Abstract
Objectives:
Lung cancer is a major public health problem and one of the most costly illnesses. The study aimed to estimate the economic burden of lung cancer in Iran in 2014.
Methods:
A cross-sectional study was conducted to estimate the direct and indirect costs for patients with lung cancer using a prevalence-based approach. A human capital approach was employed to estimate the indirect costs. Data were obtained from several sources such as through patient interview using structured questionnaire, medical records, the GLOBOCAN databases, the Iranian Statistical Center, the Iranian Ministry of Cooperation, Labor and Social Welfare, and the Institute for Health Metrics and Evaluation (IHME).
Results:
The economic burden of lung cancer in Iran in the year 2014 was 3,225,998,555,090 IR. The main components of the cost were associated with mortality (81.9 %) and hospitalization (7.6 %). The costs of direct medical care, non-medical aspects, patient time, and mortality accounted for 10.8%, 2.7%, 4.5%, and 81.5% of the total cost, respectively.
Conclusion:
Findings from this study indicated that the economic burden of lung cancer is substantial both to Iran’s health system and to society as a whole. Early diagnosis, strengthening cancer prevention, implementing new cancer therapy and medical technology, and effective smoking-cessation interventions could offset some of the costs associated with lung cancer in Iran.
Keywords: lung cancer, prevalence approach, economic burden, Iran
Introduction
Lung cancer (LC) is one of the major cause of cancer deaths in the world regardless of the economic status of countries (Yabroff, Lund et al. 2011, Pakzad, Mohammadian-Hafshejani et al. 2015). According to the WHO, LC was the 9th cause of death and accounted for about 2 % of the total deaths in 2002. It is estimated that LC will be the 7th cause of death and will attribute to 3 % of the total deaths by 2030 (WHO, 2006; Bab et al., 2016). In Iran in 2012, there was a total of 4361 lung cancer-related death. This figure accounted for close to 10 % and 6 % of the deaths due to the top ten cancer related deaths among males and females respectively (Khorasani et al., 2015).
The American Cancer Society estimated that the total cost of lung cancer in the United States for the year 2010 was 268 billion USD consisting of 102.8 billion USD direct and 165.2 billion USD indirect costs. Lung cancer is usually closely associated with smoking. In Iran the prevalence of smoking among adult (15 - 64 years) males is about 26.6% while among females it is 4.2% (Mehrabi et al., 2007). Evidence indicates that 54.7% the deaths from lung cancer among the males and 20.3 % among the females was attributable to smoking (Rezaei et al., 2015). Another study also has revealed that cigarette smoking imposes a significant financial burden on hospitals in Iran. The mean cost of hospitalization and length of hospital stay among lung cancer patients of current and former smokers was more than those never smoke (Akbari Sari et al., 2016). Generally, the LC poses a high financial burden both to the health system and society as a whole. In Iran, the total cost of premature mortality due to the 10 most common cancers was estimated at US$ 1.93 billion. Of which the cost of death due to LC attributed to about 10% males and 5% females respectively (Khorasani et al., 2015).
Health policy makers are concerned about the high financial burden of cancers on society. Besides, they are interested in understanding the actual economic burden of the disease to decide on better ways of healthcare resources allocation among disease categories and to investigate the cost - effectiveness of public health intervention. To our best knowledge few studies reported about the economic burden of lung cancer in Iran. One study examined the cost of lung cancer treatment in the first year after diagnosis (Mohagheghi et al., 2011) while another study measured the direct cost of cancer treatment (Akbarzadehbaghban et al., 2009). This study aims to estimate the economic burden of lung cancer (both direct and indirect costs) using the prevalence of LC approach in Iran for the year 2014.
Material and Methods
This cross-sectional study was carried out during 21 March 2014 to 22 March 2015. The prevalence- and incidence-based approaches are the two main methods employed to estimate the economic burden of diseases such as cancers (Hodgson and Rice, 1982; Yabroff et al., 2011; Daroudi et al., 2015). In this study, the prevalence-based approach was used to estimate the direct and indirect costs of patients with LC. The direct costs include direct medical costs (such as the cost of doctor’s visit, surgery, diagnostic tests, medications, hoteling and nursing care) and direct non-medical costs (costs of travel to the health provider, accommodation, food, caring for family members such as the elderly or children in the absence of the patient and other utility costs such telephone bill). The indirect costs are related to premature mortality and patient time costs. The patient time costs include the value of time lost from activities due to the illness and disability and the mortality costs including the value of life lost prematurely from the disease. The total number of LC patient estimate for the analysis was obtained from the GLOBOCAN database of 5-year prevalence estimate for Iran.
