Abstract
Objective
Posttraumatic stress disorder (PTSD) is a debilitating psychiatric illness that frequently remains undiagnosed and untreated. While extensive research has been conducted among veterans, little research has evaluated course of treatment for PTSD in a general hospital setting.
Method
We utilized data from the Partners Healthcare Research Patient Database Registry to evaluate mental health treatment utilization, including psychotherapy and pharmacotherapy, by patients with recently diagnosed primary PTSD following Diagnostic and Statistical Manual IV criteria between January 1, 2002 and June 30, 2011. We additionally evaluated predictors of treatment utilization 6 months post-diagnosis.
Results
Among 2,475 patients with recently diagnosed prim ary PTSD, approximately half (55.7%) had any therapy visit and 10% at least 12 therapy visits in the 6 months following diagnosis. Approximately half (47.0%) received a psychiatric prescription, with 29.3% receiving a selective serotonin reuptake inhibitor (SSRI), 11.8% an atypical antipsychotic and 24.4% a benzodiazepine. Latinos were 25% more likely to have an SSRI prescription, 35% more likely to have an atypical antipsychotic prescription and 28% more likely to have any psychotherapy. Men were 96% more likely to have an atypical antipsychotic prescription. Patients with Medicare were 20% less likely to have any psychotherapy, and patients with Medicaid were 35% less likely to have 12 or more therapy visits.
Conclusion
Many patients with a primary diagnosis of PTSD do not receive psychotherapy, and psychiatric prescriptions, including atypical antipsychotics and benzodiazepines, are common. Future research is needed to determine quality of care received and explore sub-population specific barriers limiting access to care.
Introduction
Posttraumatic stress disorder (PTSD) is a complex mental health condition that can arise after the experience of one or more traumatizing events.1 Individuals who develop PTSD experience intrusive thoughts of the trauma, avoidance of reminders of the trauma, negative alterations in thought processes and mood and alterations in reactivity.1 These symptoms cause significant distress and impairment in occupational and social functioning.1, 2 Approximately 6.8% of U.S. adults experience PTSD in their lifetime.3
Evidence-based psychotherapy is regarded as the first-line of treatment for PTSD.4 Per a recent meta-analysis conducted within the Agency for Healthcare Research and Quality, psychotherapeutic approaches with a moderate or greater strength of evidence in treating PTSD include exposure-based therapy, such as prolonged exposure (PE), cognitive processing therapy (CPT), cognitive therapy, cognitive behavioral therapy-mixed therapies, eye movement desensitization and reprocessing (EMDR), interpersonal therapy (IPT) and narrative exposure therapy.5 Pharmacological treatments with a moderate evidence-base for treating symptoms of PTSD include the selective serotonin reuptake inhibitors (SSRIs) fluoxetine, paroxetine, and sertraline, the serotonin norepinephrine reuptake inhibitor (SNRI) venlafaxine, and the anticonvulsant topiramate.5 The antihypertensive Prazosin has additionally shown efficacy in treating the nightmares and sleep disturbances that can accompany PTSD.6 The atypical antipsychotic risperidone has a low evidence-base for treating symptoms of PTSD,5 although risperidone may be potentially efficacious for addressing comorbid depressive symptoms.7 However, due to potential serious side effects, atypical antipsychotics are not recommended as first-line treatments.7
Despite the evidence-base for effective treatments for PTSD, many individuals with PTSD do not received adequate care.8 The majority of past research evaluating utilization of mental health treatment by patients diagnosed with PTSD has been conducted within the Veterans Affairs (VA) Healthcare System. In a study of 482 VA patients with a diagnosis of PTSD, Rosen et al. found that 58% of patients had initiated psychotherapy within the year following diagnosis, and, of those who initiated treatment, only 33.3% completed 8 or more visits.9 Additionally, in a study of 186,240 VA patients with PTSD, Cohen et al. found that 80.1% had been prescribed a psychiatric medication.10 A handful of studies, mostly conducted among veterans, have additionally evaluated predictors of treatment utilization among those diagnosed with PTSD, finding lower treatment utilization among both Latinos and African Americans as compared to non-Latino whites,11, 12 among those who were married or divorced/separated/widowed,11 those who were older,10, 13, 14 and those without a mental health comorbidity.11, 15, 16
Little research has evaluated the normal course of care for individuals diagnosed with PTSD in general hospital settings outside of the VA, where patient populations likely differ with respect to demographics, access to mental health care and trauma history. Additionally, little research has evaluated whether certain groups may be more or less likely to receive treatment for PTSD after initial diagnosis. To address this gap in the literature, we conducted a retrospective analysis of a longitudinal electronic medical record for all patients with recently diagnosed primary PTSD.
Methods
Our target study population included patients attending Massachusetts General Hospital (MGH), a major academic medical center within the Partners Healthcare System, who were recently diagnosed with primary PTSD between January 1st, 2002 and June 30th, 2011. We chose to limit follow up through 2011 to ensure that all patients were diagnosed and treated under the same diagnostic criteria (Diagnostic and Statistical Manual IV [DSM-IV]). To obtain information on these patients, we queried the Research Patient Data Registry (RPDR), a longitudinal electronic medical record including information from all patients receiving care at Partners Healthcare sites. We requested information on patients with either a primary or secondary diagnosis of PTSD and a visit for any reason at MGH between January 1st, 2000 and December 31st, 2011 (n=24,417). Information on patient demographics, diagnoses, procedures and medications were merged using the unique identifier assigned to each patient. Patients were excluded if they: 1) had a primary or secondary diagnosis of PTSD in the 2 years prior to their index diagnosis, 2) were less than 18 years old at the index diagnosis, 3) had a diagnosis of a serious mental illness (SMI) (i.e., schizophrenia, psychosis or bipolar disorder) or dementia in the two years prior to or six months following the index diagnosis, or 4) received inpatient psychotherapy in the six months following the index diagnosis. Patients were not excluded if they had received either psychotherapy or psychiatric medications in the 2 years prior to their PTSD diagnosis. This project received approval by the Partners Healthcare Institutional Review Board.
