Abstract
The worldwide population is aging, and the number of surgeries performed in geriatric patients is increasing. This systematic review evaluated anesthetic procedures to assess global data on perioperative and anesthesia-related cardiac arrest (CA) rates in geriatric surgical patients. Available data on perioperative and anesthesia-related CA rates over time and by the country’s Human Development Index (HDI) were evaluated by meta-regression, and a pooled analysis of proportions was used to compare perioperative and anesthesia-related CA rates by HDI and time period. The meta-regression showed that perioperative CA rates did not change significantly over time or by HDI, whereas anesthesia-related CA rates decreased over time (P = 0.04) and in high-HDI (P = 0.015). Perioperative and anesthesia-related CA rates per 10,000 anesthetic procedures declined in high-HDI, from 38.6 before the 1990s to 7.7 from 1990–2017 (P < 0.001) and from 9.2 before the 1990s to 1.3 from 1990–2017 (P < 0.001), respectively. The perioperative CA rate from 1990–2017 was higher in low-HDI than in high-HDI countries (P < 0.001). Hence, a reduction in anesthesia-related CA rates over time was observed. Both perioperative and anesthesia-related CA rates only decreased with a high-HDI between time periods, and perioperative CA rates during 1990–2017 were 4-fold higher with low- compared to high-HDI in geriatric patients.
Introduction
The number of elderly individuals is increasing more rapidly than that of other age groups1. By 2050, the number of people aged 60 years old and older is expected to be 2 billion, whereas it was 900 million in 20152. Therefore, the number of geriatric patients who undergo anesthetic and surgical procedures will continue to increase. Additionally, the elderly experience a higher incidence of perioperative cardiac arrest (CA) than other adult age groups3–10.
Perioperative and anesthesia-related CA rates may be good indicators that can be used to analyze a country’s socioeconomic and health development over time, and it is advisable to explore the differences between hospital facilities for anesthetic and surgical procedures across different countries11, 12. A country’s developmental status is assigned by the Human Development Index (HDI)13, a national development status index based on enrollment in higher education, literacy, per-capita income, and life expectancy. As previously described14, 15, high- and low-income countries are defined as those having an HDI ≥ 0.8 and <0.8, respectively. A previous meta-analysis including patients in all age groups revealed a decreased in the risk of both perioperative and anesthesia-related mortality rates over the last five decades, especially in high-HDI countries14. A recent systematic review involving patients in all age groups employed meta-analysis to show that there was a reduction in perioperative and anesthesia-related CA rates in high-income countries and an increase in perioperative CA rates, but with no change in the anesthesia-related CA procedures, in low-income countries when comparing pre-1990s with 1990–201415. In this aforementioned study, anesthesia-related and perioperative CA rates were found to be reduced with increasing HDI status but not with time by meta-regression analysis.
Although there is a consensus that anesthesia and surgery are now safer than they were in the past and that more geriatric patients are undergoing these procedures16, no systematic review using meta-regression and regarding worldwide rates of perioperative and anesthesia-related CA events in geriatric patients is available in the literature. We hypothesized that perioperative and anesthesia-related CA rates have decreased over time in high- and low-HDI countries by performing a weighted meta-regression and weighted CA rates for geriatric patients published in cohort and cross-sectional studies.
The current study aimed to perform the first meta-regression analysis of the worldwide data on perioperative and anesthesia-related CA rates in geriatric patients over time and according to national HDI values. Additionally, we examined pooled weighted CA rates of perioperative and anesthesia-related CA events in low- and high-HDI countries during the pre-1990s and the 1990–2017 period.
Results
Selection of studies
Our literature search yielded 20,074 citations in addition to 71 potential studies that were identified in the references of related articles. We excluded 2,648 duplicate studies, and after reviewing the titles and abstracts, we retrieved 290 potentially relevant full-text articles for more detailed evaluation. Of these articles, 16 studies met the inclusion criteria (Fig. 1).
Figure 1.
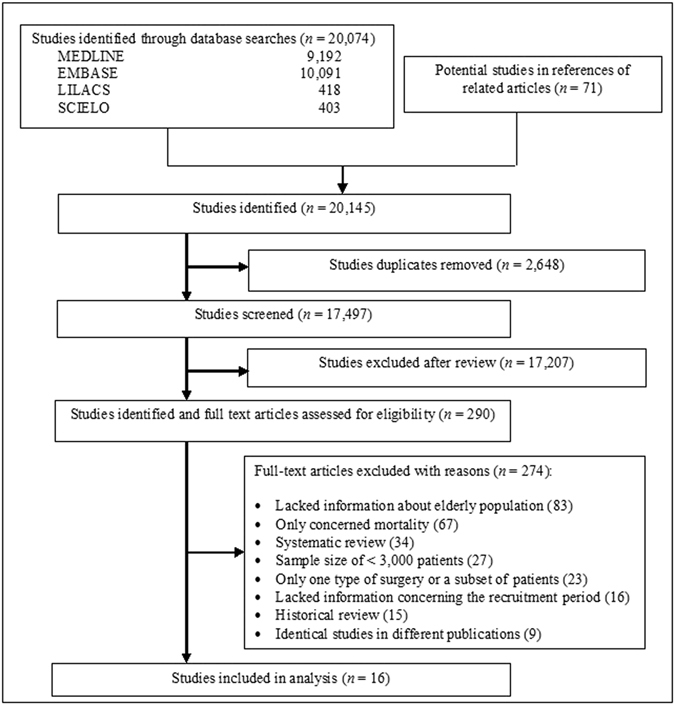
Flowchart of the process used to identify studies for inclusion.
