Abstract
Objective:
The aim of this study was to identify associations of internal motivation, perceived health competency, and health literacy with primary and secondary cancer prevention.
Methods:
A telephone survey was conducted with a sample of 2,700, 30-69 year olds, proportionally extracted from Gangwon Province, South Korea. The dependent variables were actions in primary and secondary prevention and the explanatory variables were 13 questions in three areas: internal motivation (4 items), perceived health competency (4 items), and health literacy (5 items).
Result:
Multiple linear regression analysis showed that internal motivation, perceived health competency, and health literacy positively impacted primary prevention after controlling for gender and age. As internal motivation, perceived health competency, and perceived literacy increased by 1 point, primary prevention scores increased by 0.11, 0.11, and 0.07 points, respectively. In addition, logistic regression results for secondary prevention showed that health literacy had a positive impact on secondary behavior. As health literacy increased by 1 point, the odds ratio of the practice of secondary prevention was 1.4 times higher.
Conclusion:
This study suggests that primary and secondary prevention of cancer are significantly related to intrinsic motivation factors, perceived health competency, and actual health literacy. Health literacy concepts that cover the capacity of health management in comprehensive areas need to be applied to education and promotion for improvement of primary and secondary prevention of cancer.
Keywords: Internal motivation, perceived health competency, health literacy, cancer prevention
Introduction
Mortality from cancer in Koreans has accounted for 28.6% of the top 10 mortality ratio by 150.9 people per 100,000 population and is still No. 1, accounting for a high disease burden of 4.5 trillion won (Statistics Korea, 2014). In addition, the age-standardized incidence rate of cancer in Koreans—285.7 people per 100,000 population is higher than the Organization for Economic Cooperation & Development (OECD) average of 270.3 people per 100,000 population (National Cancer Information Center, 2015).
Considering the high mortality rate from cancer, prevention is an important factor. Cancer prevention can be divided into primary prevention (before cancer occurrence) and secondary prevention (diagnosing cancer at an early stage). The World Health Organization (WHO) has stressed that lack of primary prevention behaviors, including physical activity, healthy dietary habits, and non-smoking accounted for 60% of the total causes of cancer, and suggested that improvement in habits could reduce the risk of cancer to a third of the current level. In addition, secondary prevention such as regular cancer screening programs, which have the ability to detect cancer in early stages and prevent aggravated conditions, has been the most effective and efficient method to improve quality of life (WHO, 2014).
In response to these issues, Korea has strengthened institutional and financial support for primary and secondary prevention of cancer at the national level. The first primary prevention plan was established in 1996 and has been renewed every 10 years. In addition, the 10-Year Cancer Control Plan was developed in 1996 and the practice of healthy behaviors has been encouraged (Yoo, 2008).
Furthermore, to increase regular cancer screening in secondary prevention, the National Cancer Screening Program was initiated in 1999, through which the national health insurance system provides cancer screening for five types of cancer. For people with low income, the national health insurance system supports cancer screening programs free of charge.
Despite many resources having been invested, the performance rates of primary and secondary prevention of cancer among Koreans has been low. For Korean adults, the occurrence rate of chronic disease increased to 24.2% in 2014. In addition, the rate of high-risk drinking in adults has never been below 13.5%, and the rate of moderate activity has been only 23.5%. Although the activity rate has been increasing, it remains low (Korea Centers for Disease Control and Prevention, 2016). Furthermore, although the government has supported cancer screening programs, the rate of cancer screening over the last five years decreased from 44.7% in 2010 to 44.2% in 2014. These indices suggest that the public lacks the ability to play a leading role in managing health care.
To solve this problem, it is necessary to establish a concrete strategy to influence individual behavior change; We believe the answer can be found in self-determination theory (SDT). Deci and Ryan (2000) explained that the key of SDT was “the degree to which people endorse their actions at the highest level of reflection and engage in the actions with full sense of choice.” Thus, intrinsic interest in an activity that reflects one’s own will and individual experiences of self-motivation, or choosing for oneself, affects the formation of regular habits (Spigner et al., 2007). Internal motivation presented in SDT is a desire of the self to makes changes effectively and continuously. Thus, internally motivated action is more successful than that directed by the instruction and requirements of others or experts. Jung and Jo (2014), in ongoing studies of cancer screening-related factors among Koreans, found that intrinsic motivation was a significant factor in regular breast cancer screening.
