BPD/DS were referred for malnutrition. Dysphagia was the second most common reason for referral to the revision clinic, regardless of primary surgery type (26%). In total, 21% of patients who underwent primary LAGB were referred for band complications, and 9% of all patients were referred solely for nutritional management. The final concern leading to referral was complications from the primary surgery, such as bowel obstruction. Many patients were referred for several simultaneous concerns (e.g., dysphagia and weight regain). In total, 7% of patients had already undergone some form of previous revision of the primary procedure before entering the revision clinic, and 12% of patients had undergone multiple bariatric procedures before presenting to clinic. In cases where patients presented years after their original procedures, records of what surgery was performed were often unavailable.
Owing to the rigorous screening process, only 22% (117 of 534) of patients ultimately received a revision surgery. Predictably, this rate differed significantly from that of the primary clinic (32%, p < 0.001). There were a total of 134 operations performed in 117 revision clinic patients (51 band removals and 83 bariatric revision procedures; Table 2). The most common revision surgery performed was ORYGB. This procedure was chosen because of its long safety and efficacy record as well as the relative ease of converting a vertical banded gastroplasty (VBG) pouch to an RYGB pouch. Patients were also offered sleeve gastrectomy (SG) if it was felt to be anatomically compatible with their previous operation(s). Patients who were not medically fit for RYGB or who did not want a major surgery but still had considerable symptoms from bands were offered band removal. Of the patients undergoing revision surgery, 4.9% had a combination of procedures (e.g., ORYGB and hernia repair). Of the patients who underwent LAGB, 36% (n = 48) required a band removal, and 35% (n = 17) of them went on to have a second definitive procedure. A few patients had anatomy compatible with laparoscopic RYGB (LRYGB; n = 4) or SG (LSG; n = 13), but most needed an open procedure because of scar tissue from multiple previous open operations.
Table 2.
Type of revision surgery performed in revision clinic patients, by primary surgery
| Revision surgery | Primary surgery; no. of patients | |||||
|---|---|---|---|---|---|---|
| 1° VBG (n = 259) | 1° LAGB (n = 132) | 1° LSG (n = 44) | 1° LRYGB (n = 27) | 1° ORYGB (n = 69) | 1° BPD/DS (n = 4) | |
| Band removal (n = 51) | 3 | 48 | — | — | — | — |
| 2° LSG (n = 13) | — | 11 | — | — | 1 | 1 |
| 2° LRYGB (n = 4) | 1 | 1 | 1 | — | 1 | — |
| 2° ORYGB (n = 66) 60* | 5 | — | 1 | 1 | — | |
| Total | 64 | 65 | 1 | 1 | 3 | 1 |
BPD/DS = biliopancreatic diversion with duodenal switch; LAGB = laparoscopic adjustable gastric band; LRYGB = laparoscopic Roux-en-Y gastric bypass; LSG = laparoscopic sleeve gastrectomy; ORYGB = open Roux-en-Y gastric bypass; VBG = vertical banded gastroplasty.
One patient had both a primary VBG and revised ORYGB before presenting for a second ORYGB.
The average duration of surgery in the revision clinic was 0.6 ± 0.2 hours (range 0.4–1.0 hours) for band removal and 2.8 ± 0.7 hours (range 1.4–5.1 hours) for revision surgery. The average duration of primary surgery was 1.3 ± 0.5 hours for LSG, 2.4 ± 0.8 hours for LRYGB and 0.6 ± 0.4 hours for LAGB. The duration of revision ORYGB was 0.4 hours longer than the duration of primary LRYGB (p = 0.001). Median length of stay in hospital for primary procedures was 2 days (range 0–9 days) compared with 4 days (range 0–84 days) for revision procedures (p < 0.001).
