Abstract
Background:
The aim of this study is to determine the prevalence and characteristics of youth with attention-deficit hyperactivity disorder (ADHD) in Ontario, Canada, and to determine the predictors of psychotropic medication prescriptions in youth with ADHD.
Method:
This is a cross-sectional retrospective chart abstraction of more than 250 000 medical records from youth aged 1 to 24 years in a large geographical region in Ontario, Canada, linked to population-based health administrative data. A total of 10 000 charts were randomly selected and manually reviewed using predetermined criteria for ADHD and comorbidities. Prevalence, comorbidities, demographic indicators, and health service utilization characteristics were calculated. Predictors of treatment characteristics were determined using logistic regression modelling.
Results:
The prevalence of ADHD was 5.4% (7.9% males, 2.7% females). Youth with ADHD had significant psychiatric comorbidities. The majority (70.0%) of ADHD patients received prescriptions for stimulant or nonstimulant ADHD medication. Antipsychotic prescriptions were provided to 11.9% of ADHD patients versus 0.9% of patients without ADHD. Antidepressant prescriptions were provided to 19.8% versus 5.4% of patients with and without ADHD, respectively. Predictors of antidepressant prescriptions were increasing age (odds ratio [OR], 1.14; 95% confidence interval [CI], 1.07 to 1.21), psychiatric consultation (OR, 2.04; 95% CI, 1.16 to 3.58), and diagnoses of both anxiety and depression (OR, 18.4; 95% CI, 8.03 to 42.1), whereas the only predictor of antipsychotic prescriptions was psychiatric consultation (OR, 3.85; 95% CI, 2.11 to 7.02).
Conclusions:
Youth with ADHD have more psychiatric comorbidities than youth without ADHD. The majority of youth with ADHD received stimulant medications, and a significant number received additional psychotropic medications, with psychiatric consultation predicting medication use.
Keywords: ADHD, epidemiology, pharmacoepidemiology, antipsychotics, child and adolescent psychiatry
Abstract
Objectif:
Déterminer la prévalence et les caractéristiques des adolescents souffrant du trouble de déficit de l’attention avec hyperactivité (TDAH) en Ontario, au Canada. Déterminer les prédicteurs des prescriptions de médicaments psychotropes chez les adolescents souffrant du TDAH.
Méthode:
Nous présentons une extraction transversale rétrospective des données de plus de 250 000 dossiers médicaux d’adolescents âgés de 1 à 24 ans d’une grande région géographique de l’Ontario, au Canada, liée aux données de santé administratives dans la population. Dix mille dossiers ont été choisis au hasard et examinés manuellement à l’aide de critères prédéterminés pour le TDAH et les comorbidités. La prévalence, les comorbidités, les indicateurs démographiques et les caractéristiques de l’utilisation des services de santé ont été calculés. Les prédicteurs des caractéristiques de traitement ont été déterminés à l’aide d’un modèle de régression logistique.
Résultats:
La prévalence du TDAH était de 5,4% (7,9% hommes, 2,7% femmes). Les adolescents souffrant d’un TDAH avaient des comorbidités psychiatriques significatives. La majorité (70,0%) des patients du TDAH recevait des prescriptions de médicaments du TDAH stimulants ou non stimulants. Des prescriptions d’antipsychotiques ont été données à 11,9% des patients du TDAH, contre 0,9% des patients sans TDAH. Des prescriptions d’antidépresseurs ont été offertes à 19,8% contre 5,4% des patients avec et sans TDAH, respectivement. Les prédicteurs des prescriptions d’antidépresseurs étaient l’augmentation de l’âge (RC 1,14; IC à 95% 1,07 à 1,21), la consultation psychiatrique (RC 2,04; IC à 95% 1,16 à 3,58) et les diagnostics d’anxiété et de dépression (RC 18,4; IC à 95% 8,03 à 42,1), alors que le seul prédicteur de prescriptions d’antipsychotiques était la consultation psychiatrique (RC 3,85; IC à 95% 2,11 à 7,02).
Conclusions:
Les adolescents souffrant du TDAH ont plus de comorbidités psychiatriques que les adolescents qui n’en souffrent pas. La majorité des adolescents souffrant du TDAH a reçu des médicaments stimulants et un nombre significatif a reçu des médicaments psychotropes additionnels. La consultation psychiatrique prédisait l’utilisation de médicaments.
If mental health is “the leading children’s health problem today,”1 Attention-deficit hyperactivity disorder (ADHD) is of particular concern given that ADHD has a significant impact on functional outcomes,2,3 and its prevalence appears to be increasing.4 To promote the health of children with ADHD, it is important to understand the prevalence of both this diagnosis and associated comorbidities and the factors that determine treatment outcomes. ADHD treatment can be challenging for clinicians, as first-line treatment involves the use of stimulant medications, which may be abused and pose the risk of psychosis (although rare).5,6 Beyond drug misuse and serious adverse effects, there is considerable variability in how ADHD is treated, including the use of off-label, nonstimulant medication, such as antipsychotics.7 A comparison of guidelines between the United States and the United Kingdom indicates that American guidelines (American Academy of Child & Adolescent Psychiatry) suggest “medications not FDA approved” as a treatment option if first-line treatment fails in preschool children, whereas the United Kingdom (National Institute for Health and Care Excellence) guidelines say, “drug treatment is not recommended” in preschool children who do not respond to first-line treatment.8
Despite the widespread use of antipsychotics for ADHD, the evidence for their use is sparse. Risperidone has a moderate impact on certain behaviours in youth with ADHD,9,10 such as oppositional and aggressive behavior, but there is limited evidence to support the use of other antipsychotic medications, and they are not indicated for the core symptoms of inattention and hyperactivity.11 There are limited data concerning longer-term efficacy of antipsychotics for disruptive behavior and appropriate timelines for discontinuation.11 A recent study revealed that children with ADHD who are prescribed antipsychotics have higher health care resource use than children who are not prescribed such medications.12 ADHD is common, and the treatment for ADHD appears to be highly varied and includes medications such as atypical antipsychotics, for which there is little evidence of benefit and substantial evidence of potential harm (weight gain, dyslipidemia, extrapyramidal side effects).13 Consequently, it is important to understand why these medications are being used. Population-based primary care data are a good source of information for understanding the circumstances in which nonstimulant medications are being used to treat ADHD.
