Abstract
Many countries have implemented nonmedical prescribing (NMP) and many others are scoping prescribing practices with a view to developing NMP. This paper provides a future perspective on NMP in light of findings of an umbrella review of aspects of NMP. This is followed by coverage of the Scottish Government strategy of pharmacist prescribing and finally, consideration of two key challenges. The review identified seven systematic reviews of influences on prescribing decision-making, processes of prescribing, and barriers and facilitators to implementation. Decision making was reported as complex with many, and often conflicting, influences. Facilitators of NMP included perceived improved patient care and professional autonomy, while barriers included lack of defined roles and resource pressures. Three systematic reviews explored patient outcomes that were noted to be equivalent or better to physician prescribing. In particular, a Cochrane review of 46 studies of clinical, patient-reported, and resource-use outcomes of NMP compared with medical prescribing showed positive intervention-group effects. Despite positive findings, authors highlighted high bias, poor definition and description of ‘prescribing’ and the ‘prescribing process’ and difficulty in separating NMP effects from the contributions of other healthcare team members. While evidence of benefit and safety is essential to inform practice, for NMP to be implemented and sustained on a large scale, there needs to be clear commitment at the highest level. The approach being taken by the Scottish Government to pharmacist prescribing implementation may inform developments in other professions and countries. The vision is that by 2023, all pharmacists providing pharmaceutical care will be pharmacist-independent prescribers. There are, however, challenges to implementing NMP into working practice; two key challenges are the need for sustainable models of care and evaluation research. These challenges could be met by considering the theoretical basis for implementation, and robust and rigorous evaluation.
Keywords: Nonmedical prescribing, Umbrella review, Systematic review, Evaluation research, Theory
Nonmedical prescribing models
The roles and responsibilities of all health professionals have undergone tremendous transformation in recent years. One key development has been the implementation of prescribing by nonmedical health professionals across many countries including Australia, Ireland, New Zealand, the United Kingdom (UK) and the United States (US).1 Many other countries are scoping current prescribing practices with a view to developing nonmedical prescribing (NMP) models. A range of health professionals (e.g. dieticians, nurses, pharmacists, physiotherapists, radiographers) now have prescribing rights. The specific professions, their training and accreditation, and models of prescribing practice vary in different countries. Specific aims of NMP vary from country to country but are focused generally on: improving patient care outcomes without compromising patient safety; increasing patient access to medicines; and making better use of the skills of health professionals.1,2
For example, in the UK, there are two models of NMP: supplementary prescribing (SP) and independent prescribing (IP). SP, introduced in 2003, is defined as a ‘voluntary partnership between an independent prescriber (doctor or dentist) and a supplementary prescriber to implement an agreed patient-specific clinical management plan (CMP) with the patient’s agreement’.3 A later development was the introduction in 2006 of IP, defined as ‘prescribing by a practitioner (e.g. doctor, dentist, nurse, pharmacist) responsible and accountable for the assessment of patients with undiagnosed or diagnosed conditions and for decisions about the clinical management required, including prescribing’.4 Qualification as an independent prescriber now also confers SP status. The similarities and differences between SP and IP are summarized in Table 1.
Table 1.
Scope of different models of nonmedical prescribing in the UK. Adapted from Stewart et al.1
| SP | IP | |
|---|---|---|
| Eligible health professionals | Dieticians, nurses, optometrists, pharmacists, physiotherapists, podiatrists, radiographers | Nurses, optometrists, pharmacists, physiotherapists, podiatrists, therapeutic radiographers |
| Clinical conditions managed | Any, within their clinical competence | Any, within their clinical competence |
| Diagnosis responsibilities | A doctor (or dentist) must diagnose the condition before prescribing can commence | The independent prescriber can assess and manage patients with diagnosed or undiagnosed conditions |
| Need for CMP | A written or electronic patient-specific CMP must be in place before prescribing can commence | No need for a CMP |
| Need for formal agreement | The CMP must be agreed with the doctor (or dentist) and patient before prescribing can commence | No need for any formal agreement |
| Drugs prescribed | Any, within their clinical competence | Any licensed medicines within their clinical competence. Nurse- and pharmacist-independent prescribers in particular can prescribe unlicensed medicines and controlled drugs |
SP, supplementary prescribing; IP, independent prescribing; CMP, clinical management plan.
In a recent paper in this journal, Cope and colleagues described the development of NMP, the processes required to qualify in the UK and the potential influences on NMP practice.2 In the remainder of this paper, we consider the complexities of prescribing in general and in relation to NMP, followed by an umbrella review of all published systematic literature reviews on aspects of NMP, detailed coverage of the policy driven Scottish Government strategy relating to pharmacist prescribing and reflect on the future of NMP in light of accumulated evidence.
Complexities of prescribing
The 10 principles of good prescribing, articulated by the British Pharmacological Society, underline that prescribing is a complex and challenging task requiring considerable knowledge, skills and self-belief in capabilities (Box 1).
Box 1. Ten principles of good prescribing, British Pharmacological Society.5.
Be clear about the reasons for prescribing
Take into account the patient’s medication history before prescribing
Take into account other factors that might alter the benefits and risks of treatment
Take into account the patient’s ideas, concerns and expectations
Select effective, safe, and cost-effective medicines individualized for the patient
Adhere to national guidelines and local formularies where appropriate
Write unambiguous legal prescriptions using the correct documentation
Monitor the beneficial and adverse effects of medicines
Communicate and document prescribing decisions and the reasons for them
Prescribe within the limits of your knowledge, skills and experience
These principles apply to all prescribers, and should be borne in mind as new professional groupings are afforded prescribing rights. Point 10 is especially pertinent for newly qualified nonmedical prescribers who, despite being experienced practitioners, are inexperienced prescribers and must be prepared to seek the advice and support of their professional colleagues.