Recent Diagnosis of Primary PTSD
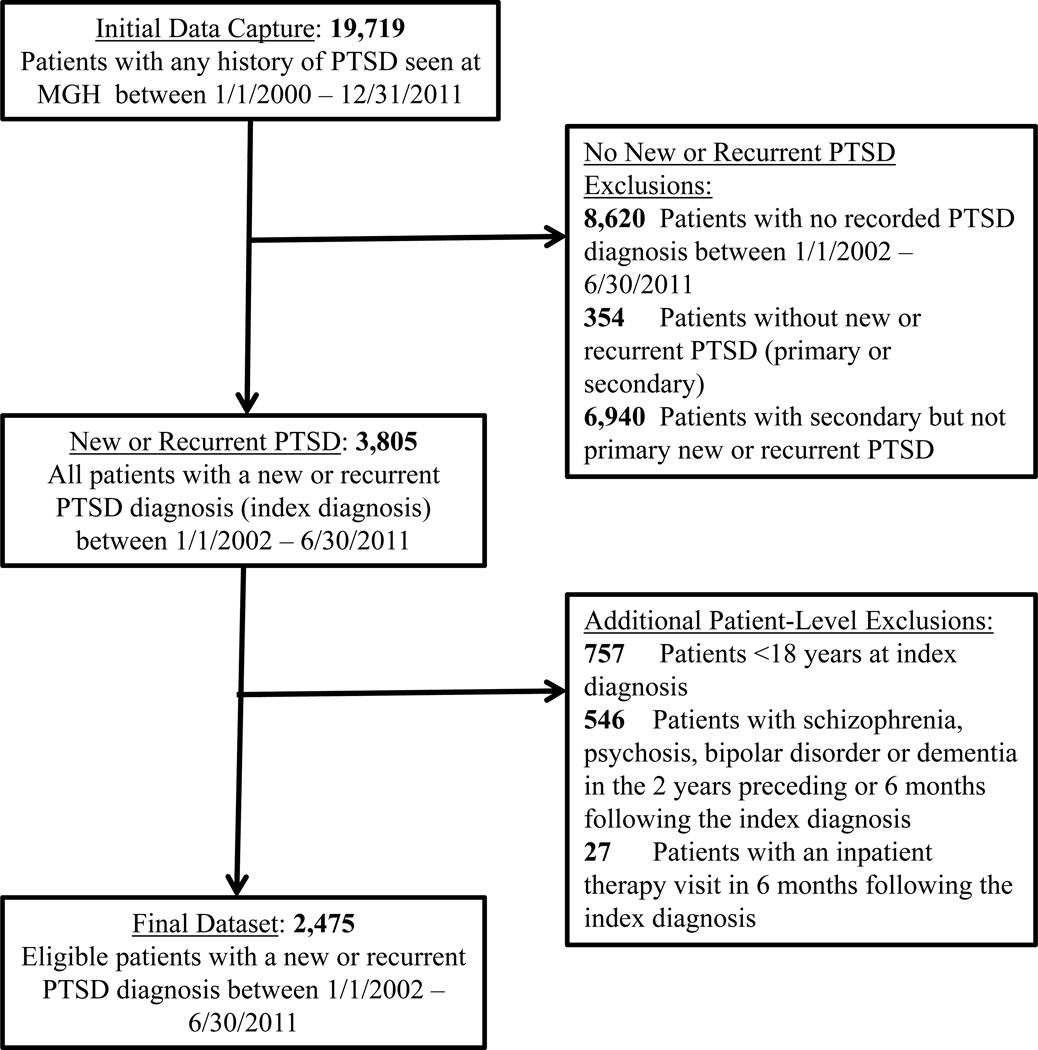
Having a recent diagnosis of primary PTSD was defined as having a primary diagnosis of PTSD (DSM-IV diagnosis code 309.81) with no primary or secondary diagnosis of PTSD in the 2 years preceding the index diagnosis. Diagnoses were based on clinical judgment. For patients presenting with more than one time period with a recent diagnosis PTSD diagnosis (n=115 with 2 and n=4 with 3 recent PTSD diagnoses), we included data only for their first diagnosis. After excluding patients who had no recorded PTSD diagnosis between January 1, 2002 and June 30, 2011 (n = 13,318), patients without recently diagnosed PTSD (n =354), and patients who had newly diagnosed secondary but not primary PTSD (n=6,940), our initial sample size was 3,805 (Figure 1).
Figure 1.
Flow chart for selecting eligible patients with new or recurrent posttraumatic stress disorder between January 1, 2002 and June 30, 2011
Treatment utilization
To evaluate treatment utilization, we captured data on psychotherapy visits and psychiatric prescriptions for medications commonly used to treat PTSD within a 6-month window following the date of primary PTSD diagnosis. We captured psychotherapy visits using current procedural terminology (CPT) codes, and calculated the proportion of patients receiving any psychotherapy visit and receiving 12 or more psychotherapy visits. Information on type of therapy received was not available in the electronic medical record. Receiving 12 sessions of treatment was chosen as a proxy for receiving a full course of prolonged exposure therapy (8–15 90-minute weekly therapy sessions)4 or cognitive processing therapy (12 or more 90-minute weekly sessions).17
We captured data on psychiatric prescriptions by searching for both generic and brand medication names. We calculated the proportion of patients receiving any psychiatric prescription and receiving a prescription for medications of select classes (SSRIs, tricyclic antidepressants, SNRIs, serotonin antagonist and reuptake inhibitors [SARIs], benzodiazepines, non-benzodiazepine hypnotics, atypical antipsychotics, mirtazapine and prazosin).10 We lacked data on whether patients filled or regularly took prescribed prescriptions, however, and our data therefore reflect provider prescribing behavior rather than treatment received by patients. To evaluate the impact of past therapy and medication use on current treatment for recently diagnosed PTSD, we calculated proportion of participants with any therapy visit and any psychiatric prescription in the 2 years prior to the index diagnosis.
