Abstract
Background
It has been suggested that anti-hypertensive medications may worsen leg ischemia in peripheral artery disease (PAD) patients. We undertook a meta-analysis to assess the effect of anti-hypertensive medications on measures of leg ischemia including maximum walking distance (MWD), pain free walking distance (PFWD) and ankle brachial pressure index (ABPI). A meta-regression was performed to evaluate whether the effect of the anti-hypertensive medications on mean arterial pressure (MAP) was associated with changes in ABPI, MWD or PFWD.
Method
A systematic literature search was performed to identify placebo controlled randomized control trials (RCT) testing anti-hypertensive medications, which reported baseline and follow-up measurements of: MAP and MWD, PFWD or ABPI in patients with intermittent claudication (IC) due to PAD.
Result
A meta-analysis was performed on 5 RCTs comprising a total of 180 and 127 patients receiving anti-hypertensive medications and placebo respectively. This analysis suggested that anti-hypertensive medication did not significantly affect MWD, PFWD or ABPI. In contrast, the meta-regression analysis showed that the reduction in MAP due to the anti-hypertensive drugs was positively correlated with increased MWD during follow-up (β = 8.371, p = 0.035). Heterogeneity across studies, as assessed by I2, was high. The follow-up period within the included trials was generally short with 3 out of 5 studies having a follow-up period of ≤ 6 weeks.
Conclusion
This study suggests that anti-hypertensive treatment does not worsen but may improve leg ischemia in PAD patients. Larger multicenter trials with longer anti-hypertensive treatment periods are required to clarify the effect of anti-hypertensives on leg ischemia in PAD patients.
Introduction
Lower limb peripheral artery disease (PAD) results from narrowing and occlusion of the arteries supplying blood to the legs, usually due to atherosclerosis and associated thrombosis[1, 2]. Approximately 200 million people worldwide were estimated to have PAD in 2010, a rise of 25% since 2000[3]. The most recognised presenting complaint for PAD patients is intermittent claudication (IC). Patients with IC have significantly impaired walking ability, high rates of cardiovascular events, such as myocardial infarction and stroke, and reduced disease-related quality of life[4]. Approximately 20% of patients with PAD will die from a cardiovascular event within 5 years[5] and therefore aggressive management of cardiovascular risk factors is the primary focus of treatment[6].
Hypertension was identified by the global burden of disease study as the leading risk factor for mortality and disability-adjusted life years lost in 2010[7]. Hypertension is considered an important risk factor for PAD and its complications and approximately 50% of patients presenting with PAD are reported to have hypertension[8–12]. Clinical trials including PAD patients (in addition to those with other atherosclerosis-related diseases) have reported a relative reduction in cardiovascular events in those receiving blood pressure lowering medications of 20–30%[13, 14]. Therefore current recommendations advise that PAD patients should receive anti-hypertensive medications if their blood pressure (BP) is >140/90[15–17]. However, the use of some anti-hypertensives, particularly β blockers, has been traditionally contraindicated in PAD patients due to concerns regarding reducing peripheral perfusion[18, 19]. This opinion has been challenged by others who have reported that BP lowering medications do not worsen leg ischemia[20–22]. Some previously published randomised trials in PAD patients have reported improvements in maximum walking distance (MWD), pain free walking distance (PFWD), ankle brachial pressure index (ABPI) and calf blood flow (CBF) after commencing anti-hypertensive medications[23–30]. Other trials have reported no effect of anti-hypertensive medications on PAD patients[31, 32]. A previous Cochrane review concluded that there was lack of evidence on the efficacy of anti-hypertensive medication in patients with PAD, but did not perform a meta-analysis or meta-regression to definitely assess this[33]. In view of the current controversy regarding the effect of BP lowering medication on symptoms of PAD, we undertook a systematic review and meta-analysis to assess if anti-hypertensive medications worsen leg ischemia in PAD patients.
Materials and methods
This meta-analysis was performed in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines[34]. A protocol was developed following the guidelines of the PRISMA-P statement[34] and was published in the PROSPERO database (CRD42016038338).
