Abstract
Objective
To understand what influences surrogates decision-makers’ expectations that a patient with a disorder of consciousness (DOC), those in a coma, the vegetative state or the minimally conscious state, will recover.
Subjects
41 surrogates representing 37 DOC patients completed a survey about their experiences in having a family member with a DOC.
Methods
A quantitative questionnaire assessed surrogate’s demographic, medical and psychosocial features that may explain their own expectations of patient recovery. Results: Surrogates who were more relationally enmeshed with the patient, thought the patient could communicate better, and thought technology would improve treatment of patients with brain injury had greater expectations of recovery. Source of injury and patient’s current diagnosis did not explain expectations.
Conclusion
Relational factors between the patient and the surrogate may explain the surrogate’s expectation that the patient will recover more than factors that matter to clinicians, such as the source of injury or the patient’s diagnosis.
Keywords: Severe Brain Injury, Disorders of Consciousness, Surrogate Decision-Makers, Caregivers
Introduction
To treat a patient with a disorder of consciousness (DOC) clinicians must understand the family that speaks on their behalf. Family members of DOC patients, those in a coma, the vegetative state (VS) or the minimally conscious state (MCS) are caught in a complex and prolonged pseudo-grieving period where they must advocate for the patient’s right to receive care [1] in a culture of medical neglect [2]. The juxtaposing roles as near-griever and advocate create a state of emotional burden for family members and other intimates who serve as surrogate decision-makers. We know that a surrogate’s psychological state can directly impact the patient [3–6] and that the strain of caring for a severely brain-injured patient can negatively affect both the patient’s well-being and their rehabilitative outcome [4, 7]. What is less well understood is why, in such a state of ambiguity, some surrogates expect that the patient will improve, and why some do not, even in the face of negative prognostic information from clinicians.
While it is important in any clinical setting to understand expectations of decision-makers, it is particularly pertinent to DOC because surrogates are often making medical decisions in the absence of prognostic clarity [8–9] or even diagnostic certainty. Diagnostic accuracy in assessing DOC is uniquely low, with 41% of nursing home patients with traumatic brain injury being misdiagnosed [10]. It is known that under conditions of heightened prognostic ambiguity, designated surrogates make discretionary judgments about what they perceive is in the best interest of the patient which health care providers may not know [11]. We feel that this may be particularly true for surrogates of DOC patients because of both the ambiguity in treatment and diagnosis, and because of the consequences of lost or displaced consciousness. Expectations are central to family members’ understanding of how the severely brain-injured patients will fare. For example, surrogates’ positive expectation that an intervention will succeed improves their well-being even more than the actual success of that particular intervention [12, 13]. While this may seem illogical, that a surrogate’ hopes for improvement might have a greater effect than actual improvement, such data speaks to the power of hope and expectation to inform surrogate experience.
In this work, we explore what guides surrogate expectations of patient recovery and how this may differ from clinical criteria that a physician might use to predict outcomes, such as current clinical status or brain injury etiology [14, 15]. This empirical effort builds upon a narrative approach employed by one us to interview over 35 family members of patients with a DOC [16]. From that effort it has become clear that relationship dynamics shape surrogate expectations of recovery.
In this paper we begin to quantify these observations by studying degrees of closeness between injured patients and their surrogates and seeing if surrogates who identify as closer to the patient have different expectations about patient recovery. Closeness is an important variable in relationship research [17–18]. When two people become close, they extend their idea of themselves to include that other person; it is as if the other person becomes a part of them. With severe brain injury, degree of closeness between patient and surrogate has the possibility to inform the surrogate’s perception of illness and expectation of recovery. When the patient is very close, the injury has affected both the patient and the surrogate; recovery is as much manifested in the patient as in the surrogate.
The Inclusion of the Other in Self (IOS) is the process by which two people become close. To understand and quantify the process of IOS, researchers use the analogy of overlapping circles (i.e., a Venn diagram) representing the self and other to illustrated this theoretical foundation for understanding closeness [19]. Conceptually, this hypothesis is informed by knowledge that as an individual’s relationship becomes closer, distinctions between the self and the other are minimized [20] with closer individuals seeing the other’s resources, perspective and identity as their own (for example of the IOS diagram, see figure 1).
Figure 1.
