Abstract
Background:
Though people of color (POC) are less likely to become afflicted with skin cancer, they are much more likely to die from it due to delay in detection or presentation. Very often, skin cancer is diagnosed at a more advanced stage in POC, making treatment difficult. The purpose of this research was to improve awareness regarding skin cancers in people of color by providing recommendations to clinicians and the general public for early detection and photo protection preventive measures.
Methods:
Data on different types of skin cancers were presented to POC. Due to limited research, there are few resources providing insights for evaluating darkly pigmented lesions in POC. Diagnostic features for different types of skin cancers were recorded and various possible risk factors were considered.
Results:
This study provided directions for the prevention and early detection of skin cancer in POC based on a comprehensive review of available data.
Conclusions:
The increased morbidity and mortality rate associated with skin cancer in POC is due to lack of awareness, diagnosis at a more advanced stage and socioeconomic barriers hindering access to care. Raising public health concerns for skin cancer prevention strategies for all people, regardless of ethnic background and socioeconomic status, is the key to timely diagnosis and treatment.
Keywords: Skin Cancer, types, people of color, risk and prevention
Introduction
The color of skin in humans is primarily determined by the presence of melanin and dark skin has larger melanocytes that produce more melanin which protects the deeper layers of the skin from harmful effects of the sun (Kaidbey et al., 1979). Human skin is repeatedly exposed to ultraviolet radiation that influences the function and survival of many cell types and is regarded as the main causative factor in the induction of skin cancer (D’Orazio et al., 2013). Ionizing radiation, pollutants, chemicals and occupational exposures are also linked with skin cancers (El Ghissassi et al., 2009). The superior photo protection in people of color (POC) is related to packaging and distribution of melanosomes which are distributed individually in keratinocytes rather than in aggregates. It is estimated that the epidermis of blacks has an intrinsic sun-protection factor (SPF) of 13.4, whereas light skin has an SPF of 3.3 (Kaidbey et al., 1979; Tadokoro et al., 2003). The increased melanin and more dispersed melanosomes appear to absorb and deflect UV light more efficiently, conferring significant photo protection to skin (Cummins et al., 2006). Higher amount of epidermal melanin in people of color filters at least twice as much UV radiation as the epidermis of whites (Brenner and Hearing, 2008) (Montagna and Carlisle, 1991). This is the reason that white population is the primary victims of skin cancer (Gloster and Neal, 2006; Markovic et al., 2007)and the incidences of skin cancer are lower in people of color (POC) when compared with whites (D’Orazio et al., 2013). Whites have highest rate of getting melanoma of the skin followed by American Indian/Alaska Native, Hispanic, Asian/Pacific Islander and black. The incidence rates for new melanoma of the skin cases have been rising on average 1.4% each year over the last 10 years (CDC Statistics, 2016) (Figure 1).
Figure 1.
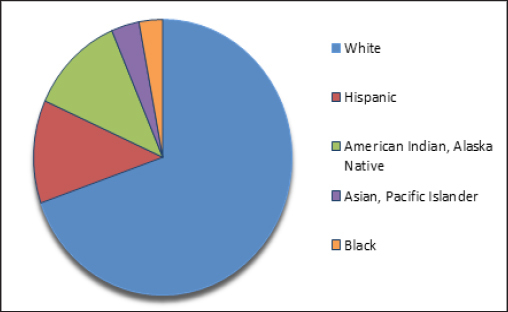
Incidence of Skin Cancer by Race/Ethnicity
However, there is growing evidence that the relationship between pigmentation and photo protection is far more complex than assumed (Brenner and Hearing, 2008). Most of the people of color have misconception that they are immune to skin cancer but recent studies indicate that skin cancer does not discriminate, it can occur in all populations whatever their skin color (Lozano et al., 2012). Skin cancer represents the most common worldwide malignancy and its incidence shows no signs of plateauing. It is estimated that in 2016, there will be 76,380 new cases of melanoma of the skin (Jacobsen et al., 2016) and an estimated 10,130 people will die of this disease in US alone (Figure 2). Mortality per year from skin cancer has more than doubled since 1990 to 2010 (Imahiyerobo-Ip et al., 2011). Over the past three decades, more people have been affected by skin cancer than all other cancers combined (Stern, 2010). Thus skin cancer is emerging as pre-eminent global public health problem encompassing every ethnicity, socio- economic and demographic cohort, geographic region, and covers the entire lifespan. (CDC Statistics, 2016) (Figure 2).
Figure 2.
