Abstract
Background:
There has not been a general estimation about survival rates of breast cancer cases in Iran. Therefore, the present study aimed to assess survival using a meta-analysis.
Materials and Methods:
International credible databases such as Scopus, Web of Science, PubMed, Science direct and Google Scholar and Iranian databases such as Magiran, Irandoc and SID, from 1997 to 2015 were searched. All articles covering survival rate of breast cancer were entered into the study without any limits. Quality assessment of the articles and data extraction were performed by two researchers using the modified STROBE checklist, which includes 12 questions. Articles with scores greater than 8 were included in the analysis. A limitation of this meta-analysis was different methods for presenting of results in the papers surveyed.
Results:
A total of 21 articles with a sample of 12,195 people were analyzed. The one-year, three-year, five-year and ten-year survival rates of breast cancer in Iran were estimated to be 95.8% (94.6-97.0), 82.4% (79.0-85.8), 69.5% (64.5-74.5), 58.1% (39.6-76.6), respectively. The most important factors affecting survival of breast cancer were age, number of lymph nodes involved, size of the tumor and the stage of the disease.
Conclusion:
The five- and ten- year survival rates in Iran are lower than in developed countries. Conducting breast cancer screening plan support (including regular clinical examination, mammography), public training and raising awareness should be helpful in facilitating early diagnosis and increasing survival rates for Iranian women.
Keywords: Breast cancer, neoplasm, survival rate, meta-analysis, Iran
Introduction
Breast cancer is the most common cancer among women (Baghestani et al., 2015). Over the past fifty years, changes in human lifestyle have led to occurrence and spread of breast cancer throughout the world. The most common symptom of the breast cancer is painless mass which is expressed alone or together with other complaints in 50.0 to 97.0 percent of the cases (Salehi et al., 2011). The rate of breast cancer is 11.0 percent of the total cancers in both men and women (Akbari et al., 2012). Mean age of Iranian breast cancer patients is ten years less than other countries. According to the Iranian report, the age of the disease has decreased in Iranian women from 40.0 to 30.0 years (Fouladi et al., 2011). The results of other study showed, one of the reasons patients attend for treatment in the advanced stages of the disease is lack of screening tests (Brunicardi et al., 2004).
The results of researches done in Iran show that 12.6% of all cancers are breast cancer (Azizi et al., 2000). In Iran, the disease broke out around a decade before developed countries and more than 30% of the patients are under 30 years old (Mousavi et al., 2007).
Around the world, Thirty eight in every one thousand and 25.0 in every one thousand in Iran suffer from cancer. In Iran, 6,456.0 women suffered from breast cancer in 2006 (Fazeli et al., 2014). It is estimated that 651,000.0 women around the world suffer from breast cancer in Asia in 2012 which accounts for 38.8% of all cases in the world, 27.7% in Europe and 15.3% in North America (Kim et al., 2015). A study in China reports that women in East Asia having breast cancer survive less than the U.S (Chuang et al., 2006). The results of a study in British Colombia revealed that Chinese women have the highest survival rate in breast cancer (Hislop et al., 2007). A 5year survival rate is reported 46.0% in India (Yeole et al., 2004), 64.0% in Oman (Al-Moundhri et al., 2004), 78.0% in Belgium (Yeole et al., 2004), and 85.6% in Spain (Martos et al., 2009). In order to estimate the rate of survival in Markazi Province, Fazeli conducted a research and came up with the results that one-, two-, three-, four- and five- year survival rates were 98.0%, 96.0%, 92.0%, 89.0% and 87.0%, respectively (Fazeli et al., 2014).
The survival rate of breast cancer shows the percentage of people who survived after diagnosis for a certain period (Fouladi et al., 2011). In societies with limited access to medical facilities, breast cancer screening can be identified at early stages and lead to increase in survival rate and reduction of mortality (Fallahzadeh et al., 2014). Breast cancer is divided to different stages in terms of the size of tumor, lymph glands involvement, and metastasis that is identified in early stages (Townsend Jr et al., 2012). During recent years, prevention, early diagnosis, and proper treatment are considered to improve survival rate of cancer (Fallahzadeh et al., 2014). It seems that survival rate of breast cancer is low in Iran (Ziaei et al., 2013). Regarding numerous studies and determining survival rate of the breast cancer there is not a pooled estimation. Meta-analysis and systematic survey is an important solution for obtaining a pooled estimation (Moosazadeh, 2013; Moosazadeh et al., 2013). Studies on the analysis of survival of breast cancer should be figured out because up-to-date information on the effective factors in cancer survival is an important factor for doctors and epidemiologists (Janbabai et al,2016). Thus, since breast cancer has a rather high breakout among women and as determining survival rate after diagnosis and treatment is crucial, the present study is performed in order to determine breast cancer survival rate using meta-analysis in Iran. The main question of this study are: 1- what are the one-year, three year and five year survival rate of Iranian women with breast cancer? 2- What are the main associated factors with survival rate?