Given the evidence base demonstrating widespread suboptimal prescribing by doctors, there is great potential for nonmedical prescribers to impact positively patient care and safety. Ross and colleagues reported a systematic review of prescribing errors by junior doctors, with error prevalence rates of between 2 and 514 per 1000 items prescribed and in 4–82% of patients or charts reviewed.6 Similarly, a systematic review by Lewis and colleagues of all prescribing errors in hospital inpatients reported median error prevalence data of 7% (interquartile range 2–14%) of medication orders, 52 (8–227) errors per 100 admissions and 24 (6–212) errors per 1000 patient days.7 As nonmedical prescribers must have several years’ experience of interacting with patients prior to commencing their prescribing training, it could be hypothesized that this experience, together with specific prescribing training and assessment of competence, will translate into safer, more appropriate prescribing. To date, however, there has been little published research on NMP error rates. In one small study conducted in three hospitals in England, pharmacists prescribing of 1415 items revealed errors in only four items (0.3%).8 While this appears to be positive, there is a need for further largescale research to confirm safety and appropriateness of all NMP.
One future development in the preparation of all prescribers (medical and nonmedical) may be harmonization of training, assessment, registration and regulation processes. Indeed, the National Prescribing Centre (now part of the National Institute for Health and Clinical Excellence for England and Wales) has produced a single competency framework for all prescribers.9 The framework comprises 72 competency statements, organized into nine themed areas of knowledge, options, shared decision making, safe, professional, always improving, the healthcare system, information, self and others, in three overarching domains of the consultation, prescribing effectively and prescribing in context. It is anticipated that, if acquired and maintained, these competencies will help all prescribers become and remain effective and safe in their area of practice.
Nonmedical prescribers’ training, achieving these competencies and ongoing continuing professional development may lead to safe and effective prescribing. There remains, however, a need for robust and rigorous evidence of NMP safety and effectiveness on which to base future developments. While there are multiple published literature reviews exploring different aspects of NMP, to date there has been no comprehensive overview. Such a review would summarize the evidence from multiple-research syntheses and provide an assessment of the body of evidence to further inform developments.
Reviews of nonmedical prescribing
Aim
Umbrella reviews provide synthesis of the findings of systematic reviews.10 Conducting such a review involves examining the quality of the included systematic review but does not require repeating the searches, assessment of study eligibility or quality assessment of the included reviews. The focus is on providing an overall picture of findings for the particular umbrella review aim. The aim of this umbrella review was to collate and summarize all the published systematic reviews on NMP in order to report aspects, including, but not limited to: models and definitions; legal frameworks; outcomes and benefits; perceptions and satisfaction of different stakeholders (e.g. general public, patients, health professionals and decision makers); and facilitators and barriers to implementing NMP. The search was conducted between March and November 2016.
Methods
Search strategy
Systematic reviews meeting the above criteria and published in English were included in the review. The following electronic bibliographic databases were searched: Medline, Cumulative Index of Nursing and Allied Health Literature, Science Direct, International Pharmaceutical Abstracts and Google Scholar. The Cochrane Library, the Centre for Reviews and Dissemination (Prospero) and Joanna Briggs Institute databases were also searched to identify any registered systematic review protocols. The reference lists of the retrieved reviews were examined to locate any further reviews.
The search strategy included only terms relating to or describing NMP, with no limits placed on the search. Alerts were created to check for further reviews for inclusion while conducting the review. An example of the search for Medline is given in Box 2.
Box 2. Medline search string.
(“non-medical prescrib*” OR “non medical prescrib*” OR NMP OR “pharmac* prescrib*” OR “nurse* prescrib*” OR “midwi* prescrib*” OR “podiatrist* prescrib*” OR “chiropodist* prescrib*” OR “optometrist* prescrib*” OR “orthoptist* prescrib*” OR “optician* prescrib*” OR “physiotherapist* prescrib*” OR “physical therapist* prescrib*” OR “dieti* prescrib*” OR “occupational therapist* prescrib*” OR “paramedic* prescrib*” OR “radiographer* prescrib*” OR “respiratory therapist* prescrib*” OR “audiologist* prescrib*”) AND (review)
Title, abstract and full text screening and assessment for inclusion was conducted by one of the reviewers (TJ), with another (DS) reviewing independently a 10% random sample to ensure sensitivity (comprehensiveness of search) and specificity (precision and relevance of reviews retrieved). Any disagreements were resolved through discussion without having to consult a third reviewer.
Quality assessment
The quality of systematic reviews that met the inclusion criteria was assessed using the Critical Appraisal Skills Programme (CASP) tool.11 Quality assessment was conducted independently by two reviewers (TJ and DS or KM or SC or AA or ARP) and disagreements resolved through discussion without having to consult a third reviewer.
Data extraction
The characteristics of the included reviews were extracted and summarized in tables. Data extracted were: authors; year of publication; country/countries of focus; type of review; objectives; NMP definition; databases searched; number of articles; and major findings. As with the quality assessment, data extraction was undertaken independently by two reviewers.
Data synthesis
Due to heterogeneity of reviews in terms of objectives and data, a narrative synthesis was most appropriate.