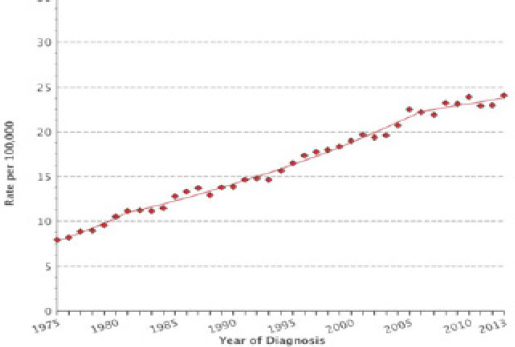
Year-wise Melanoma Incidence Rate in all Races. Age-Adjusted, Both Sexes (Source: Surveillance, Epidemiology, and End Results 9 (SEER) Program of NCI (1975-2013))
Studies consistently show that as compared to whites people of color are more likely to die from this curable disease (Merrill et al., 2016). Though melanoma incidence among white population has risen almost 20 percent in the past two decades alone, (Mann D, 2016) a recent epidemiological review published by the American Academy of Dermatology showed that the 5-year survival rates for non-white population is 70%, which is significantly lower than that of whites (92%) (Wu et al., 2011; Gohara, 2008). According to U.S. Census Bureau 2012 press release, minorities, now 37 percent of the U.S. population, are projected to comprise 57 percent of the population in 2060. The total minority population would more than double, from 116.2 million to 241.3 million, over the period. It is estimated that people of color i.e. black, Hispanic, and Asian Americans will comprise approximately 50% of the US population by the year 2050 (Gloster and Neal, 2006) and skin cancer rate is rather alarming among these darker-skinned populations in California, New Mexico, and Texas, Arizona, Nevada, Georgia, New York, and Florida (Mann D, 2016). Reason for high mortality in the non white population is that in most forms of skin cancer, symptoms are not easily visible and it becomes too late before cancer is diagnosed (Pipitone et al., 2002). Early signs of melanoma, the deadliest form of skin cancer in people of color are shown up in unusual places such as the palms and soles, fingernails and toe nails and the inner surface of the mouth and genitals and so are missed most of the times (Madankumar et al., 2016). Further, studies revealed that people of color (POC) receive little or no education from their doctors concerning the risks and prevention of the disease (Kim et al., 2009b). People of color do not understand their risk for skin cancer as false belief that darker skin is protected from the sun’s harmful rays is the main contributing factor in these delays making skin cancers often advanced and potentially fatal (Hansen, 2014; Jacobsen et al., 2016). Further, there is limited research on skin cancer in POC (Buster et al., 2012). The World Health Organization predicts a 70% increase in new cases of cancer expected over the next two decades, with most occurring in low and middle income countries. It is often difficult for many second and third world countries in Asia to establish uniform tumor registries in hospitals or large clinics due to logistical considerations and associated costs (Koh et al., 2003). This population has the least percentage of medical coverage, which decreases access to care and also account for late diagnosis and poor prognosis. Few resources provide insight on evaluating darkly pigmented lesions in POC posing diagnostic challenges in the identification of characteristics such as variation in color within the lesions (Agbai et al., 2014). Thus, outcome of skin cancers in dark-skinned people is far worse than whites. With changing demographics and a steady rise in the minority population in the western world, there is an increased need for further studies of cutaneous malignancies within Asian and other ethnic populations (Halder and Ara, 2003). These evolving demographics, elevated rates of skin cancer morbidity and mortality in POC and limited clinical data on adverse effects of UV exposure in this population makes it mandatory to create awareness in people of color by early detection, preventive photo protection measures and provide recommendations to clinicians and general public to accelerate the efforts.
Risk factors and causes of skin cancer
Despite the fact that high melanin content confers better photo protection, significant photo damage in the form of epidermal atypia and atrophy, dermal collagen and elastin damage (Griffiths et al., 1992; Larnier et al., 1994) and pigmentary disorders can cause skin cancer which could be fatal due to delay in detection in skin of color (Buster et al., 2012). Skin cancer is skin growth with varying degrees of malignancy (Donaldson and Coldiron, 2011). It is not yet very clear why skin cancer incidence has grown so dramatically over the past decades (Rigel, 2010) but the reason is likely to be multi factorial which includes increased UV exposure, environmental, hereditary risk factors and improved surveillance and earlier recognition (Nikolaou and Stratigos, 2014). In addition, genetic polymorphisms also modulate the susceptibility to skin cancer (Meyer, 2009).
UV Radiations from sun produces DNA damage, gene mutations, immunosuppression, oxidative stress, and inflammatory responses, all of which play a pivotal role in photo aging of the skin and skin cancer genesis (Del Bino et al., 2006; Young, 2009). Several factors influence the amount of UVR reaching the earth’s surface, UV light elevation, latitude, altitude, and weather conditions (D’Orazio et al., 2013). There are two main types of UVR rays: ultraviolet A (UVA) and ultraviolet B (UVB). UVA rays pass deeper into the skin and can induce deeper skin damage, such as elastosis than UVB rays. The damage to DNA from UVA rays is indirect, mediated by free radical formation and damage to cellular membranes (Gordon, 2013). UVB rays predominantly cause erythema or sunburn. Even low exposure to UVA/UVB radiation induced some appreciable DNA damage in all skin types, dispelling the myth that those with very dark skin are completely immune to UVA-/UVB-induced DNA damage (Tadokoro et al., 2003). It is likely that most skin damage from ultraviolet light occurs before the age of 20, but it doesn’t show up until many years later (Longstreth et al., 1998). UVA rays have an important role in the carcinogenesis of stem cells of the skin, and UVB rays induce DNA damage through inflammatory responses and tumorigenesis (Narayanan et al., 2010).
People who work outdoors for a living, such as farm workers, builders and gardeners, are at an increased risk of developing skin cancer because of prolonged exposure to the sun (Leiter and Garbe, 2008). Along with UV exposure from sunlight, UV exposure from sun beds for cosmetic tanning also account for the growing incidence of melanoma (Cristina et al., 2014). This is the reason, it is women younger than 45 years who are disproportionately affected (Al-Dujaili et al., 2015). Gender differences in melanoma prognosis have been reported in several studies indicating an increased survival proportion in females compared with men (Weinstock, 2006; Nikolaou and Stratigos, 2014). Tanning and sunburns are analogous to cigarettes in that just one can increase your risk of cancer, regardless of skin color (Anand et al., 2008). Depletion of the ozone layer in the stratosphere has augmented the dose-intensity of ultraviolet rays from sun which further increases the incidence of skin cancer (Norval et al., 2011). With increasing use of lasers and light sources in Asians, prevention and management of skin related diseases is of great research interest (Ho and Chan, 2009).
Organ transplant receivers especially kidney and HIV patients have an increased frequency of skin cancers (Togsverd-Bo et al., 2013). Some treatments, including radiation therapy, phototherapy, psoralen and long-wave ultraviolet radiation (PUVA) can also predispose to skin malignancies (Saladi and Persaud, 2005). Viral infections such as the human papilloma virus (HPV) can cause cancer. Patients with familial genetic patterns are vulnerable to particular types of skin cancers (Cristina et al., 2014). Certain drugs, from common antibiotics to heart medications, can increase the skin’s sensitivity to sunlight, causing the skin to burn in less time and may increase the incidence of skin cancer (Drucker and Rosen, 2011).
Major types of skin cancers and their distribution in people of color
Skin cancer is mainly divided into two main categories as Non melanoma Skin Cancer (NMSC) and Melanoma Skin Cancer (MSC). Non-Melanoma Skin Cancer (NMSC) includes basal cell carcinoma and squamous cell carcinoma (Mueller and Reichrath, 2008). Each of these most common cancers viz. Basal cell carcinoma (BCC), squamous cell carcinoma (SCC), and melanoma is named after the type of skin cell from which it arises and has been linked to the varying degree of sun exposure (Leiter et al., 2014).
