Key Points
CDX genes are differentially expressed in mesoderm harboring definitive hematopoietic potential in a WNT-dependent manner.
CDX4 expression during mesoderm specification regulates human definitive hematopoietic specification.
Abstract
The generation of hematopoietic stem cells from human pluripotent stem cells (hPSCs) is a major goal for regenerative medicine. Achieving this goal is complicated by our incomplete understanding of the mechanism regulating definitive hematopoietic specification. We used our stage-specific hPSC differentiation method to obtain and identify, via CD235a expression, mesoderm harboring exclusively primitive or definitive hematopoietic potential to understand the genetic regulation of definitive hematopoietic specification. Whole-transcriptome gene expression analyses on WNT-dependent KDR+CD235a− definitive hematopoietic mesoderm and WNT-independent KDR+CD235a+ primitive hematopoietic mesoderm revealed strong CDX gene expression within definitive hematopoietic mesoderm. Temporal expression analyses revealed that CDX4 was expressed exclusively within definitive hematopoietic KDR+CD235a− mesoderm in a WNT- and fibroblast growth factor-dependent manner. We found that exogenous CDX4 expression exclusively during mesoderm specification resulted in a >90% repression in primitive hematopoietic potential, but conferred fivefold greater definitive hematopoietic potential, similar to that observed following WNT stimulation. In contrast, CDX4 knockout hPSCs had intact primitive hematopoietic potential, but exhibited a fivefold decrease in multilineage definitive hematopoietic potential. Taken together, these findings indicate that CDX4 is a critical transcription factor in the regulation of human definitive hematopoietic specification, and provides a mechanistic basis for WNT-mediated definitive hematopoietic specification from hPSCs.
Introduction
The generation of hematopoietic stem cells (HSCs) from human pluripotent stem cells (hPSCs) is a major goal for regenerative medicine. To reproducibly achieve this goal, we must first understand human hematopoietic ontogeny. Embryonic hematopoiesis is classically defined by the spatiotemporal emergence of at least 2 distinct programs.1 The first, primitive hematopoiesis, does not give rise to HSCs,2 but instead transiently gives rise to a limited subset of lineages, including HBE-expressing erythroblasts or primitive erythroid colony-forming cells (EryP-CFCs), which can be reliably used as an indicator of the primitive hematopoietic program.3,4 Shortly thereafter, the definitive program emerges and gives rise to all lineages found in the adult, including the HSC.5,6 When differentiating hPSCs, the development of the definitive program can be distinguished from the primitive program by using in vitro assays for HBG-expressing erythroblasts and T lymphocytes.3 However, the genetic regulation of human definitive hematopoietic specification, both in vivo and in vitro, remains unclear.
We recently developed a method to independently specify progenitors of the primitive or definitive hematopoietic programs from hPSCs via stage-specific manipulation of canonical WNT signaling.4 This approach generates a WNT-dependent KDR+CD235a− mesodermal population that gives rise to CD34+ definitive hematopoietic progenitors, as well as a WNT-independent KDR+CD235a+ mesodermal population that gives rise to CD43+ primitive hematopoietic progenitors. Using this tractable system, we interrogated the transcriptional regulation of definitive hematopoietic specification at its earliest identifiable mesodermal progenitor, and identified CDX4 as a critical regulator of human definitive hematopoietic progenitor specification.
Study design
Culture and differentiation
The hPSC line H1 (WA01; WiCell) was grown and differentiated as described previously.4 CD34+CD43− hemogenic endothelium (HE) was isolated by fluorescence-activated cell sorting (FACS) and allowed to undergo the endothelial-to-hematopoietic transition as described in detail previously.7 Analysis of hematopoietic colony potential was performed as described previously.3,7 Full experimental details are found in the supplemental Methods, available on the Blood Web site.
