Abstract
Superior capsule reconstruction is a recently-developed surgical technique for the treatment of massive, irreparable rotator cuff tears. So far, biomechanical cadaveric studies and clinical outcomes results have been promising concerning integrity, stability, and ROM after superior capsule reconstruction. As this technique has only been recently developed, an evidence-based rehabilitation protocol has not been previously designed. Thus, the purpose of this clinical commentary is to provide an overview of superior capsule reconstruction and to propose a rehabilitation program based on the available scientific evidence. The existing evidence is supplemented by the experience of the senior author who has performed more than forty superior capsule reconstruction procedures to date. This proposed rehabilitation protocol consists of four distinct phases, focusing on maximal protection, range of motion and muscular endurance, muscular strength and return to activity.
Level of Evidence
5
Keywords: Irreparable rotator cuff tears, rehabilitation, shoulder, superior capsule reconstruction
INTRODUCTION AND BACKGROUND
The prevalence of massive rotator cuff tears has been reported to be as high as 40% of all rotator cuff tears.1,2 If not treated in a timely manner, muscle atrophy and fatty infiltration often ensue, resulting in irreparable tears.3 But even if treated in time, the failure rates of massive rotator cuff repairs are higher than those following the repair of smaller tears.4 Once a tear is irreparable, a spectrum of treatment options exists. Non-operative management may be indicated in patients with low demands and symptoms that occur predominantly with use, but it has been shown to lead to the progression of osteoarthritis.5,6 Partial rotator cuff repair and debridement have shown good results;7-10 however, there is limited long-term outcome data of 10 years or more to support its use, as well as the risk of continued pain, loss of motion and function, and worsening arthritic changes.7-10 In elderly patients with advanced shoulder osteoarthritis, reverse total shoulder arthroplasty may be indicated to address cuff tear arthropathy.2 However, limited implant longevity and activity restrictions from high-impact activities make joint replacement a less desirable option in younger patients. Therefore, additional options have been developed for younger patients. Latissimus dorsi tendon transfers have been shown to be a reasonable treatment method for posterosuperior massive rotator cuff tears. However, high complication rates, difficult revisions following failure, and poor outcomes in certain patient populations make stringent patient selection for this procedure particularly important.11
Less invasive than latissimus dorsi tendon transfer, the superior capsule reconstruction (SCR) procedure is a novel technique developed in Japan by Mihata et al.12 as reverse arthroplasty was not approved in Japan at the time. The original technique used fascia lata autograft to reconstruct the superior capsule in the presence of an irreparable rotator cuff tear. Today, a number of allograft options, including a human acellular dermal allograft (Arthroflex, Arthrex, Naples, FL), can be used instead of fascia lata autograft. As demonstrated both biomechanically and clinically by Mihata et al.,12,13 the graft design and surgical placement prevents the humeral head from migrating superiorly and thus enables efficient biomechanics of the shoulder. Additionally, the graft acts as a mechanical spacer between the humeral head and the undersurface of the acromion. Improved range of motion, joint space, and American Shoulder and Elbow Surgeons (ASES) scores following SCR have been reported.13 This arthroscopic technique has a low complication rate and short-term follow-up at a minimum of two years postoperatively shows limited progression of osteoarthritis and rotator cuff muscle atrophy.13
As this innovative technique is only emerging from its infancy, an evidence-based rehabilitation protocol has not been previously designed since the technique was only developed in 2007.12,14 Therefore, the purpose of this clinical commentary is to provide an overview of SCR for the treatment of massive rotator cuff tears and to propose a rehabilitation program based on the available scientific evidence.
ANATOMY / BIOMECHANICS / PATHOBIOMECHANICS
Movement at the shoulder complex arises from a combination of glenohumeral and scapulothoracic motion. The scapula provides a muscle attachment site and allows load transfer from the upper limb to the thorax. The bony architecture, labrum, joint capsule, ligaments and negative pressure within the glenohumeral joint space all provide passive stability. In addition, the rotator cuff and long head of the biceps tendon center the humeral head on the glenoid and provide active stability, thereby allowing effective shoulder function. The rotator cuff consists of four muscles working synergistically: the supraspinatus, infraspinatus, teres minor, and subscapularis. Each muscle's origin and insertion sites determine its function. The supraspinatus forms the superior aspect of the rotator cuff and initiates abduction. The infraspinatus and teres minor comprise the posterior aspect of the rotator cuff and contribute to abduction and function primarily to initiate external rotation. The subscapularis makes up the anterior portion of the rotator cuff and is primarily responsible for internal rotation. In healthy shoulders, a balanced force couple for the glenohumeral joint in both the coronal and the axial planes is maintained by the synergistic action of the deltoid and rotator cuff muscles. In the axial plane, the subscapularis and infraspinatus/teres minor complex maintain a balanced force couple, while the deltoid and rotator cuff inferior to the humeral head equator form a balanced force couple in the coronal plane. As such, the rotator cuff muscles function as primary dynamic stabilizers to maintain concentric joint reduction during rotation of the humeral head on the glenoid.1
Small to medium size rotator cuff tears involving the supraspinatus and the anterior portion of the infraspinatus do not affect stability in the coronal and axial planes because the balanced force couples are maintained. These can be differentiated from massive tears involving at least two tendons including the postero-inferior part of the rotator cuff where the balance of the force couple in the coronal plane is lost, thereby compromising the fulcrum that is necessary for normal glenohumeral mechanics.1,15-20 To restore normal kinematics in patients with massive tears of the postero-superior rotator cuff tendons, greater forces are required by both the deltoid and the intact rotator cuff muscle-tendon units, particularly the subscapularis, to achieve stable abduction.21 The progression of a rotator cuff tear leads to disruption of the axial force couple and subsequent superior subluxation of the humeral head and shoulder dysfunction.19 The force required to move the arm increases with tear size making the biomechanics less efficient. The tensile load on the intact fibers increases because the torn tendons cannot contribute to load sharing, and this leads to tear propagation, especially if the remaining tendon is of poor quality.