Study characteristics
Sixteen studies from nine countries fulfilled the inclusion criteria. These studies involved 1,758,153 anesthetic procedures performed during surgery in geriatric patients. The characteristics and designs of these studies are listed in Table 1.
Table 1.
Characteristics of included studies with references.
| Investigator and year of publication | Data source and study period | Median year | HDI average | Primary outcome | Weight % | Cardiac arrest | Patients | Excluded | Age group included |
|---|---|---|---|---|---|---|---|---|---|
| Ahmed et al.39 2008 | Single University Hospital Audit – Pakistan 1992–2006 | 1999 | 0.527 | Cardiac arrest in OR and PACU | 1: 20.3 | 1: 14 | 32,742 | Cardiac surgery | ≥60 years |
| Aubas et al.3 1991 | Single University Hospital Chart review – France 1983-1987 | 1985 | 0.974 | Cardiac arrest in OR and PACU | 2: 21.3 | 2: 8 | 8,432 | — | ≥75 years |
| Biboulet et al.4 2001 | Single University Hospital Database – France 1989–1995 | 1992 | 0.960 | Cardiac arrest within 12 hours | 2: 7.5 | 2: 4 | 7,544 | ASA V patients | ≥75 years |
| Braz et al.40 1999 | Tertiary University Hospital Database – Brazil 1988–1996 | 1992 | 0.759 | Cardiac arrest in OR and PACU | 1: 19.7 | 1: 35 | 6,982 | — | ≥65 years |
| Braz et al.7 2006 | Tertiary University Hospital Database – Brazil 1996–2005 | 2001 | 0.767 | Cardiac arrest in OR and PACU | 1: 19.7, 2: 27 | 1: 48, 2: 4 | 6,796 | — | ≥65 years |
| Dam & Vimtrup31 1967 | Single Hospital Database – Denmark 1955–1965 | 1960 | 0.971 | Cardiac arrest in OR | 1: 25.0 | 1: 14 | 12,737 | — | ≥70 years |
| Deiner et al.10 2014 | Multicentric - University and Community Hospitals Database – USA 2010–2013 | 2012 | 0.908 | Cardiac arrest within 48 hours | 1: 25.6 | 1: 557 | 972,505 | — | ≥65 years |
| Fiscella et al.41 1991 | Single Private Hospital Prospective survey – Argentina 1980–1990 | 1985 | 0.953 | Cardiac arrest within 24 hours | 1: 24.5 | 1: 15 | 5,473 | — | > 60 years |
| Goswami et al.8 2012 | Multicentric - 304 Hospitals Prospective survey – USA 2005–2007 | 2006 | 0.953 | Cardiac arrest in OR | 1: 24.0 | 1: 130 | 80,834 | Cardiac surgery Trauma cases | ≥70 years |
| Kawashima et al.6 2002 | Multicentric - 467 Hospitals Questionnaire – Japan 1999 | 1999 | 0.928 | Cardiac arrest within 7 days | 1: 25.1, 2: 45.2 | 1: 224, 2: 21 | 208,568 | — | > 65 years |
| Kubota et al.42 1994 | Tertiary University Hospital Database – Japan 1962–1992 | 1977 | 0.989 | Cardiac arrest in OR | 1: 25.1 | 1: 1 | 15,351 | Cardiac surgery, Organ transplantation | ≥65 years |
| Morita et al.43 2002 | Multicentric - 536 Hospitals Questionnaire – Japan 2000 | 2000 | 0.933 | Cardiac arrest within 7 days | 1: 25.2, 2: 47.3 | 1: 282, 2: 22 | 272,734 | — | ≥65 years |
| *Nunes et al.16 2014 | Tertiary University Hospital Database - Brazi1 1996–2010 | 2003 | 0.716 | Cardiac arrest in OR and PACU | 1: 20.2, 2: 73.0 | 1: 100, 2: 6 | 18,367 | — | ≥60 years |
| Olsson & Hallén5 1988 | Single Hospital Database – Sweden 1976–1984 | 1980 | 0.987 | Cardiac arrest in OR | 2: 40.8 | 2: 43 | 60,563 | — | > 60 years |
| Otteni et al.44 1986 | Multicentic - 460 Hospitals Prospective survey – France 1978–1982 | 1980 | 0.974 | Cardiac arrest within 24 hours | 1: 25.3, 2: 37.8 | 1: 252, 2: 50 | 39,620 | — | ≥60 years |
| *Tamdee et al.17 2009 | Single University Hospital Database – Thailand 2003–2007 | 2005 | 0.780 | Cardiac arrest within 24 hours | 1: 19.9 | 1: 36 | 8,905 | Cardiac surgery | ≥65 years |
Abbreviations. HDI: Human Development Index, the score ranges from 0 to 1, which represents the lowest and highest levels of development, respectively; OR: operating room; PACU: postanesthesia care unit; Weight (%): study weight contribution to the pooled analysis of the proportion effect size; 1: perioperative cardiac arrest; 2: anesthesia-related cardiac arrest; *Studies that included only geriatric patients.
Meta-regression analysis
Of the evaluated studies (n = 16), 13 were related to perioperative CA (Figs 2 and 3), and eight were related to anesthesia-related CA (Figs 4 and 5).
Figure 2.
