Abstract
Background
Two=dimensional motion analysis of lower=extremity movement typically focuses on the knee frontal plane projection angle, which considers the position of the femur and the tibia. A measure that includes the pelvis may provide a more comprehensive and accurate indicator of lower=extremity movement.
Hypothesis/Purpose: The purpose of the study was to describe the utility of a two=dimensional dynamic valgus index (DVI) in females with patellofemoral pain. The hypothesis was that the DVI would be more reliable and valid than the knee frontal plane projection angle, be greater in females with patellofemoral pain during a single=limb squat than in females without patellofemoral pain, and decrease in females with patellofemoral pain following instruction.
Study Design: Controlled Laboratory Study
Methods
Data were captured while participants performed single limb squats under two conditions: usual and corrected. Two=dimensional hip and knee angles and a DVI that combined the hip and knee angles were calculated. Three=dimensional sagittal, frontal, and transverse plane angles of the hip and knee and a DVI combining the frontal and transverse plane angles were calculated.
Results
The two=dimensional DVI demonstrated moderate reliability (ICC=0.74). The correlation between the two=dimensional and three=dimensional DVI's was 0.635 (p<0001). Females with patellofemoral pain demonstrated a greater two=dimensional DVI (31.14 °±13.36 °) than females without patellofemoral pain (18.30 °±14.97 °; p=0.010). Females with patellofemoral pain demonstrated a decreased DVI in the corrected (19.04 °±13.70 °) versus usual (31.14 °±13.36 °) condition (p=0.001).
Conclusion
The DVI is a reliable and valid measure that may provide a more comprehensive assessment of lower=extremity movement patterns than the knee frontal plane projection angle in individuals with lower=extremity musculoskeletal pain problems.
Level of Evidence
2b
Keywords: Frontal plane projection angle, movement, rehabilitation
INTRODUCTION
Lower-extremity musculoskeletal pain problems, including anterior cruciate ligament injuries, iliotibial band friction syndrome, and patellofemoral pain (PFP) may be associated with faulty movement patterns of the hip and knee.1 For this reason, movement patterns and the effect of movement retraining have been investigated, most often with three-dimensional (3D) motion analysis. Two-dimensional (2D) motion analysis, however, has become a more commonly utilized tool for answering clinical questions as it is cost-effective, available to clinicians, and less time intensive than 3D motion analysis. The reliability of 2D measures also has been reported to be acceptable with reliability values ranging from 0.59 to 0.98 depending on the 2D method, task analyzed, and type of reliability reported.2-6
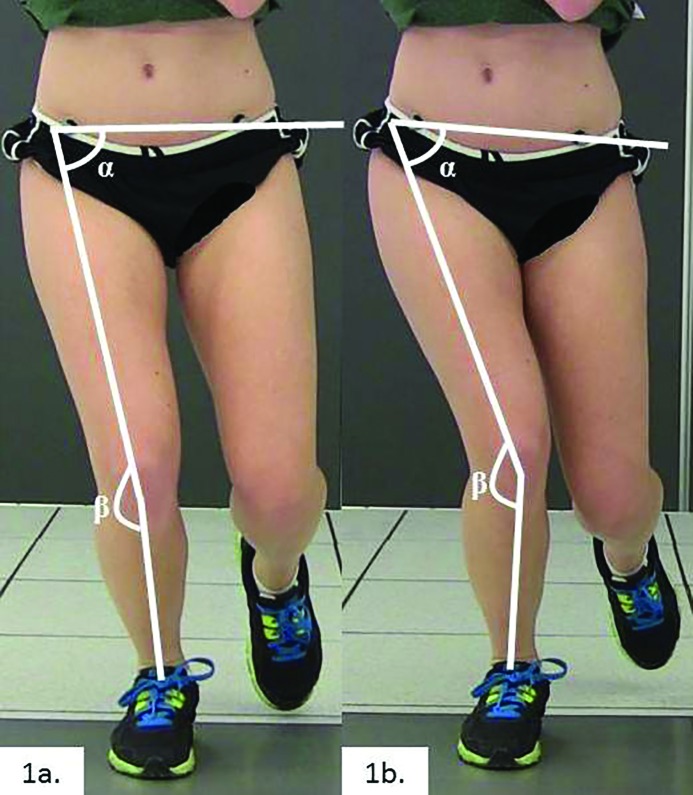
Three-dimensional and 2D motion analysis both have been utilized to assess an abnormal movement pattern often called dynamic knee valgus (Figure 1). Three-dimensional kinematic components of dynamic knee valgus have been quantified during single limb squat,7 providing insight into the contribution of hip adduction, hip medial rotation, knee adduction, and knee lateral rotation to the dynamic knee valgus movement pattern. Two-dimensional motion analysis, however, typically focuses solely on the knee using a knee frontal plane projection angle (FPPA; Figure 1).4,5,8-13 The knee FPPA visually appears to be knee abduction, although it is likely created by a combination of hip adduction, hip medial rotation, knee abduction, and knee lateral rotation that occurs during weight bearing knee flexion.13,14 The knee FPPA, while capturing the 2D orientation of the femur and tibia, may not accurately reflect the entire lower-extremity movement pattern, as 3D motion analysis does, because the pelvis’ contribution to the lower extremity movement pattern is not taken into account. Pelvic drop may contribute to a hip adducted position. Noehren et al15 reported a greater hip adduction position in individuals with iliotibial band friction syndrome, suggesting the adducted position led to increased tension on the lateral structures of the knee, resulting in