Results and discussion
Mesodermal CDX4 expression is specific to definitive hematopoietic specification
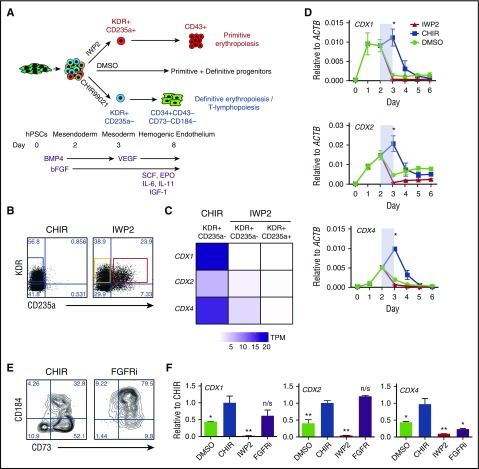
Given that our hPSC differentiation system gives rise to populations of mesoderm harboring exclusively primitive or exclusively definitive hematopoietic progenitors (Figure 1A),4 we asked whether these populations could identify which transcription factor(s) regulate definitive hematopoietic specification within early mesoderm. We isolated by FACS KDR+CD235a− and KDR+CD235a+ mesoderm, generated by CHIR99021 or IWP2 treatment, respectively (Figure 1B),4 and performed whole-transcriptome expression analyses. Differential gene expression analysis8 revealed significant enrichment of the CDX and HOX genes within definitive hematopoietic mesoderm (Figure 1C; supplemental Figure 1; supplemental Table 1). CDX1, CDX2, and CDX4 were all highly expressed in definitive, but not primitive, hematopoietic mesoderm, and have been previously identified as being expressed during hPSC-derived definitive hematopoietic specification.9
Figure 1.
CDX4 is expressed at the onset of definitive hematopoietic progenitor specification within mesoderm. (A) Differentiation schematic and hematopoietic progenitor identification. hPSCs are differentiated using a serum-free, stroma-free approach, with stage-specific application of WNT signal manipulation. Inhibition of WNT signaling within mesendoderm with 3 μM IWP2 leads to the generation of KDR+CD235a+ mesodermal population, which gives rise to CD43+ primitive hematopoietic progenitors, whereas WNT activation with 3 μM CHIR99021 generates a KDR+CD235a− mesodermal population that gives rise to CD34+CD43−CD73−CD184− HE. No manipulation of WNT signaling leads to a heterogeneous population of primitive and definitive hematopoietic progenitors. (B) Representative cell-sorting strategy employed for RNA-seq analyses. Mesoderm harboring definitive (blue) or primitive (red) progenitors were isolated by FACS. (C) Heatmap of CDX gene expression within different mesodermal populations, as determined by RNA-seq. n = 4. (D) qRT-PCR analyses of CDX1 (top), CDX2 (middle), and CDX4 (bottom) expression during the first 6 days of differentiation as in panel A. Period of WNT manipulation is shaded in light blue. n ≥ 3 mean ± standard error of the mean (SEM). Student t test compared with DMSO control: *P < .05. (E) Representative flow cytometric analysis of CD73 and CD184 expression, gated on CD34+CD43− cells following either CHIR99021 (CHIR) treatment or CHIR + 1 μM PD173074 (FGFRi) treatment as in panel A. (F) qRT-PCR analyses of CDX1 (left), CDX2 (middle), and CDX4 (right) expression on day 3 of differentiation, following treatment with either vehicle (DMSO), CHIR99021 (CHIR), IWP2, or PD173074 (FGFRi) as in panel A. Normalized to CHIR treatment. n = 3 mean ± SEM. Student t test compared with CHIR treatment: *P < .05; **P < .01. BMP4, bone morphogenetic protein 4; DMSO, dimethylsulfoxide; EPO, erythropoietin; IGF-1, insulin-like growth factor 1; IL-6, interleukin-6; qRT-PCR, quantitative reverse transcription polymerase chain reaction; RNA-seq, RNA sequencing; SCF, stem cell factor; TPM, transcripts per million; VEGF, vascular endothelial growth factor.
Interestingly, qRT-PCR analyses of each gene over the first 6 days of differentiation revealed that CDX1 and CDX2 are expressed within 24 hours of differentiation, whereas CDX4 was instead upregulated twofold at the time of CHIR99021 treatment (Figure 1D). CDX expression immediately decreased following CHIR99021 removal. This suggested that CDX1 or CDX2 may not specifically regulate definitive hematopoietic progenitor specification, but instead regulate mesendoderm specification, and thus may affect the emergence of both programs, whereas CDX4 expression correlates with definitive hematopoietic progenitor specification by WNT signaling.
