Abstract
This review provides a comprehensive assessment on polymer blends and nanocomposite systems for articular cartilage tissue engineering applications. Classification of various types of blends including natural/natural, synthetic/synthetic systems, their combination and nanocomposite biomaterials are studied. Additionally, an inclusive study on their characteristics, cell responses ability to mimic tissue and regenerate damaged articular cartilage with respect to have functionality and composition needed for native tissue, are also provided.
Keywords: blend, nanocomposite, biomaterial, articular cartilage, tissue engineering
1. Introduction
Polymeric materials are widely used in several biomedical fields. A large body of biomaterials have been considered and reviewed for tissue repairs [1,2,3]. There are a lot of literature surveys and comprehensive review papers covering several natural and synthetic polymers that have been studied for cartilage tissue engineering [4,5,6,7].
Among these polymers, natural polymers could provide some properties such as biocompatibility, biodegradability, low toxicity, and cell signaling [8,9] whereas synthetic polymers provide some other properties such as mechanical and physical properties and thermal stability [10]. Some of these polymeric three-dimensional (3D) scaffolds could provide microenvironments for cell supporting, cell migration, cell proliferation, cell fate and differentiation [11,12]. Not surprisingly, many of them do not provide sufficient mechanical properties to continuously support the formation of cartilage tissue. Some examples of widely used natural and synthetic biomaterials are summarized in Table 1.
Table 1.
List of some natural and synthetic polymers have been extensively surveyed for cartilage tissue engineering.
| Polymers | Examples |
|---|---|
| Natural polymers | Proteins: collagen [13], gelatin [14], fibrin glue [15] Polysaccarides: Agarose [16], alginate [17], cellulose [18], chitosan [19], chondroitin sulphate [20], and hyaluronic acid [21] |
| Synthetic polymers | poly(α-hydroxy esters): Poly(L-lactic-co-glycolic acid) [22], poly(ε-caprolactone) [23], Poly(NiPAAm) [24], poly(vinyl alcohol) [25], Polyurethane [26] |
Synthetic polymers could be fabricated into different shapes with various microstructures [5] but the processability of natural polymers is more difficult than synthetic ones due to their sensitivity to process conditions such as temperature [27]. Although it is much easier to use synthetic polymers in the biomedical field, natural polymers are also required due to their specific characteristics mentioned above. Moreover, the pure polymer and also polymer blends could be strengthened by the inclusion of nanomaterilas [28]. Therefore, the use of materials that combine and provide the characteristic features of both natural and synthetic polymers is of interest.
As alluded above, the organized structure of natural polymers in comparison with synthetic polymers accounts the specific characteristics such as improved cell viability and tissue ingrowth [3] which is their single most advantage. In addition, some natural polymers (e.g., collagen and chondroitin sulphate) are present in cartilage tissues; therefore the similar structure could impart cartilage characteristics to the scaffolds [29].
Polymer blending, making composites, and synthesizing copolymers and interpenetrating polymer networks (IPNs) are some of different methods of polymer modifications and they are of significant interests, since these modifications could lead to the development of a new range of biomaterials with full set of desired properties [23,30,31,32]. The history of blending dates back to the in 19th century, when Parkes (1846) introduced the first blends of trans- and cis-1,4-polyisoprene including fillers [33]. Polymer blending and compositing of biomaterials have attracted an increasing attention over the last two decades due to biocompatibility and providing special properties considered for the application.
Polymer blends are mixtures containing two or more polymers and/or copolymers [33], while nanocomposites are comprised of polymers (natural; synthetic) and nanomaterilas, which refer to materials with a nano-sized topography or composed of nano-sized building components [27,34].
Since basic information on tissue engineering principles is amply available to the reader in the open literature, we focus on articular cartilage. Cartilage tissue engineering does not require extensive vascularization, hence a lot of polymeric scaffolds were evaluated [35] but clinical trials are limited and need to be assessed through long-term outcomes [36]. Synthetic polymers such as poly(lactic-co-glycolic) acid (PLGA) and poly(caprolactone) (PCL) are already used for clinically established products. It is worth to point out that some polymers, such as poly(urethanes) (PURs), poly(phosphazenes), and natural polymers such as collagen, fibrin and hyaluronic acid polymers are under current clinical investigation [37].
Articular cartilage is a connective tissue that lines the ends of articulating bones and provides frictionless motion in diarthrodial joints whilst protecting the bones of joints from being damaged when subjected to impact and load bearing. Unlike many other tissues, articular cartilage is the avascular, aneural, and alymphatic tissue so its ability to regenerate itself remains challenging [38]. Moreover, repairing articular cartilage in organized zones with functional mechanical properties such as viscoelasticity, anisotropy, nonlinearity and inhomogeneity has to be carefully considered and remains one of the primary obstacles in cartilage repair from a biomechanical standpoint. The purpose of this review is to highlight the available published information and recent progress on blends and biocomposite systems with respect to the preparation, evaluation, and their potentials as biomedical implant or scaffold materials for articular cartilage tissue engineering. The fabrication strategies for polymeric scaffolds are beyond the scope of this paper and will not be discussed here [6]. Firstly, the anatomy and properties of the natural articular cartilage tissue are discussed, and then the necessary requirements for engineering scaffolds are identified. Secondly, we address some of the most common natural and synthetic polymers including strategies for fabrication of blends and nanocomposite scaffolds. Finally, some of the most critical challenges for future approaches to form cartilaginous tissues that provide a functional replacement and restoration of articular cartilage from biomaterial point of view are introduced. Furthermore, a brief outline on the state of the art of current progress in terms of material properties, composite development and cartilage applications is presented.
2. Articular Cartilage Tissue Engineering
2.1. Structure-Property Relationships of Native Articular Cartilage
In order to engineer articular cartilage; there is a need to understand its composition; architecture and function for identifying the essential requirements for matrixes or scaffolds used for this application; because the composition and structure of extracellular matrix (ECM) within this tissue has a direct role in its function as a mechanical surface through regulation of its tensile, shear and compressive properties [39]. The primary roles of this highly specialized tissue are to facilitate articulation; distribute the loads uniformly to the underlying bone and provide the joint with essential biomechanical functions such as wear resistance; load bearing and shock absorption with low friction under high joint loads [40]. Articular cartilage is a connective tissue that lines the ends of articulating bones forming freely moving in diarthrodial joints [41]. It forms a layer; normally 3–4 mm thick and its whitish color is owing to its lack of vascularity [38]. The tissue is not only compositionally complex but also biologically active [42]. A growing body of literature investigating the cartilage tissue engineering has published papers about articular cartilage structure and biology in detail [39,43,44,45].
Articular cartilage represents the only remnant of the original cartilage template to persist throughout adult life where it is divisible into four horizontal layers with their hierarchical network structure determining its mechanical behaviors [46,47]. The mechanics, structure, and organization of articular cartilage are only summarized here as it has been previously reviewed in detail by several authors [36,48,49]. With respect to depth within the tissue from the surface through to the bone [50], four distinct zones can be distinguished by extracellular matrix structure and composition, as well as cell shape and arrangement within the tissue [4,51] (Figure 1). In other words, the composition and organization of the matrix, cell morphology, orientation, density and metabolic activity, collagen fiber assembly and thickness vary from the surface respect to the depth and give it anisotropic properties in some mechanical environments [52]. In fact, these zonal gradients determined the functional and mechanical properties of articular cartilage; hence, designing and preparation of this tissue have remained challenging.
Figure 1.
Zonal organization in normal articular cartilage, the black lines and the red solids represent collagen fibrils and chondrocytes, respectively.
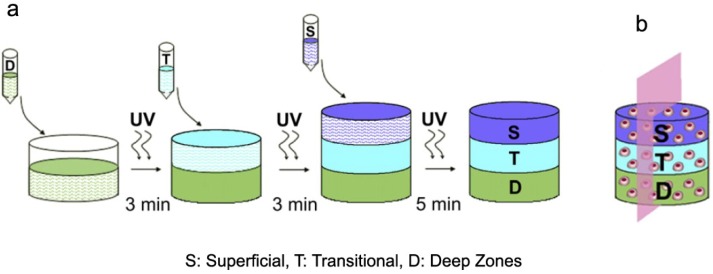
Three possible approaches were reported for articular cartilage repair: scaffold and matrix free, scaffold based and matrix based. According to zonal organization mimicking, matrix based approach is the effective one [53] in which scaffolds can be formed in various shapes and polymerized with different methods such as light curing, or with chemical materials and some of them could be injected into cartilage defect [54]. Nguyen et al. [55] fabricated 3D scaffolds with layer-by-layer organization of PEG-based hydrogel with chondroitin sulfate and matrix metalloproteinase-sensitive peptides, which were seeded with stem cells, resulted in to differentiate into zone-specific chondrocytes and organize into a complex tissue structure. The superficial zone composition consists of PEG, chondroitin sulfate and matrix metalloproteinase-sensitive peptides, the transitional zone composition consists of PEG, and chitosan, and finally the deep zone composition consists of PEG and hyaluronic acid [55] (Figure 2).
Figure 2.
(a) Multi-layer scaffold fabrication with three distinctive layers; (b) Schematic of a cell laden in composite multi-layer hydrogel, reprinted with permission from [55]. Copyright 2011 Elsevier.
It is noteworthy that there is a second type of organization of articular cartilage at the microscale. At this classification, matrix structure and composition are varying with respect to distance from the chondrocyte membrane [50].
First zone, superficial zone, is characterized by having dense thin collagen fibrils parallel to the articular surface which possesses greater tensile stiffness and strength than the deeper zones, and it may resist shear forces generated during use of the joint as well as relatively low proteoglycan content, low permeability [56]. Enhancing the mechanical properties of the tissue surface is resulted from cross-linking of proteoglycans and collagens [56]. It has high-density flattened chondrocytes in ellipsoid-shaped but in small volume relative to the other cartilage zones. The main role of this zone is to facilitate the wear and provide low frictional surfaces of the tissue. Second zone is middle zone in which cells are spheroidal shape and appear randomly distributed in less parallel thick collagen fibrils. Proteoglycan content is at maximum level and the cell density is much lower than the superficial zone. This zone comprises 40%–60% of total thickness and several times the volume of the superficial zone [57]. Third zone is a deep zone in which the cells appear to line up vertically in short, oriented irregular columns in the direction of thick collagen fibrils perpendicular to the articular surface. The water content is lowest in respect to the other zones [58]. Its collagen structure is characterized by large fibers that form bundles oriented perpendicular to the articular surface. Proteoglycan content is much lower than in the middle zone, and the cell density is also the lowest of all cartilaginous zones [39]. The final zone is a calcified zone separated from the deep zone by the tidemark. The stiffness values vary between the more flexible cartilage and rigid bone. In this zone, the cells in small size are distributed randomly in a matrix filled with hydroxyapatitic crystals [58].
The functional properties of cartilage under compression (especially repeated loading) are highly dependent on fluid pressurization within the tissue [59]. The articular cartilage shows both creep and stress-relaxation behaviors [60,61]. When a compressive load is applied onto the tissue, fluid phase bears it, and the nonlinear permeability acts as a protective mechanism. Then the solid matrix begins to bear more of the load as the fluid exudes from cartilage. Finally by lasting time, just tissue bears the load [39]. It is worth to point out that articular cartilages show anisotropic behavior in some mechanical testing such as tension [62]. The nonlinear characteristics of articular cartilage are due to collagen recruitment and energy absorption properties of the tissue. These compressive properties are a direct result of its biphasic nature due to the nonlinear permeability response [63]. The viscoelastic properties of articular cartilage are dependent of the interactions between collagen and proteoglycan networks [60].
Modeling cartilage is challenging mainly because it becomes anisotropic when it undergoes deformation [64]. There are several theoretical models have been used for articular cartilage, such as physico-chemical, elastic and viscoelastic, biphasic/poroelastic, thermoanalog, electro-magnetic, biocompanent, fiber-reinforced, and triphasic models [48,65]. These models have several limitations. The physico-chemical model is based on Donnan theory applied for homogeneous only. The linear elastic model of articular cartilage cannot be implemented to model the time-dependent or dynamic behavior of the articular cartilage tissue such as the fluid flow or solid consolidation. Therefore, it may be only applicable for simplistic mechanical models of articular cartilage under static or quasi-static loading conditions [48]. Fiber-reinforced models are other ones, which are capable of capturing the material nonlinearity of the cartilage tissue but not the geometric nonlinearity [66] and the quantitative measurements of collagen orientation have been neglected. Under large deformation assumptions, linear elasticity is no longer valid and the solid phase behavior of the articular cartilage tissue is better represented by a viscous and hyperelastic material model [48]. Some researcher view several of the models of cartilage discussed as equivalent to treating articular cartilage as a porous rock with extensive flow of fluid, whereas, there is evidence that hydrogel models [67] better describe the physical behavior of articular cartilage, including being consistent with its low permeability in comparison with assessment performed by Maroudas et al. [68].