Additionally, with initiation of abduction, superior subluxation of the humeral head can occur as a result of muscle weakness or tendon retraction, leading to increased cuff impingement between the greater tuberosity and the inferior aspect of the acromion.16,22 This increased cuff impingement can cause medial extension of supraspinatus tears, leading to a cycle of superior humeral head migration and tear propagation. Usually, a massive rotator cuff tear involving at least two torn tendons is needed to provoke superior migration of the humeral head.23 Non-anatomical superior subluxation of the humeral head against the glenoid produces shear forces at the articular surfaces that cause cartilage destruction. Without early intervention, pain and loss of function ensue, along with the development of disabling osteoarthritis that often progresses to rotator cuff arthropathy.22
SURGICAL TREATMENT
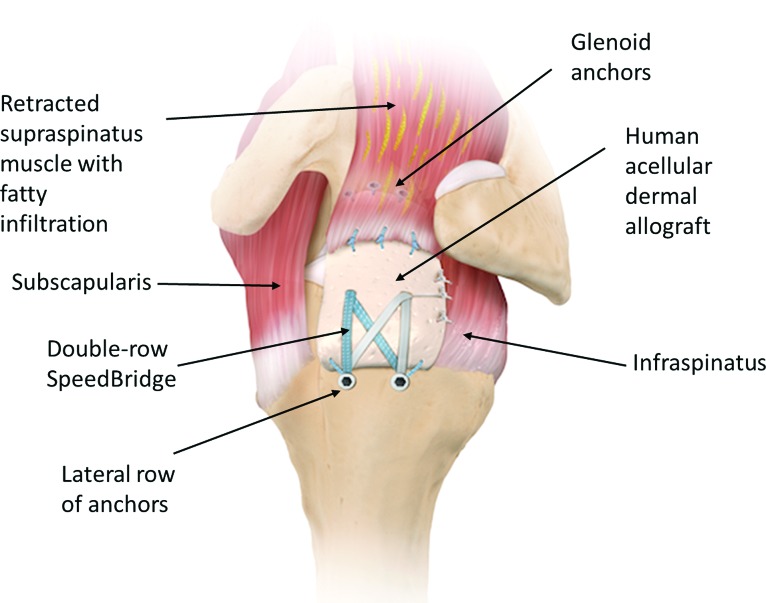
Many operative procedures, including those previously outlined, have been used to treat massive rotator cuff tears, but this commentary focuses on SCR (Figure 1) of which the senior author has performed more than 40 to date. The arthroscopic SCR technique has previously been described in detail by Katthagen et al.24 The retracted, deficient supraspinatus tendon is arthroscopically confirmed and extensively debrided. After the superior glenoid and greater tuberosity bony surfaces are prepared, three anchors are inserted into the glenoid at the 10, 12, and 2 o’clock positions. The rotator cuff defect is measured to determine the size of the human acellular dermal allograft. The patch is then introduced into the shoulder through the anterolateral portal, and the graft is fixed medially. On the humeral side, two anchors are inserted for medial-row fixation at the articular cartilage margin. Two lateral anchors are then inserted for lateral-row fixation. Finally, the lateral part of the graft is compressed down onto the footprint using a suture bridge technique (Figure 2). The native rotator cuff tissue may require margin convergence and is then sutured into the graft for additional stability.
Figure 1.
Diagram from superolateral view of a left shoulder illustrating the final superior capsule reconstruction (SCR) construct, using a human dermal acellular allograft.
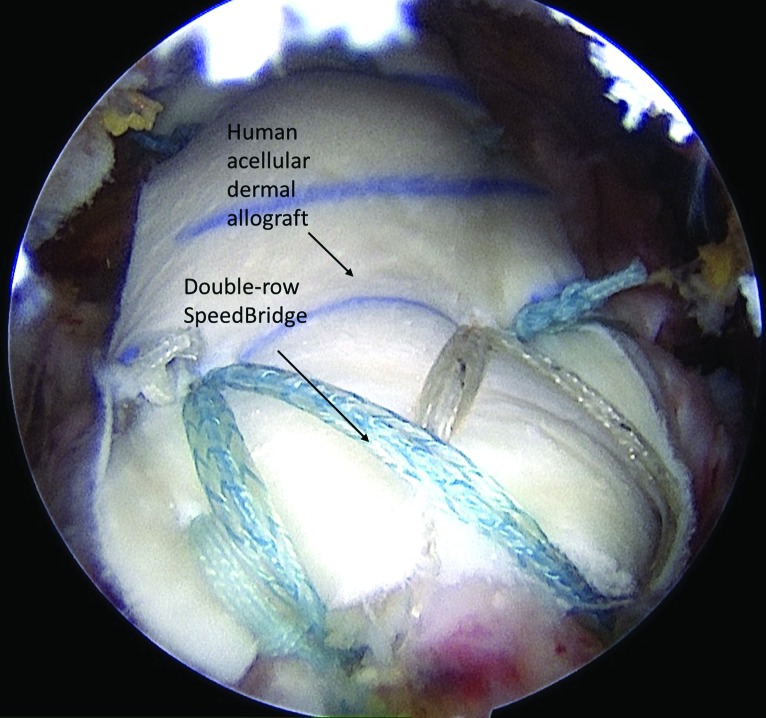
Figure 2.