In addition to WNT signaling, differentiation cultures at this stage employ the use of BMP4 and basic fibroblast growth factor (FGF),4,7 both of which contribute to the expression of CDX genes in early mesoderm.10,11 Although inhibition of BMP4 signaling with recombinant NOGGIN caused a complete block in mesoderm formation (not shown), the inhibition of basic FGF signaling with PD173074 at the same time as CHIR99021 treatment led to the emergence of a CD34+CD43− population that lacked a distinct CD73−CD184− HE (Figure 1E).7,12 Interestingly, FGF receptor inhibition (FGFRi) had no effect on the expression of CDX1 or CDX2, but did repress CDX4 expression (Figure 1F). Collectively, these results suggested that CDX4 is a relevant transcriptional target during human definitive hematopoietic specification.
CDX4 is required for efficient human definitive hematopoietic specification
In both mouse and zebrafish models, cdx4 deficiency has been implicated in the regulation of embryonic hematopoiesis.11,13-17 Although Cdx4−/− mice showed no significant definitive hematopoietic defects,18 zebrafish exhibit a moderate decrease in definitive hematopoietic potential that was significantly enhanced when combined with cdx1 knockdown,13,14,16 suggesting species-specific usage of different Cdx genes during definitive hematopoietic specification. As we observed definitive hematopoietic mesoderm-specific expression of CDX4 (Figure 1C), we reasoned that the role of CDX4 in human embryonic hematopoiesis may be elucidated using our hPSC model system, by monitoring the ontogeny of primitive and definitive hematopoietic progenitors from early mesoderm.4
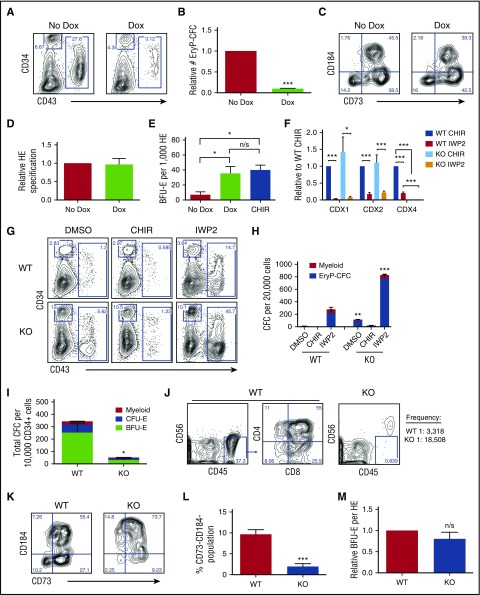
We first generated an inducible expression system using the AAVS1 locus19 to allow for CDX4 expression at any stage of differentiation. Exogenous CDX4 expression from days 2 to 3 of differentiation (supplemental Figure 2A) repressed the specification of the primitive hematopoietic progenitors, as we observed a dramatic decrease in the emergence of CD43+ primitive hematopoietic progenitors20 (Figure 2A), and a 10-fold decrease in detectable EryP-CFCs (Figure 2B). Because this resembled CHIR99021 treatment of differentiation cultures,4 which causes CDX4 expression (Figure 1C-D), we asked whether induction of CDX4 expression during the same window of time would yield a similar effect as CHIR99021 treatment, resulting in an enrichment of definitive hematopoietic specification.4 Therefore, differentiation cultures did not have WNT signaling manipulated, so as to allow for the specification of both programs (Figure 1A). Under these conditions, the definitive hematopoietic progenitors were still specified with doxycycline treatment, because functional CD34+CD43−CD73−CD184− HE7,12 was still specified with similar efficiency to control conditions (Figure 2C-D; supplemental Figure 2B). However, CDX4 overexpression caused a functional increase within this population, as indicated by a fivefold increase in definitive erythroid progenitors, similar to that observed following CHIR99021 treatment (Figure 2E). Collectively, these observations indicate that mesodermal CDX4 expression recapitulates WNT activation during mesoderm specification,4 resulting in definitive hematopoietic specification and primitive hematopoietic repression.
