Background
Obesity is one of the most significant public health problems facing our society today. Not only do high rates of obesity contribute to soaring healthcare costs, the condition may also contribute to diminished quality of life among those affected.1 There is clear evidence of the negative impact of obesity on general health, with increased risk of some chronic diseases demonstrated in both pediatric and adult populations.2 For youth and adolescents especially, weight management efforts come at a critical time as pediatric obesity has been shown to persist into adulthood, with the prevalence of comorbid chronic disease increasing as weight gain continues over time.3,4
In 2011-2012, NHANES data indicated the nationwide prevalence of overweight and obesity among all youth aged 2-19 to be 14.9% and 16.9%, respectively.5 Recent studies suggest that the obesity rate in the population of people with intellectual disabilities (ID) may be even higher, with estimates as high as 28.9% among children aged 10-17 with ID, compared to 15.5% in typically developing children.6 Among adolescents with Down syndrome, estimates suggest that 47.8% have obesity.7 Likewise, children and adolescents with autism spectrum disorder (ASD) are at increased risk for overweight and obesity as compared with their typically-developing peers.8 Despite the elevated prevalence of obesity in these populations of children and youth, no evidence-based guidelines for weight management have been developed. Current weight-management practices for the typically developing pediatric population may be difficult to implement given the unique challenges faced by youth with ID, including food refusal, sensory issues, and cognitive and communication impairments.
To date, relatively few studies have examined the impact of nutrition and physical activity interventions on weight loss in adolescents and young adults with ID. Notably, in the 1970s and 1980s, several weight-control interventions were designed by Rotatori and colleagues and tested in the adolescent ID population.9 Although these studies had several strengths, including relatively long intervention periods and use of behavior management techniques to promote positive behavior change, they were conducted primarily among institutionalized adolescents who had limited daily exposure to the complex variety of foods seen in the community environment. More recently, two small weight loss intervention studies showed promising results. In one, Ptomey and colleagues 10 found that in a 2-month weight-loss study, adolescents with ID given a diet intervention based on the Stoplight Diet with prepackaged meals or a conventional reduced-energy diet were able to lose weight and participants were able to successfully use electronic tablets to track their food intake. In the other, researchers at the Eunice Kennedy Shriver Center, University of Massachusetts Medical School, compared two versions of a 6-month family-based weight-loss intervention (named Health U.) for teenagers with Down syndrome. Weight loss and weight maintenance were greater in the condition in which parents received training on behavioral strategies compared with a group that received education only.11 Given that today’s adolescents with ID are far more likely to live at home with family or in semi-independent settings than in institutions, they face the same everchanging food landscape filled with endless varieties of snacks, convenience foods, and sugar-sweetened beverages as the general population. Consequently, adolescents with ID need to learn how to make healthy food choices independently in a variety of situations such as choosing an afterschool snack at home, preparing food for themselves, or going out to eat with their friends.
In the aforementioned Health U. study, All participants received a Healthy Eating Plan (HEP), an individualized, calorie-based, highly visual plan that provides a framework for consuming a healthy diet and pursuing weight loss.11 The purpose of this article is to describe in detail the HEP and companion Food Guide used originally in the Health U. research study and slightly modified for use in an ongoing study with adolescents with ID. The HEP is a unique weight-loss tool created specifically for adolescents with ID.
Development
Health U began as a pilot study designed to help adolescents with intellectual disabilities lose weight, increase their physical activity, and reduce sedentary time. It takes a family-based approach in which parents or caregivers participate alongside their adolescent or young adult and learn behavioral strategies to assist him or her in losing weight and improving lifestyle habits.