Comorbid Mental Health Conditions
We evaluated the presence of comorbid mood or anxiety conditions in the 6 months following the primary PTSD diagnosis using DSM-IV diagnostic codes.18
Predictors of Treatment Utilization
To evaluate factors that may predict patterns of treatment for PTSD, we captured information on patient age (18–34, 35–64, 65+ years), sex, race/ethnicity (Latino, non-Latino black, non-Latino white, non-Latino Asian, other race/ethnicities), primary language (English, Spanish, other language), partner status (partnered, single, separated/divorced/widowed), veteran status, and insurance status (private insurance, Medicare, Medicaid, no insurance). Insurance status was selected as the insurance billed closest to the date of the index diagnosis.
Analysis
Descriptive statistics were calculated using frequencies and percents or means and standard deviations. Differences in distribution of demographic factors by treatment utilization were assessed using Pearson’s chi-square test. To assess demographic predictors of treatment utilization, we evaluated six types of treatment utilization: 1) receiving any psychiatric prescription, 2) receiving an SSRI, 3) receiving an atypical antipsychotic, 4) having at least one therapy visit, 5) having at least 12 therapy visits, and 6) both receiving a psychiatric prescription and having at least one therapy visit. Relative risk of treatment utilization for each predictor was calculated using log-binomial regression, or modified Poisson regression where log-binomial regression failed to converge. All regression models were adjusted for any psychiatric prescription in the 2 years prior to diagnosis, any therapy visit in the 2 years prior to diagnosis and current mood or anxiety comorbidity. We conducted a secondary analysis evaluating predictors of having at least 8 therapy visits, to assess whether predictors were robust to potential misclassification of the number of visits representing a full course of treatment. We additionally evaluated a joint model adjusting for both race/ethnicity and language as predictors of treatment utilization. Analyses were performed in STATA version 14 (StataCorp. 2015).
In our evaluation of demographic predictors of treatment utilization, we chose to not adjust for multiple comparisons, due to the exploratory nature of this analysis and the inflation of type II error for each individual predictor with adjustment for multiple comparisons.19 However, to facilitate evaluation of the potential for inflation of type I error in our overall set of predictors, all predictors were chosen a priori and are presented in table 3.
Table 3.
Risk of treatment type by predictor, adjusted for past use of medication, past use of therapy and current comorbid mood or anxiety condition
| Risk of any medication |
Risk of SSRI | Risk of atypical antipsychotic |
Risk of psychotherapy |
Risk of 12 sessions of psychotherapy |
Risk of both medication and psychotherapy |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RR | 95% CL | RR | 95% CL | RR | 95% CL | RR | 95% CL | RR | 95% CL | RR | 95% CL | |
| Race/ethnicity | ||||||||||||
| Non-Latino white | ref | ref | ref | ref | ref | ref | ||||||
| Non-Latino black | 0.94 | (0.82, 1.09) | 1.02 | (0.82, 1.27) | 0.96 | (0.64, 1.45) | 1.02 | (0.89, 1.17) | 1.01 | (0.66, 1.54) | 0.94 | (0.74, 1.20) |
| Latino | 0.98 | (0.88, 1.08) | 1.25 | (1.09, 1.43) | 1.35 | (1.05, 1.75) | 1.28 | (1.19, 1.38) | 0.75 | (0.54, 1.03) | 1.14 | (0.99, 1.31) |
| Asian | 1.01 | (0.82, 1.25) | 1.05 | (0.77, 1.46) | 0.96 | (0.54, 1.72) | 1.06 | (0.88, 1.28) | 0.94 | (0.49, 1.80) | 0.96 | (0.70, 1.32) |
| Other race/ethnicity | 0.86 | (0.71, 1.03) | 1.04 | (0.81, 1.33) | 0.80 | (0.46, 1.41) | 1.08 | (0.93, 1.24) | 0.78 | (0.44, 1.37) | 1.00 | (0.77, 1.30) |
| Missing | 0.82 | (0.60, 1.11) | 0.76 | (0.47, 1.23) | 0.59 | (0.23, 1.51) | 0.99 | (0.78, 1.26) | 1.05 | (0.50, 2.23) | 0.61 | (0.35, 1.06) |
| Language | ||||||||||||
| English speaking | ref | ref | ref | ref | ref | ref | ||||||
| Spanish speaking | 1.01 | (0.90, 1.12) | 1.35 | (1.16, 1.56) | 1.17 | (0.86, 1.60) | 1.24 | (1.15, 1.34) | 0.60 | (0.41, 0.89) | 1.17 | (1.01, 1.37) |
| Other language | 1.21 | (1.06, 1.38) | 1.50 | (1.24, 1.80) | 1.13 | (0.73, 1.77) | 0.89 | (0.74, 1.08) | 0.33 | (0.13, 0.88) | 1.23 | (0.99, 1.54) |
| Missing | 0.80 | (0.53, 1.21) | 1.11 | (0.68, 1.81) | 1.11 | (0.46, 2.71) | 0.86 | (0.60, 1.24) | 1.54 | (0.74, 3.20) | 0.77 | (0.41, 1.46) |
| Age | ||||||||||||
| 18–34 | ref | ref | ref | ref | ref | ref | ||||||
| 35–64 | 1.07 | (1.00, 1.14) | 1.07 | (0.95, 1.20) | 1.24 | (0.99, 1.56) | 0.87 | (0.81, 0.93) | 1.01 | (0.80, 1.29) | 0.96 | (0.86, 1.07) |
| 65+ | 1.09 | (0.93, 1.28) | 0.88 | (0.61, 1.26) | 0.51 | (0.19, 1.33) | 0.73 | (0.56, 0.94) | 1.29 | (0.67, 2.48) | 0.77 | (0.50, 1.17) |
| Sex | ||||||||||||
| Female | 0.96 | (0.90, 1.02) | 0.99 | (0.88, 1.11) | 0.51 | (0.42, 0.63) | 1.07 | (1.00, 1.16) | 0.90 | (0.70, 1.14) | 0.96 | (0.85, 1.09) |
| Male | ref | ref | ref | ref | ref | ref | ||||||
| Partner Status | ||||||||||||
