Abstract
OBJECTIVE
To conduct a systematic literature review to determine what telemedicine services are provided by pharmacists and the impact of these services in the nursing facility setting.
DATA SOURCES
MEDLINE®, Scopus®, and Embase® databases.
STUDY SELECTION
The terms “telemedicine” or “telehealth” were combined by “and” with the terms “pharmacist” or “pharmacy” to identify pharmacists’ use of telemedicine. Also, “telepharmacy” was added as a search term. The initial search yielded 322 results. These abstracts were reviewed by two individuals independently, for selection of articles that discussed telemedicine and involvement of a pharmacist, either as the primary user of the service or as part of an interprofessional health care team. Those abstracts discussing the pharmacist service for purpose of dispensing or product preparation were excluded.
DATA EXTRACTION
A description of pharmacists’ services provided and the impact on resident care.
DATA SYNTHESIS
Only three manuscripts met inclusion criteria. One was a narrative proposition of the benefits of using telemedicine by senior care pharmacists. Two published original research studies indirectly assessed the pharmacists’ use of telemedicine in the nursing facility through an anticoagulation program and an osteoporosis management service. Both services demonstrated improvement in patient care.
CONCLUSION
There is a general paucity of practice-related research to demonstrate potential benefits of pharmacists’ services incorporating telemedicine. Telemedicine may be a resource-efficient approach to enhance pharmacist services in the nursing facility and improve resident care.
Keywords: Clinical decision support systems, Clinical pharmacy information systems, Communication, Long-term care, Medication errors, Nursing facility, Patient safety, Pharmacists, Telehealth, Telemedicine
Introduction
Telemedicine is defined as the use of electronic communications, such as two-way video, e-mail, smartphones, or wireless tools to provide clinical care at a distance so that information can be exchanged from one site to another.1,2 The most common way to use telemedicine is a responsive model, primarily physician-led with virtual visits stimulated by alerts using interactive services, which facilitates real-time interaction between the patient and provider.3,4 Telemedicine is used in a variety of health care settings, including the nursing facility, where it is employed to provide wound care, glycemic management, and after-hours physician care, with improved patient outcomes and reduced costs.5–7 The use of telemedicine for timely communication and counseling of patients with chronic conditions demonstrate improvement in patient outcomes inclusive of mortality, quality of life, and reductions in hospital admissions.8 Telemedicine is successfully employed by nursing facilities, but its use is limited to a finite number of patient-care issues, and little is known about how it can support pharmacist services.7
Outside of the nursing facility, pharmacists’ use of telemedicine to aid in the provision of care has shown to be effective. Telemedicine services provided after-hours by pharmacists in three community hospitals without 24-hour pharmacy services resulted in improved drug safety since prescribing accuracy was verified.9 Pharmacist interventions were five times greater for resolving drug-related problems with a telemedicine service compared with not providing telemedicine services. The estimated annual costs avoided were $261,109 per hospital by employing telemedicine services. Nurses’ satisfaction indicated that their level of comfort improved with the medication use process after exposure to pharmacist telemedicine services.
There is a potential to expand the role of pharmacist services using telemedicine in the nursing facility. The Centers for Medicare & Medicaid Services outlines the expectations of the nursing facility consultant pharmacist in the State Operations Manual (Tags F329, F332, F333, F425, F428, and F429). The State Operations Manual requires that: 1) the drug regimen of each resident must be reviewed at least monthly and 2) the pharmacist reports any irregularities, including the presence of adverse drug events (ADEs) to the attending physician.10,11 Unfortunately, retrospective medication regimen reviews (MRRs) conducted every 30 days are not ideal for timely intervention, as the attending provider may not receive timely notification about medication safety issues, including potential ADEs.11 Regulations also indicate that more frequent MRRs are needed, depending on resident’s condition and risk of ADEs. For example, residents receiving high-risk medications such as antidiabetics, anticoagulants, and opioids may require more frequent reviews.11 A single consultant pharmacist provides services for many nursing facilities and typically does not have allocated time to visit more frequently than once every 30 days. Evaluating medication prescribing when residents are at a known risk for ADEs, and correcting prescribing and monitoring of drugs, should help prevent patient harm.12,13 The retrospective 30-day medication review process is shown to be faulty and needs to be improved, especially with the increasing frequency of short-term stays.