The objective of this study was to determine the prevalence of ADHD and to compare demographic, comorbidity, health service utilization, and medication use between ADHD and non-ADHD subjects. We also evaluated predictors of nonstimulant medication use among children and youth with ADHD.
Methods
Data Sources and Chart Abstraction
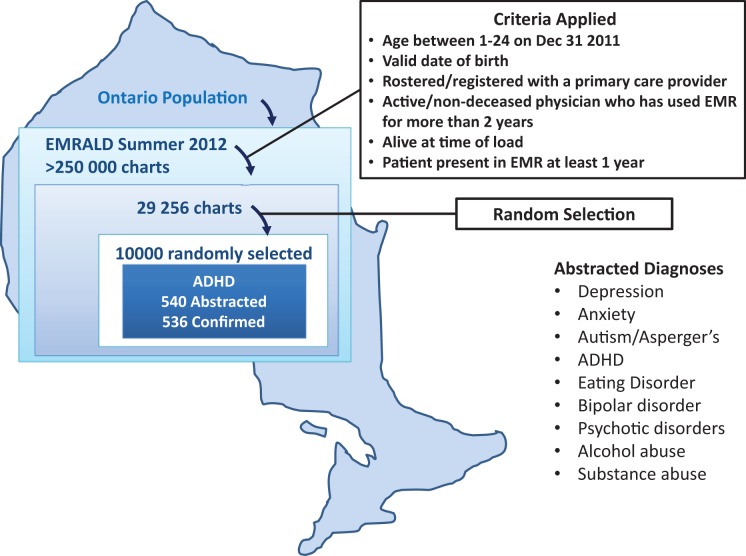
At the time of this study, there were more than 250 000 patients contained in the previously described Electronic Medical Record Administrative data Linked Database (EMRALD) primary care electronic medical record data set.14 EMRALD is a collection of data from family physicians in Ontario and includes the contents of medical charts, such as test results, prescriptions, visit notes, consultation correspondence, and notes about the patients’ medical history. Selection criteria (described in Figure 1) were applied, resulting in 29 256 children and youth patients who met eligibility criteria of persons aged 1 to 24 years. Of these, 10 000 were randomly selected and were individually read and manually abstracted for 9 mental health diagnoses by trained abstractors. A medical expert (T.S.H.) reviewed all definite and possible cases of ADHD and adjudicated questionable cases. ADHD diagnosis was abstracted from EMRALD, as were consultations with paediatricians, psychiatrists, psychologists, and social workers available in the entire chart. Comorbid diagnoses (alcohol abuse, anxiety, depression, autism/Asperger’s, bipolar disorder, drug abuse, eating disorders, and psychotic disorders) were also abstracted at the same time as ADHD diagnoses.
Figure 1.
Method of chart abstraction and validation, including criteria applied to select charts and diagnoses used in abstraction. All possible and definite cases were reviewed by a psychiatry resident (T.S.H.), resulting in 536 confirmed charts with a definite attention-deficit hyperactivity disorder diagnosis.
The 10 000 abstracted charts were linked to population-based administrative health records housed at the Institute for Clinical Evaluative Sciences (ICES). ICES is an independent, nonprofit research organization that holds population-level data, including administrative data, for the purpose of evaluating health care services and their effectiveness in Ontario. Patient-level records in these data are linked to each other with a unique encoded identifier using the Registered Persons Database (RPDB) for every Ontario resident with an assigned health card number. The RPDB was used to measure demographic variables such as age, neighbourhood income quintile (derived from Statistics Canada Census data), and rural residence. Income quintile measures household income and adjusts for household size and community size (quintile 1 is the lowest income). This is derived by linking the postal code of the patient to national Canadian census data. Rurality is an indicator of the size of the patient’s community, where a community smaller than 10 000 people is defined as being rural. The Ontario Health Insurance Plan (OHIP) lists medical service billings by Ontario physicians since 1991 and was used to measure visits to family doctors, psychiatrists, paediatricians, and neurologists (family doctors include general practitioners). As children and youth may be in the electronic medical record (EMR) for variable amounts of time, the duration of OHIP eligibility was assessed. The Canadian Institute for Health Information–National Ambulatory Care Reporting System (CIHI-NACRS), includes patient-level details on hospital visits and community-based ambulatory care, outpatient clinics, day surgery, and emergency department (ED) visits since 2002 and provided information on the number of ED visits. The look-back period for family physician (general practitioner) billings was 1 year from the look-back date of April 1, 2012. The look-back period for specialist billings and health service use was 10 years from the same date (April 1, 2012).
Subjects
As illustrated in Figure 1, inclusion criteria were applied prior to randomly selecting the 10 000 EMRALD subjects. Inclusion criteria included the following: age of 1 to 24 years as of December 31, 2011, valid date of birth, rostered/registered with a family doctor, active/practicing physician who has used an EMR for more than 2 years, patient alive at the time the EMR data were extracted, and patient present in the EMR for at least 1 year. Within the EMRALD database, ADHD cases were ascertained by applying predetermined selection criteria developed by the EMRALD team consisting of both family doctors and psychiatrists. Definite cases of ADHD were charts in which the family physician recorded a diagnosis of attention-deficit disorder/ADHD, if a neuropsychological test or report indicated a diagnosis, or if correspondence from a school/school board indicated a diagnosis of ADHD. All other EMRALD subjects were controls. The ascertainment of ADHD resulted in a prevalence-based cohort. We were not able to determine the date of first ADHD diagnosis within the EMR data, as the diagnosis may have occurred prior to the start of the EMR record and diagnosis dates were not consistently recorded.
Outcomes
For the ADHD prevalence objective, the outcome was a diagnosis of ADHD (and these subjects were compared with youth with no ADHD diagnosis). For the nonstimulant or adjuvant treatment ADHD treatment objective, the primary outcomes were prescriptions for antipsychotics and antidepressants from the family physician.