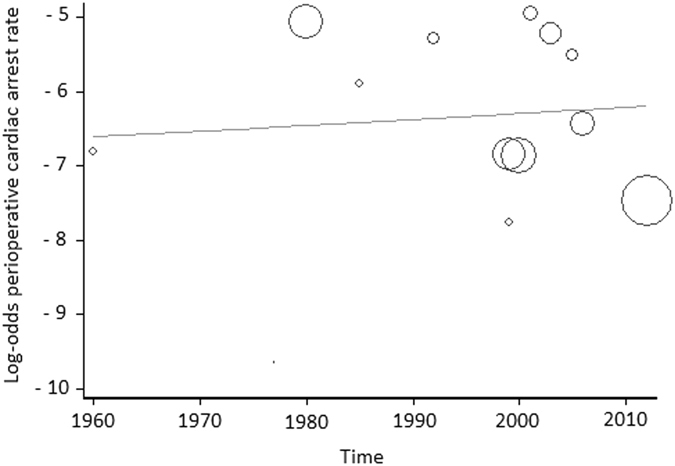
Meta-regression of perioperative cardiac arrest rates according to time. Each circle represents a study and indicates its weight in the analysis. The correlation between perioperative cardiac arrests and time was not significant (slope: 0.0079; 95% CI: −0.0483 to 0.0642; P = 0.76).
Figure 3.
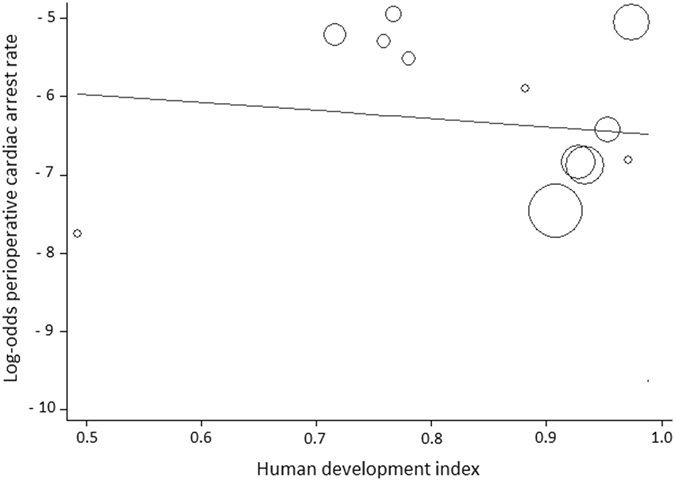
Meta-regression analysis of perioperative cardiac arrest rates according to Human Development Index (HDI) status. Each circle represents a study and indicates its weight in the analysis. The correlation between perioperative cardiac arrests and HDI was not significant (slope: −1.0389; 95% CI: −6.7380 to 4.6601; P = 0.69).
Figure 4.
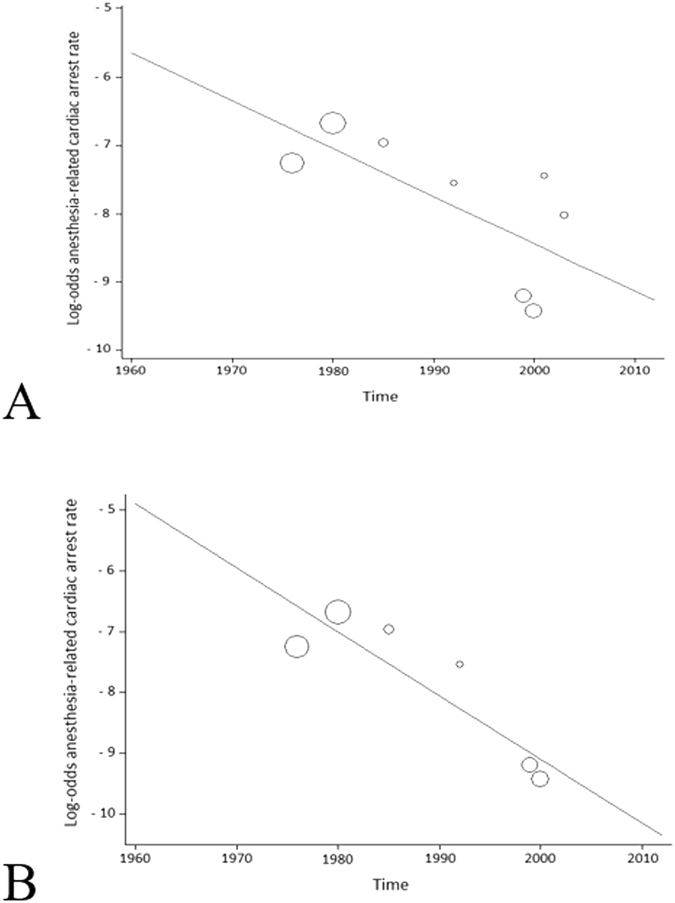
Meta-regression of anesthesia-related cardiac arrest rates according to time. Each circle represents a study and indicates its weight in the analysis. (A) The correlation between anesthesia-related cardiac arrests and time was significant considering both low- and high-HDI countries (slope: −0.0699; 95% CI: −0.1394 to −0.0003; P = 0.04). (B) The correlation between anesthesia-related cardiac arrests and time was significant in only high-HDI countries (slope: −0.1049; 95% CI: −0.1762 to −0.0336; P = 0.015).
Figure 5.