In addition to internal motivation, health competency is an essential component of cancer prevention programs. Pender’s health promotion model (HPM) (Pender et al., 2011) stressed that factors influencing health behaviors were self-esteem and internal motivation, in addition to biological factors or health status. The goal of empowerment programs comprising education for chronic disease management is to strengthen health competency. Regarding health competency, it has been suggested that high self-confidence, responsibility for one’s own health care, and efficacy related to potential and strengths, promote the capacity for chronic disease management (Verekamp et al., 2009). In addition, health literacy is a key factor in the management of chronic disease, and is receiving increased attention. At the patient population level, good health literacy is foundational to the successful management and prevention of chronic disease. As the leading cause of global mortality (WHO, 2014), with increasing rates worldwide, chronic disease constitutes a complex, long-term challenge for patients, providers, and the healthcare system (U.S. Department of Health and Human Services, 2010). When the concept of health literacy was first introduced, it reflected simple literacy (Simonds, 1974). However, its scope is being expanded from the concept of health information literacy to that of utilization of health information. WHO defines health literacy as cognitive and social skills that underlie motivation and efforts to access, understand, and utilize information for health maintenance and promotion (WHO, 2014). Early evidence indicates that deficits in health literacy are associated with poorer health outcomes and higher health-related costs for both individuals and systems (Berkman et al., 2011). Improved health literacy has been associated with reductions in risk behaviors for chronic disease (Lynn, 2006; Taggart et al., 2012), higher self-reported health status (OECD, 2013), and decreased rates of hospitalization (Cho et al., 2008).
Despite the importance of these factors, research has focused solely on the segmentation and identification of awareness about the practice of cancer prevention in Koreans (Jo and Jung, 2011; Jo et al., 2014), and the identification of factors influencing motivation for cancer screening (Jung and Jo, 2014; Kim et al., 2015). No research has been conducted to understand the relevance of intrinsic motivation, perceived health competency, and health literacy for primary and secondary cancer prevention.
Therefore, in this study, we aimed to provide concrete information as to how internal motivation, perceived health competency, and health literacy relate to the influence of cancer information on primary prevention, such as healthy lifestyle factors, and secondary prevention, such as regular cancer screening.
Materials and Methods
Study design
This study was designed to identify factors that affect internal motivation, perceived health competency, and health literacy in relation to primary and secondary cancer prevention-related behavior.
Subjects and data collection
The study selected 2,700, 30–69-year-old men and women-proportionally extracted by age and gender-who resided in 6 cities and 12 counties in Gangwon Province from February 3 to 21, 2016.
While there are disadvantages to a telephone survey, such as a higher rejection rate and difficulty communicating complex questions, we selected this methodology for ease of questionnaire administration, speed of survey completion, and the ability to easily access the large representative population over a wide area in Gangwon Province. The Korea Data Network, a professional survey company and experts in telephone surveys, performed our survey under strict and precise guidelines.
Variables
The dependent variables of the study were primary and secondary prevention, specifically 10 rules based on cancer prevention tips from the National Cancer Institute. The cancer screening rule was classified as secondary prevention and the other nine rules were defined as primary prevention. Practice of each item was measured with yes/no answers (Figure 1).
Figure 1.
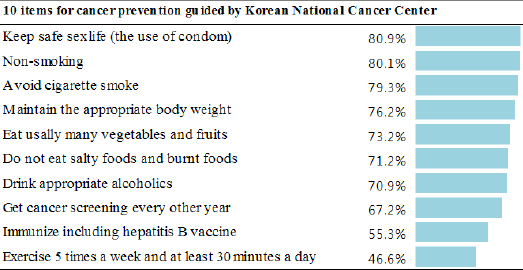
Practice of Primary Cancer Prevention Among Respondents
Thirteen questions were used to assess explanatory variables in three areas: internal motivation (4 items), perceived health competency (4 items), and health literacy (5 items). These questions were modified for the purposes of this study from the Personal Competence of Health Care (PCHC) scale, which was developed as a capacity tool of cancer management in Korean (Lee et al., 2012). The variables and their definitions were as follows: 1) Primary cancer prevention referred to the implementation of cancer prevention rules; 2) Secondary cancer prevention referred to finding cancer early and cancer screening for early treatment; 3) Internal motivation referred to voluntary, continuous, and positive incentives for healthcare management; 4) Perceived health competency referred to recognizing the efficacy of healthcare management; and 5) Health literacy referred to understanding health information literacy.