Material and Method
Research strategy
In this research, in order to find published articles from March 1997 until august 2015, national credible databases such as SID, Magiran and Irandoc and international databases including PubMed, Google scholar, Scopus, and Science Direct were searched by two researchers using key words: Iran, survival rate, breast cancer, tumor, malignancy and neoplasm as a MeSH term and their Farsi equivalents. This searched was carried out from June 9th until August 29th. To ensure receiving all articles, the references were also studied.
Selecting studies: all articles studying survival rate of breast cancer (including cohort, survival and cross-sectional studies) entered the study without any limits. After the title, abstract, and the full-text were studied, repetitive and unrelated articles were excluded. Moreover, in order to avoid bias resulting from re-publication (publication bias) the findings of the articles were analyzed to assess researches published in two journals and omitted from one. Studies with insufficient data not determining the survival rate, abstracts without full-text, case studies, observational-case studies and intervention type studies were excluded.
Quality control: in order to assess the quality of the chosen articles, a checklist prepared in previous research was used (Moosazadeh et al., 2014). Being prepared by analyzing the content of checklist STROB (Von Elm et al., 2008), this checklist includes 12 questions that cover various aspects of methodology like determining proper sample size, type of the study, sampling method, population, data gathering procedures, defining variables and how to analyze the samples, data gathering tools, statistical tests, purposes of the study, presenting findings properly and presenting results based on the stated aims. Each question was scored 1.0 and any study obtaining at least 9.0 scores (Moosazadeh et al., 2014) was sent to meta-analysis.
Criteria for including data
All qualified articles with English and Persian format with one-, two-, three-, four- and five-, seven or ten-years survival rates were selected.
Extracting data: data for each study were extracted based on title of the articles, name of the first author, year, place of conducting the study, size of the sample in each study, diagnosis, one-, two-, three-, four-, five-, seven- and ten-year survival rate and the level of significance of correlation between breast cancer survival rate and variables including side of involvement, size of the tumor, level of tumor malignancy, number of lymph nodes involved, estrogen receptors, the condition of progesterone receptor, age, stage of the disease, condition of metastasis, type of pathology and type of surgery. Moreover, entering data was done by two researchers (Tahmasbi and Farshidi) in Excel spreadsheet.
Analysis: to analyze the data the Stata software was used. The analysis was done using the random effects model. Within-study and between-study heterogeneity were evaluated using the l2.0 and the Tau2 statistics. In this study, survival of 12,195.0 cases of breast cancer was analyzed. It should be noted that Movahedi’s study with a sample of 6,147.0 has determined the survival rate of all patients having breast cancer in Iran between the years 2001 to 2006 (Movahedi et al., 2012). To avoid transverse bias, 1.0 article (Heydari et al., 2012) which overlapped Movahedi’s study in terms of time was excluded.
Publication bias was assessed using Egger’s tests. Results of Egger’s tests showed lack of publication bias (p=0.59).
Results
Description of selected studies
After a preliminary search a number of 21,223.0 documents were identified. after assessing the articles with full text, finally 21.0 articles entered the meta-analysis and systematic survey (Figure 1).
Figure 1.
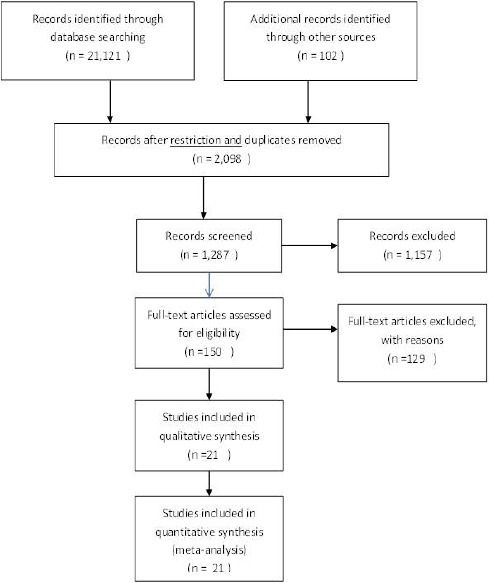
The Process of Search and Selection of Studies According to PRISMA
Figure 2.