Figure 2.
Mesodermal CDX4 expression is critical for efficient definitive hemogenic endothelial specification. (A-E) Analyses of primitive and definitive hematopoietic potential following doxycycline-inducible CDX4 expression via the AAVS1 locus. (A) Representative flow cytometric analysis of CD34 and CD43 expression on day 9 of differentiation, following IWP2 and doxycycline treatment from days 2 to 3 of differentiation. (B) Normalized EryP-CFC potential at day 9 of differentiation as in panel A. n = 3 mean ± SEM. Student t test: ***P < .001. (C) Representative flow cytometric analysis of CD73 and CD184 expression within CD34+CD43− cells obtained on day 8 of differentiation, following DMSO treatment, with or without doxycycline, from days 2 to 3 as in Figure 1A. (D) Quantification of CD73−CD184− HE as in panel C. n = 4. Student t test: P > .05. (E) Quantification of definitive erythroid burst forming unit (BFU-E) potential from 1000 CD34+CD43−CD73−CD184− hemogenic endothelial progenitors, following 9 days of hemato-endothelial culture to promote the endothelial-to-hematopoietic transition. n = 3 mean ± SEM. Student t test compared with DMSO: *P < .05. (F-M) Analyses of primitive and definitive hematopoietic potential from CDX4−/Y hPSCs. (F) qRT-PCR analysis of CDX1, CDX2, and CDX4 expression on day 3 of differentiation within wild-type (WT) and CDX4−/Y (knockout [KO]) hPSCs, following CHIR99021 or IWP2 treatment as in Figure 1A. n = 4 mean ± SEM. Student t test: *P < .05; ***P < .001. (G) Representative CD34 and CD43 flow cytometric analyses on day 9 of differentiation following WNT manipulation from days 2 to 3 as in Figure 1A. (H) Primitive hematopoietic potential within day 9 differentiation cultures of WT and CDX4−/Y (KO) hPSCs, following WNT manipulation as in Figure 1A. n ≥ 4 mean ± SEM. Student t test compared across WT and KO, per condition: **P < .01; ***P < .001. (I) Quantification of definitive erythro-myeloid colony-forming potential from CHIR99021-derived CD34+ progenitors, following 9 days of hemato-endothelial culture to promote the endothelial-to-hematopoietic transition. Cultures were treated with CHIR99021 from days 2 to 3 as in Figure 1A. Normalized to 10 000 CD34+CD43− day 8 input cells. n ≥5 mean ± SEM. Student t test: *P < .05. (J) Representative flow cytometric analysis of T-lymphoid potential of WT and CDX4−/Y (KO) hPSCs, under limiting dilution conditions. Shown is T-lymphoid analyses following 28 days OP9−DL4 coculture under T-lymphopoiesis promoting conditions. Input population shown is 10 000 CD34+ progenitors. Limiting dilution analyses indicate WT CD34+ cells possess lymphoid progenitors at a 1:3318 frequency, and KO cells at 1:18 508 frequency. n = 3. P = .00224. (K) Representative flow cytometric analysis of CD73 and CD184 expression within CD34+CD43− cells obtained on day 8 of differentiation, following CHIR99021 treatment from days 2 to 3 as in Figure 1A. (L) Quantification of CD73−CD184− HE as in (K). n > 6. Student t test: ***P < .001. (M) Normalized definitive BFU-E potential from CD34+CD43−CD73−CD184− hemogenic endothelial progenitors, following 9 days of hemato-endothelial culture to promote the endothelial-to-hematopoietic transition. n = 5 mean ± SEM. Student t test: P > .05. CFU-E, erythroid colony-forming unit; DOX, doxycycline; n/s, not significant.