Gender, age group (30s, 40s, 50s, 60s), income (quartiles), and marital status were collected as demographic characteristics.
Data analysis
Demographic variables were summarized through frequencies. Primary prevention dependent variables covered various areas such as exercise and diet, making it difficult to calculate composite scores. Therefore, we demonstrated through item factor analysis based on item response theory (IRT) that these variables could be grouped within a single concept of cancer prevention activities. The expected a posteriori (EAP) scores calculated in the process-with a mean of 0 and standard deviation 1 were used with each respondent’s PCP score. EAP is one of the IRT parameter estimation methods based on the Bayesian approach. Given the use of a Likert scale with 5 response options on an ordinal scale, the 13 survey questions were checked using item factor analysis based on the IRT graded response model (GRM) (Jeong and Lee, 2016), to assess whether internal motivation, health literacy, and perceived health competencies were reflected properly. The results are shown in Table 1. Scores were calculated with EAP scores like the primary prevention.
Table 1.
Factor Loadings of Item Response Theory (IRT) Graded Response Models (GRMs)
| Item | standardized | loading | (s.e.) |
|---|---|---|---|
| Internal motivation | |||
| I think I am worthy of myself. | 0.8 (0.02) | ||
| I try to make my life worthwhile. | 0.9 (0.02) | ||
| I want to change my lifestyle in a more healthy way. | 0.7 (0.03) | ||
| When I need help, I can get help from other people. | 0.7 (0.02) | ||
| Perceived health competency | |||
| I can control my health with my own will. | 0.6 (0.03) | ||
| I can act to prevent and treat disease. | 0.8 (0.02) | ||
| I can reduce my stress and fatigue. | 0.6 (0.03) | ||
| I have enough money to prevent the disease and to treat. | 0.6 (0.03) | ||
| Health literacy | |||
| I know about the common health problems in my age group. | 0.7 (0.03) | ||
| I have an interest in health information provided by a television, newspapers, the Internet and so on. | 0.6 (0.03) | ||
| I know about health insurance system to prevent and treat disease. | 0.7 (0.03) | ||
| I can understand that doctors explained about health. | 0.6 (0.03) | ||
| I can ask about my health problems to the doctor when necessary. | 0.7 (0.03) |
s.e., standard error
The model of primary prevention was confirmed through multiple regression regarding how much the primary prevention scores increased as each area increased by 1 point. For secondary prevention, the dependent variables were evaluated as “action/no action.” Thus, these were dichotomous variables, and the odds ratio of secondary prevention was identified using logistic regression according to an increase by 1 point in each area. Demographic characteristics were included as calibration parameters. As data were collected from 18 counties (clustered data). Therefore, the generalized estimating equation (GEE) was used. Multicollinearity issues were checked with the variance inflation factor (VIF). The “marital status” item had no effect on the results and caused multicollinearity. Therefore, this item was removed for model parsimony.
Factor loadings were all greater than 0.5. The model fit Root Mean Square Error of Approximation (RMSEA) was 0.03 and Tucker-Lewis Index (TLI) was 0.99. In the final logistic regression, the validity of the structure to calculate and analyze scores in the three domains for all questions was confirmed.
All analyses were performed using SAS Version 9.4(Cary, NC) and STATA Version 14.0.
Results
Sociodemographic characteristics of the surveyed population
The sample of 2,540 subjects was 48.6% male and 51.4% female. The percentages of subjects in their 30s, 40s, 50s, and 60s were 22.4%, 28.9%, 30.3%, and 18.5%. In terms of marital status, 13.2% were single and 86.8% were married. For annual average family income, there were 24.6% in the 1st quartile, 24.5% in the 2nd quartile, 27.0% in the 3rd quartile, and 23.8% in the 4th quartile.
