Abstract
Cancer care is highly complex and suffers from fragmentation and lack of coordination across provider specialties and clinical domains. As a result, patients often find that they must coordinate care on their own. Coordinated delivery teams may address these challenges and improve quality of cancer care. Task interdependence is a core principle of rigorous teamwork and is essential to addressing the complexity of cancer care, which is highly interdependent across specialties and modalities. We examined challenges faced by a patient with early-stage breast cancer that resulted from difficulties in understanding and managing task interdependence across clinical domains involved in this patient’s care. We used team science supported by the project management discipline to discuss how various task interdependence aspects can be recognized, deliberately designed, and systematically managed to prevent care breakdowns. This case highlights how effective task interdependence management facilitated by project management methods could markedly improve the course of a patient’s care. This work informs efforts of cancer centers and practices to redesign cancer care delivery through innovative, practical, and patient-centered approaches to management of task interdependence in cancer care. Future patient-reported outcomes research will help to determine optimal ways to engage patients, including those who are medically underserved, in managing task interdependence in their own care.
INTRODUCTION
Contemporary oncology offers unprecedented scientific achievements that promise treatments or cures for many cancers by a multitude of diagnostic and treatment modalities.1 Yet, equally unprecedented are the complexity, fragmentation, and poor coordination in the delivery of these modalities to patients with cancer across clinical specialties.2 Patients often must coordinate their own care, which increases their burden and potentially leads to life-saving treatments being delayed or forgone while avoidable care and costs are incurred.3-7 These issues contribute to the situation the Institute of Medicine (IOM) describes as a system in crisis.2
The delivery of cancer care as a team—defined as two or more people interacting dynamically, interdependently, and adaptively to achieve a common goal8,9—is hoped to provide a solution to care fragmentation.10,11 Success of rigorous teamwork in non–health care industries12,13 and in treating chronic diseases14,15 creates a unique opportunity to apply teamwork principles to oncology. In this article, we focus on one of the central teamwork principles: task interdependence. We define task interdependence, describe it in the context of cancer care, and demonstrate how its active management can mitigate and/or prevent care delivery breakdowns as a result of poor coordination. In the effort to follow IOM recommendations,16 we propose an adaptation of concepts from the project management discipline to facilitate task interdependence management in oncology. We use the example of early breast cancer diagnosis and treatment, which could be considered the epitome of multidomain complexity and fragmentation.4,10,17-19
This article builds upon work by Taplin et al,20 which explored team interdependence during breast cancer diagnosis. We advance this topic by focusing on the next challenging phase of breast cancer care (ie, postdiagnosis treatment), which further examines the principle of task interdependence as a component of team interdependence and describes the systematic application of this principle in cancer care by using project management.
CASE SUMMARY
The patient is a 32-year-old female who is newly married, wishes to have children, and lives in a low-income suburb of an urban area. She is unemployed and has Medicaid insurance. The patient has stage II, 3-cm, triple-positive, clinically node-negative breast cancer. Parties involved in the patients’s case are the patient, the surgical office at a large hospital, the local oncology office, genetic counseling at the large hospital, an out-of-state genetic laboratory, a stand-alone fertility clinic, a local dental office, a local primary care provider, the psychosocial office at the large hospital, and the patient’s Medicaid insurance.
During her care, the patient experiences four situations in which parties fail to recognize that their tasks are interdependent with those of the other parties and/or do not effectively manage this interdependence. Consequently, the patient’s care is delayed or missed, which leads to suboptimal outcomes.
Neoadjuvant Therapy
Neither the patient nor the provider offices (surgical, oncology, PCP) manage the interdependence among the oncologist consult, completion of neoadjuvant therapy, and surgery. After referral mishaps and difficulty in finding an oncologist who accepts Medicaid insurance, the patient receives a much-delayed oncology consult when she is already scheduled for a preoperative surgical appointment, which left no time for neoadjuvant therapy. Having not received psychosocial assessment and care until adjuvant therapy, the patient experiences anxiety about delays and proceeds with a mastectomy and thus forgoes a chance for preoperative tumor reduction and breast-conserving surgery.
Genetic Testing
The patient undergoes a genetic assessment preoperatively to incorporate the results in her surgical decision. However, the interdependence between obtaining genetic results and the surgical decision was not managed by the providers involved (surgical office, genetic counseling, genetic laboratory). Delay in Medicaid’s authorization contributes to task misalignment. Consequently, results arrive on the day of the patient’s mastectomy. The patient regrets not knowing her positive mutation status; with that information, she would have preferred a bilateral mastectomy and oophorectomy. Eventually, she receives contralateral mastectomy, additional reconstruction, and oophorectomy.
Fertility Preservation
The patient and her husband wish to undergo fertility preservation, but the interdependence between completion of fertility preservation and start of systemic therapy is not recognized by the fertility office or is managed by the oncology office. A delayed fertility appointment and projected start of the procedure conflict with the beginning of systemic therapy. Filled with anxiety, the patient proceeds with the latter without the former. Her fertility is impaired by systemic therapy.
Dental Care
Although repeatedly warned by her oncologist, the patient procrastinates in obtaining much-needed dental care before the start of systemic therapy. When she finally seeks dental care, she has difficulty finding a dentist who accepts Medicaid. She develops a severe dental infection and a subsequent drop in blood count, which causes hospitalization, interruption of systemic therapy, and the need for colony-stimulating factor support. Here, the patient first ignored the interdependence between completion of dental work and the start of systemic therapy and then had difficulty managing this interdependence due to out-of-pocket costs. The full case study appears in the Data Supplement along with two additional studies not analyzed in the article.