Covariates
We measured demographic characteristics such as age, sex, neighbourhood income quintile (using census data), and rural residence. We also measured visits with paediatricians, psychiatrists, and neurologists in the previous 10-year period based on OHIP billings. OHIP billings were used to determine the number of total, mental health–related, and non–mental health–related family physician visits in the past year. Mental health– and non–mental health–related physician visits were distinguished based on a validated algorithm.15 We measured the number of ED visits in the past 10-year period for psychiatric and nonpsychiatric reasons. Psychiatric ED visits were those in which the reason for visit ICD10 diagnosis was F00 to F99 OR X60-X84; nonpsychiatric ED visits were ED visits for any other diagnosis. Finally, we measured notes and consultation letters (social workers, paediatricians, psychiatrists, and psychologists) available from the EMRALD medical chart.
Statistical Analyses
Continuous data were summarized using means, standard deviations, and medians. Categorical data were summarized using frequencies and percentages. Patient demographics and health service use between the ADHD and non-ADHD cohort were compared by using a chi-squared test for categorical variables and 1-way analysis of variance for continuous variables.
Multivariable logistic regression was used to evaluate the factors that influenced whether an ADHD patient received a prescription drug (antipsychotics or antidepressants). Explanatory variables included patient and geographic characteristics and frequency of health care services use. During the model-building process, a univariate analysis was performed for each variable to evaluate significance for inclusion into the model. Variables that were hypothesized a priori to have clinical relevance were also included in the final multivariable regression model. All analyses were performed using SAS statistical software (version 9.4, SAS Institute Inc., Cary, NC).
Results
Demographics
Abstraction yielded 540 definite cases of ADHD; 4 of these cases were rejected during confirmation or adjudication, resulting in a final ADHD sample of 536 subjects (99.3% agreement) and an overall prevalence of 5.4% (7.9% males, 2.7% females), as seen in Supplementary Table 1. Individuals diagnosed with ADHD were older than those without ADHD, and boys in particular acquired the diagnosis with increasing age, with noticeable increases in prevalence among boys 14 to 17 years (11.7%) versus girls (4.9%; Suppl. Table 1). There were no significant differences in income distribution or rural residence between those with and without an ADHD diagnosis (Suppl. Table 2). Additional measures of socioeconomic status and marginalization were not significantly different between those with and without ADHD and are not shown.
Health Service Use
Children and youth with ADHD had significantly more visits to family doctors for mental health–related conditions but not more visits for non–mental health–conditions (Suppl. Table 3). They also had significantly greater psychiatrist and paediatrician visits, although not neurology visits (Table 1). Patients with ADHD were much more likely to visit a psychiatrist more than twice in 10 years (27.7% for males with ADHD versus 3.2% for males without ADHD). ED visits for psychiatric conditions were low throughout the sample, but youth with ADHD were more likely to visit an ED for nonpsychiatric conditions, and 62.6% of youth with ADHD versus 48.9% of males without ADHD visited an ED for nonpsychiatric reasons more than twice in 10 years.
Table 1.
Characteristics of ADHD versus Non-ADHD Patients Including Prior Health Service Use in the Past 10 Years and Consultations Based on Physician Billings, Consultations Received Based on the EMR, and Psychiatric Comorbidities Identified in the Manual Chart Abstraction.a
| No ADHD | ADHD | |||||
|---|---|---|---|---|---|---|
| Male (n = 4661) | Female (n = 4803) | Male (n = 401) | Female (n = 135) | P Value | ||
| Service use (billings) | ||||||
| Psychiatrist visits | Mean ± SD | 0.53 ± 5.39 | 0.61 ± 5.71 | 3.73 ± 10.72 | 6.30 ± 17.87 | <0.001 |
| Median (IQR) | 0 (0-0) | 0 (0-0) | 0 (0-3) | 0 (0-5) | <0.001 | |
| Psychiatrist visits (categories) | 0 | 4412 (94.7%) | 4528 (94.3%) | 252 (62.8%) | 74 (54.8%) | <0.001 |
| 1-2 | 100 (2.1%) | 105 (2.2%) | 38 (9.5%) | 14 (10.4%) | ||
| 2+ | 149 (3.2%) | 170 (3.5%) | 111 (27.7%) | 47 (34.8%) | ||
| Paediatrician visits | Mean ± SD | 2.47 ± 6.12 | 2.37 ± 6.07 | 7.75 ± 12.00 | 8.67 ± 10.99 | <0.001 |
| Median (IQR) | 0 (0-2) | 0 (0-2) | 4 (1-11) | 4 (1-12) | <0.001 | |
| Paediatrician visits (categories) | 0 | 2713 (58.2%) | 2887 (60.1%) | 87 (21.7%) | 33 (24.4%) | <0.001 |
| 1-2 | 902 (19.4%) | 888 (18.5%) | 68 (17.0%) | 18 (13.3%) | ||
| 2+ | 1046 (22.4%) | 1028 (21.4%) | 246 (61.3%) | 84 (62.2%) | ||
| Neurologist visits | Mean ± SD | 0.06 ± 0.75 | 0.05 ± 0.51 | 0.10 ± 0.60 | 0.11 ± 0.69 | 0.076 |