Study Sampling and Data Collection
Direct cost
Inpatient care costs
In Iran, inpatient care is delivered in hospitals owned by different providers of the health system network. The public hospitals under the Ministry of Health and Medical Education (MOHME) are the main providers of inpatient services with 68% of the total hospital beds. This is followed by the private hospitals with 12%, social security organization hospitals with 9%, and armed force hospitals with 4% of the total hospital beds for providing inpatient service in the country respectively. The rest of the hospital beds are related to the Oil Company and non-governmental organizations (NGOs) that are considered public hospitals in this study.
To determine the samples size for the study, initially medical records of 50 patients discharged from one public hospital were reviewed. Based on the average and variance of the cost of hospitalization, a total of 501 patients were discharged during the study period. The medical records of patients were randomly selected using the proportionate allocation to hospital beds of the different providers. Thus, 373 records were from six public hospitals, 61 from two private hospitals, 45 from two social security hospitals and the remaining 22 from one armed forces hospital.
A self-constructed pre-tested checklist was used to obtain the hospitalization costs. The data on age, sex, length of hospital stay and cost of hospitalization and its subgroups (such as the cost of physician’s visit, surgery, hoteling, medication, nursing care, diagnostic tests) was extracted from the medical records of the patients.
Out patient cost and non-medical costs
A self-administered structured questionnaire was adapted from that developed by Longo for a similar study in Canada (Longo 2005), by Gordon in Australia (Gordon, Ferguson et al. 2009) and Bazyar et al in Iran (Bazyar, Akbari et al. 2012) to collect the data. We A pilot study among 20 patients with lung cancer using face-to-face interview was initially carried out to estimate the cost of outpatient service in the last month. Then, the cost for the month was multiplied by 12 to estimate the total outpatient cost for the past one year. Based on the average and variance of the cost of outpatient, the computed sample size for the study was 200 patients. The questionnaire was completed by the patients or by their families when they need assistance in writing their responses. The data on age, sex, income, work days lost due to receiving healthcare, total direct healthcare cost and total direct non-healthcare costs was obtained using the questionnaire.
Indirect costs
Patient Time Costs
The patient time costs were estimated from the average number of days each patient lost due to receiving healthcare. This was obtained from the medical records on hospitalization and from the outpatient care using the self-administrated questionnaire. Then the average number of the lost days was multiplied by the average daily wage. The minimum daily wage approved by the Iranian Ministry of Cooperation, Labor and Social Welfare in 2014 was used to calculate the cost of time due to hospitalization. For the outpatient care, the average daily income of the patient was estimated by dividing the monthly wage by thirty. Finally, the patient time costs were calculated by multiplying the average number of lost days by the average daily wage.
Premature Mortality Costs
The human capital and willingness to pay approaches are two main approaches for estimating the mortality costs. As in previous studies (Yabroff et al., 2011, Daroudi et al., 2015, Rezaei et al., 2015), this study applied the human capital approach for estimating the mortality costs of lung cancer. The total number of deaths of persons in different age groups due to LC in 5-years was extracted from the Institute for Health Metrics and Evaluation (IHME), and Global Burden of disease (GBD). The present discounted value of lifetime earnings (PVLE) per death by gender and age group was estimated using an approach developed by Max and Rice et al (Max et al., 2004) as follow:
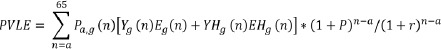
Where:
PVLEa, g = Present discounted value of lifetime earnings for a person of age a and gender g
Pa, g(n) = Probability that a person of age a and gender g will survive to age n
a = Age of the person at death
g = Gender of the person
Yg(n) = Mean annual earnings of an employed person of gender g and age n
Eg(n) = Proportion of the population of gender g and age n that are employed in the labor market
YHg (n) = Mean annual imputed value of household production for a person of gender g and age n
EHg (n) = Proportion of the population of gender g and age n that are doing housekeeping
P = Growth rate of labor productivity (3 % was considered, mean economic growth in the past 30 years)
r = Discount rate (5 % was considered)
Furthermore, the total mortality cost was estimated by following equation:
Premature Mortality Cost=Tdeath*PVLE
Where: Tdeath is the total number of deaths from lung cancer.
