Abstract
Background and Objectives:
Over the past few years, ultrasonography is increasingly being used to confirm the correct placement of endotracheal tube (ETT). In our study, we aimed to compare it with the traditional clinical methods and the gold standard quantitative waveform capnography. Two primary outcomes were measured in our study. First was the sensitivity and specificity of ultrasonography against the other two methods to confirm endotracheal intubation. The second primary outcome assessed was the time taken for each method to confirm tube placement in an emergency setting.
Methods:
This is a single-centered, prospective cohort study conducted in an emergency department of a tertiary care hospital. We included 100 patients with indication of emergency intubation by convenient sampling. The intubation was performed as per standard hospital protocol. As part of the study protocol, ultrasonography was used to identify ETT placement simultaneously with the intubation procedure along with quantitative waveform capnography (end-tidal carbon dioxide) and clinical methods. Confirmation of tube placement and time taken for the same were noted by three separate health-care staffs.
Results and Discussion:
Out of the 100 intubation attempts, five (5%) had esophageal intubations. The sensitivity and specificity of diagnosis using ultrasonography were 97.89% and 100%, respectively. This was statistically comparable with the other two modalities. The time taken to confirm tube placement with ultrasonography was 8.27 ± 1.54 s compared to waveform capnography and clinical methods which were 18.06 ± 2.58 and 20.72 ± 3.21 s, respectively. The time taken by ultrasonography was significantly less.
Conclusions:
Ultrasonography confirmed tube placement with comparable sensitivity and specificity to quantitative waveform capnography and clinical methods. But then, it yielded results considerably faster than the other two modalities.
Keywords: Capnography, emergency, intubation, ultrasonography
INTRODUCTION
Airway management skills are indispensable for an emergency physician. Unrecognized airway accidents such as esophageal intubation tend to occur more in emergency settings,[1] where it is reported as 6%-16%.[2]
Numerous studies have compared methods used for distinguishing between endotracheal and esophageal placement of the tube. Visual confirmation during laryngoscopy, expansion of the chest wall during ventilation, auscultatory method, capnography, and chest X-ray are modalities currently used in practice. These techniques vary in their degree of accuracy.[3,4,5,6]
The Advanced Cardiac Life Support (ACLS) 2015 guidelines recommend continuous waveform capnography in addition to clinical assessment as the most reliable method of confirming and monitoring correct placement of an endotracheal tube (ETT).[7] In 1989, in a study, Vaghadia et al. came to a conclusion that end-tidal carbon dioxide (ETCO2) is most accurate for identifying esophageal intubation.[8] Capnography has also been found to be the best method for rapid assessment of tube position.[2] Capnography is considered as the gold standard, but it has many limitations. Waveform capnography works on the principle of detection of carbon dioxide. This is only possible when there is sufficient pulmonary blood flow. In conditions where pulmonary blood flow is compromised such as massive pulmonary embolism and cardiac arrest, capnography is not reliable.[9]
Capnography is freely available in operation theaters but not in many emergency departments (EDs). Ultrasound, on the contrary, is emerging in most EDs as it is used in point of care imaging for trauma as well for guided interventions.[10] Ultrasound machine is portable, noninvasive, and the images are easily reproducible.[11] Various studies have shown that ultrasound is a potential method to confirm proper ETT placement.[12,13,14,15,16,17,18] In our study, we aim to find the effectiveness of tracheal ultrasonography to confirm ETT placement with the existing methods.
METHODS
This study was initiated after obtaining clearance from the Institutional Research and Ethics Committee. One hundred consecutive patients presented to ED with indication for endotracheal intubation were recruited into the study. Patients with significant neck or lung pathologies that would affect the study methods were excluded from the study. Tracheal sonography was performed using a SonoSite M-Turbo linear probe (13-6 MHz). A Philips M-20 monitor with a mainstream ETCO2 analyzer was used for capnography.
