Abstract
Background
This study reports the clinical and pathological features of 12 cases of primary Sjogren syndrome (pSS) with renal involvement presenting with proximal tubular dysfunction in a single center, and investigates the possible correlation of ectopic germinal center formation and megalin/cubilin down-expression.
Method
Clinical and pathological records were reviewed. Immunohistochemistry was carried out to detect megalin, cubilin, CD21 and IL-17 expression.
Results
Patients presented with different degrees of proximal renal tubule lesion and decreased estimated glomerular filtration rate (eGFR). Renal biopsy revealed tubulointerstitial nephritis, with tubular epithelial cell degeneration, tubular atrophy, interstitial inflammation and focal fibrosis. Immunohistochemistry revealed decreased expression of megalin and cubilin, two important multiligand protein receptors on the brush border of proximal tubular epithelial cells. IL-17 secreted by Th17 subtype effector T cells was diffusely detected in the renal proximal tubule, with a negative correlation of IL-17 and megalin expression. In addition, ectopic germinal centers characterized by CD21+ follicular dendritic cells were present in the renal interstitium. In patients with a decreased eGFR, treatment with 4 weeks of glucocorticoid therapy resulted in an improved eGFR in 75% of patients.
Conclusion
We report 12 cases of pSS characterized by Fanconi syndrome. The decreased megalin and cubilin expression may contribute to the proximal tubular reabsorption defect, possibly secondary to Th17 infiltration and formation of ectopic germinal centers.
Keywords: Primary Sjogren syndrome, Ectopic germinal center, Megalin, Cubilin, IL-17
Background
Primary Sjogren syndrome (pSS) is a chronic autoimmune epithelialitis targeting exocrine glands, with possible multisystem involvement [1]. Characteristic pathological changes are focal lymphocytic infiltration around the epithelial ducts and production of autoantibody by hyperactive B cells [2]. Renal involvement is observed in pSS, with both tubular and glomerular abnormalities reported. Tubulointerstitial nephritis (TIN) as a result of periepithelial inflammation is a predominant feature of pSS, often with evidence of a distal renal tubule acidosis (RTA) [3–5]. Fanconi syndrome, the result of proximal tubule epithelial cell (PTEC) injury leading to proximal RTA (type II RTA), hypophosphatemia, hypouricemia, aminoaciduria, glycosuria and urine loss of low molecular weight proteins, is a rare manifestation of pSS. To date, fewer than 20 cases have been reported and the underlying pathogenesis or mechanism remains unclear [6].
Ectopic germinal centers (EGCs), nonlymphoid collections of mature B lymphocytes, have been observed in the labial glands of pSS patients, believed to be the result of chronic inflammation [7]. The presence of CD21+ follicular dendritic cells is one of the hallmarks of EGCs [8, 9]. EGCs are suggested to be the site of immune stimulation and have been identified in other autoimmune diseases, such as rheumatoid arthritis and Grave’s disease. Self-reactive T lymphocytes and antibodies contribute to the process of tissue destruction and disease progression [10]. Recent studies suggest that Th17 cells, a subset of CD4+ T cells, may directly contribute to lymphoneogenesis in labial glands of pSS patients [11], but it is unclear whether a similar process occurs in the kidney of pSS patients with Fanconi syndrome. Inhibition of receptor-mediated endocytosis has been proposed as the mechanism of Fanconi syndrome in other disease states. Megalin and cubilin are multiligand protein receptors expressed at the brush border membrane and involved in endocytosis in PTECs. Megalin-knockout mice and cubilin-deficient dogs demonstrate deficient endocytosis, reproducing low-molecular proteinuria and vitamin D deficiency, which are the main characteristics of human Fanconi syndrome [12, 13].
In this study, we report the clinical and pathological characteristics and therapeutic outcomes of 12 patients with pSS and Fanconi syndrome. We describe the presence of EGCs in the renal interstitium, the prevalence of Th17/IL-17 expression, and alterations in megalin and cubilin expression, to investigate their possible correlation.
Methods
Patients and controls
All patients diagnosed with primary Sjogren syndrome with renal Fanconi syndrome in Peking Union Medical College Hospital (PUMCH) from 1994 to 2014 were enrolled. The diagnosis of pSS was made according to the American–European Consensus Group criteria for pSS [14]. Fanconi syndrome was defined by the coexistence of hypokalemia, hypophosphatemia, normoglycemic glycosuria, generalized aminoaciduria and hyperphosphaturia [15]. Clinical records and follow-up data of enrolled patients were carefully reviewed to understand demographic characteristics, symptoms, physical examination and laboratory tests. Laboratory examinations included routine tests: blood, urine, liver and renal function, 24-h urine protein, erythrocyte sedimentation rate (ESR), C-reactive protein and plasma protein electrophoresis. Renal tubular function assay included: blood and urine electrolytes, blood and urine α1-microglobulin (α1-MG), β2-microglobulin (β2-MG), blood pH, carbon dioxide combining power, urine N-acetyl-β-amino-glucosidase (NAG), retinol binding protein (RBP) and blood and urine osmotic pressure tests. Immunology assay included: immunoglobulin (IgG, IgA, IgM), rheumatoid factor (RF), blood complement and antinuclear antibodies spectrum. Screening for autoantibodies to SSA/Ro and SSB/La was performed systematically using Ouchterlony double-gel immunodiffusion and western blotting. Other tests included lacrimal and salivary gland secretion test (Schirmer test), salivary scintigraphy, parotid sialography and labial biopsy. The estimated glomerular filtration rate (eGFR) was calculated by the Modification of Diet in Renal Disease (MDRD) study equation [16]. Systemic manifestations of these patients were evaluated by Eular Sjogren’s Syndrome Disease Activity Index (ESSDAI) [17]. Twenty patients with pSS and tubulointerstitial nephritis (pSS + TIN) were included as the control group. TIN clinically manifested as hematuria, leucocyturia, proteinuria (24-h urine protein < 2 g), renal function impairment, distal RTA and hypokalemia, with mainly tubulointerstial impairment in renal biopsies, with or without minor glomerular damage. They had the same workup to exclude proximal tubule injury. Six cases of glomerular minor lesion (GML) were selected as normal controls. These normal patients underwent renal biopsy in the setting of mild isolated hematuria and strong desire for renal biopsy to figure out the etiology, but were not found to have underlying pathology.
Pathologic studies of kidney tissue
Two-micrometer slides were cut from formalin-fixed and paraffin-embedded (FFPE) sections of kidney tissues, stained with hematoxylin and eosin, periodic acid–Schiff, periodic acid–silver metheramine and Masson trichrome for light microscopy in the laboratory of Nephrology Department at PUMCH. At least eight sections were examined for each patient. All sections were examined by an experienced pathologist who was blinded to the patient’s characteristics. Tubulointerstitial injury was evaluated based on the Oxford Classification of IgA glomerulonephritis [18]. The classification used to describe the degree of lymphocytic infiltration in renal tissue was similar to that used in previous studies of the labial gland in patients with Sjogren syndrome: grade 0 (G0), absent, no lymphocyte infiltration; grade 1 (G1), slight infiltration, scattered lymphocytes infiltrating with an aggregate of fewer than 50 cells; grade 2 (G2), moderate infiltration, focal periductal lymphocytes aggregating in the labial gland, with 50 or more cells per one lesion; and grade 3 (G3), dense infiltration showing EGC-like structures in labial gland and CD21 staining positive [19].