Practice of primary and secondary cancer prevention
Results regarding practice of primary cancer prevention showed a high rate of ‘condom usage’ (80.9%),’ non-smoking’ (80.1%), ‘maintenance of appropriate body weight’ (76.2%), and ‘avoid cigarette smoke’ (79.3%). However, the rates of ‘hepatitis B vaccination’ (55.3%) and ‘exercising at least 30 minutes a day’ (46.6%) were low (Figure 1).
Factors related to the practice of primary and secondary cancer prevention
Multiple linear regression analysis confirmed that after controlling for gender and age, internal motivation, health literacy, and perceived health competency had a statistically significant impact on primary prevention. Women compared to men (coefficient = 0.40), and subjects in their 40s compared to those in their 30s (coefficient = 0.13), 50s (coefficient = 0.20), and 60s (coefficient = 0.27) had higher scores for primary prevention. In addition, as internal motivation, health literacy, and perceived health competency increased by 1 point, primary prevention scores increased by 0.11, 0.07, and 0.11 points, respectively. Therefore, internal motivation, health literacy, and perceived health competency all positively impact the actions of primary prevention.
Logistic regression results demonstrated that gender, age, and health literacy had a statistically significant impact on secondary prevention (Table 2). The more women compared to men (odds ratio 2.53) higher. For age, there were statistically significant that all age groups (40s, 50s, 60s) were higher than 30s higher was the probability of secondary prevention behavior (40s, 50s, 60s respectively, odds ratio 4.41, 8.79, 14.23). In addition, as the health literacy score increased by 1 point, the odds ratio of the practice of secondary prevention was 1.4 times higher. Therefore, health literacy had a positive impact on secondary prevention behavior.
Table 2.
Regression and Logistic Model of Factors Related to Primary and Secondary Cancer Prevention.
| Category (reference) | "Primary cancer prevention | (PCP)” | "Secondary cancer | prevention(SCP)” |
|---|---|---|---|---|
| standardized coefficient | 95% CI | Odds Ratio | 95% CI | |
| Self-Management Ability | ||||
| internal motivation | 0.11 | (1.08-1.15) | 1.08 | (0.96-1.22) |
| health literacy | 0.07 | (1.03-1.11) | 1.4 | (1.22-1.62) |
| perceived health competency | 0.11 | (1.08-1.16) | 0.95 | (0.83-1.10) |
| Sex (Male) | ||||
| Female | 0.4 | (1.42-1.57) | 2.53 | (2.09-3.07) |
| Age group (30-39) | ||||
| 40-49 | 0.13 | (1.06-1.22) | 4.41 | (3.45-5.65) |
| 50-59 | 0.2 | (1.14-1.31) | 8.79 | (6.75-11.46) |
| 60-69 | 0.27 | (1.21-1.42) | 14.23 | (10.10-20.04) |
| Income level (1stquartile) | ||||
| 2ndquartile | 0.04 | (0.97-1.12) | 1.16 | (0.88-1.55) |
| 3rdquartile | 0.05 | (0.98-1.14) | 1.22 | (0.92-1.62) |
| 4thquartile | 0.04 | (0.96-1.13) | 1.57 | (1.16-2.13) |
CI, Confidence Interval
Discussion
Cancer prevention is important both theoretically and practically. However, there is a gap between knowledge and practice. Previous studies analyzing factors related to the awareness of 10 cancer prevention rules in a representative sample from Gangwon Province in 2008 showed relatively high levels of awareness of the importance of non-smoking (81.1%), needing to walk (88.3%), appropriate weight (90.3%), and hepatitis B vaccinations (71.5%) (Jo and Jung, 2011). This study of a representative sample from the same region showed comparable awareness levels of the importance of non-smoking (80%), but lower awareness of the importance of hepatitis B vaccinations (55%) and exercising for at least 30 minutes a day (47%).
Knowledge and information is transmitted by the provider, while putting knowledge into practice is the responsibility of individuals. Therefore, it is important to understand factors influencing how individuals behave, and to strengthen and support these factors. This study suggests that primary and secondary prevention of cancer are significantly related to intrinsic motivation factors, health literacy, and health competency.