NMSC greatly outnumber melanomas in incidence but fortunately most are much easier to treat and have much better long-term prognosis (Ho and Chan, 2009). They are less deadly than melanoma mainly due to their tendency to remain confined to their primary site of disease which makes their management much more straightforward. The devastating majority of keratinocyte malignancies progress in the areas of skin most exposed to UV such as on the face and arms (Narayanan et al., 2010). The BCC and the SCCs often carry a UV-signature mutation indicating that these cancers are caused by UV-B radiation via the direct DNA damage (Young, 2009). Although Asians display relative protection from basal cell carcinoma and squamous cell carcinoma, incidence rates of these non melanoma skin cancers have been increasing over 3 to 8 percent annually in the past three decades (Kim et al., 2009a). Features of different types of skin cancers are listed in Table 1.
Table 1.
Features of Different Types of Skin Cancers
| Type | Squamous cell | Basal cell | Melanoma |
|---|---|---|---|
| Occurrence | Most common in African Americans and Asian Indians 250,000 new cases per year | Most common in Hispanics and then in blacks, >1 million cases each year | Not very common but fatal if not treated early, 63,000 new cases per year |
| Scaly red patch, open sores, wart like or an elevated growth | Normally small reddish patch, shiny bump but in POC, present as black pearly translucent skin growth, | Usually a brown or black mark. Sometimes red or white too. | |
| Physical appearance | Rapidly growing but confined to primary site. | Confined to an area but clinically not very apparent in dark skin types due to pigmentation | Can metastasize quickly and spread to other body part. |
| Treatment | Very treatable by simple surgery or burning with cauterizing pen | Easily treatable by simple surgical removal of small area or burning with cauterizing pen | Treatment is intense, needs surgical removal of large areas of body part as it is deep rooted in skin. |
| Anatomic distribution | Face is commonly effected is whites but in POC it is seen in non sun-exposed lower body parts like hips, legs, feet. | Head and neck most commonly effected in all races | Lower part of the body from the hip to the toes and soles of the feet are affected |
| Risk factor | Causes chronic scarring and inflammation | Rarely metastasize but causes significant disfigurement | Primary risk factor is undetermined in POC but others include albinism, burn scar and trauma |
Many cases of NMSC are reported in Asians (Lee and Lim, 2003) and studies showed that incidence of NMSC between 1990 and 1999 in Hong, Kong, China underwent a threefold increase in 10 years (Cheng SY Luk NM, 2001). Similarly, Sng et al reported an increase of all types of skin cancers in Singapore between the years of 1998 and 2006 (Sng et al., 2009).
Squamous cell carcinoma (SCC)
Squamous Cell Carcinoma is usually a very rapidly growing dangerous tumor arising in the squamous cells of epidermis of the skin and usually develops from a scar or burn (Gordon, 2013). This cancer is commonly presents as scaly red patches, open sores, elevated growths with a central depression or warts on the skin. (Figure 3) They can also crust or bleed but are less dangerous than a melanoma (Hemminki et al., 2003). Squamous cell carcinoma is the most common skin malignancy among African Americans and Asian Indians, and the second most common skin cancer among Hispanics and Chinese/Japanese Asians thereby representing 30%-65% of skin cancers in dark skinned people and only 15%-25% in whites (Gloster and Neal, 2006). In African-Americans, squamous cell carcinoma often develops on the but tocks, hip, legs, and feet (Halder and Bridgeman-Shah, 1995). Risk factors for the development of SCC in darkly pigmented individuals are chronic scarring and areas of chronic inflammation. SCCs in Asians have a greater tendency to occur in non sun-exposed sites with a higher potential for metastasis possibly due to advanced disease stage at the time of diagnosis (Kim et al., 2009a). Information from the Singapore Cancer Registry suggests that UV light plays an appreciable role in skin cancer development among fair-skinned Asian populations. There is an increase of skin cancers including BCC, SCC and MM in Singapore between the years of 1998 and 2006 (Sng et al., 2009). Among African Americans and native Africans, SCCs occur mainly on the legs but scarring, leprosy and non-healing skin ulcerations causes lot of physical or mental trauma (Halder and Ara, 2003).
Figure 3.

Common Types of Skin Cancers
Sun exposure over a lifetime is more significant for squamous cell cancers (Young, 2009) and is found to be more closely related to increased risk in women whereas sun exposure at an early age showed more relevance to SCC risk in men (Chen et al., 2010). SCC accounts for 30 percent of all skin cancers in Japan. General trends in the numbers of deaths from NMSC in Japan have risen since 1995 (Gloster and Neal, 2006).
Basal cell carcinoma (BBC)
BCC is a malignant neoplasm of skin derived from the basal cells of the epidermis or hair follicles. It is the most common cutaneous malignancy in whites and the second most common after Squamous cell carcinoma in people of color (Rubin et al., 2005). BCC contributes to 65%-75% of skin cancers in whites and 20%-30% in people of color (Gloster and Neal, 2006). They rarely metastasize and rarely cause death but can result in significant disfigurement, leading to physical and emotional adverse consequences for the patients. The incidence of BCC increased approximately 3% yearly with peak incidence in the age of forties (D’Orazio et al., 2013).
Basal cell carcinomas is usually linked to ultraviolet (UV) light exposure and in all races BCC is normally present on sun-exposed areas of the skin especially the face in people of color (Steding-Jessen et al., 2010). BCCs frequently is characterized by black pearly translucent and a fleshy color of the skin growth with tiny blood vessels on the surface and sometime ulceration of the tumor (Bigler et al., 1996). (Figure 3) almost 90 percent of basal cell carcinomas are found on the head or the neck in POC (Halder and Bridgeman-Shah, 1995). The correlation between UV light and BCC in darker skin types explains the relatively higher incidence of this malignancy among darker-skinned populations living in sunnier climates (Chang et al., 2009). That is the reason, Latinos, Chinese and Japanese Asians tend to develop basal cell carcinoma whereas squamous cell carcinoma is more common among African Americans and Asian Indians (Leiter et al., 2014). The incidence of pigmented BCC in Hispanics was found to be twice than that of white patients due to high index of suspicion in evaluating pigmented lesions (Bigler et al., 1996).