Results
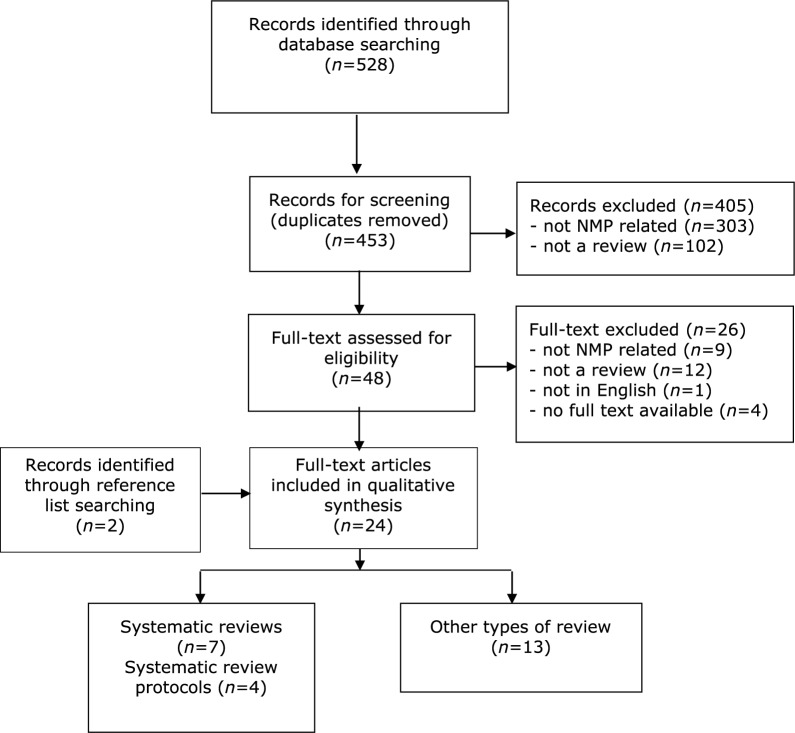
Searching identified 528 studies, which was reduced to 453 after removing duplicates. A total of 405 were excluded on review of titles and abstracts (no search strategy included or not related to NMP) leaving 48, with two more identified from reference lists, making 50. Full-text screening excluded a further 26 (reasons as before). Of the remaining 24, there were 13 nonsystematic reviews, four were protocols, leaving seven systematic reviews for quality assessment, data extraction and synthesis. The PRISMA flow chart is provided in Figure 1.
Figure 1.
PRISMA flow chart detailing the inclusion process.
NMP, nonmedical prescribing.
Quality assessment
The quality assessment of the seven systematic reviews is given in Table 2. Most were deemed of high quality, although one would have benefited from searching country-specific databases and lacked quality assessment,12 and qualitative findings could have been subjected to meta-synthesis in another.13
Table 2.
Quality assessment of the seven systematic reviews.11
| Authors | Are the results of the review valid? |
What are the results? |
Will the results help locally? |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Review addressed a clearly focused issue | Search relevant | Important and relevant studies included | Rigorous assessment of quality of included studies | Reasonable to combine results of review | Overall results of review | Precision of results appropriate | Applicable to local population | All important outcomes considered | |
| Van Ruth et al.14 | Yes | Yes | Yes | Yes | Yes, pooled if homogenous (for one review question) but noted high risk of bias in some studies | Very clear presentation of results according to aim | Yes (pooled data) | N/A | Yes |
| Kroezen et al.12 | Yes | Partially (peer reviewed literature less appropriate for some questions, e.g. extent of legal, educational conditions) | Partially | No explicit coverage of quality assessment | N/A as no meta-analysis or meta-synthesis | Very clear presentation of results according to aim | N/A as no pooling | N/A | Yes |
| Gielen et al.15 | Yes | Yes | Yes | Yes | Yes, pooled if homogenous but noted high risk of bias in some studies | Very clear presentation of results according to aim | Yes (pooled data) | N/A | Yes |
| Darvishpour et al.16 | Yes | Yes | Yes | Yes | Yes, qualitative meta-synthesis | Very clear presentation of results according to aim | N/A for meta-synthesis | N/A | Yes |
| McIntosh et al.17 | Yes | Yes | Yes | Yes | Yes, qualitative meta-synthesis | Very clear presentation of results according to aim | N/A for meta-synthesis | N/A | Yes |
| Ness et al.13 | Yes | Yes | Yes | Yes | No meta-synthesis of qualitative studies given | Very clear presentation of results according to aim | N/A for meta-synthesis (although not conducted) | N/A | Yes |
| Weeks et al.18 | Yes | Yes | Yes | Yes | Yes, pooled if homogenous but noted high risk of bias in some studies | Very clear presentation of results according to aim | Yes (pooled data) | N/A | Yes |
N/A, not applicable.
Data extraction
The data extraction is given in Table 3. Five focused solely on nurse prescribing,12–16 with two discussing all nonmedical prescribers.17,18 While five included all studies irrespective of country or setting,13–16,18 one included only those conducted in Western European and Anglo-Saxon countries,12 and one was restricted to the UK.17 The number of studies reviewed ranged from 3 to 124. Two reviews focused on aspects of influences on prescribing decision making generally17 and prescribing behaviour related to antimicrobials.13 One reported the extent of implementation of nurse prescribing,12 one processes of prescribing and associated barriers and facilitators to implementation,16 with three on various patient outcome measures.14,15,18
Table 3.