The most popular theory for articular cartilage compressive viscoelastic behaviors is the biphasic theory developed by Mow et al. [63]. This model considers the collagen-proteoglycan matrix as an elastic solid which is intrinsically incompressible, porous and permeable. The main advantage of this model is particularly efficient for addressing time-dependent aspect of cartilage mechanics [48]. Lai et al. [65] developed their theory in to triphasic model with considering electrolytes and ions as a separated phase. In other words, negatively charged proteoglycans are modeled to be fixed to the solid matrix, and monovalent ions in the interstitial are modeled as additional fluid phases. Swelling property of articular cartilage could be described by this model [65]. The thermodynamic plausibility of the triphasic theory was studied by Huyghe and coworkers. They reported that unphysiological generation of free energy during each closed cycle of loading and unloading conflicting with second law of thermodynamics was a limitation of the triphasic model [69]. The correspondence between equilibrium biphasic and triphasic material properties of articular cartilage was investigated by Ateshian et al. [70]. It is worthy of note; however, the triphasic model of cartilage provides a more accurate description of the tissue composition and mechano-electrochemical response, the biphasic model is preferable to use because of its ability to successfully describe the response of cartilage to various loading conditions [70].
Some mechanical properties of cartilage are summarized in Table 2. The data show that material selection and scaffold preparation, which fulfill these requirements, are very challenging subjects whereas the structure of zone organization should be mimicked [53,55]. In other words, the mechanical thresholds that engineered tissue will likely encounter after performance. From a biomechanical perspective, engineered scaffolds of articular cartilage should behave as a multiphasic fiber-reinforced permeable composite with inhomogeneous, anisotropic, nonlinear, and viscoelastic properties [71]. For example, it has been reported that the tensile modulus of human knee joint cartilages was higher in the superficial zone as compared to the other zones due to the different organizations and thickness variation of collagen fibrils within different zones [72]. Tensile and compressive moduli of native cartilage typically have two-orders of magnitude difference due to the tension-compression nonlinearity attributed to the reinforcing characteristics of the stiff collagen fibers embedded within the ECM [73]. Hence, tissue repair could be carried out using a liable approach to satisfy these zonal organization properties. There are some strategies to repair articular cartilage tissue with respect to the injury type.
Table 2.
Mechanical properties of articular cartilage tissue (regardless of location).
| Mechanical Properties | Articular Cartilage |
|---|---|
| Tensile Modulus (at 10% ε) | 5–25 MPa [62,74] |
| Equilibrium Relaxation Modulus | 6.5–45 MPa [63] |
| Elongation to Break | 80% [32] |
| Ultimate Tensile Stress | 15–35 MPa [75] |
| Equilibrium Compressive Aggregate Modulus a | 0.1–2.0 MPa [37] |
| Hydraulic Permeability | 0.5–5.0 × 10−15 m4 N−1∙s−1 [37] |
| Intrinsic, Equilibrium Young’s Modulus in Compression b | 0.4–0.8 MPa [56] |
| Compressive Strength | 14–59 MPa [76] |
| Equilibrium Shear Modulus | 0.05–0.25 MPa [77] |
2.2. Joint Disease and Medical Interventions
There are different defects of articular cartilage with respect to the size, depth, and lesion locale including matrix disruption, partial-thickness and full-thickness [78]. Therefore, several treatments were suggested to repair and heal the defects [78]. Arthritis is one the most common disease caused trauma and inflammation hence cartilage repair is necessitate [79]. Exercises, use of anti-inflammatory medications and possibly an injection of steroid are some conservative treatments [78]. Tissue grafting, implantation of prostheses, autologous chondrocyte transplantation, microfracture, resection, and osteotomy are surgical interventions to repair cartilage [51,80,81]. Each treatment option has its own benefits, limitations, and clinical performance [37]. For example, donor site morbidity, risk of infection and inflammation of donor site, immune response and disease transmission are some important disadvantages of tissue grafting strategy. For example, donor site morbidity, risk of infection and inflammation of donor site, immune response and disease transmission are some important disadvantages of tissue grafting strategy [45].
2.3. Tissue Engineering of Cartilage and Scaffold Requirements
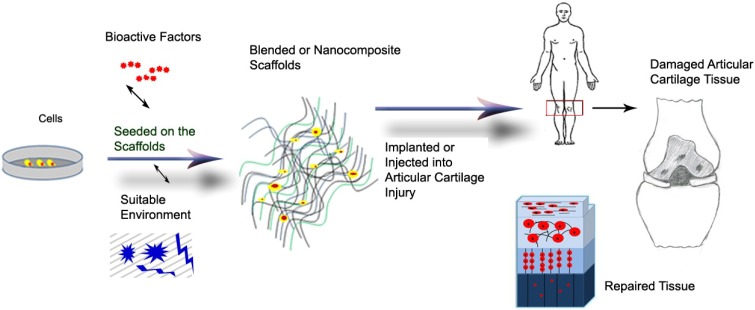
Tissue engineering is a promising approach to repair or regenerate damaged tissues, organs with respect to recover them in the maximum efficiency with hopes of improving clinical outcomes. Tissue engineering could be a promising alternative approach to regenerate articular cartilage tissue using three main parts: cells, biomaterial scaffolds and environment including mechanical stimuli and bioactive factors (Scheme 1) [78,82]. Articular chondrocytes, stem cells (induced pluripotent cells, IPCs; mesenchymal stromal cells, MSCs; and human embryonic stem cells, hESCs) and their combination are some examples of cells used for tissue engineering [83]. Because of low cellularity, there is a limitation of cell sources to clinical translation. Stimulating environment factors (e.g., growth factors, oxygen tension, gene, drugs and bioreactors) used to encourage appropriate in situ cell differentiation, cell proliferation and chondrogenesis for cartilage tissue engineering on the scaffolds [45,81,84,85,86,87,88,89,90,91]. The emphasis of this paper is on biomaterial scaffolds.
Scheme 1.
Schematic representation of the articular tissue engineering procedure.
There are some properties essential for scaffolds used as a matrix for articular tissue engineering to support cell fate and tissue mechanical properties for tissue or organ repair and regeneration [92,93,94,95]. The scaffolds should be porous and inter-connected so that cells could migrate and penetrate through the interstices. Surface properties of the scaffolds as well as materials play important roles such as cell attachment. Matrix biocompatibility and non-toxicity of degraded byproducts as well as matrix biodegradability are vital properties for good contact with native tissue compartment such as collagen fibrils and physiological remodeling, respectively. For enhancing interfacial integration between collagen fibrils and native tissue, the scaffold should be able to bond whilst it should be secured internal cohesiveness. There are some more factors, which should be considered for design and preparation of scaffolds, such as viscoelastic properties, which are responsible to resiliency during and following dynamic or static deformation; and structural anisotropy which provide anisotropic tissue organization similar to the native articular cartilage [45,84,85,86,89].
Scaffolds play a prominent role in encouraging chondrogenesis of the cell lineages due to providing structures for cells and facilitating the cellular and cell-matrix interactions, as well as affecting how cells sense mechanical loads [96]. They can be applied with cells or cell-free and also broadly categorized according to their chemical nature into natural, synthetic and their blend polymers. Composite and nanocomposite polymers are alternatives for engineered scaffolds of articular cartilage tissue [36]; they should help to mimic ECM structure and function of articular cartilage.
The success of tissue engineering depends on selecting materials with suitable properties such biocompatibility, cytotoxicity, suitable mechanical strength, implantability. Many natural polymers such as collagen [97], gelatin [98], hyaluronan [99], chondroitin sulphate [100], alginate [101], and chitosan [102] have been widely explored as promising biomaterials for tissue engineering, regenerative medicine and controlled delivery of biomolecules such as drugs, growth factors and cells to induce chondrogenic fate [89,103]. Although natural polymers are biocompatible, have good cell interactions and minimal stimulation to inflammatory or immunological responses of the host tissues they do not possess good mechanical properties. Modification of these polymers chemically or physically is an alternative process to improve their mechanical properties provided that their biological properties are not compromised [23,30,31].
3. Biomaterial Blends
Polymer blending is a well-known technique whenever property modification is required, because this inexpensive technology enables materials with full set of tailored properties and improved specific properties [104]. The main reason of blending is to widen the range of properties while obviating their drawbacks. Several advantages and disadvantages of some natural and synthetic polymers have been studied for the scaffold preparations of cartilage tissue engineering are summarized in Table 3. Usually the combination of natural polymers with synthetic polymers preserves the advantages of polymers. IPN or semi-IPN hydrogels are also other approaches to prepare materials that enable the scaffold mimics the structural properties of the articular tissue, as well as possess load-bearing properties [105].
Table 3.
Advantages and disadvantages of several natural and synthetic polymers have been extensively studied for cartilage tissue engineering, reprinted with permission from [6]. Copyright 2010 Elsevier.
| Polymers | Disadvantages | Advantages |
|---|---|---|
| Chitosan | Low tensile and compressive properties, low processability. |
Antibacterial activity, low toxicity, good cell interaction, good biocompatibility, renewability, water solubility, stability to variations of pH. |
| Collagen | Low tensile and compressive properties, high degradation rate. |
Low antigenicity, good cell adhesion, biological signaling, biodegradability. |
| Hyaluronic acid | Not support thermodynamically cell attachment. Hydrophilic surface. | No immunogenicity, good cell interaction. |
| Alginates | Hard processability, low tensile properties. | Injectable polymers, easily crosslinking under mild condition, high and tunable porosity scaffold, high diffusion rates of macromolecules, good cell incorporation. |
| Poly(ε-caprolactone) | Long term degradation application due to slow degradation rate, susceptible to undergo auto-catalyzed bulk hydrolysis, hydrophobic surface then no cell interaction. |
FDA approval, easily processable. |
| Polyurethane | Acidic degradation byproducts in poly(esther urethanes) causing autocatalyzed degradation and in vivo inflammation. |
Good tensile and compressive properties and also biological properties such as cell attachment, incorporation and supporting chondrocyte phenotype, and low infection. |
| PLGA | Low biological properties such as cell attachment, incorporation and supporting chondrocyte phenotype, releasing acidic degradation byproducts caused inflammatory response. |
FDA approval, tailorable physicomechanical properties. |
Blends of chitosan and collagen [106], collagen/hyaluronan/chitosan [107] and hydroxyapatite/collagen/chondroitin sulfate nanocomposite [108] are some examples of this classification. Sometimes, synthetic polymers, such as polyvinyl alcohol, are mixed with other synthetic ones to modify its drawbacks such as poor bioactivity. It must be borne in mind that the engineered articular cartilage should match the mechanical functionality of the native tissue. Therefore, engineered articular cartilages should have properties such as anisotropic, nonlinear, viscoelastic, and inhomogeneity. Preparation of composites based on material, which has a similar structure to glycosaminoglycans (GAGs) as a key component of cartilage ECM, could be considered as an attractive approach to achieve biomaterials for articular cartilage repair. Important characteristics of these polymer blends are provided in the following sections.
3.1. Blends with Collagen
Among natural biomaterials, collagen has attracted many interests because it is the most abundant protein constituting the natural ECM of articular cartilage which is responsible for expressing the chondrocytes phenotype, maintaining GAG production and supporting the chondrogenesis [84,109]. Collagen is synthesized by appropriate cells such as fibroblasts and osteoblasts [110,111]. The 90% of the dry weight of articular cartilage is composed of type II collagen in the form of crosslinked fibrils [112]. Collagen is a biocompatible, low antigenic and biodegradable polymer, which forms the extracellular framework, serves as a natural substrate for cell fate and provides the mechanical strength and shape of cartilages during articulation [97,111,113]. Adherent cells from bone marrow or periosteum were dispersed in collagen gel and transplanted into medial femoral condyle of rabbit model repair large and full thickness defect of articular cartilage [114]. It must be born in mind that the repair without chondrocyte transplantation resulted in fibrocartilage formation then the articular cartilage structure was not achieved [115]. The use of cells embedded in collagen gel instead of periosteal patches allowed rapid circumferential accumulation of newly synthesized matrix [116]; hence, the osteochondral progenitor cells had uniformly differentiated into chondrocytes and cartilage restored whilst mechanical properties of the repair defect were compliant [114].
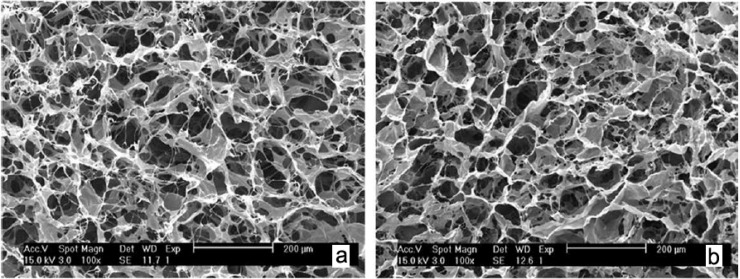
Two important limitations of collagen are low mechanical stability and rapid biodegradation rate causing it not to be used alone for application of articular cartilage tissue engineering. Hence, crosslinking [117], making blend or composite crosslinked collagen with natural or synthetic polymers are important approaches to overcome these problems [118]. Blend scaffolds of crosslinked collagen and chitosan are reported to have higher mechanical stability than pure collagen [106]. In this cited study, cell attachment and proliferation and viability were evaluated and revealed that the blended scaffolds were biocompatible and noncytotoxic and it may serve as a 3D matrix for cartilage tissue engineering [106]. As chitosan has more amino groups than collagen more cross-linking points will lead to higher biostability. Since collagen and chitosan are miscible at molecular level, they exhibit hydrogen bonding or electrostatic interaction that could reinforce the mechanical stability [106,119]. Adding chitosan to collagen could increase these susceptible sites to be crosslinked therefore it is difficult for enzymes to access the cleavage sites in collagen thereby increasing biostability and easily regulate the degradation rate (Figure 3) [106,118].
Figure 3.