Intubation was performed as per the standard hospital protocol which includes confirmation by quantitative waveform capnography and clinical methods looking for bilateral chest rise and 5- point auscultation. The tube was deemed as endotracheal if a typical square waveform capnography was observed along with detection of carbon dioxide of more than 4 mmHg after five breaths.
The sonographer identified the placement of tube as tracheal or esophageal as follows:
Tracheal intubation if only one air-mucosal (A-M) interface with reverberation artifact and posterior shadowing was observed [Figure 1]
Esophageal intubation if two A-M interfaces posterior shadowing were noted, which is called a double tract sign [Figure 2].
Figure 1.
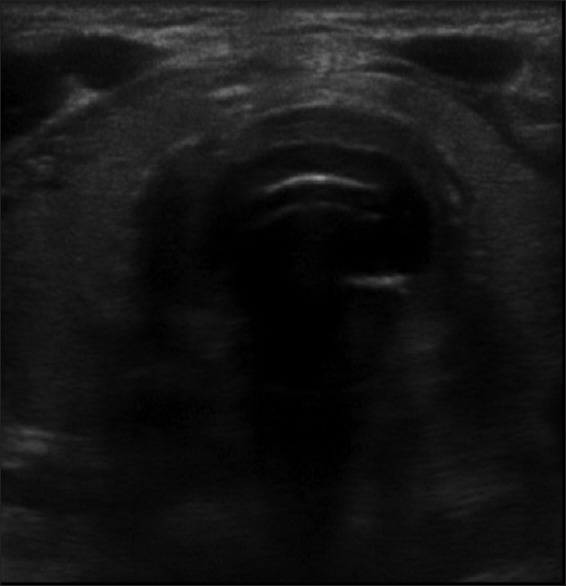
Sonographic image of tracheal intubation
Figure 2.
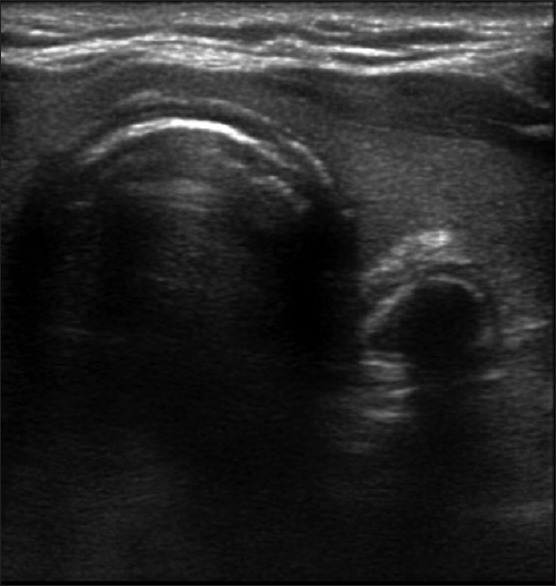
Sonographic image of esophageal intubation with “double tract” sign
Time zero was the time at which the person who did the intubation confirmed the completion of intubation. Following this, three different health-care staff simultaneously confirmed the tube placement, and the time taken by each method was noted using a stopwatch. End time noted was the time when individual health-care staff confirmed tube placement with their modality [Pro forma 1].
Two primary outcomes were measured in our study. First was the sensitivity and specificity of ultrasonography against the other two methods to confirm endotracheal intubation. The second primary outcome assessed was the time taken for each method to confirm tube placement in an emergency setting.
RESULTS
Among the 100 patients who underwent intubation, 59 were male and 41 were female. The mean age ± standard deviation was 50.79 ± 16.15 years. The most common indication for intubation was for airway protection (56%), followed by respiratory failure (23%) and for hemodynamic instability (21%).
Out of the 100 patients who underwent intubation, 95% were tracheal and 5% were esophageal. Tracheal ultrasonography correctly detected all 5% of esophageal intubations but misinterpreted 2% of tracheal intubations as esophageal.
