Abstract
Background
Following the development of breakthrough techniques for percutaneous coronary intervention (PCI) in the treatment of chronic total occlusions (CTO), the initial success rate of PCI in CTO lesions (CTO-PCI) has improved; however, there are few reports regarding the effects of successful CTO revascularization on long-term mortality in Japan. The aim of this study was to compare the long-term clinical outcomes of patients with successful versus failed CTO recanalization and to identify related factors.
Methods and results
From all PCI procedures performed in our hospital between 2006 and 2013, CTO-PCIs were extracted and classified into two groups: PCI success (n = 656 patients) and PCI failure (n = 82 patients). Patients with successful procedures only on a second attempt, CTO-PCI in small branches, or CTOs in more than one vessel were excluded. Survival was determined from a telephone interview or the consultation history in the outpatient clinic. Initial angiographic success was achieved in 88.9% of the patients. A Kaplan–Meier plot with log-rank analysis showed that cumulative all-cause death was significantly lower in the success group than in the failure group (p = 0.0003; average follow-up duration in success group vs. failure group was 1531.3 ± 33.5 vs. 1565.3 ± 97.5 days, p = 0.7). Moreover, the rate of evident cardiac death was significantly lower in the success group than in the failure group (3.5% [23/656] vs. 15.9% [13/82], p < 0.0001).
Conclusions
This study suggests that successful revascularization in patients with CTO improves their long-term clinical outcomes.
Keywords: Coronary artery disease, Percutaneous coronary intervention, Drug-eluting stent, Chronic total coronary occlusion
1. Introduction
The technology and techniques for the interventional treatment of chronic total occlusion (CTO) in patients with coronary artery disease have advanced significantly over recent years, and have contributed to the higher initial success rate of percutaneous coronary intervention (PCI) for treating CTO (CTO-PCI) [1], [2]. However, the effect of this improvement on the chronic outcomes of patients who undergo CTO-PCI is still unclear. It has been reported that successful CTO-PCI might be associated with symptom relief, a lower rate of subsequent myocardial infarction (MI) and coronary artery bypass graft (CABG) surgery, and improved long-term survival, compared with unsuccessful PCI [3], [4], [5], [6], [7]. While the initial success rate of CTO-PCI has also reached an acceptable level in Japan, with an acute result that is widely recognized to be better than in other countries, its long-term outcome has not been fully investigated. Therefore, the aim of this study was to compare the long-term clinical outcomes of patients with successful versus failed CTO recanalization and to identify related factors.
2. Methods
2.1. Study design
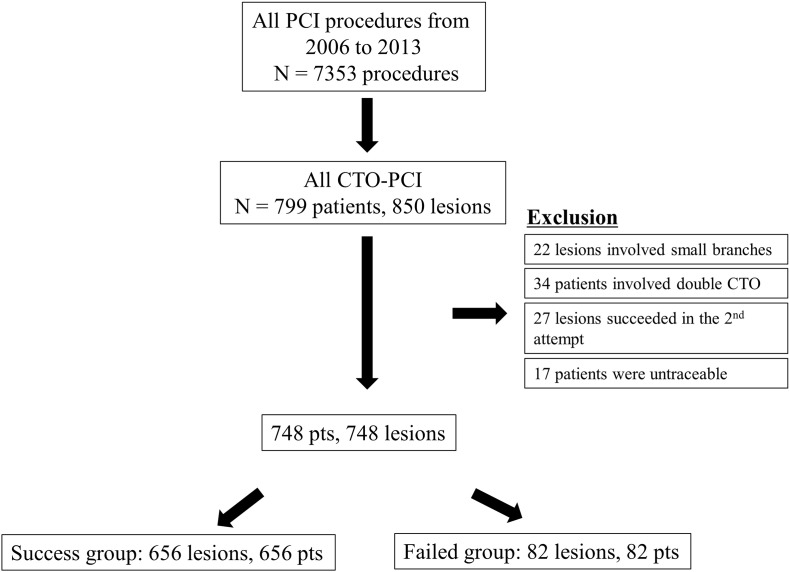
Consecutive patients who underwent CTO-PCI were extracted from the database at Toyohashi Heart Center, Toyohashi, Japan, in which data were entered prospectively. The database included relevant patient information as well as angiographic and procedural characteristics. A total of 7353 PCI procedures performed between 2006 and 2013 were screened for this study, of which 848 involved revascularization of a CTO. Any patients with CTOs in more than one vessel or lesions in a small coronary branch vessel, as well as those in whom a repeat procedure succeeded after an initial failure, were excluded from the study, as were 17 patients who were untraceable (Fig. 1). We excluded patients with CTO lesions in more than one vessel in order to evaluate the effect of a single CTO-PCI recanalization, while small-branch lesions were excluded because of the known lesser