The SEM images of (a) uncross-linked and (b) 0.3% genipin cross-linked collagen/chitosan scaffolds with 90/10 in blend ratio, reprinted with permission from [106]. Copyright 2010 Wiley Periodicals, Inc.
Lin et al. [107] also indicated that collagen/chitosan/hyaluronan hybrid polymer scaffold showed great potential as a desirable biomaterial for articular cartilage due to its excellent characters of cell adhesion, proliferation and matrix secretion. As chitosan shows cationic behavior due to its glucosamine residues and hyaluronan is an anion polysaccharide, tight ionic interaction bonds are present among them. The existence of such interactions of all compartment molecules could influence mechanical properties [107]. This behavior has been reported for collagen/chondroitin sulphate/chitosan hybrids in comparison to collagen scaffolds [29]. The scaffolds of collagen/chondroitin sulphate were not strong enough but incorporation of chitosan resulted in importing ionic interaction, tensile strength, and Young’s modulus [29]. Moreover, collagen/PVA nanofibers scaffold seeded with autologous MSCs was prepared by Abedi et al. [120] for the osteochondral defects repair of the rabbit joints due to the possibility of controlling cell fate to chondrogenicity.
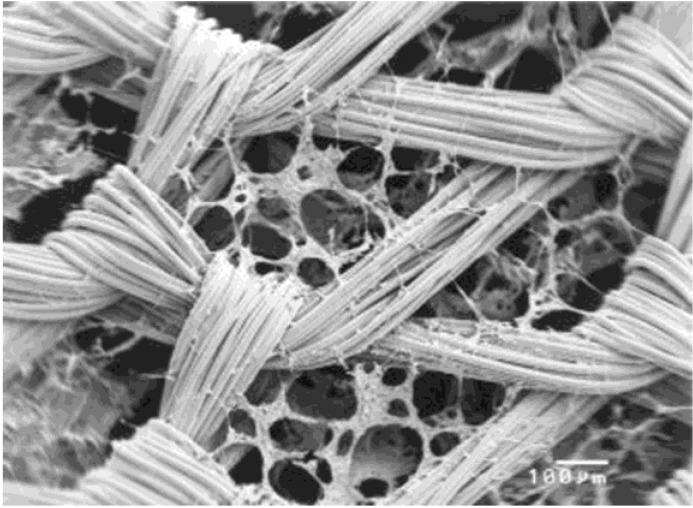
Biochemical and architectural development of the blend scaffolds could be regulated by chemical and mechanical environments. For example, cell differentiation and ECM production could be influenced by surface area, pore size and interconnectivity of the scaffold mesh. Chen et al. [121] prepared web-like collagen microsponges in the knitted mesh of PLGA with adjustable thickness and enhanced biomechanical properties (Figure 4). Overall, MSCs cultured in PLGA/collagen cobweb-like scaffold for ten weeks showed the mentioned microenvironment could induce chondrogenic differentiation due to the specific tailored architecture of the composite mesh. Switching gene expression from type I collagen to type II collagen, cell density and distribution uniformity throughout the scaffold as well as comparable mechanical properties to native articular cartilage indicated that this scaffold is applicable for articular cartilage repair [122].
Figure 4.
The SEM images of chondrocytes on the PLGA/collagen web after 1 day culturing, reprinted with permission from [121]. Copyright 2003 Wiley Periodicals, Inc.
3.2. Blends with Chondroitin Sulphate
Chondroitin sulphate is of GAGs, which is a major component of the ECM of cartilage [123]. ECM molecules of cartilage could regulate metabolism and gene expression in chondrocytes as well as stimulate cell proliferation and differentiation [124]. It was reported that chondroitin sulphate presence could influence mechanical properties of the scaffold, demonstrating its incorporation with desired guest materials could enhance compressive strength due to proteoglycan secretion promotion [125]. Nanda et al. [124] fabricated a hydrogel scaffold of PVA/chondroitin sulphate imitating the ECM thereby provides suitable environment for better articular cartilage repair in vivo. They studied the effect of hydrogel composition and crosslinking agent content on the physico-chemical, and mechanical properties of the scaffold. As a result, the surface of the hydrogel not only could fill the cartilage defect without any inflammation but also could integrate with surrounded tissues. Therefore, chondroitin sulphate release from the scaffold due to biodegradability could play an important role in articular cartilage repair for regulate metabolism. In a different approach, Ko and coworkers [126] attempted to mimic the native ECM of articular cartilage by incorporating type II collagen with chondroitin sulphate and hyaluronan to up-regulate biosynthetic activities. This group used freeze-drying and chemical crosslinking procedures to fabricate highly porous and interconnected network composite scaffold. Since type II collagen provides mechanical properties such as tensile strength which influences the bioactivity of the seeded chondrocytes and performs important biological functions, its incorporation of type II collagen with chondroitin sulphate could show synergistic effect on cartilage repair [125]. Not only material properties and scaffold pore structure could influence cell fate but also applying mechanical forces such as pressure gradient, fluid flow, mechanical strain can support and regulate chondrogenic lineage of MSCs [127]. Chen et al. [128] fabricated a microenvironment of composite based on chitosan, chondroitin sulphate and dermatan sulphate, which plays critical roles in stimulating ECM production and cartilage regeneration in the native articular cartilage ECM for mimicking native tissues. They used Response Surface Method to predict the incorporation of GAGs with chitosan then the optimal formulation with considering proper amounts and ratios was predicted [128]. In line with this, incorporation of gelatin, chondroitin sulphate with hyaluronan in fibrin glue, which makes a suitable environment for cell distribution and seeding was assessed by Chou et al. [129].
3.3. Blends with Chitosan
Chitosan, a deacetylated derivative of chitin, is the linear polysaccharide composed of glucosamine and N-acetyl glucosamine linked in a β(1-4) manner with cationic nature and high charge density in solution [130]. Due to its beneficial intrinsic properties such as biodegradablity, biocompatiblity, nonantigenicity, nontoxicity, biofunctionality, antimicrobiality besides similar characteristics with various GAGs and hyaluronic acid present in articular cartilage, it is well known functional aid in terms of connective tissue in-growth and neo-vascularization for the ordered regeneration of human cartilage tissues [9,131]. Although chitosan has a lot of intrinsic properties, which make it applicable for tissue engineering applications, but chitosan suffers from a relatively poor mechanical characteristic, therefore preparing blends and composites with other biomaterials attracted much interest [132,133]. Incorporation of chitosan into another biopolymer, such as collagen and alginateimproved its mechanical property and reduced the biodegradation rate [134]. In order to improve cell attachment, cell proliferation and biosynthetic production as well as spherical morphology maintenance, blending and surface modification with chitosan are two important approaches [135]. Alginate, a family of polyanionic copolymers derived from brown sea algae, could promote cell proliferation, maintain cell functionality and enhance phenotype [136]. Li et al. [135] fabricated chitosan/alginate scaffold via thermally induced phase separation followed by freeze drying. Combining chitosan with alginate led to increased cell viability, promoted production of type II collagen as well as retaining spherical morphology; therefore, these scaffolds could be used for cartilage repair. A new approach to prevent osteoarthritis development was attempted by Oprenyeszk et al. [133] who prepared a biphasic biomaterial scaffold comprised of alginate-chitosan beads dispersed in chitosan hydrogel and injected into rabbit knee. The overall outcome showed the presence of alginate/chitosan beads could affect cartilage structure and cellularity, maintain the morphology of chondrocytes, and decreased friction coefficient [133].
Poly(L-lactide-co-ε-caprolactone) (PCLC), a highly viscoelastic biomaterial with hydrophilic nature could be used to simulate the elastic collagen in the ECM of articular cartilage tissue when applied in vitro for long-term cyclic compression on the cell–scaffold construct [137]. Yan et al. [138] produced and characterized PCLC scaffold modified with chitosan and seeded with human mesenchymal stem cells (hMSCs) for achieving appropriate surface properties such as wettability and ionic charges essential for cell attachment. The porosity was kept constant while improving cell functionality and induction differentiation. Overall outcomes revealed the GAGs deposition, type II collagen production (ECM protein expression) as well as cartilage tissue formation through PCLC modified with chitosan were higher than PCLC scaffold due to improvement cell distribution through the scaffold. This was probably due to overcoming on confined high aggregation of cells within a small region. Furthermore mechanical properties such as elasticity improved relatively to PCLC alone and deformation recovery ratio was very similar to native tissue. The confined high aggregation of cells within a small region in the PCLC scaffold might have caused a deficit in nutrient supply locally, thus impeding long-term cellular proliferation [138]. The final Young’s modulus of modified scaffold was lower than the native articular cartilage hence some further research should be performed to overcome this inefficiency.
3.4. Blends with PVA
Given PVA’s anisotropy, viscoelastic and biphasic nature, high permeability to fluid, and biotribological properties, PVA hydrogels have been extensively studied and employed in artificial articular cartilage repair [63,105].
Fabrication of PVA hydrogels via freeze-thaw process makes them to exhibits mechanical properties approximately similar to articular cartilage [139]. Moreover, it seems that the PVA plays an effective role for chondrocyte activity [140]. In view of this, its clinical applications are still limited due to limited stability for long-term utility, and non-bioactivity in vivo in comparison with native cartilage [31]. There are some techniques to modify PVA, for instance, co-polymerization, blending, or compositing with nanoscale materials [31,141]. Such modification may influence biological properties such as biocompatibility or cytocompatibility of composites hence selecting suitable second material could be challenging [142].
However PVA was a candidate material for articular cartilage repair, preparation PVA with acrylamide as a crosslinking agent was one of strategies used to increase PVA water permeability thereby improving the lubrication for articulation [31,143]. Adding hydrophilic polymers such as polyethylene glycol or acrylamide while preparation could be an approach to increase lubricity as well as stability by preventing pore collapses due to removing from the hydrogels.
The presence of hydrogen bonding between hydroxyl groups of polymer surface and polar groups on cell surface makes PVA to be very adhesive for cells but this property should be tailored. PCL with hydrophobicity has been well known for cell attachment therefore this property would be controlled by blending these polymers together to balance hydrophilic-hydrophobic moieties. Mohan and Nair [144] have prepared a porous scaffold of PVA/PCL followed modifying with Arginine-Glycine-Aspartic acid (RGD) peptide coupling to impart cell anchoring and stable linking for chondrocyte attachment. They reported that PCL acted as reinforcement for PVA in the semi IPN scaffold with viscoelastic characteristics, provided a favorable cell environment for GAG secretion as well as good medium uptake ability; hence the supply of nutrients to cells penetrated within the scaffold would be adequate [144]. Similarly, the effect of some signaling molecules released from the scaffold like TGF-β1, TGF-β3, and BMP-2on the MSC fate and secretion of ECM molecules was also evaluated [145]. It was shown that the scaffold microenvironment promoted better differentiation of MSCs to chondrocytes.
Preparation of blends based on biomaterials with similar structure to ECM or with similar mechanical properties to hyaline cartilage could be appropriate strategy for articular cartilage repair. Lee et al. [146] used porous scaffolds of PVA and N,O-carboxymethylated chitosan (NOCC) to evaluate mechanical properties for articular cartilage tissue engineering applications. NOCC induces suitable results in regard to articular cartilage, because it is a derivative of chitosan, a semi-natural polymer similar to GAGs and may play role in modulating the morphology, differentiation, and function of chondrocytes. In line with this, Ibrahim et al. [147] proposed the use of hydroxyapatite reinforced bilayered scaffolds of PVA/NOCC seeded with hMSCs as a promising biomaterial to repair osteochondral defect. Since hydroxyapatite is osteoconductive, the first layer could mimic bone and increase osteocyte proliferation structure [148] while the mechanical properties of the scaffold’s upper layer mimics articular cartilage [146]; therefore; these biocompatible bilayered scaffolds would be promising candidates for osteochondral damage [147].
Tribiology and wear characteristic of PVA as an articular cartilage replacement as well as wear mechanism in reciprocating sliding against articular cartilage under certain conditions was assessed by Sardinha et al. [149]. These authors demonstrated that very low friction coefficient values from 0.02 to 0.05 and no degenerative changes with different applied loads or lubricant fluid were obtained for PVA. To increase water absorption of PVA hydrogel, Polyvinylpyrrolidone (PVP), is a good alternative material for blending due to amide groups with strong hydrophilicity rather than hydroxyl and carboxyl groups. Enhanced water content value up to 1.14% for 15 wt% PVP due to PVP addition causes friction coefficient decrement needed for hyaline cartilage during articulation, as well as providing viscoelastic behavior similar to articular cartilage tissue [150]. Ma et al. [151] evaluated some parameters on the tribiology behavior of PVA/PVP blends. The presence of bovine serum as a lubrication fluid in the blended material showed minimal wear behavior (friction coefficient: ca. 0.05) due to the formation a thick fluid film for friction reduction.
Long fixation of scaffolds comprised of PVA could be achieved by preparation of hydrogel scaffolds contain inter-connected porous network. Scholten et al. [152] used alginate microspheres for fabrication IPN scaffolds of PVA to support chondrocyte phenotype. The authors demonstrated that the presence of internal porous network within hydrogel not only could facilitate integration with the host tissue as well as promoting inward cellular migration but also the blended scaffold could perfectly control load bearing behavior similar to that of articular cartilage after implantation [152]. In another study, Bichara et al. [153] fabricated neocartilage tissue from PVA/alginate hydrogel cultured with human nasoseptal chondrocytes, demonstrating auricular cartilage achieved by a predefined-shape-specific construct via controlling gelation kinetics.
