Abstract
Background:
Femoroacetabular impingement (FAI) is a well-recognized condition that causes hip pain and can lead to early osteoarthritis if not managed properly. With the increasing awareness and efficacy of operative treatments for pincer-type FAI, there is a need for consensus on the standardized radiographic diagnosis.
Purpose:
To perform a systematic review of the evidence regarding imaging modalities and radiographic signs for diagnosing pincer-type FAI.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A literature review was performed in 2016 using the Cochrane, PubMed, and Embase search engines. All articles focusing on a radiographic diagnosis of pincer-type FAI were reviewed. Each of the included 44 articles was assigned the appropriate level of evidence, and the particular radiographic marker and/or type of imaging were also summarized.
Results:
There were 44 studies included in the final review. Most of the articles were level 4 evidence (26 articles), and there were 12 level 3 and 6 level 2 articles. The crossover sign was the most commonly used radiographic sign (27/44) followed by the lateral center-edge angle (22/44). Anteroposterior (AP) pelvis plain radiographs were the most commonly used imaging modality (33 studies). Poor-quality evidence exists in support of most currently used radiographic markers, including the crossover sign, lateral center-edge angle, posterior wall sign, ischial spine sign, coxa profunda, acetabular protrusion, and acetabular index. There is poor-quality conflicting evidence regarding the use of the herniation pit to diagnose pincer-type FAI. Some novel measurements, such as β-angle, acetabular roof ratio, and acetabular retroversion index, have been proposed, but they also lack support from the literature.
Conclusion:
No strong evidence exists to support a single best set of current radiographic markers for the diagnosis of pincer-type FAI, largely due to the lack of better quality trials (levels 1 and 2) that compare conventional radiographic findings with the gold standard, which is the intraoperative findings. More sophisticated imaging modalities such as computed tomography and magnetic resonance arthrography are often needed to diagnose pincer-type FAI, and these investigations are relatively accurate in assessing labral pathology or cartilage damage.
Keywords: femoroacetabular impingement (FAI), pincer impingement, hip impingement, radiographic diagnosis
Femoroacetabular impingement (FAI) has been recently recognized as a cause of hip pain in young adult and middle-age populations and can potentially contribute to early hip osteoarthritis.3,16 FAI is associated with deformities in the proximal femur, the acetabulum, or both, which leads to impingement symptoms within the functional range of motion of the hip joints.3,36,44 FAI is categorized into 2 subgroups based on the location of the deformity. A cam-type impingement is caused by a decreased femoral head to neck ratio where the abnormally large femoral neck impinges on the acetabular rim.16 On the other hand, a pincer-type impingement is caused by overcoverage of the acetabulum.3
Accurate diagnosis of FAI is crucial to provide appropriate treatment. Thorough clinical examinations combined with proper radiographic findings are necessary for accurate diagnosis. Radiographic findings for a cam-type impingement are well established and include the increased alpha angle, decreased femoral head to neck ratio, and pistol-grip deformity.6,36 Radiographic findings suggestive of a pincer impingement include acetabular retroversion (crossover sign, posterior wall sign, and ischial spine sign) and coxa profunda.11,46 Both cadaveric and clinical studies have suggested that the accuracy of the crossover sign and the posterior wall sign can be limited by pelvic tilt.44,50 In addition, coxa profunda does not appear to correlate with overcoverage of the acetabulum.1
The current study is a systematic literature review of all articles that contain diagnostic imaging modalities and radiographic findings for pincer-type FAI. This literature search aims to serve 3 purposes. First, it will allow us to assess the prevalence of each imaging modality and radiographic finding in the current literature. Second, we aim to increase the potential for a recommended set of imaging modalities for initial consultations to standardize the diagnostic tools for pincer-type FAI. Finally, this systematic literature review could help suggest the direction of future research for diagnostic tools for pincer-type FAI.
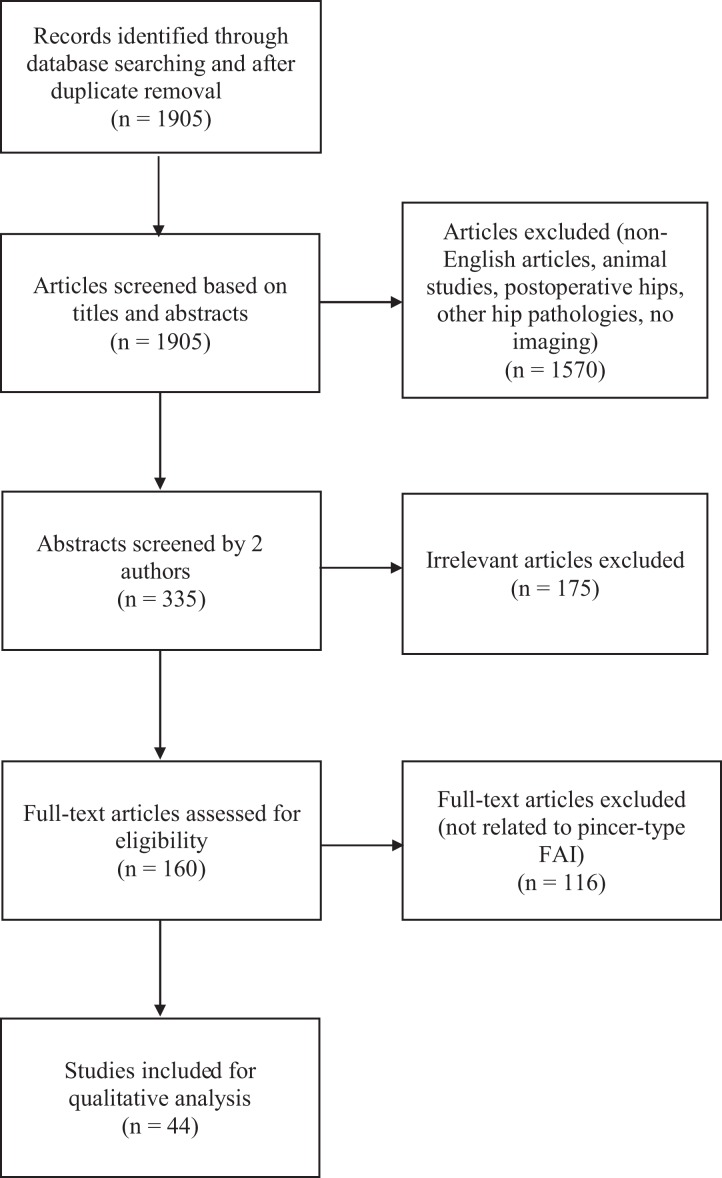
Methods