clinical advantage in such cases. The remaining 738 patients represented the total population of this study. These patients were then classified into 2 study groups: those with successful CTO-PCI (success group; 656 patients) and those with failed CTO-PCI (failed group; 82 patients) (Fig. 1). The protocol was approved by the ethics committees in each participating center and all participants gave written informed consent. The PCI and stent implantation were performed in a standard manner. Heparin was administered to maintain an activated clotting time > 250 s. The PCI strategy was left to the discretion of the treating physician. The PCI of the CTO was performed using contemporary techniques as they became available: bilateral injection; specialized hydrophilic, tapered-tip, and stiff wires; parallel wires; micro-catheters; and a retrograde approach. In this study, all the stents deployed were drug-eluting stents (DES). After PCI, all patients were prescribed lifelong aspirin; in addition, clopidogrel was prescribed for at least 6 months after implantation of DES. Demographic and procedural data for all patients undergoing PCI were prospectively entered into a dedicated database. Patients were followed prospectively by telephone interview or on regular outpatient visits.
Fig. 1.
Flow diagram of the study population.
PCI procedures performed between 2006 and 2013. The flowchart indicates lesions, exclusions, and the composition of the study population.
CTO = chronic total occlusion; PCI = percutaneous coronary intervention.
2.2. Definitions
Coronary CTO is defined as a true total occlusion with complete interruption of antegrade blood flow as assessed by coronary arteriography (Thrombolysis In Myocardial Infarction [TIMI] flow grade 0) and with an estimated occlusion duration of 3 months or more. For the procedural background inherent in this study, we examined the total amount of contrast medium, procedure time, and radiation dose. Procedure time was defined as the total duration for which the patient was in the catheterization room (from entry until exit). Fluoroscopy time and radiation dose were recorded automatically by the cine device. Coronary perforation was examined as a complication during the procedure. The following endpoints were evaluated to compare patients with a failed versus a successful procedure: all-cause death, evident cardiac death, MI, and subsequent coronary artery bypass grafting (CABG). The following definitions were used:
-
•
Evident cardiac death was defined as death within 7 days after MI, death associated with cardiovascular interventions within 30 days after CABG or within 7 days after PCI, or unexpected death presumed to be due to ischemic cardiovascular disease and arrhythmia occurring within 24 h after the onset of symptoms, without clinical or postmortem evidence of another cause, as judged according to the information from the telephone interview. Death from uncertain causes was also classified as cardiac death.
-
•
Double CTO was defined as the presence of a CTO lesion in more than one vessel at the same time.
-
•
Procedural success was defined as residual stenosis less than 50% with TIMI flow grade 3 and without major adverse cardiovascular events.
-
•
MI was diagnosed by an increase in creatine kinase level to twice the upper limit of normal.
2.3. Guidewire crossing strategies
Guidewire crossing strategies were followed in a stepwise manner, as described in our previous report [8]. Briefly, as for antegrade approaches, single wiring, parallel wiring, and wiring techniques guided by intravascular ultrasound (IVUS) were included. For retrograde attempts, retrograde wire cross, kissing wire cross, controlled antegrade and retrograde subintimal tracking (CART), and reverse CART (r-CART) techniques were performed.