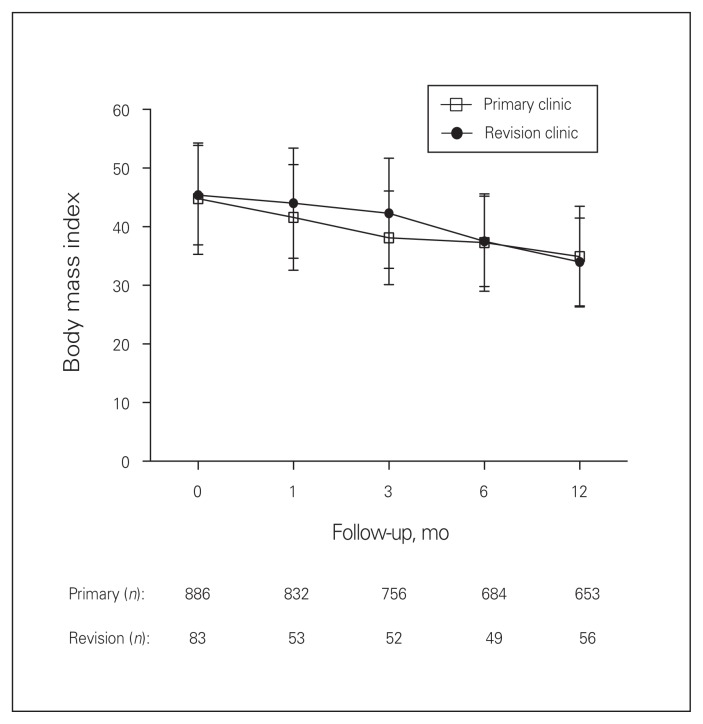
Revision clinic patients experienced a significant decrease in BMI (from 44.7 ± 9.5 to 33.8 ± 7.5, percent excess weight loss [%EWL] 61.2%, p < 0.001); their BMI at 12-month follow-up was similar to that of primary clinic patients (34.5 ± 7.0, %EWL 56.0%, p = 0.7; Fig. 2). Patients who were not considered appropriate for surgery and elected to be managed medically on average had a decrease in BMI from 42.5 ± 10.9 to 40.9 ± 10.7 (%EWL 14.3%, p = 0.007) within a median clinic follow-up time of 6 months (range 1–25 months). Follow-up at 1 year was 68% in the revision clinic compared with 74% in the primary clinic. Revision surgery had a higher complication rate than primary surgery; 41% of revision clinic patients experienced a complication compared with 15% of primary clinic patients (p < 0.001). Most of the revision surgery complications were wound infections (24%), and 56% of all complications resolved within 3 months. Table 3 lists the complications from the ORYGB. One patient who underwent LSG had a stricture, and 1 patient who underwent LRYGB had a bleed. Reoperation rates were significantly different between the revision and primary groups (10.8% v. 5.4%, p = 0.033). There were no deaths in either group.
Fig. 2.
Change in body mass index after surgery.
Table 3.
Complications of patients in the primary and revision bariatric clinic
| Complication | Group, procedure; %* | p value† | ||
|---|---|---|---|---|
| Primary LSG (n = 366) | Primary LRYGB (n = 397) | Revision ORYGB (n = 66) | ||
| Leak | 0 | 0.9 | 4.5 | 0.09 |
| Bleed | 1.7 | 6.0 | 0 | 0.03 |
| SSI/abscess | 1.3 | 15.3 | 36.4 | < 0.001 |
| Stricture | 0.4 | 7.4 | 4.5 | 0.3 |
| Ulcer | 1.3 | 8.7 | 9.1 | 0.5 |
| Fistula | 0 | 0.4 | 9.1 | < 0.001 |
| Bowel obstruction | 0 | 0.7 | 4.5 | 0.03 |
| Hernia | 0.9 | 3.7 | 12.1 | 0.02 |
| Other | 0 | 1.2 | 6.1 | 0.06 |
LRYGB = laparoscopic Roux-en-Y gastric bypass; LSG = laparoscopic sleeve gastrectomy; ORYGB = open Roux-en-Y gastric bypass; SSI = surgical site infection.
Patients who received laparoscopic adjustable gastric bands (n = 122) had none of the perioperative complications listed above.
Comparing primary and revision Roux-en-Y gastric bypass.
Discussion
There is growing evidence to support treating obesity as a chronic disease. An emerging area of concern is patients with weight recidivism and complications after bariatric surgery seeking further surgical treatment. The Adult Bariatric Surgery Revision Clinic was created to manage the large number of such patients contacting the primary Edmonton Adult Bariatric Specialty Clinic, which already had a wait time of approximately 1 year for initial assessment. The revision program began with a single surgeon, and a second recently joined the program to manage the increasing volume of patients. To our knowledge the revision clinic is the first of its kind to solely manage revision patients and includes a multidisciplinary team based on our primary clinic. This clinic not only offers surgery, but also dietary advice, surgical follow-up for medical tourists and LAGB adjustments. Because some surgeons may decide not to manage these complex patients, without the revision clinic many patients are left without surgical or specialized lifestyle follow-up.