Data on age- and sex-specific wages for the study period was used from the Iranian Ministry of Cooperation, Labor and Social Welfare. Besides, the data on age and sex-specific employment and housekeeping rate for the study period was obtained from the Iranian Statistical Center (Arrieta et al., 2015). Because there was no any data concerning the wage for housekeeping activity in Iran, the minimum daily wage approved by the Iranian Ministry of Cooperation, Labor and Social Welfare was used for the females engaged in housekeeping activities. The probability that a person of age a and gender g will survive to age n was obtained from the World Health Organization. Our study considered the age of less than 65 years (retirement age in Iran is 65 year old) to determine the cost of lost productivity both for the patient time and premature mortality. The cost data is presented in the original currency, Iranian Rial (IR), where 25,825 IR was approximately equivalent to one USD in the year 2014 to 2015.
Ethics
The Ethics Committee of the Deputy of Research of the Kermanshah University of Medical Sciences approved the study protocol (KUMS.REC.1395.401).
Results
Based on the 5-year prevalence, the number of patients and deaths due to lung cancer in Iran was estimated to be 4777 and 4509, respectively.
Inpatient costs (cost of hospitalization)
Of the total sample 501 patients, review of the medical records indicated that males accounted for 72.5%. The mean age of the patients with standard deviation (SD) was 61.4 ± SD 9.4 years. The length of hospital stay ranged from one to 52 days with mean length of stay of 10.7 ± SD 8.6 days. The average cost of hospitalization was 41,276,720 ±SD 38,631,730 IR. The average cost of hospitalization for male was 40,937,790 IR while for female it was 42,168,250 IR. Further analysis revealed that the average cost of hospitalization per day for male and female LC patients was 3,858,414 and 3,861,559 IR respectively. The distribution of cost drivers for hospitalization among LC patients is presented in Table 1.
Table 1.
Average Cost and Total Cost of Hospitalization for Patients with Lung Cancer in Iran, 2014
| Service Item | Mean cost | Total cost | Total cost (%) | |||
|---|---|---|---|---|---|---|
| Male | Female | Male | Female | Male | Female | |
| Visiting physicians | 5,583,580 | 6,173,130 | 18,208,054,380 | 9,346,118,820 | 13.6 | 14.6 |
| Medication | 12,643,230 | 14,097,300 | 41,229,573,030 | 2,134,331,220 | 30.9 | 33.4 |
| Surgery | 3,314,110 | 1,980,340 | 10,807,312,710 | 2,998,234,760 | 8.1 | 4.7 |
| Diagnostic tests | 7,674,740 | 7,889,040 | 25,027,327,140 | 11,944,006,560 | 18.7 | 18.7 |
| Hoteling | 10,771,600 | 10,644,880 | 35,126,187,600 | 16,116,348,320 | 26.3 | 25.2 |
| Nursing Care | 950,520 | 1,383,540 | 3,099,645,720 | 2,094,679,560 | 2.3 | 3.3 |
Based on the total number of LC patients and the average cost of hospitalization, the total cost of hospitalization among the LC patients in Iran for the year 2014 was computed at 197,340,800,800 IR. The total cost of hospitalization for males was 133,498,100,580 IR while for females it was 63,842,700,220 IR. The main cost derivers of hospitalization were related to medication (30.9 % in male vs. 33.4 % in female) and hoteling (26.3 % in male vs. 25.2 % in female). There was no difference between male and female patients in the distribution of the cost derivers of hospitalization.
Outpatient and Direct Non-Medical Costs
Of the 200 LC patients studied to estimate the cost of outpatient and non-medical costs, males attributed to 71.5%. The age of the patients ranged from 39 to 91 years with average age of 64.2 ±SD years. The average medical outpatient costs for males aged 35-64 years, and 65 years and above were 21,465,000 and 21,028,570 IR respectively while for females in the same age category, the costs were 21,069,230 and 24,096,770 IR respectively. The average non-medical costs for males aged 35-64 years, and 65 years and above were 17,812,500 and 18,247,620 IR respectively whereas for females in the same age category the costs were 18,692,310 and 18,774,190 IR respectively.
Patient time costs
The average lost workdays for males in receiving outpatient care was 40.9 days whereas for females it was 31.2 days. Beside, the average lost workdays for males and females in receiving inpatient care was 22.2 days and 18.8 days respectively. The total patient time cost was 136,860,835,250 IR for males and 9,613,058,920 IR for females.