2.4. Statistical analysis
Data distribution was assessed by the F-test. Variables that did not follow a normal distribution were expressed as medians and interquartile ranges, whereas other continuous variables were expressed as mean ± standard error. Student's t-test or the Mann–Whitney U test was used for the comparison of continuous variables, as appropriate. Event rates were estimated using the Kaplan–Meier method. Follow-up was censored at date of last follow-up or at 7 years, whichever came first. Survival curves with all available follow-up data were constructed for time-to-event variables using Kaplan–Meier methodology and compared by log-rank test. Data on patients who were lost to follow-up were censored at the time of the last contact. Logistic regression analysis was used to identify the independent predictors for the procedural success of CTO-PCI. The predictors of the multivariate model were entered if their univariate p-value was at the p = 0.1 level. The results are reported as odds ratios (OR) with associated confidence intervals (CI). An OR of < 1 indicated better mortality, while that of > 1 indicated worse. A value of p < 0.05 was considered statistically significant, and all reported p-values were two-sided. Statistical analysis was performed using SAS software (SAS Institute, Cary, North Carolina).
3. Results
3.1. Patient, lesion and procedural characteristics
Baseline patient characteristics are shown in Table 1. Renal insufficiency requiring hemodialysis after the procedure (serum creatinine level > 2 mg/dL) was observed more often in the failed group than in the success group (12.4% [11/89] vs. 5.8% [38/656]; p = 0.007). Notably, the mean preprocedural creatinine level was significantly higher in the failed group than in the success group (1.4 ± 0.1 vs. 2.0 ± 0.3 mg/dL; p = 0.03). Preprocedural LVEF obtained by echocardiography was lower in the failed patients (50.4 ± 12.5 vs. 45.8 ± 12.8; p = 0.04). Lesion and procedural characteristics in both groups are shown in Table 2. CTO lesions were located predominantly in the right coronary artery. Although this tendency was similar in both groups, CTO in the left circumflex artery was observed more frequently in the failed patients (34.2% [28/82] vs. 19.7% [129/656]; p = 0.01). Severe calcified lesions were identified more often in the failed patients (27.0% [22/82] vs. 9.0% [59/656]; p < 0.0001). Similarly, severely tortuous vessels were observed more often in the failed patients (12.2% [10/82] vs. 5.2% [34/656]; p < 0.001). Regarding the procedural background, the procedure time was significantly longer in the failed group (236.0 ± 10.7 vs. 184.4 ± 3.4 min; p < 0.0001). The amount of skin radiation dose measured in frontal view was significantly greater in the failed patients (6.4 ± 0.6 vs. 4.7 ± 0.2 Gy; p = 0.002). Among procedural complications, coronary perforation was observed more frequently in the failed group (31.7% [26/82] vs. 9.0% [59/656]; p < 0.0001).
Table 1.
Patient characteristics in the success and failure groups.
| Variables | Success (656 pts) | Failure (82 pts) | p-Value |
|---|---|---|---|
| Age (years) | 65.7 ± 0.4 | 67.6 ± 1.3 | 0.12 |
| Male (%) | 544 (82.9) | 68 (82.9) | 0.75 |
| Diabetes mellitus | 78 (11.9) | 11 (13.4) | 0.89 |
| Hypertension | 387 (59.0) | 51 (62.2) | 0.76 |
| Hyperlipidemia | 254 (38.7) | 38 (46.3) | 0.13 |
| Familial history | 97 (14.8) | 8 (9.8) | 0.24 |
| Smoking | 158 (24.1) | 17 (20.7) | 0.74 |
| CKD | 38 (5.8) | 11 (13.4) | 0.007 |
| Preprocedural creatinine | 1.4 ± 0.1 | 2.0 ± 0.3 | 0.03 |
| Previous CABG | 66 (10.1) | 8 (9.8) | 0.73 |
| Preprocedural LVEF(%) | 50.4 ± 12.5 | 45.8 ± 12.8 | 0.04 |
Values are median (interquartile range), or number, (%). Pts = patients; CKD = chronic kidney disease; CABG = coronary artery bypass grafting; LVEF = left ventricular ejection fraction.