4. Biomaterial Nanocomposites
Articular cartilage tissue shows unique combinations of nonlinear properties as well as anisotropic behaviors due to composition and orientation of tissue components [63]. Scientists have been interested in regenerating articular cartilage using nanobiomaterials to achieve similar mechanical and physical properties with the natural tissue [154]. Nanocomposite refers to multiphase materials at the nanometric scale within polymer matrix could mimic native tissue properties; therefore, it could be another approach to gain this goal. These nanobiomaterials in different shapes, such as particles, fibers, etc., are mixed at the nanometer scale and they could show specific characteristics respect to the considered properties [155].
4.1. Polymer-Polymer Nanofiber Composites
It has been reported that ECM mimicry and maintenance of the chondrocytic phenotype are enhanced or promoted on the nanofiber scaffolds [156]. Li et al. [85] showed the enhanced chondrogenesis on nanofibrous scaffolds of the PCL in comparison with microfiber ones. Furthermore, Casper et al. [92] fabricated chitosan-coated PCL nanofiber scaffolds and placed them in the subperiosteal environment that behaves as a bioreactor and, hence, periosteal cells would penetrate into the scaffolds. They have reported that coating does not support cell penetration, proliferation and chondrogenic differentiation while this notion is in contrast to several published reports [102]. Likewise, Wise et al. [157] have reported that oriented nanofiber scaffolds of PCL could mimic the cell and ECM organization presented in the superfacial zone of articular cartilage. In another research, Coburn et al. [156] have demonstrated the chondrogenesity of nanofiber composite-base of PVA-methacrylate and chondroitin sulfate-methacrylate for articular cartilage repair. The low density scaffolds were cultured with MSCs for six weeks in both chondrogenic induction medium and in vivo. The presence of PVA with non-adhesive nature not only resulted in fibroblast invasion reduction in vivo but also enhanced GAG production while the presence of chondroitin sulfate in the fibers had a positive impact on increasing type II collagen synthesis and mechanical properties of tissues. Cell proliferation and differentiated into the chondrogenic lineage were confirmed by producing patterned ECM features and cartilage specific gene expression due to early cell infiltration and cartilage repair in an in vivo osteochondral defect of rat model [156]. Shin et al. [158] developed nanofiber scaffold of blend of PLGA (a blend of PLGA75/25 and PLGA50/50 in 1:1 blend ratio; 75/25 and 50/50 are lactic acid/glycolic acid ratios) and cultured them with porcine articular cartilage cells. Cellular responses such as GAG content, DNA content, as well as physical and mechanical properties, showed these blends were appropriate candidates for articular cartilage regeneration [158].
4.2. Polymer-Silica Nanoparticle Composites
Polymer-silica composites are another attractive class of materials for cartilage regeneration [159]. For example, Buchtova et al. [160] have fabricated improved hydrogel based on siloxane derived hydroxypropylmethylcellulose with mesoporous silica nanofibers, and yield efficient bionanocomposite ECMs resulted in mimicking cartilage tissue. The nanocomposite possessed dispersion at the nanoscale due to the chemical affinity between the hydrophilic silica nanofibers and the pendant silanolate groups of the polymer chains influenced gel point. Tuning the amount of nanocharges resulted by adding small amount of anisotropic, rod-like shape of the silica nanofibers, mechanical properties of the nanocomposite supported cartilage tissue requirements. Despite this, low compressive elastic moduli in comparison with native tissue caused them not to be applicable for articular cartilage repair except as a favorable environment for cells [160].
The feasibility of PVA/Si nanocomposite fabricated from PVA and tetra ethoxy silanena nospheres by sol-gel method for articular cartilage has been studied [80]. This nanocomposite could improve adhesion of the hydrogel on underlying bone with high bond strength so that it could not be loosen their integrities under applied loads [80]. Although these results show the improvement of durability of hydrogel and adhesion to the underlying tissue, further study is required in order to mimic composition and zonal organization of articular cartilage.
Enhancement of hydrogel mechanical properties, control and sustained co-delivery of biomacromolecules and therapeutic agents, as well as induce chondrogenicity function, are achieved by using mesoporous structure of silica nanoparticles. Zhu et al. [28] fabricated controlled release systems of composite hydrogel based on chitosan and silica nanoparticle for drug delivery applications. Introduction of nanoparticles with the rigid structure in hydrogels and then the existence of strong intermolecular interaction between nanoparticles silanol groups as well as chitosan susceptible groups resulted in improving hydrogel strength. Chitosan could use as a drug delivery system for biomacromolecules due to its positive charges but studies demonstrated a difficulty for hydrophilic drugs [161]. Introducing silica nanoparticle with mesoporous structure could resolve the release problem as well as produced GAGs and DNA demonstrate chondrocyte fate promotion due to lower concentration of released silicate ions in the inner environment [28].
4.3. Polymer-Hydroxyapatite Nanoparticle Composites
Hydroxyapatite nanocomposites have been used in several application fields especially in bone tissue engineering [148]. Hydroxyapatite is a biocompatible and bioactive material for construction of bone composition and it is osteoconductive [162]. Many studies demonstrated polymer-hydroxyapatite nanocomposites can stimuli osteoblast growth and proliferate [163]; however, there are also some studies regarding to cartilage tissue engineering and cartilage replacement [164,165]. The incorporation of these nanopoarticles with polymers, such as PVA, PLLA and chitosan can obviate some drawbacks of pure hydrogels by enhancing its physical and mechanical properties, biocompatibility, bioactivity and elasticity [165,166,167].
The use of bilayered or biphasic scaffold structures is an approach to promote the regeneration of articular cartilage while allowing for the repair of the underlying subchondral bone [168,169]. 3D macroporous chitosan-hydroxyapatite bilayered scaffolds were synthesized by Oliveira et al. [167] via a two-step procedure including sintering and freeze-drying as a bone layer and a cartilage layer, respectively. When bone marrow stromal cells (GBMCs) were cultured on these materials showed that the spongy structure with anisotropic porosity, adequate pore size and distribution with interconnectivity were supportive structure for cells to differentiate GBMCs into the chondrogenic lineage. Fabrication of controlled design of such scaffolds play more important role from manipulation point of view and make them good promising tissue substitutes for the regeneration of osteochondral defects but it may not be adequately applicable for the repair of articular cartilage of large animal models [170].
Shi et al. [171] prepared porous scaffolds of nanocomposites based on amphiphilic chitosan and hydroxyapatite by freeze-drying method for tracheal cartilage regeneration application. These scaffolds with pore size in the range of 200–500 μm and porosity more than 85% were cultured by rabbit chondrocytes and implanted subcutaneously into nude mice for eight weeks. The results of histomorphologic and biochemical assays revealed neonatal cartilage-like tissue were generated which were similar to mature hyaline cartilage.
As mentioned previously, PVA is a high promising material for cartilage [139] but its durability and week tissue adherent for a long term may not be ignored [172]. It has been claimed that compositing PVA with a bioactive and biocompatible material such as hydroxyapatite could improve fixation ability of the scaffolds to the surrounded tissues [173,174]. Pan and Xiong [166] have reported that the combination of PVA with hydroxyapatite can enhance not only mechanical properties and bioactivity but also adherent to around natural tissue [175]; therefore the aforementioned problem of PVA was omitted. They prepared PVA/hydroxyapatite nanocomposite by in situ synthesis method and incorporation with several repeated freeze-thaw cycle process (frozen at −20 °C for 12 h, and then thawed at 25 °C for 6 h). Viscoelastic properties of these PVA/hydroxyapatite nanocomposites were similar to viscoelastic behavior of articular cartilage [176]. Qu et al. [169] studied on PVA/gelatin/nano hydroxyapatite/polyamide-6 bilayered scaffolds via freeze-drying method for in situ osteochondral defect repair. The highly porous scaffolds possessed inter-connective pores structure assures morphological features necessary for regenerative medicine. Since gelatin may facilitate cellular adhesion and proliferation [31] and also PVA showed a good integrity and functionality of the osteochondral construct; hence, nanohydroxyapatite/polyamide-6 serves as a skeleton, providing the composite with high mechanical strength and promotes cell adhesion and proliferation. These scaffolds possessed biphasic behavior, which showed articular cartilage behavior in the upper layer and bone behavior within the lower layer [169]. The biocompatibility and chondrogenesis of the PVA- nano hydroxyapatite/polyamide-6 bilayered scaffolds were studied by culturing neonatal rabbit MSCs for two and results demonstrated good influence on the growth, proliferation and differentiation of chondrogenic MSCs. In vivo results revealed the induced BMSCs after seeding were well distributed in PVA-nano hydroxyapatite/polyamide-6 scaffold, in which they produced sufficient ECM to chondroid and or osteoid aggregates, and the neo-cartilage formed a new matrix, which was not seen in other bilayered scaffolds [177].
Polylactide (PLA) is of biocompatible, biodegradable and renewable materials, which could be modified to enhance its biological properties for cartilage engineering applications [178]. Spadaccio et al. [165] prepared a composite of electrospun PLA nanofiber with nanoparticle-hydroxyapatite to obviate the mentioned drawback as well as mimic the native histoarchitecture of osteochondral tissue thereby inducing chondrogenic differentiation of hMSCs toward chondrocyte by providing biological signaling and the biochemical effect of hydroxyapatite. It is worthy of note that the presence of hydroxyapatite may balance the pH of the cell environment containing acidic degradation byproducts. Tamai et al. [30] developed a triple composite scaffold of nanohydroxyapatite and poly-D,L-lactic acid/polyethylene glycol (PLA-PEG) as a carrier for recombinant human bone morphogenetic protein-2 (rhBMP-2) to stimulate the in vitro and in vivo. However, the mechanical properties of the scaffolds have not been reported; however, this bioactive scaffold could promote the repair of full-thickness articular cartilage defects within three weeks and hyaline cartilage appearance with a columnar organization of cells and mature matrix was observed after six weeks [30].
5. Conclusions
There is an increasing need for novel materials with desired properties for tissue engineering and regenerative medicine. This review article outlined the significant studies that have been performed in cartilage tissue engineering especially articular cartilage. Recent progress in the preparation material blends (natural-based and synthetic-based) and nanocomposite, as well as fabrication porous scaffolds with tailored properties, in the field of articular cartilage tissue engineering have been discussed. Having advanced engineering approaches suggests combination of material and biological science as well as technology needed for preparation novel biomaterials and for designing and controlling the polymeric scaffolds for tissue repair as the synergistic combinations of material characteristics and scaffold design play critical roles in cell interaction, provide mechanical properties and then tissue regeneration. A lot of research papers published regarding blends and composite materials for tissue engineering reveal there is a huge interest in this field; however most of results are far from clinical trials. In the near future, one can design multilayered biomaterial scaffolds, which may adequately mimic human articular cartilage tissue with respect to property and functionality of each zone while provides functional performance needed in long-term use with no sign of inflammation in vivo.
Acknowledgments
The authors would like to thank the University of British Columbia (Startup Grant) and NSERC (Discovery Grant) for financially supporting this work.
Author Contributions
Azadehsadat Hashemi Doulabi made substantial contributions to conception and acquisition of data, and analysis and interpretation of data, Kibret Mequanint participated in drafting the article and revising it critically for important intellectual content and Hadi Mohammadi gave final approval of the version to be submitted and any revised version. Acquisition of data: (Azadehsadat Hashemi Doulabi and Kibret Mequanint), analysis and interpretation of data: (Azadehsadat Hashemi Doulabi, Kibret Mequanint and Hadi Mohammadi), drafting of manuscript: (Azadehsadat Hashemi Doulabi and Hadi Mohammadi), Critical revision: (Azadehsadat Hashemi Doulabi, Kibret Mequanint and Hadi Mohammadi).
