Abstract
Background
Muscular weakness of the shoulder complex is commonly found in patients presenting with scapular dyskinesis; however, little is known regarding muscular performance in healthy individuals with scapular dyskinesis.
Purpose
To compare isometric strength measures of the shoulder complex between healthy individuals with and without scapular dyskinesis. It was hypothesized that healthy individuals with scapular dyskinesis would demonstrate decreased isometric strength of the scapular stabilizers and rotator cuff when compared to healthy individuals without scapular dyskinesis.
Study Design
Cross-sectional study.
Methods
Forty healthy, college-aged participants were recruited. Sixty-eight percent of subjects (27 of 40) presented with scapular dyskinesis. Thus, a matched-pairs analysis was conducted with 26 subjects (age: 22.00 ± 2.06 y; height: 168.77 ± 8.07 cm; mass: 70.98 ± 13.14 kg; BMI: 24.75 ± 3.04 kg/m2; 6 males; 20 females). The presence of scapular dyskinesis was determined visually using the scapular dyskinesis test with a dichotomous outcome (yes/no). Strength of the scapular stabilizers and rotator cuff was assessed via manual muscle testing using a handheld dynamometer. Force measures obtained with the handheld dynamometer were used to quantify strength. For each muscle tested, the mean peak force of three trials were normalized to body weight and used for data analysis. Additionally, strength ratios were calculated and analyzed. Differences in strength and strength ratios between those with and without scapular dyskinesis were compared using separate two-way mixed ANOVAs with repeated measures.
Results
No significant differences for either strength (F1.83,43.92 = 1.10, p = .34) or strength ratios (F1.83,44.02 = 1.93, p = .16) were observed between those with and without scapular dyskinesis. A significant main effect (F1.83,43.92 = 239.32, p < .01) for muscles tested was observed, and post-hoc analysis revealed significant trends resulting in a generalized order: the upper trapezius generated the greatest amount of force, followed by serratus anterior and middle trapezius, lower trapezius, supraspinatus, medial rotators, and lateral rotators.
Conclusion
The results of this study indicate that differences in shoulder muscle strength do not exist between healthy subjects with and without scapular dyskinesis. Additionally, scapular dyskinesis appears to be prevalent in healthy populations.
Level of Evidence
Level 3
Keywords: Muscular performance, rotator cuff, scapular dysfunction, scapular stabilizers, shoulder
INTRODUCTION
Musculoskeletal disorders of the shoulder complex are common among the general population and those who participate in overhead sports. Incidence rates for shoulder pain in the general population are between 0.9 – 2.5% with a lifetime prevalence between 6.7-66.7%.1 The frequency of shoulder pain is much higher in those individuals participating in overhead sports.2-4 As such, the socioeconomic impact can be quite substantial. In fact, direct health care expenditures associated with treatment of shoulder dysfunction in the year 2000 totaled $7 billion.5
The occurrence of shoulder pain has been linked to scapular dysfunction.6-8 Scapular dyskinesis is used to describe aberrant movement patterns of the scapula, which may serve as a potential source of impairment to normal shoulder function.8 It is common to find scapular dyskinesis associated with a variety of shoulder pathologies including, but not limited to, impingement, rotator cuff tears, labral pathology, acromioclavicular separations, and multidirectional instability of the glenohumeral joint.8 However, it is increasingly apparent that scapular dyskinesis exists in healthy populations as well.9-11 Therefore, the question remains as to whether scapular dyskinesis predisposes an individual to injury. Unfortunately, conflicting evidence exists among prospective studies regarding whether scapular dyskinesis is a causative factor for upper extremity injury.9,12-14
While the amount of research on the role of the scapula continues to increase, the exact cause for the development of scapular dyskinesis is not fully understood. There are several probable causes including, bony pathology (e.g., clavicular fracture), joint pathology (e.g., acromioclavicular separation), neurological pathology (e.g., long thoracic nerve palsy), soft tissue inflexibility (e.g., pectoralis minor tightness), and decreased muscle performance (e.g., altered activation patterns or strength deficits).7,8 Decreased muscle performance of the scapulothoracic musculature has been linked to altered shoulder kinematics,15,16 which may predispose an individual to injury.17,18 Thus, rehabilitation programs have been suggested to focus on improving the performance of the rotator cuff and scapular stabilizers.7,8,19-23
Clinicians may benefit from collecting shoulder strength data to better identify those with scapular dyskinesis who would benefit from a rehabilitation program focused on improving muscle performance. These data can easily be collected with a handheld dynamometer given that it is cost-effective, reliable, and valid.24,25 Normative strength data, including antagonist ratios, exists for the rotator cuff26 and scapular stabilizers27 in healthy populations. Others have reported strength profiles of the shoulder in healthy overhead athletes.28,29 While these studies included only healthy participants, none of these studies controlled for the presence of scapular dyskinesis. Those studies that have controlled for scapular dyskinesis have revealed rotator cuff weakness.22,23,30-32 However, it is important to note that these studies delimited the scapular dyskinesis groups with only symptomatic participants.22,23,30-32 In addition, authors have speculated that weakness of the scapular stabilizers exists in those with scapular dyskinesis based on studies examining electromyographic activity, or comparing strength data in those with and without shoulder impingement.6-8
Currently, only one study has directly compared strength measures between groups with and without scapular dyskinesis in a population of asymptomatic overhead athletes.10 While significant weakness of the lower trapezius was demonstrated in the scapular dyskinesis group, the authors limited their strength measurements to only the lower trapezius and serratus anterior.10 Additional studies are needed that examine strength data of the scapular stabilizers and rotator cuff to gain a better understanding of the clinical relevance of scapular dyskinesis, as well as providing additional means to diagnose, monitor, and measure patient outcomes during the rehabilitation process. Therefore, the primary aim of this study was to compare strength measures of the shoulder complex between healthy individuals with and without scapular dyskinesis. It was hypothesized that healthy individuals with scapular dyskinesis would demonstrate decreased strength when compared to healthy individuals without scapular dyskinesis.