| Median (IQR) | 0 (0-0) | 0 (0-0) | 0 (0-0) | 0 (0-0) | <0.001 | |
| Neurologist visits (categories) | 0 | 4574 (98.1%) | 4698 (97.8%) | 380 (94.8%) | 129 (95.6%) | <0.001 |
| 1-2 | 60 (1.3%) | 83 (1.7%) | * (*) | ≤5 (*) | ||
| 2+ | 27 (0.6%) | 22 (0.5%) | ≤5 (*) | ≤5 (*) | ||
| ED visits for psychiatric conditions | Mean ± SD | 0.07 ± 0.75 | 0.08 ± 0.50 | 0.18 ± 0.64 | 0.41 ± 0.90 | <0.001 |
| Median (IQR) | 0 (0-0) | 0 (0-0) | 0 (0-0) | 0 (0-0) | <0.001 | |
| ED visits for psychiatric conditions (categories) | 0 | 4469 (95.9%) | 4576 (95.3%) | 355 (88.5%) | 103 (76.3%) | <0.001 |
| 1-2 | 169 (3.6%) | 196 (4.1%) | * (*) | * (*) | ||
| 2+ | 23 (0.5%) | 31 (0.6%) | ≤5 (*) | ≤5 (*) | ||
| ED visits for nonpsychiatric conditions | Mean ± SD | 3.97 ± 5.12 | 3.79 ± 5.41 | 5.55 ± 6.22 | 6.08 ± 6.77 | <0.001 |
| Median (IQR) | 2 (1-5) | 2 (1-5) | 4 (2-7) | 4 (2-7) | <0.001 | |
| ED visits for nonpsychiatric conditions (categories) | 0 | 895 (19.2%) | 1068 (22.2%) | 46 (11.5%) | 14 (10.4%) | <0.001 |
| 1-2 | 1489 (31.9%) | 1658 (34.5%) | 104 (25.9%) | 34 (25.2%) | ||
| 2+ | 2277 (48.9%) | 2077 (43.2%) | 251 (62.6%) | 87 (64.4%) | ||
| Consultations in EMR | ||||||
| Paediatrician consult | 1,096 (23.5%) | 971 (20.2%) | 202 (50.4%) | 67 (49.6%) | <0.001 | |
| Psychiatrist consult | 150 (3.2%) | 191 (4.0%) | 111 (27.7%) | 48 (35.6%) | <0.001 | |
| Psychologist consult | 95 (2.0%) | 73 (1.5%) | 55 (13.7%) | 27 (20.0%) | <0.001 | |
| Social worker consult | 38 (0.8%) | 53 (1.1%) | 12 (3.0%) | 6 (4.4%) | <0.001 | |
| Psychiatric comorbidities | ||||||
| Alcohol abuse | 17 (0.4%) | 31 (0.6%) | 15 (3.7%) | <=5 (*) | <0.001 | |
| Anxiety only | 156 (3.3%) | 213 (4.4%) | 53 (13.2%) | 20 (14.8%) | <0.001 | |
| Depression only | 81 (1.7%) | 147 (3.1%) | 30 (7.5%) | 7 (5.2%) | <0.001 | |
| Anxiety and depression | 87 (1.9%) | 165 (3.4%) | 26 (6.5%) | 32 (23.7%) | <0.001 | |
| Autism/Asperger’s | 67 (1.4%) | 19 (0.4%) | 19 (4.7%) | 7 (5.2%) | <0.001 | |
| Bipolar disorder | 7 (0.2%) | 19 (0.4%) | 6 (1.5%) | ≤5 (*) | <0.001 | |
| Substance abuse | 74 (1.6%) | 59 (1.2%) | 32 (8.0%) | 13 (9.6%) | <0.001 | |
| Eating disorder | ≤5 (*) | 41 (0.9%) | ≤5 (*) | ≤5 (*) | 0.131 | |
| Psychotic disorder | 15 (0.3%) | ≤5 (*) | ≤5 (*) | ≤5 (*) | 0.356 | |
ADHD, attention-deficit hyperactivity disorder; ED, emergency department; EMR, electronic medical record.
aValues given as “≤5 (*)” indicate data omitted because they were too small to show (≤5 cases) and “* (*)” shows data suppressed so that other small cells cannot be calculated.
Consultations available in the EMR were significantly higher for youth with ADHD for paediatricians, psychiatrists, psychologists, and social workers, with 23.5% of males without ADHD having a paediatric consultation versus 50.4% with the diagnosis (Table 1). The burden of comorbid psychiatric illness was much higher in the cases with ADHD, and rates of alcohol abuse, anxiety, depression, autism spectrum disorder, bipolar disorder, and other drug abuse were all significantly higher among youth with ADHD. Eating disorders and psychotic disorders did not vary significantly between the 2 groups. Anxiety was more than 4 times more prevalent among youth with ADHD (13.2% of males and 14.8% of females) compared with youth without ADHD (3.3% of males and 4.4% of females; Table 1).
Prescriptions
Table 2 shows prescriptions based on ADHD status. For all 4 classes of medications (antidepressants, antipsychotics, ADHD medications, and benzodiazepines), ADHD patients received significantly more prescriptions. Of the 64 patients with ADHD who received a prescription for an antipsychotic, 18 (28.1%) had no other mental health diagnoses based on the chart abstraction.
Table 2.
Prescriptions Provided by Attention-Deficit Hyperactivity Disorder (ADHD) Status.
| Prescription Type | ADHD (n = 536) | No ADHD (n = 9464) | Standardized Difference | P Value |
|---|---|---|---|---|
| Antidepressants | 106 (19.8%) | 515 (5.4%) | 0.60 | <0.001 |
| Antipsychotics | 64 (11.9%) | 89 (0.9%) | 0.91 | <0.001 |
| Benzodiazepines | 28 (5.2%) | 175 (1.8%) | 0.24 | <0.001 |
| ADHD drugs | 375 (70.0%) | 48 (0.5%) | 5.48 | <0.001 |
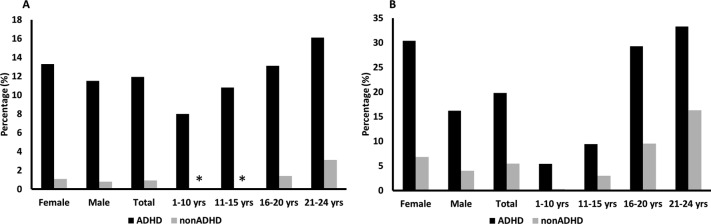
Figure 2A shows the breakdown of antipsychotic prescriptions by age and sex. Prescriptions are significantly higher in individuals with a diagnosis of ADHD and increase with age in both groups. The most prescribed antipsychotic among individuals with a diagnosis of ADHD was risperidone, and it represented 55.8% of antipsychotic prescriptions. Among individuals without ADHD, the most commonly prescribed antipsychotic was quetiapine, and it represented 51.3% of antipsychotic prescriptions. Figure 2B shows the breakdown of antidepressant prescriptions by age and sex. Prescriptions for antidepressants are also significantly higher in individuals who have a diagnosis of ADHD and increase with age regardless of diagnosis.
