Abstract
Preeclampsia is a pregnancy-specific condition that leads to increased cardiovascular risk in later life. A decrease in cholesterol efflux capacity is linked to CVD. We hypothesized that in preeclampsia there would be a disruption of maternal/fetal plasma to efflux cholesterol, as well as differences in the concentrations of both placental sterol 27-hydroxylase (CYP27A1) and apoA1 binding protein (AIBP). Total, HDL-, and ABCA1-mediated cholesterol effluxes were performed with maternal and fetal plasma from women with preeclampsia and normotensive controls (both n = 17). apoA1 and apoE were quantified by chemiluminescence, and 27-hydroxycholesterol (27-OHC) by GC-MS. Immunohistochemistry was used to determine placental expression/localization of CYP27A1, AIBP, apoA1, apoE, and SRB1. Maternal and fetal total and HDL-mediated cholesterol efflux capacities were increased in preeclampsia (by 10–20%), but ABCA1-mediated efflux was decreased (by 20–35%; P < 0.05). Maternal and fetal apoE concentrations were higher in preeclampsia. Fetal plasma 27-OHC levels were decreased in preeclamptic samples (P < 0.05). Placental protein expression of both CYP27A1 and AIBP were localized around fetal vessels and significantly increased in preeclampsia (P = 0.04). Placental 27-OHC concentrations were also raised in preeclampsia (P < 0.05). Increased HDL-mediated cholesterol efflux capacity and placental CYP27A1/27-OHC could be a rescue mechanism in preeclampsia, to remove cholesterol from cells to limit lipid peroxidation and increase placental angiogenesis.
Keywords: lipid/efflux, 27-hydroxycholesterol, apolipoproteins, pregnancy, hypertension, sterol 27-hydroxylase
Preeclampsia is one of the three leading causes of maternal morbidity and mortality worldwide, complicating around 2–8% of pregnancies (1). This disorder increases the chance of adverse perinatal outcomes, such as fetal growth restriction and preterm delivery (2). Both the women who develop preeclampsia and their babies are at increased risk of hypertension in later life. Moreover, women with a history of preeclampsia have an 8-fold greater risk of death from CVD (3). The American Heart Association has included preeclampsia as a risk factor in guidelines for preliminary risk evaluation for CVD in women (4). The cause of preeclampsia remains unknown; different lines of evidence indicate that abnormal lipid metabolism is involved in the pathogenesis; the acute atherosis seen in uteroplacental beds in preeclamptic women is one of these (5).
Cholesterol is an essential component required for both placental and fetal development as a precursor of metabolic mediators such as oxysterols (6). The sterol 27-hydroxylase (CYP27A1), a ubiquitously expressed mitochondrial enzyme belonging to the cytochrome P450 family, catalyzes the hydroxylation of cholesterol at C-27 to form 27-hydroxycholesterol (27-OHC) and cholestenoic acid (7). CYP27A1 is also involved in cholesterol efflux, the first and rate-limiting step of reverse cholesterol transport (RCT). RCT is defined as the transport of cholesterol from peripheral organs/macrophages to an acceptor in plasma, followed by its transfer to the liver in order to be eliminated/recycled. Overexpression of CYP27A1, as seen in Chinese hamster ovary cells expressing polyoma LT antigen (CHOP) cells and macrophages (8, 9), results in enhanced cholesterol efflux. Indeed, the appearance of 27-OHC may produce conformal changes in the plasma membrane and facilitate the release of cholesterol and 27-OHC to an acceptor in plasma. The 27-OHC is also a ligand of the liver X-activated receptor, which regulates a number of genes involved in cholesterol homeostasis, in particular ABCA1 (8). Little is known about CYP27A1 expression in the placenta, and we are not aware of any study reporting placental 27-OHC concentrations.
Apolipoproteins are proteins that interact with lipids to form soluble lipid-complexes, allowing the transport of lipids via the circulation. apoE is a major constituent of VLDLs and is an essential ligand for the uptake and clearance of atherogenic lipoproteins, playing important roles in atherosclerosis by modifying inflammatory responses and facilitating cholesterol efflux from foam cells (10, 11). apoA1 is a major apolipoprotein of HDL cholesterol (HDL-C) and is significantly involved in the regulation of lipid transport and metabolism of HDL particles (12). apoAI binding protein (AIBP) is secreted from tissue and physically binds with apoAI (13). AIBP accelerates cholesterol efflux from endothelial cells to HDL-C, thereby regulating angiogenesis via alterations in the composition of the lipid rafts, possibly due to reduced caveolin-1 (CAV-1) and interference with vascular endothelial growth factor receptor (VEGFR)2 signaling (14, 15). Alterations in angiogenic factors have been repeatedly observed in preeclamptic placentae (16) with decreased VEGF-A and VEGFR1 in the cytotrophoblast. Increased plasma apoE polymorphisms have been reported in women with preeclampsia (17, 18); however, findings relating to apoA1 measurements in preeclampsia are conflicting (19, 20). To date, it is not known whether AIBP is expressed in the placenta or altered in preeclampsia.
In our previous study with the same patients used in this study, no significant differences could be demonstrated between groups with regard to the maternal and umbilical venous (fetal) serum LDL cholesterol (LDL-C), HDL-C, total cholesterol (TC), and triglycerides (TGs). However, fetal serum concentrations were significantly lower compared with maternal concentrations in both groups (21).
In a recent study of 2,924 nonpregnant individuals, where baseline assessments were compared with measurements at a mean follow-up of 9.4 years, the addition of cholesterol efflux to traditional risk factors was associated with improved discrimination/reclassification indexes of cardiovascular risk (22). The authors suggested that cholesterol efflux capacity may be a more important factor than simply HDL-C concentrations alone when assessing the risk of a cardiovascular event occurrence. Increased cholesterol efflux capacity was associated with a reduced cardiovascular risk (22).
We hypothesized that maternal and fetal cholesterol efflux, as well as placental CYP27A1 expression, would be increased in preeclampsia. This could be an attempt to remove cholesterol from cells and thus prevent further lipid peroxidation and subsequent oxidative stress, while simultaneously having an atheroprotective role, during pregnancy.
MATERIALS AND METHODS
Subjects and selection criteria
The study consisted of two groups of white European women (17 normotensive, 17 with preeclampsia; Table 1) , where matched maternal, fetal, and placental samples were available. Detailed demographics and outcome data have previously been published (23). Back power calculations using our cholesterol efflux capacity data revealed an 85.5% power with an α of 0.5 to detect the differences observed. The study was approved by the Hospital Ethics Committee of the Nottingham University Hospitals; written informed consent was obtained from each participant. Preeclampsia was defined as systolic blood pressure of ≥140/90 mmHg on two occasions and proteinuria ≥300 mg/l, 500 mg/day, or ≥2+ on a dipstick analysis of midstream urine after 20 weeks (24). The birthweight centile for each baby was computed, correcting for gestation age, sex, maternal parity, and BMI (25). Small-for-gestational-age (SGA) was defined as a centile below the 10th percentile, and appropriate-for-gestational-age (AGA) when the individualized birthweight ratio was between the 10th and 90th percentile (26). All women who took part in this study were laboring and either delivered vaginally or by emergency Caesarean section; no differences were observed in any measurements between Caesarean section and vaginal deliveries.
TABLE 1.
