Abstract
Objective
To synthesise lessons learnt and determinants of success from human papillomavirus (HPV) vaccine demonstration projects and national programmes in low- and middle-income countries (LAMICs).
Methods
Interviews were conducted with 56 key informants. A systematic literature review identified 2936 abstracts from five databases; after screening 61 full texts were included. Unpublished literature, including evaluation reports, was solicited from country representatives; 188 documents were received. A data extraction tool and interview topic guide outlining key areas of inquiry were informed by World Health Organization guidelines for new vaccine introduction. Results were synthesised thematically.
Results
Data were analysed from 12 national programmes and 66 demonstration projects in 46 countries. Among demonstration projects, 30 were supported by the GARDASIL® Access Program, 20 by Gavi, four by PATH and 12 by other means. School-based vaccine delivery supplemented with health facility-based delivery for out-of-school girls attained high coverage. There were limited data on facility-only strategies and little evaluation of strategies to reach out-of-school girls. Early engagement of teachers as partners in social mobilisation, consent, vaccination day coordination, follow-up of non-completers and adverse events was considered invaluable. Micro-planning using school/ facility registers most effectively enumerated target populations; other estimates proved inaccurate, leading to vaccine under- or over-estimation. Refresher training on adverse events and safe injection procedures was usually necessary.
Conclusion
Considerable experience in HPV vaccine delivery in LAMICs is available. Lessons are generally consistent across countries and dissemination of these could improve HPV vaccine introduction.
Introduction
Globally, an estimated 528,000 new cervical cancer cases and 266,000 deaths occur annually [1]. Over 85% of new cervical cancer cases occur in women living in low and middle-income countries (LAMICs), who have limited access to screening services [1–4]. There are three licensed prophylactic HPV vaccines against persistent infection with HPV vaccine genotypes and high-grade cervical intraepithelial neoplasia, pre-requisites for cervical cancer development [5]. Cervarix® (GlaxoSmithKline Biologicals) targets HPV genotypes 16 and 18; GARDASIL® (Merck & Co. Inc.) targets HPV 16, 18, 6, 11 [6]; GARDASIL-9 (Merck & Co. Inc.) targets an additional five oncogenic genotypes [7]. As HPV is sexually transmitted, the World Health Organization (WHO) recommends targeting HPV vaccination to girls prior to sexual debut (e.g. age 9–13) because it is most efficacious in those who have not been exposed to HPV [8].
Between 2007 and 2012, several LAMICs conducted HPV demonstration projects with vaccines provided by the GARDASIL® Access Program (GAP) [9], Merck & Co., the Bill & Melinda Gates Foundation through PATH, or through other means. Demonstration projects are small-scale pilots through which experience can be gained in delivering the vaccine to what is often a novel target age group [10]. In 2012 Gavi, the Vaccine Alliance, commenced support for demonstration projects and national introductions to increase access to HPV vaccine worldwide. The majority of demonstration projects are now Gavi-funded. National programmes may also be funded by Gavi if the country has prior experience of vaccination in the target age group and achieved over 50% vaccination coverage. By May 2016, over 80 countries or territories had commenced national HPV vaccination and another 38 had completed or started HPV vaccine demonstration projects [11].
Country decision-makers face several challenges when applying for support and introducing HPV vaccine including selection of delivery strategy, effective communication with communities and determining how to maximise coverage [12, 13]. At the time of this study, no comprehensive review of results and lessons learnt from demonstration projects or early scale-up in LAMICs had been conducted. This study aimed to synthesise lessons learnt from the HPV demonstration projects and national programmes in LAMICs implemented between January 2007 and May 2016 to develop recommendations for HPV vaccine delivery and accelerate scale-up of national programmes.
Methods
This ecological study included semi-structured key informant interviews, a systematic literature review and a review of unpublished reports. Units of analysis were: 1) countries, 2) projects/programmes, and 3) delivery experiences (Table 1).
Table 1. Key definitions.
| Delivery experience | The specific target population (age range in years or school grade) and vaccination venue (health facility-based, school-based, outreach, or a combination of the three) within a specific project/programme (defined by the funding source). E.g. A country that was funded for 2 years for a demonstration project and implemented one year of school-based delivery and a second year of health facility based strategy, was classified as having contributed information from one project but two delivery experiences. |
| Programme | A national HPV vaccination programme. |
| Project | The activities funded through a specific GAP, Gavi or other funder support for a demonstration/pilot project. A distinct project was defined by the funder and/or implementer and grant award details. |
A mapping exercise identified all low and lower-middle income countries that had completed at least six months of an HPV vaccine demonstration project or national programme by the end of April 2016. Data from upper-middle or high-income countries were only included if they conducted a demonstration project or utilised an innovative dosing schedule (n = 46; Table 2) [14]. At least another 6 LAMICs were planning to start Gavi-supported demonstration projects, but did not have data in time for inclusion in this study.
Table 2. Countries included in this study with publications included from the systematic literature search.
| Country | Income1 | Primary school net enrolment ratio2 | Demo3/ National (funding source)3 | Vaccination venue(s) | Year/s HPV vaccination |
|---|---|---|---|---|---|
| Bhutan [15–21] | Lower-middle | 88.1 (2013) | Demo (GAP) | School | 2009 |
| National (ACCF) | School | 2010 | |||
| Health facility + outreach | 2011–13 | ||||
| School + health facility + outreach | 2014- | ||||
| Bolivia [19, 20] | Lower-middle | 81.6 (2013) | Demo 1 (GAP) | School + health facility | 2009 |
| Demo 2 (GAP) | School + health facility + outreach | 2009 | |||
| Demo 3 (GAP) | School + health facility | 2010 | |||
| Demo 4 (GAP) | School + health facility | 2010–11 | |||
| Botswana [22–24] | Upper-middle | 83.8 (2009) | Demo (WB) | School | 2013 |
| Demo (MOH) | School + health facility | 2014 | |||
| National (Govt.) | School + health facility | 2015 | |||
| Brazil [25–29] | Lower-middle | 94.4 (2005) | Demo (GAP) | School | 2010–11 |
| Demo (MOH) | School + outreach | 2010–12 | |||
| National (Govt.) | School + health facility | 2014- | |||
| Burkina Faso | Low | 67.5 (2013) | Demo (Gavi) | School + health facility + outreach | 2015- |
| Cambodia [19, 20] | Low | 98.4 (2012) | Demo 1 (GAP) | Health facility | 2009–10 |
| Demo 2 (GAP) | School + health facility | 2010–11 | |||
| Cameroon [19, 20, 30–34] | Lower-middle | 91.5 (2012) | Demo 1 (GAP) | School + health facility | 2010 |
| Demo 2 Gavi) | School + health facility + outreach | 2015- | |||