We next used a CDX4 knockout (CDX4−/Y) hPSC line, which completely lacked WT CDX4 expression, whereas CDX1 and CDX2 were still expressed (Figure 2F). Under all differentiation conditions (Figure 1A), CDX4−/Y cultures gave rise to approximately threefold more CD43+ cells (Figure 2G). CDX4−/Y hPSCs gave rise to threefold more EryP-CFCs in the absence of WNT signaling (Figure 2H), likely due to the complete absence of CDX4 expression in comparison with control IWP2-treated cultures (Figure 2F). CHIR99021 treatment still repressed primitive hematopoiesis, suggesting other β-catenin transcriptional targets also repress primitive hematopoietic specification. In contrast, when CHIR99021-derived definitive CD34+CD43− cells were assessed for hematopoietic potential, the CDX4−/Y cells exhibited an approximately sevenfold reduction in HBG-expressing BFU-E potential, and a fourfold decrease in myeloid potential (Figure 2I; supplemental Figure 2C). Further, limiting dilution analyses of T-lymphoid potential revealed a fivefold decrease in lymphoid potential in CDX4−/Y CD34+ cells (Figure 2J), indicating a broad decrease in multilineage definitive hematopoietic potential.
To determine the cause of this, we asked whether CDX4−/Y hPSCs have either defective HE specification or an impaired endothelial-to-hematopoietic transition. CDX4−/Y CD34+CD43− cells exhibited an average fivefold reduction in the specification of CD73−CD184− HE (Figure 2K-L), indicating they have impaired definitive hematopoietic specification. However, this HE population remained functional, giving rise to definitive BFU-E with similar efficiency to control hPSCs (Figure 2M). Because both CDX1 and CDX2 were still expressed under these conditions (Figure 2F), it is possible that either may be redundantly21 contributing to definitive hematopoietic specification in the absence of CDX4, similar to that observed in zebrafish.18 Collectively, these results establish that CDX4 is a key regulator of specifying human definitive hematopoietic progenitors within mesoderm, by regulating the specification of HE, and thus provides a mechanistic basis for WNT-mediated definitive hematopoietic progenitor specification.4
CDX/HOX expression has been suggested to be essential for definitive hematopoietic specification from hPSCs.9,22 Together, our data demonstrate the importance of CDX4 expression for human definitive, but not primitive, hematopoietic progenitor specification within mesoderm, prior to HE emergence. With this insight, it will be possible to interrogate the intrinsic and extrinsic regulators of human definitive hematopoietic specification, so as to ultimately increase hPSC-derived definitive hematopoiesis for regenerative medicine applications.
Acknowledgments
This work was supported by T32 training grants from the National Institutes of Health, National Heart, Lung, and Blood Institute (HL007088-41) (J.P.C. and C.D.) and (HG000045) (M.C.V.); T.E.D. is supported by a grant from the Children’s Discovery Institute of Washington University and St. Louis Children’s Hospital; and C.M.S. is supported by an American Society of Hematology Scholar Award.
Footnotes
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: J.P.C., Q.R., and C.D. designed and performed experiments, and analyzed the data; J.T.K.H. and M.C.V. analyzed expression data; T.E.D. supervised expression analyses; and C.M.S. designed and supervised the research project, performed experiments, analyzed the data, and wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Christopher M. Sturgeon, Washington University in St. Louis, 660 South Euclid Ave, Box 8125, St. Louis, MO 63110; e-mail: csturgeon@wustl.edu.