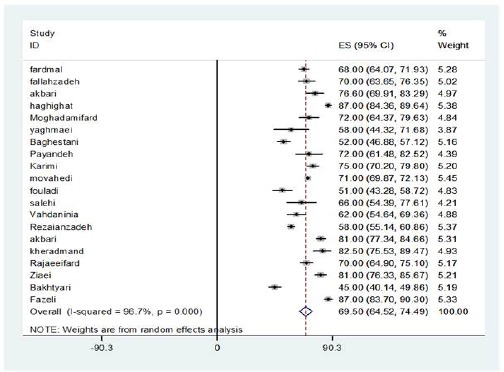
The Rate of Five Year Survival of Breast Cancer in Per Study and Pooled Estimate in Iran
In this meta-analysis, survival rate of 12,195.0 patients having breast cancer in Iran was analyzed. The one-year survival rate-ranging from 92.0% in Sajjadi’s study to 98.0% in Fazeli’s study- is mentioned in 8.0 articles. Regarding the existence of heterogeneity based on random effect model, the one-year survival rate of breast cancer in Iran was estimated to be 95.8% (94.6-97.01) (Q=27.1, I-Squared=74.2%, P=0.04).
The three-year survival rate is reported in 9 studies with a level ranging from 75.0% in Baghestani’s study to 92.0% in Fazeli’s study. The three-year survival rate of breast cancer in Iran was estimated to be 82.4% using random effect model (Q=90.9, I-Squared=91.2%, P<0.001).
The second graph shows the five-year survival rate of breast cancer in each study in general. The five-year survival year ranging from 45.0% in Bakhtiari’s study to 87.0% in Haghighat’s and Fazeli’s study is reported in 20 studies. The five-year survival rate of breast cancer in Iran is estimated to be 69.5% (64.5-74.5) (Q=570.9, I-Squared=96.7%, P<0.001).
The ten-year survival rate of breast cancer ranging from 31.0% in Fardmal’s to 77.0% in Akbari’s study is reported in 6.0 studies. The ten-year breast cancer in Iran was estimated to be 58.1% (39.6-76.6) (Q=329.4, I-Squared=98.5%, P<0.001).
In the present study the mean age of the patients ranged from 46.0 years in Fardmal’s study in 2014 with a sample of 542.0 to 60.3 years in Salehi’s in 2012 with a sample of 64.0. The articles were published from 2004 to 2015. The one-year survival rate was reported in studies (Rajaeefard et al., 2009; Movahedi et al., 2012; Ziaei et al., 2013; Fallahzadeh et al., 2014; Faradmal et al., 2014; Fazeli et al., 2014; Baghestani et al., 2015) with a sample of 7,877.0 people, the two-year survival rate was reported in studies (Movahedi et al., 2012; Haghighat, 2013; Fallahzadeh et al., 2014; Fazeli et al., 2014) with a sample of 7,456.0, the three-year survival rate were reported in studies (Rajaeefard et al., 2009; Rezaianzadeh et al., 2009; Movahedi et al., 2012; Ziaei et al., 2013; Fallahzadeh et al., 2014; Faradmal et al., 2014; Fazeli et al., 2014; Baghestani et al., 2015; Payandeh et al., 2015) with a sample of 9,454 people, the four-year survival rate was reported in studies (Movahedi et al., 2012; Fallahzadeh et al., 2014; Fazeli et al., 2014) with a sample of 6,747.0 people, the five-year survival rate was reported in studies (Vahdaninia and Montazeri, 2004; Akbari et al., 2006; Bakhtiari and Hajian, 2007; Yaghmaei et al., 2008; Rajaeefard et al., 2009; Rezaianzadeh et al., 2009; Kheradmand et al., 2010; Fouladi et al., 2011; Moghadami et al., 2011; Salehi et al., 2011; Akbari et al., 2012; Movahedi et al., 2012; Haghighat, 2013; Ziaei et al., 2013; Fallahzadeh et al., 2014; Faradmal et al., 2014; Farzianpour et al., 2014; Fazeli et al., 2014; Karimi et al., 2014; Baghestani et al., 2015; Payandeh et al., 2015) with a sample 11,923.0 people, the seven-year survival rate was reported in studies (Ziaei et al., 2013; Faradmal et al., 2014) with a sample of 813.0 people and the ten-year survival rate was reported in studies (Yaghmaei et al., 2008; Rajaeefard et al., 2009; Akbari et al., 2012; Ziaei et al., 2013; Faradmal et al., 2014; Payandeh et al., 2015) with a sample of 1,489.0 people (Table 1).
Table 1.