| Chile [35] | High | 92.7 (2012) | National (Govt.) | School + health facility | 2014- |
| Côte d’Ivoire | Lower-middle | 61.9 (2009) | Demo (Gavi) | School + health facility + outreach | 2015- |
| Ethiopia | Low | 67.9 (2006) | Demo (Gavi) | School + outreach | 2015- |
| The Gambia | Low | 68.7 (2013) | Demo (Gavi) | School + health facility + outreach | 2015- |
| Georgia [20] | Lower-middle | 96.5 (2013) | Demo 1 (GAP) | Health facility | 2010 |
| Demo 2 (GAP) | Health facility + outreach | 2010–14 | |||
| Ghana | Lower-middle | 88.9 (2014) | Demo 1 (GAP) | School | 2013 |
| Demo 2 (Gavi) | Year 1: School. Year 2: School + health facility + outreach | 2013–15 | |||
| Guyana | Lower-middle | 71.5 (2012) | Demo (GAP) | School + health facility | 2012–13 |
| National (Govt) | NA | 2014 | |||
| Haiti [19, 20] | Low | NA | Demo (GAP) | School | 2009 |
| Honduras [20] | Lower-middle | 89.3 (2013) | Demo 1 (GAP) | School + health facility + outreach | 2011 |
| Demo 2 (GAP) | School | 2012–13 | |||
| Demo 3 (GAP) | School + health facility | 2014 | |||
| National (Govt.) | School + health facility | 2015- | |||
| India [36–40] | Lower-middle | 93.3 (2011) | Demo (PATH) | School + health facility campaign | 2009–10 |
| School and health facility monthly delivery | 2009–10 | ||||
| Kenya [20, 41, 42] | Low | 83.6 (2012) | Demo (GAP) | School | 2011 |
| Demo (Gavi) | School | 2013–15 | |||
| Kiribati | Lower-middle | NA | Demo (GAP/ ACCF) | School | 2011–13 |
| Laos PDR | Lower-middle | 97.3 (2013) | Demo (Gavi) | School + health facility + outreach | 2013–15 |
| Lesotho [19, 20] | Lower-middle | 79.6 (2013) | Demo 1 (GAP) | School | 2009 |
| Demo 2 (GAP) | School | 2010–11 | |||
| National | School | 2012- | |||
| Madagascar | Low | 77.1 (2003) | Demo (Gavi) | School + health facility | 2013–15 |
| Malawi | Low | 96.9 (2009) | Demo (Gavi) | School + health facility | 2013–15 |
| Mali | Low | 64.4 (2013) | Demo 1 (GAP) | Health facility | 2012 |
| Demo 2 (Gavi) | School + health facility + outreach | 2015- | |||
| Moldova [20] | Lower-middle | 87.9 (2013) | Demo (GAP) | School | 2010–11 |
| Mongolia | Lower-middle | 94.7 (2013) | Demo (GAP) | School + health facility + outreach | 2012 |
| School | 2014 | ||||
| Mozambique | Low | 87.4 (2013) | Demo (Gavi) | School + health facility + outreach | 2014–15 |
| Nepal [19, 20, 43] | Low | 98.5 (2013) | Demo 1 (ACCF) | School | 2008 |
| Demo 2 (GAP/ACCF) | School + health facility | 2010 | |||
| Demo 3 (ACCF) | School + health facility | 2011–14 | |||
| Demo 4 (Gavi) | School + health facility | 2015- | |||
| Niger | Low | 62.8 (2012) | Demo (Gavi) | School + outreach | 2014–15 |
| Papua New Guinea | Lower-middle | 85.6 (2012) | Demo (GAP) | School + health facility | 2012 |
| Peru [37–39, 44–49] | Upper-middle | 91.8 (2013) | Demo (PATH) | School + health facility + outreach | 2007–08 |
| 2009–10 | |||||
| National (Govt) | School | 2011–12 2014- | |||
| Philippines | Lower-middle | 88.2 (2009) | Demo (Jhpiego) | NA | 2010 |
| Rwanda [50–53] | Low | 93.4 (2013) | National (Merck) | School + health facility + outreach | 2011–13 |
| National (Gavi) | School + health facility | 2014- | |||
| Senegal | Lower-middle | 73.4 (2014) | Demo (Gavi) | School + health facility + outreach | 2015- |
| Sierra Leone | Low | NA | Demo (Gavi) | NA | 2013 |
| Solomon Islands | Lower-middle | 80.7 (2007) | Demo (Gavi) | School + health facility + outreach | 2015- |
| South Africa [54–61] | Upper-middle | 89.6 (2005) | Demo 1 (UCT) | Health facility | 2010 |
| Demo 2 (KZN DoH) | School | 2011 | |||
| Demo 3 (UoS) | School | 2013 | |||
| National (Govt.) | School | 2014- | |||
| Tanzania [20, 39, 62–68] | Low | 83.5 (2013) | Demo 1 (GAP) | School—age and grade criteria tested | 2010–11 |
| 2010–11 | |||||
| Demo 2 (Gavi) | Year 1: School & health facility. Year 2: Health facility + outreach | 2014- | |||
| 2016- | |||||
| Thailand [69, 70] | Upper-middle | 95.6 (2009) | Demo (Jhpiego) | NA | 2010 |
| Togo | Low | 97.5 (2013) | Demo (Gavi) | School + health facility + outreach | 2015- |
| Uganda [20, 37–39, 48, 71–81] | Low | 91.5 (2013) | Demo 1 (PATH/ MOH) | School + health facility | 2008–09 2010–11 |
| School + health facility + outreach | 2008–09 2010–11 | ||||
| Demo 2 (GAP) | Health facility | 2010 | |||
| Demo 3 (Merck) | School + outreach | 2012–14 | |||
| Natl (Gavi) | Health facility + outreach | 2015- | |||
| Uzbekistan [20] | Lower-middle | 88.5 (2011) | Demo (GAP) | Health facility | 2009 |
| National (Gavi) | School + health facility | 2016- | |||
| Vanuatu | Lower-middle | 98.9 (2005) | Demo (ACCF) | School | 2009 |
| National (ACCF) | School + outreach | 2013- | |||
| Vietnam [37–39, 48, 72, 79, 82–84] | Lower-middle | 98.1 (2012) | Demo (PATH/ MOH) | School + health facility | 2008–10 |
| Health facility | 2008–10 | ||||
| Zambia | Lower-middle | 91.4 (2013) | Demo (GAP) | School + health facility | 2013–14 |
| Zimbabwe | Low | 93.9 (2012) | Demo (Gavi) | School + health facility + outreach | 2015- |
1 World bank classifications of income group, February 2014.
2 Information sourced from UNESCO Institute of Statistics, educational attainment most recently available data; year is indicated in brackets.
Italicised text indicates experiences with incomplete data due to start date; this data was obtained in the process of data collection when countries were questioned about future or current HPV vaccine activity; only experiences with at least one year of implementation were included in analyses.
Abbreviations: ACCF, Australian Cervical Cancer Foundation; CHW, community health worker; Demo, demonstration/pilot project; GAP, Gardasil® Access Program; est., estimated; HPV, human papillomavirus; KZN DoH, KwaZulu-Natal Department of Health; MOH, ministry of health; national, national programme; NA, not available; UCT, University of Cape Town; UNESCO, the United Nations Educational Scientific and Cultural Organisation; UoS, University of Stellenbosch; WB, World Bank.
Systematic literature review
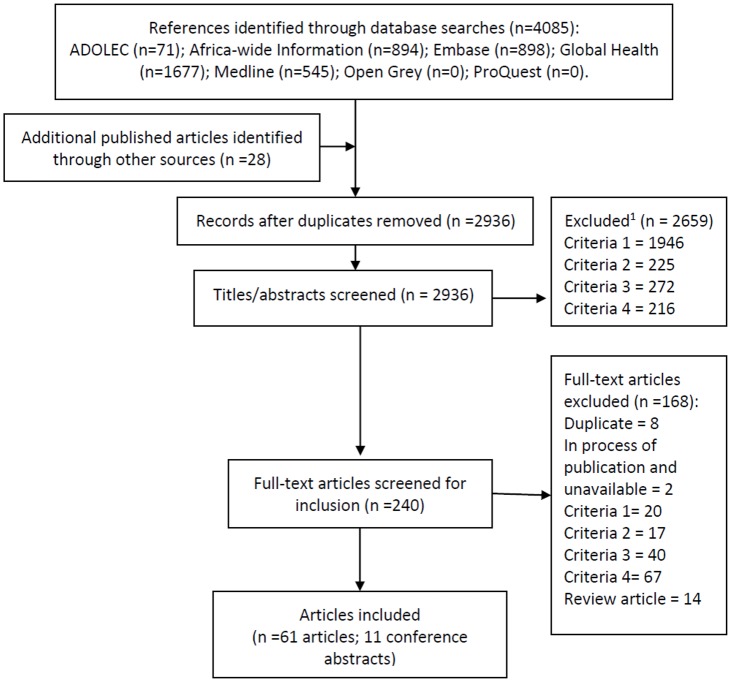
Five databases (Medline, Embase, Global Health, Africa-wide Information, ADOLEC) were searched systematically for published literature in April 2016. Search terms relating to HPV and vaccination were combined with country terms, with no language restrictions (S1 Table). For each country, searches were limited to publications from the first year of HPV vaccine experience onwards, to reduce the number of articles retrieved that did not document vaccine delivery (e.g. hypothetical acceptance studies). Reference lists of identified reviews and retrieved papers were checked for missing papers. One author was contacted for an unpublished manuscript. Titles and abstracts of 2936 references were double screened by two of three study investigators using exclusion criteria set a-priori in a protocol as per PRISMA guidelines [85] (Fig 1). Exclusion criteria were: 1) not focused on HPV vaccination; 2) not focused on one of our countries of interest; 3) did not include any results from after the vaccine was delivered; 4) not focused on, or relevant to, the demonstration project or vaccine introduction. Any conflicting opinions between investigators on the exclusion of abstracts were noted and resolved after full text review by the third investigator. A total of 240 full texts were screened by the same study personnel using the same exclusion criteria. Review articles were identified and searched for further references but were not included in the final selection of articles for data extraction.