A systematic literature search was performed in July 2016 using Cochrane, PubMed, and Embase search engines. In the Cochrane search, the terms “femoroacetabular,” “femoro-acetabular,” and “hip impingement” were used, and this resulted in the total of 63 articles. The term “femoroacetabular impingement” came into use in the Medical Subject Headings (MeSH) thesaurus in the PubMed database in 2011. Prior to that, it was indexed as either acetabulum (1999-2010) or hip joint (2001-2010). The first search was performed using either “acetabulum” [MeSH] or “hip joint” [MeSH] and “impingement.” The second search used either “femoroacetabular,” “femoro-acetabular,” or “femoro acetabular” and “impingement.” After duplicates were removed, the PubMed and Embase searches yielded a total of 1905 articles. The Embase search was performed using “femoroacetabular impingement” and “diagnostic imaging” as search terms, and no new articles were added. Articles not in English were excluded, as well as articles on other hip pathologies (eg, tumor, trauma, neuromuscular disorder, slipped capital femoral epiphysis, Legg-Calve-Perthes disease), postoperative hips (eg, hip arthroplasty, pelvic osteotomy, posttrauma), and animal studies. The titles and/or the abstracts were reviewed to identify studies that included any type of imaging modality. This process was done by 2 authors (C.R. and T.L.), and when there was disagreement between the authors, the articles were included for full-text review to prevent exclusion of potentially relevant articles. This resulted in 335 articles that underwent further review. The abstracts were reviewed by the same 2 authors to exclude articles that were specific to cam-type FAI, review articles, those related to other hip pathologies, or those not containing any imaging modalities. Again, any articles where there was disagreement between the 2 authors were included for full-text review. All articles that did not describe pincer-type FAI or did not have any information about imaging modalities were excluded. The final 44 articles were summarized in a format that was agreed upon by all authors. The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram (Figure 1) reports the total number of included studies throughout the screening process.
Figure 1.
Flowchart summarizing the study selection based on PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines.32
The following information from each article was extracted: author, year of publication, title, type of study, level of evidence, demographics, imaging modalities, radiographic markers, and interpretation of the study. The level of evidence of each article was determined by the criteria described by Wright et al52 (Table 1). In addition, each radiographic marker was graded using the Grades of Recommendations guideline, also described by Wright et al52 (Table 2).
TABLE 1.
Levels of Evidence for Diagnostic Studies52
| Levels of Evidence for Diagnostic Studies | |
|---|---|
| Level 1 | Testing of previously developed diagnostic criteria in a series of consecutive patients (with universally applied reference “gold” standard); systematic review of level 1 studies |
| Level 2 | Development of diagnostic criteria on basis of consecutive patients (with universally applied reference “gold” standard); systematic review of levels 1 and 2 studies |
| Level 3 | Study of nonconsecutive patients (no consistently applied reference “gold” standard); systematic review of level 1 to 3 studies |
| Level 4 | Case-control study; poor reference standard |
| Level 5 | Expert opinion |
TABLE 2.
Grades of Recommendations for Investigations
| Grades of recommendation | Description |
|---|---|
| A | Good evidence (level 1 studies with consistent findings) for or against recommending investigations |
| B | Fair evidence (level 2 or 3 studies with consistent findings) for or against recommending investigations |
| C | Conflicting or poor-quality evidence (level 4 or 5 studies) not allowing a recommendation for or against investigations |
| I | Insufficient evidence to make a recommendation |
| Proposed subscale | |
| Cf | Representing literature “for,” or in support of, an investigation |
| Ca | Representing literature “against,” or not in support of, an investigation |
| Cc | Representing conflicting literature, some of which is in support of an investigation and some of which is not in support of an investigation |
Results
Of the final 44 articles reviewed, there were 6 level 2 studies, 12 level 3 studies, and 26 level 4 studies. The majority of studies were noncomparative retrospective studies. The most frequently used plain radiograph was an anteroposterior (AP) view of the pelvis. Other radiographs include cross-table lateral, frog-leg lateral, and false profile views. Multiple radiographic findings suggestive of pincer-type FAI were identified through the literature search. Six articles conducted studies on patients who had undergone either hip dislocation surgery or arthroscopy and utilized intraoperative information in varying degrees. The summary of the level of evidence, imaging modalities, and radiographic markers in each study is shown in Table 3. The frequency of each of the radiographic markers used to diagnose pincer-type FAI is summarized in Table 4.
TABLE 3.
