Abstract
Present paper offers considerable information on traditional uses of medicinal plants by the inhabitants of Hafizabad district, Punjab-Pakistan. This is the first quantitative ethnobotanical study from the area comprising popularity level of medicinal plant species intendedby using relative popularity level (RPL) and rank order priority (ROP) indices.Ethnobotanical data were collected by interviewing 166 local informants and 35 traditional health practioners (THPs) from different localities of Hafizabad district. Demographic features of informants; life form, part used, methods of preparation, modes of application and ethnomedicinal uses were documented. Ethnobotanical data were analyzed using quantitative tools, i.e. Relative frequency citation (RFC), use value (UV), informant consensus factor (ICF) fidelity level (FL), RPL and ROP indices. A total of 85 species belonging to 71 genera and 34 families were documented along with ethnomedicinal uses. Solanum surattense, Withania somnifera, Cyperus rotundus, Solanum nigrum and Melia azedarach were the most utilized medicinal plant species with highest used value. The reported ailments were classified into 11 disease categories based on ICF values and highest number of plant species was reported to treat dermatological and gastrointestinal disorders. Withania somnifera and Ranunculus sceleratus with maximum FL (100%), were used against gastrointestinal and urinary disorders, respectively. The RPL and ROP values were calculated to recognize the folk medicinal plant wealth; six out of 32 plant species (19%) were found popular, based on citation by more than half of the maximum number of informant viz. 26. Consequently, the ROP value for these species was more than 75. The comparative assessment with reported literature revealed 15% resemblance and 6% variation to previous data;however79% uses of the reported species were recorded for the first time. The diversity of medicinal plant species and associated traditional knowledge is significant in primary health care system. Medicinal plant species with high RPL values should be screened for comprehensive phytochemical and pharmacological studies. This could be useful in novel drug discovery and to validate the ethomendicinal knowledge.
Introduction
Ethnomedicinal studies are of significant value to discover contemporary drugs from indigenous medicinal plant resources. There are appropriate sources of information about useful medicinal plant species, which can be targeted for management and domestication [1,2]. The documentation of traditional knowledge of native plant species has contributed a number of vital drugs [3,4]. Currently, 25% of herbal drugs in modern pharmacopeia are plant based and several synthetic drugs are manufactured by using chemical substances isolated from plants [5]. The fundamental role of natural products in the development of new drugs has been reported [6–8]. In recent era, the role of medicinal plant species in traditional health practice has diverted the attention of researchers towards ethnomedicines.
The use of plant species as traditional medicines provides a real substitute in healthcare services for rural communities of the developing nations [9]. It has been estimated that around 80% of the population in developing countries depends on traditional medicines for primary health care system. These traditional medicines are cost-effective, safe and affordable [5]. Globally, approximately 85% of the traditional medicines used in primary healthcare are derived from plantspecies [10]. Therefore, medicinal plants are the indigenous heritage of global importance [11]. Around, 50,000 flowering plants are used as medicinal [12], out 422,000 reported species of flowering plants [13]. At present, research on traditional uses of plant species has attained notableattention in the scientific community. Various workers have reported indigenous knowledge of medicinal plants from different parts of Pakistan [2,4,14–20], and few reports have been published in recent years [21–26].
The documentation of information on traditional herbal remedies is an important aspect of conservation approach. The present study, therefore, documents the traditional knowledge of local communities of Hafizabad district on medicinal uses of surrounding plant diversity. This work, being the first collation and listing of all available data on medicinal plants in this area, provides first ethnomedicinal and cultural assessment of these species. Specifically, present study was aimed: (i) to document the medicinal flora and traditional knowledge of local communities on indigenous plants used for medicinal purposes, (ii) to compile data on traditional treatments against various ailments, including method of preparation, plant part(s) utilization and application; (iii) to evaluate the ethnomedicinal data using RPL and ROP indices in order to explore most popular species, which could be useful for in depth pharmacological screening.
Materials and methods
Description of the study area
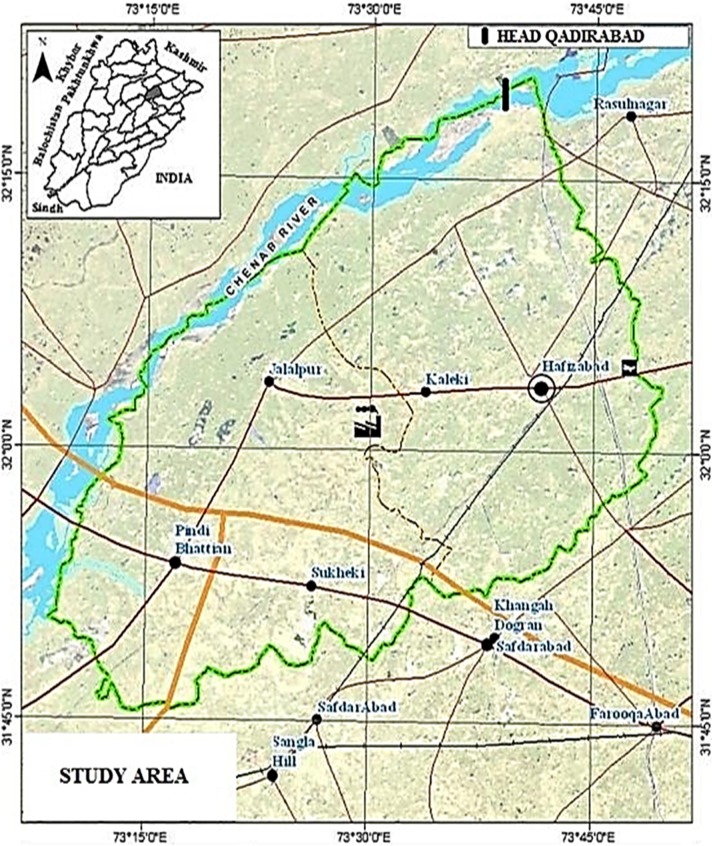
The present study was conducted to document the traditional knowledge of local communities on medicinal plant species from six localities i.e. Kaleke Mandi, Head Qadirabad, Hafizabad city, Sukhakee, Pindi Bhattian and Jalalpur of district Hafizabad, Punjab province-Pakistan (Fig 1). The study area lies between 32° 20′N and 73° 46′E, surrounded by Sheikhupura on south, Sargodha on west, Gujranwala on east and by Mandi Bahuadd in on north-west. The survey site spreads an area of 2,367 km2 along with altitudinal variation of 207m above sea level. The forest cover is approximately 550.4ha (0.23%) of the total of the district. The Chenab River spreads from north to north west of the district. Climate of the study area falls in semi-arid type with temperature ranged from 48°C (in summer) to 1°C (in winter). The study area receives highest rainfall during monsoon (July to September). The annual rainfall and humidity varies from 50–70mm and 25–85%, respectively [27,28]. According to Punjab development statistics 2011, total human population of the study area was 1,038,000, which includes: 52% males and 48% females. Around 27.26% of the population lives in urban areas, while remaining 72.74% comprises rural communities. The major ethnic group speaks Punjabi (98.7%), while other languages spoken are Urdu (0.8%), Pushto (0.4%) and Siraiki (0.1%).
Fig 1. Map of district Hafizabad-Pakistan.
Data collection and identification of plant species
Semi structured interviews and group conversation with local inhabitants were conducted to gather information on medicinal uses of plant species from 201 informants including male, female respondents and traditional healers. Data on age, gender, educational status and linguistics of respondents were also gathered. Information regarding the local plant names, part(s) used, methods of preparation and application were documented. The medicinal plant species used by the local communities of the study area were authenticated using the international plant name index (http://www.ipni.org), the plant list (www.theplantlist.org) and GRIN taxonomy site (http://www.ars-grin.gov/cgi-bin/npgs/html/queries.pl), while that of families follow A.P.G. system [29]. The species entries were complemented along with data on taxonomic position (family), vernacular name, common name, flowering period, life form and folk medicinal uses. The life form was categorized into herbs, shrubs, grasses and trees (annual, biennial or perennial), according to the system proposed by Raunkiær [30,31] and modified by Brown [32]. Collected plant species were identified by Prof. Dr. Rizwana Aleem Qureshi (Plant Taxonomist, Quaid-i-Azam University, Islamabad and by using Flora of West Pakistan [33] and Flora of Punjab [34]. The voucher specimens were submitted in Herbarium of Pakistan (ISL) Quaid-i-Azam University Islamabad.
Quantitative analysis
The ethnobotanical data was analyzed using different quantitative indices including Informant Consensus Factor (ICF), Use value (UV), Relative frequency citation (RFC), Fidelity level (FL), Relative popularity level (RPL), Rank order priority (ROP). Data were reported in proportions and percentages.
Informant consensus factor (ICF)
ICF value describes informants’ consensus on the medicinal plant consumption species, and evaluates variability in mode of utilization against reported diseases. Before calculating ICF value, ailments are broadly categorized into different categories [35]. The maximum ICF value i.e. close to 1 indicates that well known species are used by a large proportion of local communities due to their authenticity regarding diseases. However, low ICF index close to 0 specifies that the informants use this species randomly to treat reported diseases[35].
The ICF value was calculate using the formula as described earlier [36,37]:
Where, “Nur” is the total number of use reports for each disease category and “Nt” indicates the number of species used in said category.
Use value (UV)
Use value (UV) determines the relative importance on uses of plant species. It is calculated using the following formula as explained before [37,38]:
Where, “UV” indicates use value of individual species, “U” is the number of uses recoded for that species and “N” represents the number of informants who reported that species.
Relative frequency of citation (RFC)
Relative frequency of citation(RFC)signifies the local importance of each species in a study area [39,40]. This index is determined by dividing the number of informants citing a useful species (FC) by total number of informants in the survey (N). RFC is calculated by the formula as described earlier [41]:
Fidelity level (FL)
FL is the percentage of informants who mentioned the uses of certain plant species to treat a particular ailment in a study area. The FL index is calculated using formula as reported previously [42,43]:
Where, ‘Np’ is the number of informants that claimed a use of certain plant species for a particular disease and ‘N’ is the total number of informants citing the species for any disease. The maximum FL indicates the frequency and high use of the plant species for treating a particular ailment by the informants of the study area.
Relative popularity level (RPL)
RPL is the ratio between number of ailments treated by a particular plant species and the total number of informants for any disease. However, plant species with comparable FL may vary in their healing potential. A correction scale is therefore introduced, in which all the encountered plant species are divided into popular and unpopular groups. The relative popularity level (RPL) assumes a value 0 and 1.0, with ‘1’ being complete popularity of a plant for major ailments and ‘0’ no ailments treated by a plant species. When all plant species are frequently used to treat some major ailments, popularity index would be maximum (1.0); then decrease towards zero as the relative popularity of the species diverge away from popular side. For popular plant species, the RPL value is rationally selected to equal unity (i.e. equal to 1), while RPL value is less than 1 for unpopular plant species. The relative popularity level (RPL) of the plant species is calculated and designated as popular or unpopular. The RPL value may be determined for each specific plant in accordance with its exact position on graph [43,44].
Rank order priority (ROP)
ROP is a correction factor, used for appropriate ranking of the plant species with different FL and RPL values. The ROP is derived from FL; by multiplying RPL and FL values as explained earlier [43,44].