Fig 1. Systematic literature review flow.
1Exclusion criteria were: 1) not focused on HPV vaccination; 2) not focused on one of our countries of interest; 3) did not include any results from after the vaccine was delivered; 4) not focused on, or relevant to, the demonstration project or vaccine introduction. Review articles were identified and searched for further references but were not included in data extraction.
Unpublished reports
Authors systematically searched two databases (Open Grey, ProQuest) and several websites (national Ministries of Health (MOH), WHO Global Immunization News, Pan-American Health Organization newsletters, scientific conferences on HPV) for unpublished literature through March 2016. Unpublished data were solicited directly from country representatives and stakeholders involved in HPV projects/programmes.
Key informant interviews
Representatives from each HPV vaccine project/programme in 44 of the 46 countries were approached for interview in order to fill gaps in the data in the published and unpublished literature. No significant gaps were identified in two countries. After written informed consent was obtained, interviews were conducted by phone or in-person. A topic guide was adapted to address identified knowledge gaps. All interviewees were assured of confidentiality and anonymity to encourage openness about experiences.
Data extraction
KG, NH, SK, SMJ extracted data during February-May 2016, using an Excel-based matrix of key areas of inquiry informed by WHO’s new vaccine introduction guidelines [86]. The matrix was piloted and revised twice, with two consistency checks conducted. Data from published, unpublished and interview sources were extracted into the same matrix.
Data analysis
Country data from all sources were triangulated and analysed together in seven themes: preparation, communications, delivery, achievements, sustainability, integration and value of demonstration projects. Data were grouped by calendar year, world region and type of funder or implementer to analyse patterns.
Qualitative data were analysed thematically across data sources. Quantitative data (e.g. coverage, adverse events) were analysed descriptively to present frequencies and proportions. Reported coverage estimates were categorised as percentages because not all projects/programmes shared numerator and denominator data to enable coverage calculations.
The London School of Hygiene & Tropical Medicine Research Ethics Committee approved the study in March 2015.
Results
In total, 61 published articles, 11 conference abstracts, and 188 unpublished documents were included in the review. Unpublished documents received from country representatives and international partners from 44 of the 46 countries included: GAP final reports (n = 16); Gavi post-introduction evaluations (PIEs; n = 9); other PIEs (n = 2); Gavi cost analyses (n = 6); Gavi coverage surveys (n = 9); and other internal reports (n = 146). Additionally, 56 interviews were conducted covering experiences from 40 countries (59 demonstration projects, 11 national programmes). Four country representatives invited to interview either refused to participate or did not respond.
The 46 countries that implemented HPV vaccination projects/programmes between January 2007 and May 2016 accumulated 120 years of implementation experience (Table 2). This included 12 national programmes and 66 demonstration projects. By May 2016, 39% of countries (n = 18) had 2–3 years of experience, 35% (n = 16) had one year of experience and 26% (n = 12) had four or more years of experience in national programmes or multiple demonstration projects. Twenty-one projects/programmes in 19 countries had implemented a two-dose HPV vaccine schedule by May 2016; all others implemented a three-dose schedule. HPV vaccination was free-of-charge to recipients in all projects/programmes.
Preparation
Leadership and planning
Three-quarters of projects/programmes were led by the MOH, with lead departments varying between cancer, school/sexual/reproductive health and immunisation. Some early demonstration projects were led by hospitals or non-governmental organisations (NGOs) with varying degrees of national immunisation team (EPI) involvement, a few operated without government input. Some interviewees from countries without school/adolescent health programmes reported confusion over which department should lead coordination of HPV vaccination and leadership was decided opportunistically, based on capacity. However, it was clear that EPI involvement was necessary to ensure smooth implementation and reduce workload (e.g. to avoid establishment of parallel vaccine management and reporting systems). Delivery experiences with MOH ownership and high EPI involvement were more likely to achieve good coverage in comparison to others run by external partners or with low EPI involvement. Sources indicated that to be effective, microplanning needed involvement of the Ministry of Education (MOE), teachers and school administrators and health representatives.
District selection
Among the 53 projects in 40 countries with data, areas included in a quarter of the demonstration projects represented those with routine immunisation coverage and education performance similar to the national average (15 projects), a fifth represented convenient districts (i.e. close to the capital city and/or had good infrastructure; 10 projects), 30% were representative of both urban and rural areas (16 projects). Projects could be classified in more than one of these categories. Some projects selected districts that included varied or particularly challenging areas (13%, 7 projects) but 17% (5 projects) selected areas with higher than national average EPI coverage and educational attainment.
Enumeration of the population eligible for vaccination
Accurate enumeration was challenging in most countries and affected estimations of the doses required, transport and coverage calculations. School headcounts/ register checks used in conjunction with school enrolment rates, were the most accurate methods to calculate the target population number, aside from conducting a full census, which was prohibitively expensive in most countries. However, the number of out-of-school girls was often unknown throughout projects/ programmes.
Cold-chain and waste management
The most efficient method of transporting HPV vaccines was alongside other routine vaccines. However, in some countries this proved problematic due to the demonstration project timeline not aligning with quarterly vaccine delivery schedules. Providing separate transport increased the cost of delivery. Routine national immunization cold-chain facilities were generally used. Waste management generally followed routine practices and needed improvement in many countries.
Staff training
Cascade training (i.e. national staff training regional staff, who train district-level, who train field-staff), was reportedly less expensive than transporting teams of national trainers around the country. However, periodic supervision was considered necessary in order to ensure that the quality of information transfer between levels in the cascade was maintained.
Communications
HPV vaccination as a cancer prevention method was more frequently emphasized than its role in sexually transmitted infection (STI) prevention, in order to avoid stigmatising the vaccine and to reduce confusion with other STI prevention messages [87]. Messages targeted the whole community with information focused on cervical cancer, the importance of HPV vaccination, government endorsement, doses required, timing and venues, and lack of long-term adverse effects. Problems were reported when social mobilisation occurred less than a month before vaccination and high-level officials did not deal with rumours rapidly.
Delivery
Venue and target
Schools were the most commonly used vaccination venue, with 87% (78/89) of delivery strategies using them, with or without additional health facility or outreach components (Table 2). Strategies including schools gained high coverage but were reported to be resource intensive in countries without existing school-based health programmes. There were limited data on strategies that used health facilities as the only sites of vaccine delivery (11 experiences, 5 with coverage data). In experiences that used schools, 52% (39/75) vaccinated a specific age group of girls, 31% (23/75) selected a school grade(s) and 17% (13/75) vaccinated girls of a certain age within a specific school grade. Some MOH-led projects/ programmes made changes to the delivery strategy for a variety of reasons that illustrate the trade-offs inherent in different strategies (Table 3).