Arthroscopic photograph in a left shoulder taken from the lateral portal, showing the final SCR construct.
POST-OPERATIVE REHABILITATION
Post-operative rehabilitation following SCR begins with close communication between the surgeon and the physical therapy team. This communication continues throughout the recovery process and is an essential component to ensuring a successful outcome. The physical therapist should discuss expected functional outcomes as well as specifics of the surgery with the surgeon prior to discussing expectations with the patient in order to gain a better understanding of each individual's prior level of function, chronicity of injury, tissue integrity, and goals. The authors always promote a high level of activity in their patients post-operatively while making them aware of the risks of certain activities and sports, particularly contact or overhead sports. Moreover, the authors make patients aware of the limited evidence that currently exists regarding long-term outcomes or risk factors for failure after SCR.
The protocol detailed below is consistent with that suggested by Petri et al.,14 allowing limited and protected PROM initially. However, progression is not as gradual as that suggested by Mihata et al.13 who, after using a fascia lata allograft, advocate for four weeks immobilization, then four weeks of passive and active assisted exercises and finally gradual strengthening beginning at eight weeks. On the other hand, the protocol described herein is not as aggressive as Gupta et al.25 (surgical procedure with a xenograft) who advocate allowing unrestricted passive range of motion exercises with scapular stabilization for the first eight weeks.
Phase I – Maximal Protection
The rehabilitation goals of Phase I include protecting the surgical repair, minimizing pain and inflammation, maintaining mobility of accessory joints and providing patient education. Physical therapy typically begins on post-operative day one in order to review post-operative restrictions and precautions, rehab protocol and progressions, and initial home exercise program, as well as to discuss expected functional outcomes.
Post-operatively, patients are immobilized in a sling limiting passive range of motion (PROM) as much as possible. This is in order to protect the surgical repair by allowing sufficient time for healing to occur prior to introducing controlled, progressive load to the graft. The patient is placed in a sling with abduction pillow to support the glenohumeral joint in the scapular plane, which is worn for six weeks. Patients are instructed to wear compression stockings for two weeks and to perform ankle pumps for up to six weeks post-operatively in order to reduce the risk of deep vein thrombosis.
Although the patient is not initially allowed PROM of the glenohumeral (GH) joint, it is important to ensure maintenance of accessory joint mobility throughout the six-week immobilization period of the shoulder. Patients are instructed on proper performance of active range of motion (AROM) of the cervical spine as well as AROM of the elbow, wrist and hand outside of the sling. Concurrent scapular retraction and depression is also initiated at this time in order to facilitate activation of postural musculature and prevent tightness of the anterior shoulder musculature. Patients are also encouraged to perform gentle ball squeezes using the hand on the involved side in order to facilitate circulation throughout the upper extremity while immobilized in the sling.
Instruction is provided to the patient and caregiver, if present, regarding donning/doffing of the sling as well as how to properly don and doff clothing. It is recommended that patients use a second sling to support their shoulders while showering. Five to six times daily, patients are encouraged to apply cryotherapy and compression for no more than 30 minutes to the involved shoulder the first two weeks post-operatively in order to assist with minimizing pain and inflammation and to provide comfort while sleeping.26
Phase II – Range of Motion and Muscular Endurance
The range-of-motion (ROM) and muscular endurance phase is typically introduced 6 weeks post-operatively. The rehabilitation goals of Phase II consist of restoring passive and active range of motion while managing pain, improving rotator cuff endurance, establishing normal scapulohumeral rhythm and returning to light functional activities of daily living.
Following six weeks of immobilization, the patient is cleared by the surgeon to begin restoring full PROM and AROM of the GH joint without restrictions other than patient tolerance. Rehabilitation of the shoulder at this point generally follows a rehabilitation program typical of a post-operative massive rotator cuff repair. This includes both healing timelines and criteria-based progression as outlined by the multi-disciplinary Level V consensus statement by Thigpen et al.27 allowing for special considerations specific to SCR rehabilitation. It is important to remember the SCR procedure is indicated for massive, irreparable rotator cuff tears in select patients with a functioning deltoid and at least a partially functioning subscapularis and that not all rotator cuff musculature is repaired with this procedure. Moreover, the patient who has undergone SCR may not meet the criteria for rehabilitation progression at the same rate as a patient who has undergone a rotator cuff repair.
Most candidates for SCR present pre-surgically with a retracted, full thickness tear of the supraspinatus and a partial- to full-thickness tear of the infraspinatus and teres minor. Emphasis should be placed on muscle activation of the deltoid, specifically the middle and posterior fibers, along with on regaining as much external rotation function as possible. The external rotators of the glenohumeral joint may be difficult to activate initially, and activation is dependent upon the amount and tissue integrity of the retracted infraspinatus/teres minor surgically attached to the superior capsule graft. Along with the superior capsule graft, the deltoid and internal and external rotation musculature make up the primary force couples about the glenohumeral joint.28 Force couples result in rotational movement; the balance of muscular forces creates dynamic stabilization of the glenohumeral joint through humeral head compression.28 The graft will prevent superior migration of the humeral head during active elevation of the glenohumeral joint. The deltoid and internal/external rotation musculature provide the force couple to approximate the humeral head in the glenoid throughout active and resisted range of motion.