Immunohistochemistry staining of megalin, cubulin, CD21 and IL-17A
Immunohistochemical (IHC) staining was performed on serial sections using standard methods in five pSS patients with Fanconi syndrome who underwent renal biopsy, five pSS + TIN patients (randomly selected from 20 patients in the control group) and six GML patients. Three-micrometer sections cut from paraffin-embedded tissue were deparaffinized and rehydrated. Sections were heated in a pressure cooker with 0.01 mol/L citrate buffer (pH 6.0) for 5 min to expose antigen and then incubated with the primary antibody (megalin, IL-17A and CD21, rabbit polyclonal antibodies; Abcam, Cambridge, MA, USA; cubilin, goat polyclonal antibody; Santa Cruz, CA, USA) overnight at 4 °C. After incubation with 0.3% H2O2 for 15 min, sections were incubated with the 1:500 HRP-conjugated anti-rabbit or anti-goat IgG (ImmunoReagents, USA) for 1 h at 37 °C. 3,3′-Diaminobenzidine (DAB) was used as a staining substrate. All section images were captured by a Nikon microscope (Eclipse 80i; Nikon, Japan) equipped with a digital photograph camera (DS-U1; Nikon, Japan).
Megalin immunofluorescence staining was done on 3-μm paraffin sections. The slides were incubated with primary antibody (megalin, rabbit polyclonal antibody; Abcam) overnight at 4 °C. Secondary antibody fluorescein-conjugated AffiniPure donkey anti-rabbit IgG (EarthOx, USA) was applied and incubated at 37 °C for 1 h. The micrographs were taken by confocal laser microscopy (Leica, Germany).
The degree of IHC staining was evaluated by calculating the percentage of positive glomeruli. Staining and scoring were performed blindly on coded slides. At least six fields were selected randomly in the renal cortex of each specimen for photo-documentation. Analytical measurements were done using Image Pro Plus 6.0.
Statistical analysis
Continuous variables are presented as the mean ± standard deviation. The variables consistent with normal distribution were compared using Student’s t test, one-way analysis of variance or Pearson’s correlation coefficients; skewed distribution samples were compared using the Mann–Whitney test or Spearman’s correlation. Categorical variables are expressed as percentages and are compared using the chi-square test. Statistical processing was performed using Graphpad Prism 6.0 and p <0.05 was considered statistically significant.
Results
Clinical characteristics
From January 1994 to August 2014, 2546 hospitalized patients in PUMCH were diagnosed of pSS, 335 of them presenting with renal manifestation (different degree of haematuria, proteinuria, tubule acidosis or renal function defect). By screening the medical records, 12 (0.47%) pSS patients with Fanconi syndrome were identified, five of whom underwent renal biopsy due to renal function impairment (eGFR compared with those without renal biopsy: 30.0 ± 8.5 vs 98.1 ± 27.5, p < 0.001). They were predominantly female, with a mean age of 39.3 ± 8.6 years. The male:female ratio was 1:5. At the onset, six patients presented with fatigue or anoxia, two developed hypokalemia paralysis, one developed bone pain and one had proteinuria. Two patients had sicca syndrome as the chief complaint initially. Systemic manifestations evaluated by ESSDAI ranged from 7 to 27, with an average of 18.8 ± 7.8. Weight loss (58.3%) was the most prominent symptom. Anemia (58.3%, hemoglobin averaged 105.3 ± 25.3 g/L), glandular involvement (16.7%), cutaneous lesion (8.3%) and pulmonary involvement (8.3%) were also observed. ANA was elevated in 75% of patients, and anti-Ro/SSA or anti-La/SSB antibodies were detected in eight (42.7%) and three (25.0%) patients, respectively. Eight of 11 (72.7%) patients showed increased immunoglobulin level. Two of 12 (16.7%) patients had increased RF level, and 3/12 (25%) patients showed decreased blood complement level. Laboratory studies consistent with proximal tubular injury were common with hypokalemia (100%), hypophosphatemia (83.3%), glycosuria (83.3%), RTA (75.0%) and aminoaciduria (72.7%). It is noteworthy that a majority of patients were associated with defects in other parts of the tubule, as proximal and distal RTA always coexistent. Eleven of 12 patients presented with albuminuria, ranging from trace to 1.0 g/L. Increased total protein in the urine was elevated in 10 patients, averaging 1.8 ± 0.5 g/24 h. Average eGFR was 69.8 ± 40.9 ml/min/1.73 m2, with five patients (41.7%) under 60 ml/min/1.73 m2. Table 1 compares the clinical profile between pSS patients with Fanconi syndrome and those with tubulointerstitial nephritis (pSS + TIN) who did not present with proximal tubule dysfunction. The pSS + Fanconi group had lower serum phosphorus level and more prominent proteinuria. Systemic manifestations showed no significant difference.
Table 1.
Comparison of clinical profile between patients with pSS + Fanconi syndrome and pSS + TIN
| pSS with Fanconi syndrome | pSS with TIN | P value* | |
|---|---|---|---|
| (N = 12) | (N = 20) | ||
| Age (years) | 39.3 ± 8.6 | 37.6 ± 12.2 | 0.366 |
| Gender (female %) | 10 (83.3) | 18 (90.0) | 0.620 |
| Presenting symptoms | |||
| Polyuria | 8 (66.7) | 10 (50.0) | 0.471 |
| Muscle weakness | 9 (75.0) | 14 (70.0) | 1.000 |
| Nocturia | 7 (58.3) | 5 (25.0) | 0.130 |
| dRTA | 9 (75.0) | 11 (55.0) | 0.452 |
| Paralysis | 3 (25.0) | 6 (30.0) | 1.000 |
| SCr elevation | 9 (75.0) | 12 (60.0) | 0.465 |
| eGFR (ml/min/1.73 m2) | 66.08 ± 38.20 | 76.14 ± 39.57 | 0.716 |
| Serum potassium (mmol/L) | 2.79 ± 0.14 | 2.76 ± 0.24 | 0.120 |
| Serum calcium (mmol/L) | 2.23 ± 0.14 | 2.13 ± 0.09 | 0.104 |
| Serum phosphorus (mmol/L) | 0.69 ± 0.33 | 1.02 ± 0.29 | 0.001 |
| 24-h urine protein (g/24 h) | 1.51 ± 0.84 | 1.00 ± 0.61 | 0.019 |
| Systemic manifestations | |||
| ESSDAI | 18.83 ± 7.83 | 15.50 ± 6.53 | 0.289 |
| Weight loss (>5%) | 7 (58.3) | 6 (30.0) | 0.150 |
| Glandular | 2 (16.7) | 3 (15.0) | 1.000 |
| Cutaneous | 1 (8.3) | 1 (5.0) | 1.000 |
| Pulmonary | 1 (8.3) | 3 (15.0) | 1.000 |
| Lymphadenopathy | 0 (0.0) | 2 (10.0) | 0.516 |
| HGB (g/L) | 105.3 ± 25.2 | 113.4 ± 13.6 | 0.408 |
| Immune profile | |||
| ESR (mm/h) | 58.8 ± 30.9 | 42.7 ± 30.9 | 0.141 |
| ANA positive | 9 (75.0) | 18 (90.0) | 0.338 |
| SSA positive | 5 (41.7) | 14 (73.7) | 0.130 |
| SSB positive | 3 (25.0) | 19 (47.1) | 0.273 |
| IgG (g/L) | 18.3 ± 8.2 | 19.7 ± 6.3 | 0.588 |
Data presented as number (%) or mean ± SD unless otherwise noted
ANA antinuclear antibody, dRTA distal renal tubule acidosis, eGFR estimated glomerular filtration rate, ESR erythrocyte sedimentation rate, ESSDAI Eular Sjogren’s Syndrome Disease Activity Index, HGB hemoglobin, IgG immunoglobulin G, pSS primary Sjogren syndrome, SCr serum creatinine, SSA Sjogren-syndrome-related antigen A, SSB Sjogren-syndrome-related antigen B, TIN tubulointerstitial nephritis
*Mann–Whitney (two-tailed) test for continuous variables and Fisher’s exact (two-tailed) test for categorical variables
Histopathological features
The biopsies of five pSS patients with Fanconi syndrome who underwent renal biopsy were reviewed. The primary lesion was moderate TIN with minimal glomerular injury and notable proximal tubular injury. Changes included tubule atrophy with defective brush border (64.0 ± 12.1%) and interstitial fibrosis (58.0 ± 12.8%) (Fig. 1a, b). Renal biopsy of Patient 3 revealed acute interstitial nephritis (AIN) with lymphocytic infiltration. Dense lymphocytes, monocytes, eosinophils and plasma cells could be identified in the focal lesion (Fig. 1c, d).