Internal motivation is a key element in self-determination theory. Voluntary internal motivation causes patients to recognize their own problems, to establish objectives for action to improve these problems, to experience fulfillment step-by-step, and to achieve continuous change (Deci and Ryan, 2000).
The results of this study show that internal motivation and perceived health competency, as health literacy, improve healthy living practices related to primary prevention of cancer. This is similar to previous studies, which suggested a positive relation between intrinsic motivation and the practice of healthy living.
Leong et al., (2012) focused on healthy eating behaviors in women in their 40s and 50s, and argued that the stronger the tendency connected with the intrinsic value targeted behavior, the more positive changes for healthy eating behavior. In addition, Seo and Choi, (2011) indicated that specific behaviors were determined by individual intrinsic value, selected, and given motivation autonomously. Furthermore, the significant relevance of health competency proved the importance of self-efficacy presented recently as an important concept in self-management (Bodenheimer et al., 2002). Unlike past health education focused on arising complications without treatment and understanding of disease, it is important to develop the ability of solving problems themselves. Therefore, it is necessary to approach specifically to improve self-efficacy.
In this study, perceived healthy competency was applied to increase efficacy for health management. The perception of being able to control resources for oneself for disease prevention and health improvement affects behavior. If negative and obstructive factors related to competency are perceived by subjects, they may establish plans to overcome them and to practice specifically.
Fan et al (2016) studied multi-dimensional health locus of control (MHLoC) and self-management behaviors in hemodialysis patients, which are similar to the concepts of internal and external locus of control. The concept of MHLoC suggests that locus of control behaviors that could control outcomes and lead to positive change had limitations in their positive effects on physical and psychological health rather than external locus of control thus, fate or the external environment could control outcomes. This study found that health competency was measured by internal and external locus of control, health behaviors, stress reduction skills, and cognitive ability to use financial resources. As a result, health competency was significantly positively associated with primary cancer prevention activities.
The positive relevance of health competency also was suggested by Jo et al., (2012) who studied a health coaching intervention for 6 months, targeting patients with a metabolic syndrome. Health coaching means that a person identifies a health problem and establishes self-directed goals and problem-solving. The most important concept in this coaching is that a counselor helps to improve health competency through a motivational interview. After 6 months of consultation, patients change eating habits, exercise, and manage their health themselves. This study suggests that improving health competency is important for the practice of a healthy lifestyle among patient populations as well as the general population.
Meanwhile, health literacy has been proposed as a significant influencing factor in both secondary prevention of cancer screening as well as primary prevention. These findings are similar to those of Kim et al., (2015), who suggested that to understand factors impacting the practice of cancer screening for same residents in 2015 and the information, motivation and behavioral skill have significantly positive effect on cancer screening. Recently, health literacy has been expanded and conceptualized as the application of a set of skills including reading, numeracy, and problem solving (Poureslami I et al., 2016). Health literacy empowers people with skills to improve their health (Nutbeam, 2000). It is necessary to apply a comprehensive concept of health literacy to the development of education and cancer prevention programs. Nutbeam (2000) stressed that health literacy would be the most important concept in public health for contemporary health education and communication strategies into the 21st century.
Recently, Health literacy in Europe (HLS-EU) research focused on WHO Europe suggested that the elements of health literacy access, understanding, appraise and apply be expanded and three sections health care, disease prevention, and health promotion be classified and the goals and evaluation of health literacy in each matrix should be performed (Sørensen et al., 2013). Considering these points, it is necessary to define the capacity of health literacy needed for primary and secondary prevention in each area and to provide education and information to enhance this progress.
On the other hand, internal motivation and perceived health competency had no significant effects on secondary prevention of cancer. This is different from previous studies (Jung and Jo, 2014), which demonstrated that internal motivation had a significant effect on regular breast screening. There are a few possible reasons for this. Jung and Jo (2014) set up the continuous habit-more than twice- of a breast cancer screening as dependent variables and one time screening as a control group. For one-time cancer screenings, correct information should be directly provided to guide initial practice. For continuous habits, it is necessary for internal motivation to be considered. Currently, there is no approach that incorporates internal motivation and perceived health competency in education of cancer screening and provision of information. Only simple information such as cancer screening support or screening agencies of the government has been provided and the cancer screening practice rate has remained at 67%. Therefore, an intervention that can enhance motivation needs to be identified and evaluated.