The clinical presentation of BCCs in Asian skin ranges from nodules to papules, plaques, and ulcers (Bradford,2009). Differential diagnosis for BCC in POC includes seborrheic keratosis, blue nevus, trauma, lupus erythematosus, nevus sebaceous, sarcoidosis, and melanoma (Jackson, 2009). In contrary to whites, pigmentation is present in over 50% of basal cell carcinomas in POC posing challenges in the physical examination for BCC as the characteristic features are not clinically very apparent in dark skin types. So there remains a great deal of suspicion in POC in diagnosing the cancer (Hu et al., 2009).
2650 new cases of BCCs were reported in a study between 1986 and 1997 among Asians living in Singapore (Koh et al., 2003). Age-standardized incidence rates for BCC were greatest in fair-skinned Chinese followed by Malays and Indians (Cheng et al., 2001). Incidence of BCC correlated directly with the degree of skin pigmentation being higher with fairer skin complexion in comparison with those with darker complexions (Lallas et al., 2015). Chinese individuals, who are generally of lighter skin type, are twice as likely to develop BCC and SCC as the darker skinned Malays and Indians (Koh et al., 2003). Incidence of pigmented BCC in Hong Kong, China between 1990 and 1999 were found in approximately 60% of Chinese patients with skin cancer (Cheng et al., 2001). Basal cell carcinoma followed by squamous cell carcinoma are the most common skin cancers in Japanese individuals (Kikuchi et al., 1996). The incidence of BCC in Japanese individuals living in native Japan was much lower demonstrating the harmful effects of UV radiation (Ichihashi et al., 1995; Lee and Lim, 2003).
Malignant melanoma(MM)
Malignant melanoma is a skin cancer that begins in the melanocytes – the cells that produce the skin coloring or pigment known as melanin which helps protect the deeper layers of the skin from the harmful effects of the sun. Though Melanoma accounts for less than one percent of skin cancer cases but causes vast majority of skin cancer deaths. An estimated 10,130 people will die of melanoma in 2016 (American cancer Society, 2016). Melanoma is the third most common type of skin cancer among all racial groups (Riker et al., 2010). More African Americans, Asians and Latino people die of melanoma than white Americans (Goss et al., 2014). It is more difficult to detect in blacks, Asians, Filipinos, Indonesians and native Hawaiians because 60-75 percent of tumors arise on areas of the less pigmented skin that are not usually exposed to the sun like soles of the feet are the most common place, skin cancer begins in people of color. Because of this, lesions or dark spots can go unnoticed or misdiagnosed as warts, fungus or dark nail (Tucker and Goldstein, 2003).
Nearly eight percent of melanomas in Asian-Americans occur in the mouth on the palms of the hands, soles of the feet and under the nails account for more than half of all melanoma cases in people of color as compared to less than 1 in 10 among white Americans. Although UV light, along with heredity, plays a role in the causation of melanoma in Caucasians, the primary risk factor for melanoma in people of color is undetermined and under diagnosed (Friedman et al., 1994). Other reported risk factors for melanoma in people with color include: albinism, burn scars, radiation therapy, trauma, immuno suppression and preexisting moles. Due to delayed diagnoses in blacks, Hispanics and Asians, melanoma have a tendency to be diagnosed at a late stage in comparison with whites (Cress and Holly, 1997).
People in second and third world countries and racial and ethnic minorities in others do not have access to cancer screening facilities and are often misdiagnosed by medical professionals (Zell et al., 2008). Physical examination of peripheral body parts like toes, palms, soles, finger and toe nails is often ignored for melanoma (Kundu et al., 2010). The incidence of melanoma has been reported to range between 0.2 and 2.2 per 100 000 in Asians. In a Singapore study, the incidence of melanoma was reported to be 0.2 per 100,000 in darker skinned Indians and 0.5 per 100,000 in fairer skinned Chinese (Sng et al., 2009). The Japanese have roughly double the incidence of melanoma (2.2 per 100,000) than other Asian races (Ishihara et al., 2001). The 5-year survival for melanoma in Hispanic and black populations has been shown to be consistently lower than in whites (Byrd et al., 2004).
Major Types of Treatments
Although surgical modalities remain the mainstay of treatment, new research and fresh innovation are still required to reduce morbidity and mortality (Lazareth, 2013; Simões et al., 2015). There has been innovation in skin cancer treatment in the last few years than in the previous 30 years (Galiczynski and Vidimos, 2011). Here, we are not discussing treatment methodology in details but just an outline of currently applicable standard treatments for skin cancer is given (Finn et al., 2012;Cooley and Quale, 2013).
Surgery: Most basal cell and squamous cell skin cancers can be successfully treated with surgery and early-stage melanomas are also cured. Thin layers are removed until no more cancer cells are seen.
Radiation Therapy: Radiation therapy uses high-energy rays (such as x-rays) or particles to kill cancer cells or prevent them from growing. It is used when cancer is widely spread, recurred and surgery is not possible.
Chemotherapy: Chemotherapeutic drugs are usually given as injection or taken by mouth as a pill. They travel through the bloodstream to all parts of the body and attack cancer cells and stop their growth by killing them or by stopping them from dividing.
Photodynamic Therapy (PDT): PDT is a relatively new type of treatment alternative to surgery. PDT uses a drug that makes skin cells sensitive to light. The area of affected skin is exposed to laser light which activates the drug which kills cancer cells.
Immunotherapy: Immunotherapy is the emerging new type of treatment that stimulates a person’s own immune system to recognize and destroy cancer cells more effectively.
Targeted therapy: Targeted therapy is a type of treatment that uses drugs or other substances to attack cancer cells. Targeted therapies usually cause less harm to normal cells than chemotherapy or radiation therapy do.
Recommendations for prevention and early detection of skin cancer in people of color
Prevention is better than cure and more than 90% of skin cancers are preventable (Anand et al., 2008). Because many people of color believe that they are not at risk of skin cancer, education through media and doctor’s offices is extremely important. People of color should perform regular self examination of their skin from head to the toe carefully every month. There are various types of skin tumors, many are benign which include moles (nevi), warts and lipomas etc that can develop from different types of skin cells (Markovic et al., 2007). However, unusual moles, sores, lumps, blemishes, markings or changes in the way an area of the skin looks or feels may be a sign of melanoma or another type of skin cancer or a warning that it might occur. Know your ABCDEs can be a good guide for people of color to detect melanoma at an early stage (Figure 4).
Figure 4.