INTRODUCTION OF TASK INTERDEPENDENCE
Task interdependence is the degree to which the interaction and coordination of team members are required to complete tasks.21,22 It is considered one of the most important team design features23-25 and has been found to be a crucial contributor to team effectiveness.26-28 In health care, task interdependence affects provider performance across conditions and settings29-33 and improves the patient-centered focus of care teams.34
Although the importance of task interdependence has been recognized for decades,35-37 its significance in contemporary teamwork continues to increase. As teams become dynamic, fluid, and less formal, task interdependence defines a team and is the link that connects team members, even those not belonging to one formal organizational unit.38 This is highly relevant in health care, where teams are inherently fluid.33,34,39
Studies have shown that task interdependence management is challenging in cancer care because of the complexity of cancer care delivery, lack of tools to coordinate tasks across providers and organizations, care delays caused by insurance authorization, and other reasons.17,40,41 However, the opportunities to address these challenges, optimize task interdependence, and assess its impact on cancer care remain unexplored.9
EXPLANATION OF TASK INTERDEPENDENCE
Task interdependence is not merely a boundary of teamwork but an object of deliberate design and management.24,42,43 For it to contribute to team effectiveness in health care, task interdependence must be understood, designed within a specific care setting, and managed for individual patients. Following is an explanation of task interdependence in the context of these three steps (Table 1).
Table 1.
Understanding, Design, and Management of Task Interdependence
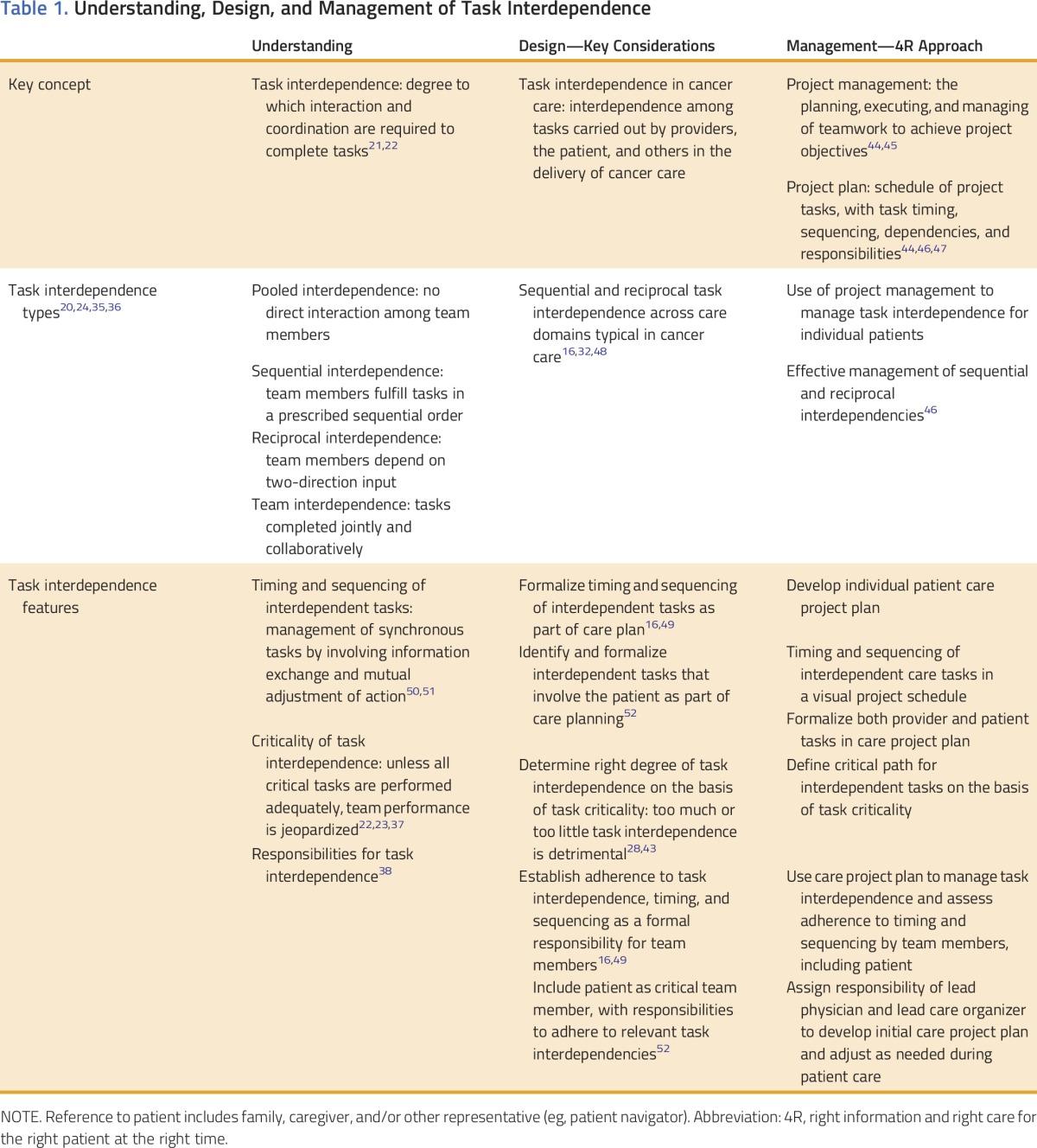
Understanding and Design of Task Interdependence in a Cancer Care Setting
An initial step in understanding task interdependence is the recognition of the types that exist in a specific setting. The literature describes four task interdependence types20,24,35,36 (Table 1), which in the real world exist in a hybrid.24,28,33,35 In cancer care, a complex hybrid of sequential and reciprocal task interdependence is common,16,32,48 where participants are both sequentially and reciprocally interdependent (eg, in the patient’s case, the genetic assessment depends on a surgeon’s referral, whereas the surgical decision depends on the genetic results). This complexity creates challenges and potential care breakdowns.4,16,17 Following are the features that further explain sequential and reciprocal task interdependence in general and in the context of cancer care.
Timing and sequencing.
These are inherently required for orchestrating sequentially interdependent tasks13,22,28,50 (Table 1). Timing is particularly central to designing and managing task interdependence in two aspects: relative timing of interdependent tasks13,50 and elapsed timing (the timeframe required to complete a task sequence53). Timeliness is an IOM-recommended dimension of quality10 and an important metric of care delivery.16,54 However, timing of cancer care remains challenging2,3 because it causes breakdowns in interdependent care, delays, and patient loss to follow-up.17,19,49,55 To ensure effective cancer care delivery, timing and sequencing of interdependent tasks should be formalized and documented in a written patient care plan16,49,56 (Table 1). We propose that care planning be the responsibility of the lead physician supported by the lead care organizer, both of whom are described later in this article.