Summary of Imaging Modalities and Radiographic Signs Used in the Articles Included in the Final Analysisa
| Authors (Year) | Level of Evidence and Type of Study | Sample Size | Images | COS | PWS | ISS | Coxa Profunda | Acetabular Protrusio | Herniation Pit | CEA | AI | Other |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Beck et al (2005)3 | Retrospective, level 4 | 54 hips | AP, cross-table | Yes | Yes | Yes | ||||||
| Pfirrmann et al (2006)40 | Retrospective, level 4 | 17 pts (17 hips) | MRA | Yes | ||||||||
| Guevara et al (2006)19 | Retrospective, level 4 | 94 pts (99 hips) | AP, frog-leg | Yes | Yes | Yes | Acetabular depth-to-width index | |||||
| Tannast et al (2007)48 | Retrospective, level 4 | 67 hips (36 control, 31 FAI, 7 pincer) | SuAP, cross-table, CT | |||||||||
| Kalberer et al (2008)24 | Retrospective, level 4 | 149 pts (298 hips) | AP | Yes | Yes | Crossover ratio | ||||||
| Panzer et al (2008)38 | Retrospective, level 4 | 200 pts, avg 55.5 y old | CT | Yes | Yes | |||||||
| Martinez et al (2006)33 | Retrospective, level 4 | 498 pts | AP, MRA | Yes | Yes | Yes | ||||||
| Dandachli et al (2009)11 | Retrospective, level 3 | 33 pts (64 hips), avg 28 y old | AP, CT | Yes | Yes | Yes (CT) | ||||||
| Gu et al (2009)18 | Prospective, level 4 | 17 pts (34 hips) | AP, cross-table, CT, MRI | Yes | ||||||||
| Arbabi et al (2010)2 | Simulation, level 4 | 25 models | ||||||||||
| Ochoa et al (2010)37 | Retrospective, level 4 | 73 pts | AP, frog-leg | Yes | Yes (LCEA ≥39) | |||||||
| Hong et al (2010)21 | Retrospective, level 4 | 8 pts | AP, frog-leg, MRA | Yes | Yes | Yes (MRA) | ||||||
| Kappe et al (2011)25 | Retrospective, level 4 | 20 pts (40 hips), avg 26 y old | SuAP | Yes | Yes | Yes | ||||||
| Kim et al (2011)26 | Retrospective, level 4 | 62 pts (80 hips) | AP | Yes | Yes | Yes (LCEA >40) | Yes (≤0) | Extrusion index <25% | ||||
| Werner et al (2010)51 | Retrospective, level 4 | 1350 hips | AP | Yes | Yes | Yes | ||||||
| Brunner et al (2010)7 | Retrospective, level 4 | 50 pts (avg 35 y old), 50 controls | β-view | Yes (>40) | β-angle | |||||||
| Bellaiche et al (2010)4 | Prospective, level 4 | 65 pts with pincer | StAP, MRA | Yes | Yes | |||||||
| Corten et al (2011)10 | Retrospective, level 4 | 121 pts (148 hips) | AP, cross-table, MRA | Yes | Yes | Yes (LCEA) | Extrusion index, recess sign, double-line sign | |||||
| Laborie et al (2011)29 | Prospective, level 4 | 2060 pts (4080 hips) | StAP, frog-leg | Yes | Yes | Excessive acetabular coverage | ||||||
| Kutty et al (2012)28 | Retrospective, level 3 | 19 pts (19 hips), 30 controls | AP, cross-table | Yes (LCEA ≥40) | ||||||||
| Carlisle et al (2011)8 | Retrospective, level 4 | 45 hips | AP, cross-table, frog-leg | Yes (LCEA) | ||||||||
| Botser et al (2012)6 | Retrospective, level 3 | 121 pts (129 hips) | AP, cross-table, false-profile, CT, MRI | Yes | Yes | Yes | Anteversion on CT and MRI | |||||
| Sutter et al (2012)46 | Prospective, level 4 | 63 pts (30 pincer), 63 controls | SuAP, MRI | Yes | Yes | Yes | Yes | MRI for femoral anteversion | ||||
| Wassilew et al (2012)50 | Retrospective, level 3 | 25 pts (50 hips, 26 pincer) | SuAP, CT | Yes | Yes | CT for acetabular version | ||||||
| Dandachli et al (2012)12 | Retrospective, level 3 | 15 hips, 16 controls | AP, CT (3D recon) | Yes (on CT, LCEA, ACEA, PCEA, A+P CEA) | ||||||||
| Ranawat et al (2011)41 | Retrospective, level 4 | 100 pts (100 hips, 57 pincer) | AP, cross-table | Yes | Yes | Yes | Yes | Yes | ||||
| Anderson et al (2012)1 | Retrospective, level 3 | 175 pts (179 hips), 67 controls (134 hips) | AP, false profile | Yes | Yes | Yes | Yes | Yes (LCEA >40) | Yes (<0) | |||
| Boone et al (2012)5 | Retrospective, level 2 | 144 hips (52 pincer) | SuAP | Yes | Yes (LCEA >35) | Acetabular roof ratio, intraoperative findings | ||||||
| Stelzeneder et al (2013)45 | Retrospective, level 3 | 103 pts (103 hips, 46 pincer) | AP, false profile, MRI | Yes | Yes | Yes (on AP and false profile, also MRI) | Extrusion index | |||||
| Nepple et al (2013)34 | Retrospective, level 4 | 150 hips (50 pincer) | AP | Yes | Yes (LCEA >40) | |||||||
| Tibor et al (2013)49 | Retrospective, level 4 | 112 hips (41 pincer) | AP, MRA | Yes | Yes | Yes (LCEA >35) | ||||||
| de Bruin et al (2013)13 | Retrospective, level 4 | 262 pts (522 hips) | SuAP | Yes | Yes | Yes | Yes | |||||
| Diaz-Ledezma et al (2013)14 | Retrospective, level 2 | 93 pts | AP | Yes | Yes | Yes | Acetabular retroversion index, intraoperative findings | |||||
| Schmitz et al (2013)43 | Retrospective, level 3 | 180 hips, avg 16 y old | StAP (EOS) | Yes | Yes | Yes | Yes | Yes (LCEA ≥39) | ||||
| Henebry and Gaskill (2013)20 | Cadaveric, level 4 | 8 hips | AP | Yes | Yes (LCEA) | |||||||
| Ji et al (2014)23 | Retrospective, level 4 | 151 pts (151 hips), 151 controls | CT arthro | Yes | Yes (LCEA >39) | Central acetabular version, cranial acetabular version | ||||||
| Sutter et al (2014)47 | Prospective, level 2 | 28 pts | MRA, MRI | Intraoperative findings | ||||||||
| Lattanzi et al (2014)31 | Retrospective, level 3 | 20 pts | dGEMRIC at 3 T | Intraoperative findings | ||||||||
| Sahin et al (2014)42 | Prospective, level 2 | 14 pts | CT arthro, MRA | Intraoperative findings | ||||||||
| Petchprapa et al (2015)39 | Prospective, level 2 | 14 pts | Direct and indirect MRA | Intraoperative findings | ||||||||
| Diesel et al (2015)15 | Retrospective, level 2 | 129 pts (257 hips) | AP | Yes | Yes | Yes (LCEA >40) | Yes (<0) | |||||
| Nissi et al (2015)35 | Prospective, level 3 | 10 pts | MRI, MRA | |||||||||
| González Gil et al (2015)17 | Retrospective, level 3 | 36 pts | MRA | Intraoperative findings | ||||||||
| Jackson et al (2016)22 | Retrospective, level 3 | 46 pts | SuAP, StAP | Yes | Yes | Yes (LCEA) | Yes | Tip-symphysis distance, sacrococcygeal-symphysis distance |
a3D, 3-dimensional; ACEA, anterior center-edge angle; AI, acetabular index; AP, anteroposterior pelvis, position unspecified; CEA, center-edge angle; COS, crossover sign; CT, computed tomography; dGEMRIC, delayed gadolinium-enhanced magnetic resonance imaging of cartilage; EOS, EOS imaging system (low-dose, 3D imaging technology); ISS, ischial spine sign; LCEA, lateral center-edge angle; MRA, magnetic resonance arthrography; MRI, magnetic resonance imaging; PCEA, posterior center-edge angle; PWS, posterior wall sign; pts, patients; StAP, standing AP pelvis; SuAP, supine AP pelvis.
