Abstract
Our case describes the efforts of team members drawn from oncology, palliative care, supportive care, and primary care to assist a woman with advanced cancer in accepting care for her psychosocial distress, integrating prognostic information so that she could share in decisions about treatment planning, involving family in her care, and ultimately transitioning to hospice. Team members in our setting included a medical oncologist, oncology nurse practitioner, palliative care nurse practitioner, oncology social worker, and primary care physician. The core members were the patient and her sister. Our team grew organically as a result of patient need and, in doing so, operationalized an explicitly shared understanding of care priorities. We refer to this shared understanding as a shared mental model for care delivery, which enabled our team to jointly set priorities for care through a series of warm handoffs enabled by the team’s close proximity within the same clinic. When care providers outside our integrated team became involved in the case, significant communication gaps exposed the difficulty in extending our shared mental model outside the integrated team framework, leading to inefficiencies in care. Integration of this shared understanding for care and close proximity of team members proved to be key components in facilitating treatment of our patient’s burdensome cancer-related distress so that she could more effectively participate in treatment decision making that reflected her goals of care.
CASE SUMMARY
Martha was a 48-year-old woman with widely metastatic breast cancer who transferred care to our institution in June 2014. During the initial visit with the oncologist and oncology nurse practitioner (ONP), Martha seemed to be tolerating first-line treatment with minimal adverse effects, but she presented with a high degree of cancer-related emotional distress. The oncology team referred Martha via face-to-face handoff to the embedded palliative care nurse practitioner (PCNP) who saw her in the oncology clinic on the same day and found concerning scores on the patient’s Edmonton Symptom Assessment Survey for anxiety (score of 7 out of 10) and mild depression (score of 2 out of 10). Martha presented with a flat, withdrawn affect and emotional lability, and she endorsed suffering from intrusive thoughts and guilt about her diagnosis. Her stated goal of care was to follow the treatment regimen recommended by oncology, adding that she did not want a lot of information about prognosis or disease status or trajectory. Despite encouragement, Martha was reluctant to involve her sister (her closest family member) in her care or treatment decision making because of concerns about burdening her. Attempts to engage her in decision making related to depression and anxiety treatment were challenging. The PCNP referred Martha via face-to-face handoff to the embedded oncology clinical social worker (OCSW), who saw Martha on the same day of initial consultation in the oncology clinic. The PCNP also referred Martha to a primary care provider (PCP) through the electronic medical record (EMR). There was no verbal handoff to the PCP, and she was not located near the oncology clinic. The PCP, noting Martha’s emotional distress and depression during her initial visit 3 months later, referred Martha to an additional psychologist, although Martha was by this time already well connected with the oncology-specific psychosocial services. Martha was confused by the additional referral and was not sure with whom she should follow-up.
As her disease progressed despite successive therapies, Martha was hospitalized for hypercalcemia of malignancy. During her hospitalization, inpatient palliative care consultation was requested of the primary team via EMR in-basket messaging by her outpatient team; however, inpatient palliative consultation was not performed. (Currently, our outpatient palliative care program does not round on inpatients.) After discharge, Martha continued to suffer with severe distress that greatly hindered her ability to integrate prognostic information and to engage in shared decision making (SDM), especially as the end of life approached. The team perceived an urgency for prognostic awareness and end-of-life decision making, which would ideally occur in collaboration with her sister (named as her surrogate). Once Martha agreed to let the team discuss her care with her sister, the team engaged in ongoing communication with her to convey the team’s shared understanding of Martha’s disease status, prognosis, and options for care. This enabled Martha’s sister to make informed decisions on her behalf, and eventually, Martha was transitioned to home hospice services.