METHODS
Participants
A convenience sample of 40 participants volunteered to participate in the study (age = 22.2 ± 2.4 years; height = 169.9 ± 8.7 cm; mass = 68.7 ± 13.0 kg; body mass index (BMI) = 23.7 ± 3.1 kg/m2; sex = 12 males, 28 females; arm dominance = 3 left, 37 right). Participants were recruited from the School of Health Sciences at Duquesne University. All participants were included that met the following inclusion criteria: 1) between the ages of 18 and 40, and 2) no history of neck or dominant shoulder injury or pathology. Shoulder dominance was determined by which arm the participant would use to throw a ball. Exclusion criteria included 1) the presence of any neurological condition that affected muscular strength and consequent upper extremity range of motion, 2) inability to achieve ≥ 140 ° of shoulder elevation, 3) any previous surgery on the dominant shoulder, 4) diagnosis of rheumatoid arthritis, and 5) if the participant was currently pregnant. The University's institutional review board approved the study and all participants were required to provide written informed consent prior to participation.
To ensure adequate statistical power, a power analysis was performed using G*Power 3.1.9.2. Based on preliminary data from 10 subjects, an effect size was calculated (f = .313), and operating at a power of 80% and α = .05, it was determined that an estimated sample size of 22 participants was needed to detect significant differences in strength.33 While collecting data, an apparent disparity was revealed in the number of participants with and without scapular dyskinesis. Scapular dyskinesis, as defined by the methods described in this study, was observed in 68% (10/13 males, 17/27 females) of the participants. Therefore, a matched-pairs analysis was utilized, which yielded 13 matched-pairs from the sample. (Table 1) The participants were matched according to sex and BMI. The remaining 14 participants from the sample were excluded from the study because suitable pairings were unavailable.
Table 1.
Participant Demographics for Matched-Pairs Analysis
| Variable | With Dyskinesis | Without Dyskinesis | p |
|---|---|---|---|
| Age (y ± SD) | 21.5 ± 1.2 | 22.5 ± 2.6 | .188 |
| Height (cm ± SD) | 170.1 ± 9.0 | 167.5 ± 7.1 | .420 |
| Mass (kg ± SD) | 72.7 ± 14.6 | 69.3 ± 11.9 | .523 |
| BMI (kg/m2 ± SD) | 24.9 ± 3.4 | 24.6 ± 2.8 | .770 |
| Sex (n) | 3 males; 10 females | 3 males; 10 females | |
| Arm Dominance (n) | 0 left; 13 right | 2 left; 11 right |
BMI = body mass index.
Procedures
All participants completed the Physical Activity Readiness Questionnaire (PAR-Q)34 to establish general health fitness. If participants checked “yes” for any of the listed items they were disqualified from the study. To confirm a healthy shoulder status, all participants completed the patient self-report section and underwent the physical examination section of the American Shoulder and Elbow Surgeons Standardized Shoulder Assessment (ASES).35 Any presence of decreased range of motion, strength, or other clinical findings that suggested shoulder pathology upon examination would have resulted in exclusion from the study.
Scapular Dyskinesis Test
Participants were evaluated for scapular dysfunction of the dominant shoulder utilizing the scapular dyskinesis test.36 The participants performed separate trials of bilateral shoulder flexion and abduction while holding either a 1.4 kg or 2.3 kg weight: 1.4 kg for body masses < 68.1 kg and 2.3 kg for body masses > 68.1 kg.36,37 The test was modified by having the participants perform 10 repetitions for each movement. Movement velocity was standardized across all participants by way of a metronome set at 80 beats per minute resulting in a movement velocity of approximately 120 °/s; therefore, each trial lasted 30 seconds. Performance of the test was digitally recorded from a standardized distance and height for documentation purposes.
The presence of scapular dyskinesis was determined by scapular winging, dysrhythmia, or both as defined by McClure et al.37 Scapular winging was defined as any posterior displacement of the medial border and/or inferior angle of the scapula away from the thorax.37 Dysrhythmia was defined as any early or excessive elevation or protraction, non-rhythmical motion while raising or lowering the arm, or rapid downward rotation while lowering the arm.37 A dichotomous method (yes/no) was used to categorize those with and without scapular dyskinesis.38 One investigator, with 14 years of clinical experience as an athletic trainer, evaluated all participants and determined the presence of scapular dyskinesis. Test-retest reliability (coefficient of agreement = .99) was assessed using digital recordings of 10 subjects that were randomly chosen from the sample. Reassessment occurred within a period of 48 hours. The investigator was blinded to the original scoring, and subject ordering was randomized to decrease bias.
Manual Muscle Tests
Participants underwent eight manual muscle tests of muscles around the shoulder complex: upper trapezius (two methods), middle trapezius, lower trapezius, serratus anterior, supraspinatus, and the medial and lateral rotators of the humerus. The order of the strength tests were randomized. A handheld dynamometer (ergoFET 300, Hogan Health Industries©, West Jordon, UT), with a manufacturer's reported accuracy of +/- 2%, was used to assess the peak force (N) exerted during the tests. Measures of force captured by the handheld dynamometer during the manual muscle tests were used to quantify measures of strength. Prior to data collection, the dynamometer was assessed for accuracy by comparing known loads applied to the dynamometer and its recorded values (r = .9998). For each muscle test, the participants were asked to generate a maximal effort against the resistance being applied by the investigator. Thus, participants performed a “make test” rather than a “break test” as it is commonly used in handheld dynamometry studies.24-28 Participants were asked to gradually build up their effort over a two-second period and maintain a maximum effort for three seconds. Three trials were performed for each manual muscle test with a 30-second rest period between each trial, and approximately one minute of rest between each muscle. Prior to performing the manual muscle tests, participants were provided instruction on proper performance of the test. Additionally, participants performed two to three sub-maximal efforts in order to become accustomed to the testing procedures.
