Abstract
Objectives:
To determine the frequency of delayed diagnosis of oral squamous cell carcinoma in our setup; highlighting factors responsible for any delay and their possible relevance to demographic and diagnostic features.
Methods:
This cross sectional study of six months duration was conducted in the Oral and Maxillofacial Surgery Department of the Armed Forces Institute of Dentistry, Rawalpindi, Pakistan. A total of 246 patients, both male and female, having a biopsy proven definitive diagnosis of OSCC were included using a consecutive sampling technique. Delay in diagnosis was assessed from the stated period of time from when the patient first noticed symptoms of disease until a definitive diagnosis was made. We concluded delayed diagnosis if this was more than 40 days.
Results:
The ages of patients ranged from 27 to 60 years with a mean of 46.7 ± 10.2 years and a marked male predominance (3.7:1). Delayed diagnosis was observed in 91.5% of cases. However, statistically no significant differences were found with age, gender, marital, education status, household income and time of biopsy.
Conclusion:
Our primary finding of delayed diagnosis with no prior contact with any health care professional clearly reflects a need of taking urgent measures to avoid serious impacts on morbidity and mortality associated with OSCC.
Keywords: Squamous cell carcinoma, frequency, diagnosis, oral cancer
Introduction
Oral squamous cell Carcinoma (OSCC) is amongst the ten commonest malignancies in Pakistan and also in many other countries of the world (Petersen PE, 2008; Zulfiqar et al., 2013; Gröbe et al., 2014) accounting more than 90% of head and neck tumours (Huang et al., 2014; Vigneswaran, and Williams, 2014).. Staging of the Oropharyngeal carcinoma at diagnosis remains the most important prognostic factor as advanced stages frequently results in higher mortality. Almost half of them get diagnosed at an advanced stage (III or IV) and depending on their site have 20-50% low survival rate of 5 years (Seoane-Romero et al., 2012).
Staging of a tumour at its diagnosis is an essential parameter that needs intense research. If left undiagnosed, untreated or even if treatment is delayed can results in regional and distant metastasis with more adverse health outcomes. No doubt, some predictors of survival can vary from patient to patient like gender, race, socio-economic status, education while others are linked to its biology; location, grade and stage. Numerous studies have emphasized the importance of timely diagnosis for better prognosis, elsewise severe outcomes may occur. Lack of awareness, late presentation and delayed referral by medical professionals are major causes for its delayed diagnosis resulting in poor prognosis. Keeping all this in mind, the present study was designed to determine frequency of delay in diagnosis of OSCC in our setup. We also tried to highlight various factors that can contribute in its delayed diagnosis and their possible relevance with demographic and diagnostic elements.
Material and Methods
This cross sectional study of six months duration was conducted at Oral and Maxillofacial Surgery department of Armed Forces Institute of Dentistry (AFID) Rawalpindi, Pakistan. A total of 246 patients recruited for the study were diagnosed with OSCC through clinical and histological examination reporting at Oral and Maxillofacial Surgery department of AFID and ENT department of Combined Military Hospital (CMH) Rawalpindi, Pakistan. All these cases were selected by consecutive sampling technique and their demographic data was collected from hospital request forms. Only biopsy proven definitive diagnosed cases were included and their signed informed consents along with a detailed history were obtained. Aged, bed ridden, critically ill or patients unable to give proper history due to psychotic illness or any other reason were excluded from study. We assessed the delay in diagnosis from history i.e. time elapsed when the patient noticed first symptoms of the disease and till a definitive diagnosis was made. We labeled all such cases as delayed who took more than 40 days for a confirmed diagnosis.
Means and standard deviations were calculated for all quantitative variables like age and time taken from appearance of first symptoms till a definitive diagnosis was made. Percentages and frequencies were presented for all qualitative variables like gender, marital status, education, monthly household income and frequency of patients delay in diagnosis of OSCC. Stratification with respect to age (quantitative), gender, marital status, education and monthly household income was done to see effects of these parameters on outcome variables (delayed and non-delayed diagnosis) through t-test and chi square test. Data was analyzed using SPSS software version 16 and p value < 0.05 was taken as significant.
Results
The mean age of selected patients of our study was 46.70 ± 10.18 years; ranging from 27 to 60 years with a male predominance of 3.7: 1. Of these 178 (72.4%) were currently married, 15 (6.1%) widowed, 9 (3.7%) divorced, 30 (12.2%) single, and 14 (5.7%) separated. Regarding their education status 29.7% were graduated while 28.9% and 26.4% have completed secondary and intermediate education respectively; 10.2% had done post-graduation while the remaining 4.9% could attain just primary level of education.
Most of these patients were either very poor or belonged to lower middle class; only 4.9% had a monthly income of over 20,000 rupees. 13.8% of these patients noticed symptoms of the disease in a period of less than 3 months before being reported to a health care provider, 29.7% took 3 to 4 month, 42.7% took 4 to 6 months while rest 13.8% had these for over 6 months before consulting a doctor. Most of them (58.54%) reported for the first time to AFID or CMH and just 102 (41.46%) had a previous exposure to other health care professional. Only 8.5% got their diagnosis confirmed within 40 days of appearance of first symptoms of disease and the rest 91.5% showed a clear delay in their diagnosis (Figure 1).