Results and discussion
Demographic features of the informants
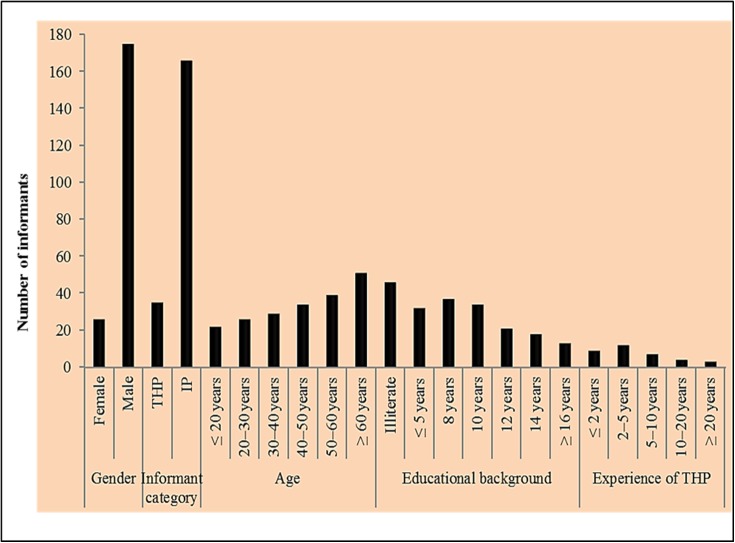
A total of 201 local informants including 175 males and 26 females were interviewed. Based on demography these informants were categorized into different classes as given in Fig 2. In the present survey male participants were higher than females. The prevalence of male informants is due to the fact that females of the study area were reluctant in conversation with male strangers (the interviewers). The local informants were farmers, foresters or herdsmen, craftsmen, shopkeepers, teachers and housewives. The traditional health practioners (THPs) hold significant information on the medicinal uses of local plant species to treat various ailments. THPs were classified into five groups on the basis of their experience such as THPs having less than 2 years’ experience (9), THPs with 2–5 years’ experience (12), THPs of 5–10 years’ experience (7), THPs of 10–20 years’ experience (4) and 3 THPs have more than 20 years’ experience. Among others, maximum informants having traditional knowledge regarding the use of medicinal plants were fall in secondary school education level or even below this and often spoke only Punjabi language. The maximum information was collected from the informants above 60 years age possess significant traditional knowledge whereas little information was shared by young respondents. Moreover, illiterate informants shared possess more information on the traditional use of medicinal plant species compared to educated respondents. This may be due to changing lifestyle, increase in the use of allopathic medicine and urbanization. Similar findings have also been reported from Bangladesh [45]and Turkey[9,46].
Fig 2. Demographic data of local informants (THPs. traditional health practioners, IP. indigenous peoples).
Taxonomic classification
In total 85 medicinal plant species belonging to 71 genera and 34 families were documented(Table 1). All reported species were angiosperms, which include: monocotyledonous and dicotyledonous groups (10.6 and 89.4%, respectively). Asteraceae and Poaceae were the most dominant families (with 9 species each), followed by Fabaceae (8 species), Moraceae and Euphorbiaceae (6 species each), Chenopodiaceae (5 species), Malvaceae and Solanceae (4 species each), Amaranthaceae (3 species) and Meliaceae, Myrtaceae, Oleaceae, Polygonaceae and Rhamnaceae (2 species each), while other families were represented by one species only (S1 Fig) The utilization of medicinal plant species belonging to Asteraceae and Poaceae families was in agreement with ethnomedicinal flora reported from other parts of Pakistan and in other areas of the world [23,47–49]. This may be due to their wide distribution of plant species belonging to Asteraceae [50] and Poaceae [51] and their traditional uses known by the indigenous communities living in different parts of the world.
Table 1. Ethnomedicinal plant species of the study area.
| S #. | Plant species with families and Accession number | Common Name | Local Name | Flowering Period | A Life Habits/ Life forms | B Part (s)/Mode of utilization | Application mode | Therapeutic uses | CRFC | CUV | D Previously Used | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Achyranthes aspera L. Amaranthaceae, HAF-01 | Prickly-Chaff flower | Puthkanda | March-October | W | H | P | WP. decoction, extract; ST. powder; LE. paste, powder; RT. decoction; RT. juice | Oral, Topical and as Toothbrush | Pneumonia, kidney stone, ulcer, chest pain, external wounds, dysmenorrhea, toothache, asthma | 0.11 | 0.43 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 2 | Amaranthus spinosus L. Amaranthaceae, HAF-02 | Spiny pigweed | Gnar | May-July | W | H | A | LE. cooked, juice, extract; RT. juice, decoction; SD. powder; BA. decoction | Oral, Gargle | Anthelminthic, stomachache, diuretic, cataract, toothache, constipation | 0.09 | 0.32 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 3 | Amaranthus viridis L. Amaranthaceae, HAF-03 | Slender amaranth | Ganhar | March-October | W | H | A | LE. extract, cooked, juice. paste; SD. powder; RT. decoction | Oral, Topical | Cough and asthma, eye vision, constipation, file, painful urination, snakebite | 0.08 | 0.35 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 4 | Mangifera indica L. Anacardiaceae, HAF-04 | Mango | Aam | March-April | C | T | P | LE and BA. latex; FR. juice; LE. decoction, paste. infusion; SD. extract | Topical, Oral | Heel cracks, diarrhea, fever, snake bite, diabetes, blood pressure | 0.14 | 0.21 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 5 | Anethum graveolens L.* Apiaceae, HAF-82 | Dill | Sowa | May-July | W/C | H | A/P | LE. powder, infusion; SD. powder | Oral | Indigestion, flatulence, bronchitis | 0.10 | 0.14 | 26◆101∎21◆102●103∎104◆66●105∎80◆◆ |
| 6 | Calotropis procera Br. Asclepiadaceae, HAF-05 | Milk weed | Akh | Throughout the year | W | S | P | LE. paste, extract, poultice. latex; ST. latex; ST and LE. decoction | Oral, Topical and as Inhale | Wound healing, asthma, toothache, T.B., hepatitis, burns, malarial fever, lice killer | 0.13 | 0.31 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 7 | Ageratum conyzoides L. Asteraceae, HAF-06 | Goat weed | Knaar | July-September | W | H | A | LE. paste, juice, extract; FL. decoction; ST. powder; WP. juice; RT. juice | Oral, Topical and as Eye drop | Cut and wounds, fever, flu and cough, infertility, jaundice, hair tonic, conjunctivitis, stomachache | 0.12 | 0.36 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 8 | Cirsium arvense (L.) Scop* Asteraceae, HAF-07 | Creeping thistle | Kandaal/Leh | May-August | W | H | P | LE. Juice; ST.FL.RT. decoction | Topical, Oral | Wounds, peptic ulcer, tonic, cough and bronchitis | 0.06 | 0.33 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 9 | Conyza ambigua DC.Asteraceae, HAF-08 | Hairy fleabane | Gider buti | August-October | W | H | A/P | WP. Extract; RT. Decoction; LE. Infusion, juice | Oral | Diarrhea and dysentery, painful menstruation, bleeding piles, diabetes, hypertension | 0.08 | 0.47 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 10 | Coronopus didymus (L.) Sm. Asteraceae, HAF-09 | Swine-cress | Jangli haloon | May-August | W | H | A/B | ST. powder; LE. infusion; WP. Juice; SH. Extract; FL. decoction | Oral, Topical | Bone fracture, tumors, rheumatism, blood purifier, nerve tonic, cold, fever and flu | 0.13 | 0.33 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 11 | Eclipta alba (L.) Hassk Asteraceae, HAF-10 | Trailing ecliptic Plant | Sofed banghara | July-October | W | H | P | WP. Powder, poultice, decoction; LE. powder, juice/tea; RT. decoction | Oral, Topical | Malarial fever, burns, blood purifier, burning urination, liver cancer, hair tonic | 0.15 | 0.37 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 12 | Launaea procumbens Roxb. Asteraceae, HAF-12 | Creeping-launaea | Pili dodhak | March-August | W | H | P | LE. extract, powder, paste; WP. infusion | Oral, Topical | Dysuria, ringworm, fever, galactagogue | 0.10 | 0.20 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 13 | Parthenium hysterophorus L* Asteraceae, HAF-14 | Feverfew | Gandi boti | April-August | W | H | A/P | LE. juice, extract; WP. juice, decoction; FL. Powder; RT. Juice | Oral | Constipation, toothache, vermifuge, diabetes, emmenagogue, tonic | 0.05 | 0.60 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 14 | Sonchus asper Hill. Asteraceae, HAF-11 | Spiny leaved so whistle | Asgandh | May-July | W | H | A | LE.RT. SH. decoction; LE. paste; WP. powder | Oral, Topical | Fever, cough, asthma, constipation, wounds, dyspepsia | 0.11 | 0.27 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 15 | Xanthium strumarium L. Asteraceae, HAF-13 | Cocklebur | Chhota dhatura | May-July | W | H | A | LE. decoction, powder; FR. decoction; RT. Powder | Oral, Topical and as Toothbrush | Malarial fever, skin burn, paralysis, stomachache, small pox, scrofulous tumors, dental soreness | 0.07 | 0.47 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 16 | Brassica rapa L. Brassicaceae, HAF-16 | Field mustard | Sarsoon | January-March | C | H | B | LE. decoction; WP. cocked; SD. powder | Oral, Topical | Skin edema, blood purifier, tonic | 0.09 | 0.16 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 17 | Sisymbrium irio L. Brassicaceae, HAF-15 | London rocket | Khoob kalan | March-May | W | H | A | WP. juice; FR. infusion; decoction, powder; SD. poultice | Oral, Topical | Ophthalmia, mumps and measles, dyspepsia, face pimples, cuts and wounds | 0.11 | 0.22 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 18 | Cassia fistula L. Caesalpiniaceae, HAF-17 | Golden shower | Amaltas | April-June | W | T | P | FR. BA. Powder; FL. ash; LE. decoction, paste; RT. powder | Oral, Topical | Constipation, gastric, jaundice, cough, urinary tract infection, eczema, wounds, rheumatism | 0.10 | 0.38 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 19 | Capparis deciduas (Forssk.) Edgew Capparidaceae, HAF-18 | Caper plant | kerda, kair | April-July | W | T | P | FL.ST.RT. powder; FR. BA. powder; SH. decoction; LE. paste; FL.SD. decoction | Oral, Topical | Male sexual dysfunction, hemolytic anemia, vermifuge, stomachache, liver tonic, boils and swellings, sciatic | 0.05 | 0.64 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 20 | Stellaria media L. Caryophyllaceae, HAF-19 | Chickweed | Gandhar | April-August | W | H | A | WP. decoction; SD. LE. paste, extract, poultice | Oral, Topical | Regular bowl, itchy skin, wounds, swelling joints, bone fracture | 0.11 | 0.23 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 21 | Chenopodium album L. Chenopodicaeae, HAF-20 | Lamb’s quarter | Bathu | January-September | W/C | H | A | LE. juice, infusion; WP. cooked; RT. decoction; SH.FL. juice | Oral | Laxative, gastritis, hepatic and urinary disorder, rheumatism, constipation, vermifuge | 0.11 | 0.74 |