Clinical and obstetric data of subject groups
| Parameter | NC (n = 17) | PE (n = 17) |
| Age (years) | 28.2 ± 7.2 | 31 ± 6.5 |
| BMI at first visit (<14 weeks’ gestation; kg/m2) | 26.4 ± 5.5 | 24.8 ± 3.5 |
| Smoking status | ||
| Nonsmoker | 9 (53) | 11 (65) |
| Smoker | 8 (47) | 6 (35) |
| Parity | ||
| Nulliparous | 11 (65) | 10 (59) |
| Multiparous | 6 (35) | 7 (41) |
| Maximum systolic blood pressure (mmHg) | 114 ± 3.8 | 155 ± 3.8a |
| Maximum diastolic blood pressure (mmHg) | 75 ± 2.1 | 97 ± 5.0a |
| Proteinuria (g/l), median [minimum, maximum] | — | 1.0 [0.3, 9.4] |
| Gestational age at delivery (weeks) | 40 ± 1.0 | 37.7 ± 1.8 |
| Mean birthweight (g) | 3439 ± 498 | 2993 ± 735a |
| Corrected birthweight centile | 27.9 [17.5, 66.8] | 35.1 [8.6, 76.3] |
| Caesarean section | 4 (24) | 13 (76) |
Data represented as mean ± SD or median [IQR] as appropriate, except for smoking status, parity, Caesarean sections, and early-onset PE, which are shown as number (percentage). NC, normotensive control; PE, preeclampsia.
P < 0.05 between NC and women with PE.
Sample collection and measurements
Maternal venous blood samples were taken prior to delivery. Where possible, fetal blood samples were collected from the umbilical cord vein immediately after delivery of the placenta, as previously described (23). All blood samples were collected in EDTA (plasma) or plain tubes (serum).
Full-depth tissue biopsies were collected within 10 min of the placenta being delivered, as previously described (23), sampling half-way between the cord insertion and periphery of the placenta, avoiding infarcts. The lipoproteins (LDL-C, HDL-C, TC, and TG) were previously measured in maternal and fetal serum from the same sample collection (21).
Cholesterol efflux
Cholesterol efflux was determined in RAW264.7 cells (ATCC), as previously described (8), using maternal or fetal plasma as acceptors. Briefly, following labeling for 48 h with 0.2 μCi/ml [3H]cholesterol (Anawa, Switzerland), cells were washed with PBS (pH 7.4), equilibrated for 18 h in OptiMem, and incubated for 2 h in the presence or absence of 5% maternal or fetal plasma. The HDL-mediated cholesterol efflux was performed as described above, using 5% apoB-depleted plasma as the acceptor. For preparation of apoB-depleted plasma, 40 μl polyethylene glycol (20% in 200 mmol/l glycine buffer) were added to 100 μl plasma, incubated at room temperature for 20 min, and the supernatant was recovered after centrifugation (10,000 rpm, 20 min, 4°C), as described by Holzer et al. (27). To measure the ABCA1-mediated efflux, the difference in efflux between control and 8-bromoadenosine 3′,5′-cyclic monophosphate sodium salt-cAMP (8Br-cAMP)-stimulated cells was assessed using 5% plasma as the acceptor. For this, the incubation with OptiMem was replaced with DMEM containing 0.2% fatty acid-free BSA and 0.3 mM 8Br-cAMP.
For all three types of assays, radioactivity was measured in both supernatant and cells. Cholesterol efflux was calculated as the percentage of labeled cholesterol released to the medium divided by the amount of total labeled cholesterol in the medium and cells in each well. To control for inter-assay plate variability, standard pooled plasma was prepared from several healthy (non-pregnant) volunteers and run on each plate as a reference; all assay plates were processed together in a single run. Both intra- and inter-assay coefficients of variation were <5%.
Quantification of apoA1 and apoE
apoA1 and apoE concentrations were determined in plasma using ELISA kits following the manufacturer’s protocol (apoA1, 3710-1HP-2; apoE, 3712-1HP-2; Mabtech, Nacka Strand, Sweden). The inter- and intra-assay coefficients of variation were: apoA1, 2.5% and 2.2% and apoE, 2.5% and 2.8%, respectively.
Cholesterol concentrations
The lipoproteins (LDL, HDL, TC, and TG) were measured in serum as previously described (21) using MicroSlide technology on the Vitros Fusion 5.1 chemistry system (New York, NY). All samples were analyzed in triplicate, with the inter-assay variation being less than 10% and the intra-assay variation less than 5%.
The 27-OHC concentrations
The 27-OHC was quantified by GC-MS in plasma (28) and placenta. For plasma, 200 μl were used. The volume was adjusted to 500 μl with saline and 100 μl butylated hydroxytoluene in 1% pyridine were added to avoid auto-oxidation. One hundred nanograms of 5α-cholestan-3β,6α-diol were used as an internal standard. Saponification was performed with 1.5 ml of ethanolic NaOH 1 M for 2 h at 50°C, neutralized with 1 ml of phosphate buffer 0.1 M (pH 7.0), and pH adjusted to 7 with phosphoric acid. Samples were centrifuged for 5 min at 1,000 g and supernatants were harvested for the following clean-up procedure performed by solid-phase extraction: Sep Pak C18 cartridges were preconditioned with n-heptane/2-propanol (1:1, v/v), methanol, and water before application of the supernatants. The cartridges were washed with methanol/water (3:1, v/v) and dried with nitrogen. The 27-OHC was eluted by n-heptane/2-propanol (1:1) in a tube containing 100 μl butylated hydroxytoluene in 1% pyridine and 100 ng of stigmasterol as a standard for chromatography and derivatization. After evaporation of the solvent under nitrogen, samples were derivatized with 100 μl pyridine and 100 μl N,O-bis-trimethylsilyl-trifluoroacetamide for 1 h at 60°C (29, 30). Samples were diluted with 200 μl of cyclohexane and analyzed by GC-MS by selected ion monitoring. A standard curve containing a mixture of known amounts of each 27-OHC was performed.
For 27-OHC quantification in placenta, 100 mg powdered tissue was homogenized in 1 ml potassium phosphate buffer (pH 7.2) (containing 300 mM sucrose, 0.5 mM dithiothreitol, 10 mM EDTA) and 100 μl butylated hydroxytoluene in 1% pyridine, in Lysing matrix tubes (MPI, Lucerna Chem AG, Switzerland). Cell debris was removed by centrifugation at 1,500 g for 1 min. The supernatant was collected, 100 ng internal standard (5α-cholestan-3β,6α-diol) were added, and lipids were extracted with 19 vol chloroform/methanol (2:1, v/v) for 30 min. Samples were centrifuged at 2,000 g for 5 min and the lipid-containing chloroform layer was collected and transferred into a fresh tube containing 100 μl butylated hydroxytoluene in 1% pyridine. Solid phase extraction, desorption, and derivatization were performed as described for plasma.
CYP27A1 activity was determined in plasma by calculating the ratios of 27-OHC/(27-OHC + cholesterol). Cholesterol values were previously measured and reported in these samples (21).
RNA extraction, cDNA synthesis, and quantitative real-time PCR
Total RNA was extracted from ∼100 mg placental tissue using QIAzol lysis reagent (Qiagen, UK), as previously described (31). RNA (1 μg) was reverse transcribed using the QuantiTect reverse transcription kit (Qiagen) in a Primus96 thermocycler (Peqlab Ltd., UK).
Real-time PCR was carried out using SYBR Green chemistry (2× QuantiFast SYBR Green; Qiagen) on an AB7500 Fast (Life Technologies, UK) using the primers in supplemental Table S1. Abundance data for the genes of interest were expressed following normalization using GeNORM (https://genorm.cmgg.be/), with stably expressed housekeeping genes (GAPDH, β-2-microglobulin, and β-actin) expressed as normalized copy number.