pain. Takacs and Hunt16 and Dunphy et al17 reported increased knee adduction moments in individuals who demonstrated contralateral hip drop without concomitant ipsilateral trunk lean. A more adducted position of the hip or increased knee adduction moment may alter or increase the stress to the patellofemoral joint, thus contributing to PFP. Knowledge of the pelvis’ contribution to hip motion during a particular task may provide important information about different movement strategies used by individuals to accomplish a task. Furthermore, because people may present with varying degrees of hip and knee angles that contribute to the pain problem, a 2D variable that combines the hip and knee angles may be a more comprehensive representation of the entire lower-extremity movement pattern than the knee FPPA alone.
Figure 1.
Dynamic knee valgus two-dimensional angular measures. 1a. Hip frontal plane projection angle, calculated as 90 ° minus the angle (α) between the pelvis segment and the thigh segment. Knee frontal plane projection angle, calculated as 180 ° minus the angle (β) between the thigh segment and the shank segment. 1b. Example of individual demonstrating an observable dynamic knee valgus, resulting in increased hip and knee frontal plane projection angles and a larger dynamic valgus index.
To the authors’ knowledge, a hip and knee combined variable has not previously been reported. Therefore, the purpose of the current study was to describe the utility of a dynamic valgus index (DVI) in females with PFP. The authors hypothesized that the 2D DVI (1) would be more reliable and valid than the knee FPPA in the current study, (2) would be greater in females with PFP during a single-limb squat compared to females without PFP, and (3) would decrease in females with PFP following within-session verbal instruction. Identifying a 2D variable that is potentially more comprehensive, reliable, and valid than the knee FPPA may result in a measure that more accurately reflects the entire lower-extremity movement pattern and lead to better identification and treatment of lower-extremity movement impairments. Furthermore, demonstrating successful utility of a comprehensive 2D variable provides additional support for the use of 2D measures during clinical assessment and to answer clinical questions related to lower-extremity movement impairments in individuals with musculoskeletal pain problems, particularly active individuals.
METHODS
Participants
Twenty women with chronic PFP and 16 women without PFP participated. Chronic PFP was defined as pain located at the patellofemoral articulation (behind or around the patella) of at least two months duration.18 To be included in the study, average pain reported for the prior week had to be a minimum of 3/10 using a verbal pain rating scale (0 representing no pain, 10 representing severe pain). Pain also had to be reproduced by at least two of the following tests: resisted isometric quadriceps contraction performed with the knee in approximately 10 ° of flexion, squatting, prolonged sitting, and stair ascent or descent.19 Females with PFP also had to demonstrate observable dynamic knee valgus during single limb squat. Observable dynamic knee valgus was defined as a visual frontal plane knee angle increase of 10 ° or more during the decent phase of the single limb squat test.7,8 Females without PFP qualified for the study if they had no history or current report of PFP and did not demonstrate an observable dynamic knee valgus during a single-limb squat. Exclusion criteria for both groups included (1) body mass index greater than 30 kg/m2, (2) history of knee ligament, tendon, or cartilage injury; traumatic patellar dislocation; patellar instability; or prior knee surgery, (3) known pregnancy, and (4) neurological involvement that would influence balance and coordination during kinematic testing. Saint Louis University's Institutional Review Board approved the study protocol and informed consent. All federal and state regulations for the protection of human participants were followed, as were the guidelines of the Declaration of Helsinki. Prior to participation in the study, all participants read and signed the informed consent.