TABLE 4.
Frequency of the Radiographic Markers Used Based on the Level of Evidence of the Articlea
| COS | PWS | ISS | Coxa Profunda | Acetabular Protrusio | HP | CEA | AI | |
|---|---|---|---|---|---|---|---|---|
| Level 2 | 2 | 1 | 1 | 2 | 0 | 0 | 2 | 1 |
| Level 3 | 7 | 4 | 2 | 3 | 3 | 0 | 7 | 2 |
| Level 4 | 18 | 7 | 6 | 4 | 5 | 6 | 13 | 3 |
| Total | 27 | 12 | 9 | 9 | 7 | 6 | 22 | 6 |
aAI, acetabular index; CEA, center-edge angle; COS, crossover sign; HP, herniation pit; ISS, ischial spine sign; PWS, posterior wall sign.
AP pelvis plain radiographs were utilized in 33 studies, making it the most frequently used imaging modality. Most studies did not specify whether these radiographs were taken in a standing or supine position. For the studies that did specify, 7 utilized supine films while 4 utilized standing AP pelvis films. Among the 33 studies, crossover signs were used in 27 articles (82%), lateral center-edge angle in 22 articles (67%), posterior wall sign in 12 articles (36%), coxa profunda in 9 articles (27%), and ischial spine sign in 9 articles (27%).
The center-edge angle was the most commonly used sign for acetabular overcoverage, utilized in 22 articles with plain radiographs, 2 articles with computed tomography (CT), and 1 article with magnetic resonance imaging (MRI). A center-edge angle greater than 35° to 40° was used as the criterion in most articles. The acetabular index was another marker for acetabular overcoverage, which was used in 4 studies. An acetabular index of 0 or less on AP pelvis radiographs was used to indicate overcoverage of the lateral acetabulum.1,26 Diagrams of each of the radiographic markers are shown in Figure 2.
Figure 2.
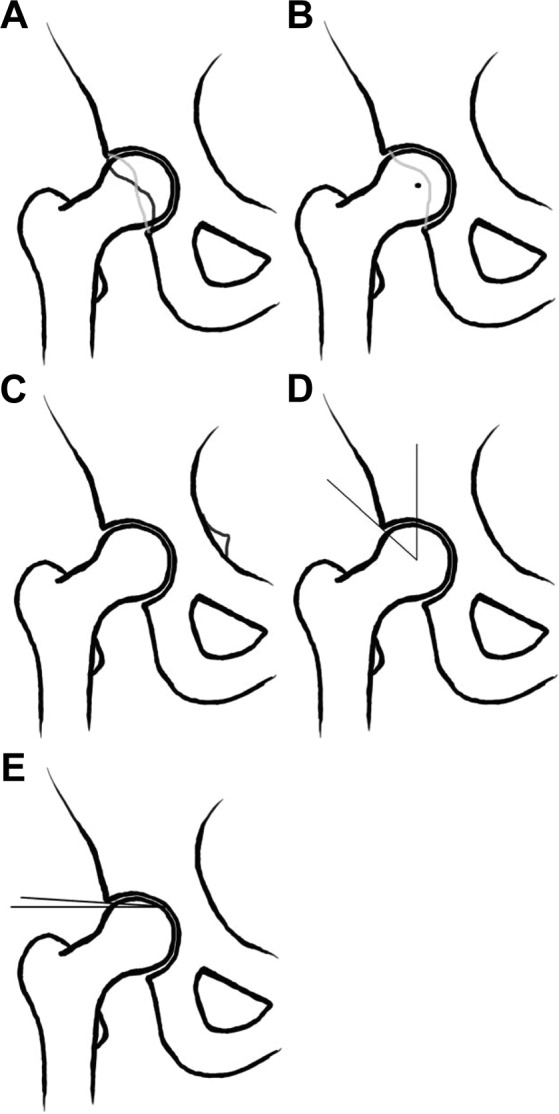
Commonly used radiographic markers for pincer-type femoroacetabular impingement. (A) Crossover sign, (B) posterior wall sign, (C) ischial spine sign, (D) center-edge angle, and (E) acetabular index.
Discussion
Femoroacetabular impingement is a well-recognized phenomenon that commonly causes pain in young populations and potentially leads to early osteoarthritis of the hip.16 Despite its clinical relevance, accurate diagnosis can be challenging as the screening imaging modalities are plain radiographs, which can only show a 2-dimensional snapshot of the dynamic 3-dimensional pathology. As mentioned previously, the challenge is more apparent in diagnosing pincer-type impingement, as the accuracy of the radiographic markers and imaging tools is more questionable. Consequently, there are no standardized, evidence-supported sets of diagnostic tools for pincer-type impingement.