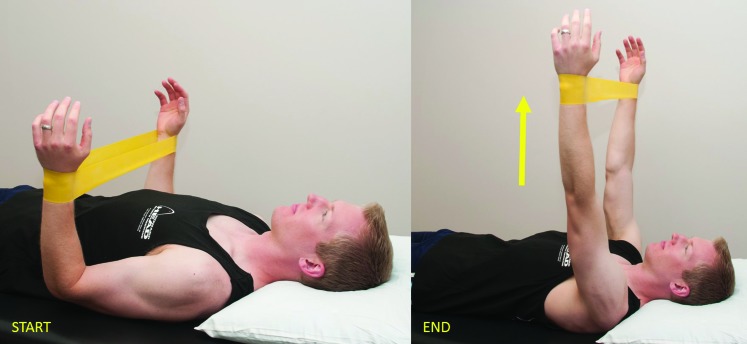
Pain-free glenohumeral PROM is initiated in the supine position prior to beginning active assisted range of motion (AAROM), which typically commences during the seventh post-operative week if PROM is progressing appropriately and pain is properly managed. Generally, AAROM is initiated in positions that place less gravitational demand on the musculature, such as supine, prone or side-lying positions, and can be progressed to seated or standing positions as tolerated. PROM and AAROM exercises should focus on planes of glenohumeral motion including forward elevation, scaption, and internal and external rotation. Supine AAROM forward elevation to 90 ° and external rotation are initiated utilizing a dowel or the contralateral upper extremity for assistance. Based on the authors’ experience, a slideboard can also be utilized in the supine (Figure 1), side-lying, or prone (Figure 2) positions in order to facilitate deltoid activation with scaption and forward elevation movements. Open chain proprioception, pendulums (i.e. Codman's exercise) and gentle aquatic therapy can also be initiated at this time in accordance with patient comfort. Emphasis should be placed on maintaining scapular control with all AAROM and AROM therapeutic exercises.
Scapular and glenohumeral isometrics, as well as initial proprioceptive therapeutic exercises, should be incorporated into treatment at this time as the patient is just beginning to re-learn muscle activation patterns associated with movement of the glenohumeral joint. Sub-maximal glenohumeral isometrics should include the deltoid, subscapularis, infraspinatus, teres minor, triceps and biceps. Isometrics are initiated in a supine, neutral scaption position and can be progressed to varying degrees of abduction, forward elevation, and external rotation. Biofeedback may be useful with isometrics in order to facilitate neuromuscular re-education of the external rotators. Scapular isometrics are progressed from initial activation in Phase 1 to side-lying or prone positions and should focus on retraction, protraction, depression and elevation from a neutral scapular position. These exercises should begin without resistance before progressing to the application of manual resistance, which provides effective biofeedback regarding scapular proprioception. Progression of scapular isometrics in a side-lying or prone position can be performed with the upper extremity supported in various degrees of external rotation or scaption.
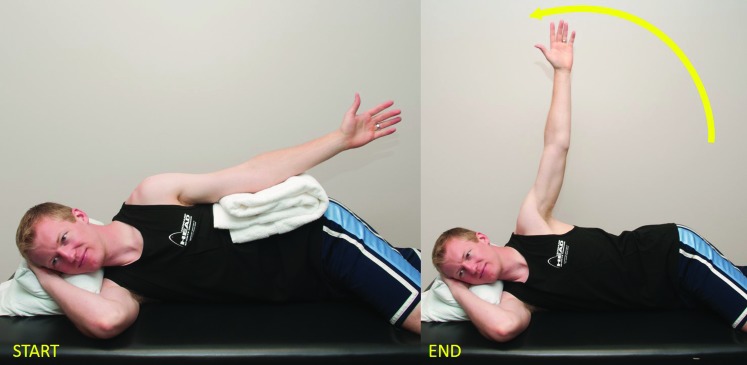
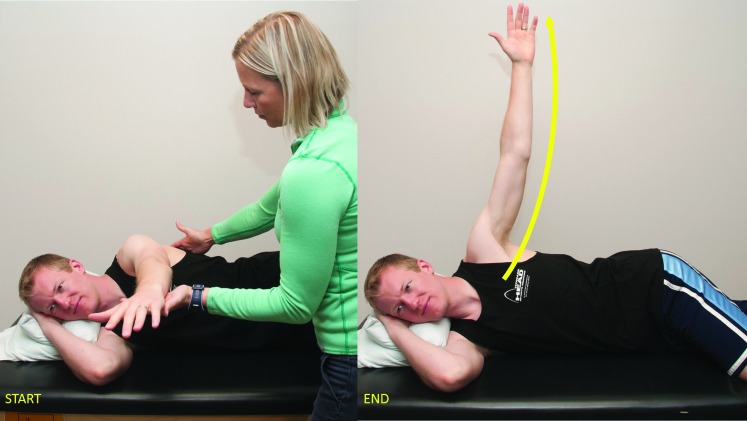
When the patient exhibits effective isometric muscle contraction as well as fair muscle activation with AAROM therapeutic exercises with pain managed effectively, AROM is then initiated. AROM is typically incorporated into treatment one to two weeks after the initiation of PROM, per proper progression of PROM/AAROM and adequate pain control. PROM and AAROM should be incorporated into physical therapy sessions as needed in conjunction with AROM in order to restore functional range of motion. Sling use is also discontinued at this time via a gradual progressive weaning process, and patients can begin utilizing the upper extremity with light activities of daily living, typically at and below waist level. AROM is generally initiated in a supine position. Modifications may be necessary based on each individual's progression at this point in their rehabilitation, and side-lying (Figures 3 and 4) and prone (Figure 5) positions may be utilized prior to progression to standing and seated positions as neuromuscular control and endurance improves. The following exercises have been indicated in the literature to produce the highest electromyographic (EMG) activity of the rotator cuff musculature without compensation of larger muscle groups. These exercises may require modification based on each patient's ability to recruit the proper musculature following SCR. Biofeedback can be a beneficial tool to improve functional neuromuscular re-education of the rotator cuff, deltoid, and periscapular musculature in this phase of rehabilitation.