Kinematic Assessment
Two-dimensional and 3D data were captured simultaneously while participants completed single limb squats under two conditions: usual and corrected. Single limb squat was performed because it is often pain provoking and likely to induce dynamic knee valgus.13,20,21 Participants with PFP performed the squats on their involved limb. Participants without PFP were randomly assigned to perform the squat on their right or left leg. All participants completed trials using their usual method first. For the usual trials, participants were instructed to keep their trunk straight and arms at their side while bending their knee to at least 60 ° (visually confirmed by investigator). No additional instructions were given about the position of the knee relative to the hip or foot. During the corrected trials, participants repeated the single limb squat with additional instructions. Participants were instructed to “keep your knee over the middle of your foot (don't let your knee fall in”) during the descent phase of the squat. The corrected squat was demonstrated to the participants before they were allowed to practice the task. For both conditions, participants were allowed several practice trials prior to data collection to become comfortable with the task. Three trials were collected for the usual and corrected conditions; the average of three trials was used for data analysis.
Two-dimensional data were captured with a Sony DCR-HC96 Handycam camcorder (Sony Corporation of America, Park Ridge, NJ, USA). The camera was positioned at a height of 45 cm, 3 meters anterior to the participant. Data were processed with Dartfish ProSuite 7 (Dartfish, Switzerland). All 2D angles (Figure 1) were measured from a frontal plane view by one investigator blinded to condition. A line drawn between markers placed on the anterior superior iliac spines defined the pelvic segment. A line drawn from the midpoint of the knee, bisecting the thigh, defined the thigh segment. A line drawn from the midpoint of the knee to the midpoint of the ankle defined the shank segment. For each trial, hip and knee angles were obtained at peak knee flexion determined visually by the investigator. The knee FPPA angle was calculated as 180 ° minus the angle between the thigh segment and the shank segment (Figure 1a). A positive knee FPPA angle indicated apparent knee abduction. The hip FPPA was calculated as 90 ° minus the angle between the pelvis segment and the thigh segment (Figure 1a). A positive hip FPPA indicated apparent hip adduction. The 2D DVI was calculated as the sum of the hip and the knee FPPAs.
Three-dimensional data were captured with an 8-camera motional analysis system (Vicon, Oxford Metrics LTD. Oxford, England) sampled at 120 Hz. Data were captured and processed using previously described methods.7 Prior to data collection, reflective markers were placed over the second sacral vertebrae, bilateral iliac crests, anterior superior iliac spines, medial and lateral femoral epicondyles, medial and lateral malleoli, calcaneus, lateral midfoot, anterior midfoot, and 1st and 5th metatarsal heads. Thermoplastic shells with four reflective markers were placed on the lateral mid-thigh and lateral mid shanks. Data captured from these markers were processed using Visual3DTM software (C-Motion, Inc., Rockville, MD, USA). Marker trajectories were low-pass filtered using a 4th-order Butterworth filter with a 6 Hz cutoff frequency. A six degrees of freedom model incorporating the pelvis (CODA model, Charnwood Dynamics Ldt., UK), thigh, shank, and foot was used for data processing. Hip and knee angles in the sagittal, frontal, and transverse planes were calculated and expressed in the reference frame of the proximal segment. For each trial, hip and knee angles were obtained at peak knee flexion determined by the Visual3DTM software. The 3D DVI was the sum of hip and knee frontal and transverse plane angles, where hip adduction, hip medial rotation, knee abduction, and knee lateral rotation were considered positive values. The ICC3,1 (0.81-0.98) and SEM (1.0-3.5 °) values for the trial-to-trial variability of 3D hip and knee angles have been reported previously.7
STATISTICAL METHODS
Data were analyzed with IBM SPSS Statistics version 20 (SPSS, Chicago, IL, USA).
Intra-rater reliability of Dartfish measurements for repeated measures of hip and knee FPPAs completed a minimum of five days apart was assessed with intraclass correlation coefficients (ICC2,1). Inter-rater reliability of Dartfish measurements for hip and knee FPPAs, completed on a smaller sample by two individuals was assessed with intraclass correlation coefficients (ICC2,1).