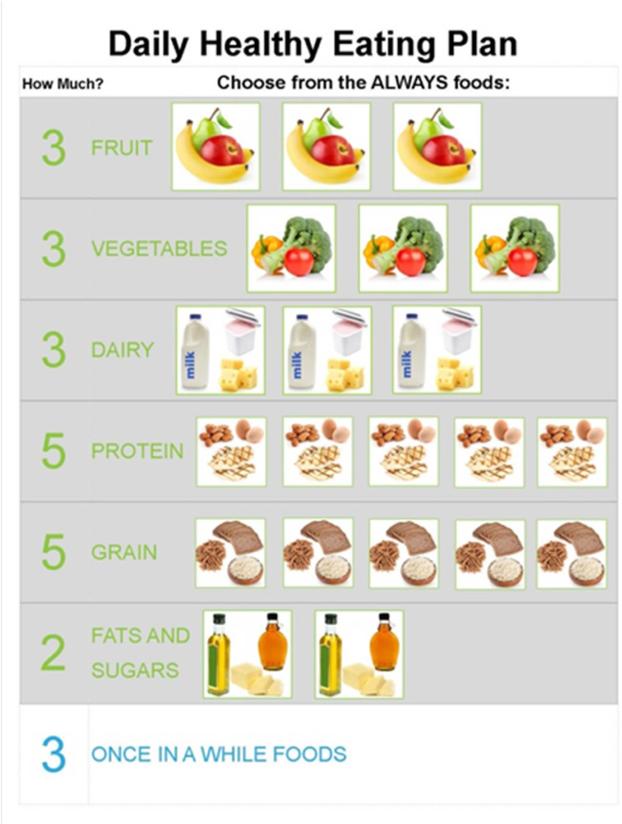
The HEP was designed to organize and simplify daily food choices for a population with limited literacy skills. It uses pictures to display the number of daily recommended servings from each food group: dairy, fruit, vegetable, protein, grain, and fat/sugar (Figure 1 – sample HEP). The HEP is designed to be nutritionally adequate while promoting gradual weight loss. HEPs are created for each individual based on their estimated daily calorie needs, calculated using the factorial approach. The Dietary Reference Intake equation was used for overweight/obese youth ≤19 years, and the Mifflin St. Jeor equation was used for young adults ≥20 years to estimate resting metabolic rate (RMR).12,13 The RMR was multiplied by an activity factor between 1.4-1.6, as determined by a brief assessment of each participant's activity level to estimate total energy expenditure (TEE). The HEP is based on the USDA Daily Food Plan (now known as MyPlate Daily Checklist) that provides recommendations for the number of daily food group servings that should be consumed to meet nutritional needs based on age, sex, and energy needs.14 Since the HEP is designed to promote gradual weight loss, a deficit of 250 calories per day was subtracted from estimated daily energy needs to promote a weight loss of approximately a ½ pound per week. Although the HEPs are calorie-based, Health U. messaging focused more simply on making healthy food choices.
Figure 1.
The Healthy Eating Plan provides individualized recommendations on the number of daily servings from each food group.
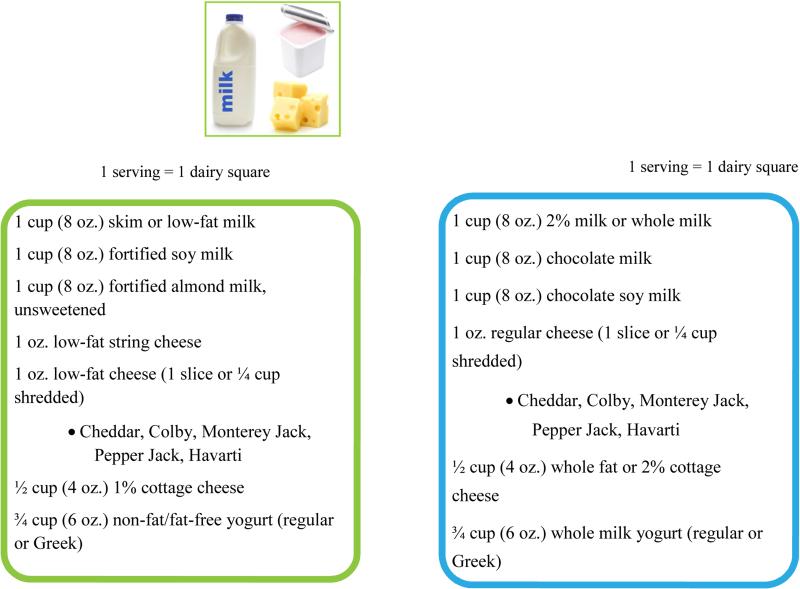
On the HEPs, each of the 6 food groups (fruits, vegetables, dairy, protein, grains and fats/sugars) is represented by a food group square of easily recognizable food items from that group. Each of the squares represents one serving from the food group. A serving size is a standard unit based on the type of food, as recommended by the USDA. For example, a serving size for grains includes 1 slice of bread or ½ cup of pasta or rice. To help guide healthy food choices and account for discretionary calories, each food group is broken down into two subgroups: always and once in a while foods. The always choices are foods that should be eaten often and contain all nutrients necessary for a nutritionally balanced diet. The once in a while foods represent choices in each food group that have more fat, calories, or added sugar, and thus should be limited to facilitate weight loss. For example, both nonfat and low-fat milk are categorized as always choices, whereas reduced fat and whole milk are considered once in a while foods since they contain more fat and calories than the lower-fat milks (Figure 2 – Dairy page from Food Guide). Each participant's HEP includes recommended servings per day from each of the food groups as well as the number of once in a while foods they can include daily from any food group. The concept of once in a while foods provides flexibility so participants are able to consume discretionary calories in moderation. The use of always and once in a while foods was a subsequent modification to the original HEP to improve clarity and choices in the use of discretionary calories.