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Kohane D.S., Langer R. Polymeric biomaterials in tissue engineering. Pediatr. Res. 2008;63:487–491. doi: 10.1203/01.pdr.0000305937.26105.e7. [DOI] [PubMed] [Google Scholar]
- 2.Cheung H.-Y., Lau K.-T., Lu T.-P., Hui D. A critical review on polymer-based bio-engineered materials for scaffold development. Compos. B. 2007;38:291–300. doi: 10.1016/j.compositesb.2006.06.014. [DOI] [Google Scholar]
- 3.Thomson R.C., Wake M.C., Yaszemski M.J., Mikos A.G. Biodegradable polymer scaffolds to regenerate organs. In: Peppas N.A., Langer R.S., editors. Biopolymers II. Springer; Berlin/Heidelberg, Germany: 1995. pp. 245–274. [Google Scholar]
- 4.Temenoff J.S., Mikos A.G. Injectable biodegradable materials for orthopedic tissue engineering. Biomaterials. 2000;21:2405–2412. doi: 10.1016/S0142-9612(00)00108-3. [DOI] [PubMed] [Google Scholar]
- 5.Middleton J.C., Tipton A.J. Synthetic biodegradable polymers as orthopedic devices. Biomaterials. 2000;21:2335–2346. doi: 10.1016/S0142-9612(00)00101-0. [DOI] [PubMed] [Google Scholar]
- 6.Puppi D., Chiellini F., Piras A.M., Chiellini E. Polymeric materials for bone and cartilage repair. Prog. Polym. Sci. 2010;35:403–440. doi: 10.1016/j.progpolymsci.2010.01.006. [DOI] [Google Scholar]
- 7.Nesic D., Whiteside R., Brittberg M., Wendt D., Martin I., Mainil-Varlet P. Cartilage tissue engineering for degenerative joint disease. Adv. Drug Deliv. Rev. 2006;58:300–322. doi: 10.1016/j.addr.2006.01.012. [DOI] [PubMed] [Google Scholar]
- 8.Ratner B.D., Bryant S.J. Biomaterials: Where we have been and where we are going. Annu. Rev. Biomed. Eng. 2004;6:41–75. doi: 10.1146/annurev.bioeng.6.040803.140027. [DOI] [PubMed] [Google Scholar]
- 9.Muzzarelli R.A.A., Greco F., Busilacchi A., Sollazzo V., Gigante A. Chitosan, hyaluronan and chondroitin sulfate in tissue engineering for cartilage regeneration: A review. Carbohydr. Polym. 2012;89:723–739. doi: 10.1016/j.carbpol.2012.04.057. [DOI] [PubMed] [Google Scholar]
- 10.Gunatillake P.A., Adhikari R. Biodegradable synthetic polymers for tissue engineering. Eur. Cells Mater. 2003;5:1–16. doi: 10.22203/ecm.v005a01. [DOI] [PubMed] [Google Scholar]
- 11.Patterson J., Martino M.M., Hubbell J.A. Biomimetic materials in tissue engineering. Mater. Today. 2012;13:14–22. doi: 10.1016/S1369-7021(10)70013-4. [DOI] [Google Scholar]
- 12.Aizawa Y., Owen S.C., Shoichet M.S. Polymers used to influence cell fate in 3D geometry: New trends. Prog. Polym. Sci. 2012;37:645–658. doi: 10.1016/j.progpolymsci.2011.11.004. [DOI] [Google Scholar]
- 13.Mimura T., Imai S., Kubo M., Isoya E., Ando K., Okumura N., Matsusue Y. A novel exogenous concentration-gradient collagen scaffold augments full-thickness articular cartilage repair. Osteoarthr. Cartil. 2008;16:1083–1091. doi: 10.1016/j.joca.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 14.Lien S.-M., Chien C.-H., Huang T.-J. A novel osteochondral scaffold of ceramic-gelatin assembly for articular cartilage repair. Mater. Sci. Eng. C. 2009;29:315–321. doi: 10.1016/j.msec.2008.07.017. [DOI] [Google Scholar]
- 15.Könst Y.E., Benink R.J., Veldstra R., van der Krieke T.J., Helder M.N., van Royen B.J. Treatment of severe osteochondral defects of the knee by combined autologous bone grafting and autologous chondrocyte implantation using fibrin gel. Knee Surg. Sports Traumatol. Arthrosc. 2012;20:2263–2269. doi: 10.1007/s00167-012-1891-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Buschmann M.D., Gluzband Y.A., Grodzinsky A.J., Hunziker E.B. Mechanical compression modulates matrix biosynthesis in chondrocyte/agarose culture. J. Cell Sci. 1995;108:1497–1508. doi: 10.1242/jcs.108.4.1497. [DOI] [PubMed] [Google Scholar]
- 17.Fragonas E., Valente M., Pozzi-Mucelli M., Toffanin R., Rizzo R., Silvestri F., Vittur F. Articular cartilage repair in rabbits by using suspensions of allogenic chondrocytes in alginate. Biomaterials. 2000;21:795–801. doi: 10.1016/S0142-9612(99)00241-0. [DOI] [PubMed] [Google Scholar]
- 18.Lopes J.L., Machado J.M., Castanheira L., Granja P.L., Gama F.M., Dourado F., Gomes J.R. Friction and wear behaviour of bacterial cellulose against articular cartilage. Wear. 2011;271:2328–2333. doi: 10.1016/j.wear.2010.12.042. [DOI] [Google Scholar]
- 19.Alves da Silva M.L., Crawford A., Mundy J.M., Correlo V.M., Sol P., Bhattacharya M., Hatton P.V., Reis R.L., Neves N.M. Chitosan/polyester-based scaffolds for cartilage tissue engineering: Assessment of extracellular matrix formation. Acta Biomater. 2010;6:1149–1157. doi: 10.1016/j.actbio.2009.09.006. [DOI] [PubMed] [Google Scholar]
- 20.Basalo I.M., Chahine N.O., Kaplun M., Chen F.H., Hung C.T., Ateshian G.A. Chondroitin sulfate reduces the friction coefficient of articular cartilage. J. Biomech. 2007;40:1847–1854. doi: 10.1016/j.jbiomech.2006.07.007. [DOI] [PubMed] [Google Scholar]
- 21.Toh W.S., Lee E.H., Guo X.-M., Chan J.K.Y., Yeow C.H., Choo A.B., Cao T. Cartilage repair using hyaluronan hydrogel-encapsulated human embryonic stem cell-derived chondrogenic cells. Biomaterials. 2010;31:6968–6980. doi: 10.1016/j.biomaterials.2010.05.064. [DOI] [PubMed] [Google Scholar]
- 22.Zhang Y., Yang F., Liu K., Shen H., Zhu Y., Zhang W., Liu W., Wang S., Cao Y., Zhou G. The impact of PLGA scaffold orientation on in vitro cartilage regeneration. Biomaterials. 2012;33:2926–2935. doi: 10.1016/j.biomaterials.2012.01.006. [DOI] [PubMed] [Google Scholar]
- 23.Neves S.C., Moreira Teixeira L.S., Moroni L., Reis R.L., van Blitterswijk C.A., Alves N.M., Karperien M., Mano J.F. Chitosan/Poly(e-caprolactone) blend scaffolds for cartilage repair. Biomaterials. 2011;32:1068–1079. doi: 10.1016/j.biomaterials.2010.09.073. [DOI] [PubMed] [Google Scholar]
- 24.Bartlett Ii R.L., Sharma S., Panitch A. Cell-penetrating peptides released from thermosensitive nanoparticles suppress pro-inflammatory cytokine response by specifically targeting inflamed cartilage explants. Nanomedicine. 2013;9:419–427. doi: 10.1016/j.nano.2012.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Noguchi T., Yamamuro T., Oka M., Kumar P., Kotoura Y., Hyonyt S.-H., Ikada Y. Poly (vinyl alcohol) hydrogel as an artificial articular cartilage: Evaluation of biocompatibility. J. Appl. Biomater. 1991;2:101–107. doi: 10.1002/jab.770020205. [DOI] [PubMed] [Google Scholar]
- 26.Lee C.R., Grad S., Gorna K., Gogolewski S., Goessl A., Alini M. Fibrin-polyurethane composites for articular cartilage tissue engineering: A preliminary analysis. Tissue Eng. 2005;11:1562–1573. doi: 10.1089/ten.2005.11.1562. [DOI] [PubMed] [Google Scholar]
- 27.Sionkowska A. Current research on the blends of natural and synthetic polymers as new biomaterials: Review. Prog. Polym. Sci. 2011;36:1254–1276. doi: 10.1016/j.progpolymsci.2011.05.003. [DOI] [Google Scholar]
- 28.Zhu M., Zhu Y., Zhang L., Shi J. Preparation of chitosan/mesoporous silica nanoparticle composite hydrogels for sustained co-delivery of biomacromolecules and small chemical drugs. Sci. Technol. Adv. Mater. 2013;14 doi: 10.1088/1468-6996/14/4/045005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Berthod F., Saintigny G., Chretien F., Hayek D., Collombel C., Damour O. Optimization of thickness, pore size and mechanical properties of a biomaterial designed for deep burn coverage. Clin. Mater. 1994;15:259–265. doi: 10.1016/0267-6605(94)90055-8. [DOI] [PubMed] [Google Scholar]
- 30.Tamai N., Myoui A., Hirao M., Kaito T., Ochi T., Tanaka J., Takaoka K., Yoshikawa H. A new biotechnology for articular cartilage repair: Subchondral implantation of a composite of interconnected porous hydroxyapatite, synthetic polymer (PLA-PEG), and bone morphogenetic protein-2 (rhBMP-2) Osteoarthr Cartil. 2005;13:405–417. doi: 10.1016/j.joca.2004.12.014. [DOI] [PubMed] [Google Scholar]
- 31.Bodugoz-Senturk H., Macias C.E., Kung J.H., Muratoglu O.K. Poly(vinyl alcohol)-acrylamide hydrogels as load-bearing cartilage substitute. Biomaterials. 2009;30:589–596. doi: 10.1016/j.biomaterials.2008.10.010. [DOI] [PubMed] [Google Scholar]
- 32.Corkhill P.H., Trevett A.S., Tighe B.J. The potential of hydrogels as synthetic articular cartilage. Proc. Inst. Mech. Eng. H. 1990;204:147–155. doi: 10.1243/PIME_PROC_1990_204_249_02. [DOI] [PubMed] [Google Scholar]
- 33.Utracki L.A. History of commercial polymer alloys and blends (from a perspective of the patent literature) Polym. Eng. Sci. 1995;35:2–17. doi: 10.1002/pen.760350103. [DOI] [Google Scholar]
- 34.Ma P.X. Scaffolds for tissue fabrication. Mater. Today. 2004;7:30–40. [Google Scholar]
- 35.Khademhosseini A., Vacanti J., Langer R. Progress in tissue engineering. Sci. Am. 2009;300:64–71. doi: 10.1038/scientificamerican0509-64. [DOI] [PubMed] [Google Scholar]
- 36.Duarte Campos D.F., Drescher W., Rath B., Tingart M., Fischer H. Supporting biomaterials for articular cartilage repair. Cartilage. 2012;3:205–221. doi: 10.1177/1947603512444722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hunziker E.B. Articular cartilage repair: Basic science and clinical progress. A review of the current status and prospects. Osteoarthr. Cartil. 2002;10:432–463. doi: 10.1053/joca.2002.0801. [DOI] [PubMed] [Google Scholar]
- 38.Chung C., Burdick J.A. Engineering cartilage tissue. Adv. Drug Deliv. Rev. 2008;60:243–262. doi: 10.1016/j.addr.2007.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Athanasiou K.A., Darling E.M., Hu J.C. Articular cartilage tissue engineering. In: Athanasiou K.A., editor. Synthesis Lectures on Tissue Engineering. Morgan & Claypool Publishers; San Rafael, CA, USA: 2009. [Google Scholar]
- 40.Mankin H., Mow V., Buckwalter J., Iannotti J., Ratcliffe A. Articular cartilage structure, composition, and function. In: Buckwalter J., Einhorn T., Simon S., editors. Orthopaedic Basic Science: Biology and Biomechanics of the Musculoskeletal System. 2nd ed. American Academy of Orthopaedic Surgeons Publishers; Rosemont, IL, USA: 2000. pp. 443–470. [Google Scholar]
- 41.Mow V.C., Holmes M.H., Lai W.M. Fluid transport and mechanical properties of articular cartilage: A review. J. Biomech. 1984;17:377–394. doi: 10.1016/0021-9290(84)90031-9. [DOI] [PubMed] [Google Scholar]
- 42.Mow V.C., Lai W.M. Mechanics of animal joints. Annu. Rev. Fluid. Mech. 1979;11:247–288. doi: 10.1146/annurev.fl.11.010179.001335. [DOI] [Google Scholar]
- 43.Heinegard D., Oldberg A. Structure and biology of cartilage and bone matrix noncollagenous macromolecules. FASEB J. 1989;3:2042–2051. doi: 10.1096/fasebj.3.9.2663581. [DOI] [PubMed] [Google Scholar]
- 44.Buckwalter J.A., Mankin H.J. Articular cartilage: Tissue design and chondrocyte-matrix interactions. Instr. Course Lect. 1998;47:477–486. [PubMed] [Google Scholar]
- 45.Temenoff J.S., Mikos A.G. Review: Tissue engineering for regeneration of articular cartilage. Biomaterials. 2000;21:431–440. doi: 10.1016/S0142-9612(99)00213-6. [DOI] [PubMed] [Google Scholar]
- 46.Poole C.A. Articular cartilage chondrons: Form, function and failure. J. Anat. 1997;191:1–13. doi: 10.1046/j.1469-7580.1997.19110001.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Weiss C., Rosenberg L., Helfet A.J. An ultrastructural study of normal young adult human articular cartilage. J. Bone Joint Surg. Am. 1968;50:663–674. doi: 10.2106/00004623-196850040-00002. [DOI] [PubMed] [Google Scholar]