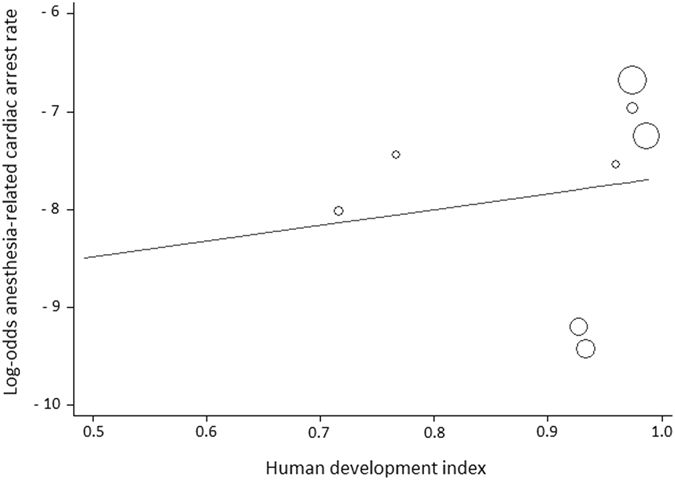
Meta-regression analysis of anesthesia-related cardiac arrest rates according to Human Development Index (HDI) status. Each circle represents a study and indicates its weight in the analysis. The correlation between anesthesia-related cardiac arrests and HDI was not significant (slope: 1.6188; 95% CI: −8.6021 to 11.8399; P = 0.71).
Time (study year)
The data from all of countries assessed in the weighted meta-regression showed no statistically significant relationship between perioperative CA and time (slope: 0.0079; 95% CI: −0.0483 to 0.0642; P = 0.76; Fig. 2). However, there was a significant decrease in the anesthesia-related CA rate over time, regardless of HDI status (slope: −0.0699; 95% CI: −0.1394 to −0.0003; P = 0.04; Fig. 4A). There was also a significant decrease in this rate over time in high-HDI countries (slope: −0.1049; 95% CI: −0.1762 to −0.0336; P = 0.015; Fig. 4B). Correlation between anesthesia-related CA rates and time was not calculated for low-HDI countries because these rates were described in only two articles, which made the meta-regression analysis impossible.
HDI status
The weighted meta-regression analysis revealed no relation between the perioperative CA rate and HDI status (slope: −1.0389; 95% CI: −6.7380 to 4.6601; P = 0.69; Fig. 3). Similarly, there was no significant correlation between the anesthesia-related CA rate and a country’s HDI (slope: 1.6188; 95% CI: −8.6021 to 11.8399; P = 0.71; Fig. 5).
Pooled weighted analysis of CA rate
When we compared studies to determine whether a country’s HDI status had an effect on CA events during the two evaluated time periods (pre-1990s versus 1990–2017), we found that in high-HDI countries, perioperative CA rates decreased from 38.6 (95% CI: 37.8–39.6) per 10,000 procedures before the 1990s to 7.7 (95% CI: 7.6–7.8) per 10,000 procedures in 1990–2017 (P < 0.001); anesthesia-related CA rates decreased from 9.2 (95% CI: 8.9–9.5) per 10,000 procedures before the 1990s to 1.3 (95% CI: 0.2–6.5) per 10,000 procedures in the 1990–2017 (P < 0.001; Table 2). None of the studies evaluated perioperative or anesthesia-related CA rates in low-income countries before the 1990s, making sub-analysis of data for these periods impossible.
Table 2.
Perioperative and anesthesia-related cardiac arrests by time period and by human development index (HDI) status.
| Studies | I 2 | Events | Patients | Pooled weighted event rate per 10,000 anesthetic procedures (95% CI) | P Value for Subgroup | |||
|---|---|---|---|---|---|---|---|---|
| High- vs low-HDI | High-HDI per time period* | Low-HDI per time period* | ||||||
| Perioperative cardiac arrest | ||||||||
| Pre-1990s | 4 | 282 | 73,181 | NA | ||||
| High-HDI | 4 | 98.9 | 282 | 73,181 | 38.6 (37.8–39.6) | <0.001 | ||
| Low-HDI | NR | NR | NR | NR | NR | NA | ||
| 1990–2017 | 9 | 1,426 | 1,608,433 | <0.001 | ||||
| High-HDI | 4 | 98.0 | 1,193 | 1,534,641 | 7.7 (7.6–7.8) | |||
| Low-HDI | 5 | 98.0 | 233 | 73,792 | 31.3 (30.4–32.2) | |||
| Anesthesia-related cardiac arrest | ||||||||
| Pre-1990s | 3 | 101 | 108,615 | NA | ||||
| High-HDI | 3 | 73.9 | 101 | 108,615 | 9.2 (8.9–9.5) | <0.001 | ||
| Low-HDI | NR | NR | NR | NR | NR | NA | ||
| 1990–2017 | 5 | 57 | 514,009 | 0.57 | ||||
| High-HDI | 3 | 71.8 | 47 | 488,846 | 1.3 (0.2–6.5) | |||
| Low-HDI | 2 | NA | 10 | 25,163 | 4.6 (0.1–264.9) | |||
Abbreviations. I 2: heterogeneity among studies; CI: confidence interval; NR: not reported; NA: not available; vs: versus; *Pre-1990s versus 1990–2017.
In the period from 1990 to 2017, perioperative CA rates were 4-fold lower in high-HDI countries [7.7 per 10,000 procedures (95% CI: 7.6–7.8)] than in low-HDI countries [31.3 per 10,000 procedures (95% CI: 30.4–32.2; P < 0.001; Table 2)], though there were no significant differences between low- [4.6 per 10,000 procedures (95% CI: 0.1–264.9)] and high-HDI countries [1.3 per 10,000 procedures (95% CI: 0.2–6.5; P = 0.57; Table 2)] concerning anesthesia-related CA rates.
For all event rates, the proportion of heterogeneity (I 2) varied from 71.8% to 98.9% (Table 2).