How to Detect Melanoma Source:The Skin Cancer Foundation
Primary care physicians should be educated on high-risk sites for skin cancer especially melanoma. A thorough skin examination, including examination of nails, oral cavity, gums, palms, soles, groin, and perianal area should be performed regularly by a dermatologist (Cooley and Quale, 2013). Physicians should encourage persons to perform monthly self-skin examinations paying close attention to subungual skin, palms, soles, mucous membranes, and groin and perianal area. Pigmented lesions on gums and streaks in nails should be monitored regularly for changes as malignant transformation or suspicious lesion in people with color. Nearby lymph nodes should also be assessed (Gritz et al., 2003). For patients with history of NMSC or melanoma or multiple nevi, monthly self-skin examination is a must (Mahon et al., 2003).
It is best to avoid exposure during the high intensity hours of sunlight between 10 a.m. to 4 p.m. POC are advised to use a daily broad-spectrum sunscreen lotion or cream of at least SPF 30 with active ingredients like zinc oxide, titanium oxide or avobenzone which protect against both UVA and UVB rays (Gordon et al., 2009). Sunscreens should be applied liberally 30 minutes before going out and reapplied every 2 hours while outdoors. It is advisable to avoid tanning salons and intentional tanning with natural sunlight (Cho et al., 2010). A healthy diet that includes calcium and vitamin D supplements is recommended these days by doctors rather seeking the sun (Peterlik et al., 2009). Severe sunburns, especially during childhood, increase the risk of developing melanoma and other skin cancer as just one blistering sunburn can double the chances of developing melanoma later in life (Hughes et al., 1996; Sánchez et al., 2016). practicing sun-protective behavior such as seeking shade and use of protective clothing that covers head, neck and feet, sunglasses with ultraviolet-absorbing lenses (Zhu et al., 2016) should result in reduction or earlier detection of skin cancers in all communities.
Though skin cancer is less prevalent in people of color but when skin cancer occurs in non-whites, it often presents at a more advanced stage and thus the prognosis is worse as compared with white patients. The US Census Bureau projects that by the year 2050, fifty percent of the US population will comprise of Hispanics, Asians, and African Americans, so it becomes more important to raise awareness of skin cancer in people of color. The increased morbidity and mortality associated with skin cancer in patients of color as compared to white patients is because of the lack of awareness, diagnoses at a more advanced stage and socioeconomic factors such as access to care barriers. Physician promotion of skin cancer prevention strategies for all patients, regardless of ethnic background and socioeconomic status, can lead to timely diagnosis and treatment. Public education campaigns should be expanded to target communities of color to promote self-skin examination and stress importance of photo protection, avoidance of tanning bed use and early skin cancer detection and treatment. Efforts are needed to take the diversity in culture, beliefs and language across ethnicities into account so that skin cancer preventive education can reach the target population of color.
Conflict of Interest
Author Alpana K Gupta, Author Mausumi Bharadwaj and Author Ravi Mehrotra declare that they have no conflict of interest.
Acknowledgements
AKG (First author) acknowledges Department of Science and Technology (DST, New Delhi) for financial support under Women Scientist Project Scheme (WOS-A).
References
- Agbai ON, Buster K, Sanchez M, et al. Skin cancer and photoprotection in people of color: A review and recommendations for physicians and the public. [[Accessed September 28 2016]];J Am Acad Dermatol. 2014 70:748–62. doi: 10.1016/j.jaad.2013.11.038. Available at: http://www.ncbi.nlm.nih.gov/pubmed/24485530 . [DOI] [PubMed] [Google Scholar]
- Al-Dujaili Z, Henry M, Dorizas ASS, Sadick NSS. Skin cancer concerns particular to women. Int J Women’s Dermatology. 2015;1:123–25. doi: 10.1016/j.ijwd.2015.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anand P, Kunnumakkara AB, Sundaram C, et al. Cancer is a preventable disease that requires major lifestyle changes. Pharm Res. 2008;25:2097–116. doi: 10.1007/s11095-008-9661-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anon (n.d.) Cancer Statistics Review 1975-2013 - SEER Statistics. http://seer.cancer.gov/csr/1975_2013/
- Bigler C, Feldman J, Hall E, Padilla RS. Pigmented basal cell carcinoma in Hispanics. J Am Acad Dermatol. 1996;34:751–52. doi: 10.1016/s0190-9622(96)90007-9. [DOI] [PubMed] [Google Scholar]
- Bradford PT. Skin cancer in skin of color. Dermatol Nurs. 2009;21:170–77. [PMC free article] [PubMed] [Google Scholar]
- Brenner M, Hearing VJ. The protective role of melanin against UV damage in human skin. Photochem Photobiol. 2008;84:539–49. doi: 10.1111/j.1751-1097.2007.00226.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buster KJ, You Z, Fouad M, Elmets C. Skin cancer risk perceptions: a comparison across ethnicity, age, education, gender, and income. J Am Acad Dermatol. 2012;66:771–79. doi: 10.1016/j.jaad.2011.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrd KM, Wilson DC, Hoyler SS, Peck GL. Advanced presentation of melanoma in African Americans. J Am Acad Dermatol. 2004;50:21–4. doi: 10.1016/s0190-9622(03)02091-7. [DOI] [PubMed] [Google Scholar]