Premature mortality costs
A total of 1858 patient in the age group 35-64 years died from LC. The total mortality cost was 2,643,072,539,510 IR. Of the total cost of mortality, the costs of mortality for males and females attributed to 1,968,366,704,570 IR and 674,705,834,940 IR respectively.
Total cost of lung cancer in Iran for 2014
The total cost of LC in Iran for the year 2014 is presented in Table 2 and the economic burden was found to be 3,225,998,555,090 IR. The main cost components were mortality (81.9 %) and hospitalization (7.6 %) (Figure 1).
Table 2.
Total Cost of Lung Cancer in the Iran, 2014
| Types of costs | Gender | Total cost | Total cost (%) | |
|---|---|---|---|---|
| Male | Female | (IR) | ||
| Hospitalization | 171,842,217,730 | 74,369,134,320 | 246,211,352,050 | 7.6 |
| Medical cost of outpatients | 69,175,133,570 | 34,142,225,060 | 103,317, 358,630 | 3.2 |
| Non-medical of cost | 58,906,323,790 | 28,017,086,940 | 86,923,410,730 | 2.7 |
| Patients time | 136,860,835,250 | 9,613,058,920 | 146,473,894,170 | 4.5 |
| Mortality cost | 1,968,366,704,570 | 674,705,834,940 | 2,643,072,539,510 | 81.9 |
| Total cost | 2,405,151,214,910 | 820,847,340,180 | 3,225,998,555,090 | 100.0 |
Figure 1.

Main Components of the Cost of Lung Cancer, Iran, 2014
Discussion
Lung cancer (LC) has a significant financial burden on patients and their families, health system and a society as a whole. This study estimated the economic burden of LC in Iran in the year 2014. The total economic cost of LC accounted for 3,225,998,555,090 IR. The direct medical care costs, direct non-medical costs, patient time costs, and mortality costs accounted for 10.8%, 2.7%, 4.5% and 81.5% of the total cost respectively.
Making comparisons of the findings in our study with findings of previous similar studies is not straightforward. This is mainly due to differences in patient characteristics, wage, male and female patient participation rate, cost of health services as well as the methodologies employed. Previous studies on the cost of LC reported a total cost of 15 - 20% of all the costs of cancer care. The hospitalization, mortality and indirect costs accounted were found to account for the largest part of the direct, indirect and total costs respectively (Goodwin and Shepherd, 1998; Molinier et al., 2006, Luengo-Fernandez et al., 2013). Another study found the total economic cost of cancer to be $9.4 billion, in which it was about 1.7% of the GDP. Furthermore, the medical care, non-medical, morbidity, and mortality costs accounted for 13.7%, 6.5%, 14.5%, and 65.3% of total cost respectively (Kim et al., 2008).
Our findings revealed the total healthcare cost for LC to be 349,528,710,680 IR. The main cost derivers were the cost of hospitalization and outpatient care that accounted for 70.5% and 29.5% of the total healthcare costs of LC respectively. Others reported an average LC care cost of 85,392 USD during the last year of life. The largest proportion of this cost was associated with hospitalization costs (Yabroff et al., 2008). Kutikova et al also investigated the economic burden of LC and associated costs of treatment failure in USA. The study followed patients with LC for a maximum of two years from first LC diagnosis until death of the patient and assessed the cost of the control (people without any cancer) and patient groups. The total cost for the patients was 45,897 USD while for the controls it was 2907 USD. The main component of the cost was hospitalization cost, which accounted for 49.0% of the total cost (Kutikova et al., 2005). Besides, another study in USA on direct cost of LC during the first year after diagnosis was reported to be 39,891 USD per patient (Warren et al., 2008) while in in China it was 25,648,000 Chinese won (Kim et al., 2009).
The medical costs of LC in developing countries like Iran is lower than that in developed countries. The cost of health services in Iran is also less than the cost in some other Middle Eastern countries and developed countries (Daroudi et al., 2015). In addition, there are considerable differences in the tariff of outpatient and inpatient healthcare services between the public sector and private sector. The tariff for private sector is generally much higher than for the public sector. For example, the hospitalization tariff for private hospitals was three times higher compared to the tariff for public hospitals. Similarly, the tariff for health services in the public sector in Iran is much lower than the tariff of services in the private sector. However, the cost of care for cancer treatment including LC is not fixed and may increase in the coming years (Doshmangir et al., 2012). Generally the resources available for health-related needs are limited and demands appropriate planning for the better use of the limited healthcare resources. Availing timely and adequate information about the costs of diseases and their complications provides an opportunity for health-policy makers to make informed comparison in the use of the limited resources.