Data extraction of seven systematic reviews.
| Authors | Aims/ objective(s) | Country | NMP | Databases searched and search terms used | Number of articles | Findings |
|---|---|---|---|---|---|---|
| Van Ruth et al.14 | Aimed to review the effects of medication being prescribed by nurses The following research questions were addressed: what are the effects of nurse prescribing compared with physician prescribing, on the quantity and types of medication being prescribed? What are the effects of nurse prescribing on patient outcomes? What are the effects of nurse prescribing on physician and nurse outcomes? What are the effects of nurse prescribing on characteristics of the health care system? |
Review of all studies, irrespective of country | Nurse prescribing | Pubmed, Embase, CINAHL, Cochrane Library, Picarta, SCI, Invert, Biomed central, Virginia Henderson Library, Current Control Trials, NIVEL catalog, UK Department of Health, World Health Organization, Nurse Prescriber website, Google For PubMed, the following search terms were used: (‘Nurse prescribing’) OR (Nurs* [tiab] AND Prescri* [tiab]) OR (Nurs* AND prescriptions, drug [MeSH]) |
23 | Nurses sometimes differed from physicians in the number of patients they prescribe for and in the choice or type of medication Clinical parameters were the same or better for treatment by nurses compared with physicians across a range of conditions (diabetes and ‘various’) Perceived quality of care by nurses was similar or better The effects on professionals or on the health care system could not be described |
| Kroezen et al.12 | Aimed to gain insight into the scientific and professional literature describing the extent to and the ways in which nurse prescribing has been realized or is being introduced in Western European and Anglo-Saxon countries Secondly, to identify possible mechanisms underlying the introduction and organization of nurse prescribing on the basis of Abbott’s theory on the division of professional labour |
Western European and Anglo-Saxon countries | Nurse prescribing | PubMed, Embase, CINAHL, Web of Science, EBSCO, NIVEL, Virginia Henderson International Nursing Library, World Health Organization website, Health professionals’ website, Google scholar. The following keywords were used: ‘nurse prescribing’, ‘independent (nurse) prescribing’, ‘autonomous prescribing’, ‘supplementary (nurse) prescribing’, ‘dependent (nurse) prescribing’, ‘collaborative prescribing’, ‘group protocols’, ‘patient group directions’, ‘time and dose prescribing’, ‘nurse formulary’ |
124 | Seven countries had implemented nurse prescribing of medicines The Netherlands and Spain were in the process of introducing nurse prescribing A diversity of external and internal forces had led to the introduction of nurse prescribing internationally The legal, educational and organizational conditions under which nurses prescribe medicines varied considerably between countries; from situations where nurses prescribed independently to situations in which prescribing by nurses was only allowed under strict conditions and supervision of physicians |
| Darvishpour et al.16 | Aimed to obtain new insights on nurse prescribing drugs, and to present a schematic model of nurse prescribing that could be a useful framework for its implementation The following research questions were addressed: what is the overall view on nurse prescribing? What are the positive and negative outcomes of nurse prescribing?What are the barriers and facilitators for its implementation? |
Review of all studies, irrespective of country | Nurse prescribing | Integrated Digital National Library of Medicine, CINAHL, Medline, Cochrane Library, Scopus, Web of science, Elsevier, Emelard, JAMA journals, Wiley, Oxford journals, Springer and Thieme journals, World Health Organization website, Nurse prescriber website, Google scholar, Cambridge journals website The following were used: review AND nurs* prescri* |
11 | Studies revealed eight themes, namely: leading countries in prescribing, views, features, infrastructures, benefits, disadvantages, facilitators and barriers of nursing prescribing Despite the positive view on nurse prescribing, there were still issues such as legal, administrative, weak research and educational deficiencies in academic preparation of nurses |
| Gielen et al.15 | Aimed to identify, appraise and synthesize the evidence presented in the literature on the effectiveness of nurse prescribing compared with physician prescribing The following research questions were addressed: what are the effects of nurse prescribing on the quantity and types of medication being prescribed? What are the effects of nurse prescribing on patient outcomes? |
Review of all studies, irrespective of country | Nurse prescribing | BioMed Central, CINAHL, Cochrane Database of Systematic Reviews, Current Controlled Trials, Embase, INVERT (Dutch nursing literature index), NIVEL catalogue, PiCarta (Dutch library system), PubMed, Science Citation Index and the Virginia Henderson International Nursing Library, and the website of the UK Department of Health, the website of the World Health Organization, a website for health professionals and Google Scholar For Pubmed: (‘Nurse prescribing’) OR (Nurs* [tiab] AND Prescri* [tiab]) OR (Nurs* AND prescriptions, drug [MeSH]) |
35 | Nurses prescribed in comparable ways with physicians They prescribed for equal numbers of patients and prescribe comparable types and doses of medicines Studies comparing the total amount of medication prescribed by nurses and doctors show mixed results. There appeared to be few differences between nurses and physicians in patient health outcomes: clinical parameters were the same or better for treatment by nurses, perceived quality of care was similar or better and patients treated by nurses were just as satisfied or more satisfied |
| McIntosh et al.17 | To critically appraise, synthesize and present evidence on the influences on prescribing decision making among supplementary and independent nonmedical prescribers in the UK | UK | All nonmedical prescribers | Medline, PsycARTICLES, CINAHL, International Pharmaceutical Abstracts, Education Resources Information Centre, Cochrane Library, Google Scholar, reference lists The following search terms were used: prescrib* and (pharmacist* or nurse* or physiotherapist* or podiatrist* or radiographer* or optometrist*) and (influenc* or decision* or decid* or judge* or factor*) |
3 | While all studies reported aspects of prescribing decision making, this was not the primary research aim for any. Studies were carried out in primary care almost exclusively among nurse prescribers (n = 67). Complex influences were evident, such as experience in the role, the use of evidence-based guidelines and peer support and encouragement from doctors; these helped participants to feel more knowledgeable and confident about their prescribing decisions. Opposing influences included prioritization of experience and concern about complications over evidence base, and peer conflict |
| Ness et al.13 | To present the findings of a systematic review that explored the influences on the antimicrobial prescribing behaviour of independent nurse prescribers | Review of all studies, irrespective of country | Independent nurse prescribing | Medline, CINAHL, AMED, HealthSource Nursing/Academic Edition, Proquest Health, Internurse, Cochrane Database, Web of Knowledge, Index to Thesis, ETHOS, reference lists Search terms included: Prescri* AND Antibiotic OR antimicrobial OR antibacterial AND Nurs* |
7 | Three articles expected that an antimicrobial would be given and therefore influences discussed were on the choice of the antimicrobial. Guidelines/protocols, safety, tolerability and efficacy of the antimicrobial itself, patient/parent pressure and training/experience were mentioned as influencing factors within the reported studies The other four studies explored influences on whether to prescribe. An antimicrobial or not and also found that guidelines/protocols were an influencing factor; however, the influence occurring most frequently was diagnostic uncertainty. |
| Weeks et al.18 | To assess clinical, patient-reported, and resource-use outcomes of NMP for managing acute and chronic health conditions in primary and secondary care settings compared with medical prescribing (usual care) |
Review of all studies, irrespective of country | Healthcare providers who were not medical doctors, undertaking prescribing including, nurses, optometrist, pharmacists, physician assistants, and other allied health professionals or categories not specifically mentioned whose roles met the definition of nonmedical prescribing |
Cochrane Database, DARE, HTA, Medline, Embase, PsycINFO, CINAHL, grey literature, trial registries | 46 | A meta-analysis of surrogate markers of chronic disease (systolic blood pressure, glycated haemoglobin, and low-density lipoprotein) showed positive-intervention group effects. While there appeared little difference in medication adherence across studies, a meta-analysis of continuous outcome data from four studies showed an effect favouring patient adherence in the NMP group. Patients were generally satisfied with nonmedical prescriber care. |
CMP, clinical management plan; NMP, nonmedical prescribing.