Table 2.
Lesion and procedural characteristics in the success and failure groups.
| Variables | Success (656 pts) | Failure (82 pts) | p-Value | |
|---|---|---|---|---|
| Target vessel | ||||
| LAD | 201 (30.6) | 16 (19.5) | 0.01 | |
| RCA | 323 (49.1) | 37 (45.1) | ||
| LCX | 129 (19.7) | 28 (34.2) | ||
| LMT | 3 (0.6) | 1 (1.2) | ||
| Calcification | ||||
| None | 194 (29.5) | 27 (32.8) | < 0.0001 | |
| Mild | 228 (34.7) | 16 (19.5) | ||
| Moderate | 175 (26.6) | 17 (20.7) | ||
| Severe | 59 (9.0) | 22 (27.0) | ||
| Tortuosity | ||||
| None | 511 (77.9) | 54 (65.9) | 0.001 | |
| Moderate | 111 (16.9) | 18 (21.9) | ||
| Severe | 34 (5.2) | 10 (12.2) | ||
| Amount of contrast (mL) | 285.3 ± 5.9 | 307.5 ± 18.5 | 0.37 | |
| Procedure time (min) | 184.4 ± 3.4 | 236.0 ± 10.7 | < 0.0001 | |
| Radiation dose (frontal) (Gy) | 4.7 ± 0.2 | 6.4 ± 0.6 | 0.002 | |
| Radiation dose (lateral) (Gy) | 4.3 ± 0.2 | 4.5 ± 0.4 | 0.80 | |
| Coronary perforation | 59 (9.0) | 26 (31.7) | < 0.0001 | |
| CK at 24 h | 204.2 ± 19.0 | 221.9 ± 36.9 | 0.74 | |
| Initial success rate | 88.1% |
Values are number, (%); LAD = left anterior descending artery; RCA = right coronary artery; LCX = left circumflex; LMT = left main trunk artery; PCI = percutaneous coronary intervention; CK = creatine kinase.
3.2. Guidewire crossing strategy
The guidewire strategies adopted in all the procedures and in each study group are shown in Table 3. The antegrade wiring strategy was followed more often in the success group than in the failed group, and the frequency of the CART and r-CART techniques was significantly higher in the success group (18.0% vs. 12.1%; p < 0.0001).
Table 3.
Guidewire strategies adopted in the success and the failure groups.
| Variables | Success (656 pts) | Failure (82 pts. ) | p-Value |
|---|---|---|---|
| Guidewire strategy | |||
| Parallel wire technique | 163 (24.8) | 34 (41.5) | < 0.0001 |
| Success | 110 (67) | N/A | |
| IVUS guided | 53 (8.1) | 12 (14.6) | < 0.0001 |
| Success | 39 (70) | N/A | |
| CART or r-CART | 118 (18.0) | 10 (12.1) | < 0.0001 |
| Success | 109 (92.3) | N/A |
Values are number, (%); IVUS = intravascular ultrasound; CART = controlled antegrade and retrograde subintimal tracking; r-CART = reversed CART.
3.3. Factors in successful and failed CTO-PCI procedures that affect long-term mortality
The phenomena that were observed to be predictive of the long-term clinical outcome in the success and failed groups are shown in Table 4. Radiational dermatitis was observed more often in the failed group than in the success group (4.9% [4/82] vs. 1.1% [7/656]; p = 0.007). Successful CTO-PCI significantly decreased the need for subsequent CABG (success group 2.1% [14/656] vs. failed group 8.5% [7/82]; p = 0.001). We also observed a trend toward a lower frequency of presentation of congestive heart failure in the success group (3.4% [22/656] vs. 7.3% [6/82]; p = 0.07) as well as a significantly lower incidence of stroke (1.1% [7/656] vs. 4.9% [4/82]; p = 0.007).
Table 4.