Figure 3.
Slideboard-assisted scaption for deltoid activation.
Figure 4.
Slideboard-assisted forward elevation in the scapular plane.
Figure 5.
Sidelying abduction.
Regarding external rotation of the glenohumeral joint, side-lying external rotation and prone external rotation abduction exercises have been documented to provide the highest EMG activation of the infraspinatus.29-32 Side-lying external rotation with a towel roll in the axilla should be trialed first, as prone external rotation abduction exercises may place excessive tensile load on the repaired tissue due to insufficient muscular strength to perform these exercises effectively. The towel roll places the glenohumeral joint in the scapular plane, which facilitates an adduction moment upon the glenohumeral joint, thereby reducing capsular stress, improving scapular stability and increasing EMG activity of the targeted musculature.30,33 Initially, patients will lack sufficient strength to move through the available range of motion. The physical therapist can begin with manual placement of the glenohumeral joint in various degrees of external rotation and have the patient perform isometric holds. Alternatively, gentle rhythmic stabilization may also be utilized. The glenohumeral joint can also be placed at the end range of available external rotation following isometric holds allowing the patient to perform the eccentric portion of the exercise by returning the arm to neutral. Active external rotation can also be performed in a seated position utilizing a slideboard for assistance as needed. Keep in mind the potential limited range of motion with this movement based on each patient's pre-surgical level of function, the availability and integrity of salvageable external rotator cuff tissue.
The subscapularis and pectoralis musculature work in concert with the external rotation musculature to establish the internal/external rotator force couple that functions in concert with the deltoid. Subscapularis activation is initially facilitated with isometrics and external rotation exercises. Alizadehkhaiyat et al. reported increased EMG activity of the subscapularis with prone external rotation and horizontal abduction exercises.34 Deltoid function is imperative following SCR to restore the force couples about the glenohumeral joint. Initially, the deltoid should be activated utilizing multi-angle submaximal isometrics prior to progressing to isotonics. It is beneficial to begin deltoid isotonics with the patient in a side-lying (Figures 3 and 4) or supine (Figure 1) position. Patients can begin in a side-lying position to perform glenohumeral abduction in the coronal plane of the body (Figure 3), as well as horizontal abduction in the transverse plane (Figures 4 and 5). Assisted scaption exercises performed on a slideboard with the patient prone (Figure 2) or supine (Figure 1) are beneficial to facilitate deltoid function in a functional position without excess gravitational resistance prior to progressing to seated or standing scaption exercises.
The prone full-can exercise has been proven to generate good electromyographic activity of the posterior deltoid and the lower trapezius.35,36 This exercise may need to be performed with slideboard assistance prior to performing it unassisted in a prone position, with the final progression to an upright position. Another option to promote functional re-training of the deltoid is the patient performing a press to 90 ° of glenohumeral forward elevation in a supine position (Figure 6), and subsequently progressing to an incline press. The aforementioned exercises facilitate concentric and eccentric muscular endurance of the posterior, middle, and anterior portions of the deltoid. Isotonic external rotation exercises of the glenohumeral joint, as described above, also promote activation of the posterior deltoid.
Figure 6.
Horizontal abduction.
The serratus anterior, which protracts the scapula, plays a crucial role in establishing normal scapulohumeral rhythm and is an integral component of establishing glenohumeral motion above 90 °. Serratus anterior isotonics can be performed initially in a supine or prone position with the glenohumeral joint at 90 ° of forward elevation while performing the serratus “plus” exercise to protract the scapula while maintaining a static glenohumeral position. Emphasis is placed on proper protraction and retraction to the neutral position of the scapula at 90 °, progressing to scapular protraction at various angles of forward elevation and/or scaption in conjunction with the progression to upright positions while promoting neuromuscular control of the glenohumeral joint. Open chain scapular exercise is emphasized during this phase of rehabilitation in order to establish proper scapulothoracic force couples and improve neuromuscular endurance with AROM activities. Closed chain scapular exercise is initiated during Phase III of the rehabilitation process in order to allow sufficient time to develop proper dynamic stability prior to the initiation of compressive forces on the glenohumeral joint.
Establishing scapular stability is imperative to normalize scapulohumeral rhythm to promote optimal function following SCR. Scapular control is initiated in Phase I and is progressed during Phase II by emphasizing proper scapular position, neuromuscular control, and endurance of the serratus anterior, rhomboids, and middle and lower trapezius muscles throughout all AROM exercises while reducing upper trapezius compensation patterns. It is important to establish normal scapulohumeral rhythm with AROM prior to the initiation of resisted ROM in order to promote proper muscle activation and to reduce compensation patterns. Manual therapy techniques can also be utilized throughout this phase as indicated, keeping in mind the repaired tissues and healing timelines. Manual techniques include but are not limited to soft tissue mobilization, joint mobilizations, contract/relax techniques and low load, long duration stretching. These techniques should be appropriately selected to improve mobility and/or decrease pain.