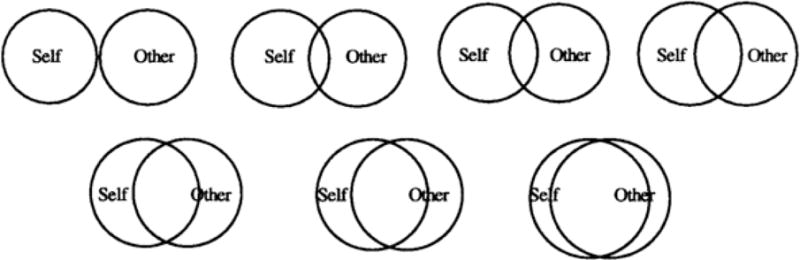
Example of Inclusion of Other in Self (IOS) Scale
What happens when a close other is lost? It has been suggested that the loss of a close ‘other’ requires some degree of exclusion of the other in self, or at least a process of slowly releasing the other’s resources, perspective and identity from one’s own self view [21]. We apply this theoretical frame to our study noting that for families of patients with DOCs, this ‘other’ remains physically present but paradoxically resides in memory. Yet owing to his or her condition, the patient as ‘other’ is unable to provide resources, a current perspective or an evolving identity to the surrogate. Thus, the surrogate’s ability to obtain resources, perspective and identity is contingent upon the patient getting better. We hypothesize that this enmeshment of needs may motivate surrogates to hold higher expectations for recovery because the stakes are so high: the surrogate is looking to recover what has been lost with the patient’s lost or displaced consciousness.
Understanding these dynamics and how they have the power to inform – and potentially distort – communication between surrogate and clinicians is necessary for medical and clinical staff who hope to be responsive to the difficulties of surrogate decision-making and the burdens associated with that role, whether it is to affirm the right to care or also let a loved one die [22–23].
Methods
Study population
405 family members contacted Weill Cornell Medical College (WCMC) or its affiliate New York Presbyterian Hospital (NYP) between August 2006 and January 2011 with interest in the scientific work being done on DOC after high profile scientific publications, [24–25] as well as a overview of the field in a 2008, 60 Minutes television special featuring our group at Weill Cornell [26].
Contact information was maintained in a confidential database, accessible only to researchers involved in WCMC IRB-approved research about DOC. 362 of those families identified as American. International inquiries were excluded for logistic and regulatory reasons. Before the research described below was initiated, 202 families were contacted by our research team for candidacy in different DOC research protocols at WCMC. These were thus excluded from this sample. Between January 2011 and June 2011, attempts were made to contact the remaining 160 family members to assess their interest in completing a mailed survey about the experience of having a family member with a DOC. We were unable to reach 89 families because of either disconnected phone numbers (45 families) or non-response after three phone calls or three emails were placed over the data collection period (44 families). 73 families were reached and mailed packages containing informed consent and HIPAA forms, our survey instrument and a stamped return envelope. If packages were unreturned, each family received two reminder calls and an additional copy of the survey, if needed. In total, 38 of those packages were returned (52% return rate). Three additional surveys were completed by family members of a patient enrolled in ongoing IRB-approved research about DOC. To address concerns that these three participants might differ from those who were mailed surveys, all reported linear regression models we report were run both with and without these three participants. Findings were unaffected by inclusion of these three additional participants and thus this data were included in reported results. A total of 41 family members representing 38 patients were collected. Demographic information for both the surrogates and the patients can be found in table 1.
Table 1.