- Chang Y, Barrett JH, Bishop DT, Armstrong BK, et al. Sun exposure and melanoma risk at different latitudes: A pooled analysis of 5700 cases and 7216 controls. Int J Epidemiol. 2009;38:814–30. doi: 10.1093/ije/dyp166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen YC, Christiani DC, Su HJ, Hsueh YM, Smith TJ RL. Early-life or lifetime sunexposure, sunreaction, andthe risk of squamous cell carcinoma in an Asian population. Cancer Causes Control. 2010;21:771–76. doi: 10.1007/s10552-010-9505-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng SY, Luk NM, Chong LY. Special features of non-melanoma skin cancer in Hong Kong Chinese patients:10-year retrospective study. Int J Women’s Dermatology. 2001;7:22–8. [PubMed] [Google Scholar]
- Cho H, Hall JG, Kosmoski C, Fox RL, Mastin T. Tanning, skin cancer risk, and prevention: a content analysis of eight popular magazines that target female readers 1997-2006. Health Commun. 2010;25:1–10. doi: 10.1080/10410230903265938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooley JH, Quale LM. Skin cancer preventive behavior and sun protection recommendations. Semin Oncol Nurs. 2013;29:223–26. doi: 10.1016/j.soncn.2013.06.008. [DOI] [PubMed] [Google Scholar]
- Cress RD, Holly EA. Incidence of cutaneous melanoma among non-Hispanic whites, Hispanics, Asians, and blacks: an analysis of California cancer registry data 1988-93. Cancer Causes Control. 1997;8:246–52. doi: 10.1023/a:1018432632528. [DOI] [PubMed] [Google Scholar]
- Cummins DL, Cummins JM, Pantle H, et al. Cutaneous malignant melanoma. Mayo Clin Proc. 2006;81:500–07. doi: 10.4065/81.4.500. [DOI] [PubMed] [Google Scholar]
- D’Orazio J, Jarrett S, Amaro-Ortiz A, Scott T. UV radiation and the skin. Int J Mol Sci. 2013;14:12222–48. doi: 10.3390/ijms140612222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Bino S, Sok J, Bessac E, Bernerd F. Relationship between skin response to ultraviolet exposure and skin color type. Pigment Cell Res. 2006;19:606–14. doi: 10.1111/j.1600-0749.2006.00338.x. [DOI] [PubMed] [Google Scholar]
- Donaldson MR, Coldiron BM. No end in sight: the skin cancer epidemic continues. Semin Cutan Med Surg. 2011;30:3–5. doi: 10.1016/j.sder.2011.01.002. [DOI] [PubMed] [Google Scholar]
- Drucker AM, Rosen CF. Drug-Induced Photosensitivity. Drug Saf. 2011;34:821–37. doi: 10.2165/11592780-000000000-00000. [DOI] [PubMed] [Google Scholar]
- El_Ghissassi F, Baan R, Straif K, et al. WHO international Agency for research on cancer monograph working group. A review of human carcinogens-part D: radiation. Lancet Oncol. 2009;10:751–52. [Google Scholar]
- Finn L, Markovic SN, Joseph RW. Therapy for metastatic melanoma: the past, present, and future. BMC Med. 2012;10:23–30. doi: 10.1186/1741-7015-10-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman LC, Bruce S, Weinberg AD, et al. Early detection of skin cancer: racial/ethnic differences in behaviors and attitudes. J Cancer Educ. 1994;9:105–10. doi: 10.1080/08858199409528281. [DOI] [PubMed] [Google Scholar]
- Galiczynski EM, Vidimos AT. Nonsurgical treatment of nonmelanoma skin cancer. Dermatol Clin. 2011;29:297–09. doi: 10.1016/j.det.2011.01.011. [DOI] [PubMed] [Google Scholar]
- Gloster HM, Neal K. Skin cancer in skin of color. J Am Acad Dermatol. 2006;55:741–60. doi: 10.1016/j.jaad.2005.08.063. [DOI] [PubMed] [Google Scholar]
- Gohara MA. Skin cancer in skins of color. J Drugs Dermatol. 2008;7:441–45. [PubMed] [Google Scholar]
- Gordon LG, Scuffham PA, van der Pols JC, et al. Regular sunscreen use is a cost-effective approach to skin cancer prevention in subtropical settings. J Invest Dermatol. 2009;129:2766–71. doi: 10.1038/jid.2009.141. [DOI] [PubMed] [Google Scholar]
- Gordon R. Skin cancer: An overview of epidemilogy and risk factors. Semin Oncol Nursing. 2013;29:160–69. doi: 10.1016/j.soncn.2013.06.002. [DOI] [PubMed] [Google Scholar]
- Goss PE, Strasser-Weippl K, Lee-Bychkovsky BL, et al. Challenges to effective cancer control in China, India, and Russia. Lancet Oncol. 2014;15:489–38. doi: 10.1016/S1470-2045(14)70029-4. [DOI] [PubMed] [Google Scholar]
- Griffiths CE, Wang TS, Hamilton TA, Voorhees JJ, Ellis CN. A photonumeric scale for the assessment of cutaneous photodamage. Arch Dermatol. 1992;128:347–51. [PubMed] [Google Scholar]
- Gritz ER, Tripp MK, De Moor CA, et al. Skin cancer prevention counseling and clinical practices of pediatricians. Pediatr Dermatol. 2003;20:16–24. doi: 10.1046/j.1525-1470.2003.03004.x. [DOI] [PubMed] [Google Scholar]
- Halder RM, Bridgeman-Shah S. Skin cancer in African Americans. Cancer. 1995;75:667–73. doi: 10.1002/1097-0142(19950115)75:2+<667::aid-cncr2820751409>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- Halder RM, Ara CJ. Skin cancer and photoaging in ethnic skin. Dermatol Clin. 2003;21:725–32. doi: 10.1016/s0733-8635(03)00085-8. [DOI] [PubMed] [Google Scholar]
- Hansen L. Skin Cancer. Ref Modul Biomed Res. 2014;10:1–4. [Google Scholar]
- Hemminki K, Zhang H, Czene K. Time trends and familial risks in squamous cell carcinoma of the skin. Arch Dermatol. 2003;139:885–89. doi: 10.1001/archderm.139.7.885. [DOI] [PubMed] [Google Scholar]