This phase of rehabilitation can potentially require a significant amount of time to properly retrain the remaining rotator cuff musculature, deltoid, and periscapular musculature to function in concert with the superior capsule graft. The level of function exhibited by each patient prior to surgery should be taken into consideration. Massive, chronic rotator cuff tears generally take an extended duration of time to rehabilitate, regardless of the type of surgical intervention performed.
Phase III – Muscular Strength
The muscular strength phase is generally introduced at 10-12 weeks postoperatively and consists of progressive resisted ROM and the initiation of closed chain exercises. The rehabilitation goals of phase III include advancement of strength and restoration of functional ROM, progressing to higher level functional activities.
Strengthening should be initiated with light resistance bands and/or light dumbbell isotonics, and the initiation of closed chain stabilization exercises should incorporate light weights or resistance and have a functional basis. All resisted exercises should be performed with the underlying goal of improving functional ROM and strength, while ensuring normal scapulohumeral rhythm is maintained.
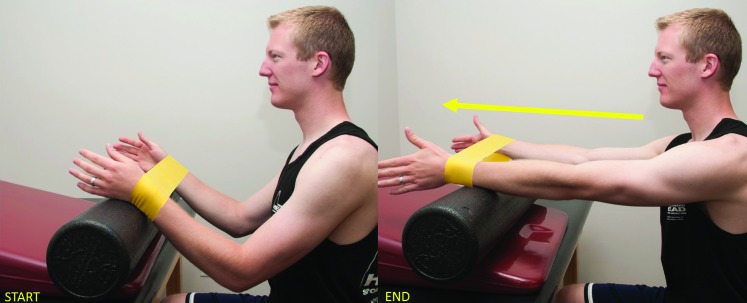
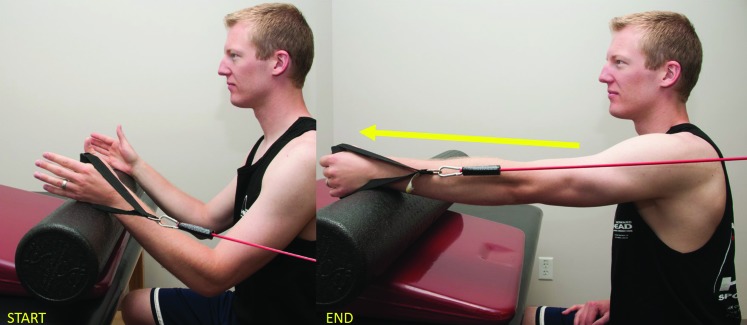
Resistance is initially applied with the addition of light dumbbells or light resistance bands to the non-resisted isotonic exercises previously described in Phase II. Resistance band exercises, which provide concentric and eccentric components, can be incorporated below shoulder level in the scapular plane at this time. Patients may not be able to perform full active motion initially with the addition of resistance; therefore, initial band strengthening may consist of isometric holds or require modified positions for optimal muscle activation without compensation. The internal and external rotators of the glenohumeral joint are commonly strengthened in a standing position with a towel roll under the arm to place the glenohumeral joint in a neutral scaption position. Forward punches to 90 ° of glenohumeral forward elevation with a “plus” are utilized to promote strengthening of the serratus anterior and for functional strength above waist level (Figures 7 and 8). These may need to be initiated in a seated assisted position prior to transition to standing. Resisted rows are also commenced at this time, beginning first in a prone position with light dumbbells prior to transitioning to standing position with resistance bands. Resisted biceps and triceps exercises can also be incorporated at this time with either light dumbbell or band resistance, progressing as appropriate. Resisted exercises can be progressed to shoulder height and above as tolerated by the patient. It is imperative to emphasize proper scapular position in order to maintain proper glenohumeral kinematics with the addition of the resisted load.
Figure 7.
Prone extension with external rotation.
Figure 8.
Forward elevation with resistance band to facilitate external rotation.
Figure 9.
Seated, assisted forward elevation with external rotation resistance.
Figure 10.
Single-arm assisted forward elevation with serratus assisted plus.
Proprioceptive exercises are also progressed within this phase with the addition of a TheraBandTM FlexBar® (Performance Health, Akron, OH, USA), resistance band, or manual perturbations in various functional positions beginning below shoulder height in the scapular plane, progressing to shoulder height as appropriate. Initial closed kinetic chain exercises are also initiated to improve neuromuscular control, muscular strength and proprioception of the glenohumeral joint. Closed chain exercises are typically initiated in a low load position while standing with hands on a wall, progressing to a declined or quadruped position. Plank positions on the floor may be too demanding at this time secondary to strength deficits for patients who have undergone SCR. Initial closed chain activities consist of weight shifts, scapular protraction/retraction “plus,” static holds with and without manual perturbations, double arm to single arm support, and shallow push-ups if appropriate. It is important to consider the functional deficits of each patient when prescribing specific exercises, ensuring they are appropriate for and relate to established functional goals.