INTRODUCTION TO THE ISSUE OR PRINCIPLE: SHARED MENTAL MODELS
Although the model of the single physician provider and patient dyad may bring forth nostalgia, the reality is that most patients with advanced cancer have diverse needs (physical, psychosocial, and/or spiritual) that are too complex to be managed in a single consultation or by a single specialist. A standard 20-minute oncology appointment is insufficient for the time needed to effectively manage patient and family emotional distress.1 A growing body of evidence supports the use of multidisciplinary teams in the care of complex patients to optimize patient and health system outcomes.2 Teams have been defined as individual agents interdependently acting toward a collective goal.3,4 In the oncology setting, multidisciplinary teams address the various needs of distressed patients with cancer and their families, many of which may fall outside the scope of the already overextended routine oncology visit. There is a dearth of research describing how teams work together to manage care, create mutual accountability, and jointly engage patients and their families in complex care decisions. Recent palliative care research suggests that oncology and palliative care teams working together have both overlapping and distinct roles.1 We argue further that effective teams are those that define team member roles, delineate tasks, assign responsibility for task completion, and agree on desired process and patient outcomes. Teams must operate within the same cognitive framework, sharing an understanding of the patient’s history, condition, prognosis, cultural context, and health care goals that function as a starting point from which all care delivered by the multidisciplinary team may proceed.
The ability to vertically and horizontally integrate goals across multiple providers working together is made possible by the operationalization of this shared understanding, also known as a shared mental model (SMM).3 Research suggests that SMMs are an important and under-recognized aspect of successful teamwork.5 SMMs allow for a collective understanding of team tasks, team member interdependency in completing tasks, and the professional culture in which the team operates.6 SMMs are facilitated by mutual trust in the integrity of individual team members to follow through on assigned tasks; honest communication, transparency, and precision; and collaboration toward shared goals without fear of subterfuge.6 It is important to note that although individual actors possess their own understanding of tasks and issues, in the team setting, these individual mental models are organized into an overarching mental model shared among team members; if teams omit this step, individual mental models may be misaligned.7 Research suggests that highly functioning teams operate under several SMMs simultaneously, with a separate SMM governing each particular aspect of teamwork (eg, team culture or task performance).8
EXPLANATION OF THE ISSUE OR PRINCIPLE: HOW THE SMM SUPPORTS SDM
The Institute of Medicine has called for health care systems to place patients and their families at the center of health care decision making.9,10 Recent data from the Cancer Care Outcomes Research and Surveillance Consortium and others show that a majority of patients preferred SDM and that patients who reported engagement in SDM had higher patient-rated overall quality-of-life and communication scores compared with patients who felt their decision making was controlled by the physician, irrespective of the decision-making preference.11,12 This suggests that most patients desire an active role in their care planning. However, discussions about goals of care often do not occur until late in the disease trajectory.13 Growing evidence suggests that earlier conversations about the goals of care allow for better end-of-life outcomes for patients and caregivers.14 Involvement of palliative care at initial diagnosis of advanced cancer is one method for initiating earlier conversations about goals of care and has been shown to positively affect quality of life and overall survival.15-18
We hypothesize that a mechanism of palliative care’s success is its ability to facilitate an SMM while maintaining the team’s central focus on the patient and family.19 A recent qualitative study revealed that, in addition to providing symptom management and assisting with advance care planning, palliative care clinicians saw their role as “interpreting the oncologist for the patient and the patient for the oncologist.”20(p1246) This underscores the responsibility felt by many palliative care clinicians to serve as a conduit of bidirectional communication between patients and families and their oncology providers. We propose that a team drawn from multiple disciplines must hold a well-defined understanding of patient-centered care to be effective. This shared understanding enables team members to mutually rely upon one another to complete tasks, as well as to trust that messaging from each team member to the patient and family will be consistent.21 This shared philosophy of care is operationalized as an SMM, which enables transparency in complex discussions about patient prognosis, treatment options, and goals of care. This, in turn, facilitates SDM.
APPLICATION TO CASE
Table 1 lists the elements and expectations of the SMM in place for patients with advanced cancer when Martha transferred her care to our oncology clinic. Approximately 6 months before Martha was initially seen by the oncologist, this SMM guided the implementation of a pilot program in which a PCNP was embedded in the oncologist’s clinic to perform early palliative care consultation and advance care planning with patients with metastatic breast cancer aiming to improve patient outcomes and reduce unwanted aggressive treatments at the end of life.
Table 1.