26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 22 | Chenopodium ambrosioides L. Chenopodicaeae, HAF-21 | Sweet pigweed | Chandanbathwa | April-February | W | H | A/P | FL. juice; LE. infusion, powder, decoction; WP. juice; SH.FL. juice | Oral, Topical | Hypertension, menstrual disorders, hemorrhoids, toothache, constipation, stomachache | 0.10 | 0.35 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 23 | Chenopodium murale L. Chenopodicaeae, HAF-22 | Australian-spinach | Karund | January-July | W | H | A | WP. decoction; LE.ST. paste; LE. powder, decoction; SD. powder + | Oral, Topical and as Snuff | Stomachache, lameness, cough and cold, infertility, vermifuge | 0.08 | 0.29 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 24 | Kochia indica Wight* Chenopodicaeae, HAF-24 | Indian bassia | Boi | July-October | W | H | A/B | FR; LE. decoction, oil | Oral, Gargle | Heart tonic, diuretic, toothache, | 0.04 | 0.38 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 25 | Suaeda fruticosa Forsk. Chenopodicaeae, HAF-23 | Seep weed | Khaari | April-September | W | S | P | LE. decoction, juice; ST. decoction, ash; WP. decoction | Oral, Topical | Diuretic, blood purifier, liver cancer, snake bites, kidney stone, hair tonic | 0.08 | 0.41 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 26 | Convolvulus arvensis L. Convolvulaceae, HAF-25 | Deer’s foot. | Lehli/Vahri | Throughout the year | W | H | A/P | RT.WP. cooked, extract; LE. juice, paste | Oral, Topical | Constipation, blood purification, rheumatic pain, hair tonic, skin ulcer | 0.08 | 0.38 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 27 | Cyperus rotundus L. Cyperaceae, HAF-26 | Nut grass | Daila | April-July | W/C | H | P | RT. infusion; LE. decoction, paste; RH. powder, paste, decoction | Oral, Topical | Diuretic, vermifuge, dermatitis, stomachache, galactagogue, hypersplenism | 0.12 | 0.84 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 28 | Chrozophora tinctoria (L.) A.Juss* Euphorbiaceae, HAF-27 | Giradol | Neeli Booti | January-September | W | H | A | LE. juice, decoction, extract; ST. juice | Oral, Eye drop | Stomachache, sore throat, emetic, cataract | 0.07 | 0.20 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 29 | Croton sparsiflorus Morong Euphorbiaceae, HAF-32 | Herb pimento | Ban tulsi | April-July | W | H | P | LE. poultice, decoction, juice; RT. powder; ST. juice; WP. juice, decoction | Oral, Topical | Bone fracture, gastric ulcer, hemorrhage, hair tonic, dermatitis, dengue fever, cardiac tonic | 0.05 | 0.64 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 30 | Euphorbia dracunculoides Lam. Euphorbiaceae, HAF-31 | Dragon spurge | Bamburi | November-April | W | H | A/P | LE. juice, paste, powder; FR. juice | Oral, Topical | Lice killer, headache, skin parasites, snake bite, epilepsy | 0.09 | 0.28 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 31 | Euphorbia helioscopia L. Euphorbiaceae, HAF-28 | Sun euphorbia | Chhatri dodak | January-July | W | H | A | RT.WP. juice, latex, powder; SH; SD | Oral, Topical, Eye drop | Anthelminthic, athlete’s foot, eye sores, asthma, constipation, cholera | 0.11 | 0.39 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 32 | Euphorbia pilulifera L. Euphorbiaceae, HAF-29 | Asthma weed | Doddak | July-December | W | H | A | LE. juice; FL and SD. powder; WP. decoction, latex, juice | Oral, Topical and as Eye drop | Asthma, cough, stomachache, diarrhea, eye redness, burns, cut and warts | 0.09 | 0.39 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 33 | Euphorbia prostrate L* Euphorbiaceae, HAF-30 | Creeping spurge | Doodi buti | Throughout the year | W | H | P | WP. extract, latex, decoction; LE. infusion | Oral, Topical | Diarrhea and dysentery, liver tonic, ringworm, blood purifier, diabetes, kidney stone | 0.12 | 0.29 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 34 | Acacia modesta Wall. Fabaceae, HAF-42 | Amritsar gum | Phulai | March-May | W | T | P | BA. powder; ST. gum, extract; LE. extract; LE. ST. latex; BA. ass | Oral, Topical, Toothbrush | Toothache, carminative, tonic, cooling agent, back pain, bronchitis, asthma | 0.06 | 0.54 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 35 | Acacia nilotica L. Fabaceae, HAF-41 | Babul acacia | Kikar | March-August | W | T | P | BA. powder, decoction; LE. decoction, paste; ST. gum; BA. ash; LE. paste; FL. powder | Oral, Anal and as Toothbrush | Hyperglycemia, stomach-ache, dysentery, backbone and joints pain, toothache, piles, jaundice | 0.10 | 0.38 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 36 | Alhagi maurorum Medik. Fabaceae, HAF-58 | Camel thorn | Jawansa | April-September | W | S | P | RT. decoction; FR. powder; LE. decoction; RT. infusion; WP. decoction; SD. powder | Oral, Topical | Kidney stone, bleeding piles, constipation, cough, asthma, blood purifier, rheumatic pain, burn | 0.07 | 0.53 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 37 | Dalbergia sissoo Roxb. Fabaceae, HAF-57 | Indian rose wood | Tali | March-May | W | T | P | LE. decoction, paste, infusion; BA. decoction; BA. powder; | Oral, Topical | Emetic, diarrhea and vermifuge, cut and wounds, fever, nosebleed, constipation, hair tonic | 0.08 | 0.44 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 38 | Pongamia pinnata (L.) Pierre Fabaceae, HAF-56 | Pongam oil tree | Sukh chain | April-May. | C | T | P | ST; LE. powder; SD. oil; BA. decoction; FL. powder; RT. juice | Oral, Topical | Toothache, carminative, rheumatism, vermifuge, diabetes, wounds and ulcer | 0.08 | 0.35 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 39 | Prosopis cineraria L. Fabaceae, HAF-43 | Prosopis | Jhand | December-March | W/C | S | P | LE. juice, paste; BA. powder; ST. decoction; FL. powder; FR. paste, powder | Oral, Topical, Eye drop | Liver tonic, boils and blisters, scorpion bite, pancreatic stone, leucorrhoea, chronic dysentery, cataract | 0.09 | 0.42 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 40 | Prosopis juliflora Swartz* Fabaceae, HAF-40 | Honey mesquite | Mosquit pod | March-June | W | T | P | WP. decoction; FL. infusion; ST.LE. juice, poultice; BA. powder | Oral, Topical and as Toothbrush | Galactagogue, kidney stones, toothache, breast cancer, asthma, boils | 0.07 | 0.40 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 41 | Trifolium resupinatum L* Fabaceae, HAF-55 | Reversed clover | Loosin | April-August | W | H | A | WP. decoction, infusion; FL. powder | Oral, Gargle | Sore throat, cough, skin sores, ulcer, sedative, liver tonic, digestion | 0.09 | 0.39 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 42 | Oxalis corniculata L. Geraniaceae, HAF-33 | Clover sorrel | Khatti buti | March-December | W | H | P | LE. cocked, paste, cooked; WP. decoction, powder; RT. decoction | Oral, Topical and as Eye drop | Diarrhea and dysentery, wounds, hepatitis and jaundice, eye ache, anthelminthic, premature ejaculation | 0.09 | 0.37 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 43 | Hibiscus rosa-sinensis L. Malvaceae, HAF-37 | Rose mallow | Gurhal | Throughout the year | C | S | P | FL. powder, juice; LE. paste, juice, tea; RT. powder | Oral, Topical | Sexual dysfunction, eczema, heart burn, loss of appetite, asthma, regular bowl, leucorrhoea | 0.09 | 0.74 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 44 | Malva parviflora L. Malvaceae, HAF-34 | Cheese-weed | Sonchal | May-September | W | H | A | SD. decoction; SH.SD. decoction; SH. LE. decoction, extract, poultice | Oral, Topical | Cough and bronchitis, abortifacient, throat-ache, cough, fever, constipation, scorpion sting | 0.11 | 0.32 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 45 | Malvastrum tricuspidatum A. Gray * Malvaceae, HAF-35 | False mallow | DhamniButi | December-August | W | H | A | LE. poultice, paste, decoction; WP. powder | Oral, Topical | Sores and wounds, eczema, asthma, diarrhea | 0.04 | 0.44 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 46 | Malvaviscus arboreus (Torr. & Gray) Schery Malvaceae, HAF-36 | Sleeping hibiscus | Max mallow | Throughout the year | C | S | P | FL. decoction, infusion; LE. decoction, juice | Oral, Topical | Sore throat, diarrhea, fever, lice killer | 0.03 | 0.67 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 47 | Azadirachta indica A. Juss. Meliaceae, HAF-39 | Neem | Neem | April-May | W/C | T | P | LE. decoction, infusion, paste; SD. oil; ST.BA. decoction; LE. paste | Oral, Topical, Toothbrush | Blood purifier, diabetes, malaria, intestinal worm, headache, toothache, liver tonic, rheumatism, small pox | 0.13 | 0.33 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 48 | Melia azedarach L. Meliaceae, HAF-38 | Chinaberry | Dhraikh | May-July | W/C | T | P | LE. decoction, juice, paste, extract, infusion; BA. powder; ST. decoction | Oral, Topical, Bath | Malarial fever, allergy, wound healing, blood purifier, urinary stones, high blood pressure, diabetes | 0.07 | 0.79 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 49 | Ficus benjamina L* Moraceae, HAF-44 | Weeping fig | Kabar | October-January | W | T | P | ST. decoction; WP. powder; LE. decoction; FR.BA and LE. cocked | Oral, Topical | Stomachache, blood purification, ulcers, carminative, joint and back pain | 0.06 | 0.42 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 50 | Ficus racemosa L. Moraceae, HAF-45 | Cluster tree | Gular | March-May | W/C | T | P | ST. latex; LE. juice; BA. FR. powder, decoction | Oral, Topical, Anal | Piles, diarrhea, obesity, carminative, boils and ulcer | 0.09 | 0.37 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 51 | Ficus religiosa L. Moraceae, HAF-46 | Sacred fig | Pipal | March-October | W | T | P | LE. decoction, paste, infusion; FR. powder; ST. powder; RT. extract | Oral, Topical | Body pain, asthma, gonorrhea, skin ulcer, heart blockage, diabetes | 0.11 | 0.27 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 52 | Ficus virens L. Moraceae, HAF-47 | White fig | Palakh | October-March | W | T | P | FR. powder; BA. infusion; ST. latex | Oral | Diabetes, ulcer, breast cancer | 0.06 | 0.25 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 53 | Morus alba L. Moraceae, HAF-48 | White mulberry | Shahtoot | April-September | C | T | P | FR. decoction, juice; ST. latex; WP. decoction; LE. juice; BA and LE. decoction | Oral, Topical | Constipation, cough, liver tonic, tonsils, snakebite, diabetes | 0.11 | 0.74 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 54 | Morus nigra L* Moraceae, HAF-49 | Black mulberry | Kala toot | March-July | C | T | P | WP. decoction; FR. juice, decoction; LE. decoction, infusion; RT. powder | Oral, Gargle | Asthma, throat ache, cough, flu, toothache, constipation, carminative, intestinal worms, diabetes | 0.13 | 0.74 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 55 | Eucalyptus camaldulensis (A.) Cunn. Myrtaceae, HAF-51 | River red-gum | Safaida | April-October | W | T | P | LE. decoction; juice, extract | Oral, Gargle | Common cold, sinusitis, sore throat, cough, flu, fever | 0.10 | 0.29 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 56 | Psidium guajava L. Myrtaceae, HAF-50 | Guava | Amrud | March-April | C | S | P | FR.LE. infusion, decoction, extract; FL. decoction | Oral, Gargle | Diarrhea, diabetes, diuretic, carminative and vermifuge, toothache, fever, flu, cough | 0.11 | 0.78 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 57 | Boerhavia diffusa L. Nyctaginaceae, HAF-52 | Horse-purslane | Itsit | September-August | W | H | A/P | WP. infusion; LE. paste; RT. decoction, powder | Oral, Topical | Dysmenorrheal, snakebite, kidney failure, cough, flu and asthma | 0.10 | 0.29 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 58 | Jasminum officinale L* Oleaceae, HAF-53 | Poet's jasmine | Malti | May July | C | S | P | ST. juice, extract; FL. decoction; LE. sap, extract; WP. extract | Oral, Topical | High fever, intestinal worms, conjunctivitis, diarrhea, scabies, heart burn and cough | 0.07 | 0.73 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 59 | Jasminum sambac (L.)Ait. Oleaceae, HAF-54 | Arabian jasmine | Motia | April-June | C | S | P | FL. juice; LE. paste, decoction, juice, extract; RT. decoction | Oral, Topical | Conjunctivitis, wound and acne, insomnia, emmenagogue, ulcer, breast tumors, high fever | 0.05 | 0.64 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 60 | Cenchrus pennisetiformis Hoschst. & Steud. Poaceae, HAF-60 | White buffalo grass | Cheetah gha | February-April | W | G | A/P | LE. extract, juice, infusion; FR. decoction; ST. juice | Oral, Topical | Asthma, T.B., Cough, bleeding piles, epilepsy, skin irritation, eczema | 0.07 | 0.50 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 61 | Cynodon dactylon Pers. Poaceae, HAF-61 | Bermuda grass | Khanbalgha | May-September | W | G | P | RH. oil, decoction WP. decoction, paste, juice; RT. infusion | Oral, Topical and as Eardrop | Hypertension, kidney stones, itching, eye pain, earache, indigestion | 0.07 | 0.73 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 62 | Dactyloctenium aegyptium Beauv. Poaceae, HAF-62 | Crow’s foot grass | Madhanagha | July-October. | W | G | A | SD; RT; WP. paste | Oral, Topical | Kidney stones, uterus problem, stomachache, wounds and ulcer | 0.04 | 0.67 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 63 | Dicanthium annulatum Stapf. Poaceae, HAF-63 | Ringed dichanthium | Murgha gha | March-November | W | G | P | LE. ST. decoction; LE. juice, infusion, paste; ST. powder | Oral, Topical | Abortifacient, diarrhea, indigestion, piles, antispasmodic, scabies | 0.06 | 0.50 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 64 | Eleusine indica (L.) Gaertn. Poaceae, HAF-64 | Goose grass | Madhani | June-August | W | G | A | RH. Extract; RT. powder; LE. juice; WP. infusion, tea, decoction | Oral, Topical | Fever, dysentery, prolapse of uterus, diabetes, food poisoning, hair loss | 0.04 | 0.75 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 65 | Imperata cylindrical L. Poaceae, HAF-65 | Cogon grass | Dabh gha | March-November | W | G | P | LE. paste; RH. decoction; LE.SH. paste; RT. decoction | Oral, Topical | Tonic, cut and wounds, urodynia, hypertension, febrifuge | 0.04 | 0.56 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 66 | Setaria glauca Beauv* Poaceae, HAF-66 | Yellow foxtail | Bajra | May-October | W | G | A/P | ST. decoction; LE.ST.SD juice, infusion | Topical | Wound healing, dermatitis, ring worm, tonic, hair tonic | 0.03 | 0.71 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 67 | Sorghum halepense Pers* Poaceae, HAF-67 | Johnson grass | Baru/Lamjack | May-October | W | G | P | RT. decoction; SD. powder; ST. juice | Oral, Topical | Indigestion, cough, boils, demulcent | 0.04 | 0.50 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 68 | Triticum aestivum L. Poaceae, HAF-59 | Wheat | Kanak | April-May | C | G | A | SH. decoction; SD. decoction, paste, powder; RT. decoction | Oral, Topical | Colon cancer, anemia, wound healing, late puberty, asthma, diabetes | 0.15 | 0.77 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 69 | Polygonum plebejum R. Br. Polygonaceae, HAF-68 | Small knotweed | Hind rani | March-June | W | H | A | WP. paste, powder, RT. decoction, SH. decoction, LE. extract | Oral, Topical | Eczema, galactagogue, pneumonia, liver-tonic, heartburn, regular bowl | 0.10 | 0.35 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 70 | Rumex dentatus L. Polygonaceae, HAF-69 | Toothed dock | Jangli palak | May-June | W | H | A | RT. powder, decoction; RH and LE. poultice; WP. decoction | Oral, Topical | Constipation, cuts and wounds, eczema, cooling agent | 0.05 | 0.64 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 71 | Anagallis arvensis L. Primulaceae, HAF-70 | Scarlet pimpernel | Bili booti | March-April | W | H | A | WP. juice, pate; FL.LE. decoction; ST. powder | Oral, Topical | Leprosy, skin ulcer, epilepsy, hepatitis | 0.09 | 0.22 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 72 | Ranunculus sceleratus L* Ranunculaceae, HAF-71 | Blister buttercup | Gul-e-ashrafi | March-April | W | H | A/B | WP. decoction, juice, infusion; SD; RT. paste | Oral, Topical | Asthma and fever, tonic, muscle hamstring, vermifuge, urinary incontinence | 0.14 | 0.25 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 73 | Ziziphus nummularia (Burm. f.) Wight &Arn. Rhamnaceae, HAF-73 | Jujube | Bair | March-June | W | S | P | LE. decoction, paste; FR. powder; BA. decoction | Oral, Topical | Tonic, diabetes, constipation, cold and sore throat, scabies | 0.09 | 0.26 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 74 | Zizyphus mauritiana Lam. Rhamnaceae, HAF-72 | Chinese apple | Bairi | July-September | W | T | P | LE.BA. decoction; LE. extract, decoction, juice; BA. powder; RT. decoction; | Oral, Topical, Bath, Gargle | Chicken pox, ulcers, diarrhea, asthma, toothache, jaundice | 0.10 | 0.30 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 75 | Murraya koenigii (L.) spreng. Rutaceae, HAF-74 | Curry leaf | Kari patta | April-June | C | T | P | LE. juice, decoction, infusion, paste; SD; BA. powder | Oral, Topical | Diabetes, diarrhea, skin eruption, rheumatic pain, eye pain, hair tonic | 0.07 | 0.79 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 76 | Veronica polita Fries* Scharopholariaceae, HAF-75 | Grey field speedwell | Veroni | March-May | W | H | A | LE.ST. cooked; LE and ST. decoction; LE. tea, juice | Oral | Indigestion, nerve-tonic, blood purifier, cough | 0.10 | 0.20 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 77 | Datura innoxia Mill. Solanaceae, HAF-79 | Thorn apple | Datura | May-October | W | S | P | SD. paste; WP. powder; LE. decoction, extract; ST. infusion; FR.RT. decoction | Oral, Topical and as Inhale | Piles, asthma, cough, laxative, lice killer, premature ejaculation, sedative and narcotic, rabies | 0.07 | 0.57 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 78 | Solanum nigrum L. Solanaceae, HAF-76 | Night shade | Mako | April-June | W | H | A | LE. decoction, powder cocked, LE. extract; LE and FL. juice; RT. pate; WP. decoction | Oral, Topical, Eye drop | Cuts and wounds, breast cancer, chicken pox, fever, diarrhea, ulcer, piles, cardiac pain, diabetes, sore eyes | 0.14 | 0.83 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 79 | Solanum surattense Burm.f. Solanaceae, HAF-77 | Thorny nightshade | Kundiari | Throughout the year | W | H | P | WP. decoction, cooked; RT. decoction; FR. paste; LE and FR. decoction; RT. decoction | Oral, Topical | High fever, foot cracks, vermifuge, liver tonic, wound healing, rheumatism, kidney stones, asthma | 0.17 | 0.86 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 80 | Withania somnifera (L.) Dunnel. Solanaceae, HAF-78 | Winter cherry | Asgandh | Throughout the year | W | H | P | LE. powder, paste, decoction; RT. powder; WP. powder; FR.FL. powder | Oral, Topical and as Snuff | Malaria, night mare, stomachache, asthma, breast cancer, diabetes, wounds, menstrual flow | 0.14 | 0.86 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 81 | Pterospermum acerifolium (L.) Willd* Starculiaceae, HAF-80 | Maple-leaved Bayer tree | Kanakchanpa | December-July | W/C | T | P | FL. infusion, decoction, paste; BA. powder | Oral, Topical | Anthelminthic, tonic, bleeding piles, body swellings, impotency | 0.04 | 0.56 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 82 | Tamarix aphylla (L.) Karst. Tamaricaceae, HAF-81 | Rukhh | Athel tamarisk | June-October | W | T | P | LE. decoction, poultice, paste; BA. ash | Oral, Topical | Fever, boils and wound healing, eye inflammation, cold and cough | 0.08 | 0.24 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 83 | Cannabis sativa L. Urticaceae, HAF-83 | Marijuana | Bhang | April-September | W/C | S | P | LE. infusion, paste, extract; SD. decoction; LE.SD. juice; WP. powder | Oral, Topical and as Inhale | Diarrhea, constipation, sedative, intoxicant, lice killer, diuretic and laxative, asthma, snake bite | 0.08 | 0.53 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 84 | Lantana camara L. Verbenaceae, HAF-84 | Lantana | Lantana | Throughout the year | W | S | P | FL. extract; RT. extract; LE. sap, juice, paste, decoction | Oral, Topical | Headache, ringworm, injuries, toothache, malaria, rheumatism, cuts and wounds, cold, cough | 0.06 | 0.69 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
| 85 | Tribulus terrestris L. Zygophyllaceae, HAF-85 | Puncture Vine | Gukhroo | Throughout the year | W | H | A/B | FR. decoction, powder; WP. decoction, powder; LE. paste | Oral, Topical | Dysentery and diarrhea, urodynia, irregular menstruation, wounds, dyspepsia | 0.13 | 0.27 | 26◆101∎21◆102●103∎104◆66●105∎80◆ |
A Habit/Life forms: W, Wild; C, Cultivated; H, Herbs; S, Shrubs; G, Grass; T, Trees; A, Annual; B, Biennial; P, Perennial
B Plant Part(s): LE, Leaf; FR, Fruit; RT, Root; ST, Stem; SH, Shoot; WP, Whole Plant; SD, Seed; FL, Flower; BA, Bark; RH, Rhizome
CRFC, Relative frequency of citation; UV, Use value
D(∎) = Plant with similar use(s); (●) = Plant with dissimilar use (s); (◆) = Plant not reported in previous study
* Plant species, which are newly reported in this study
The life forms of the reported species are mentioned in Table 1. The herbaceous flora constitutes highest contribution (44%) of the reported plant species, which is comparable to Mahmood et al. [2], who reported 54% contribution of wild herbs in medicinal plants used by the local communities of Gujranwala district, Pakistan. The herbaceous species comprise perennial, biennial and annuals (56.5, 1.2 and 27.1%, respectfully).Furthermore, wild and cultivate trees contribute (17 and 10%, respectively), wild grass (8%), wild and cultivate shrubs (9 and 7%, respectively), cultivated herbs (4%) and cultivated grasses (1%) in descending order (S2 Fig). These findings were in consistence with previous reports [19,49,52–56]. The frequent use of herbs by indigenous communities may be due to their accessibility and high efficacy in the treatment of diseases compared to other life form [57–60].It is well-known that the medicinal plants having perennial nature require prolonged period of growth i.e. about 6–8 years depending on the type of plant species. Therefore, the perennial life cycle is more prominent in medicinal plant species than annual [22,61–63].
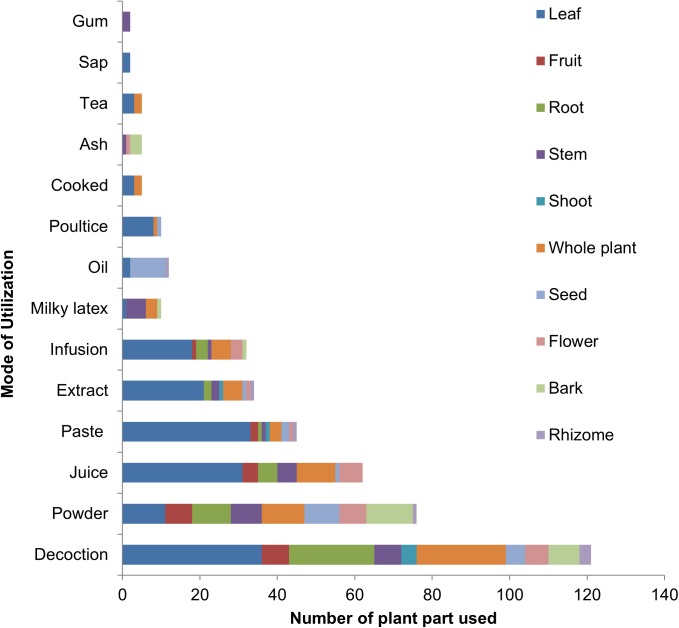
Plant part(s)used, mode of preparation and application
Even though all plant parts are significant in the treatment of different ailments; nevertheless in the present study as shown in Fig 3, leaves were the most commonly utilized plant part with38% application in traditional medicinal recipes, followed by whole plant (14%), root (10%), stem (8%), fruit, seed, flower (7% each), bark (5%), shoot and rhizome (2% each). Bradacs et al. [64] and Leto et al. [65]also reported leaves as commonly utilized plant part in herbal medicine used by the inhabitants of islands and Italy. It has been reported that the use of leaves is better for the survival of medicinal plants collected by herbalists compared to the collection of whole plant, roots and stem, which may cause severe threat to local flora [66].Even though some plant species such as Calotropis procera, Croton sparsiflorus, Datura innoxia, Euphobia spp., Lantana camara, Solanum spp. and Ranunculus sceleratus are consider as poisonous; however used to treat various ailments by local inhabitants. It has been reported that plant species with potent bioactive compounds are often characterized as poisonous and medicinal as well, and a beneficial or an adverse result may depends on method of drug preparation and utilization [67]. It was observed that inhabitants of the study area use above mentioned species in modest quantity, therefore no toxic effect was mentioned by respondents.