Criticality.
Another important task interdependence feature, criticality,23,37 determines how important the interdependence between tasks is to the overall task work performance22,25,43 (Table 1). Criticality is used to design the right level of task interdependence. The design of too much or too little task interdependence may be detrimental to teamwork,28,43 with coordination costs outweighing benefits.35,57 Thus, to achieve the right degree of task interdependence is important. The concept of criticality is instrumental in determining which tasks are included in interdependent task design and management.24 In oncology, coordination is complex and costly, and certain tasks may be performed autonomously29,30,34; thus, the attainment of the right degree of task interdependence on the basis of criticality is necessary.
Responsibilities for task interdependence.
Clear assignment of responsibilities is important for effective task interdependent teamwork.21,38,42,58 In oncology, experts call for clearly identifying responsibilities for various portions of cancer diagnosis10,20 and care.2,3 We further propose to establish an explicit, formal responsibility for timing and sequencing of critically interdependent tasks among care team members (Table 1). Of note, care coordinators or patient navigators, although beneficial overall, are not able to fully orchestrate interdependent tasks in a time-sensitive fashion unless task participants themselves recognize and incorporate interdependence in their practices.52,56 For example, in the patient’s case, the genetic office and genetic laboratory need to streamline their workflows to deliver timely genetic testing for patients like the patient who is awaiting test results for surgical decisions. Navigators or coordinators rarely have the authority to facilitate such workflow adjustment across provider offices or organizations.
Patient-centered approach to task interdependence.
An IOM report explored the merit, opportunities, and barriers of forging partnerships between patients and care teams, including patient engagement as a team member with explicit responsibilities.52 It may be particularly important to involve patients as team members because many patient tasks are interdependent with provider tasks, and task timing and sequencing may have crucial health implications. Patient tasks with critical interdependence should be identified, and their timing and sequencing should be formalized as his or her responsibility (Table 1). For patients unable or unwilling to assume task interdependent responsibilities, involvement of a family member, caregiver, or another representative (eg, navigator) who could facilitate the patient’s tasks may present a viable alternative. (In this article, reference to the patient includes the family/caregiver and/or representative.)
Management of Task Interdependence in Care for Individual Patients With Cancer as a Project: The 4R Approach
Scholars advise that task interdependence should be deliberately and explicitly managed during the course of teamwork.35,50 Accordingly, task interdependence for individual patients with cancer should be defined at diagnosis and actively managed during a patient’s care. This is challenging10,16 because of the complexity of care timing and sequencing, the multitude of providers involved in care for one patient, as well as other reasons as illustrated by the patient’s case.
To address these challenges, we propose the use of project management, the discipline of planning, executing, and managing the work of a team to achieve project objectives.44,45 Project management uses a project plan to define the timing and sequencing of tasks, clearly specify team members’ responsibilities, and specify task dependencies.44,46,47 It is broadly used to manage complex task interdependence in many industries.46,47 In health care, the approach to every patient’s care as a project has been proposed56,59,60 but unexplored. Project management is inherently fitting to manage task interdependence in cancer care because it addresses key dimensions and design considerations (Table 1) and allows adaptability during a patient’s episode of care. Many patients are familiar with project management from their workplaces as are many providers through quality improvement and other organizational projects.31,33
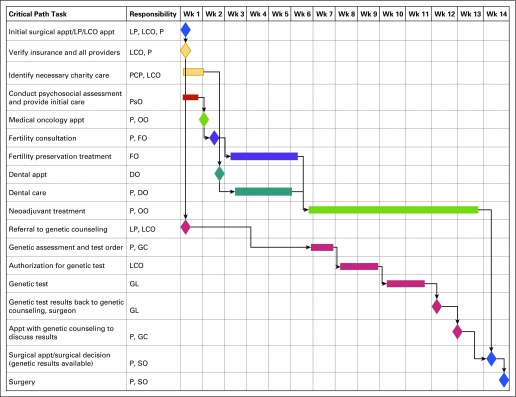
We propose that the care plan for a patient with cancer be developed at diagnosis as an individualized project plan that defines the timing and sequencing of interdependent tasks and clearly indicates patient and provider responsibilities. The patient and all providers involved in his or her care use the care project plan to manage tasks at the right time and in the right sequence (Fig 1). Plan development and management are performed by a designated role of the lead physician (assumed by a surgeon, oncologist, or another physician) and lead care organizer (assumed by a nurse and/or navigator). The lead physician and lead care organizer facilitate care planning and task interdependence management across the care team, including various specialties, offices, and practices. This approach is termed 4R—right information and right care for the right patient at the right time.61 4R facilitates patient-centered care by providing a patient with information and control over critical tasks while following the IOM mandate that the patient is the source of control in his or her care.10 For patients and/or caregivers unable or unwilling to play an active role, the team should designate a representative (eg, navigator) to facilitate the patient’s interdependent tasks on the patient’s behalf.
FIG 1.
Example of a care project plan: visual project schedule. Appt, appointment; DO, dental office; FO, fertility office; GC, genetic counseling; GL, genetic laboratory; LCO, lead care organizer; LP, lead physician; OO, oncology office; P, patient; PCP, primary care physician; PsO, psychosocial office; SO, surgical office; Wk, week.
APPLICATION TO THE CASE
In the patient’s case, task interdependence was not addressed at any of the three necessary levels. It was not understood; not explicitly designed in the patient’s care setting; and not managed by the patient, her providers, or Medicaid insurance (Table 2). Care tasks were not effectively sequenced or timed (eg, oncologist consult versus surgical decision, referral to fertility preservation versus systemic therapy); critical tasks were not treated as such (eg, receipt of the genetic results to inform the surgical decision); assumed sequential interdependencies were unnecessary and not at the right level (eg, insurance verification after genetic consult); and responsibilities for adhering to task interdependence were not clarified or fulfilled (eg, the patient did not obtain dental care before systemic therapy). Next is an optimized scenario that shows how key task interdependence aspects and the 4R approach could be applied to the patient’s case.
Table 2.
