Abstract
Objective:
To compare dosimetric parameters of 3 dimensional conformal radiotherapy (3 DCRT) and intensity modulated radiotherapy (IMRT) in terms of target coverage and doses to organs at risk (OAR) in the management of rectal carcinoma.
Methods:
In this prospective study, conducted between August 2014 and March 2016, all patients underwent CT simulation along with a bladder protocol and target contouring according to the Radiation Therapy Oncology Group (RTOG) guidelines. Two plans were made for each patient (3 DCRT and IMRT) for comparison of target coverage and OAR.
Result:
A total of 43 patients were recruited into this study. While there were no significant differences in mean Planning Target Volume (PTV) D95% and mean PTV D98% between 3 DCRT and IMRT, mean PTV D2% and mean PTV D50% were significantly higher in 3 DCRT plans. Compared to IMRT, 3 DCRT resulted in significantly higher volumes of hot spots, lower volumes of cold spots, and higher doses to the entire OAR.
Conclusion:
This study demonstrated that IMRT achieves superior normal tissue avoidance (bladder and bowel) compared to 3 DCRT, with comparable target dose coverage.
Keywords: 3 DCRT, IMRT, rectal cancer, small bowel avoidance, urinary bladder avoidance
Introduction
Over the years surgery has been regarded as the primary treatment for rectal carcinoma. Total mesorectal excision (TME) is preferred over Abdominoperineal excision (APR) due to its better overall survival rate and a lower rate of tumor recurrence (Ferlay et al., 2015). With the introduction of chemoradiation, combined modality treatment was attempted with big triumph.
With the advent of improved treatment planning, the practice of using radiotherapy by a conventional technique for treating rectal cancer is gradually declining. Nevertheless, this mode of radiotherapy delivery continues to be utilized by various institutions in developing countries, such as India, due to lack of availability of conformal techniques. Procedures, such as the utilization of prone positioning, using belly-board equipment to attain bowel dislocation away from the irradiated field have been specified for decreasing the volume of the irradiated small intestine. In recent times, there is curiosity about the use of highly advanced treatment approaches, for instance, intensity modulated radiotherapy (IMRT) that offers a treatment for the rectum. Nevertheless, there are very small number of studies that aim to evaluate the newer techniques like 3 DCRT and IMRT with respect to target volume coverage and organs at risk (OAR) (Diaz-Gonzalez et al., 2007).
This study attempts to compare the dosimetric parameters of 3 DCRT and IMRT in terms of target coverage and doses to OAR in the management of rectal carcinoma.
Materials and Methods
This was a prospective study in which 43 consecutive patients with locally advanced rectal cancer (stage II and III) who underwent neoadjuvant chemoradiation, between August 2014 and March 2016 were studied. The study was approved by the ethical board of the hospital.
The patients were simulated in the Computed Tomography (CT) simulator - SOMATOM sensation open™ (Global Siemens Healthcare Henkestr, Erlanger, Germany) in supine position and were immobilized with the help of orfit-ray™ (Orfit Industries, Wijnegem, Belgium) thermoplastic cast. Bladder protocol was followed (after voiding urine, patient was asked to drink 700 cc of water) and scans were taken after the patient had the urge to pass urine. A slice thickness of 3 mm was used for target delineation. The Digital Imaging and Communication in Medicine (DICOM) files were transferred to the Varian Eclipse™ Version 10 (Varian Medical Systems, Palo Alto, CA) where target volumes were contoured according to the Radiation Therapy Oncology Group guidelines (Myerson et al., 2009). The planning target volume (PTV) was prescribed to a dose of 50.4 Gy in 28 fractions and the OAR were given constraints as follows – small bowel (SB): SB V45Gy (Volume of SB in cc receiving more than 45 Gy) less than 195 cc, SB Davg (Average dose received by the small bowel) less than 30 Gy; urinary bladder (UB): UB V50Gy (Volume of UB in percentage receiving more than 50 Gy) less than 50%. The OAR constraints were according to institutional policy derived from protocols in various studies (Bentzen et al., 2010; Mzenda et al., 2011).