Table 3. Changes in delivery strategy.
| Countries | Original strategy | Change in strategy | Reasons for changes |
| Change from school-based campaign (3 countries) | School or school + health facility | Health facility with/ without outreach | High level of resources required for outreach visits to schools and concern over sustainability. One country subsequently switched back to school based strategy, as HPV vaccine coverage was low with health facility delivery. |
| Removal of out-of-school strategy (2 countries) | School + health facility + outreach | School + health facility or school-only | Outreach had proven resource intensive, with logistical difficulties and only incremental gains in coverage. |
| Addition of strategies to reach out-of-school girls (5 countries) | School or Health facility | School + health facility +/- outreach or Health facility + outreach | To increase coverage and equity of HPV vaccination by including out-of-school girls. |
| Countries | Original target population | Change to target population | Reasons for changes |
| Change to identification of girls by grade (5 countries) | Age | Grade | Identifying eligible girls by age was difficult if exact birth date/year was not known or documented. It was unacceptable to separate some girls from their classmates to receive the vaccine while other class members were not vaccinated. |
| Change to identification of girls by age (4 countries) | Grade or age within a grade | Age | It is easier to explain to the community and aligns with routine EPI, which used age cohorts. Easier to estimate the denominator/ target population even if girls are spread in different grades. To purposely assess a different strategy in the second year of the project. |
| Adaption of age/grade criterion to be more appropriate (5 countries) | Grade | More appropriate grade | A higher concentration of eligible girls were in a higher/lower grade. |
| Age 10 out-of-school | Age 9–13 out-of-school | The relative ease of identifying ‘pre-pubertal’ girls around the age of 9–13 years in the community in comparison to trying to find exactly age 10 girls. |
Out-of-school girls
National primary school enrolment ratios indicate the proportion of girls out-of-school was 5% or less in 23% of the countries with data (10/43), between 6% and 20% in 56% of countries (24/43), and over 20% in nine countries (range 23–38%)[14]. Almost a third of experiences (27%) had no reported strategy for reaching out-of-school girls, another third (35%) relied on them attending health facilities for vaccination and the remaining experiences used outreach. Outreach was used in all nine countries with poor school enrolment and reportedly increased coverage.
Duration of delivery per dose
Duration of delivery activities per dose ranged from 2–3 days to 1 month (data from 31 delivery experiences). Most experiences delivered each dose over the course of one week and activity was synchronized across districts (i.e. similar to a vaccination campaign). Two further experiences delivered each dose over 6 months at the health facility and during routine outreach. There was no obvious relationship between the duration of delivery activities per dose and vaccination coverage. However, countries reported that it was useful to provide a second opportunity for girls to obtain the vaccine (e.g. ‘mop-up’ vaccination days at schools) if they had initially refused or were absent. The dose schedule recommendation change in April 2014 [88, 89] resulted in data on two-dose schedules from 19 countries. The delivery of two doses rather than three doses was reported as logistically easier to fit in to the school year and cheaper by all 10 countries that had changed vaccine schedule. One country reported an extended interval of 12 months between doses made enumeration and delivery in a single campaign each year easier.
Catch-up
Three national programmes conducted catch-up vaccination in older age groups either by vaccinating girls aged 9–15 or 9–18 years, or by additionally vaccinating the second and third grades of secondary school. Two further national programmes vaccinated 9–13 year olds in a small catch-up campaign in their first year of the programme. No evaluation results were available for catch-up campaigns.
Health workforce
Almost all countries used qualified nurses to deliver the vaccine; one used community health workers (CHWs). CHWs and teachers were reportedly invaluable at vaccination venues to ensure efficient delivery. Disruption of other health services during HPV vaccine delivery was not homogenous within a country. Strategies to minimise the impact of the HPV school/outreach activities on routine services included: integration into existing outreach days, longer working days, use of staff from other areas or services and task-shifting responsibilities to CHWs. One country delivered each dose over a month instead of short ‘campaign-style’ delivery. Supervision was reported as necessary, but supervisor and vaccinator allowances and transport were frequently reported as being drivers of high delivery costs.
Adverse events
Reported adverse events (AEs) were below 1% and minor across 56 delivery strategies in 44 countries that provided data. Monitoring, reporting and response procedures were consistent with those for other vaccines, although teachers were mentioned as a useful and, in some countries, novel resource in monitoring AEs.
Achievements: Vaccine uptake, completion and coverage
Coverage was reported by 65% of experiences (60/92); only 17 projects conducted coverage surveys, the remainder relied on administrative coverage. Uptake, completion and final dose coverage achievements were high, with no estimates below 50% (Table 4). Experiences that achieved high coverage included schools as a vaccination venue, had high EPI and MOE involvement in both planning and implementation and included a strategy to reach out-of-school girls if school enrolment rates were variable. Other factors reported to encourage high coverage were: political commitment, good social mobilisation, community engagement and timely delivery of the vaccine on scheduled dates within one school year.
Table 4. Coverage achievements across delivery experiences.
| Characteristic | Uptake (number (%))1 | Completion (number (%)) | Final dose coverage2 (number (%)) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ≥90% | 70–89% | 50–69% | Total | ≥90% | 70–89% | 50–69% | Total | ≥90% | 70–89% | 50–69% | Total | |
| School only | 9 (50) | 7 (39) | 2 (11) | 18 | 13 (68) | 6 (32) | 0 | 19 | 8 (40) | 11 (55) | 1 (5) | 20 |
| Health facility (+/- outreach) | 3(60) | 2 (40) | 0 | 5 | 1 (20) | 4 (80) | 0 | 5 | 2 (40) | 1 (20) | 2 (40) | 5 |
| School + health facility (+/- outreach) | 19 (58) | 14 (42) | 0 | 33 | 17 (57) | 13 (43) | 0 | 30 | 15 (43) | 13 (37) | 7 (20) | 35 |
| All experiences | 31 (55) | 23 (41) | 2 (4) | 56 | 31 (57) | 23 (43) | 0 | 48 | 25 (42) | 25 (42) | 10 (17) | 60 |
1 Counts of the number of experiences achieving each category of coverage are presented with row percentages, i.e. among those strategies with data, 57% of school only strategies obtained #x2265;90% uptake compared to 50% of health facility strategies obtaining ≥90% uptake. Excludes projects/programmes that started in 2015 or later
2 Coverage of a 2 or 3 dose regimen (only 10 experiences had coverage data on 2-dose regimen)
Integration
Projects implemented with MOH involvement generally used EPI structures and processes for vaccine delivery. However, the small scale of projects made integration difficult to assess and sometimes led to establishment of parallel processes for monitoring and evaluation, supervision, vaccine transport and staff remuneration, as HPV vaccine was not seen as part of the ‘routine’ workload.
Joint delivery of HPV vaccine with other interventions was limited. One programme delivered HPV vaccine alongside a hepatitis B vaccination campaign. Eight projects/programmes attempted delivery with tetanus toxoid vaccine or deworming and vitamin A supplementation within school health programmes; six reported coverage estimates, which were variable. Educational messages on reproductive health or hygiene issues were delivered at the same time as HPV vaccine in eleven projects/programmes. Two externally-led projects/programmes delivered the first dose alongside a cervical cancer screening programme for mothers. No critical evaluations of joint delivery were available.
Financing and sustainability
Thirty of the 66 demonstration projects were financed by GAP, through Axios Healthcare Development. GAP donated vaccine, but no delivery costs. Gavi funded 20 demonstration projects and provided vaccine and some delivery costs. For the first year of implementation Gavi provided either US$ 4.80 per girl or US$50,000 for delivery, whichever amount was largest. In the second year, funding was halved to account for start-up costs. PATH, through funding from the Bill and Melinda Gates Foundation and donated vaccine from GSK and Merck, financed four projects; 12 were supported by other means. Gavi, Merck, the Australian Cervical Cancer Foundation (ACCF) and national governments funded the national programmes.
Countries reported considerable uncertainty over the availability of future financing. The cost of school-based delivery was of concern for many where there were not existing school-based health programmes. In addition to the delivery strategy changes in Table 3, six countries stated that they planned to change from a school-based strategy to a health facility-based strategy in the future, due to the high level of resources required for school visits, specifically for transport and staff per diems.
Discussion
There is now considerable experience in HPV vaccine delivery in LAMICs. School-based delivery to this target group is no longer ‘novel’. Many lessons have been learnt that should make planning easier for countries still considering whether to introduce HPV vaccination. Recommendations (Table 5; S2 Table) and outputs for decision-makers are available online [90].