The majority of the studies used radiographic parameters in plain radiographs to diagnose pincer-type FAI. The 3 most commonly used radiographic markers for pincer-type impingement were the crossover sign, posterior wall sign, and ischial spine sign. However, the accuracy of these radiographic signs was questioned in multiple studies. Kappe et al25 calculated the interobserver reliability of crossover sign, posterior wall sign, and ischial spine sign among 5 orthopaedic surgeons who perform approximately 200 hip-preserving operations annually. Intraobserver reliability was only moderate for crossover, posterior wall, and the ischial spine signs, with correlation coefficients of 0.514, 0.633, and 0.543, respectively. In addition, the assessment of acetabular version was related to the self-reported observer’s experiences.25 In addition, the study by Bellaiche et al4 showed that the crossover sign from AP pelvis radiographs was poorly correlated with acetabular version obtained using magnetic resonance arthrography (MRA), with a sensitivity of 23% and specificity of 84%. Wassilew et al50 conducted a similar study to assess the accuracy of the crossover sign and the posterior wall sign by comparing plain radiography with CT. Both the radiographic markers showed poor sensitivity and specificity and were limited by pelvic tilt and inherent inaccuracy associated with plain radiographs.50 The only study that used intraoperative findings as a gold standard to assess the accuracy of those radiographic markers was a retrospective study conducted by Diaz-Ledezma et al,14 and their study found that these markers do not correlate with intraoperatively found chondral damage.14 Although some studies show the accuracy of findings obtained from plain radiographs,10,11,33,45,46 diagnosing patients solely on radiographic findings may yield inaccuracies.
The center-edge angle is another commonly used radiographic marker to assess the overcoverage of the acetabulum. The lateral center-edge angle showed high intraobserver reliability8 and was shown to correlate with pincer-type FAI.11,28,45 The cutoff to diagnose acetabular overcoverage varied between 35° and 40°, but an angle greater than 40° was the most commonly used criterion in the literature.
Several studies compared the accuracy of 1 imaging modality over another, and the results are inconsistent. Corten et al10 compared radiographic signs from plain radiographs such as crossover sign, ischial spine sign, and lateral center-edge angle, which correlated well with MRA findings in terms of pincer morphology. Similarly, Stelzeneder et al45 also conducted a study that compares commonly used radiographic markers from plain radiographs, such as crossover sign, posterior wall sign, and center-edge angle, with MRI findings and found that all radiographic measurements correlated with those from MRI. Also, a study by Werner et al51 showed that the radiographic markers, namely crossover sign, posterior wall sign, and ischial spine sign, correlate well with one another. Unfortunately, some studies have found contradicting results. Bellaiche et al4 found that the crossover sign does not correlate with acetabular retroversion seen on MRA. A study by Wassilew et al50 also showed that crossover sign and posterior wall sign are not accurate markers to assess for acetabular version when compared with CT findings. In addition, a study by Diaz-Ledezma et al14 concluded that crossover sign, posterior wall sign, and ischial spine sign do not correlate with chondral damages that are identified intraoperatively, which reliably predicts symptomatic pincer-type FAI. Herniation pit is an occasionally utilized radiographic marker to diagnose FAI, but its correlation with pincer-type impingement is unclear. In the current systematic literature review, 1 study supported the use of herniation pit while 1 study did not find association with pincer-type impingement.23,26
There are several studies that have suggested novel radiographic markers to help diagnose pincer-type impingement. A study by Boone et al5 introduced acetabular roof ratios that were shown to correlate with acetabular overcoverage. The acetabular roof ratio is measured by drawing a line from the lateral edge of the acetabulum parallel to a line drawn between the centers of the femoral heads. Roof 1 is measured from the lateral edge of the sourcil until the point this line intersects with the sourcil medially. Roof 2 is measured from the end of the previous line until it reaches the ilioischial (Figure 3).5 In addition, Diaz-Ledezma et al14 introduced the acetabular retroversion index as a marker to assess the version, which is a ratio calculated by the crossover point between the anterior and posterior walls (Figure 4).14 Other markers include the extrusion index, recess sign, double-line sign, and β-angle, which are all potentially useful radiographic parameters but lack evidence to support their validity.7,10,45 In addition, a study by Larson et al30 showed a novel approach for measuring acetabular coverage using CT scanning. This approach can provide valuable information about the acetabular overcoverage and likelihood of pincer impingement when the plain radiographic findings are equivocal.
Figure 3.
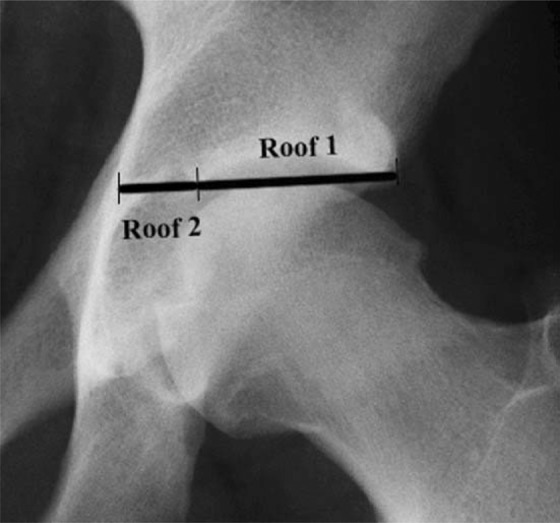
Two different acetabular roof ratios were introduced in the study by Boone et al.5 The first ratio is calculated by dividing the total roof length (roof 1 + roof 2) by roof 2, and the other by dividing roof 1 by roof 2.
Figure 4.
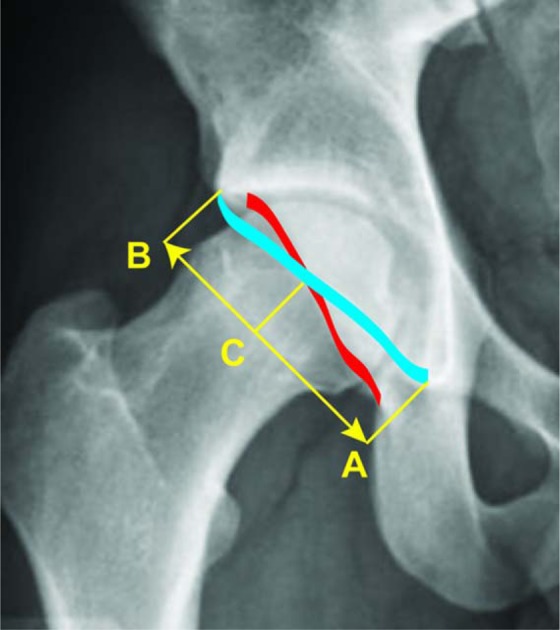
The acetabular retroversion index is calculated by dividing BC by AB then multiplying by 100.14 (A) Medial aspect of the anterior rim, (B) lateral edge of the acetabulum, and (C) crossover point.