Long-term clinical results in the success and failure groups.
| Variables | Success (656 pts) | Failure (82 pts) | p-value |
|---|---|---|---|
| Follow-up days | 1531.3 ± 33.5 | 1565.3 ± 97.5 | 0.72 |
| TVR | 94 (14.3) | N/A | N/A |
| Reocclusion | 42 (6) | N/A | N/A |
| Follow-up creatinine (mg/dL) | 1.4 ± 0.1 | 1.9 ± 0.3 | 0.17 |
| Follow-up LVEF(%) | 53.5 ± 12.7 | 49.1 ± 10.3 | 0.11 |
| Radiation dermatitis | 7 (1.1) | 4 (4.9) | 0.007 |
| Subsequent CABG | 14 (2.1) | 7 (8.5) | 0.001 |
| Subsequent hemodialysis | 16 (2.4) | 2 (2.4) | – |
| CHF | 22 (3.4) | 6 (7.3) | 0.07 |
| Stroke | 7 (1.1) | 4 (4.9) | 0.007 |
| All cause death | 64 (9.8) | 19 (23.2) | 0.0003 |
| Evident cardiac death | 23 (3.5) | 13 (15.9) | < 0.0001 |
Values are number, (%); TVR = target vessel revascularization; CABG = coronary artery bypass grafting; HD = hemodialysis; CHF = congestive heart failure; LVEF = left ventricular ejection fraction.
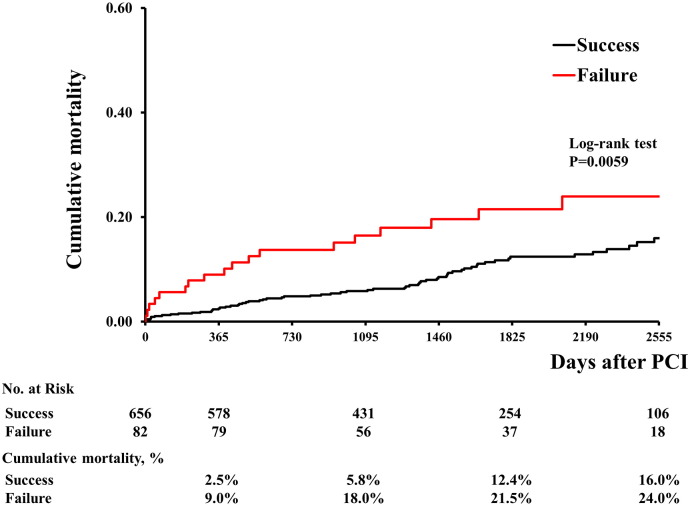
Kaplan–Meier curves for the clinical endpoints at 2500 days are shown in Fig. 2. The cumulative mortality of the success group was significantly lower than that of the failed group (log-rank test: p = 0.0059; 9.8% [65/656] vs. 23.2% [19/82]; p = 0.0003), as was the incidence of evident cardiac death (3.5% [23/656] vs. 15.9% [13/82]; p < 0.0001).
Fig. 2.
Kaplan–Meier curves for the clinical endpoints at 2500 days comparing the success and failed group.
The cumulative mortality of the success group was significantly lower than that of the failed group (log-rank test: p = 0.0059).
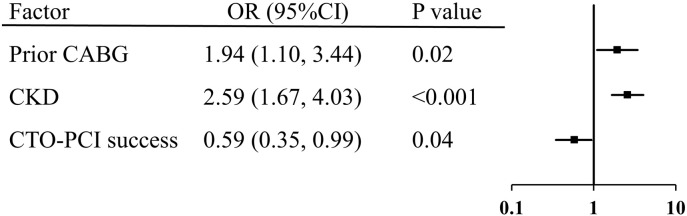
3.4. Logistic regression analysis
A Cox proportional-hazards model was used to identify variables independently associated with all-cause mortality. Prior CABG history and the presence of chronic kidney disease (CKD) were identified as unfavorable independent factors (prior CABG: OR 1.94, 95% CI: 1.10–3.44; p = 0.02; CKD: OR 2.59, 95% CI: 1.67–4.03; p < 0.001), whereas the success of CTO-PCI was identified as a favorable independent factor for all-cause mortality (OR 0.59; 95% CI: 0.35–0.99; p = 0.04; Fig. 3).