Caregivers’ (n=41); patients’ living at home (n=21); in a facitlity (n=13) and deceased (n=3)
| Caregivers | Patients @ home | Patients@ facility | Deceased Patients | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| M | SD | M | SD | M | SD | |||
|
| ||||||||
| Age (years) | 58.3 | 10.5 | 33.1 | 13.9 | 53.0 | 19.7 | – | – |
|
| ||||||||
| Time since injury (months) | – | – | 103 | 53.8 | 107 | 80.7 | – | – |
|
| ||||||||
| N | % | N | % | N | % | N | % | |
| Race | ||||||||
| White/Caucasian | 36 | 88% | 20 | 95% | 10 | 77% | 3 | 100% |
| African American | 2 | 5% | 0 | 0% | 1 | 8% | 0 | 0% |
| Asian | 1 | 2% | 0 | 0% | 1 | 8% | 0 | 0% |
| Hispanic | 1 | 2% | 1 | 5% | 0 | 0% | 0 | 0% |
| Other | 1 | 2% | 0 | 0% | 1 | 8% | 0 | 0% |
| Education | ||||||||
| No college | 13 | 32% | 13 | 62% | 9 | 69% | 1 | 33% |
| Some college/BA | 17 | 41% | 5 | 24% | 4 | 31% | 2 | 67% |
| Advanced Degree | 11 | 27% | 3 | 14% | 0 | 0% | 0 | 0% |
| Relation to Patient | ||||||||
| Parent | 27 | 66% | – | – | – | – | – | – |
| Spouse | 4 | 10% | – | – | – | – | – | – |
| Adult Child | 7 | 17% | – | – | – | – | – | – |
| Other | 3 | 7% | – | – | – | – | – | – |
| Survey collected | ||||||||
| 38 | 93% | – | – | – | – | – | – | |
| At WCMC Hospital | 3 | 7% | – | – | – | – | – | – |
| Source of injury | ||||||||
| TBI | – | – | 5 | 24% | 4 | 31% | 0 | 0% |
| Anoxic Event | – | – | 14 | 67% | 5 | 38% | 2 | 67% |
| Other | – | – | 2 | 10% | 4 | 31% | 1 | 33% |
| Current Diagnosis | ||||||||
| VS | – | – | 1 | 5% | 3 | 23% | – | – |
| MCS | – | – | 5 | 24% | 4 | 31% | – | – |
| MCS Emerged | – | – | 7 | 33% | 4 | 31% | – | – |
| LIS | – | – | 1 | 5% | 1 | 8% | – | – |
| Recovery of Consciousness | 7 | 33% | 0 | 0% | – | – | ||
| Other | 1 | 8% | ||||||
| Diagnosis between T1 and T2 | ||||||||
| Got better | – | – | 9 | 42% | 4 | 31% | – | – |
| Stayed the Same | – | – | 10 | 48% | 4 | 41% | – | – |
| Got Worse | – | – | 1 | 5% | 2 | 15% | – | – |
| Did not have T1 / did not know | 1 | 5% | 3 | 23% | – | – | ||
Survey instrument
Overview
The survey instrument collected basic information about patient demographics, medical history and current condition. This was supplemented by queries directed to surrogates and their perspectives and expectations.
Dependent variables
First, we sought information about surrogate expectations for patient recovery. Surrogates reported both on their expectations when they initially contacted WCMC/NYP and their current expectations on a three-point scale (get better, stay the same, get worse) with the option to reply don’t know/don’t remember. This allowed temporal comparisons, as well as an opportunity to assess factors that predict current expectations.
Predictor variables
Demographic and historical data included the date and source of injury and the patient’s diagnosis at the time they initially contacted WCMC or NYP. Assessment of the patient’s current condition included current diagnosis, ability (if any) to communicate (from 1, not at all, to 5, completely), pain status (from 0, no pain, to 10, worst pain) and where they were living (home or facility).
All surrogates were asked to provide their own demographic information and personal relationship to the patient as assessed through the Inclusion of Other in Self Scale, a visual representation of relational closeness through two Venn diagrams of varying overlap (1, no overlap between self and patient, to 7, near complete overlap; see figure 1) [19].
Surrogates were also asked about their satisfaction with the patient’s health care (1, not at all satisfied, to 5, completely satisfied) and whether they believe technology will improve the treatment and diagnosis of people with severe brain injury (1, not at all, to 5, completely). They also answered several questions intended to assess well-being, including a single item response to whether they were depressed (yes, no, I don’t know) [27], if they were satisfied with their life as a whole (1, completely disagree, to 5, completely agree) [28], if they felt that everything had been an effort over the last year (1, completely disagree, to 5, completely agree; highest loading item on the CESD-S of the NIMH) [29–30] and how frequently they got together with friends and family (1, never, to 5, several times a week).
Statistical approach
All analyses were run in IBM SPSS Statistics for Macintosh v 19.0.0. First, we report demographic and frequency information as well as important differences between demographic categories using independent sample t-tests. Next we report preliminary univariate analyses used to identify predictors of our dependent variable (DV) of interest: surrogate’s expectation of improvement in the patient’s condition. In our preliminary analysis we used an elimination scheme with a broad inclusion criteria of predictors for whom the univariate test has a p-value of 0.2 or less. Predictors that fell above this value are unlikely to contribute to further predictive models. Next, we conducted a series of linear regression models to predict surrogate’s expectation of improvement. The first model included all predictors that emerged in our preliminary analysis as having potential explanatory power, and the second model included only those predictor variables that showed at least a significant trend in the first model. In all analyses we consider α level of .05, and report non-significant trends with an α level of .1.