- 48.Mohammadi H., Mequanint K., Herzog W. Computational aspects in mechanical modeling of the articular cartilage tissue. Proc. Inst. Mech. Eng. H. 2013;227:402–420. doi: 10.1177/0954411912470239. [DOI] [PubMed] [Google Scholar]
- 49.Herzog W., Diet S., Suter E., Mayzus P., Leonard T.R., Müller C., Wu J.Z., Epstein M. Material and functional properties of articular cartilage and patellofemoral contact mechanics in an experimental model of osteoarthritis. J. Biomech. 1998;31:1137–1145. doi: 10.1016/S0021-9290(98)00136-5. [DOI] [PubMed] [Google Scholar]
- 50.Hunziker E.B., Michel M., Studer D. Ultrastructure of adult human articular cartilage matrix after cryotechnical processing. Microsc. Res. Tech. 1997;37:271–284. doi: 10.1002/(SICI)1097-0029(19970515)37:4<271::AID-JEMT3>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 51.Trippel S.B., Henry M.J. Articular cartilage injury and repair. In: Siliski J.M., editor. Traumatic Disorders of the Knee. Springer-Verlag; New York, NY, USA: 1994. pp. 19–36. [Google Scholar]
- 52.Buckwalter J.A., Rosenberg L., Hunziker E.B. Articular cartilage: Composition, structure, response to injury, and methods of facilitating repair. In: Ewing J.W., editor. Articular Cartilage and Knee Joint Function: Basic Science and Arthroscopy. Raven Press; New York, NY, USA: 1990. pp. 19–56. [Google Scholar]
- 53.Klein T.J., Malda J., Sah R.L., Hutmacher D.W. Tissue engineering of articular cartilage with biomimetic zones. Tissue Eng. B Rev. 2009;15:143–157. doi: 10.1089/ten.teb.2008.0563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hung C.T., Lima E.G., Mauck R.L., Taki E., LeRoux M.A., Lu H.H., Stark R.G., Guo X.E., Ateshian G.A. Anatomically shaped osteochondral constructs for articular cartilage repair. J. Biomech. 2003;36:1853–1864. doi: 10.1016/S0021-9290(03)00213-6. [DOI] [PubMed] [Google Scholar]
- 55.Nguyen L.H., Kudva A.K., Saxena N.S., Roy K. Engineering articular cartilage with spatially-varying matrix composition and mechanical properties from a single stem cell population using a multi-layered hydrogel. Biomaterials. 2011;32:6946–6952. doi: 10.1016/j.biomaterials.2011.06.014. [DOI] [PubMed] [Google Scholar]
- 56.Mow V.C., Guo X.E. Mechano-electrochemical properties of articular cartilage: Their inhomogeneities and anisotropies. Annu. Rev. Biochem. 2002;4:175–209. doi: 10.1146/annurev.bioeng.4.110701.120309. [DOI] [PubMed] [Google Scholar]
- 57.Stockwell R.A. The interrelationship of cell density and cartilage thickness in mammalian articular cartilage. J. Anat. 1971;109:411–421. [PMC free article] [PubMed] [Google Scholar]
- 58.Flik K.R., Verma N., Cole B., Bach B., Jr. Articular cartilage. In: Williams R. III, editor. Cartilage Repair Strategies. Humana Press; Totowa, NJ, USA: 2007. pp. 1–12. [Google Scholar]
- 59.Linn F.C., Sokoloff L. Movement and composition of interstitial fluid of cartilage. Arthritis Rheum. 1965;8:481–494. doi: 10.1002/art.1780080402. [DOI] [PubMed] [Google Scholar]
- 60.Mak A.F. The apparent viscoelastic behavior of articular cartilage—The contributions from the intrinsic matrix viscoelasticity and interstitial fluid flows. J. Biomech. Eng. 1986;108:123–130. doi: 10.1115/1.3138591. [DOI] [PubMed] [Google Scholar]
- 61.Cohen N.P., Foster R.J., Mow V.C. Composition and dynamics of articular cartilage: Structure, function, and maintaining healthy state. J. Orthop. Sport Phys. 1998;28:203–215. doi: 10.2519/jospt.1998.28.4.203. [DOI] [PubMed] [Google Scholar]
- 62.Moutos F.T., Freed L.E., Guilak F. A biomimetic three-dimensional woven composite scaffold for functional tissue engineering of cartilage. Nat. Mater. 2007;6:162–167. doi: 10.1038/nmat1822. [DOI] [PubMed] [Google Scholar]
- 63.Mow V.C., Kuei S.C., Lai W.M., Armstrong C.G. Biphasic creep and stress relaxation of articular cartilage in compression: Theory and experiments. J. Biomech. Eng. 1980;102:73–84. doi: 10.1115/1.3138202. [DOI] [PubMed] [Google Scholar]
- 64.Federico S., Herzog W. On the anisotropy and inhomogeneity of permeability in articular cartilage. Biomech. Model. Mechanobiol. 2008;7:367–378. doi: 10.1007/s10237-007-0091-0. [DOI] [PubMed] [Google Scholar]
- 65.Lai W.M., Hou J.S., Mow V.C. A triphasic theory for the swelling and deformation behaviors of articular cartilage. J. Biomech. Eng. 1991;113:245–258. doi: 10.1115/1.2894880. [DOI] [PubMed] [Google Scholar]
- 66.Hukins D.W.L., Aspden R.M. Fiber reinforcing in articular cartilage. In: Yettram A.L., editor. Material Properties and Stress Analysis in Biomechanics. Manchester University Press; New York, NY, USA: 1989. pp. 44–59. [Google Scholar]
- 67.Kovach I.S. A molecular theory of cartilage viscoelasticity. Biophys. Chem. 1996;59:61–73. doi: 10.1016/0301-4622(95)00115-8. [DOI] [PubMed] [Google Scholar]
- 68.Maroudas A., Bullough P., Swanson S.A.V., Freeman M.A.R. The permeability of articular cartilage. J. Bone Joint Surg. Br. 1968;5B:166–177. [PubMed] [Google Scholar]
- 69.Huyghe J.M., Wilson W., Malakpoor K. On the thermodynamical admissibility of the triphasic theory of charged hydrated tissues. J. Biomech. Eng. 2009;131 doi: 10.1115/1.3049531. [DOI] [PubMed] [Google Scholar]
- 70.Ateshian G.A., Chahine N.O., Basalo I.M., Hung C.T. The correspondence between equilibrium biphasic and triphasic material properties in mixture models of articular cartilage. J. Biomech. 2004;37:391–400. doi: 10.1016/S0021-9290(03)00252-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Moutos F.T., Guilak F. Composite scaffolds for cartilage tissue engineering. Biorheology. 2008;45:501–512. [PMC free article] [PubMed] [Google Scholar]
- 72.Akizuki S., Mow V.C., Müller F., Pita J.C., Howell D.S., Manicourt D.H. Tensile properties of human knee joint cartilage: I. Influence of ionic conditions, weight bearing, and fibrillation on the tensile modulus. J. Orthop. Res. 1986;4:379–392. doi: 10.1002/jor.1100040401. [DOI] [PubMed] [Google Scholar]
- 73.Cohen B., Lai W.M., Mow V.C. A transversely isotropic biphasic model for unconfined compression of growth plate and chondroepiphysis. J. Biomech. Eng. 1998;120:491–496. doi: 10.1115/1.2798019. [DOI] [PubMed] [Google Scholar]
- 74.Woo S.L.Y., Akeson W.H., Jemmott G.F. Measurements of nonhomogeneous, directional mechanical properties of articular cartilage in tension. J. Biomech. 1976;9:785–791. doi: 10.1016/0021-9290(76)90186-X. [DOI] [PubMed] [Google Scholar]
- 75.Kempson G.E., Freeman M.A.R., Swanson S.A.V. Tensile properties of articular cartilage. Nature. 1968;220:1127–1128. doi: 10.1038/2201127b0. [DOI] [PubMed] [Google Scholar]
- 76.Kerin A.J., Wisnom M.R., Adams M.A. The compressive strength of articular cartilage. Proc. Inst. Mech. Eng. H. 1998;212:273–280. doi: 10.1243/0954411981534051. [DOI] [PubMed] [Google Scholar]
- 77.Buckley M.R., Gleghorn J.P., Bonassar L.J., Cohen I. Mapping the depth dependence of shear properties in articular cartilage. J. Biomech. 2008;41:2430–2437. doi: 10.1016/j.jbiomech.2008.05.021. [DOI] [PubMed] [Google Scholar]
- 78.Chiang H., Jiang C.-C. Repair of articular cartilage defects: Review and perspectives. J. Formos. Med. Assoc. 2009;108:87–101. doi: 10.1016/S0929-6646(09)60039-5. [DOI] [PubMed] [Google Scholar]
- 79.Buckwalter J.A., Mankin H.J. Instructional course lectures, the American Academy of orthopaedic surgeons-articular cartilage. Part II: Degeneration and osteoarthrosis, repair, regeneration, and transplantation. J. Bone Joint Surg. 1997;79:612–632. [Google Scholar]
- 80.Bera B. Development of artificial articular cartilage. Sadhana. 2009;34:823–831. doi: 10.1007/s12046-009-0048-3. [DOI] [Google Scholar]
- 81.Brittberg M., Peterson L., Sjouml E., Tallheden T., Lindahl A. Articular cartilage engineering with autologous chondrocyte transplantation. A review of recent developments. J. Bone Joint Surg. 2003;85:109–115. doi: 10.2106/00004623-200300003-00017. [DOI] [PubMed] [Google Scholar]
- 82.Ikada Y. Challenges in tissue engineering. J. R. Soc. Interface. 2006;3:589–601. doi: 10.1098/rsif.2006.0124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Meretoja V.V., Dahlin R.L., Wright S., Kasper F.K., Mikos A.G. The effect of hypoxia on the chondrogenic differentiation of co-cultured articular chondrocytes and mesenchymal stem cells in scaffolds. Biomaterials. 2013;34:4266–4273. doi: 10.1016/j.biomaterials.2013.02.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Mauck R.L., Soltz M.A., Wang C.C.B., Wong D.D., Chao P.H., Valhmu W.B., Hung C.T., Ateshian G.A. Functional tissue engineering of articular cartilage through dynamic loading of chondrocyte-seeded agarose gels. J. Biomech. Eng. 2000;122:252–260. doi: 10.1115/1.429656. [DOI] [PubMed] [Google Scholar]
- 85.Li W.-J., Tuli R., Okafor C., Derfoul A., Danielson K.G., Hall D.J., Tuan R.S. A three-dimensional nanofibrous scaffold for cartilage tissue engineering using human mesenchymal stem cells. Biomaterials. 2005;26:599–609. doi: 10.1016/j.biomaterials.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 86.Van der Kraan P.M., Buma P., van Kuppevelt T., van den Berg W.B. Interaction of chondrocytes, extracellular matrix and growth factors: Relevance for articular cartilage tissue engineering. Osteoarthr. Cartil. 2002;10:631–637. doi: 10.1053/joca.2002.0806. [DOI] [PubMed] [Google Scholar]
- 87.Mauck R.L., Nicoll S.B., Seyhan S.L., Ateshian G.A., Hung C.T. Synergistic action of growthfactors and dynamic loading for articular cartilage tissue engineering. Tissue Eng. 2003;9:597–611. doi: 10.1089/107632703768247304. [DOI] [PubMed] [Google Scholar]
- 88.Johnstone B., Yoo J.U. Autologous mesenchymal progenitor cells in articular cartilage repair. Clin. Orthop. Relat. Res. 1999;367:156–162. doi: 10.1097/00003086-199910001-00017. [DOI] [PubMed] [Google Scholar]
- 89.Cancedda R., Dozin B., Giannoni P., Quarto R. Tissue engineering and cell therapy of cartilage and bone. Matrix Biol. 2003;22:81–91. doi: 10.1016/S0945-053X(03)00012-X. [DOI] [PubMed] [Google Scholar]
- 90.Fortier L.A., Barker J.U., Strauss E.J., McCarrel T.M., Cole B.J. The role of growth factors in cartilage repair. Clin. Orthop. Relat. Res. 2011;469:2706–2715. doi: 10.1007/s11999-011-1857-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Darling E.M., Athanasiou K.A. Rapid phenotypic changes in passaged articular chondrocyte subpopulations. J. Orthop. Res. 2005;23:425–432. doi: 10.1016/j.orthres.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 92.Casper M.E., Fitzsimmons J.S., Stone J.J., Meza A.O., Huang Y., Ruesink T.J., O’Driscoll S.W., Reinholz G.G. Tissue engineering of cartilage using poly-e-caprolactone nanofiber scaffolds seeded in vivo with periosteal cells. Osteoarthr. Cartil. 2010;18:981–991. doi: 10.1016/j.joca.2010.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Grande D.A., Halberstadt C., Naughton G., Schwartz R., Manji R. Evaluation of matrix scaffolds for tissue engineering of articular cartilage grafts. J. Biomed. Mater. Res. 1997;34:211–220. doi: 10.1002/(SICI)1097-4636(199702)34:2<211::AID-JBM10>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 94.Amanpour S., Solouk A., Mirzadeh H., Mohagheghi M.-A., Rabbani S., Tirgari F. In vitro and in vivo assays of cartilage repair by perforated polyurethane scaffold. Iran Polym. J. 2010;19:403–415. [Google Scholar]