Although all patients were treated with IMRT, another set of plans were generated for each patient by 3 DCRT. IMRT technique was planned using 7 field techniques utilizing static beam angles - 0, 60, 100, 135, 225, 260 and 310 degrees with static multi leaf collimator (MLC), while 3 DCRT technique was planned using beam angles – 0, 90, 180 and 270. A dosimetric comparison was done between the two techniques comparing target coverage and doses received by OAR. Following parameters were compared for the evaluation of target coverage – PTV D95% (Dose received by 95% of the PTV), PTV D98% (Dose received by 98% of the PTV), PTV D2% (Dose received by 2% of the PTV), PTV D50% (Dose received by 50% of the PTV), Homogeneity index (HI) {(PTV D2% - PTV D98%)/PTV D50%}, PTV V93% (PTV volume receiving less than 93% of the prescribed dose) and PTV V110% (PTV volume receiving more than 110% of the prescribed dose). The parameters used for the evaluation of OAR were SB V45Gy, SB Davg, UB V50Gy and UB Davg (Average dose received by the urinary bladder).
Statistical Analysis
The continuous measurements were reported as mean (standard deviation). The statistical comparisons for parametric quantitative variables were done using paired student‘t’ test, while Mann-Whitney ‘U’ test was used for non-parametric data. All statistical analysis were performed using statistical package for the social science system (SPSS version 20, SPSS Inc, Chicago, IL, USA), and p value <0.05 was considered statistically significant. All p values reported are two-tailed.
Results
There were no significant differences in mean PTV D95% and mean PTV D98% between 3 DCRT and IMRT, however mean PTV D2% and mean PTV D50% were significantly higher in 3 DCRT plans. Compared to IMRT, 3 DCRT resulted in significantly higher volumes of hot spots and lower volumes of cold spots. IMRT resulted in significantly lower doses to the entire OAR (Table 1).
Table 1.
Dosimetric Comparison between IMRT and 3 DCRT in Rectal Cancer
| Parameter | Mean IMRT(±SD) | Mean 3 DCRT(±SD) | Significance (p value) |
|---|---|---|---|
| PTV D95% | 50.2 (±0.4) Gy | 50.1 (±0.6) Gy | 0.447 |
| PTV D98% | 49.2 (±0.5) Gy | 49.2 (±0.7) Gy | 0.444 |
| PTV D2% | 53.8 (±0.5) Gy | 54.9 (±1.1) Gy | < 0.001 |
| PTV D50% | 52.0 (±0.4) Gy | 52.3 (±0.5) Gy | < 0.001 |
| HI | 0.1 (±0.0) | 0.1 (±0.0) | < 0.001 |
| PTV V110% | 0.1 (±0.2)% | 4.2 (±5.3)% | < 0.001 |
| PTV V93% | 0.1 (±0.1)% | 0.0 (±0.0)% | < 0.001 |
| SB Davg | 21.9 (±4.6) Gy | 25.3 (±5.6) Gy | < 0.001 |
| SB V45Gy | 78.8 (±43.4) cc | 163.5 (±60.5) cc | < 0.001 |
| UB Davg | 43.4 (±2.1) Gy | 49.9 (±1.8) Gy | < 0.001 |
| UB V50Gy | 24.7% | 78.2% | < 0.001 |
Discussion
Few dosimetric studies have compared conventional fields (bony anatomy), 3 DCRT, 3-field IMRT and multi-field IMRT planning. Amongst all the techniques conventional fields technique has been found to provide inferior target coverage and higher volume of bowel volume irradiated. The current study was undertaken to compare target coverage and normal tissue avoidance between 3 DCRT and IMRT, and demonstrated that IMRT achieves superior normal tissue avoidance (bladder and bowel) compared to 3 DCRT, with comparable target dose coverage.