This study has some limitations. The research design did not allow the determination of causal relationships pertaining to relevant factors influencing primary and secondary prevention. In addition, there was a lack of standardization in measurement tools. However, the concept of health literacy and psychological factors such as internal motivation and perceived health competency are being modified and developed, and it is difficult to develop a standardized index concepts.
Considerable effort has gone into the development of a holistic understanding of health literacy over the last decade. However, no complete agreement on definition has been reported yet; therefore, a single, authoritative definition remains elusive (Peerson and Saunders, 2009). The development of tools and measures to better understand context-specific variation, including over the life course (Berkman et al., 2011; Sørensen et al., 2012), is needed. Because of this, a contextual approach has been suggested.
In addition, our research shows that the relevance between primary and secondary prevention and the comprehensive concept comprising health literacy and psychological and motivational factors, are analyzed empirically targeting community members, and the importance of factors are suggested. The concept of public health literacy, which covers capacity for health management in comprehensive areas, may need to be applied to education and promotion related to the improvement of primary and secondary prevention of cancer.
Acknowledgments
This study was supported by 2014 Research Grant from Kangwon National University (No. 120140272).
References
- Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: An updated systematic review. Ann Intern Med. 2011;155:97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002;288:2469–75. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- Cho YI, Arozullah AM, Crittenden KS, Lee SYD. Effects of health literacy on health status and health service utilization amongst the elderly. Soc Sci Med. 2008;66:1809–16. doi: 10.1016/j.socscimed.2008.01.003. [DOI] [PubMed] [Google Scholar]
- Deci EL, Ryan RM. The “what” and “why” of goal pursuits: Human needs and the self-determination of behavior. Psychol Inq. 2000;11:227–68. [Google Scholar]
- Fan JL, Kong Y, Shi SH, Cheng YH. Positive correlations between the health locus of control and self-management behaviors in hemodialysis patients in Xiamen. Int J Nurs Sci. 2016;3:96–101. [Google Scholar]
- Jeong HJ, Lee WC. Item response theory-based evaluation of psychometric properties of the safety attitudes questionnaire-Korean version (SAQ-K) Biom Biostat Int J. 2016;3:1–15. [Google Scholar]
- Jo HS, Jung SM. Audience Segmentation to Promote Lifestyle for Cancer Prevention in the Korean Community. Asian Pacific J Cancer Prev. 2011;12:869–74. [PubMed] [Google Scholar]
- Jo HS, Jung SM, Lee HJ. The evaluation of a health coaching program on metabolic syndrome patients. Korean J Health Educ Promot. 2012;29:97–108. [Google Scholar]
- Jo HS, Kwon MS, Jung SM, Lee BY. Awareness of cancer and cancer screening by Korean community residents. Asian Pac J Cancer Prev. 2014;15:4939–44. doi: 10.7314/apjcp.2014.15.12.4939. [DOI] [PubMed] [Google Scholar]
- Jung SM, Jo HS. Intrinsic motivation factors based on the self-determinant theory for regular breast cancer screening. Asian Pac J Cancer Prev. 2014;15:10101–6. doi: 10.7314/apjcp.2014.15.23.10101. [DOI] [PubMed] [Google Scholar]
- Kim BG, Jo HS, Lee HJ. Study on the factors related with intention of cancer screening among Korean residents: application of information-motivation-behavioral skills model. Asia Pac J Public Health. 2015;27:2133–43. doi: 10.1177/1010539511422374. [DOI] [PubMed] [Google Scholar]
- Korea Centers for Disease Control and Prevention. 2016 Chronic disease status and issues: factbook (in Korean)[Online] Osong: Korea Centers for Disease Control and Prevention; 2016. [[accessed 4 Feb 2016]]. Available: http://www.guideline.or.kr/newsletter/vol1609/file/201609_01.pdf . [Google Scholar]
- Lee KS, Choi JS, So AY, Lee EH. The Reliability and validity of the personal competence of health care (PCHC) scale. J Muscle Jt Health. 2012;19:197–209. [Google Scholar]
- Leong SL, Madden C, Gray A, Horwath C. Self-determined, autonomous regulation of eating behavior is related to lower body mass index in a nationwide survey of middle-aged women. J Acad Nutr Diet. 2012;112:1337–46. doi: 10.1016/j.jand.2012.04.018. [DOI] [PubMed] [Google Scholar]
- Lynn C. Low health literacy and chronic disease prevention and control-perspectives from the health and public sectors [Online] Canadian public health association. 2016. [[accessed 4 Feb 2016]]. available: http://www.cpha.ca/uploads/portals/h-l/kl_summary_e.pdf .