Telemedicine has a promising role, to enhance pharmacists’ interactions with residents and nurses within the nursing facility. One potential model is “responsive care,” where telemedicine is prompted by an alert generated from a clinical decision-support system using an interactive service to gain information about possible drug errors or ADEs. Also, pharmacists could find added value in access to asynchronous data provided through telemedicine to aid in their comprehensive MRR.3,4 The purpose of the present review was to conduct a literature search to determine what telemedicine services are provided by pharmacists in the nursing facility and their impact on resident care.
Method
MEDLINE®, Scopus®, and Embase® databases were used to conduct a systematic literature review. Search terms were selected that would identify pharmacists’ use of telemedicine to provide services. The terms “telemedicine” or “telehealth” were combined by “and” with the terms “pharmacist” or “pharmacy”. Also, “telepharmacy” was added as a search term. The initial search of the three databases yielded 322 results. These abstracts were reviewed by two individuals independently (JN, HH) for selection of articles that discussed telemedicine and involvement of a pharmacist, either as the primary user of the service or as part of an interprofessional health care team. Abstracts discussing the pharmacist service for purpose of dispensing or product preparation were excluded. The selected 126 articles were reviewed in full-text form to determine the patient care environment. Three articles were determined to include an evaluation of pharmacist services in the nursing facility.14–16 Article selection by each independent reviewer was discussed before final selections were made. Discrepancies were resolved by consensus. Figure 1 depicts the process for the literature review.
Figure 1.
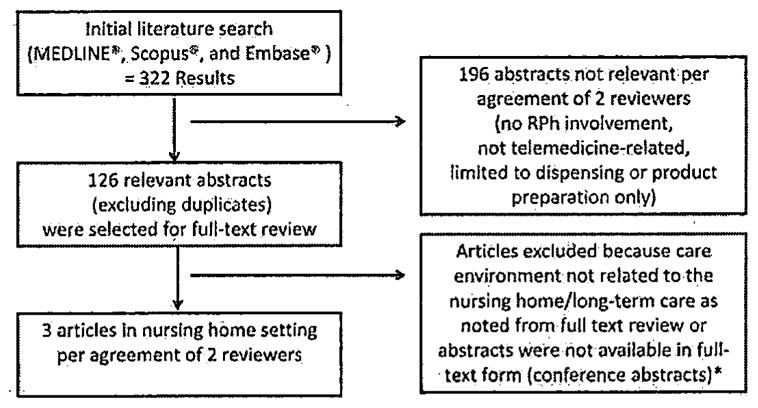
Process for literature review
* Only 1 abstract in the NH environment was unavailable in full text form and it did not discuss telemedicine services.
Results
There are at least 1,500 published articles describing telemedicine, but only 322 potentially discuss pharmacist services and only three address pharmacist services in the nursing facility.8 Of interest, our review indicated that there were substantially more articles that discussed pharmacist-led telemedicine services in the community/ ambulatory (n = 106) and inpatient (n = 19) settings than the nursing facility.
The oldest article that we identified was not a research study, but instead a proposal of the benefit of using telemedicine by senior care pharmacists.14 It highlighted the benefit of telemedicine in long-term care as a way to provide more services, more easily by eliminating travel and travel-related costs. The ability to personalize resident discussions with customized dialogue including patient-specific feedback and to provide proactive MRR was the primary suggested utility for the pharmacists. It was anticipated that use of telemedicine in long-term care could allow for early identification of risk and a quicker response to problems. It has been more than a decade since the idea of using telemedicine for pharmacist services in long-term care has been proposed. Despite potential benefits outlined in this article, the literature on the use of telemedicine in long-term care facilities is still limited to two studies indirectly evaluating pharmacist involvement.