Figure 2.
(A) Antipsychotic prescriptions by age and attention-deficit hyperactivity disorder (ADHD) diagnosis. (B) Antidepressant prescriptions by age and ADHD diagnosis. *Data suppressed due to small cell size (≤5 cases).
Of ADHD patients taking antidepressants, 7.5% had received a prescription for bupropion (further breakdown is not possible because the number of patients become too small). In patients without ADHD, 0.4% received a prescription for bupropion.
ADHD medications (stimulants and atomoxetine) were routinely prescribed to individuals with a diagnosis of ADHD (70.0%) and minimally prescribed to individuals without a diagnosis of ADHD (0.5%) and did not vary significantly by age or sex. Of patients with ADHD on a stimulant, 50% received a prescription of a short-acting stimulant and 81.1% received a prescription for a long-acting stimulant. Of individuals with ADHD, 10.3% received a prescription for atomoxetine. The numbers for patients without a diagnosis of ADHD cannot be shown for atomoxetine as the numbers of cases are too low.
In terms of polypharmacy, 25 individuals (4.7%) with ADHD received prescriptions for at least 1 antidepressant, antipsychotic, and ADHD medication in their electronic chart, whereas 5 or fewer individuals without an ADHD diagnosis received prescriptions for all 3 classes of medication.
Logistic Regression Models
The outcomes of the regression modeling were predictors for receiving an antipsychotic prescription and receiving an antidepressant prescription among the ADHD population. Univariate analyses were performed for the following predictors: age, sex, rural residence, consultations in the EMR (social worker, psychiatrist, psychologist, paediatrician), psychiatric comorbidities (anxiety and depression, anxiety, depression, autism, bipolar disorder, drug abuse, psychotic disorder, alcohol abuse, eating disorder), income by quintile, GP visits (overall, mental health), specialist billings (psychiatry, paediatrics, neurology), and ED visits (psychiatric, nonpsychiatric). Based on the univariate parameters, a priori hypothesis, and sample size limits,16 a common multivariate model was developed that included age, sex, consultation with a psychiatrist, income quintile, and ED visits for psychiatric conditions as predictors. Results are shown in Table 3. Antipsychotic prescriptions were significantly associated with psychiatric consultation (odds ratio [OR], 3.85; 95% confidence interval [CI], 2.11 to 7.02). Antidepressant prescriptions were also associated with psychiatric consultation (OR, 2.04; 95% CI, 1.16 to 3.58) as well as comorbidities of both depression and anxiety (OR, 18.4; 95% CI, 8.03 to 42.1) and increasing age (OR, 1.14; 95% CI, 1.07 to 1.21).
Table 3.
Multivariate Logistic Regression Model for ADHD Patients Receiving Antipsychotics or Antidepressants.a
| Estimate | P Value | Odds Ratio | Lower CI | Upper CI | |
|---|---|---|---|---|---|
| Variables for antipsychotic model | |||||
| Age | 0.00243 | 0.9394 | 1.002 | 0.941 | 1.067 |
| Sex, female vs male | –0.2313 | 0.5036 | 0.794 | 0.403 | 1.563 |
| Consult with psychiatrist, 1 vs 0 | 1.3489 | <0.0001 | 3.853 | 2.115 | 7.02 |
| Anxiety and depression, 1 vs 0 | 0.6149 | 0.1249 | 1.85 | 0.843 | 4.057 |
| Income quintile, 1 vs 2 | –0.652 | 0.1611 | 0.521 | 0.209 | 1.297 |
| Income quintile, 1 vs 3 | –0.2472 | 0.5615 | 0.781 | 0.339 | 1.799 |
| Income quintile, 1 vs 4 | –0.2961 | 0.4862 | 0.744 | 0.323 | 1.711 |
| Income quintile, 1 vs 5 | –0.833 | 0.1039 | 0.435 | 0.159 | 1.187 |
| Number of ED visits for psychiatric conditions | 0.2847 | 0.0708 | 1.329 | 0.976 | 1.81 |
| Variables for antidepressant model | |||||
| Age | 0.1303 | <0.0001 | 1.139 | 1.07 | 1.213 |
| Sex, female vs male | 0.2024 | 0.5148 | 1.224 | 0.666 | 2.251 |
| Consult with psychiatrist, 1 vs 0 | 0.7105 | 0.0138 | 2.035 | 1.156 | 3.583 |
| Anxiety and depression, 1 vs 0 | 2.9119 | <.0001 | 18.392 | 8.027 | 42.142 |
| Income quintile, 1 vs 2 | 0.0887 | 0.8389 | 1.093 | 0.465 | 2.569 |
| Income quintile, 1 vs 3 | –0.6104 | 0.1943 | 0.543 | 0.216 | 1.365 |
| Income quintile, 1 vs 4 | 0.0886 | 0.8339 | 1.093 | 0.477 | 2.501 |
| Income quintile, 1 vs 5 | –0.457 | 0.3301 | 0.633 | 0.252 | 1.588 |
| Number of ED visits for psychiatric conditions | 0.1746 | 0.3076 | 1.191 | 0.851 | 1.665 |
ADHD, attention-deficit hyperactivity disorder; CI, confidence interval; ED, emergency department.
aAll variables had 1 degree of freedom.
Statistically significant predictors in the model.
Discussion
Our study revealed an overall ADHD prevalence of 5.4%, with a higher prevalence in males, but not females, in older cohorts, although the reasons for higher prevalence in older age categories are unclear. There were no statistically significant differences in income or rural versus urban residence between those with and without a diagnosis of ADHD. In terms of health service use, individuals with a diagnosis of ADHD were more likely to visit their general practitioner or family physician, particularly for mental health conditions. Compared with individuals without ADHD, ADHD patients had overall higher health service utilization, including specialist consultations, and had a higher burden of psychiatric comorbidities. A substantial number of individuals with ADHD received antipsychotic medications (with the majority of prescriptions for risperidone) and antidepressants. Increasing age, diagnoses of both anxiety and depression, and seeing a psychiatrist were factors for predicting antidepressant prescriptions, whereas only consultation with a psychiatrist predicted antipsychotic prescriptions.