Elements and Expectations of the Shared Mental Model Agreed to by Oncology, Palliative Care, and Supportive Care Team Members
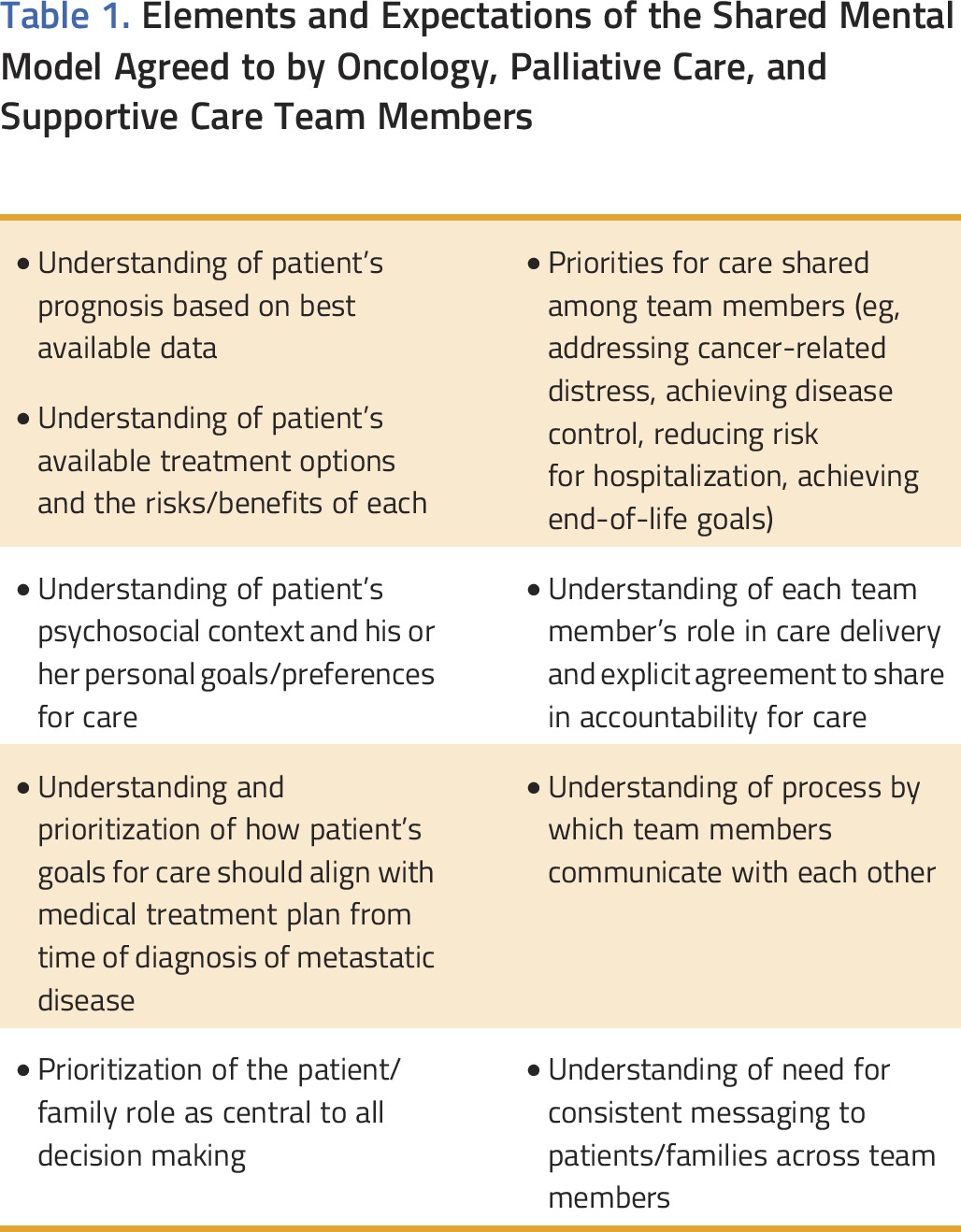
We operationalized this SMM through several discrete processes of care that were agreed upon during monthly implementation meetings attended by all team members. The team agreed that any patient with metastatic disease would be an appropriate referral to the PCNP. A patient referral form (Data Supplement) was created to elicit patient information from the oncologist and to inform next steps for the PCNP. For example, the referral form asked oncologists about patient prognosis and intent of treatment (palliative or curative) and informed the oncologist what could be expected from palliative consultation if prognosis was noted as greater than 1 year (begin advance care planning) versus less than 6 months (introduce hospice). A face-to-face handoff was established between oncology and palliative providers to ensure an understanding of patient needs and priorities for care. Systematic screening of physical and emotional symptoms and referral triggers for specialist care were enacted. Continuous quality improvement metrics, including rates of advance care planning, patient and family satisfaction scores, and end-of-life resource utilization were agreed upon at the program’s inception. We strengthened our SMM through participation in a National Cancer Institute–sponsored supportive care team building initiative. Research suggests that training may help teams successfully develop and implement SMMs, and studies of SMMs in various settings show that interprofessional training and team member acculturation are key factors in overcoming team members’ resistance to change and creating buy-in.22-24 In our case, monthly team meetings served as check-ins to ensure consistency of the SMM among team members and to identify challenges and solutions.