Figure 2.
Low fat and unsweetened dairy or non-dairy alternatives are considered always choices within the dairy group. High fat or sweetened options contain more calories due to additional fat or sugar and thus are considered once in a while choices.
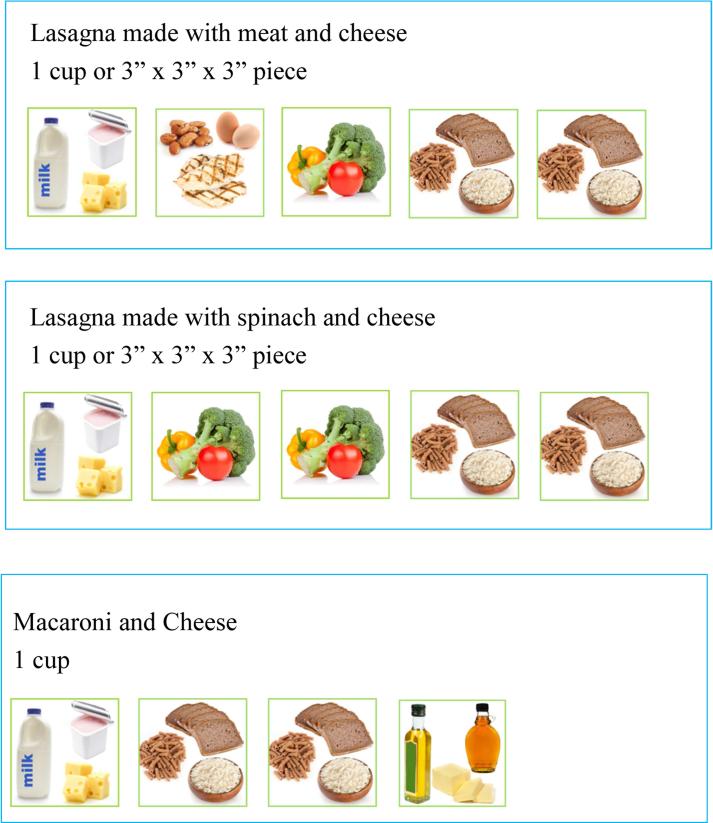
The Food Guide is a companion handbook to the HEP, designed to help parents and participants better understand food choices and serving sizes, and to guide their meal planning and management of portions. The Food Guide is organized by food group, and serving sizes are listed for common foods with many examples of always and once in a while foods in each group. Mixed dishes such as pizza, lasagna, or burritos may pose a challenge in determining which food groups are represented in a serving. Examples of common mixed dishes are listed in the Food Guide to help individuals determine how to break down the components of these dishes into the appropriate food group squares (Figure 3- Mixed Dishes).
Figure 3.
Examples shown in the Food Guide provide guidance on how to determine the food groups contained in common mixed dishes.
