Abstract
Patient: Male, 67
Final Diagnosis: Torsion of a giant antimesenteric lipoma of the ileum
Symptoms: Acute abdomen
Medication: —
Clinical Procedure: En bloc segmental resection with end-to-end anastomosis
Specialty: Surgery
Objective:
Rare disease
Background:
Torsion of an intra-abdominal lipoma is rarely the cause of acute abdominal pain. Most of the previously reported cases of intra-abdominal lipoma torsion originated in the mesentery or omentum. However, an antimesenteric lipoma of the ileum with torsion has not been reported before.
Case Report:
A 67-year-old man presented to the emergency department with acute abdominal pain. Contrast-enhanced computed tomography (CECT) of the abdomen and pelvis only showed a giant fat-containing, soft-tissue, intra-abdominal tumor, suspected to be a lipoma. Laparotomy was performed, and the presence of torsion of the antimesenteric lipoma of the ileum was confirmed. Beside tumor resection, en bloc segmental resection of the ileum with end-to-end anastomosis was performed to avoid bowel stricture and obtain tumor-free margins.
Conclusions:
CECT is the modality of choice to detect an intra-abdominal lipoma. Urgent surgical intervention should be considered if the symptoms persist and torsion cannot be excluded. If simple excision is not adequate because of poor accessibility of the tumor stalk, en bloc segmental resection with end-to-end anastomosis should be considered.
MeSH Keywords: Intra-Abdominal Fat; Mesenteric Vascular Occlusion; Panniculitis, Peritoneal; Torsion Abnormality
Background
The diagnosis of torsion of an intra-abdominal organ is a challenge in acute abdomen cases because it is usually accompanied by few abnormalities on physical examination and laboratory findings. Torsion of an intra-abdominal lipoma is a rare cause of acute abdomen. In most previously reported cases of intra-abdominal lipoma torsion, the tumor originates from the mesentery or omentum. Herein, we report a rare case of torsion of an antimesenteric lipoma of the ileum. To our knowledge, such a case has not been reported previously. Only the lipoma was identified using contrast-enhanced computer tomography (CECT). The tumor torsion was diagnosed during the surgical intervention. The tumor was successfully removed without further complications.
Case Report
A 67-year-old man presented to the emergency department with a history of intermittent nausea, vomiting, and abdominal fullness for 1 week and sudden onset of unbearable lower abdominal pain 2 h before admission. He had a history of type 2 diabetes mellitus, dyslipidemia, and hypertension. On arrival, his blood pressure was 158/86 mmHg; pulse rate, 116 beats/min; and body temperature, 37.7°C. On physical examination, we found tympanic sounds on percussion and local rebound tenderness over the periumbilical region on palpation without radiation. The laboratory test results were as follows: white blood cells, 17 350/mm3; hemoglobin, 13.3 g/dl; platelets, 249/mm3; AST/ALT, 13.9/10.6 U/L; glucose, 163.2 mg/dl; and lipase, 24 U/L. A plain abdominal radiography showed remarkable bowel gas retention. An abdominal ultrasound showed a rounded isoechoic tumor over the periumbilical region. The CECT of the abdomen and pelvis showed a huge low-attenuation well-defined, homogeneous, fat-containing, soft-tissue intra-abdominal tumor measuring approximately 12×12×7 cm (Figure 1, asterisk). Lipoma or liposarcoma was highly suspected based on imaging findings. The patient received pain control for 6 h with 10 mg of intravenous morphine and conservative treatment, but the abdominal pain did not subside. He underwent laparotomy. During surgery, we observed a huge and encapsulated tumor over the antimesenteric side of the terminal ileum, approximately 140 cm distal from the ileocecal valve, twisting around its wide and short stalk. The tumor appeared relatively congested compared to the adjacent intestine (Figure 2). Based on surgical findings, we diagnosed torsion of the lipoma. During the surgical intervention, we performed en bloc segmental resection of the ileum, including the tumor mass, of approximately 10 cm in length to obtain tumor-free margins. End-to-end anastomosis was subsequently performed. Histopathological examination of the tumor showed adipose tissue with benign-looking, diffuse congestion, panniculitis, and focal ischemic changes. No surgical drain was placed. Enteral feeding was initiated on the third postoperative day and was well tolerated thereafter. The patient was discharged uneventfully after 7 days postoperatively. At the 3-month follow-up visit, the patient was still doing well.
Figure 1.

Contrast-enhanced computed tomography (CECT) of the abdomen and pelvis showed a huge well-defined, homogeneous, fat-containing, soft-tissue, intra-abdominal tumor measuring approximately 12×12×7 cm (asterisk). Lipoma or liposarcoma was highly suspected based on these imaging findings.
Figure 2.