Martha first presented to the oncology team, which was composed of the medical oncologist and the ONP, whose role was to assess and manage her breast cancer, create the treatment plan, and evaluate response to treatment. The oncology team immediately recognized that Martha’s distress level was severe and that their team would require additional support, so the ONP stepped out of the exam room, went to the PCNP’s office, and asked her to join the patient visit. This was enabled by the shared understanding already in place between the oncology team and the PCNP, which included the mutual prioritization of identifying and treating severe cancer-related distress to enhance quality of life and increase patient participation in care.
The shared visit allowed for all providers to hear the patient recount her history and symptoms simultaneously. The shared visit also allowed the PCNP to hear the oncology treatment recommendations as described to the patient, enabling the PCNP to follow up on future questions Martha might have. The PCNP stayed in the exam room after the oncology team was finished and conducted her initial visit at that time, which (as was explicitly delineated in the SMM) consisted of assessing and treating symptoms, assessing for psychosocial and spiritual needs, making appropriate referrals using standard screening instruments, and engaging the patient (and family, if present) in complex and nuanced conversations about quality-of-life goals, values, and preferences for advance care planning while cultivating prognostic awareness.25,26
After acknowledging the severity of her distress and need for further care, Martha agreed to speak with a psychosocial provider. The PCNP stepped out of the exam room and paged the clinic’s embedded OCSW, part of an Integrative Oncology Center providing comprehensive care to patients with cancer. The OCSW came to the exam room after the PCNP’s initial visit, and consistent with his role as delineated in the SMM, he conducted a thorough intake and recommended ongoing psychosocial care, including individual counseling and support group participation within the Integrative Oncology Center. Because the Integrative Oncology Center is not located on site, the OCSW offered to update the oncology and palliative care providers about future encounters with Martha through the EMR.
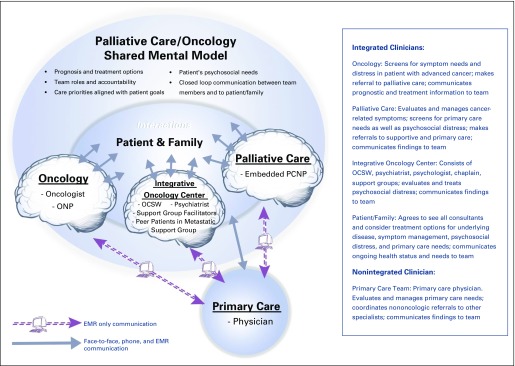
An additional referral was sent via EMR for Martha to establish primary care with a provider in our health system (Fig 1). This provider, who was not colocated with our clinic, saw Martha approximately 3 months after her first oncology visit. The PCP evaluated and managed Martha’s nononcologic medical problems and, noting her depressed and anxious appearance, made an additional referral to behavioral health. This had the unintended effect of causing confusion for Martha. No one from the colocated team had reached out specifically to the PCP; instead, the team relied on the EMR to make transparent the team’s care priorities and treatment intentions. This highlights the inefficiencies in care that can occur when clinicians outside an integrated team are not brought into the shared cognitive and interpersonal understanding operationalized by the SMM.
FIG 1.
Team roles and degree of integration of team members. EMR, electronic medical record; OCSW, oncology clinical social worker; ONP, oncology nurse practitioner; PCNP, palliative care nurse practitioner.