Trial-to-trial within-session error for the 2D hip and knee FPPAs across the three trials was assessed by calculating ICC3,1 and standard error of the measure (standard deviation*√(1-ICC3,1)). Pearson product-moment correlation coefficients were calculated to examine concurrent validity between 2D and 3D variables captured during the usual condition. Independent samples t-tests were used to compare group differences in participant characteristics, peak knee flexion, knee FPPA, hip FPPA, and dynamic valgus indices in the usual condition. Paired t-tests were used to analyze differences between the usual condition and the corrected condition in participants with PFP. The alpha level was set at 0.05 for all statistical tests.
RESULTS
There were no group differences in age (mean ± SD; PFP: 22.4 ± 4.3 years, no PFP: 21.6 ± 3.0 years; P = 0.544), BMI (mean ± SD; PFP: 22.4 ± 3.2 kg/m2, no PFP: 22.7 ± 2.8 kg/m2; P = 0.678), or angle of peak knee flexion during the usual condition (mean ± SD; PFP: 70.0 ° ± 7.49 °, no PFP: 68.3 ° ± 6.6 °; P = 0.484). There also was no difference in peak knee flexion between conditions in females with PFP (mean ± SD; usual: 70.0 ° ± 7.49 °, corrected: 66.9 ° ± 8.5 °; P = 0.86).
Reliability
The intra-rater reliability ICC2,1 of Dartfish measurements for repeated measures of hip and knee FPPAs completed a minimum of five days apart was 0.99. The inter-rater reliability ICC2,1 of Dartfish measurements for hip and knee FPPAs, completed on a smaller sample by two individuals was 0.97 for the hip FPPA and 0.99 for the knee FPPA. Trial-to-trial within-session variability ICC3,1 values ranged from 0.68-0.83 (Knee FPPA: 0.68, DVI: 0.74, Hip FPPA: 0.83) for 2D measures in the usual condition with standard error of the measures ranging from 3.29 ° to 8.63 ° (Table 1).
TABLE 1.
Intraclass correlation coefficients for trial-to-trial variability, and standard error of the measure for two-dimensional hip and knee variables.
| ICC2,1 | SEM | |
|---|---|---|
| Hip frontal plane projection angle | 0.83 | 3.29 ° |
| Knee frontal plane projection angle | 0.68 | 5.80 ° |
| Dynamic valgus index | 0.74 | 8.63 ° |
ICC = intraclass correlation coefficient; SEM = standard error of the measure
Concurrent validity
The 2D measures of hip and knee kinematics demonstrated fair to excellent concurrent validity22 when compared to 3D kinematic measures (Table 2). The 2D DVI was positively correlated with 3D hip adduction, hip medial rotation, knee lateral rotation, and the 3D DVI. The hip and knee FPPAs were positively correlated with 3D hip adduction, 3D knee lateral rotation, and the 3D DVI. The correlations between the 2D DVI and all of the 3D variables were greater than the correlations between the knee FPPA and the 3D variables.
TABLE 2.
Correlations between two-dimensional and three-dimesional variables in the usual condition.
| Hip FPPA | Knee FPPA | 2D DVI | |
|---|---|---|---|
| 3D Hip Adduction | 0.825‡ | 0.419* | 0.661‡ |
| 3D Hip Medial Rotation | 0.313 | 0.303 | 0.336* |
| 3D Knee Abduction | 0.250 | 0.036 | 0.103 |
| 3D Knee Lateral Rotation | 0.415* | 0.365* | 0.425* |
| 3D DVI | 0.627‡ | 0.541† | 0.635‡ |
FPPA = frontal plane projection angle, 2D = two-dimensional, DVI = dynamic valgus index
*p<0.05, †p<0.01, ‡p<0.001
Comparison between groups
Females with PFP demonstrated a greater 2D DVI (mean ± SD; 31.14 ° ± 13.36 °) than females without PFP (mean ± SD;18.30 ° ± 14.97 °; P = 0.010; Table 3). Females with PFP also demonstrated a greater 3D DVI (mean ± SD; 12.41 ° ± 9.77 °) than females without PFP (mean ± SD; 1.81 ° ± 13.44 °; P=0.010; Table 3). The components of the 2D DVI also were different between groups. Females with PFP demonstrated a greater hip FPPA (mean ± SD; 19.66 ° ± 7.70 °) than females without PFP (mean ± SD; 14.15 ° ± 6.53 °; P = 0.030; Table3). Females with PFP also demonstrated a greater knee FPPA (mean ± SD; 11.48 ° ± 7.45 °) than females without PFP (mean ± SD; 4.14 ° ± 9.62 °; P = 0.014; Table 3).