Table 5. Key recommendations.
| Section | Recommendations |
|---|---|
| Preparation | Planning processes should include representatives from the ministries of health, education and finance. |
| National immunisation programme involvement is critical for effective vaccine delivery | |
| Communications | Social mobilisation in communities should begin early (at least one month before vaccination, earlier if possible). |
| Messages should focus on: cervical cancer prevention; safety and efficacy, including lack of fertility impact or long-term adverse effects, government endorsement, delivery timing and venues and the need to return for a second dose | |
| Members of government or WHO representatives should issue responses to rumours as quickly as possible. | |
| Consent processes should be consistent with existing routine EPI consent policy to avoid rumours. | |
| Delivery | In areas with variable school attendance, specific mobilisation of out-of-school girls and an opportunity for them to receive the vaccine should be provided. |
| If resources allow, planning a two-stage delivery of each dose can be successful in reaching those girls who initially refused vaccination. | |
| Countries need to be aware that HIV infected girls require 3 doses and should develop specific strategies to offer them the 3-dose regimen. | |
| Vaccination teams can include teachers and CHWs in order to decrease the number of qualified nurses needed for vaccine delivery sessions | |
| Achievements | Including a component of school-based delivery can yield high coverage, if resources allow. If school enrolment is low, a mixture of strategies could be important in order to attain good coverage. |
| More evaluation of health facility only strategies is needed. | |
| An opportunity for girls who missed doses to receive the vaccine should be supplied, either at return visits to schools or referral to health facility or outreach sites, depending on the resources available. | |
| Sustainability | More research should be conducted on scale-up experiences. |
| Where feasible (e.g. in terms of funding and country experience with introducing vaccines), consider phased national implementation rather than demonstration projects | |
| Further exploration of sustainable funding options should be conducted and disseminated, to encourage countries to scale-up demonstration projects | |
| Integration | Rigorous evaluation of combined interventions with HPV vaccine delivery is needed to assess the effect on implementation, coverage, workload and cost. Funding agencies should systematically encourage this. |
| Gradual integration of processes into routine processes should be planned and formalised after the first round of vaccination is completed. | |
| Opportunities to initiate or strengthen existing school health programmes and/or pre-adolescent/adolescent health should be seized through on-going collaboration with partners (e.g. MOE, reproductive health departments). |
Our findings are limited by the variation in data availability; some topics were rarely reported, or the data was highly variable in quality (e.g. coverage). Representatives from four countries did not respond or refused interviews. As we relied on data supplied by country representatives, the availability of data may have been lower for less successful projects/programmes. Only nine of the 20 Gavi-supported projects had completed their second year during the period of data collection.
Lessons learnt, drivers of high coverage and key mobilisation messages were consistent across types of demonstration project and world regions, i.e. Africa (23 countries), Asia (10), Americas (7), Oceania (4), Europe (2). Limited EPI involvement is unlikely to be an issue in most future demonstration projects as involvement is required for Gavi applications [10]. Lessons were similar to key findings documented during initial demonstration projects in 2007 [38, 65]. However, the substantial challenges in estimating target population size have not been stressed in previous publications [12, 38]. Enumeration accuracy impacted vaccine requirement projections and coverage calculations in almost all countries included.
Most experience to date is with school-based delivery. Funders should encourage countries to test different approaches as more data is needed on more sustainable strategies. If alternative strategies result in unacceptable levels of coverage, LAMIC may need increased funding to deliver school-based programmes. Limited attempts to reach out-of-school girls did not greatly affect coverage in countries that attain over 80% net school enrolment [14]. However, not providing an opportunity for out-of-school girls to be vaccinated perpetuates inequity.
Conclusions
HPV vaccine demonstration projects and national programmes to date in LAMICs have achieved high coverage. However, the expense of school-based delivery is of concern for the future sustainability of HPV vaccination programmes. Demonstration projects could better inform national programmes if they provided lessons in challenging areas and populations or tested more sustainable delivery strategies.
Supporting information
(DOCX)
(DOCX)
Acknowledgments
Authors thank interviewees for their time and interest, source authors for their contributions, and Xeno Acharya for contributing to the grey literature search.
Data Availability
All anonymised data are available publicly in the LSHTM Research Online repository; URL: http://researchonline.lshtm.ac.uk/3351522/.
Funding Statement
This work was supported by the Bill & Melinda Gates Foundation [grant OPP1115326]. The findings and conclusions contained within are those of the authors and do not necessarily reflect positions or policies of the Bill & Melinda Gates Foundation or PATH. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.IARC. GLOBOCAN 2012. Cervical Cancer Estimated Incidence, Mortality and Prevalence Worldwide in 2012. Available at: http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx.
- 2.Parkin DM, Bray F. Chapter 2: The burden of HPV-related cancers. Vaccine. 2006;24 Suppl 3:S3/11–25. Epub 2006/09/05. S0264-410X(06)00684-0 [pii] 10.1016/j.vaccine.2006.05.111 . [DOI] [PubMed] [Google Scholar]
- 3.Ott JJ, Ullrich A, Mascarenhas M, Stevens GA. Global cancer incidence and mortality caused by behavior and infection. Journal of Public Health. 2011;33(2):223–33. 10.1093/pubmed/fdq076 [DOI] [PubMed] [Google Scholar]
- 4.Peters LM, Soliman AS, Bukori P, Mkuchu J, Ngoma T. Evidence for the need of educational programs for cervical screening in rural Tanzania. J Cancer Educ. 2010;25(2):153–9. Epub 2010/03/06. 10.1007/s13187-009-0018-9 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schiller JT, Castellsague X, Garland SM. A review of clinical trials of human papillomavirus prophylactic vaccines. Vaccine. 2012;30 Suppl 5:F123–38. Epub 2012/12/05. 10.1016/j.vaccine.2012.04.108 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bosch FX, Broker TR, Forman D, Moscicki A-B, Gillison ML, Doorbar J, et al. Comprehensive Control of Human Papillomavirus Infections and Related Diseases. Vaccine. 2013;31, Supplement 5(0):F1–F31. 10.1016/j.vaccine.2013.10.001. [DOI] [PubMed] [Google Scholar]
- 7.Joura EA, Giuliano AR, Iversen OE, Bouchard C, Mao C, Mehlsen J, et al. A 9-valent HPV vaccine against infection and intraepithelial neoplasia in women. The New England journal of medicine. 2015;372(8):711–23. Epub 2015/02/19. 10.1056/NEJMoa1405044 . [DOI] [PubMed] [Google Scholar]
- 8.WHO. Human papillomavirus vaccines: WHO position paper. Wkly Epidemiol Rec. 2009;15:118–31. [PubMed] [Google Scholar]
- 9.Merck & Co., Inc. GARDASIL Access Program,. Corporate Responsibility Report 2014. Key Initiatives: GARDASIL Access Program. http://www.merckresponsibility.com/access-to-health/key-initiatives/gardasil-access-program/ 2016 [cited 2016 04 February].
- 10.Gavi Alliance. Supplementary guidelines for human papillomavirus (HPV) vaccine demonstration project applications in 2015. Gavi Alliance, 2014. [Google Scholar]
- 11.Cervical Cancer Action. Cervical Cancer Action Progress maps; August 2015; http://www.cervicalcanceraction.org/comments/comments3.php 2015 [cited 2015 8th December].