Results
Demographics
To address concern over group differences between the mail responders and non- responders, we obtained 2000 Census data regarding average household income from the ZIP code families provided for mailing. A one-way ANOVA comparing responders and non-responders average household income by ZIP code was not significantly different, F(1, 72) = .014, p =.91, suggesting that the two groups were comparable by income.
Demographic characteristics of our patient and surrogate sample are summarized in table 1. Notably, our sample was predominantly white (88%) and well-educated, with 68% holding at least a bachelor’s degree. 66% of our surrogates were parents of the patient and 66% of surrogates were female. As reported by the surrogates, 57% of the patients suffered a TBI, 24% an anoxic event, and 19% reported ‘other’ as the source of injury. Since the surrogates made initial contact with WCMC/NYP, 3 of the 37 patients had died. Of the remaining 34, surrogates reported on their diagnosis. 4 patients were reported to be in the Vegetative State, 9 in MCS, 9 in MCS emerged (to functional communication), 5 in Locked-In State, 7 with (more complete) recovery of consciousness, and 1 reported other.
Gender difference
Independent sample t-tests revealed gender differences among the patients and surrogates that are worth noting. Surrogates in our sample are more likely to view male patients as better at communicating than female patients, t(20.22) = −3.05, p = .006, and surrogates were more likely to be satisfied with male patients’ health care t(35) = −2.06, p < .047. Female surrogates reported having been more satisfied with the patient’s health care, t(32) = 2.42, p < .021 and as having more faith in technology to help brain injury patients in the future, t (32) = 2.31, p < .027 than their male counterparts.
Living at home
Independent sample t-tests were performed comparing surrogates who live at home with the patient (n = 21) and patients who live in a facility (n = 13). Surrogates thought patients living at home were in less pain, t(32) = −2.32, p < .027, and could communicate better, t(29.77) = 3.36, p < .002.
Source of injury
Independent sample t-tests compared surrogates’ reporting when patients had a TBI (n = 21) compared to an anoxic (n = 9) or other injury (n = 7). Despite being one of the most important prognostic indications for recovery with TBI having a more favorable outcome, the source of injury neither predicted how surrogates viewed the patient’s current condition nor shaped their understanding and expectations of these conditions. Notably however, surrogates of TBI patients had significantly higher enmeshment scores than other patients t(16.87) = 2.48, p < .024 suggesting a variance in what is said about likelihood of recovery and what is experienced in the patient-surrogate dyad as one group recovers more robustly (TBI) than the next (Anoxia).
Expectation of recovery
Change from initial contact. For surrogates whose data was collected by mail and for whom the patient was still living, we compared their recall of their expectations that the patient would improve at the time they initially contacted WCMC/NYP, and the expectation of improvement that they now report. As shown in figure 1, surrogates’ expectations have changed, with a significantly smaller percentage thinking that the patient would improve now, compared to when they first contacted WCMC/NYP (42% vs. 63%), χ2 (2, n = 32) = −2.50, p < .013.
Preliminary analysis
Given that there is a decrease in the percentage of surrogates who think the patient will improve over time, we can go on to ask what demographic, medical or relational dynamic predicts surrogates’ expectations of improvement. Univariate analyses aimed to identify potential predictors indicated that several variables might be predictive of surrogates’ expectations that the patient will improve. These include factors relating to the patient 1) the time since injury, 2) communication ability, and 3) diagnostic stability. They also include factors relating to the surrogate 4) the degree of enmeshment with the patient, 5) the strength of his or her social network, and 6) the belief that technology would help brain-injured patients in the future, and the surrogate’s 7) gender, and 8) being a parent. Notably, the patient’s diagnosis or source of injury was unassociated in unviariate analysis with the surrogate’s expectation of improvement. The lack of diagnostic association could be due to a lack of sensitivity, as only 9 of our patients were reported as in VS.