Search strategy
A systematic search was performed to identify placebo controlled randomised trials (RCTs) evaluating the effects of anti-hypertensive medications on three recognised measures of the severity of leg ischemia including ABPI, MWD and PFWD in patients with IC. The search strategy undertaken and the study selection criteria are detailed in S1 File.
Data extraction
Two authors (DT and BD) extracted data independently using a predefined data extraction table (see S1 File and S1 Table for further details).
Study quality assessment
A quality assessment tool was formulated using components from the following validated tools: a) The 25 items CONSORT 2010 checklist of information to be included when reporting a randomised trial; and b) The Cochrane collaboration tool for assessing risk of bias[35, 36]. The quality assessment details are given in S1 File.
Quantitative data synthesis
The first author (DT) performed statistical analysis of data using the Meta-Analyst software (version beta 3.13)[37]. A description of the data synthesis is provided in S1 File.
Assessment of publication bias
The publication bias was assessed using funnel plots and Eggers’s test using the CMA software package (Comprehensive Meta-Analysis version 3.3.070). The first author (DT) carried out the publication bias assessment.
Results
Characteristics of the included studies
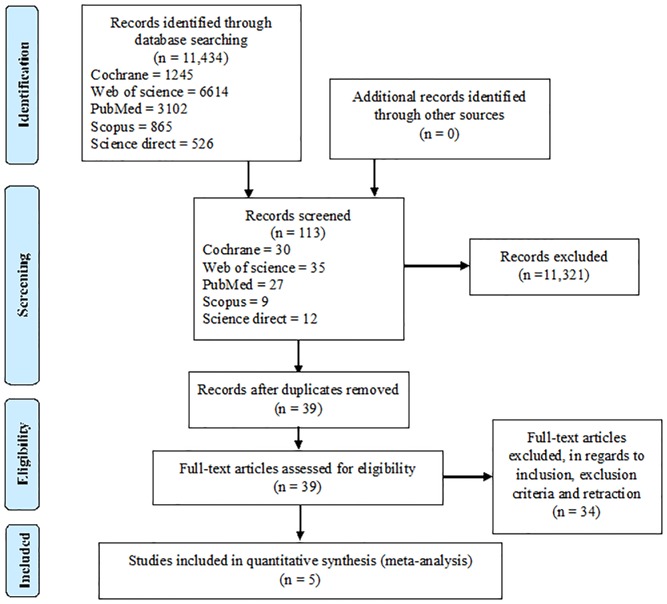
Our search identified 11,434 articles. Detailed characteristics of the included studies are given in S2 File. A PRISMA flow chart outlining the literature search and study selection process is given in Fig 1.
Fig 1. PRISMA flow chart outlining the literature search and the study selection process.
Quality assessment
The quality assessment showed that four studies were of high quality and the remaining one of moderate quality. Agreement on the quality assessment between the observers ranged from 95 to 100% (S2 File). Other details of the quality of the studies are shown in S2 File.
Description of the included studies
The characteristics of the included studies and participants are given in S2 File.
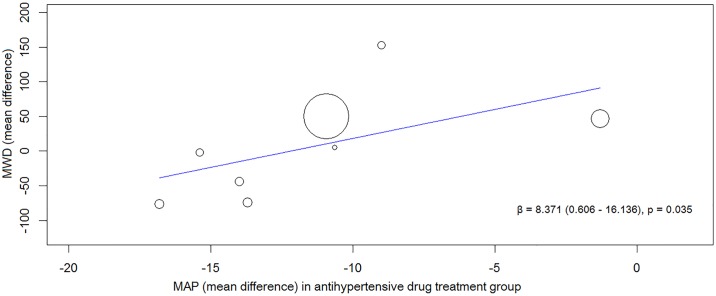
Relationship between changes in MAP and ABPI and walking ability
A meta-regression analysis was carried out to analyse whether the effect of the anti-hypertensives on MAP was associated with the changes in walking distance and ABPI recorded over the course of the trials. The change in MAP and walking distance after treatment with each anti-hypertensive drug was obtained by considering the reported parameters following a ‘washout period’ as baseline for the whole cohort. In total, 8 and 7 groups were used to evaluate the association between reduction in MAP after drug treatment with MWD and PFWD respectively. The magnitude of reduction in MAP from baseline due to the anti-hypertensive drugs showed a significant positive correlation with improved MWD (β = 8.371, p = 0.035) (Fig 2) but not PFWD or ABPI (PFWD, β = 4.276, p = 0.195; ABPI, β = -0.004, p = 0.357).