The sensitivity, specificity, positive predictive value, and negative predictive value of the ultrasound method are shown in Table 1.
Table 1.
Sensitivity and specificity of ultrasonography
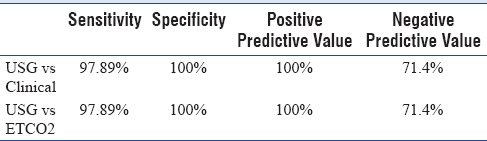
The sensitivity of the ultrasonography technique was compared with that of the other two modalities using McNemar test (two tail) which showed no statistically significant difference between the groups (P = 0.47).
The operating time of the different modalities is shown in Table 2. Statistically ultrasonography method (T1) took significantly less time compared to clinical (T2) and waveform capnography (T3) as shown in Figure 3. This was compared with Student's t-test (P < 0.001) when ultrasonography was compared with either capnography or clinical methods.
Table 2.
Operating time of different modalities
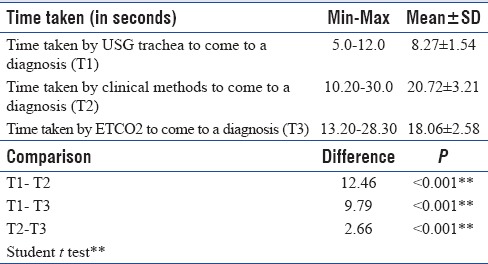
Figure 3.
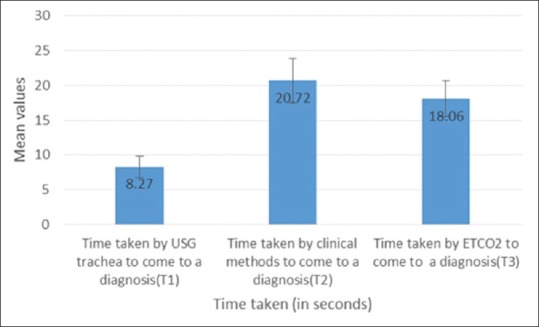
Time comparison
DISCUSSION
Identification of correct placement of ETT has been dependent on the airway specialist's skill in visualizing the vocal cords and on clinical methods to look for equal air entry on both lungs.[19] The vocal cords may not always be visualized, particularly in difficult airway and emergency settings. The accuracy of any technique to identify correct ETT placement is described by its sensitivity and specificity.[20] Many methods have evolved, but no single method has proved to be 100% reliable in distinguishing between tracheal and esophageal intubations.[19]
The ACLS, 2015, mentioned the different methods for identification of ETT placement including ultrasonography by placing a transducer transversely on the anterior part of the neck above the suprasternal notch. In addition, lung sliding sign on ultrasound of the thoracic cavity can identify movement of the lung.[18] It may also help in identifying endobronchial intubation.[20]
Quantitative waveform capnography is not widely available in EDs.[21] In a survey of the American National Emergency Airway Registry series, a total of 77% of physicians reported that colorimetric ETCO2 detectors were available in their hospitals, but only 25% of respondents used continuous quantitative capnography.[22] Hence, another confirmation technique with an easily available equipment is a welcome in EDs. Ultrasound is commonly used in EDs[10] for purposes such as focused intensive care echocardiography,[23] focused assessment of sonography in trauma,[24,25] and for vascular access.[25,26]
Of late, ultrasound is being used in ED for the confirmation of ETT placement.[27]
The use of ultrasound to confirm ETT placement is attractive due to its portability and repeatability with good sensitivity and specificity.[28,29,30,31] Moreover, ultrasonographic images are not affected by low pulmonary blood flow as compared to capnography.[32] Tracheal ultrasound detects esophageal intubation even before ventilating the patient, which prevents unnecessary forced ventilation to the stomach and its associated complications.