Task Interdependence in the Case of the Patient
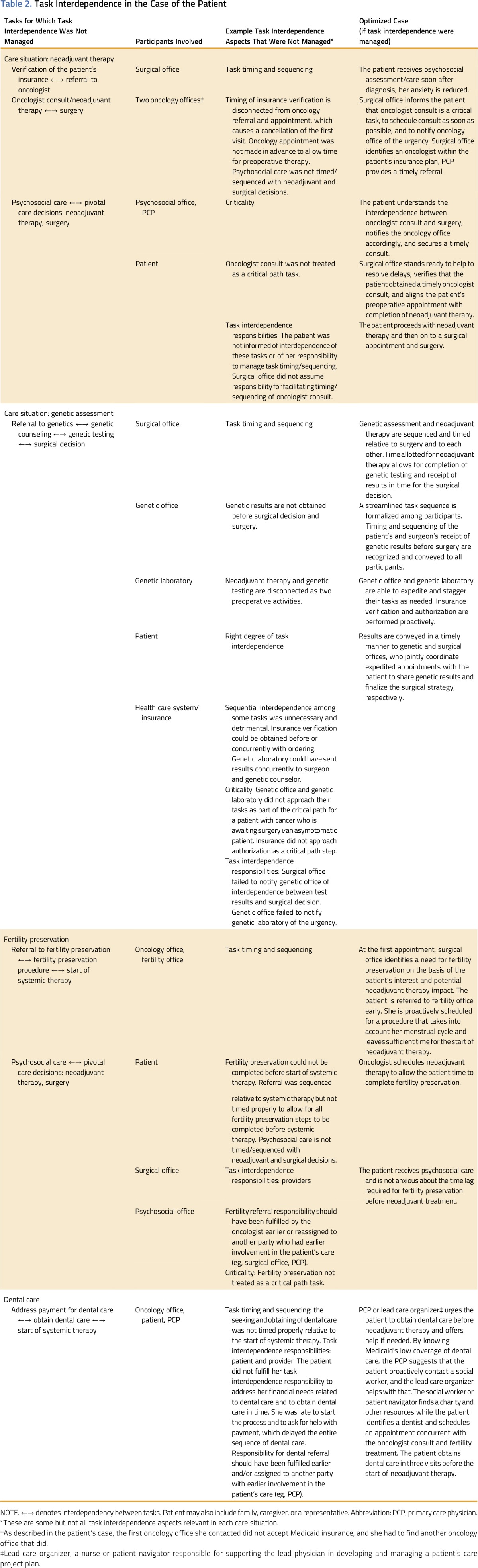
Task Interdependencies in the Patient’s Care Setting
In an optimized scenario, long before the patient’s arrival, her providers recognize the importance of task interdependence and understand how it affects care for their mutual patients. They realize the detrimental implications of ignoring task interdependence in their patients’ care and do not consider the management of task interdependence an administrative burden. They are educated on task interdependence basics, including timing and sequencing, and agree with the importance of explicit provider and patient responsibilities. Typical problematic situations in which task interdependence is mismanaged for patients (eg, the four situations in the patient’s case) are identified. Providers understand that interdependent care for one patient spans multiple domains and organizations (eg, surgical office in a large hospital, local oncology office, out-of-state genetic laboratory, stand-alone dental office) and agree to work with relevant organizations to manage task interdependence for mutual patients. The creation of such awareness requires a concerted educational effort and leadership across and within institutions. Although this effort is far from trivial, its accomplishment is feasible as institutions grow more accustomed to collaboration and as task interdependence concepts become intuitive to many providers who implicitly manage numerous interdependent tasks.
4R Approach to Task Interdependence Design in the Patient’s Care Setting
An understanding of task interdependence is necessary but not sufficient to prepare providers and the patient to systemically manage task interdependence in the patient’s care. Before the patient’s arrival, providers should collaborate to deliberately design and document task interdependence for problematic situations identified in the first step. A task interdependence working group that represents institutions and practices that share care for patients like the one in this setting should be formed to accomplish these tasks. The working group would facilitate discussions and agreement about critical interdependent care tasks, their timing and sequencing, and typical responsibilities. The working group could use the 4R approach and project management to proactively document this design in the form of templates for care project plans. A visual of the project schedule may help to depict timing, sequencing, and responsibilities for care events across the entire care episode (Fig 1). Templates that are not only disease specific (eg, breast cancer) but also patient-subgroup specific would be beneficial. For example, providers would agree on a care project template for young patients with early-stage breast cancer who are indicated for neoadjuvant therapy and genetic assessment and who are interested in fertility preservation. In this way, providers are prepared to manage critical interdependent tasks for the patient. Thereafter, the working group would convene regularly to reassess and, if needed, adjust the care project templates.
4R Approach to Managing Task Interdependencies in the Patient’s Care Setting
In an optimized scenario, after the patient’s diagnosis and referral to a surgical office, she is assigned a lead physician (eg, her surgeon) and lead care organizer who supports the lead physician (eg, a patient navigator). Jointly with the patient, they develop the patient’s initial care project plan. A project template is used and adjusted collaboratively with the patient to reflect her preferences (eg, interest in neoadjuvant therapy, preoperative genetic assessment, fertility preservation). Critical care events timing and sequencing are documented in a visual project schedule (Fig 1).
The lead care organizer identifies potential providers in the patient’s care plan, discusses them with the patient, and proactively verifies their eligibility in the patient’s insurance network. Providers are explicitly assigned to time-sensitive tasks, and their offices are alerted. The lead care organizer discusses the patient’s responsibilities for time-sensitive tasks, such as to seek timely appointments, convey care delays, and report adverse symptoms in a timely fashion to the lead physician and lead care organizer. The patient explicitly agrees to these responsibilities. She and her providers proceed with her care according to the project plan. As described in Table 2, in each of the four situations, the patient’s care is now optimized. She receives neoadjuvant therapy and genetic test results before her surgical decision, which allows a more informed and expanded set of surgical options. The patient also is able to complete her fertility preservation procedure before neoadjuvant therapy and simultaneously obtains timely dental care to prevent infection, hospitalization, and treatment interruption (Fig 1).