This is typically the final phase of rehab prior to discharge from physical therapy depending on each patient's functional requirements for daily activities, work and recreational activities. Physical therapists should expect to spend an extended duration of time in this phase of rehabilitation for patients who have undergone SCR as compared to those who have undergone massive rotator cuff repair. Patients who do not require high levels of overhead function and exhibit sufficient strength may begin to return to full daily activities and recreational activities below shoulder level. Patients whose activities demand a higher level of function from the shoulder, including repetitive or overhead activities, may find themselves limited initially as preliminary outcome studies following SCR indicate functional improvements up to two years postoperatively.13
Phase IV – Advanced Strength and Return to Activity
This phase of rehabilitation typically consists of overhead strengthening, advanced closed chain, proprioceptive and plyometric exercises. Based on the functional status and strength achieved at this point post-operatively, patients may or may not be appropriate for this phase of rehabilitation. The physical therapist should focus on specific functional requirements based on strength deficits.
As patients continue to build strength, treatment should focus on progressing endurance with high-exertion daily activities as well as work and recreational activities at or below shoulder height. It may be challenging for patients who undergo SCR to return to work activities requiring heavy lifting or repetitive overhead lifting as they may not demonstrate sufficient strength to support these types of activities. Return to higher level overhead sports may also prove difficult, and patients may not be able to achieve sufficient muscular power required for these types of activities. Physical therapists and patients can instead focus on recreational activities performed at or below shoulder height, including but not limited to cycling, shooting and golfing.
CONCLUSION
This clinical commentary describes a rehabilitation protocol following superior capsule reconstruction. Post-operative rehabilitation begins with close communication between the surgeon, the patient, and the physical therapy team. A review of surgical findings is mandatory to establish rehabilitation guidelines. Once post-operative restrictions have been established, a rehabilitation protocol is customized based on surgical findings and patient goals. The standard protocol is characterized by four phases and starts with restrictions on movement lasting six weeks. The aim is to minimize stress placed on the implanted graft to facilitate early graft-to-bone healing. Afterwards, Phase II starts with restoring passive and active range of motion, managing pain, and improving endurance of the rotator cuff. Phase III consists of advancement of strength and functional restoration of ROM followed by Phase IV consisting of overhead strengthening, advanced closed chain, proprioceptive and plyometric exercises, as appropriate.
References
- 1.Bedi A Dines J Warren RF Dines DM. Massive tears of the rotator cuff. J Bone Joint Surg Am. 2010;92:1894-1908. [DOI] [PubMed] [Google Scholar]
- 2.Greenspoon JA Petri M Warth RJ Millett PJ. Massive rotator cuff tears: pathomechanics, current treatment options, and clinical outcomes. J Shoulder Elbow Surg. 2015;24:1493-1505. [DOI] [PubMed] [Google Scholar]
- 3.Laron D Samagh SP Liu X Kim HT Feeley BT. Muscle degeneration in rotator cuff tears. J Shoulder Elbow Surg. 2012;21:164-174. [DOI] [PubMed] [Google Scholar]
- 4.Galatz LM Ball CM Teefey SA Middleton WD Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86-a:219-224. [DOI] [PubMed] [Google Scholar]
- 5.Yamaguchi K Tetro AM Blam O Evanoff BA Teefey SA Middleton WD. Natural history of asymptomatic rotator cuff tears: a longitudinal analysis of asymptomatic tears detected sonographically. J Shoulder Elbow Surg. 2001;10:199-203. [DOI] [PubMed] [Google Scholar]
- 6.Zingg PO Jost B Sukthankar A Buhler M Pfirrmann CW Gerber C. Clinical and structural outcomes of nonoperative management of massive rotator cuff tears. J Bone Joint Surg Am. 2007;89:1928-1934. [DOI] [PubMed] [Google Scholar]
- 7.Berth A Neumann W Awiszus F Pap G. Massive rotator cuff tears: functional outcome after debridement or arthroscopic partial repair. J Orthop Traumatol. 2010;11:13-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Burkhart SS Nottage WM Ogilvie-Harris DJ Kohn HS Pachelli A. Partial repair of irreparable rotator cuff tears. Arthroscopy. 1994;10:363-370. [DOI] [PubMed] [Google Scholar]
- 9.Heuberer PR Kolblinger R, Buchleitner S, et al. Arthroscopic management of massive rotator cuff tears: an evaluation of debridement, complete, and partial repair with and without force couple restoration. Knee Surg Sports Traumatol Arthrosc. 2015. [DOI] [PubMed] [Google Scholar]
- 10.Zvijac JE Levy HJ Lemak LJ. Arthroscopic subacromial decompression in the treatment of full thickness rotator cuff tears: a 3- to 6-year follow-up. Arthroscopy. 1994;10:518-523. [DOI] [PubMed] [Google Scholar]
- 11.Namdari S Voleti P Baldwin K Glaser D Huffman GR. Latissimus dorsi tendon transfer for irreparable rotator cuff tears: a systematic review. J Bone Joint Surg Am. 2012;94:891-898. [DOI] [PubMed] [Google Scholar]