Using ultrasonography, ETT placement can be confirmed using tracheal, lung, or diaphragmatic scanning. Our study was performed using tracheal sonography which is the most common ultrasound modality used for the same.[12,13,14,15,16,17,28,29,30,31,32,33,34,35,36,37] Transtracheal ultrasound has a sensitivity of 95.7%-100% and a specificity of 96.3%-100% in identifying ETT placement.[38]
Different authors describe different sonographic features to diagnose tracheal and esophageal intubations, but close examination of the ultrasound images revealed that almost similar features were described differently.[12,13,14,15,16,17,28,29,30,30,31,32,33,34,35,36,37] To date, studies are lacking that directly compare the accuracy of different sonographic features.
Our study results had 5% of esophageal intubations which was comparable to similar studies.[12,29]
Four studies which used tracheal ultrasonography had detected 10% or more esophageal intubations[15,28,32,34] with a high sensitivity and specificity. Three of these studies were conducted at the ED[15,28,32] by emergency medicine (EM) residents while one was conducted at the operating room by anesthesiologists.[34]
One study which used diaphragmatic movement to confirm tube placement had 21% esophageal intubation and detected it with a lower sensitivity (91.7%) and specificity (95.6%).[15]
Three studies which used cadaveric models had higher esophageal intubation rates of 37%-50%.[17,31,35] The sensitivity and specificity of one study was 100%.[17] The cause for high sensitivity and specificity was probably due to the fact that the operators were qualified EM physicians and the study was conducted in a planned laboratory setting.
The other two studies had a lower sensitivity and specificity, probably due to the fact that the operators were residents with <12 months’ experience showing operator dependence.
The time required to confirm ETT intubation is an important consideration for any method used. Transtracheal ultrasound can be used for verification while the intubation is being performed or upon completion. Real-time sonographic imaging during intubation had higher sensitivity for detection of esophageal intubation than postintubation scanning.[12,15,30,32,33,35,36,37,38]
Using capnography, the patient's lungs would have to be ventilated 5 times for confirmation.[13] For this reason, transtracheal ultrasound can diagnose ETT intubation faster than capnography. Various studies have reported that the time required to perform transtracheal ultrasound ranged from 5 to 45 s.[37,38,39] Two studies compared timeliness of ultrasound with that of capnography and found that the median verification time with ultrasound was significantly shorter than with capnography.[40]
CONCLUSIONS
Ultrasonography, end-tidal capnography, and conventional clinical methods have comparable sensitivity and specificity in identifying tracheal or esophageal position of ETT.
However, ultrasonography detected the tube placement faster than the other two methods. The time difference is statistically significant, and, considering that the scenario is time critical, it has significant clinical importance. However, multi-centric trials with larger patient groups are needed before routine use of this modality.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We are thankful to “Jubilee Mission Medical College and Research Institute” and “Kerala University of Health Sciences” for providing the resources to conduct the study.
PRO FORMA: Pro forma 1: Ultrasonography for Confirming Endotracheal Tube Placement