Discussion
In this systematic review of surgeries in geriatric patients, we used meta-regression analysis to show that perioperative CA rates did not change over time or with regard to HDI status; in contrast, anesthesia-related CA rates did significantly decrease over time but not according to HDI status. In addition, by using the pooled weighted CA rate analyses, we found that both perioperative and anesthesia-related CA rates were lower in high-HDI countries in the later time period. However, it was not possible to analyze changes in these event rates in the low-HDI countries because there was a lack of published studies covering the period before the 1990s. During the 1990–2017 period, perioperative CA rates were 4-fold lower in high-HDI than in low-HDI countries.
Based on these findings, the following question arose: Why did perioperative CA rates not decline over time or by HDI status in geriatric patients? A previous meta-regression analysis of data obtained from a systematic review of anesthesia-related and perioperative mortalities in high- and low-income countries showed that the baseline American Society of Anesthesiologists (ASA) physical status of patients has increased significantly in recent decades14. In the same study, meta-regression by ASA status was performed to evaluate CA events and deaths, and a significantly increasing relationship was found between a higher ASA status at baseline and CA events or deaths14. Additionally, studies evaluating low- and high-HDI countries have demonstrated that geriatric patients who present a poorer ASA physical status (III–V) are more likely than ASA I–II patients to suffer perioperative CA or death16–19.
Elderly individuals are more predisposed than young people to cardiovascular disease. For example, a ruptured aneurysm or complications associated with cardiac surgery or intraoperative myocardial infarction are important causes of intraoperative CA and death in geriatric patients16. Therefore, the baseline risk for and complexity of managing geriatric patients undergoing surgery are both increased. Geriatric patients, many of whom are frail, can experience considerable comorbidities and cognitive impairment and have reduced physical activity, all of which are associated with perioperative complications20. These factors are thought to contribute to the significant increasing correlation between perioperative CA rates and time. However, we found no significant change in this relationship, possibly indicating that increased perioperative safety measures are implemented with regard to geriatric patients.
The significant reduction we observed in anesthesia-related CA rates over time may be associated with considerable improvements in anesthesia safety since the early 1990s, especially in high-HDI countries. We can also attribute this finding to several safety improvements, such as advancement in drugs, training programs, guidelines and checklists, investments in monitoring techniques, especially the capnograph and pulse oximeter, and systematic approaches to reduce errors21–23. According to Eichhorn, these initiatives, which are aimed at achieving “safety monitoring”, have resulted in a continuous increase in intraoperative vigilance and improved patient safety during anesthesia24. In our study, the relationship between anesthesia-related CA rates and time could not be evaluated in low-income countries because only two relevant articles were identified. This made performing meta-regression analysis using these data impossible.
The results of our pooled weighted CA rate analyses, which were divided into HDI status and time period, demonstrated the existence of a considerable gap between the healthcare systems of low- and high-income countries. For example, in high-HDI countries, there were significant 5- and 7-fold reductions in perioperative and anesthesia-related CA rates, respectively, between the two time periods. Additionally, our study showed that the perioperative CA rate was 4-fold lower in high-HDI than in low-HDI countries from 1990 to 2017. Although the anesthesia-related CA rate was also 3.5-fold higher in low-HDI countries than in high-HDI countries during this period, this difference was not significant. Regardless, this result may have been influenced by the relatively small number of both studies and patients that were identified for low-HDI countries.
Several studies have highlighted the major role that pre-anesthetic management of a patient’s condition plays in minimizing complications and adverse outcomes18, 25–28. One study performed in a low-income country showed that several geriatric patients have poor health when undergoing surgery16. These findings demonstrate that there is a need for improving the quality and quantity of resources that can be used as well as access to healthcare, both of which are inadequate, in developing countries. Additionally, it is necessary to adopt perioperative medical practices that have demonstrable effectiveness, to organize multidisciplinary discussions of adverse effects, to implement evidence-based safety protocols, to provide better methods for selecting patients for surgery, and to initiate advances in techniques, protocols, and pre- and postoperative critical care to improve perioperative patient care29, 30.
There are some data limitations in the current study. One of the main limitations is that several papers were excluded from the review due to the lack of information about both the numbers of geriatric patients and the patients who developed CA in this specific age group. Additionally, many of the included papers presented different age group subdivisions, including both adult and geriatric patients who developed CA (50–698; 15–6931; 55–74 years3, 4); this only enabled the inclusion and analysis of patients ≥70 or ≥75 years, respectively, in the aforementioned studies. There were also differences across the included studies regarding surgical populations (e.g., excluded ASA V patients), time frames (e.g., intraoperative, 24 hours or 48 hours postoperatively, or seven postoperative days), and procedures (e.g., exclusion of organ transplantation, trauma, or cardiac surgery). Accordingly, these differences contributed to the high heterogeneity observed in our study. A random-effects model was applied to minimize this heterogeneity when assessing trends between the two time periods and the two HDI status categories. In addition to including ≥3,000 geriatric patients, we also calculated the weighted rate of CA events across all studies to minimize possible bias. The last limitation is that there were no pre-1990s studies performed in low-income countries that either fulfilled the inclusion criteria or were not published in an indexed journal, and the absence of such studies may have contributed to publication bias.
We evaluated a public health problem that is associated with the geriatric population. This age group experiences a considerable number of diseases and functional dependencies that contribute to higher health system costs and a substantial impact on economic, social, and family dynamics32. It is therefore necessary to expand and intensify our research into aging and evidence-based medicine to provide better geriatric care in high-HDI and, in particular, low-HDI countries33. Indeed, there is a large disparity between the healthcare systems of these countries, and our study showed that improvements have been made in geriatric patient safety care during anesthetic procedures in high- but not in low-income countries. As explained by Koga et al., future efforts and collaborations should involve improvements in perioperative safety to reduce the gap between high- and low-HDI countries in their respective health care systems15. Further reviews of perioperative and especially anesthesia-related CA must be periodically performed to obtain continued worldwide CA rates in geriatric patients in low- and high-HDI countries. We also showed that there was a decrease in anesthesia-related CA rates over time while there was an increase in the size of the geriatric population and the associated number of comorbidities.