Immunohistochemical staining
Placental protein expression was analyzed by immunohistochemistry, as previously described (31), using CYP27A1 rabbit (14739-1-AP; dilution 1:20; Proteintech), AIBP goat (sc-161321; dilution 1:50; Santa Cruz Biotechnology), SRB1 rabbit (SAB3500048; dilution 1:600; Sigma-Aldrich, UK), and apoA1 rabbit (A8599; dilution 1:300; Sigma-Aldrich) polyclonal antibodies and apoE mouse (HPA001352; dilution 1:250; Sigma-Aldrich) monoclonal antibody. All of the slides were assessed by the same observer, blinded to pregnancy outcome. Quantification was performed as described previously (31), using the Positive Pixel Algorithm of Aperio ImageScope software; a visual check was also performed.
Statistical analysis
All tests were performed using SPSS version 22. Summary data are presented as mean ± SD or median and interquartile range (IQR) as appropriate. The Kruskal-Wallis test, followed by Mann-Whitney U-test was used for multiple group analysis. The Student’s t-test or Mann-Whitney U-tests were used depending on the distribution of the data, after testing using the Kolmogorov-Smirnov test. The null hypothesis was rejected where P < 0.05.
RESULTS
Subjects
The demographic and obstetric data of the 34 participants are shown in Table 1. Within the preeclamptic group, 6 women delivered SGA infants and 11 delivered AGA infants (Table 2) ; no woman in the normotensive control group delivered an SGA infant.
TABLE 2.
Clinical and obstetrics data of the preeclamptic women delivery AGA and SGA infants
| Parameter | PE-AGA (n = 11) | PE-SGA (n = 6) |
| Age (years) | 30.6 ± 7.1 | 31.5 ± 3.9 |
| Gestational age at delivery (weeks) | 38.8 ± 1.2 | 36.5 ± 2.4 |
| Mean birthweight (g) | 3,505 ± 658 | 2,175 ± 611a |
| Corrected birthweight centile | 64.5 [33.5, 86.2] | 4.1 [0.5, 8.5]a |
Data represented as mean ± SD or median [IQR] as appropriate. PE, preeclampsia.
P < 0.05 between PE-AGA and PE-SGA.
Cholesterol efflux
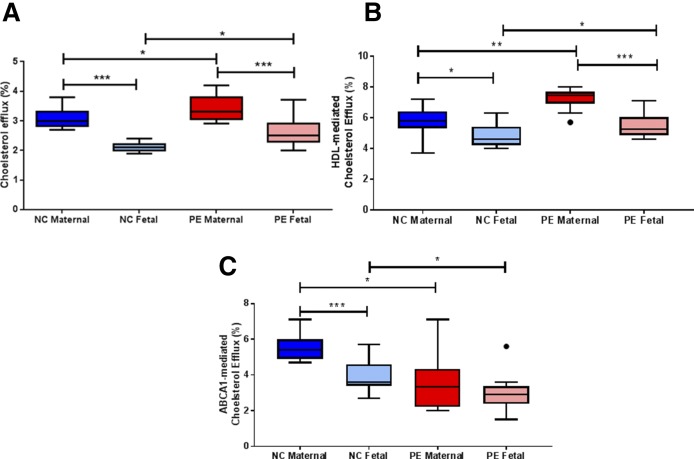
Cholesterol efflux capacity of both maternal and fetal plasma was increased in preeclampsia (by 10.2% and 9.3%, respectively; P < 0.05 for both; Fig. 1A) ; cholesterol efflux capacity was lower in fetal compared with maternal plasma in both study groups (31% and 24%, respectively; P < 0.001 for both; Fig. 1A). In addition, the same differences were observed when HDL-mediated cholesterol efflux capacity was performed with apoB-depleted plasma as an acceptor [increased in preeclamptics by maternal (19.3%) and fetal (12.7%); Fig. 1B]. Conversely, both maternal and fetal ABCA1-mediated efflux was significantly reduced in the preeclampsia samples (by 35% and 20%, respectively; P < 0.05; Fig. 1C). Data of the cholesterol efflux capacity of stimulated and nonstimulated cells can be seen in supplemental Fig. S1.
Fig. 1.
Cholesterol efflux with maternal and fetal plasma. A: Cholesterol efflux capacity (percent). B: HDL-mediated (PEG treated) cholesterol efflux (percent). C: ABCA1-mediated cholesterol efflux from normotensive controls (NC) and preeclamptic (PE) plasma. Data are represented as median [IQR]; *P < 0.05; **P < 0.001; ***P < 0.0001.
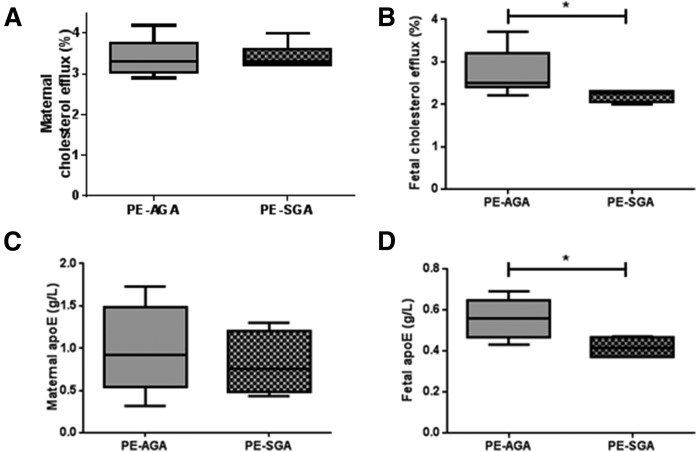
Despite no differences being observed in the maternal cholesterol efflux capacity between groups (Fig. 2A) , the fetal cholesterol efflux capacity was lower in SGA compared with AGA infants only within the preeclamptic group (median [IQR]; SGA, 2.3 [2.1, 2.3]; AGA, 2.6 [2.4, 3.2] percent cholesterol efflux; P < 0.05; Fig. 2B).
Fig. 2.
Cholesterol efflux capacity and apoE in PE with AGA or SGA. Maternal (A) and fetal (B) cholesterol efflux was quantified in preeclamptic pregnancies from AGA (n = 11) and SGA (n = 6). apoE was quantified in maternal (C) and fetal (D) plasma from preeclamptic pregnancies with and without SGA. Data are represented as median [IQR]; *P < 0.05.
apoA1 and apoE concentrations
Maternal apoA1 concentrations were higher than fetal concentrations in both groups (P < 0.05; Table 3) ; no differences were observed for either maternal or fetal apoA1 between normotensive control and preeclamptic women (P > 0.05 for all; Table 3).
TABLE 3.
Maternal and fetal lipoprotein, apoA1, and apoE concentration
| Parameter | NC (n = 17) | PE (n = 17) |
| Lipoprotein concentrations (mmol/l)a | ||
| Maternal TC | 5.6 ± 2.2 | 6.4 ± 1.1 |
| Fetal TC | 2.6 ± 1.5b | 1.7 ± 0.3b |
| Maternal TGs | 2.2 ± 0.7 | 2.6 ± 0.6 |
| Fetal TGs | 1.1 ± 0.9b | 0.7 ± 0.9b |
| Maternal HDL | 1.5 ± 0.3 | 1.4 ± 0.9 |
| Fetal HDL | 0.9 ± 0.4b | 0.6 ± 0.1b |
| Maternal LDL | 3.5 ± 1.9 | 3.8 ± 0.1 |
| Fetal LDL | 1.2 ± 0.8b | 0.8 ± 0.3b |
| apoA1 and apoE concentrations (g/l) | ||
| Maternal apoA1 | 19.3 ± 9.3 | 23.6 ± 7.4 |
| Fetal apoA1 | 2.4 ± 0.9b | 2.8 ± 1.4b |
| Maternal apoE | 0.6 ± 0.4 | 1.0 ± 0.5c |
| Fetal apoE | 0.4 ± 0.1 | 0.5 ± 0.1b,c |
Data represented as mean ± SD. NC, normotensive control; PE, preeclampsia; OHC, hydroxycholesterol.