Regression model
Informed by which predictors might explain the variance in surrogate expectation of improvement, we performed a linear regression model with expectation scored continuously (1 = get worse, 2 = stay the same, and 3 = get better). Cases where the surrogate reported I don’t know were excluded. All continuous predictor variables were grand mean centered. Categorical variables were dummy coded, including gender (male = 0; female = 1), relationship to the patient (parent = 1; other relation = 0) and whether the diagnosis had improved (improved = 1; stayed the same or gotten worse = 0). After running a model with all predictors, that emerged in our preliminary analysis, a second model was run, summarized in table 2, with only those predictors that showed at least non-significant trends.
Table 2.
Linear regression predicting expectation of improvement
| b | Std. Error | t | p | |
|---|---|---|---|---|
| Intercept | 1.820 | .429 | 4.245 | .000 |
| Diagnosis improveda | .433 | .212 | 2.045 | .054 |
| Time since injuryb | −.002 | .001 | −2.009 | .058 |
| IOS, measuring closenessb | .377 | .080 | 4.743 | .000 |
| Belief in technologyb | .236 | .112 | 2.115 | .047 |
|
| ||||
| Communication abilityb | .360 | .083 | 4.311 | .000 |
Notes: DF = 25; a dummy coded, diagnosis improved 1, stayed the same or got worse 0;
=mean centered
Overall, the model shown in table 2 significantly explained a significant proportion of variance in surrogate expectation of recovery, R2 = .773, F(5, 20) = 13.59, p < .001. As shown in figure 3, surrogates were likely to think the patient would get better if they were more enmeshed with the patient, b = .38, t(20) = 4.74, p < .001, suggesting that relational closeness leads to higher hopes of recovery. Similarly, surrogates were more likely to think the patient would get better if they thought the patient could communicate better, b = .36, t(20) = 4.31, p < .001, suggesting an overlap between expectation and perceived communication ability. Perhaps unsurprisingly, surrogates who had greater belief that technology would help brain-injured patients in the future were more likely to hold expectations of recovery, b = .25, t(20) = 2.12, p < .05. Two non- significant trends are worth reporting as well. Improvements in the patient’s diagnosis from initial contact was associated with greater expectation of improvement, b = .42, t(20) = 2.05, p = .054, and longer time since injury was associated with lower expectations of recovery, b = −.002, t(20) = −2.009, p = .058.
Figure 3.
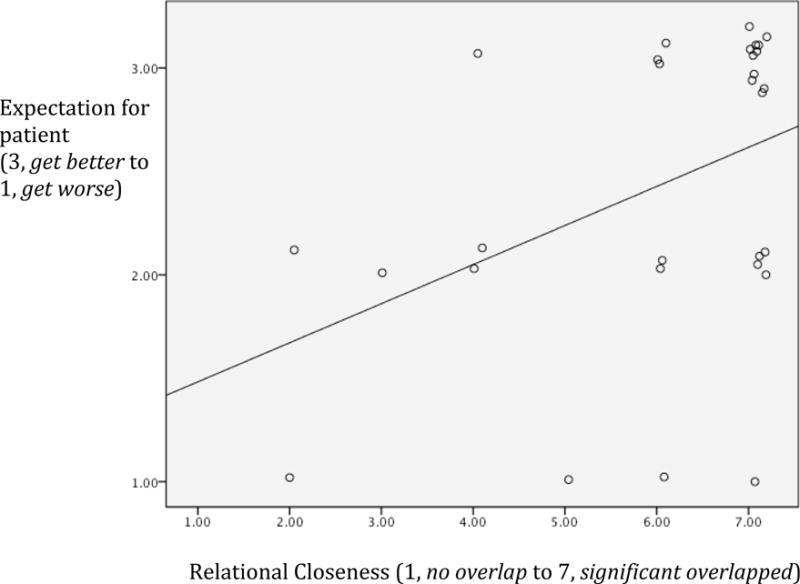
Influence of relational closeness on expectation that patient will improve
Discussion
Recent advances in the scientific understanding of brain injury and consciousness, along with the codification of diagnostic criteria for the Minimally Conscious State (31), have given many families hope that their loved one will recover, but have also created additional ambiguities regarding diagnosis and prognosis [8]. As family members navigate this increasingly complex environment, they are also being asked to make weighty medical decisions. What’s more, these patients are often young (in our own sample the average age was 40), with few having an advance directive to lay out future preferences in the event of future decisional incapacity. Without such direction, surrogates are dependent on the standard of substituted judgment, what they think the patient would want done, a task made more complicated by the prognostic uncertainty of these conditions [16], and the aforementioned relational distortions of surrogate expectations.