The prevalence found in this study is comparable to national and international prevalence for ADHD, particularly with respect to meta-analyses of ADHD prevalence.1,17–27 The patterns of medication use are also very similar to studies conducted in Canada and the United States28,29 and confirm that the number of prescriptions is high even in a diverse study of youth across Ontario. This study also confirms, in the form of health care and ED visits, that patients with ADHD require greater health care resources than those without the disorder.12 Given the known socioeconomic determinants of health,1 it is surprising that income quintile was not significantly associated with ADHD diagnosis and not predictive of prescriptions. However, recent literature suggests that ADHD is increasing similarly in both the general population and children receiving Supplemental Security Income,30 and past studies have not found an association between poverty or socioeconomic status and mental illness or ADHD diagnosis.31,32 However, summary health statistics show that ADHD is more common among children of single mothers, black children, and children identified as “poor.”33 It is also possible that socioeconomic factors simultaneously increase prescriptions (when children without psychosocial supports are encouraged to use medications for behavioural control) or decrease prescriptions (if these children have a lower chance of affording these drugs, which are not covered by the provincial health plan), and such factors may complicate a possible association.
Antipsychotic medications are prescribed for ADHD and for other psychiatric diagnoses in children and youth,34 and a recent Canadian study identified the prevalence of antipsychotic combination therapy to be 10.8%.28 In the United States, a recent study showed that antipsychotics were used in addition to stimulant medications in 5.8% to 6.8% of children and adolescents.35 A recent follow-up study of children with severe ADHD who did not respond to behaviour therapy showed rates of antipsychotic use as high as 13.4%.36 In the United States, ADHD was the most common diagnosis among children and youth treated with antipsychotics,37 and nearly 1 in 5 children on Medicaid with ADHD are treated with antipsychotics and long-acting stimulants concurrently.29
With respect to antidepressants, predictors of prescriptions in this study included age, psychiatric consultation, and a diagnosis of both anxiety and depression. It is reasonable that older individuals in this cohort, with multiple comorbidities, would be prescribed such medications. Anxiety and depression are more common among the youth with ADHD, and these are indications for the prescribed antidepressant medications.
More than 1 in 10 individuals with ADHD received a prescription for an antipsychotic medication, numbers that are similar to those recently reported elsewhere.28,36 Risperidone is the most commonly prescribed antipsychotic in this population, and it has the most evidence for use in ADHD.11 The multivariable regression model did not show that age, sex, or income predict antipsychotic prescriptions. While previous studies have identified socioeconomic predictors of health service use such as single-parent families,38 a recent study also failed to find a relationship between service use and factors such as neighbourhood advantage and caregiver education level.39 In this study, the only predictor found for antipsychotics was psychiatric consultation (OR, 3.85; 95% CI, 2.11 to 7.02), which is surprising. Psychosis is very low in this population (below 1%) and does not appear to explain the use of antipsychotics. Involvement of a psychiatrist suggests that these individuals may have a high burden of illness and complexity. Our data support this, with Table 1 showing significantly higher psychiatric comorbidity in males and females with ADHD compared with those without. Furthermore, Table 1 shows much higher rates of consultation of specialists, especially psychiatrists, in individuals with ADHD. However, given the known adverse consequences of antipsychotic exposure in youth, such as metabolic consequences,40 and the limited evidence for their use in ADHD treatment, the circumstances and outcomes related to antipsychotic use in ADHD need further exploration.
This study had several unique strengths relative to existing literature on ADHD prevalence and treatment patterns. Manual abstraction of psychiatric diagnoses allows the data set to reflect a clinically representative sample of youth with ADHD, and the manner in which they are treated in the community, although the way in which they were diagnosed with ADHD is not known. This study does not rely on self-report or symptom-based scales. The large data set consists of 10 000 charts, which were randomly identified from across the province and allows for good representation of Ontario’s socioeconomically and demographically diverse region. With linkage to ICES administrative data, it has been possible to link these carefully abstracted cases to physician billing information and health service utilization information and thereby provide detailed information about the state of youth with ADHD in North America. Children are identified as having ADHD if their primary health practitioner believes them to have ADHD, regardless of how the family physician came to this diagnosis (patient history, psychiatric consultation, psychoeducational assessment, screening questionnaires, etc.), and this has enabled a greater understanding of children with ADHD in Canada and how they are treated. A further strength of this study is that it includes all patients treated by family physicians, rather than studying prescriptions based on a particular prescriber, such as Medicaid, and is not limited to patients who are supported by social assistance.
However, there are several important methodological limitations when considering these data. This data set includes a broad sample of youth across rural and urban settings in a large and ethnically diverse Ontario province, but it does not include patients who exclusively see paediatricians for their medical care as this was a family physician/general practitioner EMR data set. This is likely not a significant limitation in Ontario because the vast majority of children and youth access family physicians for their primary health care,41 and the majority of mental health services are provided by family physicians in Ontario.42 It also does not include individuals who are not registered or rostered with a family physician and may include relatively fewer children who are in foster care or otherwise frequently moving within the province. This study shows only prescriptions, and the degree of medication adherence and whether or not the prescriptions were filled are not known. These are prescriptions provided or recorded by the family physician, and prescriptions from other providers are variably populated in the family physician EMR. The timing of prescriptions (sequential, overlapping) and duration of use are not known, limiting our ability to know if a patient was taking a medication such as bupropion before or after a trial of a stimulant or simultaneously. It should also be noted that oppositional defiant disorder, conduct disorder, and disruptive mood dysregulation disorder (added to the Diagnostic and Statistical Manual of Mental Disorders, 5th edition, in 2013) were not abstracted in this data set, and these diagnoses are often indications for antipsychotic prescription use. Further stratification of diagnosis, age, and sex within ADHD and non-ADHD cohorts would be of interest, but it was not possible as the numbers become too small to publish.