While once in a while foods are choices that contain more fat or sugar but still fit into a food group, treats are foods that include desserts, sugar-sweetened beverages, and salty snacks such as chips. The HEP incorporates a weekly budget of calories that may be used for treats. The allowance of weekly treats provides flexibility, encourages planning ahead, and offers a realistic approach to help individuals understand how treats can fit into a healthy diet. In creating the HEPs, 57 calories per day was allotted to each individual's daily plan to allow for 400 calories per week to be allocated as treats. The HEP uses coins to illustrate the concept of a weekly treat budget. Each week, participants have 8 coins (1 coin = 50 calories) to use on whichever treat food(s) they prefer. Participants can choose how they would like to use their coins each week; they can use them all at once, or they may choose to exchange them for smaller treats throughout the week. There are many examples included in the Food Guide and parents are given the formula to determine how many coins are in treats or desserts not listed in the Food Guide. (Table 1 – Coins/Treats).
Table 1.
Treats and corresponding coin values
| DRINKS | COINS |
|---|---|
| Gatorade (12 oz) | 2 |
| Vitamin Water (20oz bottle) | 2 |
| Sweetened ice tea or lemonade (12 oz) | 3 |
| Soda (12 oz) | 3 |
| Dunkin Donuts Coolatta (12 oz) | 6 |
| DESSERTS | |
| Chocolate sandwich cookie (e.g. 1 Oreo) | 1 |
| Fruit popsicle (Edy's real fruit bar) | 1 |
| Rice crispy treat (2” cube) | 2 |
| Sorbet/frozen yogurt (½ cup) | 2 |
| Ice cream (½ cup) | 3 |
| Ice cream sandwich (2 oz- e.g. Good Humor) | 3 |
| Large cookie (2 ½”) | 5 |
| Candy (1 bar or package) | 5 |
| Chipwich or Klondike bar | 5 |
| Cupcake (2”) with frosting | 6 |
Challenges
While we believe that the HEP is an extremely useful weight loss tool, it is not without limitations. The HEP was created for use within the Health U intervention, but has not yet been used outside a multi-component treatment program. Within the Health U group intervention, parents received training and guidance in weekly goal setting and behavioral strategies to help their teens meet the target servings of each food group on their specific HEP. However, based on our experiences, we believe the HEP could be adapted for use in a clinical setting where effective weight loss tools designed for individuals with ID are lacking. Under the guidance of a registered dietitian nutritionist (RDN), families could receive training to understand the concepts of serving size, healthy food choices, and use of coins to represent treats. Regular meetings with an RDN would follow, to help families implement gradual dietary changes specified in their HEPs, monitor successes, and address challenges to continued weight loss and accomplishment of healthy eating goals.
Distinguishing between always and once in a while foods was a challenge in the development of the HEP, as the diversity of food products available in today's food environment can make categorizing food choices difficult. Since our focus was on calories, we kept choices like white bread and pasta in the always category since the calories are very similar to whole grain choices. However, nutrition education was focused on making the healthiest choices in each food group and thus we stressed the benefits of choosing whole grains over white grains. In a few cases, we made the decision to take nutritional quality into account, particularly in foods rich in healthy unsaturated fats. For example, although higher in calories than other always choices within the same food group, avocados, nuts, and nut butters are listed as always choices. The decision to include some higher calorie foods and unsaturated fats in the always categories was based on the premise that these foods are an important part of a healthy diet. However, since these foods have a higher caloric content than other foods in the always category, additional counseling on portion sizes and variety is needed to ensure that participants are not exceeding their recommended calorie limits. This highlights the importance of implementing the HEP under the guidance of an RDN.
The always and once in a while categories contain a range of foods with varying calorie levels, so while on average the always foods contain fewer calories than the once in a while choices, it is not an exact science. The categories are meant to serve as a guide to participants and parents to help influence food choices and direct them towards the lower calorie, more nutrient-dense choices. If the HEP and Food Guide are adapted for different populations, RDNs could make different decisions about how to categorize always vs. once in a while foods. Since not all foods could be included in the Food Guide, calories per serving of the always and once in a while choices in each food group were averaged to provide a reference for parents or participants to use if they came across a food not listed in the Food Guide. The Food Guide was created for participants in the Health U intervention, which did not comprise an ethnically diverse sample. For this reason, the Food Guide does not include a wide range of ethnic food options. That said, we believe that RDNs could modify the Food Guide to list more culturally appropriate and ethnically diverse foods to meet the needs of the population for which it is being used.