In the first study, clinical pharmacists in Colorado provide a modern anticoagulation service that incorporates a centralized structure (i.e., location) and the use of telemedicine.15 Each pharmacist in the program cared for 150 to 500 patients, with the majority of the residents residing in a nursing facility. The anticoagulation service was prompted by a request from the patient’s physician. The method of communication with patients was telephone and regular mail. The program was evaluated in a retrospective cohort study, and demonstrated that patients were 39% (hazard ratio = 0.61, confidence interval 0.42–0.88) less likely to have a major bleed episode, thromboembolic complication, or fatal event compared with patients managed by physicians with usual care.16
In the second study, a group of pharmacists at Kaiser Permanente in Colorado were employed as decentralized pharmacists who work with primary care providers at medical offices and skilled nursing facilities.17 These pharmacists participated in an osteoporosis management service, caring for postmenopausal women after a fracture. Pharmacists were engaged in care following a monthly report generated by the pharmacy department describing a woman older than 67 years of age who suffered a fracture. They managed bone-mass density monitoring, initiation of osteoporosis therapy, and calcium/vitamin D supplements. Pharmacists communicated with patients via regular mail, telephone, and e-mail. The program resulted in a substantial increase in the provision of osteoporosis therapy compared with a similar nurse-run service.
Discussion
Telemedicine services provided by a pharmacist can improve prescribing and offer potential patient safety and financial benefits, but are limited to settings largely outside of the nursing facility. Pharmacist telemedicine services in the nursing facility have not been directly evaluated, despite an early publication proposing telemedicine as a viable tool to enhance resident care.14 The two published studies indirectly assessed the use of telemedicine in the nursing facility in specific clinical contexts. In fact, they set out to evaluate: 1) telemedicine services for an anticoagulation program; the majority of patients were located in the nursing facility, and 2) telemedicine services of decentralized pharmacists located in primarily primary care clinics (26 full-time equivalents) and skilled nursing facilities (3 full-time equivalents). One I can speculate the reason for not adopting telemedicine in the nursing facility for pharmacist services is the up-front costs associated with buying the telemedicine equipment and training the users; however, the greater vision may be the cost savings from preventing medication errors and ADEs. There is a paucity of literature highlighting possible scenarios appropriate for pharmacists’ use of telemedicine in the nursing facility and a lack of studies and evidence base to support patient-centered outcomes of this service.
Geriatric specialists in medicine encourage training on the use of telemedicine to ensure they are meeting i the needs of contemporary practices and can maximize their outreach.18 Telemedicine can help eliminate distance barriers and improve access to medical services.19,20 Moreover, when coupled with appropriate clinical protocols, treatment variability can be reduced. In a resource-conscious health care environment, providing pharmacist services remotely—but still having personalized interactions via telemedicine to resolve inappropriate prescribing and inadequate monitoring— provides a feasible approach to more frequent MRR. Patient-centered communication builds satisfaction, rapport, trust, understanding, and adherence.21 Telemedicine audiovisual services offer the potential advantage of building better patient rapport over telephonic services by putting a face with the voice.
Consultant pharmacists could expand their roles, fulfill regulatory requirements, and provide more timely care if they were to adopt a responsive-care model that uses telemedicine. Specifically, clinical decision support could be used to generate appropriate alerts to help identify medication errors and possible ADEs in a responsive-care model. This alert could be the impetus for reviewing the resident’s medical records and reaching out for a patient-centered telemedicine communication in an unscheduled manner. After the patient interaction, an enriched form of communication with nursing staff and physicians can take place to clarify medication orders, delineate drug monitoring, and provide pharmacist recommendations for drug management. Recommendations should be provided in a structured communication framework such as the situation, background, assessment, and recommendation to maximize communication.22 The telemedicine model we are proposing transforms the current MRR process and allows for timely access to consultant pharmacists, permitting more frequent interactions between the resident and pharmacist in a resource-efficient manner. Formal evaluation of the proposed model is in progress.23 This federally funded study will evaluate the impact of a pharmacist-led MRR using patient-centered telemedicine for residents receiving high-risk drugs on ADE occurrence and 30-day hospital readmissions.
The general conclusion from the Agency for Healthcare Research and Quality, which summarized telemedicine literature available in systematic reviews, is that there is sufficient evidence on the effectiveness of telemedicine, and future research is needed on implementation and practice-based methods.8 Applying telemedicine to pharmacy services in the nursing facility appears to be the next logical step. Now, implementation evaluations are necessary to understand the benefit in this context. Additionally, a cost-benefit analysis evaluating the provision of telemedicine services by the pharmacist would potentially help to justify costs.