Fig. 1.

Patients with pSS + Fanconi syndrome show remarkable pathological lesions of renal proximal tubule. a Masson staining reveals interstitial fibrosis. b Boxed area in a enlarged. c Hematoxylin and eosin E staining indicating focus of lymphocyte infiltration. d Boxed area in c enlarged, indicating plasma cells in lymphocytes focus
Megalin and cubilin expression
Compared with normal controls (GML), the expression of megalin and cubilin on proximal tubule cells was decreased (Fig. 2). As shown in semiquantitative analyses, the positive area staining ratio of megalin and cubilin in pSS patients with Fanconi syndrome was significantly lower than that in the control GML group (Fig. 2D, E) (0.10 ± 0.01 vs 0.16 ± 0.02, p = 0.030; 0.05 ± 0.01 vs 0.11 ± 0.01, p = 0.004, respectively). Megalin and cubilin expression showed no significant difference between pSS + TIN patients and the GML group (0.14 ± 0.01 vs 0.16 ± 0.01, p = 0.320; 0.10 ± 0.01 vs 0.11 ± 0.01, p = 0.628), while there was a trend toward reduced expression in SS + Fanconi syndrome patients compared with the pSS + TIN group (0.10 ± 0.02 vs 0.14 ± 0.01, p = 0.095; 0.05 ± 0.01 vs 0.10 ± 0.01, p = 0.008).
Fig. 2.
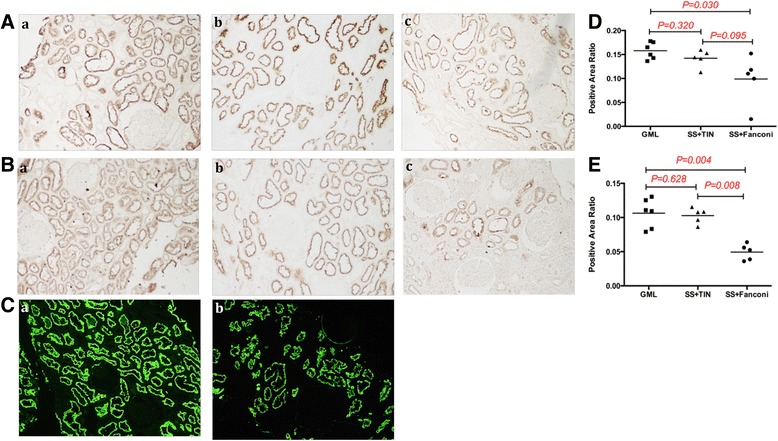
Immunohistochemistry and immunofluorescence reveals loss of megalin and cubilin expression in pSS patients with Fanconi syndrome. Staining of megalin (A, C) and cubilin (B) on kidney biopsies of patients with glomerular minor lesion (GML) (Aa, Ba, Ca), patients of pSS with tubulointerstitial nephritis (Ab, Bb), and pSS patients with Fanconi syndrome (Ac, Bc, Cb). Semiquantitative analysis shows decreased expression of megalin (D) and cubilin (E) in pSS patients with Fanconi syndrome, compared with GML and SS + TIN groups. GML glomerular minor lesion, SS Sjogren syndrome, TIN tubulointerstitial nephritis
Presence of CD21+ germinal centers
Focuses of lymphocytic infiltration could be seen in all biopsies of patients with pSS and Fanconi syndrome. There were three of G1, two of G2 and one of G3. The dendritic cell marker CD21+ was observed in one patient who showed the characteristics of AIN. There were several CD21+ focuses, indicating the presence of EGCs scattered in the renal interstitium (Fig. 3). We observed that the patient with G3 lymphocyte focus showed the lowest megalin and cubilin positive staining ratio. No specific relationship was identified between focus grading and expression levels of megalin or cubilin due to the small sample size.
Fig. 3.
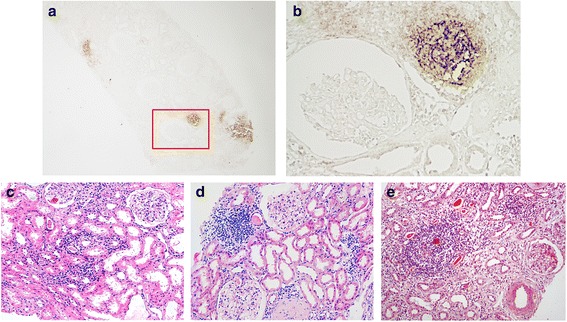
EGC of pSS with Fanconi syndrome. Immunohistochemical staining for CD21 in the kidney cortex (a, b) (boxed area in a is enlarged in b: a × 40, b × 200). Classification of lymphocytes aggregating in the proximal tubule: c G1, d G2 and e G3
Expression of IL-17A and megalin in serial sections
Diffuse expression of IL-17, a proinflammatory cytokine contributing to the formation of germinal centers, was observed in proximal renal tubules with variable intensity, while none was observed in the glomerulus. Both cytoplasm and cell membranes of the proximal renal tubule stained positively. It was noticeable that in the adjacent kidney paraffin sections of Patient 3, proximal tubules with strong IL-17A staining lacked expression of megalin, and vice versa (Fig. 4a, b). Infiltrating cells expressing IL-17A were identified in renal interstitium after hematoxylin staining of nucleus (Fig. 4c, d).
Fig. 4.