- Ho SGY, Chan HHL. The Asian dermatologic patient: review of common pigmentary disorders and cutaneous diseases. Am J Clin Dermatol. 2009;10:153–68. doi: 10.2165/00128071-200910030-00002. [DOI] [PubMed] [Google Scholar]
- Hu S, Parmet Y, Allen G, et al. Disparity in melanoma: a trend analysis of melanoma incidence and stage at diagnosis among whites, Hispanics, and blacks in Florida. Arch Dermatol. 2009;145:1369–74. doi: 10.1001/archdermatol.2009.302. [DOI] [PubMed] [Google Scholar]
- Hughes BR, Wetton N, Collins M, Newton Bishop JA. Health education about sun and skin cancer: language, ideas and perceptions of young children. Br J Dermatol. 1996;134:624–29. doi: 10.1111/j.1365-2133.1996.tb06960.x. [DOI] [PubMed] [Google Scholar]
- Ichihashi M, Naruse K, Harada S, et al. Trends in nonmelanoma skin cancer in Japan. Recent Results Cancer Res. 1995;139:263–73. doi: 10.1007/978-3-642-78771-3_20. [DOI] [PubMed] [Google Scholar]
- Imahiyerobo-Ip J, Ip I, Jamal S, Nadiminti U, Sanchez M. Skin cancer awareness in communities of color. J Am Acad Dermatol. 2011;64:198–200. doi: 10.1016/j.jaad.2010.02.012. [DOI] [PubMed] [Google Scholar]
- Ishihara K, Saida T, Yamamoto A. Japanese skin cancer society prognosis and statistical investigation committee updated statistical data for malignant melanoma in Japan. Int J Clin Oncol. 2001;6:109–16. doi: 10.1007/pl00012091. [DOI] [PubMed] [Google Scholar]
- Jackson BA. Nonmelanoma skin cancer in persons of color. Semin Cutan Med Surg. 2009;28:93–5. doi: 10.1016/j.sder.2009.04.010. [DOI] [PubMed] [Google Scholar]
- Jacobsen AA, Galvan A, Lachapelle CC, et al. Defining the need for skin cancer prevention education in uninsured, minority, and immigrant communities. JAMA Dermatol. 2016:(in print). doi: 10.1001/jamadermatol.2016.3156. [DOI] [PubMed] [Google Scholar]
- Kaidbey KH, Agin PP, Sayre RM, Kligman AM. Photoprotection by melanin-a comparison of black and Caucasian skin. J Am Acad Dermatol. 1979;1:249–60. doi: 10.1016/s0190-9622(79)70018-1. [DOI] [PubMed] [Google Scholar]
- Kikuchi A, Shimizu H, Nishikawa T. Clinical histopathological characteristics of basal cell carcinoma in Japanese patients. Arch Dermatol. 1996;132:320–24. [PubMed] [Google Scholar]
- Kim GK, Del Rosso JQ, Bellew S. Skin cancer in Asians part 1: Nonmelanoma skin cancer. J Clin Aesthetic Dermatol. 2009a;2:39–42. [PMC free article] [PubMed] [Google Scholar]
- Kim M, Boone SL, West DP, et al. Perception of skin cancer risk by those with ethnic skin. Arch Dermatol. 2009b;145:207–08. doi: 10.1001/archdermatol.2008.566. [DOI] [PubMed] [Google Scholar]
- Koh D, Wang H, Lee J, et al. Basal cell carcinoma, squamous cell carcinoma and melanoma of the skin: analysis of the Singapore cancer registry data 1968-97. Br J Dermatol. 2003;148:1161–66. doi: 10.1046/j.1365-2133.2003.05223.x. [DOI] [PubMed] [Google Scholar]
- Kundu R V, Kamaria M, Ortiz S, et al. Effectiveness of a knowledge-based intervention for melanoma among those with ethnic skin. J Am Acad Dermatol. 2010;62:777–84. doi: 10.1016/j.jaad.2009.08.047. [DOI] [PubMed] [Google Scholar]
- Lallas A, Apalla Z, Ioannides D, et al. Dermoscopy in the diagnosis and management of basal cell carcinoma. Future Oncol. 2015;11:2975–84. doi: 10.2217/fon.15.193. [DOI] [PubMed] [Google Scholar]
- Larnier C, Ortonne JP, Venot A, et al. Evaluation of cutaneous photodamage using a photographic scale. Br J Dermatol. 1994;130:167–73. doi: 10.1111/j.1365-2133.1994.tb02895.x. [DOI] [PubMed] [Google Scholar]
- Lazareth V. Management of non-melanoma skin cancer. Semin Oncol Nurs. 2013;29:182–94. doi: 10.1016/j.soncn.2013.06.004. [DOI] [PubMed] [Google Scholar]
- Lee CS, Lim HW. Cutaneous diseases in Asians. Dermatol Clin. 2003;21:669–77. doi: 10.1016/s0733-8635(03)00078-0. [DOI] [PubMed] [Google Scholar]
- Leiter U, Eigentler T, Garbe C. Epidemiology of skin cancer. Adv Exp Med Biol. 2014;810:120–40. doi: 10.1007/978-1-4939-0437-2_7. [DOI] [PubMed] [Google Scholar]
- Leiter U, Garbe C. Epidemiology of melanoma and nonmelanoma skin cancer-the role of sunlight. Adv Exp Med Biol. 2008;624:89–103. doi: 10.1007/978-0-387-77574-6_8. [DOI] [PubMed] [Google Scholar]
- Longstreth J, de Gruijl FR, Kripke ML, et al. Health risks. J Photochem Photobiol B. 1998;46:20–39. doi: 10.1016/s1011-1344(98)00183-3. [DOI] [PubMed] [Google Scholar]
- Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madankumar R, Gumaste PV, Martires K, et al. Acral melanocytic lesions in the United States: Prevalence, awareness, and dermoscopic patterns in skin-of-color and non-Hispanic white patients. J Am Acad Dermatol. 2016;74:724–30. doi: 10.1016/j.jaad.2015.11.035. [DOI] [PubMed] [Google Scholar]
- Mahon SM. Skin cancer prevention: education and public health issues. Semin Oncol Nurs. 2003;19:52–61. doi: 10.1053/sonu.2003.50005. [DOI] [PubMed] [Google Scholar]
- Mann D. Moving beyond bob marley: understanding skin cancer in skin of color. Pract Dermatology. 2016 [Google Scholar]
- Markovic SN, Erickson LA, Rao RD, et al. Malignant melanoma in the 21st century, part 1: epidemiology, risk factors, screening, prevention, and diagnosis. Mayo Clin Proc. 2007;82:364–80. doi: 10.4065/82.3.364. [DOI] [PubMed] [Google Scholar]