Another example of a challenge in extending the SMM to Martha’s other care providers emerged when Martha was admitted to the hospital. Because the outpatient PCNP program is a pilot program, many oncologists at the institution are unaware of the SMM of the core team. Additionally, the outpatient PCNP does not routinely round on inpatients because of scheduling constraints. Despite sending EMR messages to the inpatient oncology team requesting an inpatient palliative care consultation, Martha did not receive one.
Attempts to implement the SMM were made on every encounter with Martha; however, her ongoing severe distress made this challenging. As her disease progressed toward the end stages, the necessity of bringing Martha’s surrogate decision maker into the SMM became more apparent. Martha’s emotional distress hindered her ability to integrate important prognostic information. This, in turn, complicated treatment decisions; because Martha resisted awareness of the extent of her disease and her limited life expectancy, treatments defaulted toward aggressive care (eg, hospitalization). The team began advocating for Martha to involve her sister, whom she had named as her surrogate decision maker, in discussions. We held multiple joint conversations (via shared office visits as well as conference calls and e-mails) with Martha emphasizing our team’s assessment of her distress and the negative impact this distress was having on both her quality of life and her ability to engage in making treatment decisions. Martha eventually allowed us to involve her sister, which then necessitated several additional conversations (conducted face-to-face and by telephone and e-mail) with her to communicate Martha’s disease status and prognosis, as well as our recommendation to transition to comfort-oriented care, as the oncology team felt that further disease-modifying treatment was unlikely to benefit Martha in terms of survival or quality of life. Martha’s sister agreed with our assessment and felt that transitioning to home hospice care aligned well with Martha’s quality-of-life goals and preferences for care.
IMPLICATIONS FOR CLINICAL CARE
Our case demonstrates that patients with advanced cancer presenting with severe emotional distress can engage in advance care planning that reflects their values and preferences, but doing so consistently requires a team approach built on a shared understanding of priorities for care.19 Meticulous attention to and care for Martha’s distress was immediately identified as our team’s shared priority to engage her in ongoing SDM about treatment options as well as to facilitate an end-of-life transition that aligned with her goals. We were aided by the fact that the integrated team’s SMM was already in place and emphasized distress screening as a way to differentiate types and severity of distress to guide patients to appropriate psychosocial care.27 Thus, we feel that our team’s shared attention to and prioritization of treating cancer-related distress was beneficial in helping Martha and her sister participate in care decisions.
Our case also demonstrates the utility of the integrated model of palliative and supportive oncology care, which allows for richer conversation between providers, fostering a shared understanding of the case.28 In our model, the PCNP’s clinic is colocated and runs concurrently with the oncology clinic, and the Integrative Oncology Center provides an embedded OCSW to enhance access to a multidisciplinary team of psychosocial and spiritual care providers. This allowed Martha to see multiple providers within the context of the same exam room, which would not have been possible without provider proximity and the shared priorities for care already in place. The embedded clinic has resulted in efficiency gains to the oncology clinic in that team members share responsibility in assessing and managing patient distress and in communicating with the patient and family without significant redundancy and overlap. This model has the added benefit of allowing providers opportunities to debrief difficult patient cases together, which has reduced provider stress and burnout.
Our team ran into problems when we assumed that clinicians outside our integrated team shared our mental model for caring for patients with advanced cancer. First, we wrongly assumed that additional providers (eg, the PCP) would be able to understand our mental model merely by reading our progress notes in the EMR. We did not explicitly reach out to these team members to give a verbal handoff, and this omission hindered our attempts to provide seamless psychosocial care to Martha, especially when the PCP sent her to see a different psychologist. Second, when Martha was hospitalized for hypercalcemia, which carries ominous prognostic significance, our over-reliance on the EMR to communicate our SMM likely resulted in failure to involve inpatient palliative care at a time when Martha greatly needed continuity of care. One can argue that our communication failures with these other care providers undermined the very definition of a team as a group of individuals working together toward a shared goal.29 A lesson learned from this case is that as teams grow in size and scope there is even greater need to explicitly develop a shared philosophy of care. Without this shared understanding, it is difficult to envision how mutual priorities for care can be set and how messaging to patients and families can be consistent across providers. Health systems must take on the challenge of creating seamless team processes, especially for integration of early palliative care among oncology patients.30 We believe that pilot programs such as the one described here, in which team members openly and unambiguously share a mental model for care, constitute a first and essential step in changing the overall culture of a health care institution.