This study is not free from limitations and any interpretation of the results should take into account the limitations. This study was based on the prevalence of LC and deaths due to LC data extracted from GLOBOCAN, IHME and GBD estimates. Hence, it lacks precise representativeness at national level. Besides, the productivity losses due to premature mortality, absenteeism from work and other productivity losses because of morbidity including early retirement and reduction in employment are not included in this study. The human capital approach was used to estimate the premature mortality and patient time costs. This method underestimates the value of life for women, older age and children. Furthermore, this study did not consider informal and intangible costs (pain, suffer and grief as well as decreased quality of life) as it was difficult to obtain them.
In conclusion, this study indicated that the economic burden of LC in Iran in 2014 was considerable and accounted for about 3,225,998,555,090 IR. The majority of the costs were associated with premature mortality. The costs associated with LC in Iran can be reduced through strengthening preventive measures including early diagnosis and effective medical interventions.
Acknowledgments
This study was extracted from an approved project by Kermanshah University of Medical Sciences and was funded and supported by the Research Deputy of Kermanshah University of Medical Sciences. We also thank Dr. Delavari from the Department of Health Management and Economics, School of Public Health, Tehran University of Medical Sciences for the revision of our manuscript and for the constructive scientific comments to improve our work.
Conflict of Interest
The authors declare that there is no conflict of interest.
Authors’ contributions
All the authors equally contributed to the development of the manuscript and read and approved the final work.
References
- American Cancer Society. Cancer facts and figures 2006. 2010. http://www.cancer.org/downloads/STT/CAFF2006PWSecured.pdf .
- Ministry of health and medical education. Diagnostic and treatment services tariffs in public and private sectors. 1st ed. Tehran, Iran, (inpersion): Rahavard; 2012. [Google Scholar]
- Akbarzadehbaghban A, Esmaeili M, Kimiafar K. Medical information management and assessment of direct costs of treatment of lung cancer. Health Inf Manage. 2009;5:151–8. [Google Scholar]
- Akbari-Sari A, Rezaei S, Arab M, et al. Effects of Smoking on cost of hospitalization and length of stay among patients with lung cancer in Iran: a hospital based study. Asian Pac J Cancer Prev. 2016;17:4421–26. [PubMed] [Google Scholar]
- Arrieta O, Quintana-Carrillo RH, Ahumada-Curiel G, et al. Medical care costs incurred by patients with smoking-related non-small cell lung cancer treated at the National Cancer Institute of Mexico. Tob Induc Dis. 2015;12:1. doi: 10.1186/s12971-014-0025-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bab S, Abdifard E, Moradi Y, Faraj A, Heidari M. Lung cancer incidence trends in Iran and in six geographical regions of the country (2000-2005) Shiraz E-Medical Journal. 2016;17:e38237. [Google Scholar]
- Bazyar M, Akbari F, Mahmoudi M. Medical and non-medical direct costs of cancers in patients hospitalized in Imam Khomeini cancer institution-2010. Hospital. 2012;11:39–50. [Google Scholar]
- Daroudi R, Sari AA, Nahvijou A, et al. The Economic burden of breast cancer in Iran. Iran J Public Health. 2015;44:1225–33. [PMC free article] [PubMed] [Google Scholar]
- Doshmangir L, Rashidian A, Akbari SA. Unresolved issues in medical tariffs: challenges and respective solutions to improve tariff system in Iranian health sectors. Hospital. 2012;4:21–30. [Google Scholar]
- Goodwin PJ, Shepherd FA. Economic issues in lung cancer: a review. J Clin Oncol. 1998;16:3900–12. doi: 10.1200/JCO.1998.16.12.3900. [DOI] [PubMed] [Google Scholar]