Fig 3. Proportional contributions of plant part in herbal preparations.
Local inhabitants of the study area use different methods i.e. decoction, extract, juice, powder, paste, infusion, poultice, tea, and ash etc. to prepare a recipe for the treatment of various ailments (Fig 3). Decoction was the most common method of drug preparation (121 applications), followed by powder, juice, paste, extract and infusion (76, 62, 45, 34 and 32 applications, respectively). Whereas, milky latex and oil were used in 12 applications each, poultice in 10 applications, cooked food, tea and ash with 5 applications each and plant sap with 2 applications. Such a wide array of preparation methods has also been reported previously from different parts of Pakistan [2,23,68,69] and in other countries [49,70–74]. The traditional healers of the study area also use more than two plant species along with other ingredients i.e. milk, honey, egg, butter, salt, sugar and water etc. The widespread use of decoction and powder in the study area is comparable to Mahmood et al. [2], Ahmad et al. [68] and Boudjelal et al. [75] who reported decoction as a most commonly utilized method of preparation followed by powder. Decoction is used as one of the major practices to prepare drug in traditional healing system, because it is easy to make by mixing with tea, water or soup [76,77].While making decoction, plant material is boiled in water until volume of the water reduced to one-fourth of its original volume [69], whereas crude extract is obtained by squeezing or crushing the plant parts [78].
As far as mode of administration is concerned, around 69% medications were taken orally (S3 Fig), followed by administered topically (24%), as eye drops and gargle (2% each), and as toothbrush, inhale and anal application (1% each). These findings were comparable to earlier reports [45,79,80]. Moreover, some herbal preparations were used for bathing, sniff and as eardrops. The medicinal plant species used as sniff are burnt to inhale fumes. Likewise, some plant parts were just crushed and smelled. Similar modes of applications were reported in Gujranwala [2]. The leaf and bark of some plant species are boiled and decoction is used to take bath against body pain. However, the trend of herbal bath is declining due to changing life style and now days only the leaves of Zizyphus mauritiana are used to bath the dead bodies. For topical use, direct application of paste, poultice or medicated oil are common, which are mostly used to treat skin infections, cuts, wounds, scorpion bites, rheumatism headache and body pain.
Informant consensus factor (ICF)
To calculate ICF, the reported ailments were first classified into 11 different disease categories on the basis of their use reports (Table 2).Among three major disease categories, dermatological disorders were dominated with 111 use-reports, followed by glandular complaints and respiratory diseases (76 and 52 use-reports, respectively) as mentioned in S4 Fig. Around 79.1% plant species were used to treat dermatological ailments, followed by gastrointestinal track (GIT) disorders, glandular complaints, respiratory diseases, ENEM diseases, cardiovascular disorders, urinary problems, muscle and skeletal disorders, sexual diseases and nervous disorders (76.7, 62.8, 47.7, 33.7, 25.6, 24.4, 23.3, 22.1 and 14%, respectively). These findings signify that dermatological and GIT disorders are prevalent in the study area. Similar findings have already been reported [53,64,65,81–86]. However, Kadir et al. [45] and Singh et al. [57]described more number of species to treat gastrointestinal diseases compared to dermatological ailments. The ICF value of different disease categories was ranged from0 (nervous disorder) to 0.39 (GIT diseases) The average ICF value for all categories was 0.16, which was similar to previous studies carried out in Pakistan [23,48].
Table 2. Informant consensus factor (ICF) of reported plant species against various ailments.
| Category of Diseases | Number of use reports | % age of use reports | Number of taxa used | % age of taxa | *ICF |
|---|---|---|---|---|---|
| GIT diseases | 107 | 21.9 | 66 | 76.7 | 0.39 |
| Respiratory diseases | 52 | 10.6 | 41 | 47.7 | 0.22 |
| Muscles and Skeletal disorders | 23 | 4.7 | 20 | 23.3 | 0.14 |
| Urinary disorders | 22 | 4.5 | 21 | 24.4 | 0.05 |
| Sexual diseases | 20 | 4.1 | 19 | 22.1 | 0.05 |
| Glandular disorders | 76 | 15.5 | 54 | 62.8 | 0.29 |
| Ear, Nose, Eyes and Mouth (ENEM) disease | 31 | 6.3 | 29 | 33.7 | 0.07 |
| Nail, Skin and Hair disorders | 111 | 22.7 | 68 | 79.1 | 0.39 |
| Nervous disorders | 12 | 2.5 | 12 | 14.0 | 0.00 |
| Cardiovascular disorders | 23 | 4.7 | 22 | 25.6 | 0.05 |
| Body energizers | 11 | 2.2 | 10 | 11.6 | 0.10 |
*ICF = Informant Consensus Factor
Relative frequency of citation (RFC) and use value (UV)
The RFC and UV indices are applied to select potential plant species for further pharmacological study and recommendation in drug development. The relative frequency citation (RFC) index authenticates the frequency of citation of a medicinal plant species used for various ailments. The RFC of the reported species ranged from 3to 17% (Table 1). However, on average, the RFC was9%. The highest RFC was calculated for Solanum surattense (0.17), Eclipta alba (0.15) and Triticum aestivum (0.15).The positions of these plant species correspond to the fact that they were reported by maximum number of informants, therefore having high frequency of citation (FC).
The use value (UV) index demonstrates the relative importance of plant species and families for a population [87]. In the present investigation, the UV of the reported medicinal plant species varied from 0.14 to 0.86 (Table 1). The highest UV was calculated for Solanum surattense and Withania somnifera (UV = 0.86, for each), Cyperus rotundus (UV = 0.84) and Solanum nigrum (UV = 0.83). These findings demonstrate the extensive use of above mentioned species in the treatment of various ailments by local inhabitants/healers and the consciousness of indigenous peoples, which makes such medicinal plants, the first choice to treat a disease. The lowest UV of Anethum graveolens, Brassica rapa and Chrozophora tinctoria may be due to less accessibility and minimum ethnobotanical uses. The results of UV in the present study were comparable with previously reported from Gujranwala, Pakistan [2].It has been reported that S. surattense exhibits hepato-protective[88], anti-asthmatic[89],antioxidant, anthelmintic, antimicrobial[90], wound healing[91], diuretic[92] and antipyretic [93] properties.Devi et al. [94]evaluated antibacterial, anti-fungal and antitumor properties of W. somnifera while its root has been used since long time for both sexes and even during pregnancy[95]. Another medicinal plant, C. rotundus has been studied against skin disease [96]. Recently, anticancer activity of S. nigrum has been reported by Lai et al. [97]. These findings confirm high RFC and UV of these plant species in the study area.
Relative popularity level (RPL)
Our 201 informants cited 85 plant species for 11 different disease categories. Of them, 32 species as given in Table 3, received more consideration by informants; therefore included for further discussion. The correlation between number of informants citing a particular plant species and the number of application used is given in S5 Fig, whereas S6 Fig indicates relationship among the numbers of informants claimed use of certain plant species for a particular disease. For species cited by 6 to 25 informants, number of uses per plant increases linearly with the increase in number of informants i.e. correlation coefficient r = 0.10 (S5 Fig). The average number of uses for plant species cited by 26 or more informants does not increase with the increased number of informants. 26 plant species, which were cited by few to 25 informants were declared unpopular, whereas the 6 plant species mentioned by 26 informants or more were classified as popular. The separating line between the popular and unpopular groups falls at the point where average number of uses per plant ceases to increase with further increase in the number of informants. Solanum surattense (Solanaceae), Triticum aestivum (Poaceae), Solanum nigrum (Solanaceae), Withania somnifera (Solanaceae), Ranunculus sceleratus (Ranunculaceae) and Calotropis procera (Asclepiadaceae) were the popular plant species with 1.0 RPL value. The high popularity of these plant species might be attributed to their high efficacy and the awareness of indigenous peoples which specifies their use as herbal medicine. This is the first baseline study on the indigenous knowledge of local peoples regarding the use of popular plant species for a particular ailment. These findings were in consistent with previous studies on the status of medicinal plants among Bedouins of Negev district [43] and medicinal plant survey in Palestinian area [44]. In these studies Alhagimaurorum (urinary disorder) and Tamarixaphylla (eye problem) were reported as unpopular plant species due to low RPL.
Table 3. Highly utilized species of the study are along with FL, RPL and ROP.