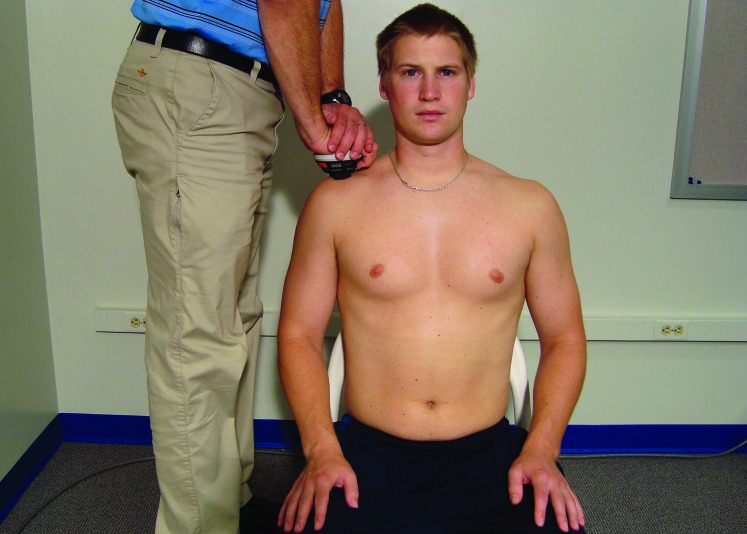
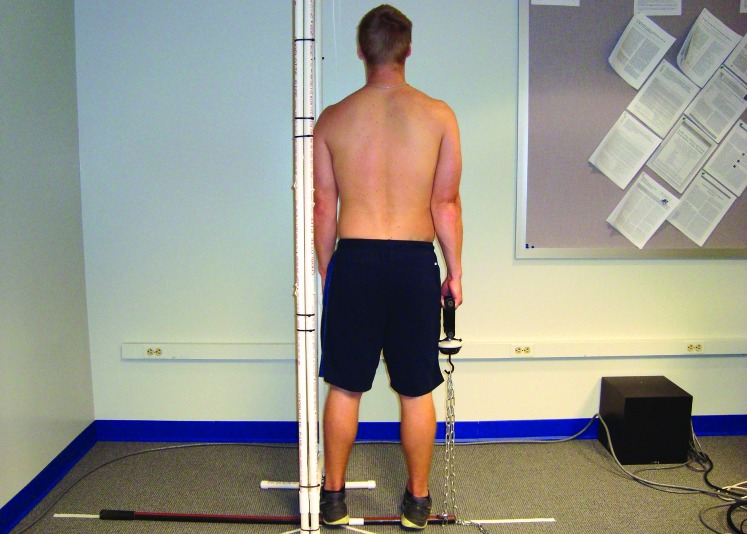
Two different methods were used to evaluate the upper trapezius. The first method (UT1) was performed as described by Hislop et al39 (Figure 1). The participant was seated with the hands resting on the thighs, and the shoulder girdle was positioned at the midrange of elevation. The dynamometer was placed on the acromion process and the resistance was directed inferiorly. The second method (UT2) was performed with the participant standing atop of a modified rake handle while grasping the dynamometer with the dominant hand (Figure 2). For this test, the manufacturer's handle and hook accessories were affixed to the dynamometer. The dynamometer was attached to the modified rake handle by a metal chain. A screen was placed immediately adjacent to the participant on the non-dominant side to aide in limiting extraneous lateral trunk motion. The dynamometer was affixed to the chain at a height that positioned the participant's shoulder girdle in the midrange of elevation. The participant was instructed to shrug their shoulder superiorly, while maintaining an extended elbow, against the resistance.
Figure 1.
Test position for the upper trapezius, method 1.
Figure 2.
Test position for the upper trapezius, method 2.
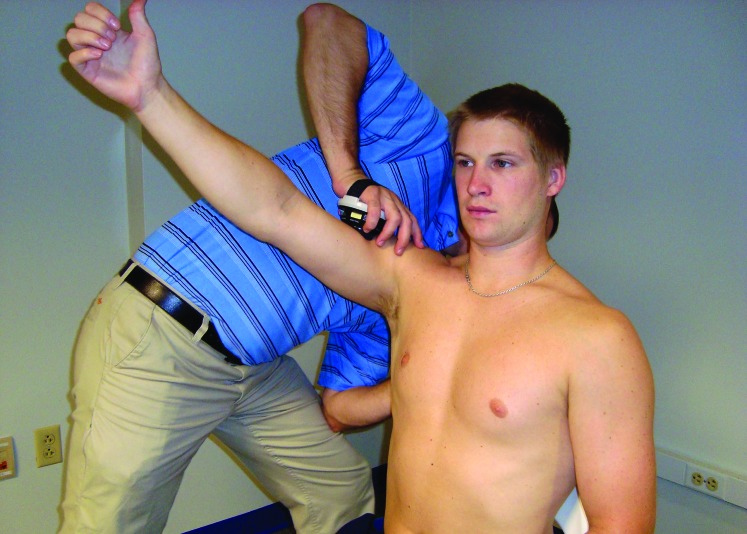
The serratus anterior (SA) was tested as described by Kendall et al40 (Figure 3). The participant was seated with the dominant arm positioned in 120 ° of shoulder flexion with the thumb pointed in an upward direction. The dynamometer was positioned on the humerus at the level of the deltoid insertion, and the resistance was applied in a downward direction that was perpendicular to the humerus.
Figure 3.
Test position for the serratus anterior.