Synthesis of findings
Decision making and prescribing behaviours were reported as complex with many, and often conflicting, influences.13,17 Of the three studies reviewed by McIntosh and colleagues,17 decision making was not the primary aim for any. Acknowledging the paucity of studies and limited evidence base, key influences on decision making included nonmedical prescribers’ experience, evidence-based guidelines and treatment protocols, peer support and encouragement from medical practitioners, and patients. Ness and colleagues13 reported similar influences on decision making in relation to antibiotic prescribing in the seven studies reviewed. Patient and parent pressure was noted as a key influence in both the decision to prescribe and which antibiotic to prescribe. These two systematic reviews have highlighted the need for further research on the decision-making processes, decisions and prescribing behaviours of nonmedical prescribers to inform NMP education, training and practice.
Facilitators of NMP included perceived improved patient care, professional autonomy and potential to apply expertise while barriers included lack of clearly defined roles of nonmedical prescribers, time for prescribing activities and other resource pressures, such as lack of funding to support prescribing roles, other competing tasks, lack of confidence of some NMPs, and the lack of acceptance of the role by other health professionals and patients.16 This review was a meta-synthesis of 11 qualitative studies. There would be merit in updating this review to incorporate qualitative, quantitative and mixed-methodology studies but with focus on how facilitators are enabled and barriers overcome. Findings would assist greatly the development and implementation of NMP in new settings and countries.
Three systematic reviews have now been published reporting data on patient outcomes.14,15,18 Despite the largely positive findings on a variety of outcome measures, the review authors all highlighted the absence of well-designed randomized controlled trials (RCTs) and high levels of bias associated with many of the studies included in their reviews that often resulted in the outcome findings being downgraded. In addition, the review authors noted the issue of often-poor definition and description of ‘prescribing’ and the ‘prescribing process’ within many studies, and the difficulty in separating NMP effects from the contributions of other members of the healthcare team. Review findings should therefore be interpreted with great caution. In 2007, Van Ruth and colleagues14 reported their review of 23 studies of nurse prescribing. Of the nine studies reporting clinical outcomes, there were no differences between nurses and GPs in terms of resolution of symptoms, health status rating, clinical improvement over 2 weeks. These studies included ‘various’ patients: those presenting acutely with sore throats, need for contraception and the chronic condition of diabetes mellitus, hence limiting the opportunity for data pooling. In 2014, Gielen and colleagues15 reported a systematic review of 35 studies of nurse prescribing. Of the 13 studies reporting clinical outcomes, there were no differences between nurse and physician prescribing in a variety of conditions including diabetes, hypertension, asthma, sore throat and contraception. The heterogeneity of patient populations and outcome measures limited the potential for any data pooling. Very recently, Weeks and colleagues18 reported a Cochrane review of 46 studies (26 nurse and 20 pharmacist prescribers) of clinical, patient-reported, and resource-use outcomes of NMP for managing acute and chronic health conditions in primary and secondary care settings compared with medical prescribing. A meta-analysis of outcome measures of chronic disease showed positive intervention group effects. There was a moderate certainty of evidence for studies of blood pressure at 12 months (12 studies, 4229 participants) and low-density lipoprotein (7 studies, 1469 participants). Patients were generally satisfied with nonmedical prescriber care (14 studies, 7514 participants). A wide variety of resource use measures were reported across studies with little difference between groups for hospitalizations, emergency department visits, and outpatient visits. The authors concluded that there remains a need for well designed, conducted and reported randomized controlled trials of NMP compared with medical prescribing. However, as NMP is implemented increasingly into practice, there may be less desire from policy makers, healthcare leaders and funders to support such studies, preferring instead robust, rigorous evaluation of real-life practice.