TABLE 3.
Between groups and between conditions comparisons for two-dimensional kinematic variables.
| Females without PFP, Usual Condition* | Females with PFP, Usual Condition* | Females with PFP, Corrected Condition* | Comparison between females with and without PFP† | Comparison between conditions in females with PFP‡ | |
|---|---|---|---|---|---|
| Hip FPPA | 14.15 ° ± 6.53 ° | 19.66 ° ± 7.70 ° | 14.48 ° ± 7.48 ° | 5.51 °(0.59 ° to 10.41 °) p = 0.030 | 5.18 °(2.30 ° to 7.35 °) p < 0.001 |
| Knee FPPA | 4.14 ° ± 9.62 ° | 11.48 ° ± 7.45 ° | 4.56 ° ± 7.48 ° | 7.34 °(1.56 ° to 13.12 °) p = 0.014 | 6.92 °(2.61 ° to 11.23 °) p = 0.003 |
| 2D DVI | 18.30 ° ± 14.97 ° | 31.14 ° ± 13.36 ° | 19.04 ° ± 13.70 ° | 12.84 °(3.23 ° to 22.44 °) p = 0.010 | 12.10 °(5.97 ° to 18.23 °) p = 0.001 |
| 3D DVI | 1.81 ° ± 13.44 ° | 12.41 ° ± 9.77 ° | 6.15 ° ± 12.00 ° | 10.59 °(2.73 ° to 18.45 °) p = 0.010 | 6.26 ° (2.35 ° to 10.16 °) p = 0.003 |
FPPA = frontal plane projection angle; 2D = two-dimensional; 3D = three-dimensional; DVI = dynamic valgus index; PFP = patellofemoral pain
Data presented as mean ± SD
Data presented as mean group difference (95% confidence interval)
Data presented as mean difference between conditions (95% confidence interval)
Comparison between conditions
Females with PFP demonstrated decreased dynamic valgus indices (mean ± SD; 2D DVI Usual Condition: 31.14 ° ± 13.36 °, Corrected Condition: 19.04 ° ± 13.70 °; P = 0.001), as well as hip (mean ± SD; Usual Condition: 19.66 ° ± 7.70 °, Corrected Condition: 14.48 ° ± 7.48 °; P < 0.001) and knee FPPAs (mean ± SD; Usual Condition: 11.48 ° ± 7.45 °, Corrected Condition: 4.56 ° ± 7.48 °; P=0.003) following verbal instruction (Table 3). Females without PFP did complete the corrected trials. However, because they did not demonstrate observable dynamic knee valgus during single-leg squat, it was not expected the movement would change with cuing. Consistent with this hypothesis, there was no statistically significant change in any of the variables in females without PFP (p > 0.05 for all comparisons).
DISCUSSION
The purpose of the current study was to describe the utility of a DVI in females with PFP. The authors hypothesized that the 2D DVI (1) would be more reliable and valid than the knee FPPA, (2) would be greater in females with PFP during a single-limb squat compared to females without PFP, and (3) would decrease in females with PFP following within-session verbal instruction. The results of the current study suggest the DVI may be an important variable to consider when examining lower-extremity movement patterns.
The DVI is a reliable and valid measure. The DVI demonstrated moderate trial-to-trial reliability, consistent with, or better than reliability of the knee FPPA reported previously in the literature and in the current study.4-6 Willson et al6 reported within-day reliability of the knee FPPA to be 0.88 during a single limb squat. Munro et al5 reported ICC values between 0.59 and 0.88 for the knee FPPA during different lower extremity tasks; the ICC value for single limb squat in females was reported to be 0.59. Using similar methods for measuring the knee FPPA, Herrington4 reported a reliability of 0.72 for the knee FPPA during a single limb squat.
The concurrent validity of the DVI during single limb squat also was consistent with or better than the concurrent validity of the knee FPPA reported in the current study and previously in the literature, when using similar methods.13 Willson et al13 reported correlations between the 2D knee FPPA and 3D segmental rotations of the pelvis, femur, and tibia to range between 0.01 and 0.61. The highest correlation reported by Willson et al13 was between the knee FPPA and the femoral adduction. This is consistent with the current study where the highest correlation between the 2D DVI and a 3D variable also was hip adduction.