- 12.World Health Organization. Monitoring the coverage and impact of human papillomavirus vaccine—report of WHO meeting, November 2009. Releve epidemiologique hebdomadaire / Section d'hygiene du Secretariat de la Societe des Nations = Weekly epidemiological record / Health Section of the Secretariat of the League of Nations. 2010;85(25):237–43. [PubMed]
- 13.World Health Organization. HPV Vaccine Communication: Special Considerations for a unique vaccine. World Health Organization, 2013. [Google Scholar]
- 14.UNESCO Institute of Statistics. Education: Enrolment by level of education: Primary. August 2015 release http://data.uis.unesco.org/Index.aspx?queryid=128
- 15.Dorji T, Tshomo U, Phuntsho S, Tamang TD, Tshokey T, Baussano I, et al. Introduction of a National HPV vaccination program into Bhutan. Vaccine. 2015;33(31):3726–30. Epub 2015/06/10. 10.1016/j.vaccine.2015.05.078 . [DOI] [PubMed] [Google Scholar]
- 16.Herrero R, Gonzalez P, Markowitz LE. Present status of human papillomavirus vaccine development and implementation. The Lancet Oncology. 2015;16(5):e206–e16. 10.1016/S1470-2045(14)70481-4. . [DOI] [PubMed] [Google Scholar]
- 17.Hanson CM, Eckert L, Bloem P, Cernuschi T. Gavi HPV programs: Application to implementation. 2015;3(2):408–19. 10.3390/vaccines3020408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sankaranarayanan R. HPV vaccination: the most pragmatic cervical cancer primary prevention strategy. (World Report on Women's Health 2015: The unfinished agenda of women's reproductive health.). International Journal of Gynecology & Obstetrics. 2015;131(Suppl. 1):S33-S5. [DOI] [PubMed]
- 19.Ladner J, Besson MH, Hampshire R, Tapert L, Chirenje M, Saba J. Assessment of eight HPV vaccination programs implemented in lowest income countries. BMC public health. 2012;12:370 10.1186/1471-2458-12-370. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ladner J, Besson MH, Rodrigues M, Audureau E, Saba J. Performance of 21 HPV vaccination programs implemented in low and middle-income countries, 2009–2013. BMC public health. 2014;14:670 Epub 2014/07/02. 10.1186/1471-2458-14-670 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Adams M, Jasani B, Fiander A. Human papilloma virus (HPV) prophylactic vaccination: Challenges for public health and implications for screening. Vaccine. 2007;25(16):3007–13. 10.1016/j.vaccine.2007.01.016. . [DOI] [PubMed] [Google Scholar]
- 22.Grover S, Raesima M, Bvochora-Nsingo M, Chiyapo SP, Balang D, Tapela N, et al. Cervical cancer in Botswana: Current state and future steps for screening and treatment programs. Frontiers in Oncology. 2015;5 (NOV) (no pagination)(239). 10.3389/fonc.2015.00239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ramogola-Masire D. Establishing a cervical cancer prevention service in Botswana. International Journal of Gynecology and Obstetrics. 2015;131:E18. [Google Scholar]
- 24.Raesima MM, Forhan SE, Voetsch AC, Hewitt S, Hariri S, Wang SA, et al. Human Papillomavirus Vaccination Coverage Among School Girls in a Demonstration Project—Botswana, 2013. Mmwr. 2015;Morbidity and mortality weekly report. 64(40):1147–9. 10.15585/mmwr.mm6440a5. [DOI] [PubMed]
- 25.Fregnani JHTG, Carvalho AL, Eluf Neto J, Ribeiro KdCB, Kuil LdM, Silva TAd, et al. A school-based human papillomavirus vaccination program in Barretos, Brazil: final results of a demonstrative study. PloS one. 2013;8(4). 10.1371/journal.pone.0062647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Baker ML, Figueroa-Downing D, Chiang EDdO, Villa L, Baggio ML, Eluf-Neto J, et al. Paving pathways: Brazil's implementation of a national human papillomavirus immunization campaign. Revista Panamericana de Salud Publica/Pan American Journal of Public Health. 2015;38(2):163–6. . [PubMed] [Google Scholar]
- 27.Chiang EDdO, Baker ML, Figueroa-Downing D, Baggio ML, Villa L, Eluf Neto J, et al. “THOSE WHO LOVE, VACCINATE”: PARENTAL PERCEPTIONS OF HPV VACCINATION. 2015. 2015;25(3):10 Epub 2015-10-25. 10.7322/jhgd.106013 [DOI] [Google Scholar]
- 28.Kury CM, Kury MM, Silva RM, Oliveira FA, de Moraes JC, De Moraes JG, et al. Implementation of the quadrivalent vaccine against HPV in the Municipality of Campos dos Goytacazes, Brazil–A combination of strategies to increase immunization coverage and early reduction of genital warts. Trials in Vaccinology. 2013;2:19–24. [Google Scholar]
- 29.Jauregui B, Sinha A, Clark AD, Bolanos BM, Resch S, Toscano CM, et al. Strengthening the technical capacity at country-level to make informed policy decisions on new vaccine introduction: Lessons learned by PAHO's ProVac Initiative. Vaccine. 2011;29(5):1099–106. 10.1016/j.vaccine.2010.11.075. [DOI] [PubMed] [Google Scholar]
- 30.Ayissi CA, Wamai RG, Oduwo GO, Perlman S, Welty E, Welty T, et al. Awareness, acceptability and uptake of human papilloma virus vaccine among Cameroonian school-attending female adolescents. Journal of community health. 2012;37(6):1127–35. 10.1007/s10900-012-9554-z. . [DOI] [PubMed] [Google Scholar]
- 31.Wamai RG, Ayissi CA, Oduwo GO, Perlman S, Welty E, Manga S, et al. Assessing the Effectiveness of a Community-Based Sensitization Strategy in Creating Awareness About HPV, Cervical Cancer and HPV Vaccine Among Parents in North West Cameroon. Journal of community health. 2012;37(5):917–26. 10.1007/s10900-012-9540-5. WOS:000308537100001. [DOI] [PubMed] [Google Scholar]
- 32.Wamai RG, Ayissi CA, Oduwo GO, Perlman S, Welty E, Welty T, et al. Awareness, knowledge and beliefs about HPV, cervical cancer and HPV vaccines among nurses in Cameroon: An exploratory study. International Journal of Nursing Studies. 2013;50(10):1399–406. 10.1016/j.ijnurstu.2012.12.020. . [DOI] [PubMed] [Google Scholar]
- 33.Ogembo JG, Manga S, Nulah K, Foglabenchi LH, Perlman S, Wamai RG, et al. Achieving high uptake of human papillomavirus vaccine in Cameroon: Lessons learned in overcoming challenges. Vaccine. 2014;32(35):4399–403. Epub 2014/06/27. 10.1016/j.vaccine.2014.06.064 . [DOI] [PubMed] [Google Scholar]
- 34.Manga S, Welty E, Welty T, Nulah K, Haritu L. Preventing cervical cancer through an HPV vaccine delivery project in cameroon. International Journal of Gynecological Cancer. 2014;4:819–20. [Google Scholar]
- 35.Abarca V K, Valenzuela B MT, Vergara F R, Luchsinger F V, Munoz M A, Jimenez de la J J, et al. Human papillomavirus vaccine. Statement of the Advisory Committee of Immunizations on Behalf of the Chilean Infectious Diseases Society. September 2008. Revista Medica de Chile. 2008;136(11):1485–92. . [DOI] [PubMed] [Google Scholar]
- 36.Larson HJ, Brocard P, Garnett G. The India HPV-vaccine suspension. The Lancet. 2010;376(9741):572–3. [DOI] [PubMed] [Google Scholar]
- 37.Tsu VD, Cernuschi T, LaMontagne DS. Lessons learned from HPV vaccine delivery in low-resource settings and opportunities for HIV prevention, treatment, and care among adolescents. J Acquir Immune Defic Syndr. 2014;66 Suppl 2:S209–16. Epub 2014/06/12. 10.1097/qai.0000000000000175 . [DOI] [PubMed] [Google Scholar]
- 38.LaMontagne DS, Barge S, Le NT, Mugisha E, Penny ME, Gandhi S, et al. Human papillomavirus vaccine delivery strategies that achieved high coverage in low- and middle-income countries. Bulletin of the World Health Organization. 2011;89(11):821–30B. Epub 2011/11/16. 10.2471/BLT.11.089862 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Levin A, Wang SA, Levin C, Tsu V, Hutubessy R. Costs of introducing and delivering HPV vaccines in low and lower middle income countries: inputs for GAVI policy on introduction grant support to countries. PloS one. 2014;9(6):e101114 Epub 2014/06/27. 10.1371/journal.pone.0101114 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sathyanarayana T, Hawkes S, Shahmanesh M, Laxminarayan R, Murthy GVS. Evidence, politics and cultures in policymaking: Policy analysis of HPV vaccine introduction in India. Sexually Transmitted Infections. 2015;91:A61 10.1136/sextrans-2015-052270.166 [DOI] [Google Scholar]