Implementing Healthy Eating Plans with Adolescents and Families
The implementation of the HEP is a gradual process. In the Health U study, parents attended a training session where the HEP was introduced and they are given the opportunity to practice using the HEP to plan their adolescents’ meals, before the start of the program.9 The RDN provides training for parents on both the HEP and the Food Guide, including a review of serving sizes, differences between always and once in a while foods, and the concept of using coins to represent treats. Implementation of the HEP is similar to many weight loss approaches in that it is important that an RDN work with the individual and family using motivational interviewing techniques, such as reflective listening and assessing readiness to change, to help determine what changes they are ready and able to make. Caregivers or participants (if able) are asked to monitor or track their daily intake to monitor progress and adherence to their HEP. Gradual progress is the goal; participants are not expected to be able to meet the recommendations of their HEP immediately, but they are encouraged to use the HEP as the means to achieving long-term goals. Education and counseling are geared toward caregivers at first, as they are responsible for driving behavior changes initially. However, the longer term objective of an RDN working with the family is to help the participant with ID to develop a good understanding of their HEP along with an improved ability to make healthy choices and stick to their goals without parental supervision.
Clinical Applications
Teaching clients, or in our case research participants, about healthy food choices as part of implementing a weight loss plan has become increasingly challenging with the vast and complex food choices available in today's food environment. The HEP is a simplified, visually-based weight loss and healthy eating tool that has many strengths, particularly for use by individuals with ID. By focusing on food groups instead of calories, we aim to promote the importance of dietary variety and inclusion of servings from all food groups daily. The HEP provides individuals with a concrete means for working towards short- and long-term goals, which can be particularly beneficial for teens and young adults with ID who respond well to structure and routine. Although structured, the HEP also leaves room for flexibility in use of discretionary calories and treats, which helps make it a realistic and sustainable weight loss tool. The effectiveness of the HEP and Food Guide as components of the larger Health U program have not been evaluated separately; however, participants and families have responded to both with very positive feedback. As noted, an earlier version of the HEP was used in the Health U pilot study, completed in 2010.11 In that study all participants received individualized HEPs. One group of families received only nutrition education and a second group of families received nutrition education supplemented with behavioral training. Behavioral training included goal-setting and reinforcement techniques to promote and reinforce adherence to the HEP. The nutrition education plus behavioral group had significantly greater weight loss that was sustained at 12 months.11 This and other research suggests that behavioral supports are needed to bolster adherence to nutritional tools such as the HEP.
Conclusions
Existing evidence-based guidelines for healthy eating, including My Plate, are useful for improving eating habits in the general population. However, tools to support healthy eating and weight loss that are adapted to meet the needs of individuals with ID are lacking. The HEP is based on the USDA Dietary Guidelines, but includes visual representations of food groups for populations with limited literacy skills. It offers simplified guidance about the daily number of recommended servings from each food group, and designates the healthiest choices within each food group in a visual format. We believe that the HEP is a uniquely adapted tool for adolescents and young adults with ID that can help improve dietary choices and aid in weight loss under the guidance of an RDN and program of behavioral support. Further research is needed to test the effectiveness and acceptance of the HEP outside of the Health U group program in a clinical setting.
Acknowledgements
The authors thank Nicole Collins, MPH, RDN for her contributions in the development and revision of the Healthy Eating Plans and Food Guide.
Funding Disclosure
Supported by the National Institutes of Health (R01 HD072573 and DK070627), the Maternal and Child Health Bureau (MCJ259631 and UA3MC25735-01-00), the John W. Alden Trust, and IDDRC 2P30HD004147.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Maresa Weems, E.K. Shriver Center, UMass Medical School, 55 Lake Ave North, S3-324B, Worcester, MA 01655, maresa.weems@umassmed.edu.
Laura Truex, E.K. Shriver Center, UMass Medical School, 55 Lake Ave North, S3-324B, Worcester, MA 01655, laura.truex@umassmed.edu, 774-455-6526.
Renee Scampini, University of Wisconsin-Milwaukee, Urban Studies Programs, 3210 N Maryland Ave, Milwaukee, WI 53211, scampin2@uwm.edu, 617-594-4787.
Richard Fleming, Department of Exercise and Health Sciences, University of Massachusetts Boston, 100 Morrissey Boulevard, Boston, MA 02125-3393, Richard.fleming@umb.edu, 774-455-6530.