Fig 2. Results of the meta-regression analysis showing the association between reduction in blood pressure and improvement in MWD after being randomised to an anti-hypertensive drug.
Fig 2 shows the association between reducing MAP and improving MWD in all the included trials. Abbreviations: β–regression coefficient, MAP—mean arterial pressure and MWD—maximum walking distance.
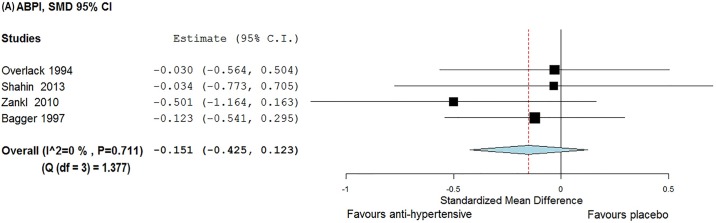
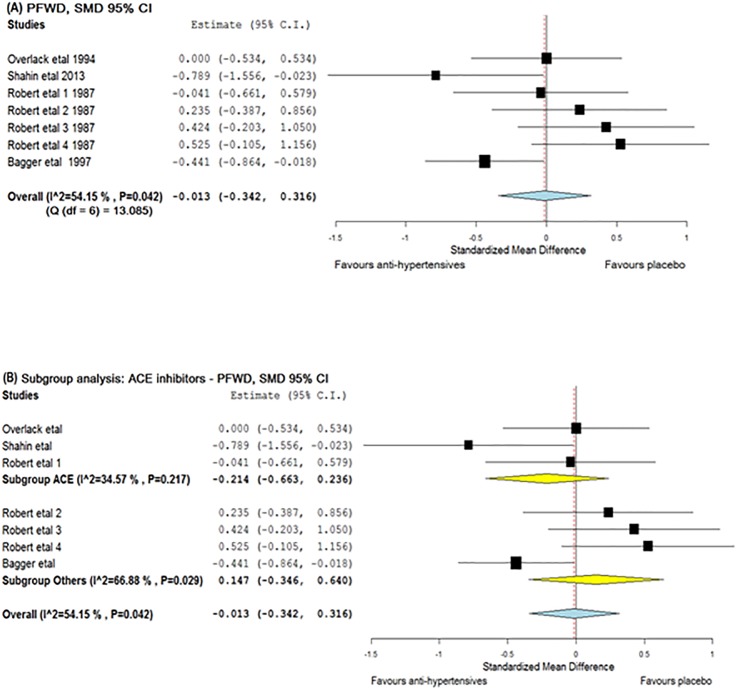
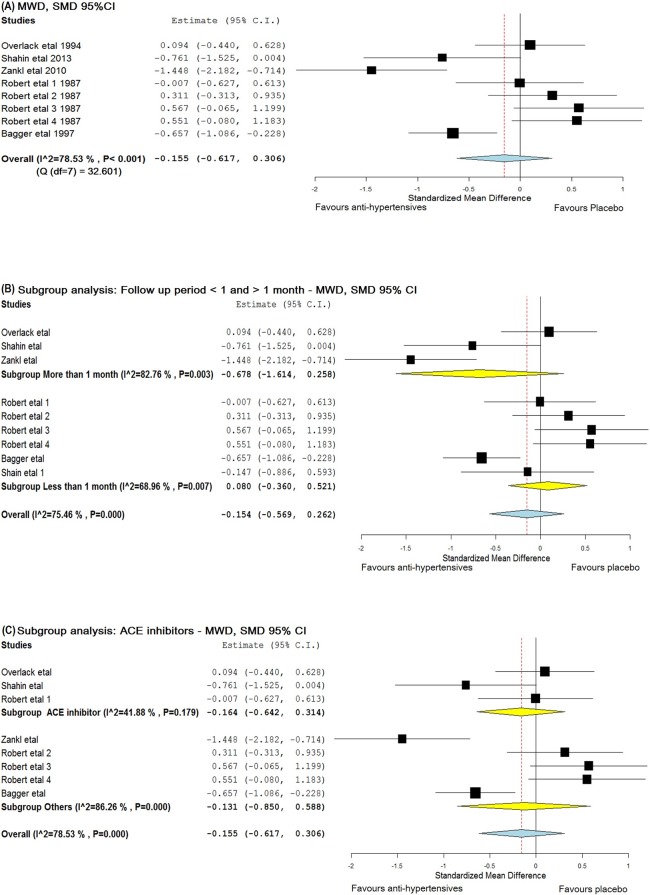
The effect of anti-hypertensives on ABPI, MWD and PFWD
Meta-analyses were conducted to see if reported reductions in BP following antihypertensive therapy led to clinically relevant improvements in ABPI, MWD or PFWD. Studies by Robert et al. and Bagger et al. were given a baseline—post-intervention correlation value of 0.5 for this analysis. Robert et al. assessed 4 anti-hypertensive drugs and placebo in a crossover design. Hence for this meta-analysis, each treatment period was considered as a separate trial. Accordingly, a total of 8 and 7 groups were used to assess the effect of anti-hypertensives on MWD and PFWD respectively (S1 Table). The meta-analysis suggested that anti-hypertensives had no significant effect on ABPI [SMD = -0.151 (95% CI, -0.425–0.123)], MWD [SMD = -0.155 (95% CI, -0.617–0.306)] or PFWD [d = − 0.013 (95% CI, -0.342–0.316)] (Figs 3–5). The findings for MWD were similar in sub-group analyses that assessed treatment periods of > 1 or < 1 month (Fig 4B).
Fig 3. Forest plot illustrating the effect of anti-hypertensive medications on ABPI.
The x-axis is the effect size expressed as SMD (standardised mean difference). The forest plot also details the 95% confidence interval. The dotted line represents the overall effect calculated in this meta-analysis. The heterogeneity estimated as I2 and Q is also provided. Abbreviation: ABPI—ankle brachial pressure index.
Fig 5. Forest plots illustrating the effect of anti-hypertensive medications on PFWD.
The x-axis is the effect size expressed as SMD (standardised mean difference). The forest plot also details the 95% confidence interval. The dotted line represents the overall effect calculated in this meta-analysis. The heterogeneity estimated as I2 and Q associated with each analysis is also provided. (A) The effect of anti-hypertensive medications on PFWD, (B) Subgroup analysis including trials which included ACE inhibitors. Abbreviations: ACE—angiotensin converting enzyme and PFWD—pain free walking distance.