Strength of the middle trapezius (MT) was measured as described by Kendall et al40 (Figure 4). The participant was positioned prone on a plinth with the shoulder abducted to 90 ° and the humerus laterally rotated where the thumb pointed toward the ceiling. The location of the resistance force applied by the tester was modified whereby the dynamometer was positioned on the spine of the scapula approximately 2/3 of the distance from the root of the spine to the posterolateral angle of the acromion. The position was modified in an effort to isolate the measured forces to the scapulothoracic musculature and prevent the involvement of other muscular forces (e.g., rotator cuff).24 The resistance was applied in an anterolateral direction in line with the humerus.
Figure 4.
Test position for the middle trapezius.
The lower trapezius (LT) was tested as described by Hislop et al39 (Figure 5). The participant was positioned prone on a plinth with the shoulder abducted to 140 ° and the humerus laterally rotated where the thumb pointed toward the ceiling. Again, the location of the dynamometer was modified and positioned on the spine of the scapula approximately 2/3 of the distance from the root of the spine to the posterolateral angle of the acromion. Collecting strength measures of the lower trapezius by placing the dynamometer on the spine of the scapula has been determined to be a valid method of assessment.24 The resistance was applied in a superior and anterolateral direction in line with the humerus.
Figure 5.
Test position for the lower trapezius.
The supraspinatus (SS) was evaluated as described by Celik et al25 (Figure 6). The participant was seated with the dominant arm positioned in 90 ° of shoulder scaption (30 ° anterior to the frontal plane) with the thumb pointed toward the ceiling. The dynamometer was positioned on the upper arm just proximal to the elbow, and the resistance was applied in a downward direction.
Figure 6.
Test position for the supraspinatus.
The medial (MR) and lateral (LR) rotators were tested as described by Riemann et al26 (Figures 7 and 8). The participant was seated with a bolster placed between the dominant upper arm and thorax to maintain a position of 30 ° abduction and 30 ° flexion of the shoulder. The elbow was positioned at 90 ° of flexion, while the forearm was positioned in 0 ° pronation/supination and aligned parallel to the sagittal plane to achieve approximately 30 ° of lateral rotation of the shoulder. The dynamometer was placed over the distal radioulnar joint on the volar and dorsal surfaces for the medial and lateral rotators, respectively.
Figure 7.
Test position for the medial rotators.
Figure 8.
Test position for the lateral rotators.
The same investigator performed all the manual muscle tests in this study. For each test, the peak force (N) from three trials was averaged, normalized to body weight (N), and used for data analysis. Excellent within-session, intrarater reliability (ICC3,1 = .920 – .970) was demonstrated for all manual muscle tests over the duration of data collection. In addition to the normalized strength data, strength ratios (UT/LT, UT/MT, LT/MT, SA/UT, SA/MT, SA/LT, and LR/MR) were calculated by dividing the averaged peak force of one muscle by the other.
Statistical Analyses
Descriptive statistics were calculated for demographic data. A two-way mixed analysis of variance was used to determine differences in strength between those with and without scapular dyskinesis, with manual muscle tests (UT1, UT2, SA, MT, LT, SS, MR, and LR) being the repeated factor. If a significant main effect for manual muscle tests was detected, pairwise comparisons were made using a Bonferonni adjustment. Also, a two-way mixed analysis of variance was used to determine differences in strength ratios between those with and without scapular dyskinesis, with strength ratios (UT/LT, UT/MT, LT/MT, SA/UT, SA/MT, SA/LT, and LR/MR) being the repeated factor. If a significant interaction was detected, pairwise comparisons were made between groups for each repeated factor, and a Bonferonni adjustment was made for multiple comparisons. All statistical analyses were calculated using SPSS version 22 (IBM Corporation, Armonk, NY), and the level of significance was set a priori at α = .05.
RESULTS
Demographic data for the 13 matched-pairs are presented in Table 1. For strength comparisons (Table 2), no significant interaction effects (F1.825,43.794 = 1.03, p = .343) were observed between manual muscle tests and scapular dyskinesis. Also, no significant main effects were demonstrated for scapular dyskinesis (F1,24 = .380, p = .543); however, significant main effects for manual muscle tests were revealed (F1.825,43.794 = 239.582, p < .001). For the strength ratios analysis (Table 3), no significant interaction effects (F1.834,44.015 = 1.933, p = .160) or main effects for scapular dyskinesis (F1,24 = 2.517, p = .126) were observed. Although significant main effects for strength ratios were revealed, these effects were not a focus of this study.
Table 2.
Manual Muscle Test Data for Matched-Pairs Analysis.
| Muscle | With Dyskinesis | Without Dyskinesis | Total |
|---|---|---|---|
| Upper Trapezius 1 | 0.292 ± 0.046 | 0.328 ± 0.085 | 0.310 ± 0.069* |
| Upper Trapezius 2 | 0.271 ± 0.047 | 0.277 ± 0.099 | 0.274 ± 0.076* |
| Serratus Anterior | 0.145 ± 0.029 | 0.149 ± 0.036 | 0.147 ± 0.032† |
| Middle Trapezius | 0.137 ± 0.013 | 0.135 ± 0.022 | 0.136 ± 0.018* |
| Lower Trapezius | 0.105 ± 0.013 | 0.109 ± 0.028 | 0.107 ± 0.022‡ |
| Supraspinatus | 0.097 ± 0.015 | 0.105 ± 0.028 | 0.101 ± 0.022§ |
| Medial Rotators | 0.089 ± 0.017 | 0.091 ± 0.028 | 0.090 ± 0.023* |
| Lateral Rotators | 0.060 ± 0.012 | 0.060 ± 0.014 | 0.060 ± 0.013 |
Data are presented as normalized strength values (M ± SD) calculated by averaging the maximum force (N) of three trials then dividing by body weight (N) for each muscle, respectively.
Significantly greater than those listed below it.
Significantly greater than lower trapezius, supraspinatus, medial and lateral rotators.