| Single | 0.97 | (0.91, 1.05) | 0.96 | (0.85, 1.08) | 1.13 | (0.89, 1.45) | 1.04 | (0.97, 1.12) | 0.90 | (0.70, 1.17) | 1.01 | (0.89, 1.13) |
| Separated/divorced widowed |
1.04 | (0.96, 1.13) | 1.09 | (0.94, 1.26) | 1.29 | (0.94, 1.76) | 0.93 | (0.83, 1.04) | 1.10 | (0.78, 1.54) | 0.99 | (0.84, 1.16) |
| Partnered | ref | ref | ref | ref | ref | ref | ||||||
| Missing | 9.97 | (0.79, 1.18) | 0.97 | (0.69, 1.37) | 1.33 | (0.74, 2.41) | 0.71 | (0.54, 0.93) | 1.15 | (0.59, 2.24) | 0.78 | (0.49, 1.23) |
| Veteran | ||||||||||||
| Yes | 1.27 | (1.13, 1.44) | 1.18 | (0.97, 1.43) | 1.00 | (0.69, 1.45) | 1.12 | (1.00, 1.25) | 1.30 | (0.89, 1.90) | 1.54 | (1.28, 1.85) |
| No | ref | ref | ref | ref | ref | ref | ||||||
| Missing | 0.88 | (0.73, 1.05) | 0.65 | (0.47, 0.89) | 1.01 | (0.66, 1.55) | 0.81 | (0.69, 0.94) | 1.13 | (0.73, 1.75) | 0.73 | (0.54, 1.00) |
| Insurance | ||||||||||||
| Private | ref | ref | ref | ref | ref | ref | ||||||
| Medicaid | 1.03 | (0.93, 1.13) | 1.07 | (0.91, 1.24) | 1.16 | (0.88, 1.53) | 0.96 | (0.88, 1.06) | 0.65 | (0.46, 0.92) | 0.91 | (0.76, 1.08) |
| Medicare | 1.06 | (0.95, 1.17) | 0.97 | (0.80, 1.18) | 1.29 | (0.94, 1.78) | 0.77 | (0.67, 0.88) | 0.80 | (0.54, 1.18) | 0.97 | (0.79, 1.19) |
| No insurance | 1.08 | (0.96, 1.22) | 1.01 | (0.81, 1.26) | 1.43 | (1.02, 2.02) | 1.09 | (0.97, 1.22) | 0.87 | (0.57, 1.35) | 1.33 | (1.10, 1.61) |
| Missing | 0.66 | (0.55, 0.79) | 0.46 | (0.36, 0.59) | 0.25 | (0.14, 0.44) | 0.75 | (0.67, 0.84) | 0.45 | (0.30, 0.69) | 0.50 | (0.40, 0.64) |
Results
A total of 3,805 patients had recently diagnosed PTSD between January 1, 2002 and June 30, 2011. After excluding patients less than 18 years old at their index diagnosis (n=757), with a diagnosis of schizophrenia, psychosis, bipolar disorder or dementia in the 2 years preceding or 6 months following their index diagnosis (n=546) or with an inpatient therapy visit in the 6 months following their index diagnosis (n=27), our final dataset included 2,475 patients.
The majority of patients were non-Latino white (67.0%), with 16.4% being Latino, 8.4% non-Latino black, 3.6% Asian and 4.6% another race/ethnicity (Table 1). Only 12.3% reported Spanish as their primary language and 4.9% reported another primary language. Mean age was 39.3 (SD 13.0) years. The majority were female (63.2%) and single (51.1%) or divorced/separated/widowed (14.3%). Veterans made up 13.8% of patients. At the time of the index diagnosis, 54.6% of patients were reimbursed through private insurance, 22.5% through Medicaid, 13.3% through Medicare and 9.5% had no insurance.
Table 1.
Characteristics of patients with new or recurrent posttraumatic stress disorder between January 1, 2002 and June 30, 2011
| Patients with new or recurrent primary PTSD (n=2475) |
Comorbidities |
||||||
|---|---|---|---|---|---|---|---|
| Patients with PTSD only (n=984) |
Patients with comorbid mood or anxiety condition (n=1491) |
||||||
| n | % | n | % | n | % | P | |
| Demographics | |||||||
| Race/ethnicity | |||||||
| Non-Latino white | 1613 | 67.0 | 659 | 69.4 | 954 | 65.4 | 0.09 |
| Non-Latino black | 202 | 8.4 | 82 | 8.6 | 120 | 8.2 | |
| Latino | 395 | 16.4 | 133 | 14.0 | 262 | 18.0 | |
| Asian | 87 | 3.6 | 37 | 3.9 | 50 | 3.4 | |
| Other race/ethnicity | 111 | 4.6 | 39 | 4.1 | 72 | 4.9 | |
| Language | |||||||
| English speaking | 2023 | 82.8 | 823 | 84.7 | 1200 | 81.6 | 0.13 |
| Spanish speaking | 301 | 12.3 | 105 | 10.8 | 196 | 13.3 | |
| Another language | 119 | 4.9 | 44 | 4.5 | 75 | 5.1 | |
| Age (years) | |||||||
| 18–34 | 1060 | 42.8 | 444 | 45.1 | 616 | 41.3 | 0.17 |
| 35–64 | 1349 | 54.5 | 516 | 52.4 | 833 | 55.9 | |
| 65+ | 66 | 2.7 | 24 | 2.4 | 42 | 2.8 | |
| Sex | |||||||
| Female | 1563 | 63.2 | 558 | 56.7 | 1005 | 67.4 | <0.001 |
| Male | 912 | 36.9 | 426 | 43.3 | 486 | 32.6 | |
| Partner Status | |||||||
| Single | 1222 | 51.1 | 475 | 50.4 | 747 | 51.6 | 0.41 |
| Partnered | 827 | 34.6 | 340 | 36.1 | 487 | 33.6 | |
| Separated/divorced/ widowed |
343 | 14.3 | 128 | 13.6 | 215 | 14.8 | |
| Veteran | |||||||
| Yes | 313 | 13.8 | 154 | 17.6 | 159 | 11.4 | <0.001 |
| No | 1954 | 86.2 | 722 | 82.4 | 1232 | 88.6 | |
| Insurance | |||||||
| Private | 1118 | 54.6 | 454 | 60.9 | 664 | 51.0 | <0.001 |
| Medicaid | 460 | 22.5 | 151 | 20.3 | 309 | 23.8 | |
| Medicare | 273 | 13.3 | 89 | 12.0 | 184 | 14.1 | |
| No insurance | 195 | 9.5 | 51 | 6.9 | 144 | 11.1 | |
|
Treatment utilization in previous 2 years |
|||||||
| None | 1165 | 47.1 | 556 | 56.5 | 609 | 40.9 | <0.001 |
| Therapy | 237 | 9.6 | 100 | 10.2 | 137 | 9.2 | |
| Medication | 717 | 29.0 | 262 | 26.6 | 455 | 30.5 | |
| Both therapy and | |||||||
| medication | 356 | 14.4 | 66 | 6.7 | 290 | 19.5 | |
In total, 1,491 patients (60.2%) had a comorbid mood or anxiety disorder diagnosis in the 6 months following their index diagnosis. Having PTSD without a mood or anxiety comorbidity was more common for males, veterans and those with private health insurance. The majority had a therapy visit or a psychiatric prescription in the 2 years preceding PTSD diagnosis (9.6% therapy alone, 29.0% prescription alone, 14.4% both therapy and prescription).