References
- 1.Dzierzak E, Speck NA. Of lineage and legacy: the development of mammalian hematopoietic stem cells. Nat Immunol. 2008;9(2):129-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Palis J, Malik J, McGrath KE, Kingsley PD. Primitive erythropoiesis in the mammalian embryo. Int J Dev Biol. 2010;54(6-7):1011-1018. [DOI] [PubMed] [Google Scholar]
- 3.Kennedy M, Awong G, Sturgeon CM, et al. . T lymphocyte potential marks the emergence of definitive hematopoietic progenitors in human pluripotent stem cell differentiation cultures. Cell Reports. 2012;2(6):1722-1735. [DOI] [PubMed] [Google Scholar]
- 4.Sturgeon CM, Ditadi A, Awong G, Kennedy M, Keller G. Wnt signaling controls the specification of definitive and primitive hematopoiesis from human pluripotent stem cells. Nat Biotechnol. 2014;32(6):554-561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de Bruijn MF, Speck NA, Peeters MC, Dzierzak E. Definitive hematopoietic stem cells first develop within the major arterial regions of the mouse embryo. EMBO J. 2000;19(11):2465-2474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ivanovs A, Rybtsov S, Welch L, Anderson RA, Turner ML, Medvinsky A. Highly potent human hematopoietic stem cells first emerge in the intraembryonic aorta-gonad-mesonephros region. J Exp Med. 2011;208(12):2417-2427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ditadi A, Sturgeon CM, Tober J, et al. . Human definitive haemogenic endothelium and arterial vascular endothelium represent distinct lineages. Nat Cell Biol. 2015;17(5):580-591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pimentel HJ, Bray N, Puente S, Melsted P, Pachter L. Differential analysis of RNA-seq incorporating quantification uncertainty [published online ahead of print 10 June 2016]. bioRxiv. doi: 1101/058164. [DOI] [PubMed] [Google Scholar]
- 9.Ng ES, Azzola L, Bruveris FF, et al. . Differentiation of human embryonic stem cells to HOXA(+) hemogenic vasculature that resembles the aorta-gonad-mesonephros. Nat Biotechnol. 2016;34(11):1168-1179. [DOI] [PubMed] [Google Scholar]
- 10.Keenan ID, Sharrard RM, Isaacs HV. FGF signal transduction and the regulation of Cdx gene expression. Dev Biol. 2006;299(2):478-488. [DOI] [PubMed] [Google Scholar]
- 11.Lengerke C, Schmitt S, Bowman TV, et al. . BMP and Wnt specify hematopoietic fate by activation of the Cdx-Hox pathway. Cell Stem Cell. 2008;2(1):72-82. [DOI] [PubMed] [Google Scholar]
- 12.Choi KD, Vodyanik MA, Togarrati PP, et al. . Identification of the hemogenic endothelial progenitor and its direct precursor in human pluripotent stem cell differentiation cultures. Cell Reports. 2012;2(3):553-567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davidson AJ, Ernst P, Wang Y, et al. . cdx4 mutants fail to specify blood progenitors and can be rescued by multiple hox genes. Nature. 2003;425(6955):300-306. [DOI] [PubMed] [Google Scholar]
- 14.Davidson AJ, Zon LI. The caudal-related homeobox genes cdx1a and cdx4 act redundantly to regulate hox gene expression and the formation of putative hematopoietic stem cells during zebrafish embryogenesis. Dev Biol. 2006;292(2):506-518. [DOI] [PubMed] [Google Scholar]
- 15.McKinney-Freeman SL, Lengerke C, Jang IH, et al. . Modulation of murine embryonic stem cell-derived CD41+c-kit+ hematopoietic progenitors by ectopic expression of Cdx genes. Blood. 2008;111(10):4944-4953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Paik EJ, Mahony S, White RM, et al. . A Cdx4-Sall4 regulatory module controls the transition from mesoderm formation to embryonic hematopoiesis. Stem Cell Rep. 2013;1(5):425-436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang Y, Yabuuchi A, McKinney-Freeman S, et al. . Cdx gene deficiency compromises embryonic hematopoiesis in the mouse. Proc Natl Acad Sci USA. 2008;105(22):7756-7761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Koo S, Huntly BJ, Wang Y, et al. . Cdx4 is dispensable for murine adult hematopoietic stem cells but promotes MLL-AF9-mediated leukemogenesis. Haematologica. 2010;95(10):1642-1650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sim X, Cardenas-Diaz FL, French DL, Gadue P. A doxycycline-inducible system for genetic correction of iPSC disease models. Methods Mol Biol. 2016;1353:13-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vodyanik MA, Thomson JA, Slukvin II. Leukosialin (CD43) defines hematopoietic progenitors in human embryonic stem cell differentiation cultures. Blood. 2006;108(6):2095-2105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van den Akker E, Forlani S, Chawengsaksophak K, et al. . Cdx1 and Cdx2 have overlapping functions in anteroposterior patterning and posterior axis elongation. Development. 2002;129(9):2181-2193. [DOI] [PubMed] [Google Scholar]
- 22.Ramos-Mejía V, Navarro-Montero O, Ayllón V, et al. . HOXA9 promotes hematopoietic commitment of human embryonic stem cells. Blood. 2014;124(20):3065-3075. [DOI] [PubMed] [Google Scholar]