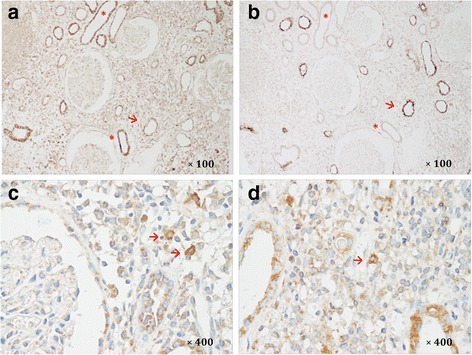
Expression of IL-17A and megalin in serial sections. Immunohistochemical staining of IL-17A (a) and megalin (b) on adjacent kidney paraffin sections from a patient with pSS + Fanconi syndrome. Proximal tubules with high expression of IL-17A show loss of megalin (asterisks), and those with preserved megalin expression have no IL-17A staining (arrow). c, d Identification of IL-17A expressing cells (arrow) in renal interstitium with hematoxylin staining of nucleus
Treatment and follow-up
All patients received treatment primarily with glucocorticosteroids with an initial dose of prednisone typically 0.5–1 mg/kg/day. Three patients also received cyclophosphamide or methotrexate in addition to prednisone. Patients generally showed good response to treatment, with a significant increase of eGFR (26–235%) over the median in-hospital time of 3 weeks. Five patients with impaired renal function were followed for an average of 59 months (1–192 months). During the follow-up, all patients showed improved renal function, with SCr decreased 39.2% on average. Their renal function remained stable with no flares (SCr higher than at onset, with/or 24-h UP > 0.3 g) and no requirement for renal replacement therapy. Electrolyte derangement also corrected with treatment, allowing a reduction in oral supplementation.
Discussion
The most common renal manifestation of pSS is a distal RTA, with proximal tubular acidosis seldom reported [20]. Fanconi syndrome, general dysfunction of the proximal tubule, is a relatively rare clinical manifestation of pSS. By searching PubMed with ((Sjogren syndrome) or (autoimmune epithelialitis)) and ((renal tubule) OR Fanconi), about 20 cases were identified [6, 21–35]. Wang et al. [6] and Shi and Chen [33] have summarized SS-related Fanconi syndrome cases that had been reported. We made a supplement to their summarization. We reported 12 cases of pSS + Fanconi syndrome cases with detailed clinical profile and follow-up records, to our limited knowledge, which is the largest sample in a single center. As presented in Table 2, similar clinical and pathological characteristics were observed in our study. In our series, 58% patients had impaired renal function with moderate TIN, and showed good response to glucocorticoid therapy. Both tubular function injury and eGFR were improved following treatment with steroids.
Table 2.
Comparison of clinical profile between our cases and pSS-related Fanconi syndrome reported in the literature
| Reference | Presenting symptoms | RTA | Cr | K (mmol/L) | Histology | Treatment | Outcome |
|---|---|---|---|---|---|---|---|
| Shearn and Tu [29] | Polyuria | + | n.a. | 3.8 | TIN, tubular atrophy | n.a. | n.a. |
| Walker et al. [30] | Paralysis, polyuria | + | n.a. | n.a. | TIN | Prednisolone 10 mg/day | n.a. |
| Kamm and Fischer [24] | Polyuria, nocturia, weight loss | + | 2.7 mg/dl | 2.9 | Diffuse TIN | Supportive only | Improved |
| Matsumura et al. [26] | n.a. | n.a. | 2.7 mg/dl | n.a. | TIN, tubulitis | n.a. | n.a. |
| Ardiles et al. [21] | Muscle weakness | + | 1.3 mg/dl | 2.5 | n.a. | Prednisolone “low dose” | Improved |
| Bridoux et al. [22] | Weight loss | + | 1.8 mg/dl | 3.5 | Diffuse TIN, proximal tubulitis | Supportive only | Dieda |
| Polyuria | + | 1.6 mg/dl | 2.4 | Diffuse TIN, proximal tubulitis | Prednisolone 10 mg/day | Improved | |
| Kobayashi et al. [25] | Muscle weakness | + | 1.3 mg/dl | 2.7 | Diffuse TIN, proximal tubule atrophy | Prednisolone 30 mg/day, 6 months later 12.5 mg/day | Improved |
| Ren et al. [32]b | n.a. | ||||||
| Yang et al. [31] | Muscle weakness, respiratory distress | + | 1.4 mg/dl | 2.7 | n.a. | Supportive only | n.a. |
| Nakamura et al. [27] | Renal dysfunction, organizing pneumonia, multiple bone fracture | + | 1.3 mg/dl | 3.0 | n.a. | Mizoribine 50 mg/day | n.a. |
| Wang et al. [6] | Hypokalemic paralysis | + | 2.2 mg/dl | 1.6 | Diffuse TIN | Mycophenolate mofetil 1 g/day | Improvedf |
| Ram et al. [28] | Paralysis | + | 2.1 mg/dl | 1.3 | Dense lymphocytic interstitial infiltrate | Supportive only | Improved |
| Celik et al. [23] | Paralysis, cardiac arrestc | + | 1.1 mg/dl | 1.1 | n.a. | Prednisone 40 mg/d iv. in acute phase | Improvedf |
| Shi and Chen [33] | Proteinuria, glycosuriad | + | 3.07 | TIN | Methylprednisolone | Improvede | |
| Saeki et al. [34] | Renal dysfunction | + | 1.07 mg/dl | 3.7 | TIN | Prednisolone 40 mg/day | Improvede |
| Kong et al. [35] | Weakness, osteodynia, impaired mobility | _ | n.a. | 1.3 | n.a. | Prednisone 30 mg/day | |
| Our cases | Fatigue, anorexia | + | 151 μmol/L | 3.4 | Diffuse TIN, diffuse tubule atrophy, lymphocyte infiltration | Prednisone 50 mg/day | Improvedf |
| Fatigue, polyuria, anorexia, osteopathy | + | 88 μmol/L | 2.1 | Focal TIN, focal tubule atrophy | Prednisone 40 mg/day | Improvedf | |
| Fatigue, anorexia, osteopathy | + | 176 μmol/L | 3.3 | Diffuse TIN, diffuse tubule atrophy, lymphocyte infiltration | Prednisone 50 mg/day | Improvede | |
| Fatigue, anorexia | + | 305 μmol/L | 2.7 | Focal TIN, focal tubule atrophy | Prednisone 45 mg/day | Improvede | |
| Fatigue, anorexia, polyuria | – | 72 μmol/L | 2.53 | Mild tubulitis | Supportive only | Improvedf | |
| Fatigue, anorexia, polyuria | + | 184 μmol/L | 3.0 | n.a. | Prednisone 35 mg + cyclophosphamide 0.2 g qod | Improvede | |
| Polyuria | – | 120 μmol/L | 3.4 | n.a. | Prednisone 60 mg/day | Improvede | |
| Fatigue, polyuria, anorexia, osteopathy | + | 202 μmol/L | 2.62 | n.a. | Prednisone 55 mg/day | Improvede | |
| Osteopathy | – | 110 μmol/L | 3.2 | n.a. | Prednisone 55 mg/day + metrotraxate 10 mg qw | Improvedf | |
| Fatigue, polyuria, osteopathy | + | 75 μmol/L | 2.88 | n.a. | Prednisone 40 mg/day + cyclophosphamide 0.2 g qod | Improvedf | |
| Hypokalemic paralysis, osteopathy | + | 65 μmol/L | 2.1 | n.a. | Supportive | Improvedf | |
| polyuria, osteopathy | + | 71 μmol/L | 2.34 | n.a. | Prednisone 30 mg/day + metrotraxate 10 mg qw | Improvedf | |
Mean age of patients with pSS-related Fanconi syndrome reported in the literature is 47.4 ± 13.2, with a female ratio of 93.3%
n.a. not available, pSS primary Sjogren syndrome, qop every other day, qw every week, RTA renal tubule acidosis, TIN tubulointerstitial nephritis
aProbable cardiovascular event
bFour cases reported in a retrospective study of 130 cases, no detailed information
cAlso diagnosed of brucellic disease
dWith autoimmune thyroiditis
eImprovement of renal function, and stable during follow-up
fCorrection of electrolyte derangement, and relief of symptoms