Females with PFP demonstrated a greater 2D DVI than females without PFP. Females with PFP also demonstrated a greater knee FPPA than females without PFP, consistent with the findings of Willson et al,13 who reported a 4.1 ° difference in the knee FPPA between females with and females without PFP. The knee FPPA, however, does not capture the position of the pelvis, thus does not capture all movement that potentially contributes to stress at the knee. Pelvic position, however, could contribute to additional stress at the knee through different mechanisms. First, contralateral pelvic drop may increase lateral tension on the structures of the knee via the stretch of the tensor fascia latae/iliotibial band across the hip and knee.15 Noehren et al15 reported individuals with iliotibial band friction syndrome demonstrated greater hip adduction during the stance phase of running, suggesting the adducted hip position led to increased tension on lateral structures of the knee, resulting in pain. Similarly, an adducted position of the hip could result in tension on the lateral structures of the knee, affecting patellar alignment, leading to PFP. Second, contralateral pelvic drop without concomitant ipsilateral trunk lean results in a medial shift of the line of gravity, which increases the knee adductor moment.1,16,17 Takacs and Hunt16 and Dunphy et al17 reported increased knee adduction moments in individuals who demonstrate contralateral hip drop without concomitant ipsilateral trunk lean when compared to individuals who do not demonstrate contralateral hip drop. The increase in knee adduction moment may alter the stress distribution on the patellofemoral joint, potentially contributing to PFP. Assessment of the DVI, which captures positioning of the tibia, femur, and pelvis, may provide important, comprehensive information about different movement strategies used to accomplish a task and contribute to the pain problem.
Females with PFP also demonstrated a decrease in the DVI following verbal instruction targeting the knee position. Prior to the current study, the ability of 2D measures to detect change in multi-joint movement patterns in females with PFP was unclear. Olson et al.10 reported that 2D methods were sensitive enough to detect changes in the knee FPPA following a 4-week neuromuscular retraining program. However, only healthy females were examined and only the knee FPPA was quantified. The current study, which detected changes in hip and knee FPPAs, as well as the 2D DVI in females with PFP following verbal instruction confirms the potential for 2D methods to be used as a research and clinical tool to examine changes in both hip and knee movement patterns in clinical populations. Both the hip and knee FPPAs decreased following instruction, but, consistent with the instruction provided, there was a greater decrease in the knee FPPA than the hip FPPA. Additional instruction targeting pelvic position may result in a greater decrease in the DVI. Further research is necessary to explore cuing of the pelvis and knee when the faulty movement pattern includes poor pelvic position.
The current study has limitations. The 2D data was captured as part of a larger 3D study; the methods for 2D motion capture may have been less precise resulting in increased error. Better positioning of the camera for 2D data collection would likely decrease some error. In the current study, however any error created by camera placement was systematic across all participants. A second limitation is that the current data is from a small sample of females performing the single-limb squat. The information may not be generalizable to a larger sample of a different population or task. Further research is necessary to explore the importance of examining the DVI with other tasks and populations.
CONCLUSION
The DVI combines 2D motion analysis of the hip and the knee, creating a more comprehensive 2D assessment of lower-extremity movement than the 2D knee FPPA alone. The DVI is reliable, valid, can discriminate between groups, and is sensitive to change. The successful utility of the DVI in the current study provides additional support for the use of 2D measures during clinical assessment and to answer clinical questions related to lower-extremity movement impairments in individuals with musculoskeletal pain problems, particularly active individuals.