During the patient’s care, her project plan may need adjustment to reflect her response to therapy and treatment strategy changes. The lead physician and lead care organizer work with the patient to adjust the project plan and alert participating providers of changes.
IMPLICATIONS FOR CLINICAL PRACTICE
At a time of health care reform, new payment and quality structures, such as accountable care organizations, embed increasing expectations for well-coordinated team-based care.62,63 This article describes a systematic, yet practical approach to facilitate cancer care coordination by managing task interdependence through the 4R method. We outlined at a high level how 4R could be applied in practice. However, the 4R implementation requires strategies to direct real-life implementation and adaptation of the approach to specific care settings and patient subgroups. The Comprehensive Dynamic Trial (CDT) method by Rapkin et al64 provides a structure for such implementation as a learning and continuous improvement system. This method recognizes over time new care settings, patient situations, and care tasks that need to be managed for interdependence and incorporates them into the care setting cyclically. Under CDT, a task interdependence champion and working group would be designated in a specific care setting to develop care project templates and establish key 4R components, including assignment of the lead physician responsibility among clinical specialties, communication mechanisms among team members, patient engagement methods that reflect patient population characteristics in a specific setting, and strategies for addressing insurance concerns. The working group would oversee the cyclical 4R implementation in its setting by using its accumulated experience to inform updates to care project templates and improve how the care teams and patients use them. (The Data Supplement describes the application of CDT to 4R implementation in more detail.)
Implementation of 4R may help cancer institutions to incorporate task interdependence–related metrics, such as timing and sequencing of guideline-recommended care, in institutional quality metrics and payer contracts. This will convey the value of their efforts and help reimbursement. Of note, payers are increasingly willing to incorporate payment for care coordination, including the role of lead physician and midlevel staff (who could assume the role of lead care organizer), in the new payment models.65,66 Further efforts will be necessary to ensure that the new payment models adequately account for these roles and activities.
Work with payers provides an opportunity to address another issue highlighted in this case study: Payer policies and practices contribute to care delays and misalignment (eg, delayed authorizations, lack of payment for a key procedure). Care project templates may be used to secure authorizations proactively or obtain an authorization for the project plan that spans an episode of care.
IMPLICATIONS FOR RESEARCH
This article raises a spectrum of research questions about the effectiveness of the 4R approach to manage task interdependence in cancer care. However, patient-centered research topics should be considered a priority. The literature demonstrates that patients desire an active role in treatment decision making and planning,67-70 but systemic, practice-level, attitudinal, and other barriers exist.70-72 Future research topics include not only patient engagement in treatment planning but also patient/caregiver involvement in the delivery of interdependent tasks as a care team member and whether the 4R approach can facilitate this involvement. Among the mechanisms of patient engagement, the role patient portals play in electronic medical records and decision support systems should be evaluated. Patient-reported outcomes research offers an effective methodology for examining these topics73,74 and informing patient-centered task interdependence management. In addition, as highlighted in this case, task interdependence may be especially challenging for medically vulnerable populations. The identification of effective mechanisms of empowering and supporting these populations to participate in teamwork will contribute to equitable cancer care delivery.
In conclusion, this article examines how task interdependence across providers and care events affects care for a patient with breast cancer and how this care can be improved by task interdependence recognition, deliberate design, and explicit management. By using project management, we describe how a patient’s care project plan that explicitly outlines sequencing, timing, and responsibilities for interdependent tasks helps to orchestrate complex care and prevent breakdowns. A patient-centered approach to task interdependence management is key to empowering patients to fulfill their tasks in care in a time- and sequence-sensitive manner that is based on patient preferences and goals. Care organizations may benefit from implementing formal task interdependence management along the cancer care continuum. Further research will guide the evolution of these concepts in cancer care.
ACKNOWLEDGMENT
The production of this manuscript was funded by the Conquer Cancer Foundation Mission Endowment. Supported by National Cancer Institute (NCI) Grant No. UG1CA189828 (J.R.T., M.A.S., C.B.W.), National Comprehensive Cancer Network/Pfizer Grant No. 22896331 (J.R.T., M.A.S., C.B.W.), grants from the Lynn Sage Cancer Research Foundation (J.R.T., M.A.S., C.B.W.; and S.A.K.); and by NCI Grant Nos. UG1CA189828 (R.C.C., A.B.B., I.F.G., L.I.W.), U54CA203000 (M.A.S.), U10CA017145 (A.B.B.), and 1UG1CA189859 (B.D.R.). This manuscript is the result of our team’s participation in the NCI-ASCO Teams in Cancer Care Delivery Project. The work was partially presented at the NCI-ASCO Teams in Cancer Care Delivery Workshop, Phoenix, AZ, February 25, 2016, in conjunction with the ASCO Quality Symposium.
AUTHOR CONTRIBUTIONS
Conception and design: Julia R. Trosman, Melissa A. Simon, Debra L. Madden, Bruce D. Rapkin, Elisa S. Weiss, Ilana F. Gareen, Lynne I. Wagner, Art Small, Christine B. Weldon
Administrative support: Julia R. Trosman, Christine B. Weldon
Collection and assembly of data: Julia R. Trosman, Ruth C. Carlos, Bruce D. Rapkin, Mikele M. Bunce, Christine B. Weldon
Data analysis and interpretation: Julia R. Trosman, Ruth C. Carlos, William J. Gradishar, Al B. Benson III, Seema A. Khan, Mikele M. Bunce, Art Small, Christine B. Weldon
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Care for a Patient With Cancer As a Project: Management of Complex Task Interdependence in Cancer Care Delivery
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or jop.ascopubs.org/site/misc/ifc.xhtml.