| S. No | Species name | N | NA | Major ailment | Np | FL | RPL | ROP |
|---|---|---|---|---|---|---|---|---|
| 1. | Solanum surattense | 52 | 8 | Kidney stones | 44 | 84.6 | 1.00 | 85 |
| 2. | Triticum aestivum | 42 | 6 | Late puberty | 33 | 78.6 | 1.00 | 79 |
| 3. | Solanum nigrum | 39 | 12 | Cardiac pain | 30 | 76.9 | 1.00 | 77 |
| 4. | Withania somnifera | 34 | 8 | Stomachache | 34 | 100 | 1.00 | 100 |
| 5. | Ranunculus sceleratus | 28 | 6 | Urinary incontinence | 28 | 100 | 1.00 | 100 |
| 6. | Calotropis procera | 26 | 8 | Wound healing | 20 | 76.9 | 1.00 | 77 |
| 7. | Cyperus rotundus | 25 | 6 | Hypersplenism | 11 | 44.0 | 0.96 | 42 |
| 8. | Achyranthes aspera | 23 | 8 | Dysmenorrhea | 10 | 43.5 | 0.88 | 38 |
| 9. | Chenopodium album | 23 | 7 | Stomachache | 7 | 30.4 | 0.88 | 27 |
| 10. | Ficus religiosa | 22 | 6 | Skin ulcer | 6 | 27.3 | 0.85 | 23 |
| 11. | Malva parviflora | 22 | 8 | Cough and bronchitis | 7 | 31.8 | 0.85 | 27 |
| 12. | Sonchus asper | 22 | 5 | Constipation | 6 | 27.3 | 0.85 | 23 |
| 13. | Acacia nilotica | 21 | 8 | Hyperglycemia | 8 | 38.1 | 0.81 | 31 |
| 14. | Anethum graveolens | 21 | 4 | Indigestion | 3 | 14.3 | 0.81 | 12 |
| 15. | Boerhavia diffusa | 21 | 5 | Asthma | 6 | 28.6 | 0.81 | 23 |
| 16. | Eucalyptus camaldulensis | 21 | 7 | Sore throat | 6 | 28.6 | 0.81 | 23 |
| 17. | Launaea procumbens | 20 | 4 | Ringworm | 4 | 20.0 | 0.77 | 15 |
| 18. | Veronica polita | 20 | 4 | Nerve tonic | 4 | 20.0 | 0.77 | 15 |
| 19. | Brassica rapa | 19 | 2 | Skin edema | 3 | 15.8 | 0.73 | 12 |
| 20. | Oxalis corniculata | 19 | 8 | Jaundice | 7 | 36.8 | 0.73 | 27 |
| 21. | Ziziphus nummularia | 19 | 6 | Constipation | 5 | 26.3 | 0.73 | 19 |
| 22. | Anagallis arvensis | 18 | 4 | Skin ulcer | 4 | 22.2 | 0.69 | 15 |
| 23. | Euphorbia dracunculoides | 18 | 5 | Headache | 5 | 27.8 | 0.69 | 19 |
| 24. | Trifolium resupinatum | 18 | 6 | Skin sores | 7 | 38.9 | 0.69 | 27 |
| 25. | Cannabis sativa | 17 | 9 | Nervetonic | 9 | 52.9 | 0.65 | 35 |
| 26. | Tamarix aphylla | 17 | 6 | Eye inflammation | 4 | 23.5 | 0.65 | 15 |
| 27. | Alhagi maurorum | 15 | 8 | Kidney stone | 8 | 53.3 | 0.58 | 31 |
| 28. | Melia azedarach | 14 | 7 | Malarial fever | 11 | 78.6 | 0.54 | 42 |
| 29. | Cirsium arvense | 12 | 5 | Peptic ulcer | 4 | 33.3 | 0.46 | 15 |
| 30. | Rumex dentatus | 11 | 4 | Ecezma | 7 | 63.6 | 0.42 | 27 |
| 31. | Kochia indica | 8 | 3 | Heart tonic | 3 | 37.5 | 0.31 | 12 |
| 32. | Malvaviscus arboreus | 6 | 3 | Diarrhea | 4 | 66.7 | 0.23 | 15 |
N. number of total informants, NA. Number of ailments, Np. No. of informants who reported use of species, FL. Fidelity level, RPL. Relative popularity level, ROP. Rank order priority
Fidelity level (FL)
The fidelity level (FL) of the 32 most important plant species ranged from 14.3 to 100% (Table 3). In general, the high FL of a species indicates the prevalence of a specific disease in an area and the utilization of plant species by the inhabitants to treat it [23,98]. Withania somnifera and Ranunculus sceleratus depicted 100% FL against stomach and urinary disorders, respectively. The fidelity levels calculated for Solanum surattense, Triticum aestivum, Melia azedarach, Solanum nigrum and Calotropis procera to treat kidney stones, late puberty, malarial fever, cardio-vascular diseases, and wound healing were 84.6, 78.6, 78.6, 76.9, 76.9%, respectively. The plant species with100% FL for instance W. somnifera have also been reported as chemo-preventive against stomach and skin carcinogenesis [99]. In another study, the R. sceleratus was reported as antiurolithiatic agent to treat urinary disorder [100].
Rank order priority (ROP)
The Rank order priority (ROP) index is used to rank appropriately the plant species with different FL values. The resultant RPL values given in S5 Fig were used as correction factor to adjust the FL values. The ROP values are thus obtained are given in Table 3. Of the 32 species, only eight species attained ROP above 50.This is probably due to decreasing popularity of herbal medicines among the local communities of the study area. Based on ROP value Withania somnifera and Ranunculus sceleratus were widely utilized species with ROP = 100 for each. The other plant species with significant ROP were: Solanum surattense, Triticum aestivum, Solanum nigrum, and Calotropis procera (86, 79, 77 and 77, respectively). The ROP values reported for medicinal plants used by Bedouins community in Negev district [43] and in Palestinian area [44] were comparable to present findings. However, Alhagim aurorum (ROP = 31) and Tamarix aphylla (ROP = 15), were used to relieve urinary system disorder and eye disease, respectively by the inhabitants of the study area.
Novelty and future impact
Present study is the first document on ethnobotanical uses of 85 medicinal plant species used by the inhabitants of Hafizabad district, Punjab-Pakistan. The current ethnomedicinal uses of reported plant species were compared previous studies conducted in Pakistan and other areas [21,26,66,80,101–105] as shown in Table 1, to find the novelty index. Approximately,15% medicinal uses of reported species were similar, whereas 6% were dissimilar to previous reports. However, 79% medicinal uses were new in the present study. Moreover, medicinal uses of plant species reported in neighboring areas i.e. from Layyah district, Punjab province, Pakistan [21] showed more resemblance compared to those documented in other areas. The data collected from the study area reveal considerable difference in plant parts used, mode of herbal preparation and its utilization as reported from other regions.
Some of the newly documented medicinal uses and relevant plant species include: Anethum graveolens (indigestion), Chrozophora tinctoria (stomachache), Cirsium arvense (to heal wounds), Euphorbia prostrate (diarrhea and dysentery), Ficus benjamina (stomach disorder), Jasminum officinale (fever), Kochia indica (toothache), Malvastrum tricuspidatum (sores & wounds), Morus nigra (asthma), Parthenium hysterophorus (constipation), Prosopis juliflora (kidney stones), Pterospermum acerifolium (bleeding piles), Ranunculussceleratus (asthma), Setaria glauca (skin disease), Sorghum halepense (indigestion), Trifolium resupinatum(sore throat) and Veronica polita (indigestion). The plant species with new medicinal uses and high RPL value could be studied further to screen bioactive compounds and their pharmacological activities to introduce novel drugs.
Conclusion
Present survey revealed that a number of medicinal plant species are used by indigenous people of the study area to treat various ailments. The indigenous community still relies on traditional medicine although; the modern health-care services are available, which indicates the significance of plant based traditional recipes. Our findings provide baseline data to establish a connection between the traditional health practioners and scientific communities, which could be substantial in novel drug discovery. Furthermore, ethnobotanical data is of significant value for conservation managers and policy makers for sustainable management of medicinal plant species, which are under threat due to over exploitation. The high RPL value of medicinal plant species is an indication of their preference by local inhabitants to treat particular ailments. Therefore such popular plant species could be further analyzed for bioactive constituents, in vivo/in vitro biological activities, which may leads to new and potential drugs.
Supporting information
(TIF)
(TIF)
(TIF)
(TIF)
Numbers represent the plant names as appear in Table 3.
(TIF)
Numbers represent the plant names as they appear in Table 3.
(TIF)
Acknowledgments
The authors gratefully acknowledge local people of district Hafizabad for sharing their traditional knowledge.
Data Availability
All relevant data are within the paper.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Njoroge G, Bussmann R, Gemmill B, Newton L, Ngumi V. Utilization of weed species as source of traditional medicines in central Kenya. Lyonia. 2004; 7: 71–87. [Google Scholar]
- 2.Mahmood A, Mahmood A, Malik RN, Shinwari ZK. Indigenous knowledge of medicinal plants from Gujranwala district, Pakistan. Journal of Ethnopharmacology. 2013; 148: 714–723. doi: 10.1016/j.jep.2013.05.035 [DOI] [PubMed] [Google Scholar]
- 3.Cox PA.Will tribal knowledge survive the millennium? Science. 2000; 287: 44–45. [DOI] [PubMed] [Google Scholar]
- 4.Gilani AH, Atta-ur-Rahman. Trends in ethnopharmacology. Journal of Ethnopharmacology. 2005; 100: 43–49. [DOI] [PubMed] [Google Scholar]
- 5.WHO.Traditional Medicinen and Alternative Medicines. Geneva. 2002; Fact Sheet. No. 271.
- 6.Verpoorte R, Kim HK, Choi YH. Plant as source of medicines In: Bogers RJ, Craker L.E., Lange D., editor. Medicinal and Aromatic Plants. Netherlands: Springer; 2006; pp.261–273. [Google Scholar]
- 7.Colvard MD, Cordell GA, Villalobos R, Sancho G, Soejarto DD, Pestle W, et al. Survey of medical ethnobotanicals for dental and oral medicine conditions and pathologies. Journal of Ethnopharmacology. 2006; 107: 134–142. doi: 10.1016/j.jep.2006.04.005 [DOI] [PubMed] [Google Scholar]
- 8.Cordell GA, Colvard MD. Natural products and traditional medicine: turning on a paradigm. Journal of Natural Products. 2012; 75: 514–525. doi: 10.1021/np200803m [DOI] [PubMed] [Google Scholar]
- 9.Hayta S, Polat R, Selvi S. Traditional uses of medicinal plants in Elazığ (Turkey). Journal of Ethnopharmacology. 2014; 155: 171–184. [DOI] [PubMed] [Google Scholar]
- 10.Farnsworth NR. Screening plants for new medicines In: Wilson E.O., Ed., Chapter 9 in Biodiversity, National Academy Press, Washington DC: 1988. [Google Scholar]
- 11.Purohit S, Vyas S. Medicinal Plant Cultivation: A Scientific Approach: Including Processing and Financial Guidelines. Agrobios (India). 2004.