The revision clinic patients had significantly less diabetes, hypertension and dyslipidemia, but more reflux than primary clinic patients. The increased reflux is likely a result of anatomic changes from the previous surgery. Reflux is a common symptom even with an intact VBG, despite studies showing that the operation (when properly performed) is designed to decrease reflux.9,10 Patients who underwent LSG had the highest rates of reflux, with 57% of patients prescribed an antisecretory therapy. There are few studies in the literature describing the presence or resolution of comorbidities in revision patients. However, 1 study11 showed similar levels of diabetes, hypertension and sleep apnea in primary and revision populations, whereas 2 others12,13 reported a marked increase in comorbidities, with weight regain after bariatric surgery and up to 22% of patients requiring further surgery. Several studies have reported pre- and postoperative BMI results similar to ours.14–16
Half of all revision patients had a prior VBG. Because of resultant complications and poor weight loss (21%–50%), this procedure was phased out as a primary bariatric procedure many years ago.17,18 Three years after VBG, 56% of patients need revisional surgery.19 Studies also suggest a 26%–48% rate of staple line failure within 5 years.20,21 Therefore, it is not surprising that a large portion of the revision clinic patients comprises those who underwent VBG. Ten-year follow-up of this procedure is uncommon, but 1 study reported only 26% of patients maintained weight loss in the long term.22
In total, 25% of the revision clinic patients underwent LAGB. This is a popular procedure among medical tourists (86% had an LAGB), and often patients are not educated about the major dietary and lifestyle changes required after this surgery. Of the patients who presented to the revision clinic with band erosion/slippage or insufficient weight loss, 78% and 88%, respectively, were medical tourists, leading us to believe that poor follow-up may play a role in these postoperative issues.
With stringent criteria, only 22% of revision patients underwent surgical management, compared with 32% of patients in the primary clinic. Both of these percentages are lower than the operative volume in a private system owing to our process for patient selection and the need to allocate limited resources to candidates most likely to be successful. In our experience, patients with uncontrolled psychosocial and medical issues are more likely to have weight recidivism despite anatomically successful surgery, which is why our red flag system was developed. A multidisciplinary team is included in the bariatric clinics to optimize and approve appropriate patients for surgery, as per the American Society for Metabolic and Bariatric Surgery (ASMBS) 2004 consensus guidelines. In our experience, RYGB is the procedure of choice for revising previous bariatric surgery, specifically VBG, because of its effective weight loss results and safety.23–25 Not surprisingly, patients who underwent VBG most often qualified for further surgery (23% underwent RYGB), whereas most patients who had anatomically successful operations, such as prior SG or RYGB, were unlikely to need further surgical management (92%). In these patients, we often repaired hernias and performed panniculectomies. The first step for patients who underwent primary LAGB is to remove the gastric band. In the literature, only 16% of patients were reported to undergo a secondary procedure after LAGB removal,26 whereas 38% of such patients underwent a secondary procedure in our study.
Revisional bariatric surgery duration was on average 0.4 hours longer than primary bariatric surgery, and revision clinic patients remained in hospital a median of 2 days longer. These were statistically significant increases in resource use; however, an economic study would need to be performed to determine whether these resources outweigh the benefits of BMI reduction and improved lifestyle management in these patients.
After 1 year of follow-up, patients in both the revision and primary clinics had similar BMI (33). Revisional bariatric surgery was successful in substantially reducing BMI — significantly more than in the group managed only with lifestyle modification.
Due to adhesions, a high percentage of revision operations needed to be performed using an open technique. Wound infections were by far the most common complication, as expected with a large open incision in morbidly obese patients. Currently a combination of delayed primary closure and vacuum-assisted wound closure are being used to try and mitigate this complication. In future, to address certain complications, such as wound infections, more revision surgeries will be first attempted laparoscopically, as all primary surgeries are now done using minimally invasive techniques. Currently, the majority of our patients had primary open surgery and often had further open revisional surgery before arriving at our clinic. This demonstrates the need for an advanced skill set for bariatric surgeons who will be asked to manage this complex group of patients. Incisional hernias were also more common in the revisional group, most likely due to the large incision; the complications of 56% of these patients resolved within 3 months.