Characteristics of Preliminary Studies into a Meta-Analysis Associated with Breast Cancer Survival Rate
| Id | first author | Publication year | Sample size | Age average | Rate | Survival | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Ten year | Seven Year | Five Year | Four Year | Three Year | Two Year | One year | |||||
| 1 | Farmal | 2014 | 542.0 | 46.1 | 31.0 | 57.7 | 68.0 | 83.8 | 96.8 | ||
| 2 | Fallahzade | 2014 | 200.0 | 48.3 | 70.0 | 76.0 | 82.0 | 86.0 | 95.0 | ||
| 3 | Akbari | 2006 | 154.0 | 48.0 | 76.6 | ||||||
| 4 | Haghighat | 2013 | 623.0 | 46.5 | 87.0 | 96.0 | |||||
| 5 | Moghadamifard | 2013 | 133.0 | 51.3 | 72.0 | ||||||
| 6 | Yaghmaei | 2007 | 50.0 | 51.5 | 47.0 | 58.0 | |||||
| 7 | Baghestani | 2015 | 366.0 | 48.1 | 52.0 | 75.0 | 93.0 | ||||
| 8 | Payandeh | 2015 | 70.0 | 64.0 | 72.0 | 82.0 | |||||
| 9 | Karimi | 2014 | 313.0 | 46.1 | 75.0 | ||||||
| 10 | Movahedi | 2012 | 6147.0 | 49.8 | 71.0 | 75.0 | 82.0 | 88.0 | 95.0 | ||
| 11 | Fouladi | 2011 | 161.0 | 51.0 | |||||||
| 12 | Salehi | 2012 | 64.0 | 60.3 | 66.0 | ||||||
| 13 | Vahdaninia | 2004 | 167.0 | 47.2 | 62.0 | ||||||
| 14 | Rezaianzadeh | 2009 | 1148.0 | 58.0 | 76.0 | ||||||
| 15 | Akbari | 2008 | 441.0 | 53.2 | 77.0 | 81.0 | |||||
| 16 | Sadjadi | 2009 | 118.0 | -- | 92.0 | ||||||
| 17 | Kheradmand | 2010 | 114.0 | 82.5 | |||||||
| 18 | Rajaeeifard | 2009 | 310.0 | 53.0 | 70.0 | 82.0 | 97.0 | ||||
| 19 | Ziaei | 2013 | 271.0 | 48.0 | 76.0 | 79.0 | 81.0 | 86.0 | 96.0 | ||
| 20 | Bakhtyari | 2007 | 403.0 | 45.0 | |||||||
| 21 | Fazeli | 2014 | 400.0 | 50.3 | 87.0 | 89.0 | 92.0 | 96.0 | 98.0 |
Side of involvement
The relationship between side of involvement in breast cancer and the survival is reported in two studies (Akbari et al., 2006; Fallahzadeh et al., 2014) as when the two sides of the breast were involved the survival rate was less (Fallahzadeh et al., 2014). And patients with a tumor in their left breast had longer lives than those with a tumor in their right breast (Akbari et al., 2006).
Size of the tumor
The relationship between size of the tumor and the survival rate of breast cancer is reported in 9 studies (Akbari et al., 2006; Rezaianzadeh et al., 2009; Kheradmand et al., 2010; Moghadami et al., 2011; Haghighat, 2013; Ziaei et al., 2013; Fallahzadeh et al., 2014; Faradmal et al., 2014; Baghestani et al., 2015) as patients with a tumor of 5.0 centimeter and bigger are prone to death twice compared to patients with a tumor of 2.0 centimeters and smaller.
Level of tumor malignancy
The relationship between level of tumor malignancy and breast cancer is reported in two studies, as higher death risk is associated with breast cancer patients with a malignancy level three than the ones with a malignancy level 1.
Number of lymph nodes involved
The relationship between number of lymph nodes involved and breast cancer survival rate is presented in 11.0 articles (Akbari et al., 2006; Bakhtiari and Hajian, 2007; Yaghmaei et al., 2008; Rezaianzadeh et al., 2009; Kheradmand et al., 2010; Moghadami et al., 2011; Salehi et al., 2011; Haghighat, 2013; Fallahzadeh et al., 2014; Faradmal et al., 2014; Baghestani et al., 2015). As the number of lymph nodes involved increases, the death risk also increases (Rezaianzadeh et al., 2009). Patients with more than 10.0 lymph nodes involved survived less than patients with 1.0 to 3.0 lymph nodes involved and patients with between 3.0 to 10.0 nodes involved (Moghadami Fard and Gohari, 2012).
Estrogen receptor
The relationship between estrogen receptor and breast cancer survival rate is reported in 3.0 articles (Akbari et al., 2006; MOGHADAMI et al., 2011; Faradmal et al., 2014). Estrogen receptor was effective in survival, as the patients’ life span with estrogen receptor positive was more than patients with estrogen receptor negative (Akbari et al., 2006).
Progesterone receptor
The relationship between progesterone receptor and breast cancer survival rate is reported in three articles (Akbari et al., 2006; Moghadami et al., 2011; Faradmal et al., 2014). The condition of progesterone receptor has a significant relationship with the patients having cancer, as the death risk of patients with progesterone receptor negative was reported to be more than 1.5 times the patients with progesterone receptor positive (Faradmal et al., 2014).