Fig 4. Forest plots illustrating the effect of anti-hypertensive medications on MWD.
The x-axis is the effect size expressed as SMD (standardised mean difference). The forest plot also details the 95% confidence interval. The dotted line represents the overall effect calculated in this meta-analysis. The heterogeneity estimated as I2 and Q associated with each analysis is also provided. (A) The effect of anti-hypertensive medications on MWD, (B) Subgroup analysis including trials with follow up period greater than and less than 1 month, (C) Subgroup analysis including trials which used ACE inhibitors. Abbreviations: ACE—angiotensin converting enzyme and MWD—maximum walking distance.
A sub-analysis was performed to determine whether ACE inhibitors had an effect on leg ischemia[18, 24, 38]. These studies had intervention period of 4, 6 and 24 weeks. No significant effect was found on either MWD (SMD = − 0.164, 95% CI -0.642–0.314) or PFWD (SMD = -0.214, 95% CI -0.663–0.236) (Figs 4C and 5B). Due to a lack of available studies, sub-analyses could not be performed for other drug classes.
Assessment of publication bias
Eggers’s test and the funnel plots (S3 File) suggested no publication bias. The intercepts of the funnel plots assessing publication bias in trials included to analyse the effect of anti-hypertensive medications on ABPI, MWD and PFWD were -0.825 (-8.779–7.129, p = 0.699), 0.388 (-11.038–11.814, p = 0.936) and -1.205 (-14.505–12.095, p = 0.825) respectively.
Discussion
The use and choice of anti-hypertensive medications in PAD patients has been debated for a long time and one of the main concerns have been that anti-hypertensive drugs may worsen leg ischemia. The main finding of this meta-analysis was that anti-hypertensive therapy did not affect leg ischemia as assessed by ABPI, MWD and PFWD. A benefit of anti-hypertensive medications on leg ischemia was suggested by the meta-regression since there was a significant positive correlation between degree of reduction in BP and improvement in MWD.