- 12.Parmesan C. Ecological and evolutionary responses to recent climate change. Annual Review of Ecology, Evolution, and Systematics. 2006; 637–669. [Google Scholar]
- 13.Govaerts R. How many species of seed plants are there? Taxon. 2001; 1085–1090. [Google Scholar]
- 14.Ibrar M, Hussain F, Sultan A.Ethnobotanical studies on plant resources of Ranyal hills, District Shangla, Pakistan. Pakistan Journal of Botany. 2007; 39: 329. [Google Scholar]
- 15.Ahmad SS, Husain SZ. Ethno medicinal survey of plants from salt range (Kallar Kahar) of Pakistan. Pakistan Journal of Botany. 2008; 40: 1005–1011. [Google Scholar]
- 16.Qureshi RA, Ghufran MA, Gilani SA, Yousaf Z, Abbas G, Batool A. Indigenous medicinal plants used by local women in southern Himalayan regions of Pakistan. Pakistan Journal of Botany. 2009; 41: 19–25. [Google Scholar]
- 17.Mahmood A, Mahmood A, Shaheen H, Qureshi RA, Sangi Y, Gilani SA. Ethno medicinal survey of plants from district Bhimber Azad Jammu and Kashmir, Pakistan. Journal of Medicinal Plants Research. 2011; 5: 2348–2360. [Google Scholar]
- 18.Abbasi AM, Khan MA, Shah MH, Shah MM, Pervez A, Ahmad M. Ethnobotanical appraisal and cultural values of medicinally important wild edible vegetables of Lesser Himalayas-Pakistan. Journal of Ethnobiology and Ethnomedicine. 2013; 9: 66 doi: 10.1186/1746-4269-9-66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Akhtar N, Rashid A, Murad W, Bergmeier E. Diversity and use of ethno-medicinal plants in the region of Swat, North Pakistan. Journal of Ethnobiology and Ethnomedicine. 2013; 9: 25 doi: 10.1186/1746-4269-9-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Murad W, Azizullah A, Adnan M, Tariq A, Khan KU, Waheed S, et al. Ethnobotanical assessment of plant resources of Banda Daud Shah, District Karak, Pakistan. Journal of Ethnobiology and Ethnomedicine. 2013; 9: 77 doi: 10.1186/1746-4269-9-77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ahmed N, Mahmood A, Mahmood A, Tahir S, Bano A, Malik RN, et al. Relative importance of indigenous medicinal plants from Layyah district, Punjab Province, Pakistan. Journal of Ethnopharmacology. 2014; 155: 509–523. doi: 10.1016/j.jep.2014.05.052 [DOI] [PubMed] [Google Scholar]
- 22.Arshad M, Ahmad M, Ahmed E, Saboor A, Abbas A, Sadiq S.An ethnobiological study in Kala Chitta hills of Pothwar region, Pakistan: multinomial logit specification. Journal of Ethnobiology and Ethnomedicine. 2014; 10: 13 doi: 10.1186/1746-4269-10-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bibi T, Ahmad M, Tareen RB, Tareen NM, Jabeen R, Rehman S, et al. Ethnobotany of medicinal plants in district Mastung of Balochistan province-Pakistan. Journal of Ethnopharmacology. 2014; 157: 79–89. doi: 10.1016/j.jep.2014.08.042 [DOI] [PubMed] [Google Scholar]
- 24.Mujtaba SG, Abbasi AM, Khan N, Guo X, Ajab Khan M, Hussain M, et al. Traditional uses of medicinal plants against malarial disease by the tribal communities of Lesser Himalayas-Pakistan. Journal of Ethnopharmacology. 2014; 155: 450–462. doi: 10.1016/j.jep.2014.05.047 [DOI] [PubMed] [Google Scholar]
- 25.Saqib Z, Mahmood A, Naseem Malik R, Mahmood A, Hussian Syed J, Ahmad T. Indigenous knowledge of medicinal plants in Kotli Sattian, Rawalpindi district, Pakistan. Journal of Ethnopharmacology. 2014; 151: 820–828. doi: 10.1016/j.jep.2013.11.034 [DOI] [PubMed] [Google Scholar]
- 26.Ullah S, Khan MR, Shah NA, Shah SA, Majid M, Farooq MA. Ethnomedicinal plant use value in the Lakki Marwat District of Pakistan. Journal of Ethnopharmacology, 2014; 158: 412–422. doi: 10.1016/j.jep.2014.09.048 [DOI] [PubMed] [Google Scholar]
- 27.Altaf M, Javid A, Irfan, Munir MA, Ashraf S, Umair M, et al. Diversity of wild mammalian fauna of Chenab riverine forest, Punjab, Pakistan. The Journal of Animal & Plant Sciences. 2014; 24: 1342–1347. [Google Scholar]
- 28.Altaf M, Javid A, Irfan, Munir MA, Ashraf S, Iqbal KJ, et al. Diversity, distribution and ecology of birds in summer season flathead Khanki, Punjab, Pakistan. Biologia (Pakistan). 2013;59: 131–137. [Google Scholar]
- 29.Stevens PF (2001 onwards) Angiosperm Phylogeny Website Version 12, July 2012. [
- 30.Raunkiær C. Plant life forms Oxford: Oxford University Press; 1937. [Google Scholar]
- 31.Raunkiaer C. The life forms of plants and statistical plant geography Oxford: Clarendon Press; 1934. [Google Scholar]
- 32.Brown CH. Folk Botanical Life‐Forms: Their Universality and Growth. American Anthropologist. 1977; 79: 317–342. [Google Scholar]
- 33.Stewart RR. Flora of West Pakistan. Karachi: Fakhri Printing Press; 1972. [Google Scholar]
- 34.Ahmad S. Flora of Punjab. Monograph 9–10. Lahore: Biological Society of Pakistan; 1980. [Google Scholar]
- 35.Heinrich M, Ankli A, Frei B, Weimann C, Sticher O. Medicinal plants in Mexico: Healers' consensus and cultural importance. Social Science and Medicine. 1998; 47: 1859–1871. [DOI] [PubMed] [Google Scholar]
- 36.Heinrich M, Edwards S, Moerman DE, Leonti M. Ethnopharmacological field studies: A critical assessment of their conceptual basis and methods. Journal of Ethnopharmacology, 2009; 124: 1–17. [DOI] [PubMed] [Google Scholar]
- 37.Trotter RT, Logan MH. Informant consensus: a new approach for identifying potentially effective medicinal plants In: Etkin NLE, editor. Plants in Indigenous Medicine and Diet, Biobehavioural Approaches. Bedford Hills, NY: Redgrave Publishers; 1986. [Google Scholar]
- 38.Phillips O, Gentry AH. The useful plants of Tambopata, Peru: I. Statistical hypotheses tests with a new quantitative technique. Economic Botany. 1993; 47: 15–32. [Google Scholar]
- 39.Ilker U, Suleyman B, Nurettin Y, Yunus D. The investigation and quantitative ethnobotanical evaluation of medicinal plants used around Izmir province, Turkey. Journal of Medicinal Plants Research. 2009; 3: 345–367. [Google Scholar]
- 40.Vitalini S, Iriti M, Puricelli C, Ciuchi D, Segale A, Fico G. Traditional knowledge on medicinal and food plants used in Val San Giacomo (Sondrio, Italy)-An alpine ethnobotanical study. Journal of Ethnopharmacology, 2013; 145: 517–529. doi: 10.1016/j.jep.2012.11.024 [DOI] [PubMed] [Google Scholar]
- 41.Tardío J, Pardo-de-Santayana M. Cultural importance indices: a comparative analysis based on the useful wild plants of Southern Cantabria (Northern Spain) 1. Economic Botany. 2008; 62: 24–39. [Google Scholar]
- 42.Alexiades MN, Sheldon JW. Selected guidelines for ethnobotanical research: A Field Manual. Boranx, NY: The New York Botanical Garden; 1996. [Google Scholar]
- 43.Friedman J, Yaniv Z, Dafni A, Palewitch D. A preliminary classification of the healing potential of medicinal plants, based on a rational analysis of an ethnopharmacological field survey among Bedouins in the Negev Desert, Israel. Journal of Ethnopharmacology. 1986; 16: 275–287. [DOI] [PubMed] [Google Scholar]
- 44.Ali-Shtayeh MS, Yaniv Z, Mahajna J. Ethnobotanical survey in the Palestinian area: a classification of the healing potential of medicinal plants. Journal of Ethnopharmacology. 2000; 73: 221–232. [DOI] [PubMed] [Google Scholar]
- 45.Kadir MF, Bin Sayeed MS, Mia M. Ethnopharmacological survey of medicinal plants used by indigenous and tribal people in Rangamati, Bangladesh. Journal of Ethnopharmacology. 2012; 144: 627–637. doi: 10.1016/j.jep.2012.10.003 [DOI] [PubMed] [Google Scholar]
- 46.Cakilcioglu U, Khatun S, Turkoglu I, Hayta S. Ethnopharmacological survey of medicinal plants in Maden (Elazig-Turkey). Journal of Ethnopharmacology. 2011; 137: 469–486. doi: 10.1016/j.jep.2011.05.046 [DOI] [PubMed] [Google Scholar]
- 47.Ahmed N, Mahmood A, Tahir S, Bano A, Malik RN, Hassan S, et al. Ethnomedicinal knowledge and relative importance of indigenous medicinal plants of Cholistan desert, Punjab Province, Pakistan. Journal of Ethnopharmacology. 2014; 155: 1263–1275. doi: 10.1016/j.jep.2014.07.007 [DOI] [PubMed] [Google Scholar]
- 48.Abbasi AM, Khan SM, Ahmad M, Khan MA, Quave CL, Pieroni A. Botanical ethnoveterinary therapies in three districts of the Lesser Himalayas of Pakistan. Journal of Ethnobiology and Ethnomedicine. 2013; 9: 84 doi: 10.1186/1746-4269-9-84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kadir MF, Bin Sayeed MS, Islam Setu N, Mostafa A, Mia M. Ethnopharmacological survey of medicinal plants used by traditional health practitioners in Thanchi, Bandarban Hill Tracts, Bangladesh. Journal of Ethnopharmacology. 2014; 155: 495–508. doi: 10.1016/j.jep.2014.05.043 [DOI] [PubMed] [Google Scholar]
- 50.Jeffrey C. In: Kadereit JW, Jeffrey C, editors. Compositae: Introduction with key to tribes Families and Genera of Vascular Plants, vol VIII, Flowering Plants, Eudicots, Asterales. Berlin: Springer-Verlag; (2007). [Google Scholar]
- 51.Stepp JR, Moerman DE. The importance of weeds in ethnopharmacology. Journal of Ethnopharmacology. 2001; 75: 19–23. [DOI] [PubMed] [Google Scholar]
- 52.Bolson M, Hefler SR, Chaves EIDO, Junior AG, Junior ELC. Ethno-medicinal study of plants used for treatment of human ailments, with residents of the surrounding region of forest fragments of Paraná, Brazil. Journal of Ethnopharmacology. 2014; 161: 1–10. doi: 10.1016/j.jep.2014.11.045 [DOI] [PubMed] [Google Scholar]
- 53.Ayyanar M, Ignacimuthu S. Ethnobotanical survey of medicinal plants commonly used by Kani tribals in Tirunelveli hills of Western Ghats, India. Journal of Ethnopharmacology. 2011; 134: 851–864. doi: 10.1016/j.jep.2011.01.029 [DOI] [PubMed] [Google Scholar]
- 54.Ju Y, Zhuo J, Liu B, Long C. Eating from the wild: diversity of wild edible plants used by Tibetans in Shangri-la region, Yunnan, China. Journal of Ethnobiology and Ethnomedicine. 2013; 9: 28 doi: 10.1186/1746-4269-9-28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mugisha MK, Asiimwe S, Namutebi A, Borg-Karlson A-K, Kakudidi EK. Ethnobotanical study of indigenous knowledge on medicinal and nutritious plants used to manage opportunistic infections associated with HIV/AIDS in western Uganda. Journal of Ethnopharmacology. 2014; 155: 194–202. doi: 10.1016/j.jep.2014.05.012 [DOI] [PubMed] [Google Scholar]
- 56.Tabuti J, Lye K, Dhillion S. Traditional herbal drugs of Bulamogi, Uganda: plants, use and administration. Journal of Ethnopharmacology. 2003; 88: 19–44. [DOI] [PubMed] [Google Scholar]
- 57.Singh AG, Kumar A, Tewari DD. An ethnobotanical survey of medicinal plants used in Terai forest of western Nepal. Journal of Ethnobiology and Ethnomedicine. 2012; 8: 19 doi: 10.1186/1746-4269-8-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Giday M, Asfaw Z, Woldu Z. Ethnomedicinal study of plants used by Sheko ethnic group of Ethiopia. Journal of Ethnopharmacology. 2010; 132: 75–85. doi: 10.1016/j.jep.2010.07.046 [DOI] [PubMed] [Google Scholar]
- 59.Ragupathy S, Steven NG, Maruthakkutti M, Velusamy B, Ul-Huda MM. Consensus of the'Malasars' traditional aboriginal knowledge of medicinal plants in the Velliangiri holy hills, India. Journal of Ethnobiology and Ethnomedicine. 2008; 4: 8 doi: 10.1186/1746-4269-4-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Uniyal SK, Singh K, Jamwal P, Lal B. Traditional use of medicinal plants among the tribal communities of Chhota Bhangal, Western Himalaya. Journal of Ethnobiology and Ethnomedicine. 2006; 2: 14 doi: 10.1186/1746-4269-2-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ahmed E, Arshad M, Saboor A, Qureshi R, Mustafa G, Sadiq S, et al. Ethnobotanical appraisal and medicinal use of plants in Patriata, New Murree, evidence from Pakistan. Journal of Ethnobiology and Ethnomedicine. 2013; 9: 13 doi: 10.1186/1746-4269-9-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Moerman DE. An analysis of the food plants and drug plants of native North America. Journal of Ethnopharmacology. 1996; 52: 1–22. [DOI] [PubMed] [Google Scholar]