IMPLICATIONS FOR FUTURE RESEARCH
This case raises several issues amenable to further research. For instance, our hypothesis that palliative care teams are associated with the development of an SMM between the palliative team and the referring team should be tested. Future research also should strive to understand how effective palliative care and oncology SMMs are developed, maintained, and disseminated across institutions and could test various methods for doing so. An additional research focus could investigate whether the presence of an SMM among colocated oncology and palliative providers is associated with more favorable patient outcomes and clinic efficiency gains compared with usual care where patients typically receive oncology and palliative services in separate locations. For example, if the oncology and palliative teams do not share an explicit understanding of patient priorities and goals or a shared understanding of team member responsibilities and coordination, one can imagine the potential pitfalls—expensive and time-consuming duplication of services provided by teams, inconsistent messaging from teams to the patient and family, and lack of accountability among teams for various aspects of care delivery.31 As was demonstrated in our case, it may be easier to place a referral to a new specialist rather than delve into the chart to determine who is already involved in the patient’s care.
In conclusion, this case demonstrates that it is possible to establish an explicitly held SMM between oncology, palliative, and supportive care providers to set mutual priorities about how best to care for patients with advanced cancer. In doing this, we mostly avoided unwanted and ineffective care, while providing support to the patient and her family. Our patient’s severe cancer-related distress presented challenges to our ability to engage her in SDM about her treatment options; however, the presence of the SMM held us accountable for making cancer-related distress a priority for care, delineating clear team member roles and task completion responsibility, and continually communicating findings and patient progress, while also maintaining consistent messaging in communication with the patient and her sister.10 The lack of an SMM with the patient’s PCP and with the inpatient care team exposed our over-reliance on the EMR to make explicit goals, priorities, and processes of care that we had made seamless within our integrated, colocated team. Future research should focus on whether involvement of palliative care in the care of oncology patients helps create the cognitive and interpersonal conditions ripe for establishing and maintaining an SMM, as well as whether SMMs held by colocated specialists are associated with better communication between team members, more consistent messaging to patients and families, and improved engagement of patients in their own health care planning.
ACKNOWLEDGMENT
The production of this manuscript was funded by the Conquer Cancer Foundation Mission Endowment. Supported by the National Cancer Institute (NCI)–ASCO Teams in Cancer Care Delivery Project. A.M.W. was also supported by National Institutes of Health/National Center for Advancing Translational Science University of California, Los Angeles (UCLA) Clinical and Translational Science Institute Grant No. UL1TR000124 and the National Institutes of Health loan repayment program. Evaluation of the clinical model was supported by the California Health Care Foundation. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the NCI or ASCO. We thank Jenn Kolu Mui, Project Manager at the Simms/Mann UCLA Center for Integrative Oncology, for her assistance in preparing the article.
AUTHOR CONTRIBUTIONS
Conception and design: All authors
Collection and assembly of data: Sarah F. D'Ambruoso, Anne Coscarelli, David Coniglio, Anne M. Walling
Data analysis and interpretation: Sarah F. D'Ambruoso, Anne Coscarelli, Sara Hurvitz, Neil Wenger, David Coniglio, Dusty Donaldson, Anne M. Walling
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Use of a Shared Mental Model by a Team Composed of Oncology, Palliative Care, and Supportive Care Clinicians to Facilitate Shared Decision Making in a Patient With Advanced Cancer
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or jop.ascopubs.org/site/misc/ifc.xhtml.