There was a higher attrition rate in the revision clinic than the primary clinic. Possible reasons include more resources in the primary clinic devoted to encouraging follow- up, medical tourism and the larger geographical area served by the revision clinic. For bariatric revision patients alone, the rate of follow-up was still lower than the primary clinic (68% vs. 74%) at 1 year. However, many of these patients were purposefully discharged after successful panniculectomies and hernia repairs.
Limitations
The limitations of this study include a large number of patients lost to follow-up in both the primary and revision clinics. However, most of these patients were not in the group treated with surgery. Furthermore, any retrospective review has limitations based on the quality of the data collection and unknown biases.
Conclusion
A bariatric revision clinic manages a wide variety of complex patients distinct from those seen in a primary clinic. Fewer revision clinic patients underwent surgery than primary clinic patients (22% v. 32%); operative candidates are chosen based on favourable medical, anatomic and psychosocial factors, keeping in mind the resource constraints of a public health care system. The initial results from this bariatric revision clinic are encouraging. The weight loss and outcomes are comparable to those of a primary bariatric clinic with a higher complication rate and slightly increased resource use.
Footnotes
Competing interests: D. Birch has received educational grants from Johnson & Johnson, Covidien and Stryker. He has also received a speaker honorarium from Cook. No other competing interests declared.
Contributors: C. Sheppard, D. Birch, S. Karmali and C. de Gara designed the study. C. Fulton and C. Sheppard acquired and analyzed the data, which S. Karmali also analyzed. C. Fulton, C. Sheppard and D. Birch wrote the article, which all authors reviewed and approved for publication.
References
- 1.Gastrointestinal surgery for severe obesity. NIH consensus development conference, March 25–7,1991. Nutrition. 1996;12:397–404. [PubMed] [Google Scholar]
- 2.Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–37. doi: 10.1001/jama.292.14.1724. [DOI] [PubMed] [Google Scholar]
- 3.Ontario HQ. Bariatric surgery: an evidence-based analysis. Ont Health Technol Assess Ser. 2005;5:1. [PMC free article] [PubMed] [Google Scholar]
- 4.Sheppard CE, Lester EL, Chuck AW, et al. The economic impact of weight regain. Gastroenterol Res Pract. 2013;2013:379564. doi: 10.1155/2013/379564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brethauer SA, Kothari S, Sudan R, et al. Systematic review on reoperative bariatric surgery: American Society for Metabolic and Bariatric Surgery Revision Task Force. Surg Obes Relat Dis. 2014;10:952–72. doi: 10.1016/j.soard.2014.02.014. [DOI] [PubMed] [Google Scholar]
- 6.Buchwald H. Revisional metabolic/bariatric surgery: a moral obligation. Surg Obes Relat Dis. 2014;10:1019–21. doi: 10.1016/j.soard.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 7.de Gara CJ, Karmali S. The anatomy of a weight recidivism and revision bariatric surgical clinic. Gastroenterol Res Pract. 2014;2014:721095. doi: 10.1155/2014/721095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Birch DW, Vu L, Karmali S, et al. Medical tourism in bariatric surgery. Am J Surg. 2010;199:604–8. doi: 10.1016/j.amjsurg.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 9.Balsiger BM, Muru MM, Mai J, et al. Gastroesophageal reflux after intact vertical banded gastroplasty: correction by conversion to Rouxen- Y gastric bypass. J Gastrointest Surg. 2000;4:276–81. doi: 10.1016/s1091-255x(00)80076-1. [DOI] [PubMed] [Google Scholar]