- 63.Shinwari MI, Khan MA. Folk use of medicinal herbs of Margalla hills national park, Islamabad. Journal of Ethnopharmacology. 2000; 69: 45–56. [DOI] [PubMed] [Google Scholar]
- 64.Bradacs G, Heilmann J, Weckerle CS. Medicinal plant use in Vanuatu: A comparative ethnobotanical study of three islands. Journal of Ethnopharmacology. 2011; 137: 434–448. doi: 10.1016/j.jep.2011.05.050 [DOI] [PubMed] [Google Scholar]
- 65.Leto C, Tuttolomondo T, La Bella S, Licata M. Ethnobotanical study in the Madonie Regional Park (Central Sicily, Italy)—Medicinal use of wild shrub and herbaceous plant species. Journal of Ethnopharmacology. 2013; 146: 90–112. doi: 10.1016/j.jep.2012.11.042 [DOI] [PubMed] [Google Scholar]
- 66.Zheng X-l Xing F-w. Ethnobotanical study on medicinal plants around Mt. Yinggeling, Hainan Island, China. Journal of Ethnopharmacology. 2009; 124: 197–210. doi: 10.1016/j.jep.2009.04.042 [DOI] [PubMed] [Google Scholar]
- 67.Bernhoft A. Bioactive compounds in plants—Benefits and risks for man and animals. The Norwegian Academy of Science and Letters, Oslo 2010. [Google Scholar]
- 68.Ahmad M, Sultana S, Fazl-i-Hadi S, ben Hadda T, Rashid S, Zafar M, et al. An Ethnobotanical study of Medicinal Plants in high mountainous region of Chail valley (District Swat-Pakistan). Journal of Ethnobiology and Ethnomedicine. 2014; 10: 36 doi: 10.1186/1746-4269-10-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kayani S, Ahmad M, Zafar M, Sultana S, Khan MPZ, Ashraf MA, et al. Ethnobotanical uses of medicinal plants for respiratory disorders among the inhabitants of Gallies–Abbottabad, Northern Pakistan. Journal of Ethnopharmacology. 2014; 156: 47–60. doi: 10.1016/j.jep.2014.08.005 [DOI] [PubMed] [Google Scholar]
- 70.Šarić-Kundalić B, Dobeš C, Klatte-Asselmeyer V, Saukel J. Ethnobotanical study on medicinal use of wild and cultivated plants in middle, south and west Bosnia and Herzegovina. Journal of Ethnopharmacology. 2010; 131: 33–55. doi: 10.1016/j.jep.2010.05.061 [DOI] [PubMed] [Google Scholar]
- 71.Belayneh A, Bussa NF. Ethnomedicinal plants used to treat human ailments in the prehistoric place of Harla and Dengego valleys, eastern Ethiopia. Journal of Ethnobiology and Ethnomedicine. 2014; 10: 18 doi: 10.1186/1746-4269-10-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Song M-J, Kim H, Heldenbrand B, Jeon J, Lee S. Ethnopharmacological survey of medicinal plants in Jeju Island, Korea. Journal of Ethnobiology and Ethnomedicine. 2013; 9: 48 doi: 10.1186/1746-4269-9-48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Manandhar NP. An inventory of some herbal drugs of Myagdi District, Nepal. Economic Botany. 1995; 49: 371–379. [Google Scholar]
- 74.Inta A, Trisonthi P, Trisonthi C. Analysis of traditional knowledge in medicinal plants used by Yuan in Thailand. Journal of Ethnopharmacology. 2013; 149: 344–351. doi: 10.1016/j.jep.2013.06.047 [DOI] [PubMed] [Google Scholar]
- 75.Boudjelal A, Henchiri C, Sari M, Sarri D, Hendel N, Benkhaled A. et al. Herbalists and wild medicinal plants in M'Sila (North Algeria): An ethnopharmacology survey. Journal of Ethnopharmacology. 2013; 148: 395–402. doi: 10.1016/j.jep.2013.03.082 [DOI] [PubMed] [Google Scholar]
- 76.Ssegawa P, Kasenene JM. Medicinal plant diversity and uses in the Sango bay area, Southern Uganda. Journal of Ethnopharmacology. 2007; 113: 521–540. doi: 10.1016/j.jep.2007.07.014 [DOI] [PubMed] [Google Scholar]
- 77.Rokaya MB, Münzbergová Z, Timsina B. Ethnobotanical study of medicinal plants from the Humla district of western Nepal. Journal of Ethnopharmacology. 2010; 130: 485–504. doi: 10.1016/j.jep.2010.05.036 [DOI] [PubMed] [Google Scholar]
- 78.Cechinel-Filho V. Plant bioactives and drug discovery: principles, practice, and perspectives: John Wiley & Sons; 2012. [Google Scholar]
- 79.Ignacimuthu S, Ayyanar M. Ethnobotanical investigations among tribes in Madurai district of Tamil Nadu (India). Journal of Ethnobiology and Ethnomedicine. 2006; 2: 25 doi: 10.1186/1746-4269-2-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Luitel DR, Rokaya MB, Timsina B, Münzbergová Z. Medicinal plants used by the Tamang community in the Makawanpur district of central Nepal. Journal of Ethnobiology and Ethnomedicine. 2014; 10: 5 doi: 10.1186/1746-4269-10-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Revathi P, Parimelazhagan T, Manian S. Ethnomedicinal plants and novel formulations used by Hooralis tribe in Sathyamangalam forests, Western Ghats of Tamil Nadu, India. Journal of Medicinal Plants Research. 2013; 7: 2083–2097. [Google Scholar]
- 82.De Wet H, Nciki S, van Vuuren SF. Medicinal plants used for the treatment of various skin disorders by a rural community in northern Maputaland, South Africa. Journal of Ethnobiology and Ethnomedicine. 2013; 9: 51 doi: 10.1186/1746-4269-9-51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Frei B, Baltisberger M, Sticher O, Heinrich M. Medical ethnobotany of the Zapotecs of the Isthmus-Sierra (Oaxaca, Mexico): Documentation and assessment of indigenous uses. Journal of Ethnopharmacology. 1998; 62: 149–165. [DOI] [PubMed] [Google Scholar]
- 84.Singh H, Husain T, Agnihotri P, Pande P, Khatoon S. An ethnobotanical study of medicinal plants used in sacred groves of Kumaon Himalaya, Uttarakhand, India. Journal of Ethnopharmacology. 2014; 154: 98–108. doi: 10.1016/j.jep.2014.03.026 [DOI] [PubMed] [Google Scholar]
- 85.Zheng XL, Wei JH, Sun W, Li RT, Liu SB, Dai HF. Ethnobotanical study on medicinal plants around Limu Mountains of Hainan Island, China. Journal of Ethnopharmacology. 2013; 148: 964–974. doi: 10.1016/j.jep.2013.05.051 [DOI] [PubMed] [Google Scholar]
- 86.Kaval I, Behçet L, Cakilcioglu U. Ethnobotanical study on medicinal plants in Geçitli and its surrounding (Hakkari-Turkey). Journal of Ethnopharmacology. 2014; 155: 171–184. doi: 10.1016/j.jep.2014.05.014 [DOI] [PubMed] [Google Scholar]
- 87.Vendruscolo G, Mentz A. Ethnobotanical survey of the medicinal plants used by the community of Ponta Grossa neighborhood, Porto Alegre, Rio Grande do Sul, Brazil. Iherigia Série Botânica. 2006; 61: 83–103. [Google Scholar]
- 88.Hussain T, Gupta RK, Sweety K, Khan MS, Hussain MS, Arif MD, et al. Evaluation of antihepatotoxic potential of Solanum xanthocarpum fruit extract against antitubercular drugs induced hepatopathy in experimental rodents. Asian Pacific Journal of Tropical Biomedicine. 2012; 2: 454–460. doi: 10.1016/S2221-1691(12)60075-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Govindan S, Viswanathan S, Vijayasekaran V, Alagappan R. A pilot study on the clinical efficacy of Solanum xanthocarpum and Solanum trilobatum in bronchial asthma. Journal of Ethnopharmacology. 1999; 66: 205–210. [DOI] [PubMed] [Google Scholar]
- 90.Pardhi P, Jain AP, Ganeshpurkar A, Rai G. Anti-microbial, anti-oxidant and anthelmintic activity of crude extract of Solanum xanthocarpum. Pharmacognosy Journal. 2010; 2: 400–404. [Google Scholar]
- 91.Kumar N, Prakash D, Kumar P. Wound healing activity of Solanum xanthocarpum Schrad. & Wendl. fruits. Indian Journal of Natural Profuct and Resources. 2010; 1(4): 470–475. [Google Scholar]
- 92.Patel P, Patel M, Saralai M, Gandhi T. Antiurolithiatic effects of Solanum xanthocarpum fruit extract on ethylene-glycol-induced nephrolithiasis in rats. Journal of Young Pharmacists. 2012; 4: 164–170. doi: 10.4103/0975-1483.100022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Singh OM, Singh TP. Phytochemistry of Solanum xanthocarpum: an amazing traditional healer. Journal of Scientific and Industrial Research. 2010; 69(10): 732–740. [Google Scholar]
- 94.Devi PU, Sharada A, Solomon F. Antitumor and radiosensitizing effects of Withania somnifera (Ashwagandha) on a transplantable mouse tumor, Sarcoma-180. Indian Journal of Experimental Biology. 1993; 31: 607–611. [PubMed] [Google Scholar]
- 95.Budhiraja R, Sudhir S. Review of biological activity of withanolides. Journal of Scientific and Industrial Research 1987. http://aims.fao.org/serials/c_a7ccc555. [Google Scholar]
- 96.Jin JH, Lee D-U, Kim YS, Kim HP. Anti-allergic activity of sesquiterpenes from the rhizomes of Cyperus rotundus. Archives of Pharmacal Research. 2011; 34: 223–228. doi: 10.1007/s12272-011-0207-z [DOI] [PubMed] [Google Scholar]
- 97.Lai Y-J, Tai C-J, Wang C-W, Choong C-Y, Lee B-H, Shi YC, et al. Anti-cancer activity of Solanum nigrum (AESN) through suppression of mitochondrial function and epithelial-mesenchymal transition (EMT) in breast cancer cells. Molecules, 2016; 21: 553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Srithi K, Balslev H, Wangpakapattanawong P, Srisanga P, Trisonthi C. Medicinal plant knowledge and its erosion among the Mien (Yao) in northern Thailand. Journal of Ethnopharmacology. 2009; 123: 335–342. doi: 10.1016/j.jep.2009.02.035 [DOI] [PubMed] [Google Scholar]
- 99.Padmavathi B, Rath PC, Rao AR, Singh RP. Roots of Withania somnifera inhibit forestomach and skin carcinogenesis in mice. Evidence-Based Complementary and Alternative Medicine. 2005; 2: 99–105. doi: 10.1093/ecam/neh064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Mikawlrawng K, Kumar S. Current scenario of urolithiasis and the use of medicinal plants as antiurolithiatic agents in Manipur (North East India): a review. International Journal of Herbal Medicine. 2014; 2: 1–12. [Google Scholar]
- 101.Verma AK, Kumar M, Bussmann RW. Medicinal plants in an urban environment: the medicinal flora of Banares Hindu University, Varanasi, Uttar Pradesh. Journal of Ethnobiology and Ethnomedicine. 2007; 3: 35 doi: 10.1186/1746-4269-3-35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Sabitha S, Maher K, Mohamed M. Medicinal plants diversity and their conservation status in the United Arab Emirates (UAE). Journal of Medicinal Plants Research. 2012; 6: 1304–1322. [Google Scholar]
- 103.Mollik MAH, Hossan MS, Paul AK, Taufiq-Ur-Rahman M, Jahan R, Rahmatullah M. A comparative analysis of medicinal plants used by folk medicinal healers in three districts of Bangladesh and inquiry as to mode of selection of medicinal plants. Ethnobotany Research and Applications. 2010; 8: 195–218. [Google Scholar]
- 104.Chaitanya M, Dhanabal S, Rajan S. Pharmacodynamic and ethnomedicinal uses of weed speices in nilgiris, Tamilnadu State, India: A review. African Journal of Agricultural Research. 2013; 8: 3505–3527. [Google Scholar]
- 105.Rahman MA, Mossa JS, Al-Said MS, Al-Yahya MA. Medicinal plant diversity in the flora of Saudi Arabia 1: a report on seven plant families. Fitoterapia. 2004; 75: 149–161. doi: 10.1016/j.fitote.2003.12.012 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(TIF)
(TIF)
(TIF)
(TIF)
Numbers represent the plant names as appear in Table 3.
(TIF)
Numbers represent the plant names as they appear in Table 3.
(TIF)
Data Availability Statement
All relevant data are within the paper.