Most notably, we found that surrogates’ expectations were not guided by the two pieces of information that a clinician would say bear the most relevance to the patient’s prognosis: the patient’s current clinical status and the sources of the injury [15]. What mattered to surrogates instead were features that reflect the depth of the their relationship as informed by past experience and the surrogates current experience of present day reality, notwithstanding objective evidence to the contrary about actual recovery or ability to communicate.
Concern that families are misperceiving communication ability is highlighted by two significant finding among surrogates who live with the patient, compared to surrogates to a patient living in a facility. First, surrogates with a patient at home think those patients can communicate better, and second that those patients are in less pain. On the one hand, this could be advantageous: surrogates who live with the patient and think he or she can communicate might correctly observe the patient’s current state, and develop an ability to communicate over time. Conversely, these perceptions could become distorted because of enmeshment with a more nefarious symbiotic process [32] when the degree of emotional overlap places the patient at risk for futile or disproportionate medical interventions [23]. This distortion may create a false impression that the patient is not in pain, an error made all the more critical because of the potential that some patients may suffer as well [33].
Appreciating the complexity of the patient-surrogate dynamic in the face of severe brain injury, we hope to draw clinicians’ attention to such risks. It might be argued that when highly enmeshed surrogates look to the patient, they see an ‘other’ but they also see part of themselves. In this way, their expectation that the patient will recover may represent not just the patient’s recovery, but also their own hopes for the future and the recovery of a mutually constructed life that has been shattered by injury. These phenomena echo the bereavement literature that proposes that grief resolution is associated with the ability of people to alter self-identity following a loss, and that those more enmeshed relations are the hardest to resolve [34–36]. What is particularly challenging is that enmeshed surrogates of DOC patients can not yet engage in healthy grieving or seek grief resolution: Patients with DOCs remain alive and also have a potentially improving condition. For the enmeshed surrogate, who lives with an increasingly isolated life with the patient, the recovery of the patient does become essential to the dyad’s reintegration into communal life.
Clinical implications
This work is intended to help inform clinicians about the factors that affect surrogate decision-makers of patients with a DOC. Our results suggest that clinical predictors may not be as important to surrogates as to medical personnel and that the surrogate’s emotional closeness to the patient has the power to inform perceptions about communication, potential for recovery and the role of technology to ameliorate such conditions. Knowledge of this complex dynamic can help clinicians work with surrogates to make informed choices about care strategies for patients with disorders of consciousness.
Figure 2.
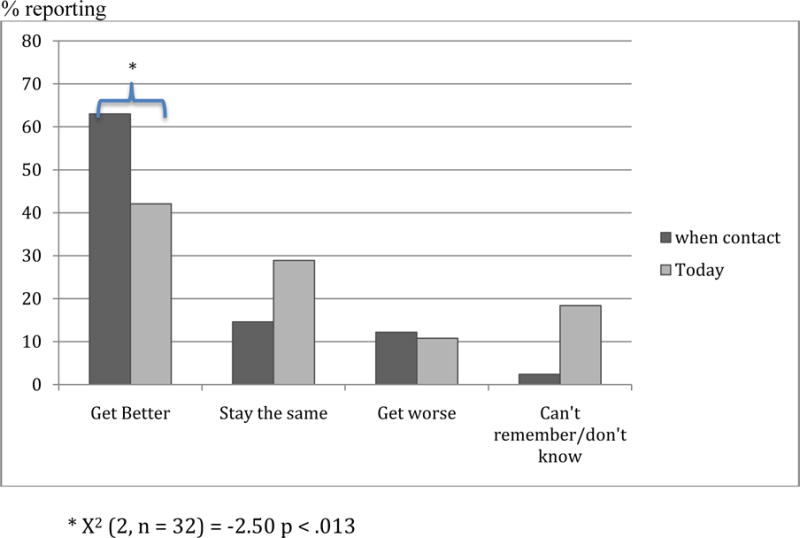
Change in expectation that the patient will improve from initial contact with WCMC to time of survey
Contributor Information
Alexandra Suppes, Postdoctoral Associate, Division of Medical Ethics, Weill Cornell Medical College