Sarah F. D'Ambruoso
No relationship to disclose
Anne Coscarelli
No relationship to disclose
Sara Hurvitz
Research Funding: Genentech (Inst), Novartis (Inst), GlaxoSmithKline (Inst), Boehringer Ingelheim (Inst), Sanofi (Inst), Pfizer (Inst), Amgen (Inst), OBI Pharma (Inst), Puma Biotechnology (Inst), Dignitana (Inst), Bayer (Inst), Biomarin (Inst), Lilly (Inst), Merrimack (Inst)
Travel, Accommodations, Expenses: Boehringer Ingelheim, Novartis, Genentech, Lilly, Pfizer, Bayer, Lilly
Neil Wenger
No relationship to disclose
David Coniglio
Employment Pinehurst Medical Clinic, Pinehurst, NC (I)
Dusty Donaldson
No relationship to disclose
Christopher Pietras
No relationship to disclose
Anne M. Walling
No relationship to disclose
REFERENCES
- 1.Yoong J, Park ER, Greer JA, et al. Early palliative care in advanced lung cancer: A qualitative study. JAMA Intern Med. 2013;173:283–290. doi: 10.1001/jamainternmed.2013.1874. [DOI] [PubMed] [Google Scholar]
- 2.Taplin SH, Weaver S, Salas E, et al. Reviewing cancer care team effectiveness. J Oncol Pract. 2015;11:239–246. doi: 10.1200/JOP.2014.003350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Salas E, Shuffler ML, Thayer AL, et al. Understanding and improving teamwork in organizations: A scientifically based practical guide. Hum Resour Manage. 2015;54:599–622. [Google Scholar]
- 4.Marks MA, DeChurch LA, Mathieu JE, et al. Teamwork in multiteam systems. J Appl Psychol. 2005;90:964–971. doi: 10.1037/0021-9010.90.5.964. [DOI] [PubMed] [Google Scholar]
- 5.McComb S, Simpson V. The concept of shared mental models in healthcare collaboration. J Adv Nurs. 2014;70:1479–1488. doi: 10.1111/jan.12307. [DOI] [PubMed] [Google Scholar]
- 6.Salas E, Sims DE, Burke CS. Is there a “Big Five” in teamwork? Small Group Res. 2005;36:555–599. [Google Scholar]
- 7.Mathieu JE, Heffner TS, Goodwin GF, et al. The influence of shared mental models on team process and performance. J Appl Psychol. 2000;85:273–283. doi: 10.1037/0021-9010.85.2.273. [DOI] [PubMed] [Google Scholar]
- 8.Lim BC, Klein KJ. Team mental models and team performance: A field study of the effects of team mental model similarity and accuracy. J Organ Behav. 2006;27:403–418. [Google Scholar]
- 9.Mitchell P, Wynia M, Golden R, et al: Core principles and values of effective team-based health care. https://www.nationalahec.org/pdfs/vsrt-team-based-care-principles-values.pdf
- 10.Ganz P, Cohen HJ, Eberlein TJ, et al: Delivering high quality cancer care: Charting a new course for a system in crisis. https://ww5.komen.org/uploadedFiles/Content_Binaries/quality%20cancer%20care.pdf [PubMed]
- 11.Kehl KL, Landrum MB, Arora NK, et al. Association of actual and preferred decision roles with patient-reported quality of care: Shared decision making in cancer care. JAMA Oncol. 2015;1:50–58. doi: 10.1001/jamaoncol.2014.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ashraf AA, Colakoglu S, Nguyen JT, et al. Patient involvement in the decision-making process improves satisfaction and quality of life in postmastectomy breast reconstruction. J Surg Res. 2013;184:665–670. doi: 10.1016/j.jss.2013.04.057. [DOI] [PubMed] [Google Scholar]
- 13.Keating NL, Landrum MB, Rogers SO, Jr, et al. Physician factors associated with discussions about end-of-life care. Cancer. 2010;116:998–1006. doi: 10.1002/cncr.24761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mack JW, Weeks JC, Wright AA, et al. End-of-life discussions, goal attainment, and distress at the end of life: Predictors and outcomes of receipt of care consistent with preferences. J Clin Oncol. 2010;28:1203–1208. doi: 10.1200/JCO.2009.25.4672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smith TJ, Temin S, Alesi ER, et al. American Society of Clinical Oncology provisional clinical opinion: The integration of palliative care into standard oncology care. J Clin Oncol. 2012;30:880–887. doi: 10.1200/JCO.2011.38.5161. [DOI] [PubMed] [Google Scholar]