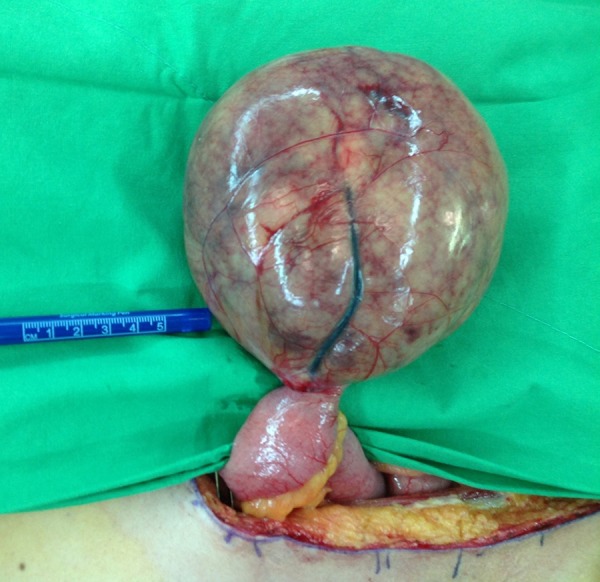
A huge and encapsulated tumor was observed over the antimesenteric side of the terminal ileum, about 140 cm distal to the ileocecal valve, twisting around its wide and short stalk. The tumor appeared relatively congested compared to the adjacent intestine.
Discussion
Lipomas are the most common benign tumors of the adipose tissue; most of them are located subcutaneously. In previously reported cases, intra-abdominal lipomas that undergo torsion arise from the mesentery, omentum, or epiploic appendices because these structures contain large amounts of adipose tissue [1–3]. Such lipomas can also originate from various internal organs where there is no or very little adipose tissue [4]. In our patient, the twisted lipoma was an antimesenteric lipoma located distal to the intestinal mesentery. To our knowledge, the torsion of a lipoma emerging from antimesenteric side of the ileum has not been reported before.
Most lipomas are small, asymptomatic, and remain untreated. However, lipomas can reach a considerable size [5]. Giant lipomas are most likely located in internal organs rather than subcutaneously, as these visceral lipomas go unnoticed. They can grow to considerable size until they became symptomatic, causing compression symptoms or torsion [6,7]. Larger lipomas with pedicles tend to twist and cannot untwist easily [8]. In our patient, the huge antimesenteric lipoma of the ileum was found twisted around its wide and short stalk.
The torsion of a lipoma restricts its blood supply, causing ischemic pain. The torsion can be either complete or incomplete or constant or intermittent. These different characteristics result in variable clinical manifestations [9]. Non-specific symptoms or even absence of abnormal physical or laboratory findings at the initial presentation make the diagnosis of tumor torsion challenging [10]. Other differential diagnoses similar to this presentation include testicular torsion, torsion of testicular appendage, ovarian torsion, epiploic appendagitis, omental infarct, and sclerosing mesenteritis [11,12]. In most cases, plain abdominal radiographs have little or no diagnostic value. Ultrasound may be useful in identifying an intra-abdominal lipoma, but it is operator-dependent and usually influenced by fat or bowel gas. The typical sonographic findings comprise iso- to hyperechoic texture, surrounded by a thin, echogenic capsule in contrast with the adjacent muscles [13]. CECT has a high detection rate for intra-abdominal lipoma, and the typical finding is a well-circumscribed ovoid mass with homogeneous imaging characteristics of fat [14]. Other pathognomonic changes associated with lipoma on CECT include large tumor size, tumor compression with intestinal obstruction, and even volvulus. CECT has limited diagnostic value for diagnosing torsion of the lipoma because of the lack of changes in ischemic patterns [15]. Although streaks of whirling and concentric patterns might be seen on CECT in some cases, the axis of rotation should be totally perpendicular to the transverse scanning plane [16, 17]. Thus, surgeons should not hesitate to perform surgery in cases in which symptoms do not improve with pain management and conservative treatment. We were able to directly visualize the twisted stalk, the color, and appearance changes of the lipoma during the surgical intervention. The histopathologic findings of diffuse congestion and focal ischemic changes in the adipose tissue of the tumor further confirmed the lipoma torsion diagnosis.
Small and asymptomatic lipomas are usually left untreated. Symptomatic intra-abdominal lipomas, however, are best treated by total excision [18]. If left untreated, these could progress to tissue necrosis, perforation, or peritonitis [19]. Most of the previously reported cases were safely and simply excised by laparoscopy or laparotomy, depending on the tumor size and location. In our patient, the huge lipoma originated from the antimesenteric side of the ileum with a wide and short stalk. Simple excision via ligating the stalk was inadequate as there were no clear boundaries. To avoid significant bowel wall injury, and even perforation or luminal stricture in the future as well as the possibility of potential malignancy, we performed en bloc segmental resection of the ileum to obtain tumor-free margins, followed by end-to-end anastomosis.
Conclusions
An antimesenteric lipoma of the ileum may twist and progress to torsion, which can be challenging to diagnose given the non-specific clinical features and acute abdominal pain. Early arrangement of CECT may allow for an earlier detection but not for all cases. CECT, however, has limited diagnostic value for lipoma torsion. Urgent surgical intervention is indicated in patients with persistent acute abdominal pain when torsion cannot be excluded. If the tumor has a short stalk or is close to the bowel wall, en bloc segmental resection with end-toend anastomosis should be considered.