- 41.Vermandere H, Naanyu V, Mabeya H, Broeck DV, Michielsen K, Degomme O. Determinants of acceptance and subsequent uptake of the HPV vaccine in a cohort in Eldoret, Kenya. PloS one. 2014;9(10). 10.1371/journal.pone.0109353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Masika MM, Ogembo JG, Chabeda SV, Wamai RG, Mugo N. Knowledge on HPV vaccine and cervical cancer facilitates vaccine acceptability among school teachers in Kitui County, Kenya. PLoS ONE. 2015;10 (8) (no pagination)(e0135563). 10.1371/journal.pone.0135563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Singh Y, Shah A, Singh M, Verma S, Shrestha BM, Vaidya P, et al. Human papilloma virus vaccination in Nepal: an initial experience in Nepal. Asian Pacific journal of cancer prevention: APJCP. 2010;11(3):615–7. Epub 2010/11/03. . [PubMed] [Google Scholar]
- 44.Bartolini RM, Winkler JL, Penny ME, LaMontagne DS. Parental Acceptance of HPV Vaccine in Peru: A Decision Framework. PloS one. 2012;7(10). 10.1371/journal.pone.0048017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Penny M, Bartolini R, Mosqueira NR, LaMontagne DS, Mendoza MA, Ramos I, et al. Strategies to vaccinate against cancer of the cervix: Feasibility of a school-based HPV vaccination program in Peru. Vaccine. 2011;29(31):5022–30. 10.1016/j.vaccine.2011.04.078. WOS:000293043500020. [DOI] [PubMed] [Google Scholar]
- 46.Levinson KL, Abuelo C, Chyung E, Salmeron J, Belinson SE, Sologuren CV, et al. The Peru Cervical Cancer Prevention Study (PERCAPS) Community-Based Participatory Research in Manchay, Peru. International Journal of Gynecological Cancer. 2013;23(1):141–7. 10.1097/IGC.0b013e318275b007. WOS:000314005000020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Abuelo CE, Levinson KL, Salmeron J, Sologuren CV, Fernandez MJ, Belinson JL. The Peru Cervical Cancer Screening Study (PERCAPS): the design and implementation of a mother/daughter screen, treat, and vaccinate program in the Peruvian jungle. Journal of community health. 2014;39(3):409–15. Epub 2013/11/28. 10.1007/s10900-013-9786-6 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Levin CE, Van Minh H, Odaga J, Rout SS, Ngoc DN, Menezes L, et al. Delivery cost of human papillomavirus vaccination of young adolescent girls in Peru, Uganda and Viet Nam. Bulletin of the World Health Organization. 2013;91(8):585–92. Epub 2013/08/14. 10.2471/BLT.12.113837 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Vallejos-Sologuren C. The health minister's response to managing cervical cancer in low-income countries. Annals of Oncology. 2010;21:viii41 10.1093/annonc/mdq511. [DOI] [Google Scholar]
- 50.Binagwaho A, Ngabo F, Wagner CM, Mugeni C, Gatera M, Nutt CT, et al. Integration of comprehensive women's health programmes into health systems: Cervical cancer prevention, care and control in Rwanda Integration de programmes de soins complets pour les femmes dans les systemes de sante: Prevention, traitement et lutte contre le cancer du col de l'uterus au Rwanda. Bulletin of the World Health Organization. 2013;91(9):697–703. 10.2471/BLT.12.116087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ngabo F, Levin A, Wang SA, Gatera M, Rugambwa C, Kayonga C, et al. A cost comparison of introducing and delivering pneumococcal, rotavirus and human papillomavirus vaccines in Rwanda. Vaccine. 2015;33(51):7357–63. 10.1016/j.vaccine.2015.10.022. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Torres-Rueda S, Rulisa S, Burchett HED, Mivumbi NV, Mounier-Jack S. HPV vaccine introduction in Rwanda: Impacts on the broader health system. Sexual and Reproductive Healthcare. 2016;7:46–51. 10.1016/j.srhc.2015.11.006. [DOI] [PubMed] [Google Scholar]
- 53.Binagwaho A, Wagner CM, Gatera M, Karema C, Nutt CT, Ngabo F. Achieving high coverage in Rwanda's national human papillomavirus vaccination programme. Bulletin of the World Health Organization. 2012;90(8):623–8. 10.2471/BLT.11.097253. WOS:000307485500013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Botha MH, Van Der Merwe FH, Snyman L, Dreyer G. The vaccine and cervical cancer screen (VACCS) project-acceptance of human papilloma virus vaccination in a school based program. International Journal of Gynecological Cancer. 2014;4:821 10.1097/01.IGC.0000457075.08973.89 [DOI] [Google Scholar]
- 55.Dreyer G, Merwe FHvd, Botha MH, Snyman LC, Constant D, Visser C, et al. School-based human papillomavirus vaccination: an opportunity to increase knowledge about cervical cancer and improve uptake of screening. SAMJ South African Medical Journal. 2015;105(11):912–6. 10.7196/SAMJ.2015.v105i11.9814. . [DOI] [PubMed] [Google Scholar]
- 56.Hoque M, Van Guido H. The knowledge about, beliefs and attitudes of medical students regarding vaccination against the human papillomavirus, in south africa: A Cross-Sectional study. Biomedical Research (India). 2015;26(1):65–70. [Google Scholar]
- 57.Snyman LC, Dreyer G, Botha MH, Merwe FHvd, Becker PJ. The Vaccine and Cervical Cancer Screen (VACCS) project: linking cervical cancer screening to HPV vaccination in the South-West District of Tshwane, Gauteng, South Africa. SAMJ South African Medical Journal. 2015;105(2):115–20. 10.7196/samj.8418. . [DOI] [PubMed] [Google Scholar]
- 58.Tathiah N, Naidoo M, Moodley I. Human papillomavirus (HPV) vaccination of adolescents in the South African private health sector: Lessons from the HPV demonstration project in KwaZulu-Natal. South African Medical Journal. 2015;105(11):954 10.7196/SAMJ.2015.v105i11.10135. . [DOI] [PubMed] [Google Scholar]
- 59.Botha MH, van der Merwe FH, Snyman LC, Dreyer G. The vaccine and cervical cancer screen (VACCS) project: acceptance of human papillomavirus vaccination in a school-based programme in two provinces of South Africa. South African medical journal = Suid-Afrikaanse tydskrif vir geneeskunde. 2015;105(1):40–3. Epub 2015/06/06. . [DOI] [PubMed] [Google Scholar]
- 60.Katz IT, Nkala B, Dietrich J, Wallace M, Bekker LG, Pollenz K, et al. A Qualitative Analysis of Factors Influencing HPV Vaccine Uptake in Soweto, South Africa among Adolescents and Their Caregivers. PloS one. 2013;8(8). 10.1371/journal.pone.0072094. WOS:000323880200008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Moodley I, Tathiah N, Mubaiwa V, Denny L. High uptake of Gardasil vaccine among 9-12-year-old schoolgirls participating in an HPV vaccination demonstration project in KwaZulu-Natal Province, South Africa. Samj South African Medical Journal. 2013;103(5):318–21. 10.7196/samj.6414. WOS:000319721900023. [DOI] [PubMed] [Google Scholar]
- 62.Hutubessy R, Levin A, Wang S, Morgan W, Ally M, John T, et al. A case study using the United Republic of Tanzania: costing nationwide HPV vaccine delivery using the WHO Cervical Cancer Prevention and Control Costing Tool. BMC medicine. 2012;10:136 Epub 2012/11/14. 10.1186/1741-7015-10-136 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Quentin W, Terris-Prestholt F, Changalucha J, Soteli S, Edmunds WJ, Hutubessy R, et al. Costs of delivering human papillomavirus vaccination to schoolgirls in Mwanza Region, Tanzania. BMC medicine. 2012;10:137 10.1186/1741-7015-10-137. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Watson-Jones D, Baisley K, Ponsiano R, Lemme F, Remes P, Ross D, et al. HPV vaccination in Tanzanian schoolgirls: cluster-randomised trial comparing two vaccine delivery strategies. Journal of Infectious Diseases. 2012:jis407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Watson-Jones D, Changalucha J, Hayes R. Delivery, uptake and acceptability of HPV vaccination in Tanzanian girls: Final report and findings of the Mwanza Human Papillomavirus (HPV) Vaccination Project. Mwanza Intervention Trials Unit, National Institute for Medical Research Mwanza, London School of Hygiene and Tropical Medicine, Institute Catala d'Oncologia, Medical Research Council UK, World Health Organization, 2013.