Figure 1.
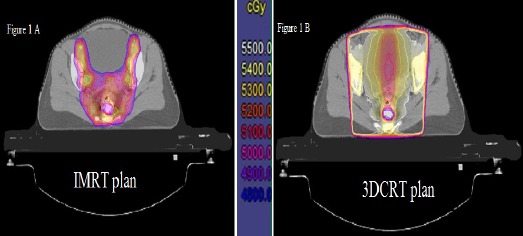
A and B Show the Dose Distribution in Axial CT Slices of Same Patient being Planned for IMRT and 3DCRT Respectively
Figure 2.
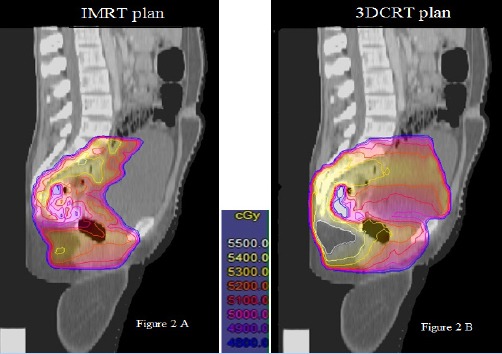
A and B Show the Dose Distribution in Sagittal CT Slices of Same Patient being Planned for IMRT and 3DCRT Respectively
Study conducted at Royal Marsden hospital showed 3 DCRT to be providing significantly higher target coverage (PTV D95%, PTV D98%, PTV D2%) compared to IMRT technique (Urbano et al., 2006). In our study similar trend was observed, however the results did not reach statistical significance. IMRT plans in our study were more homogeneous than 3 DCRT plans. This finding is in contrast with other studies which have demonstrated that IMRT generates more inhomogeneous dose distributions (Arbea et al., 2010; Urbano et al., 2006).
Mean SB V45Gy being better with IMRT than 3 DCRT (78.8 cc and 163.5 cc respectively) in our study clearly showed the greatest advantage of IMRT over 3 DCRT in sparing of small bowel. Our finding is in line with a study conducted at the Royal Marsden hospital where mean SB V45Gy for IMRT and 3 DCRT were 214 ± 183 cm3 and 69 ± 51 cm3 (Urbano et al., 2006). Similar observations were done by other authors as well (Arbea et al., 2010; Baglan et al., 2002; Chen et al., 2012). While comparing intensity-modulated arc therapy (IMAT) and 3 DCRT in rectal cancer, Duthoy (2004) showed mean dose to SB being significantly lower with IMAT than 3 DCRT, finding again reproduced in our study. None of the IMRT plans in our study had a mean dose to the SB greater than 30Gy. Arbea (2010), showed SB V40Gy (Volume of SB in cc receiving more than 40 Gy) with IMRT was approximately 1/3rd of that with 3 DCRT (68.9 cc vs. 140.3 cc). In similar line, Tho (2006) also showed that inverse planning reduced the median dose to the small bowel by 5.1Gy. Thus, ours and other studies quoted above have proved that IMRT is a very effective technique for rectal cancer as far as SB sparing is concerned. Further clinical studies are needed to confirm whether this dosimetric advantage indeed translates into clinical benefits in terms of reduced gastro-intestinal toxicities.
Urinary bladder is the next important organ at risk after SB which is expected to be spared better with IMRT than 3 DCRT. Various researchers have studied UB V50Gy, though results varied widely, IMRT scored over 3 DCRT plans in all (Mzenda et al.; Urbano et al., 2006). In our study, the mean UB V50Gy in IMRT and 3 DCRT plans was 24.7 % and 78.2 % respectively. In the Royal Marsden hospital study, it was 6.4 % in IMRT plans, while 32.7 % in 3 DCRT plans (Urbano et al., 2006). There is discordance in the absolute UB V50Gy figures between both studies, may be due to the consequence of the difference in bladder protocol, contouring, beam angles selected, weightage given for each field and priorities during planning.