- 16.Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010;363:733–742. doi: 10.1056/NEJMoa1000678. [DOI] [PubMed] [Google Scholar]
- 17.Zimmermann C, Swami N, Krzyzanowska M, et al. Early palliative care for patients with advanced cancer: A cluster-randomised controlled trial. Lancet. 2014;383:1721–1730. doi: 10.1016/S0140-6736(13)62416-2. [DOI] [PubMed] [Google Scholar]
- 18.Bakitas MA, Tosteson TD, Li Z, et al. Early versus delayed initiation of concurrent palliative oncology care: Patient outcomes in the ENABLE III randomized controlled trial. J Clin Oncol. 2015;33:1438–1445. doi: 10.1200/JCO.2014.58.6362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Greer JA, Jackson VA, Meier DE, et al. Early integration of palliative care services with standard oncology care for patients with advanced cancer. CA Cancer J Clin. 2013;63:349–363. doi: 10.3322/caac.21192. [DOI] [PubMed] [Google Scholar]
- 20.Back AL, Park ER, Greer JA, et al. Clinician roles in early integrated palliative care for patients with advanced cancer: A qualitative study. J Palliat Med. 2014;17:1244–1248. doi: 10.1089/jpm.2014.0146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Weller J, Boyd M, Cumin D. Teams, tribes and patient safety: Overcoming barriers to effective teamwork in healthcare. Postgrad Med J. 2014;90:149–154. doi: 10.1136/postgradmedj-2012-131168. [DOI] [PubMed] [Google Scholar]
- 22.Cronholm PF, Shea JA, Werner RM, et al. The patient centered medical home: Mental models and practice culture driving the transformation process. J Gen Intern Med. 2013;28:1195–1201. doi: 10.1007/s11606-013-2415-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McComb SA, Lemaster M, Henneman EA, et al: An evaluation of shared mental models and mutual trust on general medical units: Implications for collaboration, teamwork, and patient safety. J Patient Saf [epub ahead of print on February 24, 2015] [DOI] [PubMed]
- 24.Pearsall MJ, Venkataramani V. Overcoming asymmetric goals in teams: The interactive roles of team learning orientation and team identification. J Appl Psychol. 2015;100:735–748. doi: 10.1037/a0038315. [DOI] [PubMed] [Google Scholar]
- 25.Tuggey EM, Lewin WH. A multidisciplinary approach in providing transitional care for patients with advanced cancer. Ann Palliat Med. 2014;3:139–143. doi: 10.3978/j.issn.2224-5820.2014.07.02. [DOI] [PubMed] [Google Scholar]
- 26.Jackson VA, Jacobsen J, Greer JA, et al. The cultivation of prognostic awareness through the provision of early palliative care in the ambulatory setting: A communication guide. J Palliat Med. 2013;16:894–900. doi: 10.1089/jpm.2012.0547. [DOI] [PubMed] [Google Scholar]
- 27.Carlson LE, Waller A, Mitchell AJ. Screening for distress and unmet needs in patients with cancer: Review and recommendations. J Clin Oncol. 2012;30:1160–1177. doi: 10.1200/JCO.2011.39.5509. [DOI] [PubMed] [Google Scholar]
- 28.Hui D, Bruera E. Models of integration of oncology and palliative care. Ann Palliat Med. 2015;4:89–98. doi: 10.3978/j.issn.2224-5820.2015.04.01. [DOI] [PubMed] [Google Scholar]
- 29.Duthie EA. Recognizing and managing errors of cognitive underspecification. J Patient Saf. 2014;10:1–5. doi: 10.1097/PTS.0b013e3182a5f6e1. [DOI] [PubMed] [Google Scholar]
- 30.Evans JM, Baker GR. Shared mental models of integrated care: Aligning multiple stakeholder perspectives. J Health Organ Manag. 2012;26:713–736. doi: 10.1108/14777261211276989. [DOI] [PubMed] [Google Scholar]
- 31.Politi MC, Studts JL, Hayslip JW. Shared decision making in oncology practice: What do oncologists need to know? Oncologist. 2012;17:91–100. doi: 10.1634/theoncologist.2011-0261. [DOI] [PMC free article] [PubMed] [Google Scholar]