Fig. 3.
Results of logistic regression analysis.
A Cox proportional-hazards model was used to identify variables independently associated with all-cause mortality. Prior CABG history and the presence of CKD were identified as unfavorable independent factors (prior CABG: OR 1.94, 95%: 1.10–3.44, p = 0.02; CKD: OR 2.59, 95% CI: 1.67–4.03, p < 0.001), while the success of CTO-PCI was identified as a favorable independent factor for all-cause mortality (OR 0.59; 95% CI: 0.35–0.99; p = 0.04).
CABG = coronary artery bypass grafting; CI = confidence interval; CKD = chronic kidney disease; OR = odds ratio. Other abbreviations as in Fig. 1.
4. Discussion
The results of this study demonstrate that a successful CTO-PCI procedure contributes to a better long-term clinical outcome compared with failed CTO-PCI. Successful CTO-PCI significantly decreased not only all-cause death, but also evident cardiac death. Moreover, successful CTO-PCI significantly decreased the need for subsequent CABG and numerically decreased the presentation of congestive heart failure and stroke. Considering the results of this study, it is possible that successful CTO-PCI contributes not only to lower long-term mortality, but also to a better quality of life. Regarding the lesion background, severe calcified and tortuous lesions were associated with failed procedures. Regarding the procedural factors, a failed CTO-PCI required a much longer time and a greater radiation dose than a successful procedure and was associated with coronary perforation. According to the Cox proportional-hazards model for all-cause death, success of CTO-PCI, age, body mass index, the presence of CKD, and a prior history of CABG were associated with better long-term mortality.
The initial success rate of CTO-PCI in Japan is over 80% [11]. However, the long-term mortality after CTO has not been fully elucidated. We would like to stress the significance of this study, which demonstrates not only the high initial success rate of CTO-PCI, but also its better long-term cardiac mortality. Since Japan is widely recognized as a country that has strong spirit of inquiry into CTO-PCI, we believe this study adds significantly to our knowledge regarding the long-term mortality after successful CTO-PCI.
It is easy to understand why successful CTO-PCI would decrease the incidence and the severity of CHF, and a high proportion of patients treated successfully showed an improvement in left ventricular function; however, the lower frequency of stroke was unexpected. We might speculate that successful treatment with CTO-PCI would contribute to an improvement in patients' attitude to health promotion, leading to lifestyle and other changes that could decrease the risk of stroke. More information about when stroke events occurred might help toward interpreting this result.
Follow-up ejection fraction obtained by echocardiography was better in both groups. However, it is not clear whether the successful CTO-PCI or the optimal medical treatment was responsible for this improvement in LVEF. Further investigation is required to determine the relative contributions of successful CTO-PCI and optimal medical treatment to an improvement in long-term mortality.
4.1. Characteristics of the CTO-PCI candidate
Compared with the success group, more CKD patients were included in the failed group. This result might reflect the fact that patients on chronic hemodialysis tended to be in the failed group. Heavily calcified coronary lesions are often encountered in chronic hemodialysis patients in daily practice, and it has been reported that heavy calcification can be a major obstacle to the success of CTO-PCI [8], [9]. In this study, heavily calcified lesions were found more often in the failed group, as discussed below, which means that this result is consistent with previous reports.
4.2. Lesion and procedural background of CTO-PCI
The CTO was located in the left circumflex artery more often in the failed group than in the success group. It has not been clearly reported whether a lesion location in the left circumflex is a negative factor for procedural success; however, the high angulation from the left main to the left circumflex makes it difficult to cross the lesion. Apart from this issue, once a CTO lesion forms in a severely tortuous vessel it is very difficult to anticipate the trajectory of the vessel. In such a tortuous CTO lesion, preprocedural computed tomography coronary angiography is essential.