This study demonstrated that IMRT achieves superior normal tissue avoidance (bladder and bowel) compared to 3 DCRT, with comparable target dose coverage. However, the key question whether this dosimetric advantage translates into a significant and meaningful clinical benefit remains unanswered and needs clinical correlation.
References
- Arbea L, Ramos LI, Martínez-Monge R, et al. Intensity-modulated radiation therapy (IMRT) vs. 3D conformal radiotherapy (3DCRT) in locally advanced rectal cancer (LARC): dosimetric comparison and clinical implications. Radiat Oncol. 2010;5:1–9. doi: 10.1186/1748-717X-5-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baglan KL, Frazier RC, Yan D, et al. The dose-volume relationship of acute small bowel toxicity from concurrent 5-FU-based chemotherapy and radiation therapy for rectal cancer. Int J Radiat Oncol Biol Phys. 2002;52:176–83. doi: 10.1016/s0360-3016(01)01820-x. [DOI] [PubMed] [Google Scholar]
- Bentzen SM, Constine LS, Deasy JO, et al. Quantitative Analyses of Normal Tissue Effects in the Clinic (QUANTEC): an introduction to the scientific issues. Int J Radiat Oncol Biol Phys. 2010;76:3–9. doi: 10.1016/j.ijrobp.2009.09.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen RC, Mamon HJ, Ancukiewicz M, et al. Dose–Volume effects on patient-reported acute gastrointestinal symptoms during chemoradiation therapy for rectal cancer. Int J Radiat Oncol Biol Phys. 2012;83:513–7. doi: 10.1016/j.ijrobp.2012.01.013. [DOI] [PubMed] [Google Scholar]
- Diaz-Gonzalez JA, Arbea L, Aristu J, et al. Rectal cancer treatment: Improving the picture. World J Gastroenterol. 2007;13:5805–12. doi: 10.3748/wjg.v13.i44.5805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duthoy W, De Gersem W, Vergote K, et al. Clinical implementation of intensity-modulated arc therapy (IMAT) for rectal cancer. Int J Radiat Oncol Biol Phys. 2004;60:794–806. doi: 10.1016/j.ijrobp.2004.04.016. [DOI] [PubMed] [Google Scholar]
- Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:359–86. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- Guerrero Urbano MT, Henrys AJ, Adams EJ, et al. Intensity-modulated radiotherapy in patients with locally advanced rectal cancer reduces volume of bowel treated to high dose levels. Int J Radiat Oncol Biol Phys. 2006;65:907–16. doi: 10.1016/j.ijrobp.2005.12.056. [DOI] [PubMed] [Google Scholar]
- Myerson RJ, Garofalo MC, El Naqa I, et al. Elective clinical target volumes for conformal therapy in anorectal cancer: a radiation therapy oncology group consensus panel contouring atlas. Int J Radiat Oncol Biol Phys. 2009;74:824–30. doi: 10.1016/j.ijrobp.2008.08.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mzenda B, Peters P, Pettingell J, et al. 1336 poster, A comparison of doses to OARs in inverse planned IMRT and 3D conformal prostate treatment planning. Radiother Oncol. 2011;99:499–500. [Google Scholar]
- O’Connell MJ, Martenson JA, Wieand HS, et al. Improving adjuvant therapy for rectal cancer by combining protracted-infusion fluorouracil with radiation therapy after curative surgery. N Engl J Med. 1994;331:502–7. doi: 10.1056/NEJM199408253310803. [DOI] [PubMed] [Google Scholar]
- Tho LM, Glegg M, Paterson J, et al. Acute small bowel toxicity and preoperative chemoradiotherapy for rectal cancer: investigating dose-volume relationships and role for inverse planning. Int J Radiat Oncol Biol Phys. 2006;66:505–13. doi: 10.1016/j.ijrobp.2006.05.005. [DOI] [PubMed] [Google Scholar]