The current state of telemedicine is focused on increasing access to medical services.2,19,20 However, the benefits of telemedicine are shifting and now include an emphasis on reducing health care costs.2 Also, there is an emerging initiative to use telemedicine to manage chronic diseases, not simply follow-up of acute conditions. These notions are in line with using telemedicine to enhance pharmacist services by monitoring drug therapy of chronic conditions to reduce ADEs and use of health care.
Conclusion
Telemedicine use in the nursing facility appears to improve patient outcomes and reduce costs. Pharmacists effectively use telemedicine in other patient care settings. Telemedicine may be a resource-efficient approach to enhance pharmacist services in the nursing facility and improve resident care. Clearly, with the lack of studies in this area, there is a need for an evidence base from practice-related research to demonstrate these potential benefits.
Footnotes
Disclosure: This work was supported in part by grants from AHRQ (R18HS02420) and NIA (Pittsburgh Claude D. Pepper Older Americans Independence Center P30 AG024827; K01 AG044433).
Contributor Information
Sandra L Kane-Gill, Associate professor of pharmacy and critical care medicine, Biomedical Informatics and Clinical Translational Science Institute, University of Pittsburgh, and medication safety pharmacist, University of Pittsburgh Medical Center (UPMC), Pittsburgh, Pennsylvania.
Joshua D. Niznik, PhD candidate, School of Pharmacy, University of Pittsburgh, and staff pharmacist, Magee-Women’s Hospital of UPMC, Pittsburgh.
John A. Kellum, Director, The Center for Critical Care Nephrology. Department of Critical Care Medicine, UPMC, and University of Pittsburgh School of Medicine, CRISMA (Clinical Research, Investigation, and Systems Modeling of Acute Illness) Center, Department of Critical Care Medicine, University of Pittsburgh School of Medicine.
Colleen M. Culley, Associate professor of pharmacy, University of Pittsburgh, and clinical pharmacy specialist, Pharmacy Service Line, UPMC Corporate Services, Pittsburgh.
Richard D. Boyce, Assistant professor of biomedical informatics and clinical translational science, University of Pittsburgh.
Zachary A. Marcum, Assistant professor, School of Pharmacy, University of Washington, Seattle, Washington.
Harvey He, 2017 PharmD candidate, School of Pharmacy, University of Pittsburgh.
Subashan Perera, Associate professor of medicine and biostatistics, Division of Geriatric Medicine, University of Pittsburgh.
Steven M. Handler, Associate professor, Division of Geriatric Medicine, Department of Medicine; Department of Biomedical Informatics and Clinical Translational Science Institute, University of Pittsburgh.
References
- 1.American Telemedicine Association. [Accessed July 7,2016];Core operational guidelines for telehealth services involving provider-patient interactions. Available at http://www.americantelemed.org/resources/telemedicine-practice-guidelines/telemedicine-practice-guidelines/core-operational-guidelines-for-telehealth-services-involving-provider-patient-interactions#.V4e2KItXJGM.
- 2.Dorsey ER, Topol EJ. State of telehealth. N Engl J Med. 2016;375:154–61. doi: 10.1056/NEJMra1601705. [DOI] [PubMed] [Google Scholar]
- 3.McGonigle D, Mastrian K. Nursing informatics and the foundation of knowledge. Jones & Bartlett Publishers; 2014. [Google Scholar]
- 4.American Telemedicine Association. [Accessed July 7, 2016];Guidelines for TelelCU operations. Available at http://www.americantelemed.org/docs/default-source/standards/guidelines-for-teleicu-operations.pdf?sfvrsn=2.