- 66.Watson-Jones D, Tomlin K, Remes P, Baisley K, Ponsiano R, Soteli S, et al. Reasons for receiving or not receiving HPV vaccination in primary schoolgirls in Tanzania: a case control study. PloS one. 2012;7(10):e45231 Epub 2012/11/02. 10.1371/journal.pone.0045231 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Watson-Jones D, Lees S, Neke N, Mwanga J, Changalucha J, Ross D, editors. FEASIBILITY AND ACCEPTABILITY OF INTEGRATING ADOLESCENT HEALTH INTERVENTIONS WITH HPV VACCINATION IN TANZANIA. 29th International Papillomavirus Conference, HPV 2014; 2014; Washington, Seattle.
- 68.Watson-Jones D, Lees S, Mwanga J, Neke N, Changalucha J, Broutet N, et al. Feasibility and acceptability of delivering adolescent health interventions alongside HPV vaccination in Tanzania. Health policy and planning. 2016;31(6):691–9. Epub 2016/01/16. 10.1093/heapol/czv119 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Yothasamut J, Putchong C, Sirisamutr T, Teerawattananon Y, Tantivess S. Scaling up cervical cancer screening in the midst of human papillomavirus vaccination advocacy in Thailand. BMC health services research. 2010;10 Suppl 1:S5 Epub 2010/07/16. 10.1186/1472-6963-10-s1-s5 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Limpaphayom KK, Eamratsameekool W, Lu E. Implementing HPV vaccine to reach young girls in Thailand. Journal of Clinical Oncology. 2014;1. [Google Scholar]
- 71.Aujo JC, Bakeera-Kitaka S, Kiguli S, Mirembe F. No difference in sexual behavior of adolescent girls following Human Papilloma Virus vaccination: a case study two districts in Uganda; Nakasongola and Luwero. BMC public health. 2014;14:155 Epub 2014/02/14. 10.1186/1471-2458-14-155 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Galagan SR, Paul P, Menezes L, LaMontagne DS. Influences on parental acceptance of HPV vaccination in demonstration projects in Uganda and Vietnam. Vaccine. 2013;31(30):3072–8. 10.1016/j.vaccine.2013.04.056. WOS:000321178800007. [DOI] [PubMed] [Google Scholar]
- 73.Banura C, Mirembe FM, Katahoire AR, Namujju PB, Mbidde EK. Universal routine HPV vaccination for young girls in Uganda: a review of opportunities and potential obstacles. Infectious agents and cancer. 2012;7(24). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Katagwa VN, Opio RO, Niwasasira DN, Onyege A, Naisanga M, Bongomin FA, et al. Acceptability of human papilloma virus vaccination among primary school girls in Minakulu sub-county, northern Uganda. Eur J Cancer Prev. 2014;23(4):294–5. Epub 2014/05/30. 10.1097/CEJ.0000000000000021 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Katahoire AR, Wani JA, Murokora D, Mugisha E, LaMontagne DS. Acceptability of HPV vaccine among young adolescent girls in Uganda: Young people's perspectives count. International Journal of Child and Adolescent Health. 2013;6(2):211. [Google Scholar]
- 76.Mugisha E, LaMontagne DS, Katahoire AR, Murokora D, Kumakech E, Seruyange R, et al. Feasibility of delivering HPV vaccine to girls aged 10 to 15 years in Uganda. African health sciences. 2015;15(1):33–41. 10.4314/ahs.v15i1.5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Nakkazi E. Cancer vaccine boosted by infrastructure for HIV care in Africa. Nat Med. 2011;17(3):272 Epub 2011/03/09. 10.1038/nm0311-272a . [DOI] [PubMed] [Google Scholar]
- 78.Turiho AK, Okello ES, Muhwezi WW, Harvey S, Byakika-Kibwika P, Meya D, et al. Effect of school-based human papillomavirus (hpv) vaccination on adolescent girls' knowledge and acceptability of the HPV vaccine in Ibanda District in Uganda. African journal of reproductive health. 2014;18(4):45–53. Epub 2015/04/10. ; [PMC free article] [PubMed] [Google Scholar]
- 79.Jain KM, Paul P, LaMontagne DS. Monitoring adverse events following immunisation in developing countries: experience from human papillomavirus vaccination demonstration projects. Sexual health. 2013;10(1):57–63. 10.1071/SH11161. WOS:000314926700009. [DOI] [PubMed] [Google Scholar]
- 80.Turiho AK, Muhwezi WW, Okello ES, Tumwesigye NM, Banura C, Katahoire AR. Human papillomavirus (HPV) vaccination and adolescent girls' knowledge and sexuality in Western Uganda: A comparative cross-sectional study. PLoS ONE. 2015;10 (9) (no pagination)(e0137094). 10.1371/journal.pone.0137094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hasahya OT, Berggren V, Sematimba D, Nabirye RC, Kumakech E. Beliefs, perceptions and health-seeking behaviours in relation to cervical cancer: a qualitative study among women in Uganda following completion of an HPV vaccination campaign. Global health action. 2016;9:29336 Epub 2016/02/20. 10.3402/gha.v9.29336 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Cover JK, Nghi NQ, LaMontagne DS, Huyen DTT, Hien NT, Nga lT. Acceptance patterns and decision-making for human papillomavirus vaccination among parents in Vietnam: an in-depth qualitative study post-vaccination. BMC public health. 2012;12(1):629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.LaMontagne DS, Nghi NQ, Nga le T, Janmohamed A, Huyen DT, Hien NT, et al. Qualitative study of the feasibility of HPV vaccine delivery to young adolescent girls in Vietnam: evidence from a government-implemented demonstration program. BMC public health. 2014;14:556 Epub 2014/06/06. 10.1186/1471-2458-14-556 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Paul P, LaMontagne DS, Le NT. Knowledge of cervical cancer and HPV vaccine post- vaccination among mothers and daughters in Vietnam. Asian Pacific journal of cancer prevention: APJCP. 2012;13(6):2587–92. Epub 2012/09/04. . [DOI] [PubMed] [Google Scholar]
- 85.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. International journal of surgery (London, England). 2010;8(5):336–41. Epub 2010/02/23. [DOI] [PubMed] [Google Scholar]
- 86.World Health Organization. Principles and considerations for adding a vaccine to a national immunization programme: from decision to implementation and monitoring. World Health Organization, 2014. [Google Scholar]
- 87.Kabakama S, Gallagher KE, Howard N, Mounier-Jack S, Burchett HED, Griffiths UK, et al. Social mobilisation, consent procedures, and acceptability: a study of human papillomavirus vaccination in low and middle-income countries. BMC public health. 2016;9(16 (1)). 10.1186/s12889-016-3517-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Strategic Advisory Group of Experts (SAGE) on Immunization W. Evidence based recommendations on Human Papilloma Virus (HPV) Vaccines Schedules: Background Paper for SAGE Discussions. World Health Organization, 2014 March 11 2014. Report No.
- 89.World Health Organization. Human Papillomavirus vaccines: WHO position paper October 2014. 2014.
- 90.PATH. Cervical Cancer Library—HPV vaccine lessons learnt. http://www.rho.org/HPVlessons. 2015 [cited 2015 30th November].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
Data Availability Statement
All anonymised data are available publicly in the LSHTM Research Online repository; URL: http://researchonline.lshtm.ac.uk/3351522/.