Few studies have focused on the mechanism of Fanconi syndrome or PTEC injury in pSS. We observed the downregulation of megalin and cubilin in PTECs, which suggests defective endocytosis. Megalin and cubilin are endocytic receptors coexpressed in the proximal tubule, located on the brush border and endocytic vesicles. They bind and mediate the endocytosis of a variety of ligands, including enzymes or enzyme inhibitors, lipoproteins, hormones, signaling proteins, immune or stress response-related proteins, receptors and vitamin carrier proteins as well as drugs and toxins [12, 36]. Megalin and cubilin are associated with key processes to fulfill the classic reabsorption function of proximal tubules: the integrity of cell structure, such as polarity, brush border and endocytic apparatus; apical multiligand receptors megalin and cubilin; and intact transport system consisting of microvilli, clathrin-coated pits, early endosomes, late endosomes and lysosome. The other processes include energy production by mitochondria and basolateral Na+-K+-ATPase as the driving force for Na+-coupled transport [13, 37–39]. In cystinosis, a known cause of Fanconi syndrome, alterations in megalin activity have been noted on the brush border, endosomes and lysosomes by immunofluorescence under electron microscopy [40]. Megalin and cubilin have also been shown to be critical in Fanconi syndrome from other causes. Mutations in the gene low-density lipoprotein receptor-related protein 2 (LRP2), encoding the protein megalin, have been identified in Donnai-Barrow (DB) syndrome and Facio-Oculo-Acustico-Renal (FOAR) syndrome. These patients show prominent low-molecular weight proteinuria, with malabsorption of vitamin D-binding protein, retinol-binding protein and albumin [41]. Elegant experiments have suggested urinary megalin deficiency implicating abnormal tubular endocytic function in Fanconi syndrome related to Dent’s disease and Lowes syndrome [42]. In these genetic disorders, the down-expression of megalin/cubilin caused by impaired endosome–lysosome trafficking has also been shown [43, 44]. On the other hand, megalin-mediated endocytosis of excessive protein is pathogenic in light-chain tubulopathy. It has been shown that silencing megalin and cubilin genes may inhibit myeloma light chain uptake, suppressing inflammation in PTECs, and reducing the nephrotoxic effects [45]. The mechanism of drug-induced Fanconi syndrome is not fully understood at this point in time [46]. However, as far as we can see, the mechanism of Fanconi syndrome caused by pSS has not yet been discussed. The innovation of our study is to show that defect endocytosis in PTECs mediated by megalin and cubilin may contribute to the reabsorption impairment in patients with pSS and Fanconi syndrome. A trend toward loss of megalin expression was observed in pSS with TIN, but this was not significant compared with the decreased expression of megalin noted in patients with pSS and Fanconi syndrome. We propose that proximal tubule impairment was less severe in TIN with general tubule injury, because no symptoms of endocytic receptor defect were observed.
The mechanism of megalin and cubilin alteration remains poorly understood, although past studies have indicated that renal ischemia and reperfusion injury, inflammation and drugs may all be causative. Lipopolysaccharide has been shown to downregulate megalin and cubulin expression in vitro and vivo [47]. In this study, we first observed the inverse relationship of megalin and IL-17 expression with associated ectopic germinal center (EGC) formation in the kidney. IL-17 is a proinflammatory cytokine secreted by Th17 cells, which comprise a distinct subset of CD4+ T cells that play a role in autoimmune disease [48]. Th17 cells are believed to activate follicular dendritic cells and stromal cells via surface molecule LTα1β2 and they secrete IL-17, stimulating stromal cells, fibroblasts and tissue epithelial cells to produce chemokines [11]. IL-17 secretion is induced by IL-21, produced by Tfh cells, a component of EGCs. IL-17 then acts in conjunction with IFNγ to recruit lymphocytes for the formation of the germinal center [49]. In addition, we observed that renal proximal tubule cells can express IL-17. It is reasonable to assume that epithelial cells may be an important component of immune response in TIN, as has been indicated in renal transplant rejection. EGCs are highly organized lymphoid aggregates that form in tissue sites which are not typically associated with lymphoid neogenesis [50]. TIN is characterized by organized infiltration of anatomically distinct and adjacent T-cell and B-cell compartments, with the presence of follicular dendritic cells (DCs) [9]. As the infiltrating cells, DCs have been shown to be necessary and sufficient in the formation of EGCs [51–53], Depletion of DCs leads to disappearance of existing follicular germinal center structure [52]. We observed that circulating pDCs and mDCs were reduced in pSS patients with TIN, compared with patients with pSS alone. In addition, immunohistochemical staining of BDCA-2 and DC-SIGN revealed increased pDCs and mDCs in renal interstitium. Combining these findings, we assume that in the setting of local inflammation in pSS, DCs can be recruited to renal tissue from peripheral blood (unpublished data). CD21 remains the most reliable marker of follicular dendritic cells. In another study of our group, we find that in pSS with membranous nephrology, all G3 patients (30.5% of 36 patients) showed positive CD21 staining with varying degree, and typical EGC structure was seen in nine patients. The relationship of IL-17 and germinal center activity has been observed previously. In an experimental autoimmune encephalomyelitis murine model, Th17 cells also directly elicit formation of ectopic lymphoid follicle formation, by surface molecule podoplanin and secretion of IL-17 [54]. In the formation of inducible bronchus associated lymphoid tissue (iBALT), IL-17 secreted by Th17 cells contributes to the initial stage [55]. In the labial glands with pSS, germinal centers developed in 25.1 ± 5.0% of patients [56]. Both Sakai et al. and Fei et al. reported that the majority infiltrating cells in the salivary glands of SS patients were CD4+ T cells, with a predominant expression of IL-17 [56, 57], which could be modified by immunosuppressive treatment [57]. Consistent with their findings, we observed infiltrating cells expressing IL-17A present in renal interstitium (we did not perform CD4 and IL-17A double-staining to clarify Th17 cells due to limited pathological sections). There is also evidence to suggest that EGC formation may contribute to progression of disease in lupus nephritis [58, 59]. Therefore, the presence of DCs and EGCs in the interstitium of the kidney in patients with pSS suggests that the severe renal interstitial inflammation, with Th17 infiltration and IL-17 secretion, may be correlated to megalin and cubilin impairment. We suppose that local inflammation may subsequently mediate brush border destruction, characterized by decreased megalin and cubilin expression, leading to the reabsorptive dysfunction of PTECs and Fanconi syndrome.