Figure 1.
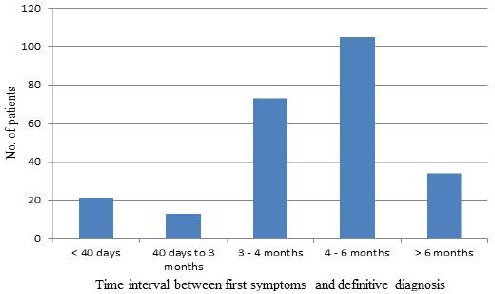
Frequency of Time Interval between First Symptom and Definite Diagnosis of Squamous Cell Carcinoma
According to various stratifications no significant difference of age, gender, marital status, education status, house hold income and time of biopsy was noted on this delay in diagnosis (p-value > 0.05) (Table 1).
Table 1.
Comparison of Delayed and Non-Delayed Diagnosis with Respect to Gender, Marital Status, Education, Monthly Income and Time of Biopsy
| Parameter | Status | Delayed | non-delayed | Total | p-value |
|---|---|---|---|---|---|
| Male | 176 | 18 | 194 | 0.421 | |
| Gender | Female | 49 | 3 | 52 | |
| Currently married | 159 | 19 | 178 | 0.367 | |
| Widowed | 14 | 1 | 15 | ||
| Divorced | 9 | 0 | 9 | ||
| Marital Status | Not married | 29 | 1 | 30 | |
| Separated | 14 | 0 | 14 | ||
| Primary | 12 | 0 | 12 | 0.532 | |
| Secondary | 66 | 5 | 71 | ||
| Education | Higher secondary | 57 | 8 | 65 | |
| Graduate | 68 | 5 | 73 | ||
| Post graduate | 22 | 3 | 25 | ||
| < 5,000 | 14 | 0 | 14 | 0.215 | |
| 6-10,000 | 32 | 6 | 38 | ||
| 11-15,000 | 132 | 9 | 141 | ||
| Monthly income | 16-20,000 | 37 | 4 | 41 | |
| > 20,000 | 10 | 2 | 12 | ||
| Same day | 172 | 17 | 189 | 0.527 | |
| Time of biopsy sample | After 1-2 days | 40 | 4 | 44 | |
| After > 2 days | 13 | 0 | 13 |
Discussion
The most frequent occurring oral cancer reported in adults is squamous cell carcinoma with smoking and alcohol attributed as its primary risk factors (Albuquerque et al., 2011; Shaikh et al., 2015). Delay in its diagnosis also contributes in aggravation of severity with complication in management plan. This study therefore was planned to evaluate frequency of this delayed diagnosis in our setup and to identify various factors that can attribute in this delay.
A Turkish case report conducted in 2011 mentioned outcomes of three oral squamous cell carcinomas with a delayed diagnosis. All patients presented with pain, swelling and similar other complaints in their jaws. The authors were of the view that early diagnosis is critical for OSCC and dentists can play a significant role in this regard and also to prevent oral cancers (Akbulut et al., 2011).
The mean age of patients in our study was 46.7 ± 10.18 years with a range of 27 to 60 years. Comparing with other studies a significant variation was observed that might be a result of difference in study settings. A Japanese study that dealt in detail six cases of spindle cell squamous carcinoma (SCSC) of oral cavity concluded mean age of 72 years which comparatively was quite higher than patients of our study. They also observed a difference in male to female ratio of 2:1 (Takata et al., 1991). However, a Chinese study on comparatively larger number of patients of oral cancer (163) showed similar trend to our study; male to female ratio of 3.66:1 and age range of 30 to 85 years with a mean 59.3 years (Zhong et al., 2008).
It is a commom belief that education brings awareness in masses, hence can prevent delay in diagnosis of any illness. However, this was not seen in our study where most of the patients despite having some level of education did not respond in time. A Malaysian study emphasized on awareness and education of patients for timely diagnosis of OSCC. The authors mentioned that 50% of their study patients seek professional advice after 3 months of becoming aware of the disease. The mean clinicians’ and patients’ delay recorded was 10.3 and 28.9 weeks respectively. No doubt, both medical and dental professionals played some role in reducing this delay in diagnosis, still more advanced lesions were referred mainly by dental practitioners. They also mentioned rise in lack of patients’ awareness, misdiagnosis by clinicians and late detection by dental practitioners; suggesting urgent measures for early diagnosis of OSCC (Khoo et al., 1998).