Recent studies utilized more advanced imaging techniques such as CT arthrography and MRA and assessed their accuracy compared with the intraoperative findings of labral tear or chondral damage, which serves as the gold standard. Sutter et al47 compared the accuracy of MRA and conventional MRI using the intraoperative findings of labral tear and acetabular cartilage damage as a reference and concluded that MRA is more accurate. A study by Sahin et al42 compared the accuracy of CT arthrography and MRA based on intraoperative findings and showed that both are accurate in detecting labral tears and cartilage pathologies. Despite the potential utility of CT arthrography, plain radiographs and MRI are the traditionally accepted imaging methods, with more studies supporting the use of these imaging modalities compared with CT arthrography. Another retrospective study by González Gil et al17 proves the accuracy of MRA when compared with the intraoperative findings.
Overall, the current systematic literature search has shown that the currently utilized markers from plain radiographs can be inaccurate and must be used in conjunction with thorough clinical examinations and appropriate advanced imaging modalities. It is also important to note that radiographic findings of pincer-type impingement are common in asymptomatic populations.13,43 In addition, a cadaveric study by Henebry and Gaskill20 showed that pelvic tilt significantly alters the measurements of crossover sign and lateral center-edge angle, which are the most commonly used radiographic parameters. Consequently, the recommendation for appropriate pelvic radiographs is to standardize the distance between the sacrococcygeal joint and pubic symphysis to 3 to 4 cm.9 However, the physiologic pelvic tilt is also altered significantly when the AP pelvis radiograph is taken in an upright position as opposed to supine.27 Considering that upright pelvic radiographs may more closely represent the functional weightbearing position and orientation of the acetabulum and the femur, it is questionable whether it is clinically significant to artificially change the pelvic tilt to meet the diagnostic criteria.
In this study, we looked at the current literature and uses of different radiographic markers. Without strong evidence to support a single best radiographic marker, the findings from plain radiographs must be interpreted with caution and in conjunction with clinical findings. Based on common practice, we recommend AP pelvis radiography as the screening imaging modality, whether it be supine or standing, and recommend utilizing crossover sign, posterior wall sign, acetabular protrusion, and lateral center-edge angle. We cannot recommend appropriate lateral hip radiographs at this point based on the literature search. When either the clinical examinations or the radiographic parameters are equivocal, we recommend obtaining MRA or high-resolution conventional MRI scans to assess the 3-dimensional anatomy to analyze acetabular version and overcoverage, as well as to assess for cartilage damage.
Most of the radiographic markers are poorly supported by the literature and were given a grade Cf, except for the herniation pit, which was given a grade Cc recommendation as there was conflicting evidence in the literature. This is summarized in Table 5.
TABLE 5.
Summary of the Grades of Recommendations for the Commonly Used Radiographic Markers to Diagnose Pincer-Type Femoroacetabular Impingement
| Radiographic Markers | Level of Evidence | Grade of Recommendation With Proposed Subscale |
|---|---|---|
| Crossover sign | Most level 4 studies support its use, level 2 and 3 studies inconclusive | Cf |
| Posterior wall sign | Most level 4 studies support its use, level 2 and 3 studies inconclusive | Cf |
| Ischial spine sign | Most level 4 studies support its use, level 2 and 3 studies inconclusive | Cf |
| Center-edge angle | Most level 4 studies support its use, level 2 and 3 studies inconclusive | Cf |
| Acetabular index | Most level 4 studies support its use, level 2 and 3 studies inconclusive | Cf |
| Herniation pit | All level 4 studies show conflicting results | Cc |
The main limitation of the current systematic literature search was the limited number of studies that compared the accuracy of imaging modalities. Some studies have utilized CT scans and MRA as gold standards to assess the accuracy of plain radiographs. However, they only produce a static representation of a dynamic anatomy, and the accuracy of these imaging modalities must be investigated as well. Therefore, future studies are required not only to assess the accuracy of commonly used radiographic parameters from plan radiographs but also to assess the accuracy of advanced 3-dimensional images by comparing them with intraoperative findings. Ideally, these studies will measure all commonly used radiographic parameters from AP pelvis and cross-table lateral radiographs, and these findings will be compared with findings from MRA and direct visualization intraoperatively. Hopefully, future studies will be able to provide the algorithm for radiographic diagnosis of pincer impingement, thus minimizing unnecessary investigations and expediting the appropriate treatment for patients.
Conclusion
The current systematic literature review shows that the most frequently employed imaging modalities are AP pelvic plain radiographs followed by MRA. Cross-table lateral plain radiography is also used frequently. The 3 most frequently used radiographic signs, in order of decreasing frequency, are the crossover sign, center-edge angle, and posterior wall sign. The reliabilitiy of these radiographic signs was overall supported by the literature, and although the body of evidence is increasing, there is a lack of consensus due to a lack of high-quality studies. MRA was shown in multiple studies to be accurate in detecting labral tear and cartilage pathologies when compared with intraoperative findings. We recommend the use of AP pelvis and cross-table lateral radiographs for initial consultations, and the use of the crossover sign, center-edge angle, and posterior wall sign on both. MRA can be ordered when the initial plain radiographs and clinical findings are consistent with the pincer-type FAI.