Lipoprotein concentrations previously measured (21).
P < 0.05 between maternal and fetal samples.
P < 0.05 between normotensive controls and women with preeclampsia.
Maternal plasma apoE was higher than fetal apoE only in preeclampsia (P < 0.0001; Table 3). apoE concentrations were higher in maternal and fetal plasma in the preeclampsia group (P < 0.05; Table 3). In the preeclamptic group, maternal apoE was not changed for SGA infants (Fig. 2C), but fetal apoE was lower in SGA compared with AGA infants (median [IQR]; SGA, 0.42 [0.37, 0.47] g/l; AGA, 0.56 [0.48, 0.64] g/l; P < 0.05; Fig. 2D).
Lipoprotein and 27-OHC concentrations
As previously reported (21), circulating TC, TGs, and lipoproteins were not significantly different between groups, although lower levels were observed in both the fetal normotensive control and preeclamptic groups compared with the maternal samples (Table 3).
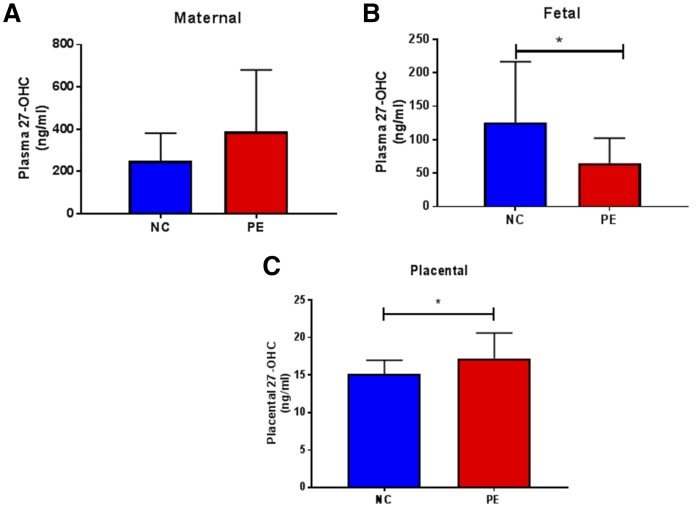
We analyzed 27-OHC concentration as a marker of CYP27A1 activity: this was reduced in fetal compared with maternal plasma, irrespective of diagnostic pregnancy group (Fig. 3A, B). Maternal 27-OHC was slightly, but not significantly, higher in preeclampsia (Fig. 3A). Fetal 27-OHC, however, was significantly reduced in the preeclamptic group (P < 0.05; Fig. 3B). CYP27A1 activity [assessed by the ratio of 27-OHC/(27-OHC + cholesterol)] was unchanged between normotensive women and those with preeclampsia in both maternal (mean ± SD; 0.97 ± 0.01 ng/ml vs. 0.97 ± 0.03 ng/ml) and fetal (0.97 ± 0.02 ng/ml vs. 0.96 ± 0.02 ng/ml) plasma (P > 0.05 for both).
Fig. 3.
Quantification of 27-OHC in maternal plasma (A), fetal plasma (B), and placental tissue (C). The 27-OHC concentrations were quantified by GC-MS in plasma from normotensive controls (NC) and preeclamptics (PE). In the graphs data are represented as mean ± SD; *P < 0.05.
Placental 27-OHC concentrations were significantly increased in tissues obtained from preeclamptic mothers (mean ± SD; normotensive controls, 15.1 ± 1.8 ng/ml; preeclampsia, 17.2 ± 3.4 ng/ml; P < 0.05; Fig. 3C).
Placental CYP27A1, AIBP, apoA1, apoE, and SCB1 expression
Expression of both CYP27A1 and AIBP mRNA was detected in placental tissue, but there were no significant differences between groups for both (median [IQR] normalized copy numbers; normotensive controls vs. preeclampsia) CYP27A1 (1,201 [293, 2,667] vs. 1,013 [677, 6,657]) or AIBP (284 [154, 526] vs. 310 [220, 616]); P > 0.05 for both.
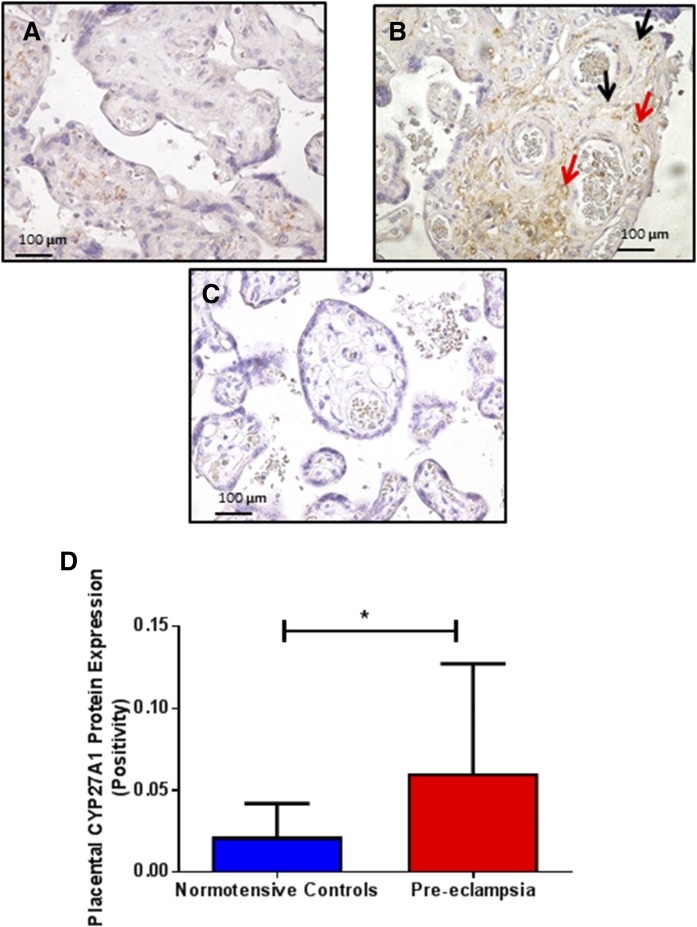
CYP27A1 protein was localized by immunohistochemistry around fetal vessels and in Hofbauer cells (Fig. 4). CYP27A1 protein expression was increased in preeclampsia (mean ± SD; preeclampsia 0.06 ± 0.07; normotensive controls, 0.02 ± 0.02; P = 0.04; Fig. 4). Within the preeclamptic group, CYP27A1 expression was higher in pregnancies delivering SGA compared with AGA infants (mean ± SD; SGA, 0.11 ± 0.01; AGA, 0.04 ± 0.04; P = 0.02). No differences were observed between early- and late-onset preeclampsia and normotensive controls (ANOVA: P > 0.05).
Fig. 4.