Course of treatment for PTSD
Over half (55.7%) of patients had at least one therapy visit within the 6 months following their PTSD diagnosis. Only 10.0% had 12 or more therapy visits (Table 2). Patients with a mood or anxiety comorbidity were more likely to have at least one therapy visit (61.4%) and 12 or more therapy visits (13.4%) than those with PTSD alone (47.1% and 4.8%, respectively).
Table 2.
Treatment utilization in the 6 months following new or recurrent posttraumatic stress disorder diagnosis
| Total (n=2,475) |
Mood or anxiety comorbidity |
||||||
|---|---|---|---|---|---|---|---|
| Yes (n=1491) |
No (n=984) |
||||||
| n | % | n | % | n | % | P | |
| Medication | |||||||
| Any medication | 1164 | 47.0 | 916 | 61.4 | 248 | 25.2 | <0.001 |
| Selective serotonin reuptake inhibitor (SSRI) |
726 | 29.3 | 614 | 41.2 | 112 | 11.4 | <0.001 |
| Tricyclic antidepressant | 124 | 5.0 | 98 | 6.6 | 26 | 2.6 | <0.001 |
| Serotonin norepinephrine reuptake inhibitor (SNRI) |
119 | 4.8 | 100 | 6.7 | 19 | 1.9 | <0.001 |
| Serotonin antagonist and reuptake inhibitor (SARI) |
237 | 9.6 | 203 | 13.6 | 34 | 3.5 | <0.001 |
| Benzodiazepine | 605 | 24.4 | 490 | 32.9 | 115 | 11.7 | <0.001 |
| Non-benzodiazepine hypnotic |
111 | 4.5 | 80 | 5.4 | 31 | 3.2 | 0.01 |
| Atypical antipsychotic | 291 | 11.8 | 243 | 16.3 | 48 | 4.9 | <0.001 |
| Mirtazapine | 94 | 3.8 | 83 | 5.6 | 11 | 1.2 | <0.001 |
| Prazosin | 65 | 2.6 | 51 | 3.4 | 14 | 1.4 | 0.002 |
| Therapy | |||||||
| At least 1 visit | 1378 | 55.7 | 915 | 61.4 | 463 | 47.1 | <0.001 |
| At least 12 visits | 247 | 10.0 | 200 | 13.4 | 47 | 4.8 | <0.001 |
| Medication and therapy | |||||||
| Neither medication nor therapy |
627 | 25.3 | 252 | 16.9 | 375 | 38.1 | <0.001 |
| Only therapy | 684 | 27.6 | 323 | 21.7 | 361 | 36.7 | |
| Only medication | 470 | 19.0 | 324 | 21.7 | 146 | 14.8 | |
| Both medication and therapy |
694 | 28.0 | 592 | 39.7 | 102 | 10.4 | |
Almost half (47.0%) of patients received a prescription for a medication commonly used to treat PTSD within 6 months of their index diagnosis. The most commonly prescribed medication classes were SSRIs (29.3%), benzodiazepines (24.4%), atypical antipsychotics (11.8%) and SARIs (9.6%). Patients with a mood or anxiety comorbidity were more likely to be prescribed medication (61.4% versus 25.2% for those with PTSD alone). Atypical antipsychotics were prescribed to 16.3% of those with a mood or anxiety comorbidity, and 4.9% of those with PTSD alone.
Overall, one-quarter of patients (28.0%) did not receive treatment, 19.0% had medication alone, 27.6% therapy alone, and 25.3% both therapy and medication. Compared to patients with a mood or anxiety comorbidity, patients with PTSD alone were more likely to not have treatment (38.1% v. 16.9%) or to have therapy alone (36.7% v. 12.7%), and less likely to have medication alone (14.8% v. 21.7%) and have both therapy and medication (10.4% versus 39.7%).
Predictors of treatment utilization
Table 3 describes risk of treatment type by demographic predictors, adjusted for past 2 year ever medication use, past 2 year ever therapy use, and current mood or anxiety comorbidity. Compared to non-Latino whites, Latinos had a 25% greater likelihood of SSRI prescription, a 35% greater likelihood of atypical antipsychotic prescription and a 28% greater likelihood of at least one therapy visit.
We observed a similar trend for Spanish-speaking patients, who had a 35% greater likelihood of SSRI prescription, a 24% greater likelihood of at least one therapy visit, and a 17% greater likelihood of both at least one therapy visit and psychiatric prescription compared to English speakers. However, Spanish-speaking patients had a 40% lower likelihood of having at least 12 therapy visits. Patients with a primary language other than English or Spanish had a 21% greater likelihood of psychiatric prescription, a 50% greater likelihood of SSRI prescription and a 67% lower likelihood of 12 or more therapy visits.
Women had a 50% lower likelihood of atypical antipsychotic prescription than men. We did not observe any other significant differences by gender. Veterans had a 27% greater likelihood of psychiatric prescription and a 54% greater likelihood of both at least one therapy visit and psychiatric prescription than non-veterans. We did not observe any significant differences in treatment utilization by age or partner status.