Joseph J. Fins, The E. William Davis, Jr., M.D. Professor of Medical Ethics, Chief, Division of Medical Ethics, Professor of Medicine, Professor of Public Health, Professor of Medicine in Psychiatry, Weill Medical College of Cornell University
References
- 1.Lanoix M. Where angels fear to tread: Proxy consent and novel technologies. Brain Inj. 2010;24:1336–42. doi: 10.3109/02699052.2010.504524. [DOI] [PubMed] [Google Scholar]
- 2.Fins JJ, Suppes A. Brain injury and the culture of neglect: Musing on an uncertain future. Soc Res. 2011;78:731–46. [Google Scholar]
- 3.Riley GA. Stress and depression in family careers following traumatic brain injury: the influence of beliefs about difficult behaviours. Clin Rehabil. 2007;21:82–8. doi: 10.1177/0269215506071279. [DOI] [PubMed] [Google Scholar]
- 4.Visser-Meily A, van Heugten C, Post M, et al. Intervention studies for caregivers of stroke survivors: a critical review. Patient Educ Cons. 2005;56:257–67. doi: 10.1016/j.pec.2004.02.013. [DOI] [PubMed] [Google Scholar]
- 5.Marsh NY, Kersel DA, Havill JH, et al. Caregiver burden at 1 year following severe traumatic brain injury. Brain Injury. 1998;12:1045–59. doi: 10.1080/026990598121954. [DOI] [PubMed] [Google Scholar]
- 6.Kreutzer JS, Gervasio AH, Camplair PS. Patient correlates of caregivers’ distress and family functioning after traumatic brain injury. Brain Injury. 1994;8:211–30. doi: 10.3109/02699059409150974. [DOI] [PubMed] [Google Scholar]
- 7.Kreutzer JS, Rapport L, Marwitz J, et al. Caregivers’ well-being after traumatic brain injury: A multi-center prospective investigation. Arch Phys Med Rehab. 2009;90:939–946. doi: 10.1016/j.apmr.2009.01.010. [DOI] [PubMed] [Google Scholar]
- 8.Fins JJ. Rethinking disorders of consciousness: New research and its implications. Hastings Cent Rep. 2005;35:22–24. [PubMed] [Google Scholar]
- 9.Zasler ND. Neurorehabilitation issues in states of disordered consciousness following traumatic brain injury. Future Neurol. 2006;1:439–452. [Google Scholar]
- 10.Schnakers CA, Vanhaudenhuyse J, Giacino M, et al. Diagnostic Accuracy of the Vegetative and Minimally Conscious State: Clinical Consensus versus Standardized Neurobehavioral Assessment. BMC Neurol. 2009;9:35–40. doi: 10.1186/1471-2377-9-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fins JJ, Maltby BS, Friedmann E, et al. Contracts, covenants and advance care planning: An empirical study of the moral obligations of patient and proxy. J Pain Symptom Manag. 2005;29:55–68. doi: 10.1016/j.jpainsymman.2004.07.004. [DOI] [PubMed] [Google Scholar]
- 12.Geurtsen GJ, van Heugten CM, Meijer R, et al. Prospective study of a community reintegration programme for patients with acquired chronic brain injury: effects on caregivers’ emotional burden and family functioning. Brain Injury. 2011;25:691–7. doi: 10.3109/02699052.2011.574675. [DOI] [PubMed] [Google Scholar]
- 13.Geurtsen GJ, van Heugten CM, Martina JD, et al. Comprehensive Rehabilitation Programmes in the Chronic Phase after Severe Brain Injury: A Systematic Review. J Rehabil Med. 2010;42:97–110. doi: 10.2340/16501977-0508. [DOI] [PubMed] [Google Scholar]
- 14.Posner JP, Saper CB, Schiff ND, et al. Plum and Posner’s Diagnosis of Stupor and Coma. New York: Oxford University Press; 2007. [Google Scholar]
- 15.Goldfine A, Schiff ND. Consciousness: It’s Nuerobiology and the Major Classes of Impairment. Neurol Clin. 2011;29:723–37. doi: 10.1016/j.ncl.2011.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fins JJ. Rights come to Mind: Brain Injury, Ethics & The Struggle for Consciousness. New York: Cambridge University Press; Undercontract. [Google Scholar]