Acknowledgment
The authors would like to acknowledge Nicole Paquet for her assistance with the production and editing of this article as well as her aid in the coordination of this systematic review.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Anderson LA, Kapron AL, Aoki SK, Peters CL. Coxa profunda: is the deep acetabulum overcovered? Clin Orthop Relat Res. 2012;470:3375–3382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Arbabi E, Chegini S, Boulic R, Tannast M, Ferguson SJ, Thalmann D. Penetration depth method—novel real-time strategy for evaluating femoroacetabular impingement. J Orthop Res. 2010;28:880–886. [DOI] [PubMed] [Google Scholar]
- 3. Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018. [DOI] [PubMed] [Google Scholar]
- 4. Bellaiche L, Lequesne M, Gedouin JE, Laude F, Boyer T. Imaging data in a prospective series of adult hip pain in under-50 year-olds. Orthop Traumatol Surg Res. 2010;96(suppl 8):S44–S52. [DOI] [PubMed] [Google Scholar]
- 5. Boone G, Pagnotto MR, Walker JA, Trousdale RT, Sierra RJ. Radiographic features associated with differing impinging hip morphologies with special attention to coxa profunda. Clin Orthop Relat Res. 2012;470:3368–3374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Botser IB, Ozoude GC, Martin DE, Siddiqi AJ, Kuppuswami S, Domb BG. Femoral anteversion in the hip: comparison of measurement by computed tomography, magnetic resonance imaging, and physical examination. Arthroscopy. 2012;28:619–627. [DOI] [PubMed] [Google Scholar]
- 7. Brunner A, Hamers AT, Fitze M, Herzog RF. The plain beta-angle measured on radiographs in the assessment of femoroacetabular impingement. J Bone Joint Surg Br. 2010;92:1203–1208. [DOI] [PubMed] [Google Scholar]
- 8. Carlisle JC, Zebala LP, Shia DS, et al. Reliability of various observers in determining common radiographic parameters of adult hip structural anatomy. Iowa Orthop J. 2011;31:52–58. [PMC free article] [PubMed] [Google Scholar]
- 9. Clohisy JC, Carlisle JC, Beaulé PE, et al. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90(suppl 4):47–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Corten K, Ganz R, Chosa E, Leunig M. Bone apposition of the acetabular rim in deep hips: a distinct finding of global pincer impingement. J Bone Joint Surg Am. 2011;93(suppl 2):10–16. [DOI] [PubMed] [Google Scholar]
- 11. Dandachli W, Ul Islam S, Liu M, Richards R, Hall-Craggs M, Witt J. Three-dimensional CT analysis to determine acetabular retroversion and the implications for the management of femoro-acetabular impingement. J Bone Joint Surg Br. 2009;91:1031–1036. [DOI] [PubMed] [Google Scholar]
- 12. Dandachli W, Najefi A, Iranpour F, Lenihan J, Hart A, Cobb J. Quantifying the contribution of pincer deformity to femoro-acetabular impingement using 3D computerised tomography. Skeletal Radiol. 2012;41:1295–1300. [DOI] [PubMed] [Google Scholar]
- 13. de Bruin F, Reijnierse M, Farhang-Razi V, Bloem JL. Radiographic signs associated with femoroacetabular impingement occur with high prevalence at all ages in a hospital population. Eur Radiol. 2013;23:3131–3139. [DOI] [PubMed] [Google Scholar]
- 14. Diaz-Ledezma C, Novack T, Marin-Peña O, Parvizi J. The relevance of the radiological signs of acetabular retroversion among patients with femoroacetabular impingement. Bone Joint J. 2013;95-B:893–899. [DOI] [PubMed] [Google Scholar]
- 15. Diesel CV, Ribeiro TA, Caussirat C, Scheidt RB, Macedo CA, Galia CR. Coxa profunda in the diagnosis of pincer-type femoroacetabular impingement and its prevalence in asymptomatic subjects. Bone Joint J. 2015;97-B:478–483. [DOI] [PubMed] [Google Scholar]
- 16. Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. [DOI] [PubMed] [Google Scholar]
- 17. González Gil AB, Llombart Blanco R, Díaz de Rada P. Validity of magnetic resonance arthrography as a diagnostic tool in femoroacetabular impingement syndrome. Rev Esp Cir Ortop Traumatol. 2015;59:281–286. [DOI] [PubMed] [Google Scholar]
- 18. Gu GS, Zhu D, Wang G, Wang CX. Roles of radiograph, magnetic resonance imaging, three-dimensional computed tomography in early diagnosis of femoro-acetabular impingement in 17 cases. Chin J Traumatol. 2009;12:375–378. [PubMed] [Google Scholar]
- 19. Guevara CJ, Pietrobon R, Carothers JT, Olson SA, Vail TP. Comprehensive morphologic evaluation of the hip in patients with symptomatic labral tear. Clin Orthop Relat Res. 2006;453:277–285. [DOI] [PubMed] [Google Scholar]
- 20. Henebry A, Gaskill T. The effect of pelvic tilt on radiographic markers of acetabular coverage. Am J Sports Med. 2013;41:2599–2603. [DOI] [PubMed] [Google Scholar]
- 21. Hong SJ, Shon WY, Lee CY, Myung JS, Kang CH, Kim BH. Imaging findings of femoroacetabular impingement syndrome: focusing on mixed-type impingement. Clin Imaging. 2010;34:116–120. [DOI] [PubMed] [Google Scholar]
- 22. Jackson TJ, Estess AA, Adamson GJ. Supine and standing AP pelvis radiographs in the evaluation of pincer femoroacetabular impingement. Clin Orthop Relat Res. 2016;474:1692–1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ji HM, Baek JH, Kim KW, Yoon JW, Ha YC. Herniation pits as a radiographic indicator of pincer-type femoroacetabular impingement in symptomatic patients. Knee Surg Sports Traumatol Arthrosc. 2014;22:860–866. [DOI] [PubMed] [Google Scholar]
- 24. Kalberer F, Sierra RJ, Madan SS, Ganz R, Leunig M. Ischial spine projection into the pelvis: a new sign for acetabular retroversion. Clin Orthop Relat Res. 2008;466:677–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kappe T, Kocak T, Neuerburg C, Lippacher S, Bieger R, Reichel H. Reliability of radiographic signs for acetabular retroversion. Int Orthop. 2011;35:817–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kim JA, Park JS, Jin W, Ryu K. Herniation pits in the femoral neck: a radiographic indicator of femoroacetabular impingement? Skeletal Radiol. 2011;40:167–172. [DOI] [PubMed] [Google Scholar]