- 95.Getgood A., Brooks R., Fortier L., Rushton N. Articular cartilage tissue engineering: Today’s research, tomorrow’s practice? J. Bone Joint Surg. Br. 2009;91:565–576. doi: 10.1302/0301-620X.91B5.21832. [DOI] [PubMed] [Google Scholar]
- 96.Toh W., Lee E., Cao T. Potential of human embryonic stem cells in cartilage tissue engineering and regenerative medicine. Stem Cell Rev. Rep. 2011;7:544–559. doi: 10.1007/s12015-010-9222-6. [DOI] [PubMed] [Google Scholar]
- 97.Eyre D. Collagen of articular cartilage. Arthritis Res. 2002;4:30–35. doi: 10.1186/ar380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Lien S.-M., Ko L.-Y., Huang T.-J. Effect of pore size on ECM secretion and cell growth in gelatin scaffold for articular cartilage tissue engineering. Acta Biomater. 2009;5:670–679. doi: 10.1016/j.actbio.2008.09.020. [DOI] [PubMed] [Google Scholar]
- 99.Kim D.-D., Kim D.-H., Son Y.-J. Three-dimensional porous scaffold of hyaluronic acid for cartilage tissue engineering. Stud. Mechanobiol. Tissue Eng. Biomater. 2011;8:329–349. [Google Scholar]
- 100.Martel-Pelletier J., Kwan Tat S., Pelletier J.P. Effects of chondroitin sulfate in the pathophysiology of the osteoarthritic joint: A narrative review. Osteoarthr. Cartil. 2010;18:7–11. doi: 10.1016/j.joca.2010.01.015. [DOI] [PubMed] [Google Scholar]
- 101.Wang C.-C., Yang K.-C., Lin K.-H., Liu H.-C., Lin F.-H. A highly organized three-dimensionalalginate scaffold for cartilage tissue engineering prepared by microfluidic technology. Biomaterials. 2011;32:7118–7126. doi: 10.1016/j.biomaterials.2011.06.018. [DOI] [PubMed] [Google Scholar]
- 102.Francis Suh J.K., Matthew H.W.T. Application of chitosan-based polysaccharide biomaterials in cartilage tissue engineering: A review. Biomaterials. 2000;21:2589–2598. doi: 10.1016/S0142-9612(00)00126-5. [DOI] [PubMed] [Google Scholar]
- 103.Seo S., Na K. Mesenchymal stem cell-based tissue engineering for chondrogenesis. J. Biomed. Biotechnol. 2011;2011:1–8. doi: 10.1155/2011/806891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hashemi Doulabi A., Mirzadeh H., Imani M. Interaction and miscibility study of fumarate-based oligomer macromers with chitosan. Mater. Chem. Phys. 2013;139:515–524. doi: 10.1016/j.matchemphys.2013.01.051. [DOI] [Google Scholar]
- 105.Kobayashi M., Chang Y.-S., Oka M. A two year in vivo study of polyvinyl alcohol-hydrogel (PVA-H) artificial meniscus. Biomaterials. 2005;26:3243–3248. doi: 10.1016/j.biomaterials.2004.08.028. [DOI] [PubMed] [Google Scholar]
- 106.Yan L.-P., Wang Y.-J., Ren L., Wu G., Caridade S.G., Fan J.-B., Wang L.Y., Ji P.H., Oliveira J.T., Mano J.F., et al. Genipin-cross-linked collagen/chitosan biomimetic scaffolds for articular cartilage tissue engineering applications. J. Biomed. Mater. Res. A. 2010;95:465–475. doi: 10.1002/jbm.a.32869. [DOI] [PubMed] [Google Scholar]
- 107.Lin Y.-C., Tan F.-J., Marra K.G., Jan S.-S., Liu D.-C. Synthesis and characterization of collagen/hyaluronan/chitosan composite sponges for potential biomedical applications. Acta Biomater. 2009;5:2591–2600. doi: 10.1016/j.actbio.2009.03.038. [DOI] [PubMed] [Google Scholar]
- 108.Rhee S.H., Tanaka J. Synthesis of a hydroxyapatite/collagen/chondroitin sulfate nanocomposite by a novel precipitation method. J. Am. Ceram. Soc. 2001;84:459–461. doi: 10.1111/j.1151-2916.2001.tb00679.x. [DOI] [Google Scholar]
- 109.Lu Z., Doulabi B.Z., Huang C., Bank R.A., Helder M.N. Collagen type II enhances chondrogenesis in adipose tissue-derived stem cells by affecting cell shape. Tissue Eng. A. 2009;16:81–90. doi: 10.1089/ten.TEA.2009.0222. [DOI] [PubMed] [Google Scholar]
- 110.Lee C.H., Singla A., Lee Y. Biomedical applications of collagen. Int. J. Pharm. 2001;221:1–22. doi: 10.1016/S0378-5173(01)00691-3. [DOI] [PubMed] [Google Scholar]
- 111.Nair L.S., Laurencin C.T. Biodegradable polymers as biomaterials. Prog. Polym. Sci. 2007;32:762–798. doi: 10.1016/j.progpolymsci.2007.05.017. [DOI] [Google Scholar]
- 112.Responte D.J., Natoli R.M., Athanasiou K.A. Collagens of articular cartilage: Structure, function, and importance in tissue engineering. Crit. Rev. Biomed. Eng. 2007;35:363–411. doi: 10.1615/CritRevBiomedEng.v35.i5.20. [DOI] [PubMed] [Google Scholar]
- 113.Lynn A.K., Yannas I.V., Bonfield W. Antigenicity and immunogenicity of collagen. J. Biomed. Mater. Res. B. 2004;71:343–354. doi: 10.1002/jbm.b.30096. [DOI] [PubMed] [Google Scholar]
- 114.Wakitani S., Goto T., Pineda S.J., Young R.G., Mansour J.M., Caplan A.I., Goldberg V.M. Mesenchymal cell-based repair of large, full-thickness defects of articular cartilage. J. Bone Joint Surg. Am. 1994;76:579–592. doi: 10.2106/00004623-199404000-00013. [DOI] [PubMed] [Google Scholar]
- 115.Wakitani S., Kimura T., Hirooka A., Ochi T., Yoneda M., Yasui N., Owaki H., Ono K. Repair of rabbit articular surfaces with allograft chondrocytes embedded in collagen gel. J. Bone Joint Surg. Br. 1989;71:74–80. doi: 10.1302/0301-620X.71B1.2915011. [DOI] [PubMed] [Google Scholar]
- 116.Kawamura S., Wakitani S., Kimura T., Maeda A., Caplan A.I., Shino K., Ochi T. Articular cartilage repair: Rabbit experiments with a collagen gel-biomatrix and chondrocytes cultured in it. Acta Orthop. 1998;69:56–62. doi: 10.3109/17453679809002358. [DOI] [PubMed] [Google Scholar]
- 117.Yang X., Guo L., Fan Y., Zhang X. Preparation and characterization of macromolecule cross-linked collagen hydrogels for chondrocyte delivery. Int. J. Biol. Macromol. 2013;61:487–493. doi: 10.1016/j.ijbiomac.2013.07.021. [DOI] [PubMed] [Google Scholar]
- 118.Taravel M.N., Domard A. Relation between the physicochemical characteristics of collagen and its interactions with chitosan: I. Biomaterials. 1993;14:930–938. doi: 10.1016/0142-9612(93)90135-O. [DOI] [PubMed] [Google Scholar]
- 119.Sionkowska A., Wisniewski M., Skopinska J., Kennedy C.J., Wess T.J. Molecular interactions in collagen and chitosan blends. Biomaterials. 2004;25:795–801. doi: 10.1016/S0142-9612(03)00595-7. [DOI] [PubMed] [Google Scholar]
- 120.Abedi G., Sotoudeh A., Soleymani M., Shafiee A., Mortazavi P., Aflatoonian M.R. A collagen-poly(vinyl alcohol) nanofiber scaffold for cartilage repair. J. Biomater. Sci. Polym. Ed. 2011;22:2445–2455. doi: 10.1163/092050610X540503. [DOI] [PubMed] [Google Scholar]
- 121.Chen G., Sato T., Ushida T., Hirochika R., Shirasaki Y., Ochiai N., Tateishi T. The use of a novel PLGA fiber/collagen composite web as a scaffold for engineering of articular cartilage tissue with adjustable thickness. J. Biomed. Mater. Res. A. 2003;67:1170–1180. doi: 10.1002/jbm.a.10164. [DOI] [PubMed] [Google Scholar]
- 122.Chen G., Liu D., Tadokoro M., Hirochika R., Ohgushi H., Tanaka J., Tateishi T. Chondrogenic differentiation of human mesenchymal stem cells cultured in a cobweb-like biodegradable scaffold. Biochem. Biophys. Res. Commun. 2004;322:50–55. doi: 10.1016/j.bbrc.2004.07.071. [DOI] [PubMed] [Google Scholar]
- 123.Athansou N.A., Puddle B., Sallie B. Highly sulphated glycosaminoglycans in articular cartilage and other tissues containing beta 2 microglobulin dialysis amyloid deposits. Nephrol. Dial. Transplant. 1995;10:1672–1678. [PubMed] [Google Scholar]
- 124.Nanda S., Sood N., Reddy B.V.K., Markandeywar T.S. Preparation and characterization of poly(vinyl alcohol)-chondroitin sulphate hydrogel as scaffolds for articular cartilage regeneration. Indian J. Mater. Sci. 2013;2013 doi: 10.1155/2013/516021. [DOI] [Google Scholar]
- 125.Yang Y.-L., Sun C., Wilhelm M.E., Fox L.J., Zhu J., Kaufman L.J. Influence of chondroitin sulfate and hyaluronic acid on structure, mechanical properties, and glioma invasion of collagen I gels. Biomaterials. 2011;32:7932–7940. doi: 10.1016/j.biomaterials.2011.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Ko C.-S., Huang J.-P., Huang C.-W., Chu I.M. Type II collagen-chondroitin sulfate-hyaluronan scaffold cross-linked by genipin for cartilage tissue engineering. J. Biosci. Bioeng. 2009;107:177–182. doi: 10.1016/j.jbiosc.2008.09.020. [DOI] [PubMed] [Google Scholar]
- 127.McMahon L., Reid A., Campbell V., Prendergast P. Regulatory effects of mechanical strain on the chondrogenic differentiation of MSCs in a collagen-GAG scaffold: Experimental and computational analysis. Ann. Biomed. Eng. 2008;36:185–194. doi: 10.1007/s10439-007-9416-5. [DOI] [PubMed] [Google Scholar]
- 128.Chen Y.-L., Lee H.-P., Chan H.-Y., Sung L.-Y., Chen H.-C., Hu Y.-C. Composite chondroitin-6-sulfate/dermatan sulfate/chitosan scaffolds for cartilage tissue engineering. Biomaterials. 2007;28:2294–2305. doi: 10.1016/j.biomaterials.2007.01.027. [DOI] [PubMed] [Google Scholar]
- 129.Chou C.-H., Cheng W.T.K., Kuo T.-F., Sun J.-S., Lin F.-H., Tsai J.-C. Fibrin glue mixed with gelatin/hyaluronic acid/chondroitin-6-sulfate tri-copolymer for articular cartilage tissue engineering: The results of real-time polymerase chain reaction. J. Biomed. Mater. Res. A. 2007;82:757–767. doi: 10.1002/jbm.a.31186. [DOI] [PubMed] [Google Scholar]
- 130.Muzzarelli R.A.A. Chitins and chitosans for the repair of wounded skin, nerve, cartilage and bone. Carbohydr. Polym. 2009;76:167–182. doi: 10.1016/j.carbpol.2008.11.002. [DOI] [Google Scholar]
- 131.Muzzarelli R.A.A. Nanochitins and nanochitosans, paving the way to eco-friendly and energy-saving exploitation of marine resources. In: Matyjaszewski K., Moller M., editors. Polymer Science: A Comprehensive Reference. Elsevier BV: Amsterdam; The Netherlands: 2012. pp. 153–164. [Google Scholar]
- 132.Hashemi Doulabi A., Mirzadeh H., Imani M., Samadi N. Chitosan/Polyethylene glycol fumarate blend film: Physical and antibacterial properties. Carbohydr. Polym. 2013;92:48–56. doi: 10.1016/j.carbpol.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 133.Oprenyeszk F., Chausson M., Maquet V., Dubuc J.E., Henrotin Y. Protective effect of a new biomaterial against the development of experimental osteoarthritis lesions in rabbit: A pilot study evaluating the intra-articular injection of alginate-chitosan beads dispersed in an hydrogel. Osteoarthr. Cartil. 2013;21:1099–1107. doi: 10.1016/j.joca.2013.04.017. [DOI] [PubMed] [Google Scholar]
- 134.Yan J., Li X., Liu L., Wang F., Zhu T.W., Zhang Q. Potential use of collagen-chitosan-hyaluronan tri-copolymer scaffold for cartilage tissue engineering. Artif. Cells Blood Substit. Biotecnol. 2006;34:27–39. doi: 10.1080/10731190500430024. [DOI] [PubMed] [Google Scholar]
- 135.Li Z., Zhang M. Chitosan-alginate as scaffolding material for cartilage tissue engineering. J. Biomed. Mater. Res. A. 2005;75:485–493. doi: 10.1002/jbm.a.30449. [DOI] [PubMed] [Google Scholar]
- 136.Häuselmann H.J., Aydelotte M.B., Schumacher B.L., Kuettner K.E., Gitelis S.H., Thonar E.J.M.A. Synthesis and turnover of proteoglycans by human and bovine adult articular chondrocytes cultured in alginate beads. Matrix. 1992;12:116–129. doi: 10.1016/S0934-8832(11)80053-3. [DOI] [PubMed] [Google Scholar]