Localization and quantification of placental CYP27A1 immunostaining in placentae from normotensive controls (NC; n = 17) (A), preeclampsia (PE; n = 17) (B), and negative control (C). In photomicrographs, positive cells appear in brown; magnification ×400. Protein expression was localized to Hofbauer cells (black arrows) and fetal vessels (red arrows). In the graph (D), data are represented as mean ± SD; *P < 0.05.
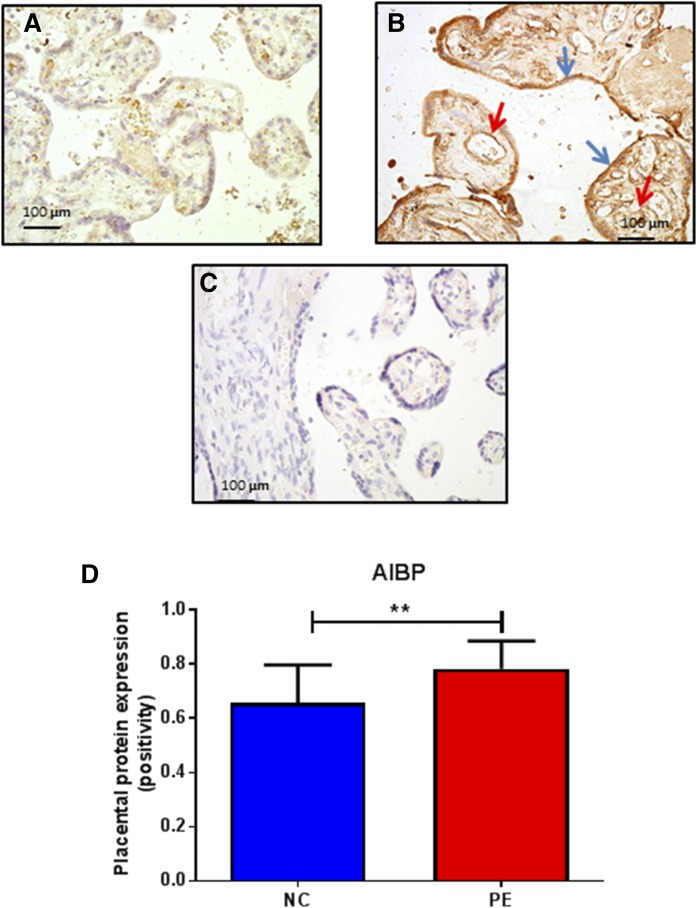
AIBP protein was localized to fetal vessels and syncytiotrophoblasts (Fig. 5). AIBP protein expression was also increased in preeclampsia compared with the control group (mean ± SD; preeclampsia, 0.78 ± 0.10; normotensive controls, 0.66 ± 0.14; P = 0.004; Fig. 5). No differences were found between preeclamptic women delivering an AGA or SGA infant (P > 0.05).
Fig. 5.
Localization and quantification of placental AIBP immunostaining in placentae from normotensive controls (NC; n = 17) (A), preeclampsia (PE; n = 17) (B), and negative control (C). In photomicrographs, positive cells appear in brown; magnification ×400. Protein expression was localized to fetal vessels (red arrows) and syncytiotrophoblasts (blue arrows). In the graph (D), data are represented as mean ± SD; **P < 0.001.
Protein expression of apoA1, apoE, and SCB1 was also confirmed and localized to syncytiotrophoblasts; there were no differences between groups for any of these proteins (P > 0.05; data not shown).
DISCUSSION
It is currently recognized that women who develop preeclampsia have an increased risk of developing atherosclerosis later on in life (32). Low birth weight is one of the classic risk factors for developing CVD in adult life: children born to women who experience preeclampsia in their pregnancy are susceptible to these risk factors in such a way as to develop increased BMI and hypertension at an earlier stage in adulthood than may otherwise occur purely due to aging (33).
Therefore in this study, we compared normotensive women to those with preeclampsia, analyzing the ability of maternal and fetal plasma to remove cholesterol from the cell. We further supplemented our previous lipid profile analyses by quantifying 27-OHC in plasma and CYP27A1 activity, and by assessing the efflux capacity of plasma under various conditions. Additionally, we were able to assess the concentration of 27-OHC in matched placental tissue. This is a novel and detailed study of placental CYP27A1, 27-OHC, and AIBP proteins, strengthened by the determination of cholesterol efflux capacity in matched maternal and fetal plasma samples.
It is well-established that in addition to hypertension, altered cholesterol metabolism is also linked to cardiovascular events. In nonpregnant individuals, a low level of HDL-C is a major independent risk factor for atherosclerotic CVD (34). However, randomized clinical trials aimed at improving HDL-C concentrations have not shown any significant protective effect in cardiovascular outcomes (35), strongly suggesting the importance of alternative mechanisms or combinations of diagnostic biomarkers. It has recently been advocated that a more important factor may actually be the ability of HDL-C to act as an acceptor for the cholesterol discharged from macrophages. Cholesterol efflux is the first and rate limiting step of RCT (22) and animal studies support a direct and causal link between macrophage-specific cholesterol efflux capacity and prevention of atherosclerosis (36). Furthermore, studies have revealed inverse relationships between cholesterol efflux capacity and prevalent coronary artery disease, which are independent of HDL-C levels (37). The role of CYP27A1 in cholesterol efflux has been shown (8), and the deleterious effect of its mutation in patients with cerebrotendinous xanthomatosis underlines the importance of this enzyme in RCT and atherosclerosis prevention.