Age
The relationship between variable ‘age’ and breast cancer survival rate is reported in 14 articles (Vahdaninia and Montazeri, 2004; Akbari et al., 2006; Bakhtiari and Hajian, 2007; Yaghmaei et al., 2008; Rajaeefard et al., 2009; Kheradmand et al., 2010; Moghadami et al., 2011; Movahedi et al., 2012; Ziaei et al., 2013; Fallahzadeh et al., 2014; Faradmal et al., 2014; Fazeli et al., 2014; Baghestani et al., 2015) as for a unit increase of age the ratio of risk becomes 1.02 (Fazeli et al., 2014).
The stage of the disease
The relationship between the stage of the disease and breast cancer survival rate is reported in 8.0 articles (Vahdaninia and Montazeri, 2004; Bakhtiari and Hajian, 2007; Yaghmaei et al., 2008; Rajaeefard et al., 2009; Kheradmand et al., 2010; Moghadami et al., 2011; Akbari et al., 2012; Haghighat, 2013).
The condition of metastasis
The relationship between metastasis and breast cancer survival rate in presented in 3 articles (Rezaianzadeh et al., 2009; Faradmal et al., 2014; Karimi et al., 2014).
Type of pathology
The relationship between type of pathology and breast cancer survival rate is reported in 3 articles (Akbari et al., 2006; Haghighat, 2013; Fallahzadeh et al., 2014). Type of pathology alone does not significantly differ from survival (Akbari et al., 2006).
Surgery
The relationship between variable ‘surgery’ and breast cancer survival rate is reported in three articles (Akbari et al., 2006; Haghighat, 2013; Fallahzadeh et al., 2014) as patients going through surgical operation as their first option survived more than the ones who first received chemotherapy. Type of surgery alone is not significantly different from survival (Akbari et al., 2006).
Discussion
One crucial indicator helping health policy-makers and physicians provide better treatment is to estimate survival rate of a disease. In the present study, the one-, two-, three-, five-, and ten-year survival rate of breast cancer in Iran was estimated to be 95.8, 82.4, 69.5, and 58.1, respectively. The five-year survival rate is reported to be 46.0% in India, 64.0%in Oman, 65.0%in Greece, 75.0%in Germany, 78.0%in Belgium, 89.0%in the United States and 84.0% in the U.K. During recent years, due to advances in health and treatment services the survival rate has increased, as studies carried out to analyze the statistics of cancer in the U.S showed that the survival rate of breast cancer has increased from 85 percent during 1989-1994 to 90.0 percent during 2001-2007. The five-year survival in Germany during the years 2005-2008 is determined to be 88.1%. During the last decade, the five-year survival rate in Eastern Europe has risen from 60 to 73.9%. During the years 2000-2002, the ten-year survival rate of breast cancer in Eastern Europe was 79% and in Englandit was 91.0%. These results reveal that the five- and ten-year survival rate in Iran is much less than European countries and the U.S. Rezaianzadeh et al., (2009) in his study states that one reason for this is Iranian women’s limited awareness of breast cancer. An occupational therapy study in Tehran showed that only 6.0 percent of women regularly self-examined their breasts. A study among immigrant Muslim women from West Asia in the United States reported that none of them regularly self-examined their breasts. Hackshaw and Paul, (2003) in his study concluded that regular self-examination of the breast can improve survival after diagnosis with cancer.
The results of the study show that the most important factors affecting breast cancer survival rate are age, number of lymph nodes involved, size of the tumor, and the stage of the disease. Kümmel et.al (2015), in a study in Germany have regarded age, condition of lymph nodes and size of tumor as risk factors.
Akbari et al., (2006) has also reported that the most important factor affecting the patients’ survival is their axillary lymph node involvement, as patients with lymph nodes involved lived longer than those without lymph nodes involved. If the disease is identified in early stages during which lymph nodes are not involved and the patients receive proper treatment, they will survive more. The death risk for patients with more than 2.0 lymph nodes involved is around two times the patients with less than 2.0 lymph nodes involved. Lymph node involvement increases the death risk by 2.6.
Movahedi et al., (2012) showed in his study that the size of the tumor and the number of nodes involved is considerably related to survival rate. Findings of Fallahzadeh’s study revealed that patients with smaller tumor size survived longer (Fallahzadeh et al., 2014). Also, Kilfoy et.al (2008), found that smaller tumor size contributes to the patient’s survival. Ivanauskiene et.al (2012), in a study in Lithuania and Pajares et al., (2013), in India found the size of tumor to affect survival. Boyages et al., (2010) in a study in Australia reported the size of tumor as an effective factor in breast cancer survival.
The stage of the disease is also reported as one of the most important factors affecting survival. According to the World Health Organization’s report on the status of eastern Mediterranean, the five-year survival rate during the stages zero to four is 92.0%, 87.0%, 75.0%, 46.0%, 13%, respectively. Less survival is observed in various stages of the disease than the zero stage. A study in Indonesia showed that breast cancer was diagnosed in the advanced stages in many cases. In developed countries, the disease is diagnosed at an early stage that leads to better treatment options contributing to patients’ survival.