- Gordon LG, Ferguson M, Chambers SK, Dunn J. Fuel, beds, meals and meds: out-of-pocket expenses for patients with cancer in rural Queensland. Cancer Forum. Cancer Council Australia. 2009;33:206–13. [Google Scholar]
- Hodgson T, Rice D. Cancer epidemiology and prevention. Philadelphia, PA: WB Saunders Company; 1982. Economic impact of cancer in the United States; pp. 208–28. [Google Scholar]
- Khorasani S, Rezaei S, Rashidian H, Daroudi R. Years of potential life lost and productivity costs due to premature cancer-related mortality in Iran. Asian Pac J Cancer Prev. 2015;16:1845–50. doi: 10.7314/apjcp.2015.16.5.1845. [DOI] [PubMed] [Google Scholar]
- Kim SG, Hahm MI, Choi KS, et al. The economic burden of cancer in Korea in 2002. Eur J Cancer Care. 2008;17:136–44. doi: 10.1111/j.1365-2354.2007.00818.x. [DOI] [PubMed] [Google Scholar]
- Kim SY, Kim SG, Park JH, Park EC. Costs of initial cancer care and its affecting factors. J Prev Med Public Health. 2009;42:243–50. doi: 10.3961/jpmph.2009.42.4.243. [DOI] [PubMed] [Google Scholar]
- Kutikova LL, Bowman S, Chang SR, et al. The economic burden of lung cancer and the associated costs of treatment failure in the United States. Lung Cancer. 2005;50:143–54. doi: 10.1016/j.lungcan.2005.06.005. [DOI] [PubMed] [Google Scholar]
- Longo CJ. Characteristics of cancer patients’ out-of-pocket costs in Ontario. J Clin Oncol. 2005;22:8251–51. [Google Scholar]
- Luengo-Fernandez R, Leal J, Gray A, Sullivan R. Economic burden of cancer across the european union: a population-based cost analysis. Lancet Oncol. 2013;14:1165–74. doi: 10.1016/S1470-2045(13)70442-X. [DOI] [PubMed] [Google Scholar]
- Max W, Rice DP, Sung HY, Michel M. Center for Tobacco Control Research and Education. UC San Francisco: Center for Tobacco Control Research and Education; 2004. Valuing human life: estimating the present value of lifetime earnings, 2000. Retrieved from: http://escholarship.org/uc/item/82d0550k . [Google Scholar]
- Mehrabi S, Delavari A, Moradi G, et al. Smoking among 15-to 64-year-old Iranian people in 2005. Iran J Epidemiol. 2007;3:1–9. [Google Scholar]
- Mohagheghi MA, Mousavi-Jarrahi Y, Mosavi-Jarrahi A. Cost of care for lung cancer in the first year after diagnosis in Iran. Asian Pac J Cancer Prev. 2011;12:1013–15. [PubMed] [Google Scholar]
- Molinier L C, Combescure C, Chouaïd C, et al. Cost of Lung Cancer. Pharmacoeconomics. 2006;24:651–59. doi: 10.2165/00019053-200624070-00004. [DOI] [PubMed] [Google Scholar]
- Pakzad R, Mohammadian-Hafshejani A, Ghoncheh M, et al. The incidence and mortality of lung cancer and their relationship to development in Asia. Transl Lung Cancer Res. 2015;4:763–74. doi: 10.3978/j.issn.2218-6751.2015.12.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rezaei S, Akbari- Sari A, Arab M, Majdzadeh R, Mohammadpoorasl A. Estimating economic burden of cCancer deaths attributable to smoking in Iran in 2012. J Res Health Sci. 2015;15:228–33. [PubMed] [Google Scholar]
- Warren JL, Yabroff KR, Meekins A, et al. Evaluation of trends in the cost of initial cancer treatment. J Natl Cancer Inst. 2008;100:888–97. doi: 10.1093/jnci/djn175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WOH. Injuries, violence and disabilities biennial report, 2004-2005 prevention and control. vi, 59. Geneva: World Health Organization; 2006. http://www.who.int/iris/handle/10665/43440 . [Google Scholar]
- Yabroff KR, Lamont EB, Mariotto A, et al. Cost of care for elderly cancer patients in the United States. J Natl Cancer Inst. 2008;100:630–41. doi: 10.1093/jnci/djn103. [DOI] [PubMed] [Google Scholar]
- Yabroff KR, Lund J, Kepka D, Mariotto A. Economic burden of cancer in the United States: estimates, projections, and future research. Cancer Epidemiol Biomarkers Prev. 2011;20:2006–14. doi: 10.1158/1055-9965.EPI-11-0650. [DOI] [PMC free article] [PubMed] [Google Scholar]