- 17.Clark MS, Lemay EP., Jr . Close relationships. In: Fiske ST, Gilbert DT, Gardner L, editors. Handbook of Social Psychology. 5th. Vol. 2. Hoboken, NJ: John Wiley & Sons, Inc; [Google Scholar]
- 18.Aron A, Mashek D, Aron EN. Closeness, intimacy, and including other in the self In: Mashek D, Aron A, editors, Handbook of closeness and intimacy. Mahwah, NJ: Erlbaum; [Google Scholar]
- 19.Aron A, Aron EN, Smollan D. Inclusion of other in the Self Scale and the structure of interpersonal closeness. J Pers Soc Psychol. 1992;63:596–612. [Google Scholar]
- 20.Aron A, McLaughlin-Volpe T, Mashek D, et al. et al. Including others in the self. Euro Rev Soc Psychol. 2004;15:101–32. [Google Scholar]
- 21.Boelen PA, van den Hout MA. Inclusion of Other in the Self and Breakup-Related Grief Following Relationship Dissolution. J Loss Trauma. 2010;15:534–47. [Google Scholar]
- 22.Fins JJ. The patient Self-determination Act and patient-physician collaboration in New York State. New York State J Med. 1992;92:489–93. [PubMed] [Google Scholar]
- 23.Fins JJ. Affirming the right to care, preserving the right to die: Disorders of consciousness and neuroethics after Schiavo. Palliative & Supportive Care. 2006;4:169–78. doi: 10.1017/s1478951506060238. [DOI] [PubMed] [Google Scholar]
- 24.Owen AM, Coleman MR, Boly M, et al. Detecting awareness in the vegetative state. Science. 2006;313:1402. doi: 10.1126/science.1130197. [DOI] [PubMed] [Google Scholar]
- 25.Schiff ND, Giacino JT, Kalmar K, et al. Behavioural improvements with thalamic stimulation after severe traumatic brain injury. Nature. 2007;448:600–3. doi: 10.1038/nature06041. [DOI] [PubMed] [Google Scholar]
- 26.60 Minutes [internet] New York (NY): CBS News; 2007. Oct, [Cited 2012 Aug 4]; Available from: http://www.cbsnews.com/stories/2007/11/21/60minutes/main3530299.shtml. [Google Scholar]
- 27.Skoogh J, Ylitalo N, Larsson Omeróv P, et al. ‘A no means no’–measuring depression using a single-item question versus Hospital Anxiety and Depression Scale (HADS-D) Ann Oncol. 2010;21:1905–9. doi: 10.1093/annonc/mdq058. [DOI] [PubMed] [Google Scholar]
- 28.Diener E, Emmons RA, Larsem RJ, et al. The Satisfaction With Life Scale. J Pers Assess. 1985;49:71–5. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- 29.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general Population. Appl Psych Meas. 1977;1:385–401. [Google Scholar]
- 30.Radloff LS, Locke BZ. The Community Mental Health Assessment Survey and the CES-D Scale. In: Weissman M, Myers J, Ross C, editors. Community Surveys. New Brunswick, NJ: Rutgers University Press; 1986. pp. 177–89. [Google Scholar]
- 31.Giacino JT, Ashwal S, Childs S, et al. The Minimally Conscious State. Neurology. 2002;58:349–53. doi: 10.1212/wnl.58.3.349. [DOI] [PubMed] [Google Scholar]
- 32.Fins JJA. Palliative Ethic of Care: Clinical Wisdom at Life’s End. Sudbury, MA: Jones and Bartlett; 2006. pp. 198–201. [Google Scholar]
- 33.Schnakers C, Zasler N. Pain assessment and management in disorders of consciousness. Curr Opin Neurol. 2007;20:620–626. doi: 10.1097/WCO.0b013e3282f169d9. [DOI] [PubMed] [Google Scholar]
- 34.Boelen PA, van den Hout MA, van den Bout J. A cognitive-Behavioral conceptualization of complicated grief. Clin Psychol-Sci Pr. 2006;13:109–28. [Google Scholar]
- 35.Shear K, Shair H. Attachment, loss, and complicated grief. Dev Psychobiol. 2005;47:253–67. doi: 10.1002/dev.20091. [DOI] [PubMed] [Google Scholar]
- 36.Fins JJ, Hersh J. Solitary Advocates: The Severely Brain Injured and their Surrogates. In: Hoffman B, Tomes N, Schlessinger M, Grob R, editors. Transforming Health Care from Below: Patients as Actors in US Health Policy. New Brunswick, NJ: Rutgers University Press; 2011. [Google Scholar]