- 10.Deitel M, Khanna RK, Hagen J, et al. Vertical banded gastroplasty as an antireflux procedure. Am J Surg. 1988;155:512–6. doi: 10.1016/s0002-9610(88)80125-9. [DOI] [PubMed] [Google Scholar]
- 11.Bairdain S, Cleary M, Litman H, et al. Revisional bariatric surgery. J Obes Bariatrics. 2015;2:5. [Google Scholar]
- 12.Sjöström L, Lindroos AK, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351:2683–93. doi: 10.1056/NEJMoa035622. [DOI] [PubMed] [Google Scholar]
- 13.Tucker O, Sucandy I, Szomstein S, et al. Revisional surgery after failed laparoscopic adjustable gastric banding. Surg Obes Relat Dis. 2008;4:740–7. doi: 10.1016/j.soard.2008.02.008. [DOI] [PubMed] [Google Scholar]
- 14.Jones KB., Jr Revisional bariatric surgery-safe and effective. Obes Surg. 2001;11:183–9. doi: 10.1381/096089201321577857. [DOI] [PubMed] [Google Scholar]
- 15.Gagner M, Gentileschi P, de Csepel J, et al. Laparoscopic reoperative bariatric surgery: experience from 27 consecutive patients. Obes Surg. 2002;12:254–60. doi: 10.1381/096089202762552737. [DOI] [PubMed] [Google Scholar]
- 16.Lim CS, Liew V, Talbot M, et al. Revisional bariatric surgery. Obes Surg. 2009;19:827–32. doi: 10.1007/s11695-008-9750-1. [DOI] [PubMed] [Google Scholar]
- 17.Marsk R, Jonas E, Gartzios H, et al. High revision rates after laparoscopic vertical banded gastroplasty. Surg Obes Relat Dis. 2009;5:94–8. doi: 10.1016/j.soard.2008.05.011. [DOI] [PubMed] [Google Scholar]
- 18.Baker MT. The history and evolution of bariatric surgical procedures. Surg Clin North Am. 2011;91:1181–201. doi: 10.1016/j.suc.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 19.Van Gemert WG, Van Wersch M, Greve J, et al. Revisional surgery after failed vertical banded gastroplasty: restoration of vertical banded gastroplasty or conversion to gastric bypass. Obes Surg. 1998;8:21–8. doi: 10.1381/096089298765555006. [DOI] [PubMed] [Google Scholar]
- 20.MacLean LD, Rhode B, Forse R. Late results of vertical banded gastroplasty for morbid and super obesity. Surgery. 1990;107:20–7. [PubMed] [Google Scholar]
- 21.Sugerman HJ, Kellum JM, DeMaria EJ, et al. Conversion of failed or complicated vertical banded gastroplasty to gastric bypass in morbid obesity. Am J Surg. 1996;171:263–9. doi: 10.1016/S0002-9610(97)89565-7. [DOI] [PubMed] [Google Scholar]
- 22.Balsiger BM, Poggio JL, Mai J, et al. Ten and more years after vertical banded gastroplasty as primary operation for morbid obesity. J Gastrointest Surg. 2000;4:598–605. doi: 10.1016/s1091-255x(00)80108-0. [DOI] [PubMed] [Google Scholar]
- 23.Khoursheed M, Al-Bader I, Mouzannar A, et al. Sleeve gastrectomy or gastric bypass as revisional bariatric procedures: retrospective evaluation of outcomes. Surg Endosc. 2013;27:4277–83. doi: 10.1007/s00464-013-3038-9. [DOI] [PubMed] [Google Scholar]
- 24.Shimizu H, Annaberdyev S, Motamarry I, et al. Revisional bariatric surgery for unsuccessful weight loss and complications. Obes Surg. 2013;23:1766–73. doi: 10.1007/s11695-013-1012-1. [DOI] [PubMed] [Google Scholar]
- 25.Deylgat B, D’Hondt M, Pottel H, et al. Indications, safety, and feasibility of conversion of failed bariatric surgery to Roux-en-Y gastric bypass: a retrospective comparative study with primary laparoscopic Roux-en-Y gastric bypass. Surg Endosc. 2012;26:1997–2002. doi: 10.1007/s00464-011-2140-0. [DOI] [PubMed] [Google Scholar]
- 26.Vijgen GH, Schouten R, Pelzers L, et al. Revision of laparoscopic adjustable gastric banding: Success or failure? Obes Surg. 2012;22:287–92. doi: 10.1007/s11695-011-0556-1. [DOI] [PMC free article] [PubMed] [Google Scholar]