In our study 13.8% of patients had symptoms of OSCC for less than 3 months prior to seeking medical advice and a similar percentage had these for over six months. Only 8.5% of patients got diagnosed within 40 days of appearance of first symptoms of the disease, 5.3% between 40 to 120 days, 29.7% between 3 to 4 months, 42.7% between 4 to 6 months and the remaining 13.8% took even more than 6 months to get diagnosis of OSCC. This delayed diagnosis observed in over 90% of our cases is compatible with the results of other studies (Driemel et al., 2007; Epstein et al., 2008). In our study the delay in diagnosis resulted mainly because ofnot reporting timely to health care professionals. They did not take initial symptoms seriously and relied on local / home remedial measures. A slight delay was attributed by concerned doctors and dentists as well by not prescribing timely investigations and referrals. There is an essential need of raising awareness in the masses for early diagnosis and better prognosis of OSCC. As our study included data from a single setup representing a small portion of our community, therefore, extensive studies are required to unveil further facts leading in its delayed diagnosis.
Various socio- economic and demographic factors played an insignificant role in its delayed diagnosis. Delayed diagnosis was significantly noted in 91.46% of our patients; over 80% of them got it diagnosed after 4 months of appearance of first symptoms. Most of these patients also had no previous contact with any health care professional. Hence, necessary measures are suggested to diagnose it at the earliest to maximally reduce associated morbidity and mortality.
Acknowledgement
We are extremely thankful to administration and technical staff of Oral and Maxillofacial Surgery Department of Armed Forces Institute of Dentistry (AFID) Rawalpindi for their support in accomplishing this project.
References
- Akbulut N, Oztas B, Kursun S, Evirgen S. Delayed diagnosis of oral squamous cell carcinoma: a case series. J Med Case Rep. 2011;5:1. doi: 10.1186/1752-1947-5-291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albuquerque R, López-López J, Marí-Roig A, et al. Oral tongue squamous cell carcinoma (OTSCC): alcohol and tobacco consumption versus non-consumption. A study in a Portuguese population. Braz Dent J. 2011;22:517–21. doi: 10.1590/s0103-64402011000600013. [DOI] [PubMed] [Google Scholar]
- Gröbe A, Blessmann M, Hanken H, et al. Prognostic relevance of circulating tumor cells in blood and disseminated tumor cells in bone marrow of patients with squamous cell carcinoma of the oral cavity. Clin Cancer Res. 2014;20:425–33. doi: 10.1158/1078-0432.CCR-13-1101. [DOI] [PubMed] [Google Scholar]
- Driemel O, Kunkel M, Hullmann M, et al. Diagnosis of oral squamous cell carcinoma and its precursor lesions. J Dtsch Dermatol Ges. 2007;5:1095–100. doi: 10.1111/j.1610-0387.2007.06397.x. [DOI] [PubMed] [Google Scholar]
- Epstein JB, Gorsky M, Cabay RJ, Day T, Gonsalves W. Screening for and diagnosis of oral premalignant lesions and oropharyngeal squamous cell carcinoma: role of primary care physicians. Can Fam Physician. 2008;54:870–5. [PMC free article] [PubMed] [Google Scholar]
- Huang WC, Chan SH, Jang TH, et al. miRNA- 491-5p and GIT1 serve as modulators and biomarkers for oral squamous cell carcinoma invasion and metastasis. Cancer Res. 2014;74:751–64. doi: 10.1158/0008-5472.CAN-13-1297. [DOI] [PubMed] [Google Scholar]
- Khoo SP, Shanmuhasuntharam P, Mahadzir WM, et al. Factors involved in the diagnosis of oral squamous cell carcinoma in Malaysia. Asia-Pac J Public Health. 1998;10:49–51. doi: 10.1177/101053959801000111. [DOI] [PubMed] [Google Scholar]
- Petersen PE. The world oral health report. 2003: Continuous improvement of oral health in the 21st century–the approach of the WHO global oral health Program. community dent oral opidemiol. 2003;31:3–24. doi: 10.1046/j..2003.com122.x. [DOI] [PubMed] [Google Scholar]
- Seoane-Romero JM, Vázquez-Mahía I, Seoane J, et al. Factors related to late stage diagnosis of oral squamous cell carcinoma. Med Oral Patol Oral Cir Bucal. 2012;17:35–40. doi: 10.4317/medoral.17399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaikh AH, Muhammad T, Rasheed T. Evaluating the correlation between histopathological patterns of Oral Squamous Cell Carcinoma, age & site. Pak Oral Dental J. 2015;35:30–2. [Google Scholar]
- Takata T, Ito H, Ogawa I, et al. Spindle cell squamous carcinoma of the oral region. Virchows Archiv A. 1991;419:177–82. doi: 10.1007/BF01626345. [DOI] [PubMed] [Google Scholar]
- Vigneswaran N, Williams Epidemiologic trends in head and neck cancer and aids in diagnosis. Oral maxillofac Surg clin North Am. 2014;26:123–41. doi: 10.1016/j.coms.2014.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong LP, Zhou XJ, Wei KJ, et al. Application of serum tumor markers and support vector machine in the diagnosis of oral squamous cell carcinoma. Shanghai Kou Qiang Yi Xue. 2008;17:457–60. [PubMed] [Google Scholar]
- Zulfiqar A, Nagi AH, Nasim N. A clinico-pathological study of orofacial squamous cell carcinoma in local population. Biomedica. 2013;29:147–150. [Google Scholar]