Julia R. Trosman
Consulting or Advisory Role: Genentech (Inst), Foundation Medicine (Inst)
Ruth C. Carlos
No relationship to disclose
Melissa A. Simon
No relationship to disclose
Debra L. Madden
Employment: Associated Neurologists
William J. Gradishar
No relationship to disclose
Al B. Benson III
Consulting or Advisory Role: Genentech, Sanofi, Bristol-Myers Squibb, Merck Serono, Merck, Schering-Plough, Spectrum Pharmaceuticals, Eli Lilly, ImClone Systems, Celgene, Genomic Health, National Cancer Institute, Vicus Therapeutics, Pharmacyclics, Holemics, Taiho Pharmaceutical, Bayer AG, Alchemia, Infinity Pharmaceuticals, Boehringer Ingelheim, Astellas, EMD Serono, IntegraGen
Research Funding: Genentech (I), Gilead Sciences, Amgen, Astellas, Advanced Accelerator Applications, Bayer AG, Onyx Pharmaceuticals, Novartis, Alchemia, AVEO Pharmaceuticals, Infinity Pharmaceuticals, Merck Serono (Inst), EMD Serono (Inst)
Travel, Accommodations, Expenses: Genentech, Eli Lilly, ImClone Systems, Bayer AG, Sanofi, Spectrum Pharmaceuticals, AVEO Pharmaceuticals, Gilead Sciences, Astellas
Bruce D. Rapkin
No relationship to disclose
Elisa S. Weiss
No relationship to disclose
Ilana F. Gareen
No relationship to disclose
Lynne I. Wagner
Consulting or Advisory Role: EveryFit, Janssen Pharmaceuticals, Gilead Sciences
Seema A. Khan
No relationship to disclose
Mikele M. Bunce
Employment: Genentech
Stock or Other Ownership: Genentech
Travel, Accommodations, Expenses: Genentech
Art Small
Employment: Genentech
Stock or Other Ownership: Genentech
Christine B. Weldon
Consulting or Advisory Role: Genentech (Inst), Foundation Medicine (Inst)
REFERENCES
- 1.Masters GA, Krilov L, Bailey HH, et al. Clinical cancer advances 2015: Annual report on progress against cancer from the American Society of Clinical Oncology. J Clin Oncol. 2015;33:786–809. doi: 10.1200/JCO.2014.59.9746. [DOI] [PubMed] [Google Scholar]
- 2. Levit L, Balogh E, Nass S, et al (eds): Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. Washington, DC, National Academies Press, 2013. [PubMed] [Google Scholar]
- 3.Balogh EP, Ganz PA, Murphy SB, et al. Patient-centered cancer treatment planning: Improving the quality of oncology care. Summary of an Institute of Medicine workshop. Oncologist. 2011;16:1800–1805. doi: 10.1634/theoncologist.2011-0252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bickell NA, McEvoy MD. Physicians’ reasons for failing to deliver effective breast cancer care: A framework for underuse. Med Care. 2003;41:442–446. doi: 10.1097/01.MLR.0000052978.49993.27. [DOI] [PubMed] [Google Scholar]
- 5.Nonzee NJ, Ragas DM, Ha Luu T, et al. Delays in cancer care among low-income minorities despite access. J Womens Health (Larchmt) 2015;24:506–514. doi: 10.1089/jwh.2014.4998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bickell NA, LePar F, Wang JJ, et al. Lost opportunities: Physicians’ reasons and disparities in breast cancer treatment. J Clin Oncol. 2007;25:2516–2521. doi: 10.1200/JCO.2006.09.5539. [DOI] [PubMed] [Google Scholar]
- 7.Gruman JC. An accidental tourist finds her way in the dangerous land of serious illness. Health Aff (Millwood) 2013;32:427–431. doi: 10.1377/hlthaff.2012.1083. [DOI] [PubMed] [Google Scholar]
- 8.Cohen SG, Bailey DE. What makes teams work: Group effectiveness research from the shop floor to the executive suite. J Manage. 1997;23:239–290. [Google Scholar]
- 9.Taplin SH, Weaver S, Salas E, et al. Reviewing cancer care team effectiveness. J Oncol Pract. 2015;11:239–246. doi: 10.1200/JOP.2014.003350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Institute of Medicine, Committee on Quality of Health Care in America: Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC, National Academies Press, 2001. [Google Scholar]
- 11.McCorkle R, Ercolano E, Lazenby M, et al. Self-management: Enabling and empowering patients living with cancer as a chronic illness. CA Cancer J Clin. 2011;61:50–62. doi: 10.3322/caac.20093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mathieu J, Maynard MT, Rapp T, et al. Team effectiveness 1997-2007: A review of recent advancements and a glimpse into the future. J Manage. 2008;34:410–476. [Google Scholar]
- 13. Salas E, Rosen MA, Burke CS, et al: The wisdom of collectives in organizations: An update of the teamwork competencies, in Salas E, Goodwin GF, Burke CS (eds): Team Effectiveness in Complex Organizations. Cross-disciplinary Perspectives and Approaches. London, UK, Routledge/Taylor & Francis, 2009, pp 39-79.