- 12.Mihata T McGarry MH Pirolo JM Kinoshita M Lee TQ. Superior capsule reconstruction to restore superior stability in irreparable rotator cuff tears: a biomechanical cadaveric study. Am J Sports Med. 2012;40:2248-2255. [DOI] [PubMed] [Google Scholar]
- 13.Mihata T Lee TQ Watanabe C, et al. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 2013;29:459-470. [DOI] [PubMed] [Google Scholar]
- 14.Petri M Greenspoon JA Millett PJ. Arthroscopic Superior Capsule Reconstruction for Irreparable Rotator Cuff Tears. Arthrosc Tech. 2015;4:e751-755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ahmad CS Kleweno C Jacir AM, et al. Biomechanical performance of rotator cuff repairs with humeral rotation: a new rotator cuff repair failure model. Am J Sports Med. 2008;36:888-892. [DOI] [PubMed] [Google Scholar]
- 16.Su WR Budoff JE Luo ZP. The effect of anterosuperior rotator cuff tears on glenohumeral translation. Arthroscopy. 2009;25:282-289. [DOI] [PubMed] [Google Scholar]
- 17.Burkhart SS. Arthroscopic treatment of massive rotator cuff tears. Clinical results and biomechanical rationale. Clin Orthop Relat Res. 1991:45-56. [PubMed] [Google Scholar]
- 18.Burkhart SS. Fluoroscopic comparison of kinematic patterns in massive rotator cuff tears. A suspension bridge model. Clin Orthop Relat Res. 1992:144-152. [PubMed] [Google Scholar]
- 19.Parsons IM Apreleva M Fu FH Woo SL. The effect of rotator cuff tears on reaction forces at the glenohumeral joint. J Orthop Res. 2002;20:439-446. [DOI] [PubMed] [Google Scholar]
- 20.Thompson WO Debski RE Boardman ND 3rd, et al. A biomechanical analysis of rotator cuff deficiency in a cadaveric model. Am J Sports Med. 1996;24:286-292. [DOI] [PubMed] [Google Scholar]
- 21.Hansen ML Otis JC Johnson JS Cordasco FA Craig EV Warren RF. Biomechanics of massive rotator cuff tears: implications for treatment. J Bone Joint Surg Am. 2008;90:316-325. [DOI] [PubMed] [Google Scholar]
- 22.Nam D Maak TG Raphael BS Kepler CK Cross MB Warren RF. Rotator cuff tear arthropathy: evaluation, diagnosis, and treatment: AAOS exhibit selection. J Bone Joint Surg Am. 2012;94:e34. [DOI] [PubMed] [Google Scholar]
- 23.Gerber C Fuchs B Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000;82:505-515. [DOI] [PubMed] [Google Scholar]
- 24.Katthagen J, Tahal D, Millett P. Arthroscopic Superior Capsule Reconstruction for Irreparable Rotator Cuff Tears. Orthopaedics Today. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gupta AK Hug K Boggess B Gavigan M Toth AP. Massive or 2-tendon rotator cuff tears in active patients with minimal glenohumeral arthritis: clinical and radiographic outcomes of reconstruction using dermal tissue matrix xenograft. Am J Sports Med. 2013;41:872-879. [DOI] [PubMed] [Google Scholar]
- 26.Osbahr DC Cawley PW Speer KP. The effect of continuous cryotherapy on glenohumeral joint and subacromial space temperatures in the postoperative shoulder. Arthroscopy. 2002;18:748-754. [DOI] [PubMed] [Google Scholar]
- 27.Thigpen CA Shaffer MA Gaunt BW Leggin BG Williams GR Wilcox RB 3rd. The American Society of Shoulder and Elbow Therapists’ consensus statement on rehabilitation following arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2016;25:521-535. [DOI] [PubMed] [Google Scholar]
- 28.Wilk KE Arrigo C. Current concepts in the rehabilitation of the athletic shoulder. J Orthop Sports Phys Ther. 1993;18:365-378. [DOI] [PubMed] [Google Scholar]
- 29.Ballantyne BT O’Hare SJ Paschall JL, et al. Electromyographic activity of selected shoulder muscles in commonly used therapeutic exercises. Phys Ther. 1993;73:668-677; discussion 677-682. [DOI] [PubMed] [Google Scholar]
- 30.Reinold MM Wilk KE Fleisig GS, et al. Electromyographic analysis of the rotator cuff and deltoid musculature during common shoulder external rotation exercises. J Orthop Sports Phys Ther. 2004;34:385-394. [DOI] [PubMed] [Google Scholar]
- 31.Blackburn TA McLeod WD White B Wofford L. EMG analysis of posterior rotator cuff exercises. Athl Train. 1990;25:41-45. [Google Scholar]
- 32.Townsend H Jobe FW Pink M Perry J. Electromyographic analysis of the glenohumeral muscles during a baseball rehabilitation program. Am J Sports Med. 1991;19:264-272. [DOI] [PubMed] [Google Scholar]
- 33.Graichen H Hinterwimmer S von Eisenhart-Rothe R Vogl T Englmeier KH Eckstein F. Effect of abducting and adducting muscle activity on glenohumeral translation, scapular kinematics and subacromial space width in vivo. J Biomech. 2005;38:755-760. [DOI] [PubMed] [Google Scholar]
- 34.Alizadehkhaiyat O Hawkes DH Kemp GJ Frostick SP. Electromyographic analysis of the shoulder girdle musculature during external rotation exercises. Orthop Journal Sports Med. 2015;3:2325967115613988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ekstrom RA Donatelli RA Soderberg GL. Surface electromyographic analysis of exercises for the trapezius and serratus anterior muscles. J Orthop Sports Phys Ther. 2003;33:247-258. [DOI] [PubMed] [Google Scholar]
- 36.Reinold MM Macrina LC Wilk KE, et al. Electromyographic analysis of the supraspinatus and deltoid muscles during 3 common rehabilitation exercises. J Athl Train. 2007;42:464-469. [PMC free article] [PubMed] [Google Scholar]