Compared to those with private insurance, those with Medicaid had a 35% lower likelihood of at least 12 therapy visits. Compared to those with private insurance, those with Medicare had a 23% lower likelihood of at least one therapy visit and those with no insurance had a 43% greater likelihood of atypical antipsychotic prescription and a 33% greater likelihood of both at least one therapy visit and psychiatric prescription.
In a secondary analysis, we evaluated predictors of receiving 8 or more therapy sessions, to account for the potential variability in the number of sessions representing a full course of care. We found that having Medicaid as compared to private insurance remained associated with a lower likelihood of receiving a full course of care using 8 or more sessions (RR 0.76, 95% CI 0.61, 0.96). However, primarily speaking Spanish or another language as compared to primarily speaking English was no longer significantly associated with a lower likelihood of a full course of care (RR 0.86, 95% CI 0.67, 1.10 for Spanish language and RR 0.88, 95% CI 0.57, 1.36 for other language). To evaluate the potential overlap of race/ethnicity and language as predictors of treatment utilization, we ran models adjusting for both race/ethnicity and language. We found that the association between Latino versus non-Latino white ethnicity and SSRI prescription was attenuated (RR 1.14, 95% CI 0.94, 1.39) as were the associations between being Spanish speaking versus English speaking and at least one psychotherapy visit (RR 1.10, 95% CI 0.99, 1.23) and 12 or more psychotherapy visits (RR 0.63, 95% CI 0.38, 1.04).
Discussion
In this study of the usual course of treatment for patients with recently diagnosed PTSD at a major academic medical center, slightly over half of patients had any psychotherapy and slightly less than half had a prescription for a medication commonly used to treat PTSD. However, only one in ten had 12 or more therapy visits, approximately one in ten had a prescription for an atypical antipsychotic, and almost one-quarter had a prescription for a benzodiazepine. Being Latino and Spanish-speaking were associated with SSRI prescription and initial engagement in therapy, although those who were Spanish-speaking were less likely to have 12 or more therapy visits. Latinos and men were more likely to be prescribed an atypical antipsychotic. Reimbursement through Medicaid and Medicare was associated with lower engagement in therapy.
We found that roughly half (47%) of patients received a prescription for a medication commonly used to treat PTSD. This proportion is lower than that found in Cohen et al., where 80% of 186,460 Iraq and Afghanistan veterans with PTSD without a comorbid SMI received prescriptions.10 The lower rate found in our study may represent differences in trauma exposure and severity of symptoms between patient populations, but also may represent differences in beliefs about treatment efficacy on the part of both patients and providers. Almost a quarter (24.4%) of patients were prescribed a benzodiazepine, including 11.7% of patients without a comorbid mood or anxiety disorder. This proportion is strikingly high given that the VA has recommended caution in prescribing benzodiazepines for patients with PTSD20 based on a lack of evidence of their effectiveness for treating PTSD and concern over side-effects in patients with PTSD.21 The high proportion of patients prescribed benzodiazepines may suggest a disconnect between clinical best practices and clinical care as implemented, wherein providers and patients weigh a multitude of factors in deciding on therapeutic approaches.
Atypical antipsychotics were prescribed to 11.8% of patients, most commonly those with a mood or anxiety comorbidity. In comparison, Cohen et al. found that 18.9% of Iraq and Afghanistan Veterans with PTSD were prescribed an antipsychotic.10 Given the side-effects associated with atypical antipsychotics,7 and that Latinos and men were more likely to be prescribed atypical antipsychotics, prescribing patterns of atypical antipsychotics for PTSD warrant further investigation. Further research is needed to determine whether differential prescription practices for Latino patients are related to objective differences in symptom presentation (i.e., severity), or if these differences conform to previous research documenting the underutilization of cultural case formulation with diverse patients and some providers’ tendency to over-pathologize ethnic minority patients.22–24
While slightly more than half of patients had at least one therapy visit (55.7%), only 10.0% had 12 or more therapy visits, a length of treatment roughly associated with receipt of evidence-based care for PTSD.4, 17 Among 482 patients in the VA healthcare system, Rosen et al. found that only 58% of patients initiated therapy for PTSD, and that two-thirds of initiators dropped out before completing 8 sessions.9 Along with findings from Rosen et al., results from this study suggest a potential difficulty with not only engaging patients in therapy for PTSD, but also with retaining patients in treatment through a window representing a full course of evidence-based care.4, 17 While many patient-level factors, such as beliefs about efficacy of treatment, may underlie lack of receipt of a complete course of care, clinical sites are an ideal location in which to evaluate and implement strategies to promote engagement and retention in psychotherapy among those with PTSD. However, given the variability in length of course of treatment for PTSD, and the potential for remission of symptoms well before 12 sessions of care, not all patients who received fewer than 12 sessions of care in this study will have received “inadequate” care.
We found that Latinos and Spanish-speaking patients were more likely to receive prescriptions for SSRIs and have at least one therapy visit. Spanish-speaking patients were additionally less likely to have 12 or more therapy visits. These findings are similar to those from a study in the VA healthcare system of 2,183 patients with PTSD by Hebenstreit et al., which found Latino ethnicity to be negatively associated with receiving minimally adequate care for PTSD.11 This finding is also consistent with several studies that have found high rates of therapy dropout among racial and ethnic minority patients compared to non-Latino white patients.25, 26 Structural barriers, including language barriers, patient-provider cultural differences, including the importance of family and religious ties,27 and social inequities likely play a role in lower access to a full course of evidence-based mental health treatment.28–30 Additionally, research suggests that beliefs about the efficacy of mental health treatment may be a mediator of the association between Latino ethnicity and receipt of therapy for PTSD.12
We observed that men were twice as likely to be prescribed atypical antipsychotics as women. Similarly, Cohen et al. found that male Iraq and Afghanistan veterans were 25% more likely to be prescribed an antipsychotic than female veterans.10 This gender difference may be socially mediated, and arise due to differences in the presentation of PTSD symptoms by gender.31 We additionally found that those receiving Medicare were less likely to have at least one therapy visit, and those receiving Medicaid were less likely to have 12 or more therapy visits, which may reflect both structural barriers to receiving mental health care, including a lower reimbursement rate for care and Medicare and Medicaid plans being exempt from complying with mental health parity laws, and differences in population characteristics for those receiving public insurance.