The RCTs included in this meta-analysis had many limitations. Notably, there was no washout period between treatment periods in the crossover trial by Robert et al.[18]. Hence significant carryover effects may have been present which may have masked the true effect of anti-hypertensive drugs tested. Furthermore, a follow-up period of at least 6 months is recommended in studies of IC to ensure that adequate time is available to demonstrate effects on the leg[39]. The trials by Bagger et al., Robert et al. and Overlack et al. had a follow-up period of two, four and six weeks respectively, which were lower than advocated[18, 23, 38]. Three trials included in this meta-analysis reported improvement in walking distance after anti-hypertensive drug treatment[23–25]. The treatment period for these trials were 52, 24 and 2 weeks, suggesting that longer duration of treatment with anti-hypertensives may be required to demonstrate their efficacy[39]. Only 2 trials achieved a SBP target according to current guidelines of ≤ 140 mmHg [24, 25]. Attaining BP goals may have improved the outcomes. The blinding details of the trial authored by Zankl et al. were unclear[25, 40]. The research was a single blinded study, however the paper did not specify whether the investigators or the patients were blinded. The risk of bias is significant when adequate blinding is not used[40]. RCTs without appropriate blinding have been demonstrated to show a larger treatment effect[41].
The overall lack of effect of anti-hypertensive medications on measures of leg ischemia reported in this meta-analysis can be attributed to many reasons. Firstly, there were few published trials that met the entry criteria and the majority of these trials included small number of patients. Secondly, there are potential methodological issues in combining crossover trials and parallel studies in a meta-analysis. The correlation co-efficient between baseline and follow-up scores in the included crossover trials were also not available hence a conservative estimate value of 0.5 was used[42]. Furthermore, the follow-up period was different in all the trials ranging from 2 to 52 weeks. Different trials also used different anti-hypertensive medications. The current meta-analysis was performed by pooling all trials together regardless of their anti-hypertensive class. In addition, the inclusion and exclusion criteria in the included RCTs were different as a result of which the baseline characteristics of the participants were noticeably different. The crossover trials excluded patients with concomitant coronary heart disease and diabetes mellitus[18, 23], whereas all the parallel trials included patients with these risk factors[24, 25, 38]. Therefore, the degree of heterogeneity between studies both in terms of the design and medications used was relatively high. Moreover, for analysis, data had to be represented as mean ± SD, hence several mathematical manipulations were needed to transform data into this format.
Despite these limitations, the current meta-analysis suggests that anti-hypertensive treatments do not worsen leg ischemia and may possibly improve MWD. This is important to confirm since lowering BP in patients with PAD has significant potential to reduce cardiovascular events. Current guidelines recommend the reduction of BP to ≤ 140/90 in PAD patients[16, 17] but a recent trial conducted by the SPRINT research group showed that a target of SBP ≤ 120 mmHg among patients at high risk of cardiovascular events, including PAD patients, resulted in substantially lower rates of cardiovascular events and associated mortality[43]. It is therefore likely that updated guidelines may advise lowering SBP in high risk patients to ≤ 120 mmHg.
The findings of one of our sub-analyses, that ACE inhibitors did not influence leg outcomes is in apparent contradiction to a previous meta-analysis which reported that ACE inhibitors improved walking ability in patients with IC[44]. It should be noted that the prior meta-analysis included two trials which have been subsequently retracted[45, 46] and positive data from these studies may have contributed to this difference in findings. However the results of this meta-analysis is comparable to an older meta-analysis which concluded that ACE inhibitors did not have any significant effect on walking distance and ABPI[47].
In conclusion, this meta-analysis suggests that reducing BP does not worsen leg ischemia in patients with IC. The role played by anti-hypertensives in improving outcomes is controversial and lacks sufficient evidence and has been clouded by retraction of two trials that reported positive outcomes[45, 46]. Large multicenter trials with prolonged anti-hypertensive treatment periods are required to clarify the effect of anti-hypertensives on symptoms of IC. However, designing such trials is difficult due to the convincing data suggesting that patients at high risk of cardiovascular events, such as PAD patients, should be on anti-hypertensive medications to reduce the incidence of such events[48, 49].