- 27. Konishi N, Mieno T. Determination of acetabular coverage of the femoral head with use of a single anteroposterior radiograph. A new computerized technique. J Bone Joint Surg Am. 1993;75:1318–1333. [DOI] [PubMed] [Google Scholar]
- 28. Kutty S, Schneider P, Faris P, et al. Reliability and predictability of the centre-edge angle in the assessment of pincer femoroacetabular impingement. Int Orthop. 2012;36:505–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Laborie LB, Lehmann TG, Engesaeter IO, Eastwood DM, Engesaeter LB, Rosendahl K. Prevalence of radiographic findings thought to be associated with femoroacetabular impingement in a population-based cohort of 2081 healthy young adults. Radiology. 2011;260:494–502. [DOI] [PubMed] [Google Scholar]
- 30. Larson CM, Moreau-Gaudry A, Kelly BT, et al. Are normal hips being labeled as pathologic? A CT-based method for defining normal acetabular coverage. Clin Orthop Relat Res. 2015;473:1247–1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lattanzi R, Petchprapa C, Ascani D, et al. Detection of cartilage damage in femoroacetabular impingement with standardized dGEMRIC at 3 T. Osteoarthritis Cartilage. 2014;22:447–456. [DOI] [PubMed] [Google Scholar]
- 32. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Martinez AE, Li SM, Ganz R, Beck M. Os acetabuli in femoro-acetabular impingement: stress fracture or unfused secondary ossification centre of the acetabular rim? Hip Int. 2006;16:281–286. [DOI] [PubMed] [Google Scholar]
- 34. Nepple JJ, Lehmann CL, Ross JR, Schoenecker PL, Clohisy JC. Coxa profunda is not a useful radiographic parameter for diagnosing pincer-type femoroacetabular impingement. J Bone Joint Surg Am. 2013;95:417–423. [DOI] [PubMed] [Google Scholar]
- 35. Nissi MJ, Mortazavi S, Hughes J, Morgan P, Ellerman J. T2* relaxation time of acetabular and femoral cartilage with and without intraarticular gadopentetate dimeglumine in patients with femoroacetabular impingement. AJR Am J Roentgenol. 2015;204:W695–W700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Notzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–560. [DOI] [PubMed] [Google Scholar]
- 37. Ochoa LM, Dawson L, Patzkowski JC, Hsu JR. Radiographic prevalence of femoroacetabular impingement in a young population with hip complaints is high. Clin Orthop Relat Res. 2010;468:2710–2714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Panzer S, Augat P, Esch U. CT assessment of herniation pits: prevalence, characteristics, and potential association with morphological predictors of femoroacetabular impingement. Eur Radiol. 2008;18:1869–1875. [DOI] [PubMed] [Google Scholar]
- 39. Petchprapa CN, Rybak LD, Dunham KS, Lattanzi R, Recht MP. Labral and cartilage abnormalities in young patients with hip pain: accuracy of 3-tesla indirect MR arthrography. Skeletal Radiol. 2015;44:97–105. [DOI] [PubMed] [Google Scholar]
- 40. Pfirrmann CW, Mengiardi B, Dora C, Kalberer F, Zanetti M, Hodler J. Cam and pincer femoroacetabular impingement: characteristic MR arthrographic findings in 50 patients. Radiology. 2006;240:778–785. [DOI] [PubMed] [Google Scholar]
- 41. Ranawat AS, Schulz B, Baumbach SF, Meftah M, Ganz R, Leunig M. Radiographic predictors of hip pain in femoroacetabular impingement. HSS J. 2011;7:115–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Sahin M, Calisir C, Omeroglu H, Inan U, Mutlu F, Kaya T. Evaluation of labral pathology and hip articular cartilage in patients with femoroacetabular impingement (FAI): comparison of multidetector CT arthrography and MR arthrography. Pol J Radiol. 2014;79:374–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Schmitz MR, Bittersohl B, Zaps D, Bomar JD, Pennock AT, Hosalkar HS. Spectrum of radiographic femoroacetabular impingement morphology in adolescents and young adults: an EOS-based double-cohort study. J Bone Joint Surg Am. 2013;95:e90. [DOI] [PubMed] [Google Scholar]
- 44. Siebenrock KA, Steppacher SD, Haefeli PC, Schwab JM, Tannast M. Valgus hip with high antetorsion causes pain through posterior extraarticular FAI. Clin Orthop Relat Res. 2013;471:3774–3780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Stelzeneder D, Hingsammer A, Bixby SD, Kim YJ. Can radiographic morphometric parameters for the hip be assessed on MRI? Clin Orthop Relat Res. 2013;471:989–999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Sutter R, Dietrich TJ, Zingg PO, Pfirrmann CW. Femoral antetorsion: comparing asymptomatic volunteers and patients with femoroacetabular impingement. Radiology. 2012;263:475–483. [DOI] [PubMed] [Google Scholar]
- 47. Sutter R, Zubler V, Hoffmann A, et al. Hip MRI: how useful is intraarticular contrast material for evaluating surgically proven lesions of the labrum and articular cartilage? AJR Am J Roentgenol. 2014;202:160–169. [DOI] [PubMed] [Google Scholar]
- 48. Tannast M, Kubiak-Langer M, Langlotz F, Puls M, Murphy SB, Siebenrock KA. Noninvasive three-dimensional assessment of femoroacetabular impingement. J Orthop Res. 2007;25:122–131. [DOI] [PubMed] [Google Scholar]
- 49. Tibor LM, Liebert G, Sutter R, Impellizzeri FM, Leunig M. Two or more impingement and/or instability deformities are often present in patients with hip pain. Clin Orthop Relat Res. 2013;471:3762–3773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Wassilew GI, Heller MO, Diederichs G, Janz V, Wenzl M, Perka C. Standardized AP radiographs do not provide reliable diagnostic measures for the assessment of acetabular retroversion. J Orthop Res. 2012;30:1369–1376. [DOI] [PubMed] [Google Scholar]
- 51. Werner CM, Copeland CE, Ruckstuhl T, et al. Radiographic markers of acetabular retroversion: correlation of the cross-over sign, ischial spine sign and posterior wall sign. Acta Orthop Belg. 2010;76:166–173. [PubMed] [Google Scholar]
- 52. Wright JG, Swiontkowski MF, Heckman JD. Introducing levels of evidence to the journal. J Bone Joint Surg Am. 2003;85-A:1–3. [PubMed] [Google Scholar]