- 137.Jung Y., Kim S.H., Kim S.-H., Kim Y.H., Xie J., Matsuda T., Min B.G. Cartilaginous tissue formation using a mechano-active scaffold and dynamic compressive stimulation. J. Biomater. Sci. Polym. Ed. 2008;19:61–74. doi: 10.1163/156856208783227712. [DOI] [PubMed] [Google Scholar]
- 138.Yang Z., Wu Y., Li C., Zhang T., Zou Y., Hui J.H., Ge Z., Lee E.H. Improved mesenchymal stem cells attachment and in vitro cartilage tissue formation on chitosan-modified poly(l-lactide-co-epsilon-caprolactone) scaffold. Tissue Eng. A. 2012;18:242–251. doi: 10.1089/ten.tea.2011.0315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Baker M.I., Walsh S.P., Schwartz Z., Boyan B.D. A review of polyvinyl alcohol and its uses in cartilage and orthopedic applications. J. Biomed. Mater. Res. B. 2012;100:1451–1457. doi: 10.1002/jbm.b.32694. [DOI] [PubMed] [Google Scholar]
- 140.Cho S.H., Lim S.M., Han D.K., Yuk S.H., Im G.I., Lee J.H. Time-dependent alginate/polyvinyl alcohol hydrogels as injectable cell carriers. J. Biomater. Sci. Polym. Ed. 2009;20:863–876. doi: 10.1163/156856209X444312. [DOI] [PubMed] [Google Scholar]
- 141.Cai C., Chen C., Chen G., Wang F., Guo L., Yin L., Feng D., Yang L. Type I collagen and polyvinyl alcohol blend fiber scaffold for anterior cruciate ligament reconstruction. Biomed. Mater. 2013;8 doi: 10.1088/1748-6041/8/3/035001. [DOI] [PubMed] [Google Scholar]
- 142.Gough J.E., Scotchford C.A., Downes S. Cytotoxicity of glutaraldehyde crosslinked collagen/poly(vinyl alcohol) films is by the mechanism of apoptosis. J. Biomed. Mater. Res. 2002;61:121–130. doi: 10.1002/jbm.10145. [DOI] [PubMed] [Google Scholar]
- 143.Bray J.C., Merrill E.W. Poly(vinyl alcohol) hydrogels for synthetic articular cartilage material. J. Biomed. Mater. Res. 1973;7:431–443. doi: 10.1002/jbm.820070506. [DOI] [PubMed] [Google Scholar]
- 144.Mohan N., Nair P.D. Polyvinyl alcohol-poly(caprolactone) semi IPN scaffold with implication for cartilage tissue engineering. J. Biomed. Mater. Res. B. 2008;84:584–594. doi: 10.1002/jbm.b.30906. [DOI] [PubMed] [Google Scholar]
- 145.Mohan N., Nair P.D., Tabata Y. Growth factor-mediated effects on chondrogenic differentiation of mesenchymal stem cells in 3D semi-IPN poly(vinyl alcohol)-poly(caprolactone) scaffolds. J. Biomed. Mater. Res. A. 2010;94:146–159. doi: 10.1002/jbm.a.32680. [DOI] [PubMed] [Google Scholar]
- 146.Lee S.-Y., Pereira B.P., Yusof N., Selvaratnam L., Yu Z., Abbas A.A., Kamarul T. Unconfined compression properties of a porous poly(vinyl alcohol)-chitosan-based hydrogel after hydration. Acta Biomater. 2009;5:1919–1925. doi: 10.1016/j.actbio.2009.02.014. [DOI] [PubMed] [Google Scholar]
- 147.Ibrahim N.S., Krishnamurithy G., Rao Balaji Raghavendran H., Puvaneswary S., Wuey Min N., Kamarul T. Novel HA-PVA/NOCC bilayered scaffold for osteochondral tissue-engineering applications—Fabrication, characterization, in vitro and in vivo biocompatibility study. Mater. Lett. 2013;113:25–29. doi: 10.1016/j.matlet.2013.09.026. [DOI] [Google Scholar]
- 148.Ahn E.S., Gleason N.J., Nakahira A., Ying J.Y. Nanostructure processing of hydroxyapatite-based bioceramics. Nano Lett. 2001;1:149–153. doi: 10.1021/nl0055299. [DOI] [Google Scholar]
- 149.Sardinha V.M., Lima L.L., Belangero W.D., Zavaglia C.A., Bavaresco V.P., Gomes J.R. Tribological characterization of polyvinyl alcohol hydrogel as substitute of articular cartilage. Wear. 2013;301:218–225. doi: 10.1016/j.wear.2012.11.054. [DOI] [Google Scholar]
- 150.Ma R., Xiong D., Miao F., Zhang J., Peng Y. Novel PVP/PVA hydrogels for articular cartilage replacement. Mater. Sci. Eng. C. 2009;29:1979–1983. doi: 10.1016/j.msec.2009.03.010. [DOI] [Google Scholar]
- 151.Ma R., Xiong D., Miao F., Zhang J., Peng Y. Friction properties of novel PVP/PVA blend hydrogels as artificial cartilage. J. Biomed. Mater. Res. A. 2010;93:1016–1019. doi: 10.1002/jbm.a.32552. [DOI] [PubMed] [Google Scholar]
- 152.Scholten P.M., Ng K.W., Joh K., Serino L.P., Warren R.F., Torzilli P.A., Maher S.A. A semi-degradable composite scaffold for articular cartilage defects. J. Biomed. Mater. Res. A. 2011;97:8–15. doi: 10.1002/jbm.a.33005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Bichara D.A., Zhao X., Hwang N.S., Bodugoz-Senturk H., Yaremchuk M.J., Randolph M.A., Muratoqlu O.K. Porous poly (vinyl alcohol)-alginate gel hybrid construct for neocartilage formation using human nasoseptal cells. J. Surg. Res. 2010;163:331–336. doi: 10.1016/j.jss.2010.03.070. [DOI] [PubMed] [Google Scholar]
- 154.Engel E., Michiardi A., Navarro M., Lacroix D., Planell J.A. Nanotechnology in regenerative medicine: The materials side. Trends Biotechnol. 2008;26:39–47. doi: 10.1016/j.tibtech.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 155.Zhang L., Webster T.J. Nanotechnology and nanomaterials: Promises for improved tissue regeneration. Nano Today. 2009;4:66–80. doi: 10.1016/j.nantod.2008.10.014. [DOI] [Google Scholar]
- 156.Coburn J.M., Gibson M., Monagle S., Patterson Z., Elisseeff J.H. Bioinspired nanofibers support chondrogenesis for articular cartilage repair. Proc. Natl. Acad. Sci. USA. 2012;109:10012–10017. doi: 10.1073/pnas.1121605109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Wise J.K., Yarin A.L., Megaridis C.M., Cho M. Chondrogenic differentiation of human mesenchymal stem cells on oriented nanofibrous scaffolds: Engineering the superficial zone of articular cartilage. Tissue Eng. A. 2009;15:913–921. doi: 10.1089/ten.tea.2008.0109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Shin H.J., Lee C.H., Cho I.H., Kim Y.-J., Lee Y.-J., Kim I.A., Park K.-D., Yui N., Shin J.-W. Electrospun PLGA nanofiber scaffolds for articular cartilage reconstruction: Mechanical stability, degradation and cellular responses under mechanical stimulation in vitro. J. Biomater. Sci. Polym. Ed. 2006;17:103–119. doi: 10.1163/156856206774879126. [DOI] [PubMed] [Google Scholar]
- 159.Shirosaki Y., Okayama T., Tsuru K., Hayakawa S., Osaka A. Synthesis and cytocompatibility of porous chitosan-silicate hybrids for tissue engineering scaffold application. Chem. Eng. J. 2008;137:122–128. doi: 10.1016/j.cej.2007.10.012. [DOI] [Google Scholar]
- 160.Buchtová N., Réthoré G., Boyer C., Guicheux J., Rambaud F., Vallé K., Belleville P., Sanchez C., Chauvet O., Weiss P., et al. Nanocomposite hydrogels for cartilage tissue engineering: Mesoporous silica nanofibers interlinked with siloxane derived polysaccharide. J. Mater. Sci. Mater. Med. 2013;24:1875–1884. doi: 10.1007/s10856-013-4951-0. [DOI] [PubMed] [Google Scholar]
- 161.Bhattarai N., Gunn J., Zhang M. Chitosan-based hydrogels for controlled, localized drug delivery. Adv. Drug Deliv. Rev. 2010;62:83–99. doi: 10.1016/j.addr.2009.07.019. [DOI] [PubMed] [Google Scholar]
- 162.Lin L., Chow K.L., Leng Y. Study of hydroxyapatite osteoinductivity with an osteogenic differentiation of mesenchymal stem cells. J. Biomed. Mater. Res. A. 2009;89:326–335. doi: 10.1002/jbm.a.31994. [DOI] [PubMed] [Google Scholar]
- 163.Ducheyne P., Qiu Q. Bioactive ceramics: The effect of surface reactivity on bone formation and bone cell function. Biomaterials. 1999;20:2287–2303. doi: 10.1016/S0142-9612(99)00181-7. [DOI] [PubMed] [Google Scholar]
- 164.Kuo Y.-C., Leou S.-N. Chondrogenesis of articular chondrocytes in hydroxyapatite/chitin/chitosan scaffolds supplemented with pituitary extract. Eng. Life Sci. 2010;10:65–74. doi: 10.1002/elsc.200900048. [DOI] [Google Scholar]
- 165.Spadaccio C., Rainer A., Trombetta M., Vadalá G., Chello M., Covino E., Denaro V., Toyoda Y., Genovese J.A. Poly-l-Lactic acid/Hydroxyapatite electrospun nanocomposites induce chondrogenic differentiation of human MSC. Ann. Biomed. Eng. 2009;37:1376–1389. doi: 10.1007/s10439-009-9704-3. [DOI] [PubMed] [Google Scholar]
- 166.Pan Y., Xiong D., Chen X. Mechanical properties of nanohydroxyapatite reinforced poly(vinyl alcohol) gel composites as biomaterial. J. Mater. Sci. 2007;42:5129–5134. doi: 10.1007/s10853-006-1264-4. [DOI] [PubMed] [Google Scholar]
- 167.Oliveira J.M., Rodrigues M.T., Silva S.S., Malafaya P.B., Gomes M.E., Viegas C.A., Dias I.R., Azevedo J.T., Mano J.F., Reis R.L. Novel hydroxyapatite/chitosan bilayered scaffold for osteochondral tissue-engineering applications: Scaffold design and its performance when seeded with goat bone marrow stromal cells. Biomaterials. 2006;27:6123–6137. doi: 10.1016/j.biomaterials.2006.07.034. [DOI] [PubMed] [Google Scholar]
- 168.O’Shea T.M., Miao X. Bilayered scaffolds for osteochondral tissue engineering. Tissue Eng. B Rev. 2008;14:447–464. doi: 10.1089/ten.teb.2008.0327. [DOI] [PubMed] [Google Scholar]
- 169.Qu D., Li J., Li Y., Khadka A., Zuo Y., Wang H., Liu Y., Cheng L. Ectopic osteochondral formation of biomimetic porous PVA-n-HA/PA6 bilayered scaffold and BMSCs construct in rabbit. J. Biomed. Mater. Res. B. 2011;96:9–15. doi: 10.1002/jbm.b.31697. [DOI] [PubMed] [Google Scholar]
- 170.Wang X., Grogan S.P., Rieser F., Winkelmann V., Maquet V., Berge M.L., Mainil-Varlet P. Tissue engineering of biphasic cartilage constructs using various biodegradable scaffolds: An in vitro study. Biomaterials. 2004;25:3681–3688. doi: 10.1016/j.biomaterials.2003.10.102. [DOI] [PubMed] [Google Scholar]
- 171.Shi H.-C., Lu D., Wang W.-P., Lu Y., Zeng Y.-J. N-carboxyethylchitosan/nanohydroxyapatite composites scaffold for tracheal cartilage tissue-engineering applications. Micro Nano Lett. 2012;7:76–79. doi: 10.1049/mnl.2011.0628. [DOI] [Google Scholar]
- 172.Gu Z.-Q., Xiao J.-M., Zhang X.-H. The development of artificial articular cartilage-PVA-hydrogel. Biomed. Mater. Eng. 1998;8:75–81. [PubMed] [Google Scholar]
- 173.Maiolo A.S., Amado M.N., Gonzalez J.S., Alvarez V.A. Development and characterization of poly (vinyl alcohol) based hydrogels for potential use as an articular cartilage replacement. Mater. Sci. Eng. C. 2012;32:1490–1495. doi: 10.1016/j.msec.2012.04.030. [DOI] [PubMed] [Google Scholar]
- 174.Pan Y., Xiong D. Stress relaxation behavior of nano-hydroxyapatite reinforced poly(vinyl alcohol) gel composites as biomaterial. J. Mater. Sci. 2010;45:5495–5501. doi: 10.1007/s10853-010-4607-0. [DOI] [Google Scholar]
- 175.Pan Y., Xiong D. Friction properties of nano-hydroxyapatite reinforced poly(vinyl alcohol) gel composites as an articular cartilage. Wear. 2009;266:699–703. doi: 10.1016/j.wear.2008.08.012. [DOI] [Google Scholar]
- 176.Pan Y., Xiong D., Gao F. Viscoelastic behavior of nano-hydroxyapatite reinforced poly(vinyl alcohol) gel biocomposites as an articular cartilage. J. Mater. Sci. Mater. Med. 2008;19:1963–1969. doi: 10.1007/s10856-007-3280-6. [DOI] [PubMed] [Google Scholar]
- 177.Zhang L., Hu J., Athanasiou K.A. The role of tissue engineering in articular cartilage repair and regeneration. Crit. Rev. Biomed. Eng. 2009;37:1–57. doi: 10.1615/CritRevBiomedEng.v37.i1-2.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Ikada Y., Tsuji H. Biodegradable polyesters for medical and ecological applications. Macromol. Rapid Commun. 2000;21:117–132. doi: 10.1002/(SICI)1521-3927(20000201)21:3<117::AID-MARC117>3.0.CO;2-X. [DOI] [Google Scholar]