This study provides a unique perspective of youth with ADHD who receive treatment from their family physicians. By using family physician EMR data, this article is able to study those individuals who have a diagnosis of ADHD recorded in their primary care record. This study was generated from large, robust data, and manual review of charts was used to confirm the diagnoses. A significant number of youth with ADHD receive prescriptions for antipsychotics, and these youth suffer from significant psychiatric comorbidities. This subset of patients requires further study to determine the impact of antipsychotic medications on their overall health and the interventions that are most helpful in light of their complex psychiatric needs.
Supplementary Material
Acknowledgments
The authors gratefully acknowledge Dr. Liisa Jaakkimainen and Dr. Debra Butt for aiding in the development of the abstraction manual and validation of anxiety and depression cases. We also acknowledge Dr. Noah Ivers and Dr. Betty Lin for aiding in the development of the abstraction manual. The statistical expert was Cindy Lau. This study was supported by the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The opinions, results, and conclusions reported in this article are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred. Parts of this material are based on data and information compiled and provided by the CIHI. However, the analyses, conclusions, opinions, and statements expressed herein are those of the authors and not necessarily those of CIHI. The study was funded by the Mental Health and Addictions Strategy and Evaluation framework.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Funding was provided by the Institute for Clinical Evaluative Sciences and the Ontario Ministry of Health and Long-Term Care.
Supplemental Material: The online tables are available at http://journals.sagepub.com/doi/suppl/10.1177/0706743716689055.
References
- 1. Waddell C, Offord DR, Shepherd CA, Hua JM, McEwan K. Child psychiatric epidemiology and Canadian public policy-making: the state of the science and the art of the possible. Can J Psychiatry. 2002;47(9):825–32. [DOI] [PubMed] [Google Scholar]
- 2. Mannuzza S, Klein RG, Bessler A, Malloy P, Lapadula M. Adult psychiatric status of hyperactive boys grown up. Am J Psychiatry. 1998;155(4):493–498. [DOI] [PubMed] [Google Scholar]
- 3. Kessler RC, Adler L, Berkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006;163(4):716–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. McMartin SE, Kingsbury M, Dykxhoorn J, Colman I. Time trends in symptoms of mental illness in children and adolescents in Canada. CMAJ. 2014;186(18):E672–E678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Advokat CD, Guidry D, Martino L. Licit and illicit use of medications for attention-deficit hyperactivity disorder in undergraduate college students. J Am Coll Health. 2008;56(6):601–606. [DOI] [PubMed] [Google Scholar]
- 6. Cressman AM, Macdonald EM, Huang A, et al. Prescription stimulant use and hospitalization for psychosis or mania: a population-based study. J Clin Psychopharmacol. 2015;35(6):667–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Epstein JN, Kelleher KJ, Baum R, et al. Variability in ADHD care in community-based pediatrics. Pediatrics. 2014;134(6):1136–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Murphy JM, McCarthy AE, Baer L, Zima BT, Jellinek MS. Alternative national guidelines for treating attention and depression problems in children: comparison of treatment approaches and prescribing rates in the United Kingdom and United States. Harvard Rev Psychiatry. 2014;22(3):179–192. [DOI] [PubMed] [Google Scholar]
- 9. Aman MG, Bukstein OG, Gadow KD, et al. What does risperidone add to parent training and stimulant for severe aggression in child attention-deficit/hyperactivity disorder? J Am Acad Child Adolesc Psychiatry. 2014;53(1):47–60.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gorman DA, Gardner DM, Murphy AL, et al. Canadian guidelines on pharmacotherapy for disruptive and aggressive behaviour in children and adolescents with attention-deficit hyperactivity disorder, oppositional defiant disorder, or conduct disorder. Can J Psychiatry. 2015;60(2):62–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Pringsheim T, Hirsch L, Gardner D, Gorman DA. The pharmacological management of oppositional behaviour, conduct problems, and aggression in children and adolescents with attention-deficit hyperactivity disorder, oppositional defiant disorder, and conduct disorder: a systematic review and meta-analysis. Part 2: antipsychotics and traditional mood stabilizers. Can J Psychiatry. 2015;60(2):52–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lachaine J, De G, Sikirica V, et al. Treatment patterns, resource use, and economic outcomes associated with atypical antipsychotic prescriptions in children and adolescents with attention-deficit hyperactivity disorder in Quebec. Can J Psychiatry. 2014;59(11):597–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Daviss WB, Barnett E, Neubacher K, Drake RE. Use of antipsychotic medications for nonpsychotic children: risks and implications for mental health services. Psychiatr Serv. 2016;67(3):339–341. [DOI] [PubMed] [Google Scholar]
- 14. Tu K, Mitiku TF, Ivers NM, et al. Evaluation of Electronic Medical Record Administrative data Linked Database (EMRALD). Am J Manage Care. 2014;20(1):e15–e21. [PubMed] [Google Scholar]
- 15. Steele LS, Glazier RH, Lin E, Evans M. Using administrative data to measure ambulatory mental health service provision in primary care. Med Care. 2004;42(10):960–965. [DOI] [PubMed] [Google Scholar]
- 16. Harrel FE. Regression Modelling Strategies: With Applications to Linear Models, Logistic Regression and Survival Analysis. New York: Springer; 2010. [Google Scholar]
- 17. Brault MC, Lacourse É. Prevalence of prescribed attention-deficit hyperactivity disorder medications and diagnosis among canadian preschoolers and school-age children: 1994-2007. Can J Psychiatry. 2012;57(2):93–101. [DOI] [PubMed] [Google Scholar]