Our study is unique in evaluating the regular course of treatment for patients with recently diagnosed PTSD in a large hospital serving the general public, and extends previous findings among veterans to the general population. However, there are key considerations to take into account in the interpretation of our findings. First, our study population only includes those receiving a diagnosis of primary PTSD, and therefore does not reflect treatment utilization and its predictors among individuals with PTSD who did not both access the health care system and receive a diagnosis. Second, we lacked information on type of therapy received, and therefore our estimates of receiving a full course of treatment (12 or more sessions) is only a proxy for receipt of a full course of evidence-based care. Additionally, we could not adequately capture type of provider seen, which limited our ability to evaluate whether patients diagnosed by mental health specialists were more likely to receive evidence-based treatment that those diagnosed by general medical providers. It is also possible that patients may have enrolled in research studies after diagnosis with PTSD, and therefore may not have information on treatment recorded in their medical record, however we believe this would not affect most patients in the time frame of the study. Third, we lacked data on severity of PTSD and its comorbidities, and changes in symptom severity over time. This limited our ability to evaluate PTSD severity as a predictor of utilization and to make any assessment of effectiveness of treatment. Fourth, we were only able to capture data on prescriptions, and not on the number of prescriptions filled or the number of patients who took a medication consistently. Therefore, our findings for medications only reflect provider prescribing behavior. Fifth, we were only able to evaluate treatment received following a “recent diagnosis” of PTSD, which likely does not capture the complex trajectory of symptoms experienced by many patients, who may delay treatment or have received treatment for a prior PTSD diagnosis more than 2 years prior to the diagnosis captured here. As patients’ exposure to trauma may have occurred from weeks to decades before the “recent” PTSD diagnosis was captured, it is also likely that there was variability in the types of treatment received based on time since trauma exposure that we were unable to evaluate. Finally, because we evaluated multiple predictors of receiving treatment, our results must be viewed in the light of a higher likelihood of type I error in the overall group of predictors assessed.
Our findings extend those of several studies in the VA healthcare system to an academic medical center setting, suggesting that most patients with PTSD without an SMI do not have an adequate number of therapy visits, more than 10% receive a prescription for an atypical antipsychotic and that several key demographic factors predict receipt of treatment for PTSD. Based on our findings and those of previous studies, addressing poor engagement and retention of patients in therapy for PTSD is an important area for further policy development. Future research is needed to identify the type and effectiveness of treatment received by patients engaging in therapy, as well as barriers to both initiation and retention in evidence-based care that can be addressed at the provider- and systems-levels.
Acknowledgments
The authors thank Shawn N. Murphy, MD PhD and Henry Chueh, MD (Harvard Medical School, Boston MA) and the Partners Health Care Research Patient Data Registry group for facilitating use of their database.
Funding/support: Time for this manuscript was funded in part by a grant from the National Institute of Mental Health (NIMH K23 MH096029-01A1) awarded to Dr. Luana Marques.
Role of the sponsor: The sponsor had no role in the design, analysis, interpretation or publication of this study.
Footnotes
Drs. Murphy and Chueh have no conflicts of interest to declare.
Additional Information: Data was obtained from the Research Patient Data Registry managed by Research Information and Services and Computing at Partners HealthCare (https://rc.partners.org/about/who-we-are-risc/research-patient-data-registry).
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®) American Psychiatric Pub; 2013. [Google Scholar]
- 2.Schnurr PP, Friedman MJ, Bernardy NC. Research on posttraumatic stress disorder: epidemiology, pathophysiology, and assessment. Journal of clinical psychology. 2002 Aug;58(8):877–889. doi: 10.1002/jclp.10064. [DOI] [PubMed] [Google Scholar]
- 3.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of general psychiatry. 2005 Jun;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 4.Difede J, Olden M, Cukor J. Evidence-based treatment of post-traumatic stress disorder. Annual review of medicine. 2014;65:319–332. doi: 10.1146/annurev-med-051812-145438. [DOI] [PubMed] [Google Scholar]
- 5.Jonas DE, Cusack K, Forneris CA, et al. Psychological and Pharmacological Treatments for Adults With Posttraumatic Stress Disorder (PTSD) Rockville (MD): Agency for Healthcare Research and Quality (US); 2013. AHRQ Comparative Effectiveness Reviews. [PubMed] [Google Scholar]
- 6.De Berardis D, Marini S, Serroni N, et al. Targeting the Noradrenergic System in Posttraumatic Stress Disorder: A Systematic Review and Meta-Analysis of Prazosin Trials. Current drug targets. 2015;16(10):1094–1106. doi: 10.2174/1389450116666150506114108. [DOI] [PubMed] [Google Scholar]
- 7.Wright BM, Eiland EH, 3rd, Lorenz R. Augmentation with atypical antipsychotics for depression: a review of evidence-based support from the medical literature. Pharmacotherapy. 2013 Mar;33(3):344–359. doi: 10.1002/phar.1204. [DOI] [PubMed] [Google Scholar]
- 8.Wang PS, Berglund P, Olfson M, Pincus HA, Wells KB, Kessler RC. Failure and delay in initial treatment contact after first onset of mental disorders in the National Comorbidity Survey Replication. Archives of general psychiatry. 2005 Jun;62(6):603–613. doi: 10.1001/archpsyc.62.6.603. [DOI] [PubMed] [Google Scholar]