Policy-driven approach to nonmedical prescribing in Scotland: pharmacist prescribing as an exemplar
While evidence of benefit and safety of NMP is essential to inform practice, for NMP to be implemented successfully and sustained on a large scale, there needs to be clear commitment at the highest level. This section provides a description of the Scottish Government strategy around the implementation of pharmacist prescribing; the approach and specific outcomes and actions described could be an exemplar for other professions and other countries. The Scottish Government strategy is to ensure that ‘all patients, regardless of their age and setting of care, will receive high quality pharmaceutical care using the clinical skills of the pharmacist to their full potential’.19 Prescription for Excellence: a Vision and Action Plan for the right pharmaceutical care through integrated partnerships and innovation, was published by the Scottish Government in September 2013. The vision articulated within this document is that by 2023, ‘all pharmacists providing National Health Service (NHS) pharmaceutical care will be NHS accredited clinical pharmacist independent prescribers working in collaborative partnerships with medical practitioners who will continue to have overall responsibility for diagnosis’. Much of the recommendations are based on a scoping review of pharmaceutical care of patients in the community in Scotland, undertaken by Wilson and Barber.20 There were several drivers for this landmark review including: the increasing work pressures in the NHS; the imminent lack of clinical capacity of the medical workforce; and an increasingly multimorbid older population with complex medicine-related needs. There was recognition that ‘significant changes will occur in medicine and therapeutics that will require new and innovative models of care to enable patients to obtain the maximum benefit’.19
Enhancing and supporting the implementation of pharmacist IP to ensure patient-centred, safe, effective and efficient pharmaceutical care is fundamental to the delivery of the ambitions of Prescription for Excellence. Key specific outcomes include:
Pharmacists in the NHS would be recognized as clinicians responsible for the provision of NHS pharmaceutical care.
Releasing capacity of pharmacists to deliver pharmaceutical care would be facilitated by full utilization of pharmacy technicians, support staff and increased use of robotics in dispensing to improve safety and efficiency.
All patients would have access to NHS pharmaceutical care by NHS-accredited clinical pharmacist independent prescribers in all settings.
Patients have a close relationship with an individual pharmacist, ensuring greater continuity and consistency of care for patients, introducing the concept of the named pharmacist and patient registration with NHS Board-listed pharmacists that will underpin professional relationships with patients and local clinical governance systems.
There is an associated workplan to ensure that these outcomes (and others) are achieved within the 10-year timeframe. This includes developing approaches to:
Embed partnership working between the patient (and possibly carer), their GP and pharmacist, therapeutic partnerships, and with other health- and social-care professionals.
Further enhance the role of pharmacist IPs who will work with GPs to deliver medication/polypharmacy reviews, using telehealthcare and domiciliary visits, where appropriate.
Further develop the pharmacist’s contribution to the management of common clinical conditions and develop new models of delivery of primary care services in partnership with GPs.
Explore making better use of pharmacist prescribing post diagnosis.
There are clearly wide-ranging implications for all involved in the education, training and regulation of the pharmacy workforce, as well as all other health- and social-care professionals with whom the pharmacist IP will work and patients, their families and carers, as well as the general public. These are highlighted in terms of:
Ensuring a workforce that is fit for purpose by implementation of NHS standards of practice for pharmaceutical care that are attained through working with the NHS, Schools of Pharmacy and Medicine, NHS Education for Scotland and the professional and regulatory bodies.
Ensuring education and training meets the needs of patients and the NHS.
Implementation of primary and secondary care-configured systems to allow electronic information sharing contributing to pharmaceutical care and electronic prescribing for all prescribers including pharmacist IPs.
It is, therefore, reassuring that specific reference is made to supporting ‘action research, practice research and clinical research that enables development and evaluation of pharmaceutical care’. Governance arrangements have been put in place to ensure delivery of the work programme and vision. These comprise: a Steering Board of key Scottish Government and NHS contacts to oversee and prioritise implementation; a Reference Group of a wide range of stakeholders to act as a sounding board; a Core Implementation/Management Group of the leads to oversee the working groups; and Working Groups developing a response to each action point contained in Prescription for Excellence.
There are now over 750 pharmacists in Scotland (around 20%) who are either pharmacist IPs or have commenced training with the potential to make a difference to patient care in line with the ambitions of Prescription for Excellence. A recent survey of pharmacist prescribers across Great Britain, conducted by the General Pharmaceutical Council, highlighted that almost three quarters of the respondents were active prescribers, with the three major areas of prescribing being antibiotics, pain management and cardiovascular agents.21 Barriers to prescribing cited included lack of resources and support networks, opportunity to prescribe and recognition of the prescribing role. These issues have been demonstrated repeatedly in previous research focusing on pharmacists in Great Britain, as well as in other countries and groups of IPs in systematic reviews.12,14,16 It is, therefore, vital that these issues of structures and processes are dealt with rigorously as Prescription for Excellence progresses in order to ensure the very best outcomes for patients. There is also a need to ensure that pharmacist IPs are truly integrated within the healthcare team and that the roles and responsibilities of all prescribers (medical and nonmedical) are understood by all.
Challenges to be overcome
There is a great opportunity for NMP to make a real difference to professional practice and patient care globally. Legislation and models of care implemented vary between countries and it is possible that this variation will widen as more countries develop their own policies, structures and processes. While there are several significant matters which must be addressed, two key issues are: the need for sustainable models of care, and robust, rigorous evaluation research.
There are many examples in healthcare of successful pilot projects not being sustained or failing once extended beyond successful pilot sites. There are also reports which indicate that a number of qualified nonmedical prescribers have not prescribed. It is, therefore, extremely important to consider the theoretical basis for implementation of any major development or change in the delivery of services. Theory is also a key consideration in the UK Medical Research Council guidance on ‘Developing and implementing complex interventions’.22 One theory which is gaining in credibility in health-related innovation is Normalization Process Theory (NPT). NPT is a set of sociological tools developed by May and colleagues, explaining ‘…the social processes through which new or modified practices of thinking, enacting and organizing work are operationalized in healthcare and other institutionalized settings’.23 It focuses on how work practices become routinely embedded (normalized) in everyday routines, with those practices which are normalized being much more likely to be sustained, leading to the long-term desired outcomes.