Footnotes
Conflicts of interest
None
References:
- 1.Wolko JD, Rosenfeld DL, Lazar MJ, et al. Torsion of a giant mesenteric lipoma. Pediatr Radiol. 2003;33:34–36. doi: 10.1007/s00247-002-0810-8. [DOI] [PubMed] [Google Scholar]
- 2.Beattie GC, Irwin ST. Torsion of an omental lipoma presenting as an emergency. Int J Clin Pract. 2005;147:130–31. doi: 10.1111/j.1368-504x.2005.00457.x. [DOI] [PubMed] [Google Scholar]
- 3.Farmlett EJ, Fishman EK, Jones B, Siegelman SS. Case report. Torsion of lipoma of appendix epiploica: CT evaluation. J Comput Assist Tomogr. 1985;9:366–68. doi: 10.1097/00004728-198503000-00027. [DOI] [PubMed] [Google Scholar]
- 4.Di B, Enedetto G, Aquinati A, et al. Giant compressing lipoma of the thigh. Plast Reconstr Surg. 2004;114:1983–85. doi: 10.1097/01.prs.0000143929.24240.9a. [DOI] [PubMed] [Google Scholar]
- 5.Ferraro GA, Salzillo R, De Francesco F, et al. Approach and management of a giant lipoma in the left lumbar region. Int J Surg Case Rep. 2015;14:189–93. doi: 10.1016/j.ijscr.2015.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kshirsagar AY, Nangare NR, Gupta V, et al. Multiple giant intra abdominal lipomas: A rare presentation. Int J Surg Case Rep. 2014;5:399–402. doi: 10.1016/j.ijscr.2014.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ilhan H, Tokar B, Işiksoy S, et al. Giant mesenteric lipoma. J Pediatr Surg. 1999;34:639–40. doi: 10.1016/s0022-3468(99)90094-5. [DOI] [PubMed] [Google Scholar]
- 8.Kinjo Y, Adachi Y, Seki K, Tsubono M. Laparoscopic resection for torsion of an omental lipoma presenting as an acute abdomen in a 5-year-old girl. J Surg Case Rep. 2014;2014(7) doi: 10.1093/jscr/rju072. pii: rju072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lubner MG, Simard ML, Peterson CM, et al. Emergent and nonemergent non-bowel torsion: spectrum of imaging and clinical findings. Radiographics. 2013;33:155–73. doi: 10.1148/rg.331125016. [DOI] [PubMed] [Google Scholar]
- 10.Cha JM, Lee JI, Joo KR, et al. Giant mesenteric lipoma as an unusual cause of abdominal pain: a case report and a review of the literature. J Korean Med Sci. 2009;24:333–36. doi: 10.3346/jkms.2009.24.2.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ayoob AR, Lee JT. Imaging of common solid organ and bowel torsion in the emergency department. Am J Roentgenol. 2014;203(5):470–81. doi: 10.2214/AJR.13.12279. [DOI] [PubMed] [Google Scholar]
- 12.Tavares Pereira JP, Romão V, Eulálio M, et al. Sclerosing mesenteritis and disturbance of glucose metabolism: A new relationship? A case series. Am J Case Rep. 2016;17:55–59. doi: 10.12659/AJCR.896145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Truong S, Pfingsten FP, Dreuw B, Schumpelick V. Value of sonography in diagnosis of uncertain lesions of the abdominal wall and inguinal region. Chirurg. 1993;64:468–75. [PubMed] [Google Scholar]
- 14.Gaskin CM, Helms CA. Lipomas, lipoma variants, and well-differentiated liposarcomas (atypical lipomas): Results of MRI evaluations of 126 consecutive fatty masses. Am J Roentgenol. 2004;182:733–39. doi: 10.2214/ajr.182.3.1820733. [DOI] [PubMed] [Google Scholar]
- 15.Murphey MD, Carroll JF, Flemming DJ, et al. From the archives of the AFIP: Benign musculoskeletal lipomatous lesions. Radiographics. 2004;24:1433–66. doi: 10.1148/rg.245045120. [DOI] [PubMed] [Google Scholar]
- 16.Yager A, Carmeci C. Torsion of the greater omentum: CT findings. Am J Roentgenol. 1999;173:1139–40. doi: 10.2214/ajr.173.4.10511205. [DOI] [PubMed] [Google Scholar]
- 17.Tandon AA, Lim KS. Torsion of the greater omentum: A rare preoperative diagnosis. Indian J Radiol Imaging. 2010;20:294–96. doi: 10.4103/0971-3026.73540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bunker DLJ, Ilie VG, Tushar K. Halder torsion of an abdominal-wall pedunculated lipoma: A rare differential diagnosis for right iliac fossa pain. Case Rep Surg. 2013;2013:587380. doi: 10.1155/2013/587380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kumar A, Shah J, Vaidya P. Primary omental gangrene mimicking appendicular perforation peritonitis – A case report. Int J Surg Case Rep. 2016;21:67–69. doi: 10.1016/j.ijscr.2016.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]