Significantly greater than medial and lateral rotators.
Significantly greater than lateral rotators.
Table 3.
Strength Ratios for Matched-Pairs Analysis.
| Strength Ratio | With Dyskinesis | Without Dyskinesis | Total |
|---|---|---|---|
| UT/LT | 2.791 ± 0.386 | 3.092 ± 0.668 | 2.941 ± 0.556 |
| UT/MT | 2.145 ± 0.333 | 2.423 ± 0.394 | 2.284 ± 0.384 |
| LT/MT | 0.771 ± 0.080 | 0.800 ± 0.117 | 0.785 ± 0.099 |
| SA/UT | 0.503 ± 0.105 | 0.461 ± 0.055 | 0.482 ± 0.085 |
| SA/MT | 1.059 ± 0.162 | 1.106 ± 0.158 | 1.082 ± 0.159 |
| SA/LT | 1.383 ± 0.229 | 1.403 ± 0.237 | 1.393 ± 0.228 |
| LR/MR | 0.676 ± 0.097 | 0.675 ± 0.118 | 0.675 ± 0.106 |
Strength Ratios (M ± SD) were calculated by dividing the averaged peak force of one muscle by the other, respectively. UT = upper trapezius, MT = middle trapezius, LT = lower trapezius, SA = serratus anterior, LR = lateral rotators, and MR = medial rotators. No significant differences were revealed between groups for any of the strength ratios.
DISCUSSION
It was hypothesized that strength differences would exist between healthy individuals with and without scapular dyskinesis, which may serve as a causative factor for scapular dyskinesis. However, the results of this study demonstrated no significant differences in strength or strength ratios of the scapular stabilizers and rotator cuff when compared between those healthy shoulders with and without scapular dyskinesis. To the authors’ knowledge, this was the first study to compare strength measures collected from a sample of healthy participants with and without scapular dyskinesis.
Scapular dyskinesis is commonly associated with numerous pathologies of the shoulder; however, it is not well understood if scapular dyskinesis is the cause or result of the injury.8 Muscle performance, specifically muscular weakness, has been implicated as a causal factor of scapular dyskinesis based on studies involving symptomatic patients.7,8 Rehabilitation programs focused on restoring muscle imbalances of the scapular stabilizers have been demonstrated to restore strength of the rotator cuff in symptomatic overhead athletes.22,23 Therefore, if muscular performance is in fact a contributory factor then it is plausible that strength deficits would be observed in healthy individuals with scapular dyskinesis. However, the results of the current study challenge the idea that healthy individuals with scapular dyskinesis have strength deficits. The results of this study are further supported in that strengthening programs designed to improve shoulder complex strength do not appear to resolve scapular dyskinesis.41 Therefore, it may be suggested that gross strength is not a contributory factor in the development of scapular dyskinesis. While the intent of this study was to determine if any strength differences existed, it was interesting to find such a disproportionate number of those with scapular dyskinesis. The disproportionate number of those with scapular dyskinesis along with no differences in strength in a sample of healthy college-aged individuals calls into question the clinical relevance of scapular dyskinesis as a movement impairment. These data may suggest that scapular dyskinesis in healthy individuals is no more than a normal variation of scapular motion. Furthermore, these data may explain the common occurrence and inconsistent patterns of scapular dyskinesis that occur in symptomatic individuals. Nonetheless, these data should not detract from evaluating and considering the role that scapular dyskinesis plays in symptomatic patients. Furthermore, there is sufficient evidence to support the use of a rehabilitation program focused on restoring scapular stabilizer recruitment and neuromuscular control.7
The prevalence of scapular dyskinesis is unknown in the healthy population, but it appears to be quite common, if not more common, than what is presently considered to be “normal” scapular motion. In the present study, 68% (27/40) of the overall sample presented with aberrant scapular motion, which led to the utilization of a matched-pairs analysis. According to the literature, scapular dyskinesis has been shown to be present in 50 – 61% of healthy overhead athletes.9,10,14,42 McClure et al37 used overhead athletes that were moderately healthy (included individuals with pain rated up to seven using a 10-point pain scale) to establish reliability of the scapular dyskinesis test, and reported 85% of participants displayed obvious scapular dyskinesis. While their study did not account for arm dominance, it adds to the argument that aberrant scapular motion is present more often than not in healthy populations. Thus, further investigations are warranted to determine the prevalence of scapular dyskinesis in the healthy population.
Significant differences were observed in strength between several of the muscles tested when the two scapular dyskinesis groups were combined (Table 2). Due to a lack of significant differences between the muscles tested, a specific rank order could not be produced. However, several trends were identified that resulted in the following generalized order: the UT generated the greatest amount of force, followed by the SA and MT, LT, SS, MR, and the LR generated the least amount of force. Interestingly, this generalized order is nearly identical to normative data collected via handheld dynamometry using similar testing procedures.26,27 In addition to strength data, strength ratios (Table 3) were calculated that have been reported in normative studies,26,27 or have been the focus of rehabilitation programs aimed at restoring balance of the scapular stabilizers.7,22,23 No significant differences were revealed for any of the strength ratios between the scapular dyskinesis groups (Table 3). The scapular stabilizer ratios calculated from the present study correspond well to those reported by Turner et al.27 However, the LR/MR ratios (0.675 – 0.676) appear to be smaller than those reported by Riemann et al,26 which ranged from 0.86 – 0.92.