Hospital Register No:
Age/Sex:
Vitals:
Indication:
Observer 1: Ultrasonography
Tube placement in – Encircle one
Trachea Esophagus
Total time taken by ultrasonography: T1 (in seconds)
Tube position: Encircle one
Endobronchial Tracheal
Observer 2: 5-point auscultation
Tube placement in – Encircle one
Trachea Esophagus
Time taken by clinical methods: T2 (in seconds)
Tube position: Encircle one
Endobronchial Tracheal
Observer 3: End-tidal capnography
Tube placement in: Encircle one
Trachea Esophagus
Time taken by capnography: T3 (in seconds)
Chest radiography finding
Tube position: Encircle one
Right main bronchus Central Left main bronchus Tube dislodged
REFERENCES
- 1.Adriani J. Unrecognized esophageal placement of endotracheal tubes. South Med J. 1986;79:1591–3. doi: 10.1097/00007611-198612000-00029. [DOI] [PubMed] [Google Scholar]
- 2.Schwartz DE, Matthay MA, Cohen NH. Death and other complications of emergency airway management in critically ill adults. A prospective investigation of 297 tracheal intubations. Anesthesiology. 1995;82:367–76. doi: 10.1097/00000542-199502000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Knapp S, Kofler J, Stoiser B, Thalhammer F, Burgmann H, Posch M, et al. The assessment of four different methods to verify tracheal tube placement in the critical care setting. Anesth Analg. 1999;88:766–70. doi: 10.1097/00000539-199904000-00016. [DOI] [PubMed] [Google Scholar]
- 4.Grmec S. Comparison of three different methods to confirm tracheal tube placement in emergency intubation. Intensive Care Med. 2002;28:701–4. doi: 10.1007/s00134-002-1290-x. [DOI] [PubMed] [Google Scholar]
- 5.Raphael DT, Benbassat M, Arnaudov D, Bohorquez A, Nasseri B. Validation study of two-microphone acoustic reflectometry for determination of breathing tube placement in 200 adult patients. J Am Soc Anesthesiol. 2002;97:1371–7. doi: 10.1097/00000542-200212000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Salem MR. Verification of endotracheal tube position. Anesthesiol Clin North America. 2001;19:813–39. doi: 10.1016/s0889-8537(01)80012-2. [DOI] [PubMed] [Google Scholar]
- 7.Link MS, Berkow LC, Kudenchuk PJ, Halperin HR, Hess EP, Moitra VK, et al. Part 7: Adult advanced cardiovascular life support: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18 Suppl 2):S444–64. doi: 10.1161/CIR.0000000000000261. [DOI] [PubMed] [Google Scholar]
- 8.Vaghadia H, Jenkins LC, Ford RW. Comparison of end-tidal carbon dioxide, oxygen saturation and clinical signs for the detection of oesophageal intubation. Can J Anaesth. 1989;36:560–4. doi: 10.1007/BF03005386. [DOI] [PubMed] [Google Scholar]
- 9.Cook TM, Nolan JP. Use of capnography to confirm correct tracheal intubation during cardiac arrest. Anaesthesia. 2011;66:1183–4. doi: 10.1111/j.1365-2044.2011.06964.x. [DOI] [PubMed] [Google Scholar]
- 10.Sustic A. Role of ultrasound in the airway management of critically ill patients. Crit Care Med. 2007;35(5 Suppl):S173–7. doi: 10.1097/01.CCM.0000260628.88402.8A. [DOI] [PubMed] [Google Scholar]
- 11.Galicinao J, Bush AJ, Godambe SA. Use of bedside ultrasonography for endotracheal tube placement in pediatric patients: A feasibility study. Pediatrics. 2007;120:1297–303. doi: 10.1542/peds.2006-2959. [DOI] [PubMed] [Google Scholar]
- 12.Chou HC, Chong KM, Sim SS, Ma MH, Liu SH, Chen NC, et al. Real-time tracheal ultrasonography for confirmation of endotracheal tube placement during cardiopulmonary resuscitation. Resuscitation. 2013;84:1708–12. doi: 10.1016/j.resuscitation.2013.06.018. [DOI] [PubMed] [Google Scholar]