- 5.Stern A, Mitsakakis N, Paulden M, et al. Pressure ulcer multidisciplinary teams via telemedicine: a pragmatic cluster randomized stepped wedge trial in long term care. BMC Health Serv Res. 2014;14:83. doi: 10.1186/1472-6963-14-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grabowski DC, O’Malley AJ. Use of telemedicine can reduce hospitalizations of nursing home residents and generate savings for Medicare. Health Aff (Millwood) 2014;33:244–50. doi: 10.1377/hlthaff.2013.0922. [DOI] [PubMed] [Google Scholar]
- 7.Edirippulige S, Martin-Khan M, Beattie E, et al. A systematic review of telemedicine services for residents in long term care facilities. J Telemed Telecare. 2013;19:127–32. doi: 10.1177/1357633X13483256. [DOI] [PubMed] [Google Scholar]
- 8.Agency for Healthcare Research and Quality. [Accessed July 2, 2016];Telehealth: mapping the evidence for patient outcomes from systematic reviews. Available at https://effectivehealthcare.ahrq.gov/search-for-guides-reviews-and-reports/?pageaction=displayproduct&productid=2254&utm_source=AHRQ&utm_medium=EN-l&utm_term=&utm_content=1&utm_campaign=AHRQ_EN7_12_2016. [PubMed]
- 9.Schneider PJ. Evaluating the impact of telepharmacy. Am J Health Syst Pharm. 2013;70:2130–5. doi: 10.2146/ajhp130138. [DOI] [PubMed] [Google Scholar]
- 10.Martin CM, McSpadden CS. Changes in the state operations manual: implications for consultant pharmacy practice. Consult Pharm. 2006;21:948–61. doi: 10.4140/tcp.n.2006.948. [DOI] [PubMed] [Google Scholar]
- 11.Clark TR. Gap analysis: assessing the value perception of consultant pharmacist services and the performance of consultant pharmacists. Consult Pharm. 2008;23(Suppl C):3–15. [PubMed] [Google Scholar]
- 12.U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. National Action Plan for Adverse Drug Event Prevention. Washington, DC: 2014. Accessed. at: https://health.gov/hcq/ade-action-plan.asp. [Google Scholar]
- 13.Rozich JD, Resar RK. Medication safety: one organization’s approach to the challenge. J Clin Outcomes Manage. 2001;8:27–34. [Google Scholar]
- 14.Kaldy J. Telehealth enables senior care pharmacists to reach beyond facility walls. Consult Pharm. 2005;20:558–67. doi: 10.4140/tcp.n.2005.558. [DOI] [PubMed] [Google Scholar]
- 15.Witt DM. The Kaiser Permanente Colorado clinical pharmacy anticoagulaiton services as a model of modern anticoagulant care. Thromb Res. 2008;123:S36–S41. doi: 10.1016/j.thromres.2008.08.004. [DOI] [PubMed] [Google Scholar]
- 16.Witt DM, Sadler MA, Shanahan RL, et al. Effect of centralized clinical pharmacy anticoagulaton service on the outcomes of anticogulation therapy. CHEST. 2005;127:1515–22. doi: 10.1378/chest.127.5.1515. [DOI] [PubMed] [Google Scholar]
- 17.Heilmann RM, Friesleben CR, Billups SJ. Impact of a pharmacist-directed intervention in postmenopausal women after fracture. Am J Health Syst Pharm. 2012;69:504–9. doi: 10.2146/ajhp110309. [DOI] [PubMed] [Google Scholar]
- 18.Tinnetti M. Mainstream or extinction: can defining who we are save geriatrics? J Am Geriatr Soc. 2016;64:1400–4. doi: 10.1111/jgs.14181. [DOI] [PubMed] [Google Scholar]
- 19.Bashshur RL, Shannon G, Krupinski EA, et al. Sustaining and realizing the promise of telemedicine. Telemed J E Health. 2013;19:339–45. doi: 10.1089/tmj.2012.0282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bashshur RL, Goldberg MA. The origins of e-health. Telemed J E Health. 2014;20:190–1. doi: 10.1089/tmj.2014.9996. [DOI] [PubMed] [Google Scholar]
- 21.Anderson WG. [Accessed July 7, 2016];Patient-centered communications: building patient rapport. Available at http://www.thedoctors.com/knowledgecenter/publications/thedoctorsadvocate/con_id_004410.
- 22.Institute for Healthcare Improvement. [Accessed July 2, 2016];SBAR communication technique. Available at http://www.ihi.org/Topics/SBARCommunicationTechnique?Pages/default.aspx.
- 23.Kane-Gill SL. Transforming the medication regimen review process of high-risk drugs using a patient-centered telemedicine-based approach to prevent adverse drug events in the nursing home. Agency for Healthcare Research and Quality; 2015. [Accessed July 2, 2016]. 1R18HS024208-01. Available at https://projectreporter.nih.gov/project_info_description.cfm?aid=8996873&icde=292039768&ddparam=&ddvalue=&ddsub=&cr=I&csb=default&cs=ASC. [Google Scholar]