- Merrill SJ, Subramanian M, Godar DE. Worldwide cutaneous malignant melanoma incidences analyzed by sex, age, and skin type over time (1955-2007): Is HPV infection of androgenic hair follicular melanocytes a risk factor for developing melanoma exclusively in people of European-ancestry? Dermatoendocrino. 2016;8:121539. doi: 10.1080/19381980.2016.1215391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer T. Molecular events in skin cancer. Cancer Treat Res. 2009;146:189–92. doi: 10.1007/978-0-387-78574-5_16. [DOI] [PubMed] [Google Scholar]
- Montagna W, Carlisle K. The architecture of black and white facial skin. J Am Acad Dermatol. 1991;24:929–37. doi: 10.1016/0190-9622(91)70148-u. [DOI] [PubMed] [Google Scholar]
- Mueller CSL, Reichrath J. Histology of melanoma and nonmelanoma skin cancer. Adv Exp Med Biol. 2008;624:215–26. doi: 10.1007/978-0-387-77574-6_17. [DOI] [PubMed] [Google Scholar]
- Narayanan DL, Saladi RN, Fox JL. Ultraviolet radiation and skin cancer. Int J Dermatol. 2010;49:978–86. doi: 10.1111/j.1365-4632.2010.04474.x. [DOI] [PubMed] [Google Scholar]
- Nikolaou V, Stratigos AJ. Emerging trends in the epidemiology of melanoma. Br J Dermatol. 2014;23:11–19. doi: 10.1111/bjd.12492. [DOI] [PubMed] [Google Scholar]
- Norval M, Lucas RM, Cullen AP, et al. The human health effects of ozone depletion and interactions with climate change. Photochem Photobiol Sci. 2011;10:199–225. doi: 10.1039/c0pp90044c. [DOI] [PubMed] [Google Scholar]
- Peterlik M, Grant WB, Cross HS. Calcium, vitamin D and cancer. Anticancer Res. 2009;29:3687–98. [PubMed] [Google Scholar]
- Pipitone M, Robinson JK, Camara C, et al. Skin cancer awareness in suburban employees: a Hispanic perspective. J Am Acad Dermatol. 2002;47:118–23. doi: 10.1067/mjd.2002.120450. [DOI] [PubMed] [Google Scholar]
- Rigel DS. Epidemiology of melanoma. Semin Cutan Med Surg. 2010;29:204–9. doi: 10.1016/j.sder.2010.10.005. [DOI] [PubMed] [Google Scholar]
- Riker AI, Zea N, Trinh T. The epidemiology, prevention, and detection of melanoma. Ochsner J. 2010;10:56–65. [PMC free article] [PubMed] [Google Scholar]
- Rubin AI, Chen EH, Ratner D. Basal-cell carcinoma. N Engl J Med. 2005;353:2262–69. doi: 10.1056/NEJMra044151. [DOI] [PubMed] [Google Scholar]
- Saladi RN, Persaud AN. The causes of skin cancer: a comprehensive review. Drugs Today. 2005;41:37–53. doi: 10.1358/dot.2005.41.1.875777. [DOI] [PubMed] [Google Scholar]
- Sánchez G, Nova J, Rodriguez-Hernandez AE, et al. Sun protection for preventing basal cell and squamous cell skin cancers. Cochrane database Syst Rev. 2016;7:CD011161. doi: 10.1002/14651858.CD011161.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simões MCF, Sousa JJS, Pais AACC. Skin cancer and new treatment perspectives: A review. Cancer Lett. 2015;357:8–42. doi: 10.1016/j.canlet.2014.11.001. [DOI] [PubMed] [Google Scholar]
- Sng J, Koh D, Siong WC, Choo TB. Skin cancer trends among Asians living in Singapore from 1968 to 2006. J Am Acad Dermatol. 2009;61:426–32. doi: 10.1016/j.jaad.2009.03.031. [DOI] [PubMed] [Google Scholar]
- Society american cancer. Melanoma Skin Cancer. Cancer Facts & Figs 2016. 2016 [Google Scholar]
- Steding-Jessen M, Birch-Johansen F, Jensen A, et al. Socioeconomic status and non-melanoma skin cancer: a nationwide cohort study of incidence and survival in Denmark. Cancer Epidemiol. 2010;34:689–95. doi: 10.1016/j.canep.2010.06.011. [DOI] [PubMed] [Google Scholar]
- Stern RS. Prevalence of a history of skin cancer in 2007: results of an incidence-based model. Arch Dermatol. 2010;146:279–82. doi: 10.1001/archdermatol.2010.4. [DOI] [PubMed] [Google Scholar]
- Tadokoro T, Kobayashi N, Zmudzka BZ, et al. UV-induced DNA damage and melanin content in human skin differing in racial/ethnic origin. FASEB J. 2003;17:1177–79. doi: 10.1096/fj.02-0865fje. [DOI] [PubMed] [Google Scholar]
- Togsverd-Bo K, Sørensen SS, Hædersdal M. Organ transplant recipients need intensive control and treatment of skin cancer. Ugeskr Laeger. 2013;175:1408–11. [PubMed] [Google Scholar]
- Tucker MA, Goldstein AM. Melanoma etiology: where are we? Oncogene. 2003;22:3042–52. doi: 10.1038/sj.onc.1206444. [DOI] [PubMed] [Google Scholar]
- Weinstock MA. Cutaneous melanoma: public health approach to early detection. Dermatol Ther. 2006;19:26–31. doi: 10.1111/j.1529-8019.2005.00053.x. [DOI] [PubMed] [Google Scholar]
- Wu X-C, Eide MJ, King J, et al. Racial and ethnic variations in incidence and survival of cutaneous melanoma in the United States 1999-2006. J Am Acad Dermatol. 2011;65:26–37. doi: 10.1016/j.jaad.2011.05.034. [DOI] [PubMed] [Google Scholar]
- Young C. Solar ultraviolet radiation and skin cancer. Occup Med (Lond) 2009;59:82–88. doi: 10.1093/occmed/kqn170. [DOI] [PubMed] [Google Scholar]
- Zell JA, Cinar P, Mobasher M, et al. Survival for patients with invasive cutaneous melanoma among ethnic groups: the effects of socioeconomic status and treatment. J Clin Oncol. 2008;26:66–75. doi: 10.1200/JCO.2007.12.3604. [DOI] [PubMed] [Google Scholar]
- Zhu G, Lin J-C, Kim S-B, et al. Asian expert recommendation on management of skin and mucosal effects of radiation, with or without the addition of cetuximab or chemotherapy, in treatment of head and neck squamous cell carcinoma. BMC Cancer. 2016;16:42–54. doi: 10.1186/s12885-016-2073-z. [DOI] [PMC free article] [PubMed] [Google Scholar]