Failed CTO-PCI procedures required more time and a higher frontal skin radiation dose than did successful procedures. The total amount of contrast used was numerically greater in the failed patients; however, the difference did not reach statistical significance. These negative factors associated with CTO-PCI were also within a high range even in the patients with successful CTO-PCI. It has been reported that a successful retrograde approach can ameliorate these limitations compared with failed procedures [11]. Therefore, a retrograde approach can be a good option for patients with CKD as a means of preserving their remaining renal function.
Regarding complications, coronary perforation was observed more frequently in the failed group than in the success group. In this study, the difference between the groups in the incidence of devastating coronary perforation, which leads to an unstable hemodynamic state, did not reach statistical significance; however, the longer procedural time and wiring difficulties in failed procedures can often result in the occurrence of complications such as coronary perforation.
4.3. Effect of guidewire strategy
Despite the higher frequency of retrograde attempts in the failed group compared with the success group, the procedural success was not satisfactory. In the failed group, the retrograde approach was attempted as a final resort; this finding may thus be due to the complexity of the lesions. Heavily calcified lesions were encountered more often in the failed group than in the success group. Heavy calcification often hinders the advance of the catheter via a retrograde approach, leaving no alternative but to use the smallest size of balloon to dilate a greatly calcified lesion. It is probably safe to say that the degree of calcification is the most important factor for the success of retrograde CTO-PCI.
4.4. Results of logistic regression analysis
In the Cox proportional-hazards model analysis, procedural success, prior CABG, and the presence of CKD were the predictors found to be significantly associated with long-term mortality. It has been reported that successful CTO-PCI improved long-term cardiac mortality [7], [10]. Consistent with previous reports, our study demonstrates that successful CTO-PCI was effective in improving the cardiac mortality of CTO patients. In our study, patients with double CTO were excluded, so we were able to specifically evaluate the effect of a single CTO lesion on long-term cardiac mortality. It has been reported that the cardiac mortality is better in CTO patients who undergo complete revascularization than in those who undergo partial revascularization [10]. Thus, if patients with double CTO had been included in this study, the evaluation of long-term mortality for each subgroup (partial and complete revascularization) would have been more complicated.
4.5. Study limitations
There are several limitations to our study. First, differences in the performance of the procedures as well as the varied clinical settings involved in the performance of PCI could differ between countries; therefore, the results may also be variable. Second, the success of CTO-PCI is highly dependent on a physician's skill and experience. Although experience in performing CTO-PCI has accumulated in our hospital, the results concerning acute success may be different under conditions with less experience. Since this is a retrospective observational study, there are also inherent limitations. Finally, it is likely that a previous history of CABG and CKD would reflect the patient's frailty and general status. In particular, the degree of renal dysfunction needs to be stratified and related to the long-term mortality.
5. Conclusions
The initial success rate of CTO-PCI in Japan has reached a satisfactory level. In line with this development, the long-term mortality among patients who undergo successful CTO-PCI is better than in those in whom CTO-PCI is unsuccessful. Multivariate analysis demonstrated that procedural success, a prior history of CABG, and the presence of CKD were associated with long-term mortality.
Authors' information
Tomohiko Teramoto MD, Ph.D is the person who designed this study and wrote the manuscript. Estuo Tsuchikane MD, Masanori Yamamoto MD and Masashi Kimura MD gave me a lot of important comments and suggestions for the design of this study. Hitoshi Matsuo MD, Seiji Kano MD, Tetsurou Shimura MD, and Hirotomo Sato MD discussed the design of this study, and gave me a lot of important comments, and helped data collection. Yoshiaki Kawase MD, Yoriyasu Suzuki MD, Maoto Habara MD, Kenya Nasu MD, Yoshihisa Kinoshita MD, Mitsuyasu Terashima MD, Tetsuo Matsubara MD, and Takahiko Suzuki MD helped make a draft of this manuscript with a lot of important suggestions. Tomohiko Teramoto MD, PhD took charge of the analysis and interpretation of data and approved the final manuscript for the submission.
Funding sources
None.
Disclosures
None.