Larranaga et al., (2009) concluded in his study in Spain that age, stage of the disease, and the level of cellular differentiation affect survival of breast cancer. Kim et al., (2007, 2015) stated in his study of Asian countries that clinical factors of breast cancer such as mean age of diagnosis, stage of the disease, and spread of estrogen and progesterone receptor in Asian countries are different, and the mean age at the time of diagnosis for breast cancer in Asian women is usually between 49.0 and 50.0 years.
The mean age for the U.S women is 56 years. Kümmel et.al (2015), reported the age of 50 as a risk factor in Germany. the results of Fallahzadeh’s study (2014) suggest that women whose age of diagnosis was less than 50 years survived more than women older than 50.
Akbari et al (2006) and Fallahzadeh et al (2014) showed that side of the tumor (left or right breast) affects survival and patients with a tumor in their left breast survived more than the ones having a tumor in their right breast. Verkooijen et al (2007) in his study in Geneva Cancer Registry compared patients infected by two-sided and one-sided tumors with ten-year survival and the results showed that the risk of mortality has considerably risen for women with two sides involved. There is a strong scientific consensus that family record of breast cancer is associated with increased risk of breast cancer, although the probability of risk is different throughout countries. This risk is 1.5 to 2.0 times for Chinese, Japanese and Korean women.
In Haghighat’s study (2013), the estrogen receptor negative is one of the most important factors that significantly cause survival to decrease, as estrogen receptor negative increased relative risk of death from cancer by 2.3. The results of Akbari’s study (2006) also suggested estrogen receptor as affecting survival. Identifying estrogen receptors is crucial in treating patients with receptors positive, since according to valid documents the condition of estrogen receptors is an important factor which prevents from cancer and causes patient’s survival to increase.
Although factors: age, number of lymph nodes involved, condition of estrogen and progesterone receptor, condition of metastasis and size of the tumor are associated with survival of breast cancer patients, early diagnosis of the disease affects some of these factors. Specifically, interventions are required for women with low education since fear and shyness as well as strong cultural factors contributes to avoiding screening services and self-examination. To expand their understanding, qualitative information about breast cancer patients and health care providers, known factors of breast cancer, healthy lifestyle and the importance of early diagnosis should be gathered and intervention educational plans should be provided for the target population in order to decrease death resulting from breast cancer. The results of this study emphasize the importance of planning for on-time diagnosis in developing women health enhancement programs.
Limitation of this meta-analysis was different method for presenting of results, so that, we had to exclude some articles from analysis.
The five-year and ten-year survival rate of breast cancer is much lower in Iran than European countries and the U.S. The most important factors affecting breast cancer survival rate are age, number of lymph nodes involved, size of the tumor and the stage of the disease. It is necessary to raise women’s awareness to regularly referring to doctors and carrying out breast cancer screening plans including regular diagnosis examination, clinical examination and mammography for all women for quicker diagnosis.
References
- Janbabai G, Abedi G, Moosazadeh M, Tahmasebi B, Farshidi F. Determining the Survival Rate of Stomach Cancer in Iran: A Systematic Review and Meta-Analysis. Res J Med Sci. 2016;10:246–255. [Google Scholar]
- Akbari M, Mirzaei H, Soori H. year survival of breast cancer in Shohada-e-Tajrish and Jorjani hospitals. Hakim. 2006;9:39–44. [Google Scholar]
- Akbari ME, Khayamzadeh M, Khoshnevis S, et al. Five and ten years survival in breast cancer patients mastectomies vs. breast conserving surgeries personal experience. Iran J Cancer Prev. 2012;1:53–6. [Google Scholar]
- Al-Moundhri M, Al-Bahrani B, Pervez I, et al. The outcome of treatment of breast cancer in a developing country--Oman. Breast. 2004;13:139–45. doi: 10.1016/j.breast.2003.10.001. [DOI] [PubMed] [Google Scholar]