In conclusion, our meta-regression analysis shows that perioperative CA rates did not change over time or based on a country’s HDI; conversely, anesthesia-related CA rates decreased over time but not according to HDI. By using pooled weighted CA rate analyses, a notable reduction in perioperative and anesthesia-related CA rates between the two time periods was observed in high-HDI countries. In addition, perioperative CA rates were 4-fold lower in high- than in low-income countries during the 1990–2017 period.
Methods
This manuscript was prepared in accordance with Meta-analyses Of Observational Studies in Epidemiology statements (MOOSE)34. According to the local institutional review board (IRB), there was no need for Ethical approval due to the type of study.
Search Strategy and Inclusion and Exclusion Criteria
The following databases were searched until April 2nd, 2017: EMBASE, MEDLINE, LILACS, and SCIELO. Additionally, we manually reviewed all potential studies and included relevant articles. No restrictions were applied for year of publication or language.
The literature search was performed using MeSH terms and text words including synonyms about perioperative and/or anesthesia-related fatal and non-fatal CA rates in geriatric patients. To achieve higher sensitivity and to identify relevant articles, the search strategy was adjusted for each database (see Supplementary S1.1 and S1.2).
The following inclusion criteria were applied for the studies: (i) included patients aged 60 years and older and reported perioperative and/or anesthesia-related CA rates; (ii) involved all age groups, including patients aged 60 years old and older; (iii) a cohort or cross-sectional study; (iv) specified perioperative and/or anesthesia-related CA rates that occurred seven days after the surgery; and (v) provided enough information to perform the analysis.
The exclusion criteria were as follows: (i) reported only one surgical procedure (e.g., cardiac surgery) or a specific anesthetic technique (e.g., regional anesthesia) or patient subtype (e.g., patients with ASA physical status I and II only); (ii) did not specify the time period; or (iii) evaluated fewer than 3,000 geriatric patients. At least 3,000 patients in each study were included to allow us to estimate the incidence of rare adverse events (≤1 per 1,000 anesthetics)35.
Data Extraction and Outcome Definitions
Two investigators (K.S.B and L.G.B.) identified studies, and consensus was reached in all cases.
The primary outcome was perioperative CA (an event resulting from any cause; e.g., patient disease/condition, surgery, or anesthesia). The secondary outcome was anesthesia-related CA (either partly or completely attributable to anesthesia) by the investigators of the included studies. Because there is no consensus regarding the definition of the postoperative period (in the worldwide literature, the definitions of postoperative period include the first 24 hours, 48 hours, and even 1 month after surgery), the period of perioperative CA was defined in this review as the date of surgery until the seventh postoperative day.
High- and low-income countries were defined as having an HDI ≥ 0.8 and <0.8, respectively. A country’s HDI status can change over time, and several studies have reported data covering a time period of many years; thus, HDI was defined as the mean of HDI values between the first and last year in which the patients were recruited for each study. When HDI was not available for the specific time period covered by the study, we used the HDI for the closest available date.
Due to the fact that many safety-improvement measures emerged in the early 1990s in high-HDI countries and later in some low-HDI countries and based on two systematic reviews of perioperative CA14, 15, the time frame evaluated in the studies included in this analysis was split into two periods (pre-1990s versus 1990–2017). These measures included improvements in the care of patients, which involved equipment sterilization, new anesthesia medications and workstations with ventilators, anesthesia-practice based on safety protocols, and an increase in the number of adult intensive care beds14, 15, 21–23.
Statistical Analysis
Our meta-regression analysis used a fixed-effect model with restricted estimated maximum likelihood (REML) and an observed log-odds ratio to predict whether CA rates in geriatric patients statistically changed over time or according to HDI (time and HDI were evaluated as continuous variables). Stata-13 (StataCorp LP, College Station, TX) was used to perform the meta-regression.
Additionally, a random-effects model was applied to calculate weighted event rates across all of the included studies with a pooled analysis (StatsDirect Ltd, Altrincham, Cheshire, UK)36. The times and HDI values were divided (i.e., pre-1990s versus 1990–2017 and low-income versus high-income, respectively) to evaluate perioperative and anesthesia-related CA rates. The event rate was defined as the number of CA events per 10,000 anesthetic procedures, and the data are reported as 95% confidence intervals (CIs). Proportion tests were performed using SAS for Windows®, v.9.4 (SAS Institute, Cary, NC). Chi-square tests were used to compare differences in the proportions of events according to time period and HDI status. Because the data were recorded as time intervals (e.g., from 06/06/1989 to 06/06/1993), the median year of the study’s patient recruitment interval (i.e., median: 1991)15 was considered. A P value < 0.05 was considered significant.
An alternative approach that is employed to quantify the effect of heterogeneity is the I 2 statistic (StatsDirect Ltd, Altrincham, Cheshire, UK)37, 38; values higher than 50% suggest heterogeneity among the studies.
Electronic supplementary material
Acknowledgements
This research was supported by grants #2013/11007-6 [São Paulo Research Foundation (FAPESP)], #0143/004/13 [Pró-Reitoria de Pesquisa (PDI-UNESP)] and #304466/2015-8 [The National Council for Scientific and Technological Development (CNPq)]. Karen S. Braghiroli and Bruna Rocha were granted a scholarship from Coordination of Improvement for Higher Academic Staff (CAPES) and FAPESP (#2016/20276-9), respectively. This study was performed by the Anesthesia Cardiac Arrest and Mortality Study Commission at the Department of Anesthesiology, Universidade Estadual Paulista (Unesp), Medical School, Botucatu, Brazil.