There are several limitations of our study. First, not all patients underwent bicarbonate loading test, and patients with isolated proximal tubule acidosis could not be identified. Second, as a retrospective study, instead of the mechanism we only suggested a correlation between EGC formation and defected endocytosis characterized by megalin/cubilin down-expression. It is possible that megalin/cubilin deficiency is a reflection of generalized proximal tubule injury, because up to 45.2% of pSS patients were present with elevated excretion of β2-microglobulin. Third, a different degree of inflammation may not explain the whole picture of why only certain pSS + TIN patients present with proximal tubule defect. Whether this is due to specific local antibody remains to be elucidated by further study.
Conclusion
Collectively, we reported 12 cases of pSS with Fanconi syndrome. They present with proximal tubular defect, decreased eGFR and tubulointerstitial nephritis, and they show good response to glucocorticosteroids therapy. Down-expression of megalin and cubilin may cause the endocytosis reabsorption dysfunction of proximal renal tubules. We suggest that this is related to Th17 infiltration, IL-17 expression and formation of ectopic germinal centers.
Acknowledgements
Not applicable.
Funding
The authors have received grants from the Key Project of Chinese National Program for Fundamental Research and Development (973 Program 2012CB517803 to LC) and the National Natural Scientific Foundation, China (81170674, 81470937 to LC).
Availability of data and materials
Not applicable.
Authors’ contributions
JW participated in the study design, obtained clinical data, conducted the immunohistochemical staining, performed the statistical analysis, and wrote the manuscript. YW participated in study design, made pathological diagnosis, obtained all of the pathological data, and was involved in data analysis. MZ participated in the study design, and in statistical analysis and helped with drafting of the manuscript. XS and LJ participated in study design, obtained clinical data, and participated in data analysis. ML, YY, XmL, and XwL participated in study design and coordination, helped with acquisition of clinical data, and was involved in revising the manuscript. WZ conceived the study and participated in interpretation of data. ALL revised the manuscript critically for important intellectual content. LC and YY conceived the study, participated in its design and coordination, and helped to draft the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethical approval and consent to participate
The study was performed in accordance with the Helsinki Declaration and approved by the local Ethic Committee of Peking Union Medical College Hospital. However, not all informed written consent was available because some patients were lost to follow-up.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- ANA
Antinuclear antibody
- DC
Dendritic cell
- EGC
Ectopic germinal center
- eGFR
Estimated glomerular filtration rate
- ESR
Erythrocyte sedimentation rate
- ESSDAI
Eular Sjogren’s Syndrome Disease Activity Index
- FFPE
Formalin-fixed and paraffin-embedded
- GML
Glomerular minimal lesion
- IL-17
Interleukin 17
- MDRD
Modification of Diet in Renal Disease
- NAG
N-acetyl-β-amino-glucosidase
- pSS
Primary Sjogren syndrome
- PTEC
Proximal tubule epithelial cell
- RBP
Retinol binding protein
- RTA
Renal tubule acidosis
- SCr
Serum creatinine
- SSA
Sjogren-syndrome-related antigen A
- SSB
Sjogren-syndrome-related antigen B
- TIN
Tubulointerstitial nephritis
- α1-MG
α1-Microglobulin
- β2-MG
β2-Microglobulin
Contributor Information
Jing Wang, Email: 15011040287@163.com.
Yubing Wen, Email: wenyubing@hotmail.com.
Mengyu Zhou, Email: zhoumengyu_helen@hotmail.com.
Xiaoxiao Shi, Email: colaxiao66@163.com.
Lanping Jiang, Email: fuzhi626@126.com.
Mingxi Li, Email: mingxili@hotmail.com.
Yang Yu, Phone: 8610-65295351, Email: yuyang@medmail.com.cn.
Xuemei Li, Email: lixmpumch@126.com.
Xuewang Li, Email: xhxwl@hotmail.com.
Wen Zhang, Email: zhangwen91@sina.com.
Andrew L. Lundquist, Email: ALUNDQUIST@mgh.harvard.edu
Limeng Chen, Phone: 8610-65295351, Email: chenlimeng@pumch.cn.
References
- 1.Moutsopoulos HM. Sjogren's syndrome: autoimmune epithelitis. Clin Immunol Immunopathol. 1994;72:162–5. doi: 10.1006/clin.1994.1123. [DOI] [PubMed] [Google Scholar]
- 2.Ramos-Casals M, Tzioufas AG, Font J. Primary Sjogren's syndrome: new clinical and therapeutic concepts. Ann Rheum Dis. 2005;64:347–54. doi: 10.1136/ard.2004.025676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maripuri S, Grande JP, Osborn TG, Fervenza FC, Matteson EL, Donadio JV, et al. Renal involvement in primary Sjogren's syndrome: a clinicopathologic study. Clin J Am Soc Nephrol. 2009;4:1423–31. doi: 10.2215/CJN.00980209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goules AV, Tatouli IP, Moutsopoulos HM, Tzioufas AG. Clinically significant renal involvement in primary Sjogren's syndrome: clinical presentation and outcome. Arthritis Rheum. 2013;65:2945–53. doi: 10.1002/art.38100. [DOI] [PubMed] [Google Scholar]
- 5.Kaufman I, Schwartz D, Caspi D, Paran D. Sjogren's syndrome—not just Sicca: renal involvement in Sjogren's syndrome. Scand J Rheumatol. 2008;37:213–8. doi: 10.1080/03009740701867323. [DOI] [PubMed] [Google Scholar]
- 6.Wang CC, Shiang JC, Huang WT, Lin SH. Hypokalemic paralysis as primary presentation of Fanconi syndrome associated with Sjogren syndrome. J Clin Rheumatol. 2010;16:178–80. doi: 10.1097/RHU.0b013e3181df903f. [DOI] [PubMed] [Google Scholar]
- 7.Theander E, Vasaitis L, Baecklund E, Nordmark G, Warfvinge G, Liedholm R, et al. Lymphoid organisation in labial salivary gland biopsies is a possible predictor for the development of malignant lymphoma in primary Sjogren's syndrome. Ann Rheum Dis. 2011;70:1363–8. doi: 10.1136/ard.2010.144782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Risselada AP, Looije MF, Kruize AA, Bijlsma JW, van Roon JA. The role of ectopic germinal centers in the immunopathology of primary Sjogren's syndrome: a systematic review. Semin Arthritis Rheum. 2013;42:368–76. doi: 10.1016/j.semarthrit.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 9.Neyt K, Perros F, GeurtsvanKessel CH, Hammad H, Lambrecht BN. Tertiary lymphoid organs in infection and autoimmunity. Trends Immunol. 2012;33:297–305. doi: 10.1016/j.it.2012.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aloisi F, Pujol-Borrell R. Lymphoid neogenesis in chronic inflammatory diseases. Nat Rev Immunol. 2006;6:205–17. doi: 10.1038/nri1786. [DOI] [PubMed] [Google Scholar]