Carol Curtin, E.K. Shriver Center, UMass Medical School, Dept. of Family Medicine & Community Health, 55 Lake Ave North, S3-324B, Worcester, MA 01655, carol.curtin@umassmed.edu, 774-455-6527.
Linda Bandini, E.K. Shriver Center, UMass Medical School, 55 Lake Ave North, S3-324B, Worcester, MA and Department of Health Science, Boston University, 635 Commonwealth Ave, Boston, MA 02215, linda.bandini@umassmed.edu.
References
- 1.Ul-Haq Z, Mackay DF, Fenwick E, Pell JP. Meta-analysis of the association between body mass index and health-related quality of life among adults, assessed by the SF-36. Obesity. Mar. 2013;21(3):E322–7. doi: 10.1002/oby.20107. [DOI] [PubMed] [Google Scholar]
- 2.Reilly JJ, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: a systematic review. Int J Obesity. 2011;35(7):891–898. doi: 10.1038/ijo.2010.222. [DOI] [PubMed] [Google Scholar]
- 3.Serdula MK, Ivery D, Coates RJ, Freedman DS, Williamson DF, Byers T. Do obese children become obese adults? A review of the literature. Prev Med. 1993;22:167–177. doi: 10.1006/pmed.1993.1014. [DOI] [PubMed] [Google Scholar]
- 4.Reilly JJ, Methven E, McDowell ZC, Hacking B, Alexander D, Stewart L, Kelnar CJ. Health consequences of obesity. Arch Dis Child. 2003;88:748–752. doi: 10.1136/adc.88.9.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Segal M, Eliasziw M, Phillips S, et al. Intellectual disability is associated with increased risk for obesity in a nationally representative sample of U.S. children. Disability and Health. 2015 Dec 17; doi: 10.1016/j.dhjo.2015.12.003. ISSN 1936-6574, http://dx.doi.org/10.1016/j.dhjo.2015.12.003. [DOI] [PMC free article] [PubMed]
- 7.Basil JS, Santoro SL, Martin LJ, Healy KW, Chini BA, Saal HM. Retrospective study of obesity in children with Down syndrome. J Pediatr. 2016 Mar 14; doi: 10.1016/j.jpeds.2016.02.046. pii: S0022-3476(16)00268-7. doi: 10.1016/j.jpeds.2016.02.046. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 8.Curtin C, Jojic M, Bandini LG. Obesity in children with autism spectrum disorder. Harvard Review of Psychiatry. 2014;22(2):93–103. doi: 10.1097/HRP.0000000000000031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rotatori A, Switzky H, Fox R. Behavioral weight reduction procedures for obese mentally retarded individuals: a review. Mental Retardation. 1981;19(4):157–161. [PubMed] [Google Scholar]
- 10.Ptomey LT, Sullivan DK, Lee J, Goetz JR, Gibson C, Donnelly JE. The use of technology for delivering a weight loss program for adolescents with intellectual and developmental disabilities. J Acad Nutr Diet. 2015;115(1):112–118. doi: 10.1016/j.jand.2014.08.031. [DOI] [PubMed] [Google Scholar]
- 11.Curtin C, Bandini LG, Must A, Gleason J, Lividini K, Phillips S, Eliasziw M, Maslin M, Fleming RK. Parent support improves weight loss in adolescents and young adults with Down syndrome. J Pediatr. 2013;163(5):1402–8. e1. doi: 10.1016/j.jpeds.2013.06.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Institute of Medicine . Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients) The National Academies Press; Washington, DC: 2005. doi:10.17226/10490. [Google Scholar]
- 13.Mifflin MD, St Jeor ST, Hill LA, Scott BJ, Daugherty SA, Koh YO. A new predictive equation for resting energy expenditure in healthy individuals. Am J Clin Nutr. 1990;51:2, 241–7. doi: 10.1093/ajcn/51.2.241. [DOI] [PubMed] [Google Scholar]
- 14.US Dept. of Agriculture . ChooseMyPlate.Gov Website. MyPlate Daily Checklist; Washington, DC: [March 22, 2016]. http://www.choosemyplate.gov/MyPlate-Daily-Checklist. Updated Febuary 8th, 2016. [Google Scholar]