Author Contributions
K.S.B., J.R.C.B. and L.G.B. designed the study. K.S.B. and L.G.B. performed the searches and screened studies for eligibility. K.S.B., B.R., RE.D., J.E.C. and L.G.B assessed the quality of the papers and performed the statistical analysis. K.S.B., B.R., M.G.B. and L.G.B. drafted the manuscript. J.R.C.B. and R.E.D. critically revised the manuscript. All authors approved the final version.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Electronic supplementary material
Supplementary information accompanies this paper at doi:10.1038/s41598-017-02745-6
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO (World Health Organization). Ageing. http://www.who.int/topics/ageing/en/ (2016).
- 2.WHO (World Health Organization). Ageing and health. http://www.who.int/mediacentre/factsheets/fs404/en/ (2015).
- 3.Aubas S, Biboulet P, Daures JP, du Cailar J. Incidence and etiology of cardiac arrest occurring during the perioperative period and in the recovery room. A propros of 102,468 anesthesia cases. Ann. Fr. Anesth. Reanim. 1991;10:436–442. doi: 10.1016/S0750-7658(05)80846-9. [DOI] [PubMed] [Google Scholar]
- 4.Biboulet P, et al. Fatal and non-fatal cardiac arrests related to anesthesia. Can. J. Anesth. 2001;48:326–332. doi: 10.1007/BF03014958. [DOI] [PubMed] [Google Scholar]
- 5.Olsson GL, Hallén B. Cardiac arrest during anaesthesia. A computer-aided study in 250,543 anaesthetics. Acta Anaesthesiol. Scand. 1988;32:653–664. doi: 10.1111/j.1399-6576.1988.tb02804.x. [DOI] [PubMed] [Google Scholar]
- 6.Kawashima Y, et al. Anesthesia-related mortality and morbidity in Japan (1999) J. Anesth. 2002;16:319–331. doi: 10.1007/s005400200049. [DOI] [PubMed] [Google Scholar]
- 7.Braz LG, et al. Perioperative cardiac arrest: a study of 53,718 anaesthetics over 9 yr from a Brazilian teaching hospital. Br. J. Anaesth. 2006;96:569–575. doi: 10.1093/bja/ael065. [DOI] [PubMed] [Google Scholar]
- 8.Goswami S, Brady JE, Jordan DA, Li G. Intraoperative cardiac arrests in adults undergoing noncardiac surgery: incidence, risk factors, and survival outcome. Anesthesiology. 2012;117:1018–1026. doi: 10.1097/ALN.0b013e31827005e9. [DOI] [PubMed] [Google Scholar]
- 9.Nunnally ME, O’Connor MF, Kordylewski H, Westlake B, Dutton RP. The incidence and risk factors for perioperative cardiac arrest observed in the national anesthesia clinical outcomes registry. Anesth. Analg. 2015;120:364–370. doi: 10.1213/ANE.0000000000000527. [DOI] [PubMed] [Google Scholar]
- 10.Deiner S, Westlake B, Dutton RP. Patterns of surgical care and complications in elderly patients. J. Am. Geriatr. Soc. 2014;62:829–835. doi: 10.1111/jgs.12794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Walker IA, Wilson IH. Anaesthesia in developing countries-a risk for patients. Lancet. 2008;371:968–969. doi: 10.1016/S0140-6736(08)60432-8. [DOI] [PubMed] [Google Scholar]
- 12.Chu KM, Ford N, Trelles M. Operative mortality in resource-limited settings: the experience of Medicins Sans Frontiers in 13 countries. Arch. Surg. 2010;145:721–725. doi: 10.1001/archsurg.2010.137. [DOI] [PubMed] [Google Scholar]
- 13.United Nations Development Programme. Human development report 2015. http://hdr.undp.org/en/2015-report (2015).