- 9.Rosen CS, Greenbaum MA, Fitt JE, Laffaye C, Norris VA, Kimerling R. Stigma, help-seeking attitudes, and use of psychotherapy in veterans with diagnoses of posttraumatic stress disorder. The Journal of nervous and mental disease. 2011 Nov;199(11):879–885. doi: 10.1097/NMD.0b013e3182349ea5. [DOI] [PubMed] [Google Scholar]
- 10.Cohen BE, Shi Y, Neylan TC, Maguen S, Seal KH. Antipsychotic prescriptions in Iraq and Afghanistan veterans with posttraumatic stress disorder in Department of Veterans Affairs healthcare, 2007–2012. The Journal of clinical psychiatry. 2015 Apr;76(4):406–412. doi: 10.4088/JCP.13m08857. [DOI] [PubMed] [Google Scholar]
- 11.Hebenstreit CL, Madden E, Koo KH, Maguen S. Minimally adequate mental health care and latent classes of PTSD symptoms in female Iraq and Afghanistan veterans. Psychiatry research. 2015 Nov 30;230(1):90–95. doi: 10.1016/j.psychres.2015.08.028. [DOI] [PubMed] [Google Scholar]
- 12.Spoont MR, Nelson DB, Murdoch M, et al. Are there racial/ethnic disparities in VA PTSD treatment retention? Depression and anxiety. 2015;32(6):415–425. doi: 10.1002/da.22295. [DOI] [PubMed] [Google Scholar]
- 13.Kehle-Forbes SM, Meis LA, Spoont MR, Polusny MA. Treatment initiation and dropout from prolonged exposure and cognitive processing therapy in a VA outpatient clinic. Psychological trauma : theory, research, practice and policy. 2016;8(1):107–114. doi: 10.1037/tra0000065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Keller SM, Tuerk PW. Evidence-based psychotherapy (EBP) non-initiation among veterans offered an EBP for posttraumatic stress disorder. Psychological services. 2016 Feb;13(1):42–48. doi: 10.1037/ser0000064. [DOI] [PubMed] [Google Scholar]
- 15.Zen AL, Whooley MA, Zhao S, Cohen BE. Post-traumatic stress disorder is associated with poor health behaviors: findings from the heart and soul study. Health psychology : official journal of the Division of Health Psychology, American Psychological Association. 2012 Mar;31(2):194–201. doi: 10.1037/a0025989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smith NB, Cook JM, Pietrzak R, Hoff R, Harpaz-Rotem I. Mental Health Treatment for Older Veterans Newly Diagnosed with PTSD: A National Investigation. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry. 2016 Mar;24(3):201–212. doi: 10.1016/j.jagp.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 17.Resick PA, Schnicke MK. Cognitive processing therapy for sexual assault victims. Journal of consulting and clinical psychology. 1992 Oct;60(5):748–756. doi: 10.1037//0022-006x.60.5.748. [DOI] [PubMed] [Google Scholar]
- 18.Organization APAP. Covered Diagnoses & Crosswalk of DSM-IV Codes to ICD-9-CM Codes. 750 First Street, NE, Washington, DC: 2002. 20002-4242. [Google Scholar]
- 19.Rothman KJ. No adjustments are needed for multiple comparisons. Epidemiology (Cambridge, Mass) 1990 Jan;1(1):43–46. [PubMed] [Google Scholar]
- 20.Department of Veterans Affairs DoD. VA/DoD Clinical Practice Guideline for Management of Post-Traumatic Stress. The Management of Post-Traumatic Stress Working Group. 2010. Version 2.0. [Google Scholar]
- 21.Guina J, Rossetter SR, De RB, Nahhas RW, Welton RS. Benzodiazepines for PTSD: A Systematic Review and Meta-Analysis. J Psychiatr Pract. 2015 Jul;21(4):281–303. doi: 10.1097/PRA.0000000000000091. [DOI] [PubMed] [Google Scholar]
- 22.Adeponle AB, Thombs BD, Groleau D, Jarvis E, Kirmayer LJ. Using the cultural formulation to resolve uncertainty in diagnoses of psychosis among ethnoculturally diverse patients. Psychiatric services (Washington, DC) 2012 Feb 1;63(2):147–153. doi: 10.1176/appi.ps.201100280. [DOI] [PubMed] [Google Scholar]
- 23.Polo AJ, Alegría M, Sirkin JT. Increasing the engagement of Latinos in services through community-derived programs: The Right Question Project-Mental Health. Professional Psychology: Research and Practice. 2012;43(3):208. [Google Scholar]
- 24.Garb HN. Race bias, social class bias, and gender bias in clinical judgment. Clinical Psychology: Science and Practice. 1997;4(2):99–120. [Google Scholar]
- 25.Wierzbicki M, Pekarik G. A meta-analysis of psychotherapy dropout. Professional Psychology: Research and Practice. 1993;24(2):190. [Google Scholar]
- 26.Blanco C, Patel SR, Liu L, et al. National trends in ethnic disparities in mental health care. Medical care. 2007;45(11):1012–1019. doi: 10.1097/MLR.0b013e3180ca95d3. [DOI] [PubMed] [Google Scholar]
- 27.Marques L, Eustis EH, Dixon L, et al. Delivering cognitive processing therapy in a community health setting: The influence of Latino culture and community violence on posttraumatic cognitions. Psychological trauma : theory, research, practice and policy. 2016 Jan;8(1):98–106. doi: 10.1037/tra0000044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Horevitz E, Organista KC, Arean PA. Depression Treatment Uptake in Integrated Primary Care: How a “Warm Handoff” and Other Factors Affect Decision Making by Latinos. Psychiatric services (Washington, DC) 2015 Aug 1;66(8):824–830. doi: 10.1176/appi.ps.201400085. [DOI] [PubMed] [Google Scholar]
- 29.Uebelacker LA, Marootian BA, Pirraglia PA, et al. Barriers and facilitators of treatment for depression in a latino community: a focus group study. Community mental health journal. 2012 Feb;48(1):114–126. doi: 10.1007/s10597-011-9388-7. [DOI] [PubMed] [Google Scholar]
- 30.Bauer AM, Chen CN, Alegria M. English language proficiency and mental health service use among Latino and Asian Americans with mental disorders. Medical care. 2010 Dec;48(12):1097–1104. doi: 10.1097/MLR.0b013e3181f80749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hourani L, Williams J, Bray R, Kandel D. Gender differences in the expression of PTSD symptoms among active duty military personnel. Journal of anxiety disorders. 2015 Jan;29:101–108. doi: 10.1016/j.janxdis.2014.11.007. [DOI] [PubMed] [Google Scholar]