- 18. Canino G, Shrout PE, Rubio-Stipec M, et al. The DSM-IV rates of child and adolescent disorders in Puerto Rico: prevalence, correlates, service use, and the effects of impairment. Arch Gen Psychiatry. 2004;61(1):85–93. [DOI] [PubMed] [Google Scholar]
- 19. Chen CY, Liu CY, Su WC, Huang SL, Lin KM. Factors associated with the diagnosis of neurodevelopmental disorders: a population-based longitudinal study. Pediatrics. 2007;119(2):e435–e443. [DOI] [PubMed] [Google Scholar]
- 20. Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry. 2003;60(8):837–844. [DOI] [PubMed] [Google Scholar]
- 21. Elberling H, Linneberg A, Olsen EM, Goodman R, Skovgaard AM. The prevalence of SDQ-measured mental health problems at age 5-7 years and identification of predictors from birth to preschool age in a Danish birth cohort: the Copenhagen Child Cohort 2000. Eur Child Adolesc Psychiatry. 2010;19(9):725–735. [DOI] [PubMed] [Google Scholar]
- 22. Knight TK, Kawatkar A, Hodgkins P, et al. Prevalence and incidence of adult attention deficit/hyperactivity disorder in a large managed care population. Curr Med Res Opin. 2014;30(7):1291–1299. [DOI] [PubMed] [Google Scholar]
- 23. Merikangas KR, He JP, Brody D, Fisher PW, Bourdon K, Koretz DS. Prevalence and treatment of mental disorders among US children in the 2001-2004 NHANES. Pediatrics. 2010;125(1):75–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Polanczyk G, De Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry. 2007;164(6):942–948. [DOI] [PubMed] [Google Scholar]
- 25. Roberts RE, Roberts CR, Xing Y. Rates of DSM-IV psychiatric disorders among adolescents in a large metropolitan area. J Psychiatr Res. 2007;41(11):959–967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ullebø AK, Posserud MB, Heiervang E, Obel C, Gillberg C. Prevalence of the ADHD phenotype in 7-to 9-year-old children: effects of informant, gender and non-participation. Soc Psychiatry Psychiatr Epidemiol. 2012;47(5):763–769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Vande Voort JL, He JP, Jameson ND, Merikangas KR. Impact of the DSM-5 attention-deficit/hyperactivity disorder age-of-onset criterion in the us adolescent population. J Am Acad Child Adolesc Psychiatry. 2014;53(7):736–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ben Amor L, Sikirica V, Cloutier M, et al. Combination and switching of stimulants in children and adolescents with attention deficit/hyperactivity disorder in Quebec. J Can Acad Child Adolesc Psychiatry. 2014;23(3):157–166. [PMC free article] [PubMed] [Google Scholar]
- 29. Kamble P, Chen H, Johnson ML, Bhatara V, Aparasu RR. Concurrent use of stimulants and second-generation antipsychotics among children with ADHD enrolled in medicaid. Psychiatr Serv. 2015;66(4):404–410. [DOI] [PubMed] [Google Scholar]
- 30. Pulcini CD, Perrin JM, Houtrow AJ, Sargent J, Shui A, Kuhlthau K. Examining trends and coexisting conditions among children qualifying for SSI under ADHD, ASD, and ID. Acad Pediatr. 2015;15(4):439–443. [DOI] [PubMed] [Google Scholar]
- 31. Merikangas KR, He JP, Burstein M, et al. Lifetime prevalence of mental disorders in U.S. adolescents: results from the national comorbidity survey replication-adolescent supplement (NCS-A). J Am Acad Child Adolesc Psychiatry. 2010;49(10):980–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Yallop L, Brownell M, Chateau D, et al. Lifetime prevalence of attention-deficit hyperactivity disorder in young adults: examining variations in the socioeconomic gradient. Can J Psychiatry. 2015;60(10):434–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Bloom B, Jones LI, Freeman G. Summary Health Statistics for U.S. children: National Health Interview Survey, 2012. Vital and Health Statistics, Series 10: Data from the National Health Survey. Rockville (MD): National Center for Health Statistics; 2014. [PubMed] [Google Scholar]
- 34. Pringsheim T, Lam D, Patten SB. The pharmacoepidemiology of antipsychotic medications for canadian children and adolescents: 2005-2009. J Child Adolesc Psychopharmacol. 2011;21(6):537–543. [DOI] [PubMed] [Google Scholar]
- 35. Betts KA, Sikirica V, Hodgkins P, et al. Period prevalence of concomitant psychotropic medication usage among children and adolescents with attention-deficit/hyperactivity disorder during 2009. J Child Adoles Psychopharmacol. 2014;24(5):260–268. [DOI] [PubMed] [Google Scholar]
- 36. Vitiello B, Lazzaretto D, Yershova K, et al. Pharmacotherapy of the Preschool ADHD Treatment Study (PATS) children growing up. J Am Acad Child Adolesc Psychiatry. 2015;54(7):550–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Olfson M, King M, Schoenbaum M. Treatment of young people with antipsychotic medications in the united states. JAMA Psychiatry. 2015;72(9):867–874. [DOI] [PubMed] [Google Scholar]
- 38. Kendall J, Leo MC, Perrin N, Hatton D. Service needs of families with children with ADHD. J Fam Nurs. [Article]. 2005;11(3):264–288. [DOI] [PubMed] [Google Scholar]
- 39. Efron D, Moisuc O, McKenzie V, Sciberras E. Service use in children aged 6-8 years with attention deficit hyperactivity disorder. Arch Dis Child. 2016;101(2):161–165. [DOI] [PubMed] [Google Scholar]
- 40. Bobo WV, Cooper WO, Stein CM, et al. Antipsychotics and the risk of type 2 diabetes mellitus in children and youth. JAMA Psychiatry. 2013;70(10):1067–1075. [DOI] [PubMed] [Google Scholar]
- 41. Guttmann A, Manuel D, Dick PT, To T, Lam K, Stukel TA. Volume matters: physician practice characteristics and immunization coverage among young children insured through a universal health plan. Pediatrics. 2006;117(3):595–602. [DOI] [PubMed] [Google Scholar]
- 42. Gandhi S, Chiu M, Lam K, Cairney JC, Guttmann A, Kurdyak P. Mental health service use among children and youth in Ontario: population-based trends over time. Can J Psychiatry. 2016;61(2):119–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.