It has commonly been suggested that decreased muscle performance of the shoulder musculature is present in individuals with scapular dyskinesis.6-8 However, the authors of these papers primarily reference studies that did not control for scapular dyskinesis, but were based on electromyographic data that demonstrated altered activation patterns of the scapular stabilizers in symptomatic shoulders (e.g., impingement).6-8 Few studies have demonstrated strength deficits of the shoulder musculature in individuals with scapular dyskinesis.10,22,23 Merolla and colleagues reported infraspinatus (IS)22,23 and SS22 strength deficits in symptomatic overhead athletes with scapular dyskinesis. In both studies, participants completed similar six-month rehabilitation programs designed to improve balance and control of the scapular stabilizers. Significant improvements (p < .01) in IS and SS strength were reported at 3 (IS = 42%,22 36%,23 SS = 23%22) and 6 (IS = 43%,22 43%,23 SS = 24%22) months. Based on these results, Merolla and colleagues22,23 speculated that imbalances in the scapular musculature led to an acquired scapular dyskinesis, which compromised the length-tension relationship of the rotator cuff muscles that resulted in weakness of the IS and SS, secondarily. However, the results of these studies should be interpreted cautiously as muscle performance measures were not collected for the scapular stabilizers. Additionally, while all participants were cleared for labroligamentous injuries, chondral lesions, and rotator cuff tears via magnetic resonance imaging, they were all symptomatic at baseline. Therefore, it is purely speculative that scapular dyskinesis was acquired, especially with the growing evidence that scapular dyskinesis is commonly found in healthy overhead athletes.9-11
Others have speculated the same regarding muscle imbalances of the scapular stabilizers, which has led to the development of a scapular repositioning maneuver to test for weakness of the IS and SS.30,31 During this maneuver, the clinician retracts the scapula and provides external stabilization that results in the ability of the rotator cuff in symptomatic individuals with scapular dyskinesis to produce greater strength output when compared to traditional manual muscle testing procedures. Yet, strength improvements have been observed in healthy, asymptomatic individuals when utilizing the repositioning maneuver as well.31,32 In contrast, Smith and colleagues43 demonstrated significantly lower measures of shoulder elevation strength when the scapula was positioned in retracted and protracted positions as compared to the normal resting position in a sample of healthy individuals without scapular dyskinesis. Nonetheless, these studies indicate scapular positioning has an impact on shoulder strength. The scapular repositioning maneuver was not utilized in the current study, and no significant differences were revealed between the scapular dyskinesis groups. These findings suggest that healthy individuals may position their scapula optimally for strength output regardless of the presence of scapular dyskinesis. Therefore, the clinical usefulness of the repositioning maneuver is debatable and should be interpreted with caution.
In addition to the current study, only one other study has compared strength measures of the MT and LT in asymptomatic individuals with and without scapular dyskinesis. Seitz et al10 reported weakness of the LT by 4% (p = .031) body mass in those with scapular dyskinesis in a sample of asymptomatic overhead athletes. Interestingly, the group with scapular dyskinesis in the current study demonstrated weakness by 4% body mass, but was not found to be significant. The conflicting results may be explained by differences in populations studied as stronger scapular muscles of the dominant shoulder,28,44 and asymmetrical positioning of the scapula are known to occur in healthy overhead athletes.45,46 Additionally, testing methods differed for the manual muscle test as Seitz et al10 applied resistance just proximal to the wrist, whereas the resistance was applied directly to the scapula in the current study. It was thought that a better representation of the strength capabilities of the scapular stabilizers would be achieved by positioning the dynamometer directly over the scapula, which is supported by others.24 In fact, Michener et al24 demonstrated that assessing strength of the lower trapezius with a handheld dynamometer placed over the scapula yielded valid measures when compared against electromyography. However, no data exist that compares strength measures of the scapular stabilizers collected with the dynamometer placed in the two different positions. Nonetheless, by positioning the dynamometer at the wrist, additional factors (e.g., glenohumeral strength) contribute to force generation that may disguise the true strength capabilities of the targeted musculature.
When evaluating the results of the current study, several limitations were identified that warrant acknowledgment. First, the generalizability of the results are limited to healthy, college-aged individuals, which consisted mostly of females (77%) and may or may not have included overhead athletes. Additionally, only data from the dominant arm was used in this study. Inclusion of data from the non-dominant arm in future studies would aid in the generalizability of the results and in determining the prevalence of scapular dyskinesis. A second limitation is the large amount of variability that is inherent to scapular kinematics, yet a dichotomous method was utilized to categorize those with and without scapular dyskinesis. Other investigators have sub-categorized movements of the scapula as normal, subtle, or obvious to maximize the detection of differences.47,48 However, for the purposes of this study, the subtle and obvious categories were combined and the yes/no method38 was utilized as it was speculated that clinicians are more likely to treat symptomatic patients the same regardless of the “degree” of scapular dyskinesis. Studies36,38 have indicated better measures of agreement in identifying scapular dyskinesis utilizing a dichotomous method over other sub-categorization methods as defined by Tate et al36 and Kibler et al.49 Regardless of the fact that the presence of scapular dyskinesis was based upon an established criteria and the implementation of that criteria by a single observer, a large amount of variability was noted in the scapular motion in the scapular dyskinesis group. Through the implementation of the match pair's criteria and merely by chance alone, those with a lesser degree of scapular dyskinesis were not included in the matched-pairs. This adds merit to the current findings because excluding those participants should have maximized any potential differences between the groups. Lastly, a ceiling effect was observed with the UT1 method as a few of the male participants were able to lift the investigator from the floor, which negated the ability to collect a maximum effort by these individuals. This, along with a similar experience by Turner et al,27 prompted the use of the UT2 method. While significant differences were revealed between the two methods, the overall results in the matched-pairs analysis were not likely affected as neither measure revealed significant differences between the two scapular dyskinesis groups.
CONCLUSION
The results of this study indicate that no differences in shoulder strength exist between individuals with and without scapular dyskinesis in a healthy population of college-aged individuals with no history of neck and shoulder pathology. As such, gross strength is not likely to be a contributing factor to the development of scapular dyskinesis, whereas other muscle performance factors, such as neuromuscular control, may be. Moreover, this study adds to a growing body of evidence that scapular dyskinesis is commonly found in healthy individuals.