Supporting information
(DOCX)
(DOCX)
(DOCX)
(DOC)
Results are expressed as mean ± SD. The mathematical approach taken for obtaining these data is given in S2 Table. Mean arterial pressure was defined from the following formula: MAP = [(2*DBP) + SBP] / 3. Different anti-hypertensives were used in the trials: Overlack trial—perindopril, Shahin et al.–ramipril, Zankl et al.–telmisartan, Bagger et al.–verapamil, Robert et al.–captopril, atenolol, labetolol and pindolol. Abbreviations: DBP- diastolic blood pressure, MAP—mean arterial pressure, PI—post-intervention and SBP—systolic blood pressure.
(DOCX)
(DOCX)
Acknowledgments
The authors would like to acknowledge the James Cook University library staff for their assistance with literature search and Professor Rhondda Jones for her statistical support.
This work was funded by grants from the National Health and Medical Research Council, the Queensland Government. JG holds a Practitioner Fellowship from the National Health and Medical Research Council, Australia (1117061) and a Senior Clinical Research Fellowship from the Queensland Government. DT is supported by a JCU Post-graduate Research scholarship and a JCU college of Medicine and Dentistry scholarship.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was funded by grants from the National Health and Medical Research Council, the Queensland Government. JG holds a Practitioner Fellowship from the National Health and Medical Research Council, Australia (1117061) and a Senior Clinical Research Fellowship from the Queensland Government. DTM is supported by JCU Post-graduate Research scholarship and JCU college of Medicine and Dentistry scholarship.
References
- 1.Au TB, Golledge J, Walker PJ, Haigh K, Nelson M. Peripheral arterial disease: diagnosis and management in general practice. Aust Fam Physician. 2013;42(6):397 [PubMed] [Google Scholar]
- 2.Krishna SM, Moxon JV, Golledge J. A review of the pathophysiology and potential biomarkers for peripheral artery disease. Int J Mol Sci. 2015;16(5):11294–322. 10.3390/ijms160511294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fowkes FGR, Rudan D, Rudan I, Aboyans V, Denenberg JO, McDermott MM, et al. Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysis. Lancet. 2013;382(9901):1329–40. 10.1016/S0140-6736(13)61249-0 [DOI] [PubMed] [Google Scholar]
- 4.Olin J. W., Sealove B. A. Peripheral artery disease: current insight into the disease and its diagnosis and management. Mayo Clin Proc. 2010;85(7):678–92. 10.4065/mcp.2010.0133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dormandy JA, Rutherford RB. Management of peripheral arterial disease (PAD). TASC Working Group. TransAtlantic Inter-Society Consensus (TASC). J Vasc Surg. 2000;31(1 Pt 2):S1–S296. [PubMed] [Google Scholar]
- 6.Clement DL, Debuyzere ML. How to treat hypertension in patients with peripheral artery disease. Curr Hypertens Rep. 2007;9(3):190–5. [DOI] [PubMed] [Google Scholar]
- 7.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2013;380(9859):2224–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Binaghi F, Fronteddu PF, Cannas F, Caredda E, Uras A, Garau P, et al. Prevalence of peripheral arterial occlusive disease and associated risk factors in a sample of southern Sardinian population. Int Angiol. 1994;13(3):233–45. [PubMed] [Google Scholar]
- 9.Cheng SW, Ting AC, Lau H, Wong J. Epidemiology of atherosclerotic peripheral arterial occlusive disease in Hong Kong. World J Surg. 1999;23(2):202–6. [DOI] [PubMed] [Google Scholar]
- 10.Johnston KW, Rae M, Steiner G, Kalman PG, Schwartz L, Hill ME, et al. An atherosclerosis risk factor assessment program for patients with peripheral arterial occlusive disease. Ann Vasc Surg. 1988;2(2):101–7. 10.1016/S0890-5096(06)60789-9 [DOI] [PubMed] [Google Scholar]