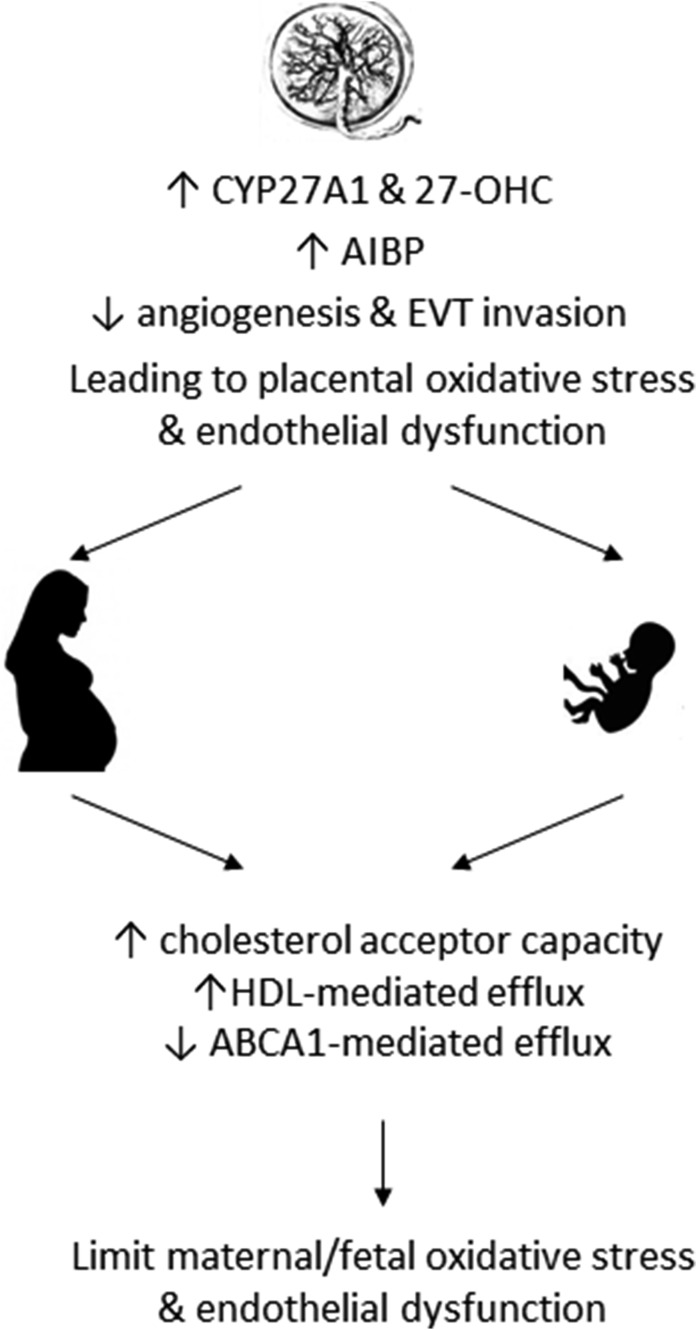
The increased maternal and fetal cholesterol efflux capacity in the preeclamptic group suggests a potential adaptation to extrude cholesterol out of cells in preeclampsia. It is conceivable that a reduction in the oxidation of LDL-C would result in attenuation of lipid peroxidation (Fig. 6). We have previously reported that these fetal samples had lower circulating HDL-C concentrations (21), but when corrected for HDL concentrations, the differences in efflux capacity remained, as did the HDL-mediated efflux. Thus, we might hypothesize that the increased cholesterol efflux capacity in both the women with preeclampsia and their fetuses could be a protective mechanism to prevent excessive lipid peroxidation in these babies. In light of the fact that overall cholesterol efflux capacity is increased in preeclampsia, the specific reduction in ABCA1-mediated cholesterol efflux in preeclampsia suggests that other components of this efflux system may be increased in order to compensate. Because apoE complexed to HDL-C has also been reported to promote cholesterol efflux (38), and as apoE is increased in our preeclampsia group, both maternal and fetal, the apoE-mediated efflux might counteract the reduction in ABCA1-mediated efflux. The increased apoE levels may also have a positive contribution toward offsetting the oxidative stress and inflammatory states reported in preeclampsia (39), through its reported antioxidant and anti-inflammatory role (40).
Fig. 6.
Schematic diagram illustrating the changes observed in preeclampsia to suggest a potential link between changes in cholesterol efflux and the alteration in cholesterol metabolism. The raised placental AIBP may contribute to the impaired angiogenesis/extravillous trophophlast (EVT) invasion, possibly leading to increased oxidative stress and endothelial dysfunction. In contrast, the increased placental CYP27A1, which parallels the increased 27-OHC placenta concentration may lead to the increased cholesterol efflux observed, thus dampening the lipid peroxidation and associated oxidative stress/endothelial dysfunction, providing a compensatory response.
The localization of CYP27A1 protein, around fetal vessels and within Hofbauer cells in the placenta, also points toward a functional role in the cholesterol efflux process facilitating the removal of the cholesterol from the tissue via the vascular circulation. The increased placental CYP27A1 expression and production of 27-OHC in preeclampsia may reflect placental dysfunction, contributing to increased lipid peroxidation within the tissue. Furthermore, placental ABCA1 is known to be downregulated in preeclampsia (41); thus, increased CYP27A1 activity could, at least in part, contribute to a protective mechanism by providing sufficient ligand to activate the LXR-ABCA1 pathway.
In addition, the higher placental CYP27A1 in preeclamptic women delivering SGA infants further supports the notion of inappropriate fetal cholesterol uptake in these cases. Higher fetal and placental oxidized LDL-C concentrations have been reported from women delivering fetal growth restriction infants (42), suggesting a disturbed cholesterol supply to these affected fetuses. Our current study further strengthens this hypothesis reporting even further reduction of fetal cholesterol efflux and apoE concentration in SGA babies from women experiencing preeclampsia in their pregnancy.
Fang et al. (14) have recently reported that effective cholesterol efflux is critical for proper angiogenesis. They observed that both AIBP- and HDL-C-mediated cholesterol efflux alters the composition of the lipid rafts due to reduced CAV-1, as well as interfering with VEGFR1 (KDR) dimerization and signaling, thus inhibiting VEGF-induced angiogenesis (14, 15). The authors concluded that AIBP positively regulates cholesterol efflux from endothelial cells and that effective cholesterol efflux is critical for proper angiogenesis (14). Our current result demonstrating increased placental AIBP together with our previously observed reduction in placental CAV-1 expression in preeclampsia (43) and the reported reduction of VEGFR2 (44), all considered together, intimate at an inappropriate lipid homeostasis. This may inhibit/disrupt placental angiogenesis, contributing to the endothelial dysfunction that is characteristic of preeclampsia. The raised expression in early-onset preeclampsia further supports this theory, as placental dysfunction is only seen in these pregnancies, but not in late-onset preeclampsia. Further studies are required to tease out the balance of positive versus detrimental effects of increased cholesterol efflux in preeclampsia.
Despite there being no significant differences between groups in the mRNA expression of either CYP27A1 or AIBP, both proteins showed an increased expression in placentae from preeclamptic, but not normotensive, women (Figs. 3, 4). This suggests the possible existence of miRNAs, some posttranslational modifications of these proteins, or changes in protein half-life in preeclampsia contributing to the lipid peroxidation. This is further substantiated by the additional increases in protein expression of CYP27A1 and 27-OHC in placentae from preeclamptic mothers.
Melchiorre et al. (45) showed that the majority (56%) of early-onset preeclampsia had stage B asymptomatic heart failure 1 year postpartum (compared with just 14% of late-onset and 8% of controls). Even more concerning was the observation that 40% of these women with previous early-onset preeclampsia developed hypertension within 2 years of pregnancy. Another prospective study, with a long-term follow-up of 37 years, reported the mutually adjusted hazard ratio of subsequent cardiovascular death in preeclamptic women was 2.14, with a 95% CI of 1.29–3.57. For the women who had early-onset preeclampsia, the hazard ratio increased to 9.54 (95% CI: 4.5–20.3), further emphasizing the importance of severity of the syndrome in terms of CVD risks (46). Although sample numbers were small in the present investigation, our data demonstrate increased cholesterol efflux capacity only in late-onset preeclampsia. This indicates that mothers with the more severe form of preeclampsia (i.e., early-onset), as well as their babies, may not have the capacity to protect against lipid peroxidation or have not been exposed to metabolic challenge as those with late-onset disease. Additionally, poor placentation, characteristic of early-onset preeclampsia, has been previously associated with increased lipid peroxidation, further compromising lipid metabolism in both the mother and the fetus. It is possible that this phenomenon may also continue postpartum, but further work is required to test this hypothesis.
Figure 6 summarizes the potential mechanisms relating CYP27A1, 27-OHC, and cholesterol efflux capacity in preeclampsia. The raised placental AIBP may contribute to the impaired angiogenesis and extravillous trophoblast invasion, possibly leading to increased oxidative stress and endothelial dysfunction. In contrast, the increased placental CYP27A1, which parallels the increased 27-OHC placenta concentration, may lead to the observed increased cholesterol efflux, thus trying to dampen the lipid peroxidation and associated oxidative stress/endothelial dysfunction, providing a compensatory response.
A limitation of this study was the relatively low participant numbers, which prevents subgroup analysis between the more severe early-onset and more moderate late-onset forms of preeclampsia (diagnosis before or after 34 weeks’ gestation). Future work includes postpartum follow-up of these women and their offspring, both in the short- and long-term. Exploring alterations in their cholesterol efflux capacity in combination with other known risk factors may provide a novel and more accurate biomarker for prediction of CVD.