- 13.Chou HC, Tseng WP, Wang CH, Ma MH, Wang HP, Huang PC, et al. Tracheal rapid ultrasound exam (T.R.U.E.) for confirming endotracheal tube placement during emergency intubation. Resuscitation. 2011;82:1279–84. doi: 10.1016/j.resuscitation.2011.05.016. [DOI] [PubMed] [Google Scholar]
- 14.Hsieh KS, Lee CL, Lin CC, Huang TC, Weng KP, Lu WH. Secondary confirmation of endotracheal tube position by ultrasound image. Crit Care Med. 2004;32(9 Suppl):S374–7. doi: 10.1097/01.ccm.0000134354.20449.b2. [DOI] [PubMed] [Google Scholar]
- 15.Hosseini JS, Talebian MT, Ghafari MH, Eslami V. Secondary confirmation of endotracheal tube position by diaphragm motion in right subcostal ultrasound view. Int J Crit Illn Inj Sci. 2013;3:113–7. doi: 10.4103/2229-5151.114269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lyon M, Walton P, Bhalla V, Shiver SA. Ultrasound detection of the sliding lung sign by prehospital critical care providers. Am J Emerg Med. 2012;30:485–8. doi: 10.1016/j.ajem.2011.01.009. [DOI] [PubMed] [Google Scholar]
- 17.Weaver B, Lyon M, Blaivas M. Confirmation of endotracheal tube placement after intubation using the ultrasound sliding lung sign. Acad Emerg Med. 2006;13:239–44. doi: 10.1197/j.aem.2005.08.014. [DOI] [PubMed] [Google Scholar]
- 18.Sim SS, Lien WC, Chou HC, Chong KM, Liu SH, Wang CH, et al. Ultrasonographic lung sliding sign in confirming proper endotracheal intubation during emergency intubation. Resuscitation. 2012;83:307–12. doi: 10.1016/j.resuscitation.2011.11.010. [DOI] [PubMed] [Google Scholar]
- 19.Williamson JA, Webb RK, Szekely S, Gillies ER, Dreosti AV. The Australian Incident Monitoring Study. Difficult intubation: An analysis of 2000 incident reports. Anaesth Intensive Care. 1993;21:602–7. doi: 10.1177/0310057X9302100518. [DOI] [PubMed] [Google Scholar]
- 20.Blaivas M, Tsung JW. Point-of-care sonographic detection of left endobronchial main stem intubation and obstruction versus endotracheal intubation. J Ultrasound Med. 2008;27:785–9. doi: 10.7863/jum.2008.27.5.785. [DOI] [PubMed] [Google Scholar]
- 21.Deiorio NM. Continuous end-tidal carbon dioxide monitoring for confirmation of endotracheal tube placement is neither widely available nor consistently applied by emergency physicians. Emerg Med J. 2005;22:490–3. doi: 10.1136/emj.2004.015818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wayne MA, Slovis CM, Pirrallo RG. Management of difficult airways in the field. Prehosp Emerg Care. 1999;3:290–6. doi: 10.1080/10903129908958956. [DOI] [PubMed] [Google Scholar]
- 23.Price S, Via G, Sloth E, Guarracino F, Breitkreutz R, Catena E, et al. Echocardiography practice, training and accreditation in the intensive care: Document for the World Interactive Network Focused on Critical Ultrasound (WINFOCUS) Cardiovasc Ultrasound. 2008;6:49. doi: 10.1186/1476-7120-6-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brenchley J, Walker A, Sloan JP, Hassan TB, Venables H. Evaluation of focussed assessment with sonography in trauma (FAST) by UK emergency physicians. Emerg Med J. 2006;23:446–8. doi: 10.1136/emj.2005.026864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maecken T, Grau T. Ultrasound imaging in vascular access. Crit Care Med. 2007;35(5 Suppl):S178–85. doi: 10.1097/01.CCM.0000260629.86351.A5. [DOI] [PubMed] [Google Scholar]
- 26.Arntfield RT, Millington SJ. Point of care cardiac ultrasound applications in the emergency department and Intensive Care Unit – A review. Curr Cardiol Rev. 2012;8:98–108. doi: 10.2174/157340312801784952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moore CL, Copel JA. Point-of-care ultrasonography. N Engl J Med. 2011;364:749–57. doi: 10.1056/NEJMra0909487. [DOI] [PubMed] [Google Scholar]