REFERENCES
- 1.Luime JJ Koes BW Hendriksen IJ, et al. Prevalence and incidence of shoulder pain in the general population; a systematic review. Scand J Rheumatol. 2004;33(2):73-81. [DOI] [PubMed] [Google Scholar]
- 2.Laudner K Sipes R. The incidence of shoulder injury among collegiate overhead athletes. J Intercolleg Sport. 2009;2(2):260-268. [Google Scholar]
- 3.Tate A Turner GN Knab SE, et al. Risk factors associated with shoulder pain and disability across the lifespan of competitive swimmers. J Athl Train. 2012;47(2):149-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mohseni-Bandpei MA Keshavarz R Minoonejhad H, et al. Shoulder pain in Iranian elite athletes: the prevalence and risk factors. J Manipulative Physiol Ther. 2012;35(7):541-548. [DOI] [PubMed] [Google Scholar]
- 5.Johnson MP Crossley KL O’Neil ME, et al. Estimates of direct health care expenditures among individuals with shoulder dysfunction in the United States. Paper presented at: American Society of Shoulder and Elbow Therapists Annual Meeting; 2004; New York City, NY. http://www.asset-usa.org/Abstracts/Johnson_Crossley_Oneil_Al-Kakwani.html. Accessed August 25, 2016.
- 6.Kibler WB Sciascia A. Current concepts: scapular dyskinesis. Br J Sports Med. 2010;44(5):300-305. [DOI] [PubMed] [Google Scholar]
- 7.Cools AM Struyf F De Mey K, et al. Rehabilitation of scapular dyskinesis: from the office worker to the elite overhead athlete. Br J Sports Med. 2014;48(8):692-697. [DOI] [PubMed] [Google Scholar]
- 8.Kibler WB Ludewig PM McClure PW, et al. Clinical implications of scapular dyskinesis in shoulder injury: the 2013 consensus statement from the ‘Scapular Summit’. Br J Sports Med. 2013;47(14):877-885. [DOI] [PubMed] [Google Scholar]
- 9.Myers JB Oyama S Hibberd EE. Scapular dysfunction in high school baseball players sustaining throwing-related upper extremity injury: a prospective study. J Shoulder Elbow Surg. 2013;22(9):1154-1159. [DOI] [PubMed] [Google Scholar]
- 10.Seitz AL McClelland RI Jones WJ, et al. A comparison of change in 3D scapular kinematics with maximal contractions and force production with scapular muscle tests between asymptomatic overhead athletes with and without scapular dyskinesis. Int J Sports Phys Ther. 2015;10(3):309-318. [PMC free article] [PubMed] [Google Scholar]
- 11.Silva RT Hartmann LG Laurino CF, et al. Clinical and ultrasonographic correlation between scapular dyskinesia and subacromial space measurement among junior elite tennis players. Br J Sports Med. 2010;44(6):407-410. [DOI] [PubMed] [Google Scholar]
- 12.Kawasaki T Yamakawa J Kaketa T, et al. Does scapular dyskinesis affect top rugby players during a game season? J Shoulder Elbow Surg. 2012;21(6):709-714. [DOI] [PubMed] [Google Scholar]
- 13.Clarsen B Bahr R Andersson SH, et al. Reduced glenohumeral rotation, external rotation weakness and scapular dyskinesis are risk factors for shoulder injuries among elite male handball players: a prospective cohort study. Br J Sports Med. 2014;48(17):1327-1333. [DOI] [PubMed] [Google Scholar]
- 14.Struyf F Nijs J Meeus M, et al. Does scapular positioning predict shoulder pain in recreational overhead athletes? Int J Sports Med. 2014;35(1):75-82. [DOI] [PubMed] [Google Scholar]
- 15.Chopp JN Fischer SL Dickerson CR. The specificity of fatiguing protocols affects scapular orientation: implications for subacromial impingement. Clin Biomech (Bristol, Avon). 2011;26(1):40-45. [DOI] [PubMed] [Google Scholar]
- 16.Tsai NT McClure PW Karduna AR. Effects of muscle fatigue on 3-dimensional scapular kinematics. Arch Phys Med Rehabil. 2003;84(7):1000-1005. [DOI] [PubMed] [Google Scholar]
- 17.Ludewig PM Cook TM. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys Ther. 2000;80(3):276-291. [PubMed] [Google Scholar]
- 18.McClure PW Michener LA Karduna AR. Shoulder function and 3-dimensional scapular kinematics in people with and without shoulder impingement syndrome. Phys Ther. 2006;86(8):1075-1090. [PubMed] [Google Scholar]
- 19.Kibler WB. The role of the scapula in athletic shoulder function. Am J Sports Med. 1998;26(2):325-337. [DOI] [PubMed] [Google Scholar]
- 20.McClure P Greenberg E Kareha S. Evaluation and management of scapular dysfunction. Sports Med Arthrosc. 2012;20(1):39-48. [DOI] [PubMed] [Google Scholar]
- 21.Voight ML Thomson BC. The role of the scapula in the rehabilitation of shoulder injuries. J Athl Train. 2000;35(3):364-372. [PMC free article] [PubMed] [Google Scholar]
- 22.Merolla G De Santis E Campi F, et al. Supraspinatus and infraspinatus weakness in overhead athletes with scapular dyskinesis: strength assessment before and after restoration of scapular musculature balance. Musculoskelet Surg. 2010;94(3):119-125. [DOI] [PubMed] [Google Scholar]
- 23.Merolla G De Santis E Sperling JW, et al. Infraspinatus strength assessment before and after scapular muscles rehabilitation in professional volleyball players with scapular dyskinesis. J Shoulder Elbow Surg. 2010;19(8):1256-1264. [DOI] [PubMed] [Google Scholar]
- 24.Michener LA Boardman ND Pidcoe PE, et al. Scapular muscle tests in subjects with shoulder pain and functional loss: reliability and construct validity. Phys Ther. 2005;85(11):1128-1138. [PubMed] [Google Scholar]