Acknowledgments
We thank Kazuki Shimizu for the data collection.
References
- 1.Galassi A.R., Tomasello S.D., Reifart N. In-hospital outcomes of percutaneous coronary intervention in patients with chronic total occlusion: insights from the ERCTO (European Registry of Chronic Total Occlusion) registry. EuroIntervention. 2011;7:472–479. doi: 10.4244/EIJV7I4A77. [DOI] [PubMed] [Google Scholar]
- 2.Kimura M., Katoh O., Tsuchikane E. The efficacy of a bilateral approach for treating lesions with chronic total occlusions the CART (controlled antegrade and retrograde subintimal tracking) registry. JACC Cardiovasc. Interv. 2009;2:1135–1141. doi: 10.1016/j.jcin.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 3.Grantham J.A., Jones P.G., Cannon L., Spertus J.A. Quantifying the early health status benefits of successful chronic total occlusion recanalization: results from the FlowCardia's Approach to Chronic Total Occlusion Recanalization (FACTOR) Trial. Circ. Cardiovasc. Qual. Outcomes. 2010;3:284–290. doi: 10.1161/CIRCOUTCOMES.108.825760. [DOI] [PubMed] [Google Scholar]
- 4.Olivari Z., Rubartelli P., Piscione F. TOAST-GISE Investigators. Immediate results and one-year clinical outcome after percutaneous coronary interventions in chronic total occlusions: data from a multicenter, prospective, observational study (TOAST-GISE) J. Am. Coll. Cardiol. 2003;41:1672–1678. doi: 10.1016/s0735-1097(03)00312-7. [DOI] [PubMed] [Google Scholar]
- 5.Hoye A., van Domburg R.T., Sonnenschein K., Serruys P.W. Percutaneous coronary intervention for chronic total occlusions: the Thoraxcenter experience 1992-2002. Eur. Heart J. 2005;26:2630–2636. doi: 10.1093/eurheartj/ehi498. [DOI] [PubMed] [Google Scholar]
- 6.Joyal D., Afilalo J., Rinfret S. Effectiveness of recanalization of chronic total occlusions: a systematic review and meta-analysis. Am. Heart J. 2010;160:179–187. doi: 10.1016/j.ahj.2010.04.015. [DOI] [PubMed] [Google Scholar]
- 7.Mehran R., Claessen B.E., Godino C. Multinational Chronic Total Occlusion Registry. Long-term outcome of percutaneous coronary intervention for chronic total occlusions. JACC Cardiovasc. Interv. 2011;4:952–961. doi: 10.1016/j.jcin.2011.03.021. [DOI] [PubMed] [Google Scholar]
- 8.Teramoto T., Tsuchikane E., Matsuo H. Initial success rate of percutaneous coronary intervention for chronic total occlusion in a native coronary artery is decreased in patients who underwent previous coronary artery bypass graft surgery. JACC Cardiovasc. Interv. 2014;7:39–46. doi: 10.1016/j.jcin.2013.08.012. [DOI] [PubMed] [Google Scholar]
- 9.Morino Y., Abe M., Morimoto T. J-CTO Registry Investigators. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: the J-CTO (Multicenter CTO Registry in Japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc. Interv. 2011;4:213–221. doi: 10.1016/j.jcin.2010.09.024. [DOI] [PubMed] [Google Scholar]
- 10.George S., Cockburn J., Clayton T.C. Long-term follow-up of elective chronic total coronary occlusion angioplasty: analysis from the U.K. Central Cardiac Audit Database. J. Am. Coll. Cardiol. 2014;64:235–243. doi: 10.1016/j.jacc.2014.04.040. [DOI] [PubMed] [Google Scholar]
- 11.Yamane M., Muto M., Matsubara T. Contemporary retrograde approach for the recanalisation of coronary chronic total occlusion: on behalf of the Japanese Retrograde Summit Group. EuroIntervention. 2013;9:102–109. doi: 10.4244/EIJV9I1A15. [DOI] [PubMed] [Google Scholar]