- 11.Novo S, Avellone G, Di Garbo V, Abrignani MG, Liquori M, Panno AV, et al. Prevalence of risk factors in patients with peripheral arterial disease. A clinical and epidemiological evaluation. Int Angiol. 1992;11(3):218–29. [PubMed] [Google Scholar]
- 12.Violi F, Criqui M, Longoni A, Castiglioni C, Group A. Relation between risk factors and cardiovascular complications in patients with peripheral vascular disease. Results from the ADEP study. Atherosclerosis. 1996;120(1):25–35. [DOI] [PubMed] [Google Scholar]
- 13.Yusuf S, Pepine CJ, Garces C, Pouleur H, Salem D, Kostis J, et al. Effect of enalapril on myocardial infarction and unstable angina in patients with low ejection fractions. Lancet. 1992;340(8829):1173–8. [DOI] [PubMed] [Google Scholar]
- 14.Pfeffer MA, Braunwald E, Moye LA, Basta L, Brown EJ Jr., Cuddy TE, et al. Effect of captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction. Results of the survival and ventricular enlargement trial. The SAVE Investigators. N Engl J Med. 1992;327(10):669–77. 10.1056/NEJM199209033271001 [DOI] [PubMed] [Google Scholar]
- 15.James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507–20. 10.1001/jama.2013.284427 [DOI] [PubMed] [Google Scholar]
- 16.Tendera M, Aboyans V, Bartelink ML, Baumgartner I, Clement D, Collet JP, et al. ESC Guidelines on the diagnosis and treatment of peripheral artery diseases: Document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteries: the Task Force on the Diagnosis and Treatment of Peripheral Artery Diseases of the European Society of Cardiology (ESC). Eur Heart J. 2011;32(22):2851–906. 10.1093/eurheartj/ehr211 [DOI] [PubMed] [Google Scholar]
- 17.Rooke TW, Hirsch AT, Misra S, Sidawy AN, Beckman JA, Findeiss L, et al. Management of patients with peripheral artery disease (compilation of 2005 and 2011 ACCF/AHA Guideline Recommendations): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61(14):1555–70. 10.1016/j.jacc.2013.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Roberts DH, Tsao Y, McLoughlin GA, Breckenridge A. Placebo-controlled comparison of captopril, atenolol, labetalol, and pindolol in hypertension complicated by intermittent claudication. Lancet. 1987;2(8560):650–3. [DOI] [PubMed] [Google Scholar]
- 19.Lepantalo M. Chronic effects of metoprolol and methyldopa on calf blood flow in intermittent claudication. Br J Clin Pharmacol. 1984;18(1):90–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bogaert MG, Clement DL. Lack of influence of propranolol and metoprolol on walking distance in patients with chronic intermittent claudication. Eur Heart J. 1983;4(3):203–4. [DOI] [PubMed] [Google Scholar]
- 21.Hiatt WR, Stoll S, Nies AS. Effect of beta-adrenergic blockers on the peripheral circulation in patients with peripheral vascular disease. Circulation. 1985;72(6):1226–31. [DOI] [PubMed] [Google Scholar]
- 22.Radack K, Deck C. Beta-adrenergic blocker therapy does not worsen intermittent claudication in subjects with peripheral arterial disease. A meta-analysis of randomized controlled trials. Arch Intern Med. 1991;151(9):1769–76. [PubMed] [Google Scholar]
- 23.Bagger JP, Helligsoe P, Randsbaek F, Kimose HH, Jensen BS. Effect of verapamil in intermittent claudication A randomized, double-blind, placebo-controlled, cross-over study after individual dose-response assessment. Circulation. 1997;95(2):411–4. [DOI] [PubMed] [Google Scholar]
- 24.Shahin Y, Cockcroft JR, Chetter IC. Randomized clinical trial of angiotensin-converting enzyme inhibitor, ramipril, in patients with intermittent claudication. Br J Surg. 2013;100(9):1154–63. 10.1002/bjs.9198 [DOI] [PubMed] [Google Scholar]
- 25.Zankl AR, Ivandic B, Andrassy M, Volz HC, Krumsdorf U, Blessing E, et al. Telmisartan improves absolute walking distance and endothelial function in patients with peripheral artery disease. Clin Res Cardiol. 2010;99(12):787–94. 10.1007/s00392-010-0184-0 [DOI] [PubMed] [Google Scholar]