- Azizi F, Hatami H, Janghorbani M. Epidemiology and control of common diseases in Iran. Tehran: Eshtiagh Publications; 2000. pp. 602–16. [Google Scholar]
- Baghestani AR, Shahmirzalou P, Zayeri F, et al. Prognostic factors for survival in patients with breast cancer referred to Cancer Research Center in Iran. Asian Pac J Cancer Prev. 2015;16:5081–4. doi: 10.7314/apjcp.2015.16.12.5081. [DOI] [PubMed] [Google Scholar]
- Bakhtiari A, Hajian K. Five year disease-free survival rate in breast cancer patients in Rajaii Hospital, Babolsar. J Sch Public Health Inst Public Health Res. 2007;5:53–9. [Google Scholar]
- Boyages J, Jayasinghe UW, Coombs N. Multifocal breast cancer and survival: each focus does matter particularly for larger tumours. Eur J Cancer. 2010;46:1990–6. doi: 10.1016/j.ejca.2010.03.003. [DOI] [PubMed] [Google Scholar]
- Brunicardi F, Andersen D, Billiar T, et al. Schwartz’s principles of surgery. McGraw-Hill Professional; 2004. [Google Scholar]
- Chuang SC, Chen W, Hashibe M, et al. Survival rates of invasive breast cancer among ethnic Chinese women born in East Asia and the United States. Asian Pac J Cancer Prev. 2006;7:221–6. [PubMed] [Google Scholar]
- Fallahzadeh H, Momayyezi M, Akhundzardeini R, et al. Five year survival of women with breast cancer in Yazd. Asian Pac J Cancer Prev. 2014;15:6597–601. doi: 10.7314/apjcp.2014.15.16.6597. [DOI] [PubMed] [Google Scholar]
- Faradmal J, Mafi M, Sadighi-Pashaki A, et al. Factors affecting survival in breast cancer patients referred to the darol Aitam-e Mahdieh center. J Zanjan Univ Med Sci. 2014;22:105–15. [Google Scholar]
- Farzianpour F, Shojaee J, Abedi G, et al. Assessment of quality of life in cancer patients. Amercian J Agri and Biol Sci. 2014;9:147. [Google Scholar]
- Fazeli Z, Najafian Zade M, Eshtati B, et al. Five-year evaluation of epidemiological, geographical distribution and survival analysis of breast cancer in Markazi province, 2007-2011. J Arak Univ Med Sci. 2014;16:73–80. [Google Scholar]
- Fouladi N, Amani F, Harghi AS, et al. Five year survival of women with breast cancer in Ardabil, north-west of Iran. Asian Pac J Cancer Prev. 2011;12:1799–801. [PubMed] [Google Scholar]
- Hackshaw AK, Paul EA. Breast self-examination and death from breast cancer: a meta-analysis. Br J Cancer. 2003;88:1047–53. doi: 10.1038/sj.bjc.6600847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haghighat S. Survival rate and its correlated factors in breast cancer patients referred to breast cancer research center. Iran J Breast Dis. 2013;6:28–36. [Google Scholar]
- Heydari ST, Mehrabani D, Tabei S, et al. Survival of breast cancer in southern Iran. Iran J Cancer Prev. 2012;2:51–4. [Google Scholar]
- Hislop GT, Bajdik CD, Regier MD, et al. Ethnic differences in survival for female cancers of the breast, cervix and colorectum in British Columbia, Canada. Asian Pac J Cancer Prev. 2007;8:209–14. [PubMed] [Google Scholar]
- Ivanauskiene R, Gedminaite J, Juozaityte E, et al. Survival of women with breast cancer in Kaunas Region, Lithuania. Medicina (Kaunas) 2012;48:272–6. [PubMed] [Google Scholar]
- Karimi A, Delpisheh A, Sayehmiri K, et al. Predictive factors of survival time of breast cancer in kurdistan province of Iran between 2006-2014: a cox regression approach. Asian Pac J Cancer Prev. 2014;15:8483–8. doi: 10.7314/apjcp.2014.15.19.8483. [DOI] [PubMed] [Google Scholar]
- Kheradmand AA, Ranjbarnovin N, Khazaeipour Z. Postmastectomy locoregional recurrence and recurrence-free survival in breast cancer patients. World J Surg Oncol. 2010;8:30. doi: 10.1186/1477-7819-8-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilfoy BA, Zhang Y, Shu XO, et al. Family history of malignancies and risk of breast cancer: prospective data from the Shanghai women’s health study. Cancer Causes Control. 2008;19:1139–45. doi: 10.1007/s10552-008-9181-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Y, Choi JY, Lee KM, et al. Dose-dependent protective effect of breast-feeding against breast cancer among ever-lactated women in Korea. Eur J Cancer Prev. 2007;16:124–9. doi: 10.1097/01.cej.0000228400.07364.52. [DOI] [PubMed] [Google Scholar]
- Kim Y, Yoo KY, Goodman MT. Differences in incidence, mortality and survival of breast cancer by regions and countries in Asia and contributing factors. Asian Pac J Cancer Prev. 2015;16:2857–70. doi: 10.7314/apjcp.2015.16.7.2857. [DOI] [PubMed] [Google Scholar]