- 14.Wagner EH. Effective teamwork and quality of care. Med Care. 2004;42:1037–1039. doi: 10.1097/01.mlr.0000145875.60036.ed. [DOI] [PubMed] [Google Scholar]
- 15.Phelan EA, Balderson B, Levine M, et al. Delivering effective primary care to older adults: A randomized, controlled trial of the senior resource team at group health cooperative. J Am Geriatr Soc. 2007;55:1748–1756. doi: 10.1111/j.1532-5415.2007.01416.x. [DOI] [PubMed] [Google Scholar]
- 16. Fanjiang G, Grossman JH, Compton WD, et al: Building a Better Delivery System: A New Engineering/Health Care Partnership. Washington, DC, National Academies Press, 2005. [PubMed] [Google Scholar]
- 17.Weldon CB, Trosman JR, Gradishar WJ, et al. Barriers to the use of personalized medicine in breast cancer. J Oncol Pract. 2012;8:e24–e31. doi: 10.1200/JOP.2011.000448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Katz ML, Young GS, Reiter PL, et al. Barriers reported among patients with breast and cervical abnormalities in the patient navigation research program: Impact on timely care. Womens Health Issues. 2014;24:e155–e162. doi: 10.1016/j.whi.2013.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bickell NA, Mendez J, Guth AA. The quality of early-stage breast cancer treatment: What can we do to improve. Surg Oncol Clin N Am. 2005;14:103–117, vi. doi: 10.1016/j.soc.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 20.Taplin SH, Weaver S, Chollette V, et al. Teams and teamwork during a cancer diagnosis: Interdependency within and between teams. J Oncol Pract. 2015;11:231–238. doi: 10.1200/JOP.2014.003376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Guzzo RA, Shea GP: Group performance and intergroup relations in organizations, in Dunnette MD, Hough LM (eds): Handbook of Industrial and Organizational Psychology, Volume 3 (ed 2). Palo Alto, CA, Sage, 1992, pp 269-313. [Google Scholar]
- 22.Langfred CW. Autonomy and performance in teams: The multilevel moderating effect of task interdependence. J Manage. 2005;31:513–529. [Google Scholar]
- 23.Kiggundu MN. Task interdependence and job design: Test of a theory. Organ Behav Hum Perform. 1983;31:145–172. doi: 10.1016/0030-5073(83)90118-6. [DOI] [PubMed] [Google Scholar]
- 24.Saavedra R, Earley PC, Van Dyne L. Complex interdependence in task-performing groups. J Appl Psychol. 1993;78:61. [Google Scholar]
- 25.Langfred CW, Moye NA. Effects of task autonomy on performance: An extended model considering motivational, informational, and structural mechanisms. J Appl Psychol. 2004;89:934–945. doi: 10.1037/0021-9010.89.6.934. [DOI] [PubMed] [Google Scholar]
- 26.Shaw ME. Scaling Group Tasks: A Method for Dimensional Analysis. Fort Belvoir, VA, Fort Belvoir Defense Technical Information Center, Document; 1963. [Google Scholar]
- 27. Steiner ID: Group Process and Productivity (Social Psychological Monograph). New York, NY, Academic Press, 1972. [Google Scholar]
- 28.Wageman R. Interdependence and group effectiveness. Adm Sci Q. 1995;40:145–180. [Google Scholar]
- 29.Sicotte C, Pineault R, Lambert J. Medical team interdependence as a determinant of use of clinical resources. Health Serv Res. 1993;28:599–621. [PMC free article] [PubMed] [Google Scholar]
- 30.Buljac M, Van Woerkom M, Van Wijngaarden JD. Are real teams healthy teams. J Healthc Manag. 2013;58:92–107. discussion 108-109. [PubMed] [Google Scholar]
- 31. doi: 10.1177/1077558709343295. Bosch M, Faber MJ, Cruijsberg J, et al: Review article: Effectiveness of patient care teams and the role of clinical expertise and coordination: A literature review. Med Care Res Rev 66:5S-35S, 2009 (suppl 6) [DOI] [PubMed] [Google Scholar]
- 32.Bharwani AM, Harris GC, Southwick FS. Perspective: A business school view of medical interprofessional rounds: Transforming rounding groups into rounding teams. Acad Med. 2012;87:1768–1771. doi: 10.1097/ACM.0b013e318271f8da. [DOI] [PubMed] [Google Scholar]
- 33.Lemieux-Charles L, McGuire WL. What do we know about health care team effectiveness? A review of the literature. Med Care Res Rev. 2006;63:263–300. doi: 10.1177/1077558706287003. [DOI] [PubMed] [Google Scholar]
- 34.Weinberg DB, Cooney-Miner D, Perloff JN, et al. Building collaborative capacity: Promoting interdisciplinary teamwork in the absence of formal teams. Med Care. 2011;49:716–723. doi: 10.1097/MLR.0b013e318215da3f. [DOI] [PubMed] [Google Scholar]
- 35.Thompson JD. Organizations in Action. Social Science Bases of Administrative Theory. New York, NY: McGraw-Hill; 1967. [Google Scholar]
- 36. Van de Ven AH, Ferry DL: Measuring and Assessing Organizations. New York, NY, Wiley, 1980. [Google Scholar]
- 37.Kiggundu MN. Task interdependence and the theory of job design. Acad Manage Rev. 1981;6:499–508. [Google Scholar]
- 38.Wageman R, Gardner H, Mortensen M. The changing ecology of teams: New directions for teams research. J Organ Behav. 2012;33:301–315. [Google Scholar]
- 39.Bedwell WL, Ramsay PS, Salas E. Helping fluid teams work: A research agenda for effective team adaptation in healthcare. Transl Behav Med. 2012;2:504–509. doi: 10.1007/s13142-012-0177-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schwartz MD, Lerman C, Brogan B, et al. Impact of BRCA1/BRCA2 counseling and testing on newly diagnosed breast cancer patients. J Clin Oncol. 2004;22:1823–1829. doi: 10.1200/JCO.2004.04.086. [DOI] [PubMed] [Google Scholar]
- 41.Weitzel JN, McCaffrey SM, Nedelcu R, et al. Effect of genetic cancer risk assessment on surgical decisions at breast cancer diagnosis. Arch Surg. 2003;138:1323–1328. doi: 10.1001/archsurg.138.12.1323. discussion 1329. [DOI] [PubMed] [Google Scholar]
- 42.Wageman R. How leaders foster self-managing team effectiveness: Design choices versus hands-on coaching. Organ Sci. 2001;12:559–577. [Google Scholar]
- 43.Courtright SH, Thurgood GR, Stewart GL, et al. Structural interdependence in teams: An integrative framework and meta-analysis. J Appl Psychol. 2015;100:1825–1846. doi: 10.1037/apl0000027. [DOI] [PubMed] [Google Scholar]
- 44. Nokes S, Kelly S: The Definitive Guide to Project Management: The Fast Track to Getting the Job Done on Time and on Budget (ed 2). Upper Saddle River, NJ, Pearson Education, 2007. [Google Scholar]
- 45. Dinsmore PC, Cooke-Davies TJ: Right Projects Done Right: From Business Strategy to Successful Project Implementation. New York, NY, Wiley, 2005. [Google Scholar]
- 46. Project Management Institute: A Guide to the Project Management Body of Knowledge (PMBOK) Guide (ed 5). Philadelphia, PA, Project Management Institute, 2013. [Google Scholar]
- 47. Havard Business Review: HBR Guide to Project Management. Boston, MA, Harvard Business Review, 2013.