- 28.Abbasi S, Farsi D, Zare MA, Hajimohammadi M, Rezai M, Hafezimoghadam P. Direct ultrasound methods: A confirmatory technique for proper endotracheal intubation in the emergency department. Eur J Emerg Med. 2015;22:10–6. doi: 10.1097/MEJ.0000000000000108. [DOI] [PubMed] [Google Scholar]
- 29.Adi O, Chuan TW, Rishya M. A feasibility study on bedside upper airway ultrasonography compared to waveform capnography for verifying endotracheal tube location after intubation. Crit Ultrasound J. 2013;5:7. doi: 10.1186/2036-7902-5-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Muslu B, Sert H, Kaya A, Demircioglu RI, Gözdemir M, Usta B, et al. Use of sonography for rapid identification of esophageal and tracheal intubations in adult patients. J Ultrasound Med. 2011;30:671–6. doi: 10.7863/jum.2011.30.5.671. [DOI] [PubMed] [Google Scholar]
- 31.Göksu E, Sayraç V, Oktay C, Kartal M, Akcimen M. How stylet use can effect confirmation of endotracheal tube position using ultrasound. Am J Emerg Med. 2010;28:32–6. doi: 10.1016/j.ajem.2008.09.024. [DOI] [PubMed] [Google Scholar]
- 32.Park SC, Ryu JH, Yeom SR, Jeong JW, Cho SJ. Confirmation of endotracheal intubation by combined ultrasonographic methods in the emergency department. Emerg Med Australas. 2009;21:293–7. doi: 10.1111/j.1742-6723.2009.01199.x. [DOI] [PubMed] [Google Scholar]
- 33.Werner SL, Smith CE, Goldstein JR, Jones RA, Cydulka RK. Pilot study to evaluate the accuracy of ultrasonography in confirming endotracheal tube placement. Ann Emerg Med. 2007;49:75–80. doi: 10.1016/j.annemergmed.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 34.Milling TJ, Jones M, Khan T, Tad-y D, Melniker LA, Bove J, et al. Transtracheal 2-d ultrasound for identification of esophageal intubation. J Emerg Med. 2007;32:409–14. doi: 10.1016/j.jemermed.2006.08.022. [DOI] [PubMed] [Google Scholar]
- 35.Ma G, Davis DP, Schmitt J, Vilke GM, Chan TC, Hayden SR. The sensitivity and specificity of transcricothyroid ultrasonography to confirm endotracheal tube placement in a cadaver model. J Emerg Med. 2007;32:405–7. doi: 10.1016/j.jemermed.2006.08.023. [DOI] [PubMed] [Google Scholar]
- 36.Das SK, Choupoo NS, Haldar R, Lahkar A. Transtracheal ultrasound for verification of endotracheal tube placement: A systematic review and meta-analysis. Can J Anaesth. 2015;62:413–23. doi: 10.1007/s12630-014-0301-z. [DOI] [PubMed] [Google Scholar]
- 37.Hoffmann B, Gullett JP, Hill HF, Fuller D, Westergaard MC, Hosek WT, et al. Bedside ultrasound of the neck confirms endotracheal tube position in emergency intubations. Ultraschall Med. 2014;35:451–8. doi: 10.1055/s-0034-1366014. [DOI] [PubMed] [Google Scholar]
- 38.Sun JT, Chou HC, Sim SS, Chong KM, Ma MHM, Wang HP, et al. Ultrasonography for proper endotracheal tube placement confirmation in out-of-hospital cardiac arrest patients: Two-center experience. J Med Ultrasound. 2014;22:83–7. [Google Scholar]
- 39.Saglam C, Unlüer EE, Karagöz A. Confirmation of endotracheal tube position during resuscitation by bedside ultrasonography. Am J Emerg Med. 2013;31:248–50. doi: 10.1016/j.ajem.2012.08.002. [DOI] [PubMed] [Google Scholar]
- 40.Pfeiffer P, Rudolph SS, Børglum J, Isbye DL. Temporal comparison of ultrasound vs. auscultation and capnography in verification of endotracheal tube placement. Acta Anaesthesiol Scand. 2011;55:1190–5. doi: 10.1111/j.1399-6576.2011.02501.x. [DOI] [PubMed] [Google Scholar]