- 25.Celik D Dirican A Baltaci G. Intrarater reliability of assessing strength of the shoulder and scapular muscles. J Sport Rehabil. 2012;Technical Notes 3:1-5. [DOI] [PubMed] [Google Scholar]
- 26.Riemann BL Davies GJ Ludwig L, et al. Hand-held dynamometer testing of the internal and external rotator musculature based on selected positions to establish normative data and unilateral ratios. J Shoulder Elbow Surg. 2010;19(8):1175-1183. [DOI] [PubMed] [Google Scholar]
- 27.Turner N Ferguson K Mobley BW, et al. Establishing normative data on scapulothoracic musculature using handheld dynamometry. J Sport Rehabil. 2009;18(4):502-520. [DOI] [PubMed] [Google Scholar]
- 28.Cools AM Johansson FR Cambier DC, et al. Descriptive profile of scapulothoracic position, strength and flexibility variables in adolescent elite tennis players. Br J Sports Med. 2010;44(9):678-684. [DOI] [PubMed] [Google Scholar]
- 29.Cools AM Palmans T Johansson FR. Age-related, sport-specific adaptions of the shoulder girdle in elite adolescent tennis players. J Athl Train. 2014;49(5):647-653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Merolla G De Santis E Campi F, et al. Infraspinatus scapular retraction test: a reliable and practical method to assess infraspinatus strength in overhead athletes with scapular dyskinesis. J Orthop Traumatol. 2010;11(2):105-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kibler WB Sciascia A Dome D. Evaluation of apparent and absolute supraspinatus strength in patients with shoulder injury using the scapular retraction test. Am J Sports Med. 2006;34(10):1643-1647. [DOI] [PubMed] [Google Scholar]
- 32.Tate AR McClure PW Kareha S, et al. Effect of the scapula reposition test on shoulder impingement symptoms and elevation strength in overhead athletes. J Orthop Sports Phys Ther. 2008;38(1):4-11. [DOI] [PubMed] [Google Scholar]
- 33.Faul F Erdfelder E Lang AG, et al. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175-191. [DOI] [PubMed] [Google Scholar]
- 34.Physical Activity Readiness Questionnaire - PAR-Q. Canadian Society for Exercise Physiology Website. http://www.csep.ca/CMFiles/publications/parq/par-q.pdf. Updated 2002. Accessed 9/28/2015.
- 35.Richards RR An KN Bigliani LU, et al. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994;3(6):347-352. [DOI] [PubMed] [Google Scholar]
- 36.Tate AR McClure P Kareha S, et al. A clinical method for identifying scapular dyskinesis, part 2: validity. J Athl Train. 2009;44(2):165-173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McClure P Tate AR Kareha S, et al. A clinical method for identifying scapular dyskinesis, part 1: reliability. J Athl Train. 2009;44(2):160-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Uhl TL Kibler WB Gecewich B, et al. Evaluation of clinical assessment methods for scapular dyskinesis. Arthroscopy. 2009;25(11):1240-1248. [DOI] [PubMed] [Google Scholar]
- 39.Hislop H Avers D Brown M. Daniels and Worthingham's Muscle Testing: Techniques of Manual Examination and Performance Testing. 9th ed. St. Louis, MO: Elsevier Health Sciences; 2013. [Google Scholar]
- 40.Kendall FP McCreary EK Provance PG, et al. Muscles: Testing and Function with Posture and Pain. 5th ed. Baltimore, MD: Lippincott Williams & Wilkins; 2005. [Google Scholar]
- 41.Hibberd EE Oyama S Spang JT, et al. Effect of a 6-week strengthening program on shoulder and scapular-stabilizer strength and scapular kinematics in division I collegiate swimmers. J Sport Rehabil. 2012;21(3):253-265. [DOI] [PubMed] [Google Scholar]
- 42.Reeser JC Joy EA Porucznik CA, et al. Risk factors for volleyball-related shoulder pain and dysfunction. PM R. 2010;2(1):27-36. [DOI] [PubMed] [Google Scholar]
- 43.Smith J Kotajarvi BR Padgett DJ, et al. Effect of scapular protraction and retraction on isometric shoulder elevation strength. Arch Phys Med Rehabil. 2002;83(3):367-370. [DOI] [PubMed] [Google Scholar]
- 44.Donatelli R Ellenbecker TS Ekedahl SR, et al. Assessment of shoulder strength in professional baseball pitchers. J Orthop Sports Phys Ther. 2000;30(9):544-551. [DOI] [PubMed] [Google Scholar]
- 45.Myers JB Laudner KG Pasquale MR, et al. Scapular position and orientation in throwing athletes. Am J Sports Med. 2005;33(2):263-271. [DOI] [PubMed] [Google Scholar]
- 46.Oyama S Myers JB Wassinger CA, et al. Asymmetric resting scapular posture in healthy overhead athletes. J Athl Train. 2008;43(6):565-570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lopes AD Timmons MK Grover M, et al. Visual scapular dyskinesis: kinematics and muscle activity alterations in patients with subacromial impingement syndrome. Arch Phys Med Rehabil. 2015;96(2):298-306. [DOI] [PubMed] [Google Scholar]
- 48.Seitz AL McClure PW Lynch SS, et al. Effects of scapular dyskinesis and scapular assistance test on subacromial space during static arm elevation. J Shoulder Elbow Surg. 2012;21(5):631-640. [DOI] [PubMed] [Google Scholar]
- 49.Kibler WB Uhl TL Maddux JW, et al. Qualitative clinical evaluation of scapular dysfunction: a reliability study. J Shoulder Elbow Surg. 2002;11(6):550-556. [DOI] [PubMed] [Google Scholar]