- 11.Grogan JL, Ouyang W. A role for Th17 cells in the regulation of tertiary lymphoid follicles. Eur J Immunol. 2012;42:2255–62. doi: 10.1002/eji.201242656. [DOI] [PubMed] [Google Scholar]
- 12.Christensen EI, Birn H. Megalin and cubilin: multifunctional endocytic receptors. Nat Rev Mol Cell Biol. 2002;3:256–66. doi: 10.1038/nrm778. [DOI] [PubMed] [Google Scholar]
- 13.Sirac C, Bridoux F, Essig M, Devuyst O, Touchard G, Cogne M. Toward understanding renal Fanconi syndrome: step by step advances through experimental models. Contrib Nephrol. 2011;169:247–61. doi: 10.1159/000313962. [DOI] [PubMed] [Google Scholar]
- 14.Vitali C, Bombardieri S, Jonsson R, Moutsopoulos HM, Alexander EL, Carsons SE, et al. Classification criteria for Sjogren's syndrome: a revised version of the European criteria proposed by the American–European Consensus Group. Ann Rheum Dis. 2002;61:554–8. doi: 10.1136/ard.61.6.554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roth KS, Foreman JW, Segal S. The Fanconi syndrome and mechanisms of tubular transport dysfunction. Kidney Int. 1981;20:705–16. doi: 10.1038/ki.1981.200. [DOI] [PubMed] [Google Scholar]
- 16.Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130:461–70. doi: 10.7326/0003-4819-130-6-199903160-00002. [DOI] [PubMed] [Google Scholar]
- 17.Seror R, Ravaud P, Bowman SJ, Baron G, Tzioufas A, Theander E, et al. EULAR Sjogren's syndrome disease activity index: development of a consensus systemic disease activity index for primary Sjogren's syndrome. Ann Rheum Dis. 2010;69:1103–9. doi: 10.1136/ard.2009.110619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Roberts IS, Cook HT, Troyanov S, Alpers CE, Amore A, Barratt J, et al. The Oxford classification of IgA nephropathy: pathology definitions, correlations, and reproducibility. Kidney Int. 2009;76:546–56. doi: 10.1038/ki.2009.168. [DOI] [PubMed] [Google Scholar]
- 19.Ohara T, Itoh Y, Itoh K. Reevaluation of laboratory parameters in relation to histological findings in primary and secondary Sjogren's syndrome. Intern Med. 2000;39:457–63. doi: 10.2169/internalmedicine.39.457. [DOI] [PubMed] [Google Scholar]
- 20.Kronbichler A, Mayer G. Renal involvement in autoimmune connective tissue diseases. BMC Med. 2013;11:95. doi: 10.1186/1741-7015-11-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ardiles L, Ramirez P, Calderon S, Aguirre V, Poblete MT. Life-threatening hypokalemic paralysis and hypophosphatemic myopathy as initial presentations of primary Sjogren's syndrome. J Clin Rheumatol. 2001;7:410–1. doi: 10.1097/00124743-200112000-00015. [DOI] [PubMed] [Google Scholar]
- 22.Bridoux F, Kyndt X, Abou-Ayache R, Mougenot B, Baillet S, Bauwens M, et al. Proximal tubular dysfunction in primary Sjogren's syndrome: a clinicopathological study of 2 cases. Clin Nephrol. 2004;61:434–9. doi: 10.5414/CNP61434. [DOI] [PubMed] [Google Scholar]
- 23.Celik G, Ozturk E, Ipekci SH, Yilmaz S, Colkesen F, Baldane S, et al. An uncommon presentation of Sjogren's syndrome and brucellosis. Transfus Apher Sci. 2014;51:77–80. doi: 10.1016/j.transci.2014.03.011. [DOI] [PubMed] [Google Scholar]
- 24.Kamm DE, Fischer MS. Proximal renal tubular acidosis and the Fanconi syndrome in a patient with hypergammaglobulinemia. Nephron. 1972;9:208–19. doi: 10.1159/000180152. [DOI] [PubMed] [Google Scholar]
- 25.Kobayashi T, Muto S, Nemoto J, Miyata Y, Ishiharajima S, Hironaka M, et al. Fanconi's syndrome and distal (type 1) renal tubular acidosis in a patient with primary Sjogren's syndrome with monoclonal gammopathy of undetermined significance. Clin Nephrol. 2006;65:427–32. doi: 10.5414/CNP65427. [DOI] [PubMed] [Google Scholar]
- 26.Matsumura R, Kondo Y, Sugiyama T, Sueishi M, Koike T, Takabayashi K, et al. Immunohistochemical identification of infiltrating mononuclear cells in tubulointerstitial nephritis associated with Sjogren's syndrome. Clin Nephrol. 1988;30:335–40. [PubMed] [Google Scholar]
- 27.Nakamura H, Kita J, Kawakami A, Yamasaki S, Ida H, Sakamoto N, et al. Multiple bone fracture due to Fanconi's syndrome in primary Sjogren's syndrome complicated with organizing pneumonia. Rheumatol Int. 2009;30:265–7. doi: 10.1007/s00296-009-0924-5. [DOI] [PubMed] [Google Scholar]
- 28.Ram R, Swarnalatha G, Ashok KK, Madhuri HR, Dakshinamurty KV. Fanconi syndrome following honeybee stings. Int Urol Nephrol. 2012;44:315–8. doi: 10.1007/s11255-010-9855-z. [DOI] [PubMed] [Google Scholar]
- 29.Shearn MA, Tu WH. Nephrogenic diabetic insipidus and other defects of renal tubular function in Sjoergren's syndrome. Am J Med. 1965;39:312–8. doi: 10.1016/0002-9343(65)90057-4. [DOI] [PubMed] [Google Scholar]
- 30.Walker BR, Alexander F, Tannenbaum PJ. Fanconi syndrome with renal tubular acidosis and light chain proteinuria. Nephron. 1971;8:103–7. doi: 10.1159/000179912. [DOI] [PubMed] [Google Scholar]
- 31.Yang YS, Peng CH, Sia SK, Huang CN. Acquired hypophosphatemia osteomalacia associated with Fanconi's syndrome in Sjogren's syndrome. Rheumatol Int. 2007;27:593–7. doi: 10.1007/s00296-006-0257-6. [DOI] [PubMed] [Google Scholar]
- 32.Ren H, Wang WM, Chen XN, Zhang W, Pan XX, Wang XL, et al. Renal involvement and followup of 130 patients with primary Sjogren's syndrome. J Rheumatol. 2008;35:278–84. [PubMed] [Google Scholar]
- 33.Shi M, Chen L. Sjogren's syndrome complicated with Fanconi syndrome and Hashimoto's thyroiditis: case report and literature review. J Int Med Res. 2016;44(3): 753-9. [DOI] [PMC free article] [PubMed]
- 34.Saeki T, Nakajima A, Ito T, Takata T, Imai N, Yoshita K, et al. Tubulointerstitial nephritis and Fanconi syndrome in a patient with primary Sjogren's syndrome accompanied by antimitochondrial antibodies: a case report and review of the literature. Mod Rheumatol. 2016;4:1–4. (Epubahead of print). [DOI] [PubMed]
- 35.Kong DH, Gao H, Qiu MC. Sjogren's syndrome, renal tubular acidosis and Fanconi syndrome—a case report. Zhonghua Yi Xue Za Zhi. 2005;85:878. [PubMed] [Google Scholar]