- Kummel A, Kummel S, Barinoff J, et al. Prognostic Factors for Local, Loco-regional and Systemic Recurrence in Early-stage Breast Cancer. Geburtshilfe Frauenheilkd. 2015;75:710–8. doi: 10.1055/s-0035-1546050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larranaga N, Sarasqueta C, Martinez-Camblor P, et al. Female breast cancer in Gipuzkoa: prognostic factors and survival. Clin Transl Oncol. 2009;11:96–102. doi: 10.1007/s12094-009-0321-2. [DOI] [PubMed] [Google Scholar]
- Martos MC, Saurina C, Feja C, et al. Accurately estimating breast cancer survival in Spain: cross-matching local cancer registries with the National Death Index. Rev Panam Salud Publica. 2009;26:51–4. doi: 10.1590/s1020-49892009000700008. [DOI] [PubMed] [Google Scholar]
- Moghadami FZ, Abolghasemi J, ASGARI DA, et al. Survival analysis of patients with breast cancer using the Aalen’s additive hazard model. J North Khorasan Univ Med Sci. 2011;3:171–80. [Google Scholar]
- Moosazadeh M. Meta-Analysis of Prevalence of Smoking in 15-64-year-old Population of West of Iran. Int J Prev Med. 2013;4:1108–14. [PMC free article] [PubMed] [Google Scholar]
- Moosazadeh M, Nekoei-Moghadam M, Emrani Z, et al. Prevalence of unwanted pregnancy in Iran: a systematic review and meta-analysis. Int J Health Plann Manage. 2014;29:277–90. doi: 10.1002/hpm.2184. [DOI] [PubMed] [Google Scholar]
- Moosazadeh M, Ziaaddini H, Mirzazadeh A, et al. Meta-analysis of smoking prevalence in Iran. Addict Health. 2013;5:140–53. [PMC free article] [PubMed] [Google Scholar]
- Mousavi SM, Montazeri A, Mohagheghi MA, et al. Breast cancer in Iran: an epidemiological review. Breast J. 2007;13:383–91. doi: 10.1111/j.1524-4741.2007.00446.x. [DOI] [PubMed] [Google Scholar]
- Movahedi M, Haghighat S, Khayamzadeh M, et al. Survival rate of breast cancer based on geographical variation in iran, a national study. Iran Red Crescent Med J. 2012;14:798–804. doi: 10.5812/ircmj.3631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pajares B, Pollan M, Martin M, et al. Obesity and survival in operable breast cancer patients treated with adjuvant anthracyclines and taxanes according to pathological subtypes: a pooled analysis. Breast Cancer Res. 2013;15:R105. doi: 10.1186/bcr3572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Payandeh M, Sadeghi M, Sadeghi E, et al. Clinicopathology figures and long-term effects of tamoxifen plus radiation on survival of women with invasive ductal carcinoma and triple negative breast cancer. Asian Pac J Cancer Prev. 2015;16:4863–7. doi: 10.7314/apjcp.2015.16.12.4863. [DOI] [PubMed] [Google Scholar]
- Rajaeefard A, Baneshi M, Talei A, et al. Survival models in breast cancer patients. Iranian Red Crescent Medical Journal. 2009;11:295. [Google Scholar]
- Rezaianzadeh A, Peacock J, Reidpath D, et al. Survival analysis of 1148 women diagnosed with breast cancer in Southern Iran. BMC Cancer. 2009;9:168. doi: 10.1186/1471-2407-9-168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salehi A, Zeraati H, Mohammad K, et al. Survival of male breast cancer in fars, South of iran. Iran Red Crescent Med J. 2011;13:99–105. [PMC free article] [PubMed] [Google Scholar]
- Townsend CM, Jr, Beauchamp RD, Evers BM, et al. Sabiston textbook of surgery. Elsevier Health Sciences; 2012. [Google Scholar]
- Vahdaninia M, Montazeri A. Breast cancer in Iran: a survival analysis. Asian Pac J Cancer Prev. 2004;5:223–5. [PubMed] [Google Scholar]
- Verkooijen HM, Chatelain V, Fioretta G, et al. Survival after bilateral breast cancer: results from a population-based study. Breast Cancer Res Treat. 2007;105:347–57. doi: 10.1007/s10549-006-9455-x. [DOI] [PubMed] [Google Scholar]
- Von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology [STROBE] statement: guidelines for reporting observational studies. Gaceta Sanitaria. 2008;22:144–50. doi: 10.1157/13119325. [DOI] [PubMed] [Google Scholar]
- Yaghmaei S, Bani Hashemi G, Ghorbani R. Survival rate following treatment of primary breast cancer in Semnan, Iran (1991-2002) Koomesh. 2008;9:111–6. [Google Scholar]
- Yeole BB, Kumar AV, Kurkure A, et al. Population-based survival from cancers of breast, cervix and ovary in women in Mumbai, India. Asian Pac J Cancer Prev. 2004;5:308–15. [PubMed] [Google Scholar]
- Ziaei JE, Sanaat Z, Asvadi I, et al. Survival analysis of breast cancer patients in northwest Iran. Asian Pac J Cancer Prev. 2013;14:39–42. doi: 10.7314/apjcp.2013.14.1.39. [DOI] [PubMed] [Google Scholar]