REFERENCES
- 1.Powers CM. The influence of abnormal hip mechanics on knee injury: a biomechanical perspective. J Orthop Sports Phys Ther. 2010;40:42-51. [DOI] [PubMed] [Google Scholar]
- 2.Mizner RL Chmielewski TL Toepke JJ, et al. Comparison of 2-dimensional measurement techniques for predicting knee angle and moment during a drop vertical jump. Clin J Sport Med. 2012;22:221-227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Miller A Callister R. Reliable lower limb musculoskeletal profiling using easily operated, portable equipment. Phys Ther Sport. 2009;10:30-37. [DOI] [PubMed] [Google Scholar]
- 4.Herrington L. Knee valgus angle during single leg squat and landing in patellofemoral pain patients and controls. Knee. 2014;21:514-517. [DOI] [PubMed] [Google Scholar]
- 5.Munro A Herrington L Carolan M. Reliability of 2-dimensional video assessment of frontal-plane dynamic knee valgus during common athletic screening tasks. J Sport Rehabil. 2012;21:7-11. [DOI] [PubMed] [Google Scholar]
- 6.Willson JD Ireland ML Davis I. Core strength and lower extremity alignment during single leg squats. Med Sci Sports Exerc. 2006;38:945-952. [DOI] [PubMed] [Google Scholar]
- 7.Salsich GB Graci V Maxam DE. The effects of movement pattern modification on lower extremity kinematics and pain in women with patellofemoral pain. J Orthop Sports Phys Ther. 2012;42:1017-1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harris-Hayes M Steger-May K Koh C, et al. Classification of lower extremity movement patterns based on visual assessment: reliability and correlation with 2-dimensional video analysis. J Athl Train. 2014;49:304-310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hollman JH Ginos BE Kozuchowski J, et al. Relationships between knee valgus hip-muscle strength, and hip-muscle recruitment during a single-limb step-down. J Sport Rehabil. 2009;18:104-117. [DOI] [PubMed] [Google Scholar]
- 10.Olson TJ Chebny C Willson JD, et al. Comparison of 2D and 3D kinematic changes during a single leg step down following neuromuscular training. Phys Ther Sport. 2011;12:93-99. [DOI] [PubMed] [Google Scholar]
- 11.Stensrud S Myklebust G Kristianslund E, et al. Correlation between two-dimensional video analysis and subjective assessment in evaluating knee control among elite female team handball players. Br J Sports Med. 2011;45:589-595. [DOI] [PubMed] [Google Scholar]
- 12.Whatman C Hume P Hing W. The reliability and validity of physiotherapist visual rating of dynamic pelvis and knee alignment in young athletes. Phys Ther Sport. 2013;14:168-174. [DOI] [PubMed] [Google Scholar]
- 13.Willson JD Davis IS. Utility of the frontal plane projection angle in females with patellofemoral pain. J Orthop Sports Phys Ther. 2008;38:606-615. [DOI] [PubMed] [Google Scholar]
- 14.McLean SG Walker K Ford KR, et al. Evaluation of a two dimensional analysis method as a screening and evaluation tool for anterior cruciate ligament injury. Br J Sports Med. 2005;39:355-362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Noehren B Davis I Hamill J. ASB clinical biomechanics award winner 2006 prospective study of the biomechanical factors associated with iliotibial band syndrome. Clinical biomechanics (Bristol, Avon). 2007;22:951-956. [DOI] [PubMed] [Google Scholar]
- 16.Takacs J Hunt MA. The effect of contralateral pelvic drop and trunk lean on frontal plane knee biomechanics during single limb standing. J Biomech. 2012;45:2791-2796. [DOI] [PubMed] [Google Scholar]
- 17.Dunphy C Casey S Lomond A, et al. Contralateral pelvic drop during gait increases knee adduction moments of asymptomatic individuals. Hum Mov Sci. 2016;49:27-35. [DOI] [PubMed] [Google Scholar]
- 18.Kannus P Natri A Paakkala T et al. An outcome study of chronic patellofemoral pain syndrome. Seven-year follow-up of patients in a randomized, controlled trial. J Bone Joint Surg Am. 1999;81:355-363. [DOI] [PubMed] [Google Scholar]
- 19.McConnell J. The management of chondromalacia patellae: a long term solution. Aust J Physiother. 1986;32:215-223. [DOI] [PubMed] [Google Scholar]
- 20.Souza RB Draper CE Fredericson M, et al. Femur rotation and patellofemoral joint kinematics: a weight-bearing magnetic resonance imaging analysis. J Orthop Sports Phys Ther. 2010;40:277-285. [DOI] [PubMed] [Google Scholar]
- 21.Willson JD Davis IS. Lower extremity mechanics of females with and without patellofemoral pain across activities with progressively greater task demands. Clin Biomech. 2008;23:203-211. [DOI] [PubMed] [Google Scholar]
- 22.Portney LG Watkins MP. Foundations of Clinical Research: Applications to Practice. Vol 2nd. Upper Saddle River, NJ: Prentice Hall Health; 2010. [Google Scholar]