- 36.Christensen EI, Birn H, Storm T, Weyer K, Nielsen R. Endocytic receptors in the renal proximal tubule. Physiology (Bethesda) 2012;27:223–36. doi: 10.1152/physiol.00022.2012. [DOI] [PubMed] [Google Scholar]
- 37.Gburek J, Verroust PJ, Willnow TE, Fyfe JC, Nowacki W, Jacobsen C, et al. Megalin and cubilin are endocytic receptors involved in renal clearance of hemoglobin. J Am Soc Nephrol. 2002;13:423–30. doi: 10.1681/ASN.V132423. [DOI] [PubMed] [Google Scholar]
- 38.Kozyraki R, Fyfe J, Verroust PJ, Jacobsen C, Dautry-Varsat A, Gburek J, et al. Megalin-dependent cubilin-mediated endocytosis is a major pathway for the apical uptake of transferrin in polarized epithelia. Proc Natl Acad Sci U S A. 2001;98:12491–6. doi: 10.1073/pnas.211291398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Leheste JR, Rolinski B, Vorum H, Hilpert J, Nykjaer A, Jacobsen C, et al. Megalin knockout mice as an animal model of low molecular weight proteinuria. Am J Pathol. 1999;155:1361–70. doi: 10.1016/S0002-9440(10)65238-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gaide Chevronnay HP, Janssens V, Van Der Smissen P, N'Kuli F, Nevo N, Guiot Y, et al. Time course of pathogenic and adaptation mechanisms in cystinotic mouse kidneys. J Am Soc Nephrol. 2014;25:1256–69. doi: 10.1681/ASN.2013060598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pober BR, Longoni M, Noonan KM. A review of Donnai-Barrow and facio-oculo-acoustico-renal (DB/FOAR) syndrome: clinical features and differential diagnosis. Birth Defects Res A Clin Mol Teratol. 2009;85:76–81. doi: 10.1002/bdra.20534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Norden AG, Lapsley M, Igarashi T, Kelleher CL, Lee PJ, Matsuyama T, et al. Urinary megalin deficiency implicates abnormal tubular endocytic function in Fanconi syndrome. J Am Soc Nephrol. 2002;13:125–33. doi: 10.1681/ASN.V131125. [DOI] [PubMed] [Google Scholar]
- 43.Santo Y, Hirai H, Shima M, Yamagata M, Michigami T, Nakajima S, et al. Examination of megalin in renal tubular epithelium from patients with Dent disease. Pediatr Nephrol. 2004;19:612–5. doi: 10.1007/s00467-004-1445-9. [DOI] [PubMed] [Google Scholar]
- 44.Wilmer MJ, Emma F, Levtchenko EN. The pathogenesis of cystinosis: mechanisms beyond cystine accumulation. Am J Physiol Renal Physiol. 2010;299:F905–16. doi: 10.1152/ajprenal.00318.2010. [DOI] [PubMed] [Google Scholar]
- 45.Li M, Balamuthusamy S, Simon EE, Batuman V. Silencing megalin and cubilin genes inhibits myeloma light chain endocytosis and ameliorates toxicity in human renal proximal tubule epithelial cells. Am J Physiol Renal Physiol. 2008;295:F82–90. doi: 10.1152/ajprenal.00091.2008. [DOI] [PubMed] [Google Scholar]
- 46.Hall AM, Bass P, Unwin RJ. Drug-induced renal Fanconi syndrome. QJM. 2014;107:261–9. doi: 10.1093/qjmed/hct258. [DOI] [PubMed] [Google Scholar]
- 47.Schreiber A, Theilig F, Schweda F, Hocherl K. Acute endotoxemia in mice induces downregulation of megalin and cubilin in the kidney. Kidney Int. 2012;82:53–9. doi: 10.1038/ki.2012.62. [DOI] [PubMed] [Google Scholar]
- 48.Gu C, Wu L, Li X. IL-17 family: cytokines, receptors and signaling. Cytokine. 2013;64:477–85. doi: 10.1016/j.cyto.2013.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kwok SK, Lee J, Yu D, Kang KY, Cho M, Kim HR, et al. A pathogenetic role for IL-21 in primary Sjogren syndrome. Nat Rev Rheumatol. 2015;11:368–74. doi: 10.1038/nrrheum.2014.225. [DOI] [PubMed] [Google Scholar]
- 50.Pitzalis C, Jones GW, Bombardieri M, Jones SA. Ectopic lymphoid-like structures in infection, cancer and autoimmunity. Nat Rev Immunol. 2014;14:447–62. doi: 10.1038/nri3700. [DOI] [PubMed] [Google Scholar]
- 51.GeurtsvanKessel CH, Willart MA, Bergen IM, van Rijt LS, Muskens F, Elewaut D, et al. Dendritic cells are crucial for maintenance of tertiary lymphoid structures in the lung of influenza virus-infected mice. J Exp Med. 2009;206:2339–49. doi: 10.1084/jem.20090410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Muniz LR, Pacer ME, Lira SA, Furtado GC. A critical role for dendritic cells in the formation of lymphatic vessels within tertiary lymphoid structures. J Immunol. 2011;187:828–34. doi: 10.4049/jimmunol.1004233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Veiga-Fernandes H, Coles MC, Foster KE, Patel A, Williams A, Natarajan D, et al. Tyrosine kinase receptor RET is a key regulator of Peyer's patch organogenesis. Nature. 2007;446:547–51. doi: 10.1038/nature05597. [DOI] [PubMed] [Google Scholar]
- 54.Peters A, Pitcher LA, Sullivan JM, Mitsdoerffer M, Acton SE, Franz B, et al. Th17 cells induce ectopic lymphoid follicles in central nervous system tissue inflammation. Immunity. 2011;35:986–96. doi: 10.1016/j.immuni.2011.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Halle S, Dujardin HC, Bakocevic N, Fleige H, Danzer H, Willenzon S, et al. Induced bronchus-associated lymphoid tissue serves as a general priming site for T cells and is maintained by dendritic cells. J Exp Med. 2009;206:2593–601. doi: 10.1084/jem.20091472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sakai A, Sugawara Y, Kuroishi T, Sasano T, Sugawara S. Identification of IL-18 and Th17 cells in salivary glands of patients with Sjogren's syndrome, and amplification of IL-17-mediated secretion of inflammatory cytokines from salivary gland cells by IL-18. J Immunol. 2008;181:2898–906. doi: 10.4049/jimmunol.181.4.2898. [DOI] [PubMed] [Google Scholar]
- 57.Fei Y, Zhang W, Lin D, Wu C, Li M, Zhao Y, et al. Clinical parameter and Th17 related to lymphocytes infiltrating degree of labial salivary gland in primary Sjogren's syndrome. Clin Rheumatol. 2014;33:523–9. doi: 10.1007/s10067-013-2476-z. [DOI] [PubMed] [Google Scholar]
- 58.Chang A, Henderson SG, Brandt D, Liu N, Guttikonda R, Hsieh C, et al. In situ B cell-mediated immune responses and tubulointerstitial inflammation in human lupus nephritis. J Immunol. 2011;186:1849–60. doi: 10.4049/jimmunol.1001983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rangel-Moreno J, Hartson L, Navarro C, Gaxiola M, Selman M, Randall TD. Inducible bronchus-associated lymphoid tissue (iBALT) in patients with pulmonary complications of rheumatoid arthritis. J Clin Invest. 2006;116:3183–94. doi: 10.1172/JCI28756. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