NPT offers an explanation of three obstacles: implementation, the social organization of bringing practices into action; embedding, the process through which practices become incorporated routinely; and integration, the process by which practices are sustained.23,24 NPT proposes that practices are embedded routinely as the result of people working individually and collectively to implement them. Implementation is operationalized through four constructs of:
Coherence, which relates to the sense-making work that people do individually and collectively.
Cognitive participation, relational work that people do to build and sustain a community of practice.
Collective action, operational work that people do to enact a set of practices.
Reflexive monitoring, appraisal work that people do to assess and understand the ways that a new set of practices affect them and others around them.
Implementing NMP into any health system is likely to be complex when considering the number of different health professionals involved, the different processes and technological systems, the central role of the patient and influences of families, friends, carers, and many other factors which could impact negatively on the implementation and sustainability of NMP. Consider the situation where NMP is to be implemented in primary care. Patients will undoubtedly be going to interact with many health professionals and may well have more than one prescriber. For example, a medical prescriber may prescribe during a consultation for an acute condition or an acute worsening of a chronic condition. A nurse IP may manage a specific medical condition such as type 2 diabetes mellitus and the pharmacist IP may review and alter all chronic medicines. There is great potential for confusion which could lead to negative patient outcomes.
Applying the principles of NPT and considering the constructs should enable clear coherence, understanding and shared decision making of all policy makers, managers, leaders, health professionals and patients. Cognitive participation should result in organized individuals working together systematically for collective action with clearly specified roles of health professionals, prescribers, patients and pathways of care. The final construct of reflexive monitoring should ensure that there is appropriate appraisal of the structures, processes and outcomes of NMP. This would facilitate successful implementation from all the different perspectives involved and sustainability of NMP. Returning to the example of Scotland and pharmacist prescribing, much effort is being expended on the governance structures to ensure coherence at all levels, cognitive participation, collective action and reflexive monitoring.19 This is being effected through a programme of widespread engagement, facilitated by several interlinked workstreams, an overarching reference group and a management group. Emphasis is being placed on the active involvement of stakeholders (e.g. patient groups, health professionals, managers, leader, policy makers, academics, researchers, etc.) and rapid communication of developments.
The second issue that relates directly to reflexive monitoring is concerned with the necessity for robust and rigorous evaluation. While evaluation-based research studies are considered to provide a lower level of evidence compared with findings derived from RCTs and associated systematic reviews and meta-analyses, evaluation designs are based on real-life settings and practice. Furthermore, as NMP becomes adopted into legislation and practice, it is less likely that policy makers, senior managers and research funders will support RCT designs.
The UK Health Foundation highlights three different definitions of evaluation that they consider relevant to health: the process of determining the merit, worth or value of something; using systematic, data-based inquiries about whatever is being evaluated; and a process undertaken for purposes of improvement, decision making, enlightenment and persuasion.25 Robust and rigorous evaluation will provide valid, reliable and trustworthy data about how, why and when services are working (or not working). Better Evaluation is an ‘international collaboration to improve evaluation practice and theory by sharing and generating information about options (methods or processes) and approaches’.26 There are seven clusters of evaluation tasks: managing an evaluation or evaluation system; defining what is to be evaluated; framing the boundaries for the evaluation; describing activities, outcomes, impacts and context; understanding causes of outcomes and impacts; synthesizing data from one or more evaluations; and reporting and supporting use of findings.
There are multiple approaches to evaluation, some examples being: case studies, focused on understanding a unit (e.g. NMP site) in its context, employing qualitative, quantitative and mixed methodologies; participatory action research, which involves practitioners in the research process from the initial design of the project through data gathering and analysis to final conclusions; and realist evaluation. In 1997, Pawson and Tilley developed the first realist-evaluation approach based on the question, ‘what works, for whom, in what respects, to what extent, in what contexts, and how?’.27 This approach differs from others in that it is grounded in theory, is claimed to be suited to assessing (a form of theory-driven evaluation) and hence may be relevant to consider if using a theory such as NPT to facilitate implementation and sustainability. As with other evaluation approaches, the methodology may be qualitative, quantitative or mixed. However, alongside consideration of the evaluation approach, attention should be paid to who conducts the evaluation, when it should be conducted, and how to use the findings. Evaluation of NMP must consider all perspectives and while there are many examples of such evaluations, most are small scale, tend to focus on a limited number of perspectives, and often omit any theoretical underpinning to data collection, analysis or interpretation.
Paying attention to these twin issues of intervention, normalization for sustainability and producing robust and rigorous evaluation data will greatly enhance NMP realization globally.
Conclusion
Many countries have implemented NMP and these models of care are now being considered by others across the globe. Given that prescribing is a complex task with high potential for error, evidence of NMP outcomes is warranted. While there are a number of systematic reviews on aspects of NMP, there is a lack of evidence of prescribing safety, and clinical and cost effectiveness. The strategic approach of the Scottish Government to the implementation of pharmacist prescribing on a large scale could inform other countries as they implement and extend NMP. There are many challenges to implementing NMP into working practice; two key challenges are the need for sustainable models of care and evaluation research. These challenges could be met by considering the theoretical basis for NMP developments, and robust and rigorous evaluation to provide valid, reliable and trustworthy data about how, why and when services are working (or not working) to inform further developments.
Footnotes
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Conflict of interest statement: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Contributor Information
Derek Stewart, Robert Gordon University, Sir Ian Wood Building, Garthdee Road, Aberdeen, AB10 7GJ, UK.
Tesnime Jebara, Robert Gordon University, Aberdeen, UK.
Scott Cunningham, Robert Gordon University, Aberdeen, UK.