- National Cancer Information Center. Cancer facts and figures 2015 [Online] Goyang: President of National Cancer Center; 2015. [Google Scholar]
- Nutbeam D. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int. 2000;15:259–67. [Google Scholar]
- Organization for Economic Co-operation and Development. Skilled for Life- Key Findings from the Survey of Adult Skills [Online]. Organization for Economic Co-operation and Development. 2013. [[accessed 8 March 2016]]. Available: http://www.oecd.org/skills/piaac/SkillsOutlook_2013_ebook.pdf .
- Peerson A, Saunders M. Health literacy revisited: what do we mean and why does it matter? Health Promot Int. 2009;24:285–96. doi: 10.1093/heapro/dap014. [DOI] [PubMed] [Google Scholar]
- Pender NJ, Murdaugh CL, Parsons MA. Health promotion in nursing practice. 6th ed. Boston, MA: Pearson; 2011. [Google Scholar]
- Poureslami I, Nimmon L, Rootman I, Fitzgerald MJ. Health literacy and chronic disease management: drawing from expert knowledge to set an agenda. Health Promot Int. 2016;107:291–95. doi: 10.1093/heapro/daw003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seo YM, Choi WH. A predictive model on self-care behavior for patients with type 2 diabetes: based on self-determination theory. J Korean Acad Nurs. 2011;41:491–9. doi: 10.4040/jkan.2011.41.4.491. [DOI] [PubMed] [Google Scholar]
- Simonds SK. Health education as social policy. Health Educ Behav. 1974;2:1–10. [Google Scholar]
- Sørensen K, Van den Broucke S, Fullam J, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. 2012;12:1–13. doi: 10.1186/1471-2458-12-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sørensen K, Van den Broucke S, Pelikan JM, et al. Measuring health literacy in populations: illuminating the design and development process of the European Health Literacy Survey Questionnaire (HLS-EU-Q) BMC Public Health. 2013;13:948. doi: 10.1186/1471-2458-13-948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spigner C, Yip MP, Huang B, Tu SP. Chinese and Vietnamese adult male smokers’ perspectives regarding facilitators of tobacco cessation behavior. Asian Pac J Cancer Prev. 2007;8:429–35. [PubMed] [Google Scholar]
- Statistics Korea. Annual report on the causes of death statistics. Daejon: Statistics Korea; 2014. [Google Scholar]
- Taggart J, Williams A, Dennis S, et al. A systematic review of interventions in primary care to improve health literacy for chronic disease behavioral risk factors. BMC Fam Pract. 2012;13:49–60. doi: 10.1186/1471-2296-13-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. National Action Plan to Improve Health Literacy [Online] Washington DC: Office of Disease Prevention and Health Promotion; 2010. [[accessed 17 March 2016]]. Available: https://health.gov/communication/hlactionplan/pdf/Health_Literacy_Action_Plan.pdf . [Google Scholar]
- Varekamp I, Heutink A, Landman S. Facilitating empowerment in employees with chronic disease: qualitative analysis of the process of change. J Occup Rehabil. 2009;19:398–408. doi: 10.1007/s10926-009-9188-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Global status report on noncommunicable diseases 2014 [Online] Geneva: World Health Organization; 2014. [[accessed 7 April 2016]]. Available: http://www.who.int/nmh/publications/ncd-status-report-2014/en/ [Google Scholar]
- Yoo KY. Cancer Control Activities in the Republic of Korea. Jpn J Clin Oncol. 2008;38:327–33. doi: 10.1093/jjco/hyn026. [DOI] [PubMed] [Google Scholar]