Supplementary Material
Acknowledgments
The authors thank the women who participated in the study and the midwives/doctors whose support made this study possible. The authors also thank Ms. Beatrice Rohrbach for performing the ELISAs and the extraction of 27-OHC from placenta, Mr. Jörn Mohaupt for assisting with immunohistochemistry, and Dr. Bernhard Dick for assistance with the GC-MS.
Footnotes
Abbreviations:
- AGA
- appropriate-for-gestational-age
- AIBP
- apoA1 binding protein
- CAV-1
- caveolin-1
- CYP27A1
- sterol 27-hydroxylase
- HDL-C
- HDL cholesterol
- IQR
- interquartile range
- LDL-C
- LDL cholesterol
- 27-OHC
- 27-hydroxycholesterol
- RCT
- reverse cholesterol transport
- SGA
- small-for-gestational-age
- TC
- total cholesterol
- TG
- triglyceride
- VEGFR
- vascular endothelial growth factor receptor
This work was supported by Swiss National Science Foundation Grants 3200B0-113902/1 and 32-135596 (M.G.M.). Additional support was provided by an ERA-EDTA Fellowship (ERA LTF 137-2013) and a British Heart Foundation Basic Science Intermediate Fellowship (FS/15/32/31604) (H.D.M.).
The online version of this article (available at http://www.jlr.org) contains a supplement.
REFERENCES
- 1.Ghulmiyyah L., and Sibai B.. 2012. Maternal mortality from preeclampsia/eclampsia. Semin. Perinatol. 36: 56–59. [DOI] [PubMed] [Google Scholar]
- 2.Duley L. 2009. The global impact of pre-eclampsia and eclampsia. Semin. Perinatol. 33: 130–137. [DOI] [PubMed] [Google Scholar]
- 3.Brown M. C., Best K. E., Pearce M. S., Waugh J., Robson S. C., and Bell R.. 2013. Cardiovascular disease risk in women with pre-eclampsia: systematic review and meta-analysis. Eur. J. Epidemiol. 28: 1–19. [DOI] [PubMed] [Google Scholar]
- 4.Mosca L., Benjamin E. J., Berra K., Bezanson J. L., Dolor R. J., Lloyd-Jones D. M., Newby L. K., Pina I. L., Roger V. L., Shaw L. J., et al. . 2011. Effectiveness-based guidelines for the prevention of cardiovascular disease in women–2011 update: a guideline from the American Heart Association. J. Am. Coll. Cardiol. 57: 1404–1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hubel C. A. 1999. Oxidative stress in the pathogenesis of preeclampsia. Proc. Soc. Exp. Biol. Med. 222: 222–235. [DOI] [PubMed] [Google Scholar]
- 6.Woollett L. A., Buckley D. D., Yao L., Jones P. J., Granholm N. A., Tolley E. A., Tso P., and Heubi J. E.. 2004. Cholic acid supplementation enhances cholesterol absorption in humans. Gastroenterology. 126: 724–731. [DOI] [PubMed] [Google Scholar]
- 7.Norlin M., von Bahr S., Bjorkhem I., and Wikvall K.. 2003. On the substrate specificity of human CYP27A1: implications for bile acid and cholestanol formation. J. Lipid Res. 44: 1515–1522. [DOI] [PubMed] [Google Scholar]
- 8.Escher G., Krozowski Z., Croft K. D., and Sviridov D.. 2003. Expression of sterol 27-hydroxylase (CYP27A1) enhances cholesterol efflux. J. Biol. Chem. 278: 11015–11019. [DOI] [PubMed] [Google Scholar]
- 9.Escher G., Hoang A., Georges S., Tchoua U., El-Osta A., Krozowski Z., and Sviridov D.. 2005. Demethylation using the epigenetic modifier, 5-azacytidine, increases the efficiency of transient transfection of macrophages. J. Lipid Res. 46: 356–365. [DOI] [PubMed] [Google Scholar]
- 10.Curtiss L. K., and Boisvert W. A.. 2000. Apolipoprotein E and atherosclerosis. Curr. Opin. Lipidol. 11: 243–251. [DOI] [PubMed] [Google Scholar]
- 11.Belo L., Gaffney D., Caslake M., Santos-Silva A., Pereira-Leite L., Quintanilha A., and Rebelo I.. 2004. Apolipoprotein E and cholesteryl ester transfer protein polymorphisms in normal and preeclamptic pregnancies. Eur. J. Obstet. Gynecol. Reprod. Biol. 112: 9–15. [DOI] [PubMed] [Google Scholar]
- 12.Zannis V. I., Kardassis D., and Zanni E. E.. 1993. Genetic mutations affecting human lipoproteins, their receptors, and their enzymes. Adv. Hum. Genet. 21: 145–319. [DOI] [PubMed] [Google Scholar]
- 13.Ritter M., Buechler C., Boettcher A., Barlage S., Schmitz-Madry A., Orso E., Bared S. M., Schmiedeknecht G., Baehr C. H., Fricker G., et al. . 2002. Cloning and characterization of a novel apolipoprotein A-I binding protein, AI-BP, secreted by cells of the kidney proximal tubules in response to HDL or ApoA-I. Genomics. 79: 693–702. [DOI] [PubMed] [Google Scholar]
- 14.Fang L., Choi S. H., Baek J. S., Liu C., Almazan F., Ulrich F., Wiesner P., Taleb A., Deer E., Pattison J., et al. . 2013. Control of angiogenesis by AIBP-mediated cholesterol efflux. Nature. 498: 118–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhu L., and Fang L.. 2015. AIBP: a novel molecule at the interface of cholesterol transport, angiogenesis, and atherosclerosis. Methodist DeBakey Cardiovasc. J. 11: 160–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maynard S. E., and Karumanchi S. A.. 2011. Angiogenic factors and preeclampsia. Semin. Nephrol. 31: 33–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Atkinson K. R., Blumenstein M., Black M. A., Wu S. H., Kasabov N., Taylor R. S., Cooper G. J., and North R. A.. 2009. An altered pattern of circulating apolipoprotein E3 isoforms is implicated in preeclampsia. J. Lipid Res. 50: 71–80. [DOI] [PubMed] [Google Scholar]
- 18.Nagy B., Rigo J. Jr., Fintor L., Karadi I., and Toth T.. 1998. Apolipoprotein E alleles in women with severe pre-eclampsia. J. Clin. Pathol. 51: 324–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Var A., Kuscu N. K., Koyuncu F., Uyanik B. S., Onur E., Yildirim Y., and Oruc S.. 2003. Atherogenic profile in preeclampsia. Arch. Gynecol. Obstet. 268: 45–47. [DOI] [PubMed] [Google Scholar]
- 20.Demir B., Demir S., Atamer Y., Guven S., Atamer A., Kocyigit Y., Hekimoglu A., and Toprak G.. 2011. Serum levels of lipids, lipoproteins and paraoxonase activity in pre-eclampsia. J. Int. Med. Res. 39: 1427–1431. [DOI] [PubMed] [Google Scholar]
- 21.Hentschke M. R., Poli-de-Figueiredo C. E., Pinheiro da Costa B. E., Kurlak L. O., Williams P. J., and Mistry H. D.. 2013. Is the atherosclerotic phenotype of preeclamptic placentas due to altered lipoprotein concentrations and placental lipoprotein receptors? Role of a small-for-gestational-age phenotype. J. Lipid Res. 54: 2658–2664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rohatgi A., Khera A., Berry J. D., Givens E. G., Ayers C. R., Wedin K. E., Neeland I. J., Yuhanna I. S., Rader D. R., de Lemos J. A., et al. . 2014. HDL cholesterol efflux capacity and incident cardiovascular events. N. Engl. J. Med. 371: 2383–2393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mistry H. D., Wilson V., Ramsay M. M., Symonds M. E., and Broughton Pipkin F.. 2008. Reduced selenium concentrations and glutathione peroxidase activity in pre-eclamptic pregnancies. Hypertension. 52: 881–888. [DOI] [PubMed] [Google Scholar]