- 14.Bainbridge D, Martin J, Arango M, Cheng D. Evidence-based Peri-operative Clinical Outcomes Research (EPiCOR) Group. Perioperative and anaesthetic-related mortality in developed and developing countries: a systematic review and meta-analysis. Lancet. 2012;380:1075–1081. doi: 10.1016/S0140-6736(12)60990-8. [DOI] [PubMed] [Google Scholar]
- 15.Koga FA, et al. Anaesthesia-related and perioperative cardiac arrest in low- and high-income countries. A systematic review with meta-regression and proportional meta-analysis. Medicine (Baltimore). 2015;94:e1465. doi: 10.1097/MD.0000000000001465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nunes JC, et al. Intraoperative and anesthesia-related cardiac arrest and its mortality in older patients: a 15-year survey in a tertiary teaching hospital. PLoS One. 2014;9:e104041. doi: 10.1371/journal.pone.0104041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tamdee D, et al. Factors related to 24-hour perioperative cardiac arrest in geriatric patients in a Thai University Hospital. J. Med. Assoc. Thai. 2009;92:198–207. [PubMed] [Google Scholar]
- 18.Story DA, et al. Complications and mortality in older surgical patients in Australia and New Zealand (the REASON study): a multicentre, prospective, observational study. Anaesthesia. 2010;65:1022–1030. doi: 10.1111/j.1365-2044.2010.06478.x. [DOI] [PubMed] [Google Scholar]
- 19.Rodanant O, et al. The Thai anesthesia incidents study (THAI Study) of perioperative death in geriatric patients. J Med Assoc Thai. 2007;90:1375–1381. [PubMed] [Google Scholar]
- 20.Pinto BB, Rached MA, Walder B. Risk prediction instruments to guide perioperative care in elderly patients with advanced disease: a basic necessity. Eur. J. Anaesthesiol. 2016;33:875–877. doi: 10.1097/EJA.0000000000000502. [DOI] [PubMed] [Google Scholar]
- 21.Cooper JB, Gaba D. No myth: anesthesia is a model for addressing patient safety. Anesthesiology. 2002;97:1335–1337. doi: 10.1097/00000542-200212000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Ivani G, Walker I, Enright A, Davidson A. Safe perioperative pediatric care around the World. Pediatr. Anesth. 2012;22:947–951. doi: 10.1111/pan.12009. [DOI] [PubMed] [Google Scholar]
- 23.Eichhorn JH. Prevention of intraoperative anesthesia accidents and related severe injury through safety monitoring. Anesthesiology. 1989;70:572–577. doi: 10.1097/00000542-198904000-00002. [DOI] [PubMed] [Google Scholar]
- 24.Eichhorn JH. Review article: practical current issues in perioperative patient safety. Can. J. Anaesth. 2013;60:111–118. doi: 10.1007/s12630-012-9852-z. [DOI] [PubMed] [Google Scholar]
- 25.Haynes AB, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N. Engl. J. Med. 2009;360:491–499. doi: 10.1056/NEJMsa0810119. [DOI] [PubMed] [Google Scholar]
- 26.Le Manach Y, et al. Preoperative score to predict postoperative mortality (POSPOM): derivation and validation. Anesthesiology. 2016;124:570–579. doi: 10.1097/ALN.0000000000000972. [DOI] [PubMed] [Google Scholar]
- 27.Pignaton W, et al. Perioperative and anesthesia-related mortality: an 8-year observational survey from a tertiary teaching hospital. Medicine (Baltimore). 2016;95:e2208. doi: 10.1097/MD.0000000000002208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Carlucci MT, et al. Intraoperative cardiac arrest and mortality in trauma patients. A 14-yr survey from a Brazilian tertiary teaching hospital. PLoS One. 2014;9:e90125. doi: 10.1371/journal.pone.0090125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pearse RM, Holt PJ, Grocott MP. Managing perioperative risk in patients undergoing elective non-cardiac surgery. BMJ. 2011;343:d5759–d5759. doi: 10.1136/bmj.d5759. [DOI] [PubMed] [Google Scholar]
- 30.Wacker J, Staender S. The role of the anesthesiologist in perioperative patient safety. Curr. Opin. Anaesthesiol. 2014;27:649–656. doi: 10.1097/ACO.0000000000000124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dam WH, Vimtrup J. Heart arrest or death on the operation table over a 10-year period in Bispebjerg Hospital. Nord Med. 1967;78:966–969. [PubMed] [Google Scholar]
- 32.Kinsella, K. & Phillips, D. R. Global aging: the challenge of success. Popul Bull, Vol 60, http://www.prb.org/pdf05/60.1globalaging.pdf (Population Reference Bureau, 2005).
- 33.Solomon DH. A statement of principles: toward improved care of older patients in surgical and medical specialties. J. Am. Geriatr. Soc. 2000;48:699–701. doi: 10.1111/j.1532-5415.2000.tb04733.x. [DOI] [PubMed] [Google Scholar]
- 34.Stroup DF, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 35.Eypasch E, Lefering R, Kum CK, Troidl H. Probability of adverse events that have not yet occurred: a statistical reminder. BMJ. 1995;311:619–620. doi: 10.1136/bmj.311.7005.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control. Clin. Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 37.Higgins, J. P. T. & Green, S. Assessment of study quality: Cochrane reviewers’ Handbook, The Cochrane Library, Issue 3 (John Wiley & Sons, Ltd., 2005).
- 38.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analysis. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ahmed A, Ali M, Khan EA, Khan MU. An audit of perioperative cardiac arrests in a Southeast Asian university teaching hospital over 15 years. Anaesth. Intensive Care. 2008;36:710–716. doi: 10.1177/0310057X0803600514. [DOI] [PubMed] [Google Scholar]
- 40.Braz JR, et al. Cardiac arrest during anesthesia at a tertiary teaching hospital (1988 to 1996) Rev. Bras. Anestesiol. 1999;49:257–262. doi: 10.1590/s0034-70942004000600002. [DOI] [PubMed] [Google Scholar]
- 41.Fiscella LF, et al. Serious or fatal complications in anesthesia. Prospective analysis in 20.840 surgical procedures. Rev. Argent. Anestesiol. 1991;49:197–263. [Google Scholar]
- 42.Kubota Y, et al. Frequency of anesthetic cardiac arrest and death in the operating room at a single general hospital over a 30-year period. J. Clin. Anesth. 1994;6:227–238. doi: 10.1016/0952-8180(94)90064-7. [DOI] [PubMed] [Google Scholar]
- 43.Morita K, et al. Perioperative mortality and morbidity in the year 2000 in 520 certified training hospitals of Japanese Society of Anesthesiologists: with a special reference to age–report of Japanese Society of Anesthesiologists Committee on Operating Room Safety] Masui. 2002;51:1285–1296. [PubMed] [Google Scholar]
- 44.Otteni JC, Pottecher L, Tiret L, Hatton F, Desmonts JM. Cardiac arrest during anesthesia and recovery. Data from a prospective survey in France, 1978–1982. Ann. Fr. Anesth. Reanim. 1986;5:287–294. doi: 10.1016/S0750-7658(86)80158-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