Ahmed Awaisu, Qatar University, Doha, Ad Dawhah, Qatar.
Abdulrouf Pallivalapila, Hamad Medical Corporation, Qatar.
Katie MacLure, Robert Gordon University, Aberdeen, UK.
References
- 1. Stewart D, MacLure K, George J. Educating non-medical prescribers. Brit J Clin Pharmacol 2012; 74: 662–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cope CP, Abuzour AS, Tully MP. Nonmedical prescribing: where are we now? Ther Adv Drug Saf 2016; 7: 165–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Department of Health. Supplementary prescribing by nurses and pharmacists within the NHS in England a guide for implementation. London: UK Department of Health, http://webarchive.nationalarchives.gov.uk/+/www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4009717 (2003, accessed 1 October 2016). [Google Scholar]
- 4. Department of Health. Improving patients’ access to medicines: A guide to implementing nurse and pharmacist independent prescribing within the NHS in England. London: UK Department of Health, http://webarchive.nationalarchives.gov.uk/+/www.dh.gov.uk/en/PublicationsandStatistics/Publications/PublicationsPolicyandGuidance/DH_4133743 (2006, accessed 1 October 2016). [Google Scholar]
- 5. British Pharmacological Society. Ten principles of good prescribing, http://main.bps.ac.uk/SpringboardWebApp/userfiles/bps/file/Guidelines/BPSPrescribingPrinciples.pdf (accessed 1 October 2016).
- 6. Ross S, Bond C, Rothnie H, et al. What is the scale of prescribing errors committed by junior doctors? A systematic review. Brit J Clin Pharmacol 2009; 67: 629–640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lewis PJ, Dornan T, Taylor D, et al. Prevalence, incidence and nature of prescribing errors in hospital inpatients: a systematic review. Drug Saf 2009; 32: 379–389. [DOI] [PubMed] [Google Scholar]
- 8. Baqir W, Crehan O, Murray R, et al. Pharmacist prescribing within a UK NHS hospital trust: nature and extent of prescribing, and prevalence of errors. Eur J Hosp Pharm 2015; 22: 79–82. [Google Scholar]
- 9. National Prescribing Centre. A single competency framework for all prescribers. National Institute for Health and Clinical Excellence, http://cfna.org.uk/3309trV/prescribers_competency_framework.pdf (2012, accessed 1 October 2016). [Google Scholar]
- 10. Aromataris E, Fernandez R, Godfrey CM, et al. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. Int J Evid Based Healthc 2015; 13: 132–140. [DOI] [PubMed] [Google Scholar]
- 11. Critical Appraisal Skills Programme (CASP), Making sense of evidence, http://www.casp-uk.net/checklists (accessed 1 October 2016).
- 12. Kroezen M, van Dijk L, Groenewegen PP, et al. Nurse prescribing of medicines in Western European and Anglo-Saxon countries: a systematic review of the literature. BMC Health Serv Res 2011; 11: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ness V, Price L, Currie K, et al. Influences on independent nurse prescribers’ antimicrobial prescribing behaviour: a systematic review. J Clin Nurs 2016; 25: 1206–1217. [DOI] [PubMed] [Google Scholar]
- 14. Van Ruth L, Francke AL, Mistiaen P. Effects of nurse prescribing of medication: a systematic review. Internet J Healthc Adm 2008; 5: 2. [Google Scholar]
- 15. Gielen SC, Dekker J, Francke AL, et al. The effects of nurse prescribing: a systematic review. Int J Nurs Stud 2014; 51: 1048–1061. [DOI] [PubMed] [Google Scholar]
- 16. Darvishpour A, Joolaee S, Cheraghi MA. A meta-synthesis study of literature review and systematic review published in nurse prescribing. Med J Islam Repub Iran 2014; 28: 77. [PMC free article] [PubMed] [Google Scholar]
- 17. McIntosh T, Stewart D, Forbes-McKay K, et al. Influences on prescribing decision-making among non-medical prescribers in the United Kingdom: systematic review. Fam Pract 2016; 33: 572–579. [DOI] [PubMed] [Google Scholar]
- 18. Weeks G, George J, Maclure K, et al. Non-medical prescribing versus medical prescribing for acute and chronic disease management in primary and secondary care. Cochrane Database Syst Rev 2016; 11: CD011227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. The Scottish Government. Prescription for excellence: a vision and action plan for the right pharmaceutical care through integrated partnerships and innovation. Edinburgh: The Scottish Government, http://www.scotland.gov.uk/Topics/Health/Policy/Prescription-for-Excellence (2014, accessed 1 October 2016). [Google Scholar]
- 20. Wilson H, Barber N. Review of NHS pharmaceutical care of patients in the community in Scotland. Edinburgh: The Scottish Government, 2013. [Google Scholar]
- 21. General Pharmaceutical Council. Prescribers survey report, https://www.pharmacyregulation.org/regulate/article/pharmacist-prescriber-survey (2016, accessed 1 October 2016).
- 22. Craig P, Dieppe P, Macintyre S, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. Brit Med J 2008; 337: a1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. May CR, Mair F, Finch T, et al. Development of a theory of implementation and integration: normalization process theory. Implement Sci 2009; 4: 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. May C, Finch T. Implementing, embedding and integrating practices: an outline of normalization process theory. Sociology 2009; 43: 535–554. [Google Scholar]
- 25. The Health Foundation. Evaluation: what to consider, http://www.health.org.uk/publication/evaluation-what-consider (2015, accessed 1 October 2016).
- 26. Better evaluation: sharing information to improve evaluation, http://betterevaluation.org/ (accessed 1 October 2016).
- 27. Pawson R, Tilley N. Realistic evaluation. London: Sage, 1997. [Google Scholar]