- 24.Brown M. A., Lindheimer M. D., de Swiet M., Van Assche A., and Moutquin J. M.. 2001. The classification and diagnosis of the hypertensive disorders of pregnancy: statement from the International Society for the Study of Hypertension in Pregnancy (ISSHP). Hypertens. Pregnancy. 20: IX–XIV. [DOI] [PubMed] [Google Scholar]
- 25.Gardosi J., and Francis A.. 2006. GROW Customised Centile Calculator. GROW-CCC software v 5.1. Gestation Network. Accessed at https://www.gestation.net. [Google Scholar]
- 26.Cetin I., Foidart J. M., Miozzo M., Raun T., Jansson T., Tsatsaris V., Reik W., Cross J., Hauguel-de-Mouzon S., Illsley N., et al. . 2004. Fetal growth restriction: a workshop report. Placenta. 25: 753–757. [DOI] [PubMed] [Google Scholar]
- 27.Holzer M., Wolf P., Inzinger M., Trieb M., Curcic S., Pasterk L., Weger W., Heinemann A., and Marsche G.. 2014. Anti-psoriatic therapy recovers high-density lipoprotein composition and function. J. Invest. Dermatol. 134: 635–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Winkler B. S., Pecks U., Najjari L., Kleine-Eggebrecht N., Maass N., Mohaupt M., and Escher G.. 2017. Maternal 27-hydroxycholesterol concentrations during the course of pregnancy and in pregnancy pathologies. BMC Pregnancy Childbirth. 17: 106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zurkinden L., Solca C., Vogeli I. A., Vogt B., Ackermann D., Erickson S. K., Frey F. J., Sviridov D., and Escher G.. 2014. Effect of Cyp27A1 gene dosage on atherosclerosis development in ApoE-knockout mice. FASEB J. 28: 1198–1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vögeli I., Jung H. H., Dick B., Erickson S. K., Escher R., Funder J. W., Frey F. J., and Escher G.. 2013. Evidence for a role of sterol 27-hydroxylase in glucocorticoid metabolism in vivo. J. Endocrinol. 219: 119–129. [DOI] [PubMed] [Google Scholar]
- 31.Mistry H. D., McCallum L. A., Kurlak L. O., Greenwood I. A., Broughton Pipkin F., and Tribe R. M.. 2011. Novel expression and regulation of voltage-dependent potassium channels in placentas from women with preeclampsia. Hypertension. 58: 497–504. [DOI] [PubMed] [Google Scholar]
- 32.Bellamy L., Casas J. P., Hingorani A. D., and Williams D. J.. 2007. Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ. 335: 974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Davis E. F., Lazdam M., Lewandowski A. J., Worton S. A., Kelly B., Kenworthy Y., Adwani S., Wilkinson A. R., McCormick K., Sargent I., et al. . 2012. Cardiovascular risk factors in children and young adults born to preeclamptic pregnancies: a systematic review. Pediatrics. 129: e1552–e1561. [DOI] [PubMed] [Google Scholar]
- 34.Stone N. J., Robinson J. G., Lichtenstein A. H., Bairey Merz C. N., Blum C. B., Eckel R. H., Goldberg A. C., Gordon D., Levy D., Lloyd-Jones D. M., et al. . 2014. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 129: S1–S45. [DOI] [PubMed] [Google Scholar]
- 35.Boden W. E., Probstfield J. L., Anderson T., Chaitman B. R., Desvignes-Nickens P., Koprowicz K., McBride R., Teo K., and Weintraub W.. 2011. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N. Engl. J. Med. 365: 2255–2267. [DOI] [PubMed] [Google Scholar]
- 36.Rader D. J., Alexander E. T., Weibel G. L., Billheimer J., and Rothblat G. H.. 2009. The role of reverse cholesterol transport in animals and humans and relationship to atherosclerosis. J. Lipid Res. 50(Suppl.): S189–S194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li X. M., Tang W. H., Mosior M. K., Huang Y., Wu Y., Matter W., Gao V., Schmitt D., Didonato J. A., Fisher E. A., et al. . 2013. Paradoxical association of enhanced cholesterol efflux with increased incident cardiovascular risks. Arterioscler. Thromb. Vasc. Biol. 33: 1696–1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mahley R. W., Huang Y., and Weisgraber K. H.. 2006. Putting cholesterol in its place: apoE and reverse cholesterol transport. J. Clin. Invest. 116: 1226–1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Poston L., Igosheva N., Mistry H. D., Seed P. T., Shennan A. H., Rana S., Karumanchi S. A., and Chappell L. C.. 2011. Role of oxidative stress and antioxidant supplementation in pregnancy disorders. Am. J. Clin. Nutr. 94: 1980S–1985S. [DOI] [PubMed] [Google Scholar]
- 40.Miyata M., and Smith J. D.. 1996. Apolipoprotein E allele-specific antioxidant activity and effects on cytotoxicity by oxidative insults and beta-amyloid peptides. Nat. Genet. 14: 55–61. [DOI] [PubMed] [Google Scholar]
- 41.Baumann M., Korner M., Huang X., Wenger F., Surbek D., and Albrecht C.. 2013. Placental ABCA1 and ABCG1 expression in gestational disease: pre-eclampsia affects ABCA1 levels in syncytiotrophoblasts. Placenta. 34: 1079–1086. [DOI] [PubMed] [Google Scholar]
- 42.Pecks U., Rath W., Caspers R., Sosnowsky K., Ziems B., Thiesen H. J., Maass N., and Huppertz B.. 2013. Oxidatively modified LDL particles in the human placenta in early and late onset intrauterine growth restriction. Placenta. 34: 1142–1149. [DOI] [PubMed] [Google Scholar]
- 43.Smith-Jackson K., Hentschke M. R., Poli-de-Figueiredo C. E., Pinheiro da Costa B. E., Kurlak L. O., Broughton Pipkin F., Czajka A., and Mistry H. D.. 2015. Placental expression of eNOS, iNOS and the major protein components of caveolae in women with pre-eclampsia. Placenta. 36: 607–610. [DOI] [PubMed] [Google Scholar]
- 44.Groten T., Gebhard N., Kreienberg R., Schleussner E., Reister F., and Huppertz B.. 2010. Differential expression of VE-cadherin and VEGFR2 in placental syncytiotrophoblast during preeclampsia - new perspectives to explain the pathophysiology. Placenta. 31: 339–343. [DOI] [PubMed] [Google Scholar]
- 45.Melchiorre K., Sutherland G. R., Liberati M., and Thilaganathan B.. 2011. Preeclampsia is associated with persistent postpartum cardiovascular impairment. Hypertension. 58: 709–715. [DOI] [PubMed] [Google Scholar]
- 46.Mongraw-Chaffin M. L., Cirillo P. M., and Cohn B. A.. 2010. Preeclampsia and cardiovascular disease death: prospective evidence from the child health and development studies cohort. Hypertension. 56: 166–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.