- 48.Charns MP. Organization design of integrated delivery systems. Hosp Health Serv Adm. 1997;42:411–432. [PubMed] [Google Scholar]
- 49. Weldon CB, Trosman J, Schink JC: Cost of cancer: There is more to it than containing chemotherapy costs. Oncology (Williston Park) 26:1116, 1118, 2012. [PubMed]
- 50.Marks MA, Mathieu JE, Zaccaro SJ. A temporally based framework and taxonomy of team processes. Acad Manage Rev. 2001;26:356–376. [Google Scholar]
- 51.Brannick MT, Roach RM, Salas E. Understanding team performance: A multimethod study. Hum Perform. 1993;6:287–308. [Google Scholar]
- 52. Okun S, Schoenbaum SC, Andrews D, et al: Patients and Health Care Teams Forging Effective Partnerships. Washington, DC, National Academies Press, 2014.
- 53.Donovan JJ, Williams KJ. Missing the mark: Effects of time and causal attributions on goal revision in response to goal-performance discrepancies. J Appl Psychol. 2003;88:379–390. doi: 10.1037/0021-9010.88.3.379. [DOI] [PubMed] [Google Scholar]
- 54.Alexander J, Prabhu Das I, Johnson TP. Time issues in multilevel interventions for cancer treatment and prevention. J Natl Cancer Inst Monogr. 2012;2012:42–48. doi: 10.1093/jncimonographs/lgs002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Freund KM, Battaglia TA, Calhoun E, et al. Impact of patient navigation on timely cancer care: The Patient Navigation Research Program. J Natl Cancer Inst. 2014;106:dju115. doi: 10.1093/jnci/dju115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Trosman JR, Weldon CB: Models of care delivery, in Benson III AB, Chakravarthy AB, Hamilton SR et al (eds): Cancers of the Colon and Rectum. A Multidisciplinary Approach to Diagnosis and Management Series. New York, NY, Demos Medical, 2014, pp 273-280. [Google Scholar]
- 57.Liden RC, Wayne SJ, Bradway LK. Task interdependence as a moderator of the relation between group control and performance. Hum Relat. 1997;50:169–181. [Google Scholar]
- 58.Wageman R, Baker G. Incentives and cooperation: The joint effects of task and reward interdependence on group performance. J Organ Behav. 1997;18:139–158. [Google Scholar]
- 59. Quinn T: Bringing a management model to healthcare: Team-based care, 2014. http://www.forbes.com/sites/groupthink/2014/12/09/bringing-a-management-model-to-healthcare-team-based-care.
- 60. Scher DL: 5 lessons healthcare can learn from project management, 2013. http://www.medicalpracticeinsider.com/blog/business/5-lessons-healthcare-can-learn-project-management.
- 61.Trosman JR, Weldon CB. Company profile: Center for business models in healthcare. Per Med. 2013;10:333–337. doi: 10.2217/pme.13.31. [DOI] [PubMed] [Google Scholar]
- 62.McClellan M, McKethan AN, Lewis JL, et al. A national strategy to put accountable care into practice. Health Aff (Millwood) 2010;29:982–990. doi: 10.1377/hlthaff.2010.0194. [DOI] [PubMed] [Google Scholar]
- 63.McClellan M. Accountable care organizations and evidence-based payment reform. JAMA. 2015;313:2128–2130. doi: 10.1001/jama.2015.5087. [DOI] [PubMed] [Google Scholar]
- 64.Rapkin BD, Weiss ES, Lounsbury DW, et al. Using the interactive systems framework to support a quality improvement approach to dissemination of evidence-based strategies to promote early detection of breast cancer: Planning a comprehensive dynamic trial. Am J Community Psychol. 2012;50:497–517. doi: 10.1007/s10464-012-9518-6. [DOI] [PubMed] [Google Scholar]
- 65. Centers for Medicare & Medicaid Services: Quality payment program: Delivery system reform, Medicare payment reform, & MACRA: The Merit-Based Incentive Payment System (MIPS) & Alternative Payment Models (APMs). https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/MACRA-MIPS-and-APMs.html.
- 66. Centers for Medicare & Medicaid Services: Oncology Care Model (OCM) request for applications (RFA), 2015. https://innovation.cms.gov/Files/x/ocmrfa.pdf.
- 67.Choy ET, Chiu A, Butow P, et al. A pilot study to evaluate the impact of involving breast cancer patients in the multidisciplinary discussion of their disease and treatment plan. Breast. 2007;16:178–189. doi: 10.1016/j.breast.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 68.Stacey D, Paquet L, Samant R. Exploring cancer treatment decision-making by patients: A descriptive study. Curr Oncol. 2010;17:85–93. doi: 10.3747/co.v17i4.527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ragas DM, Nonzee NJ, Tom LS, et al. What women want: Patient recommendations for improving access to breast and cervical cancer screening and follow-up. Womens Health Issues. 2014;24:511–518. doi: 10.1016/j.whi.2014.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Taylor C, Finnegan-John J, Green JS. “No decision about me without me” in the context of cancer multidisciplinary team meetings: A qualitative interview study. BMC Health Serv Res. 2014;14:488. doi: 10.1186/s12913-014-0488-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Byrne BE, Faiz OD, Vincent C: Do patients with gastrointestinal cancer want to decide where they have tests and surgery? A questionnaire study of provider choice. BMJ Qual Saf 10.1136/bmjqs-2015-004194 [epub ahead of print on October 14, 2015] [DOI] [PubMed]
- 72.Salloch S, Ritter P, Wäscher S, et al. Medical expertise and patient involvement: A multiperspective qualitative observation study of the patient’s role in oncological decision making. Oncologist. 2014;19:654–660. doi: 10.1634/theoncologist.2013-0268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Jensen RE, Rothrock NE, DeWitt EM, et al. The role of technical advances in the adoption and integration of patient-reported outcomes in clinical care. Med Care. 2015;53:153–159. doi: 10.1097/MLR.0000000000000289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wagner LI, Schink J, Bass M, et al. Bringing PROMIS to practice: Brief and precise symptom screening in ambulatory cancer care. Cancer. 2015;121:927–934. doi: 10.1002/cncr.29104. [DOI] [PMC free article] [PubMed] [Google Scholar]