- 26.Catalano M, Libretti A. Captopril for the treatment of patients with hypertension and peripheral vascular disease. Angiology. 1985;36(5):293–6. 10.1177/000331978503600505 [DOI] [PubMed] [Google Scholar]
- 27.Catalano M, Tomasini M, Scandale G, Galimberti P, Milani M, Di Perri T, et al. Isradipine in the treatment of peripheral occlusive vascular disease of the lower limbs: a pilot study. J Int Med Res. 1992;20(4):323–30. 10.1177/030006059202000403 [DOI] [PubMed] [Google Scholar]
- 28.Spence JD, Arnold JMO, Munoz CE, Viswanatha A, Huff M, DeRose G, Harris K. Angiotensin-converting enzyme inhibition with cilazapril does not improve blood flow, walking time, or plasma lipids in patients with intermittent claudication. J Vasc Med Biol. 1993;4(1):23–7. [Google Scholar]
- 29.Walker SR, Tennant S, MacSweeney ST. A randomized, double-blind, placebo-controlled, crossover study to assess the immediate effect of sublingual glyceryl trinitrate on the ankle brachial pressure index, claudication, and maximum walking distance of patients with intermittent claudication. J Vasc Surg. 1998;28(5):895–900. [DOI] [PubMed] [Google Scholar]
- 30.Kimose H-H, Bagger JP, Aagaard MT, Paulsen PK. Placebo-controlled, double-blind study of the effect of verapamil in intermittent claudication. Angiology. 1990;41(8):595–8. 10.1177/000331979004100802 [DOI] [PubMed] [Google Scholar]
- 31.Casiglia E, Petucco S, Pessina AC. Antihypertensive efficacy of amlodipine and enalapril and effects on peripheral blood flow in patients with essential hypertension and intermittent claudication. Clin Drug Invest. 1997;13(1):97–101. [Google Scholar]
- 32.Catalano M, Libretti A. A multicenter study of doxazosin in the treatment of patients with mild or moderate essential hypertension and concomitant intermittent claudication. Am Heart J. 1991;121(1 Pt 2):367–71. [DOI] [PubMed] [Google Scholar]
- 33.Lane DA, Lip GY. Treatment of hypertension in peripheral arterial disease. Cochrane Database Syst Rev. 2013;12:CD003075. [DOI] [PubMed] [Google Scholar]
- 34.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Higgins JPT, Green S (editors). Cochrane handbook for systematic reviews of interventions version 5.1. 0 [updated March 2011]. The Cochrane Collaboration, 2011. www.cochrane-handbook.org. [Google Scholar]
- 36.Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c332 10.1136/bmj.c332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wallace BC, Schmid CH, Lau J, Trikalinos TA. Meta-Analyst: software for meta-analysis of binary, continuous and diagnostic data. BMC Med Res Methodol. 2009;9(1):80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Overlack A, Adamczak M, Bachmann W, Bonner G, Bretzel RG, Derichs R, et al. ACE-inhibition with perindopril in essential hypertensive patients with concomitant diseases. The Perindopril Therapeutic Safety Collaborative Research Group. Am J Med. 1994;97(2):126–34. [DOI] [PubMed] [Google Scholar]
- 39.Labs KH, Dormandy JA, Jaeger KA, Stuerzebecher CS, Hiatt WR. Transatlantic Conference on Clinical Trial Guidelines in Peripheral Arterial Disease: clinical trial methodology. Basel PAD Clinical Trial Methodology Group. Circulation. 1999;100(17):e75–81. [DOI] [PubMed] [Google Scholar]
- 40.Day SJ, Altman DG. Statistics notes: blinding in clinical trials and other studies. BMJ. 2000;321(7259):504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA. 1995;273(5):408–12. [DOI] [PubMed] [Google Scholar]
- 42.Elbourne DR, Altman DG, Higgins JP, Curtin F, Worthington HV, Vail A. Meta-analyses involving cross-over trials: methodological issues. Int J Epidemiol. 2002;31(1):140–9. [DOI] [PubMed] [Google Scholar]
- 43.Wright JT Jr., Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, et al. A Randomized Trial of Intensive versus Standard Blood-Pressure Control. N Engl J Med. 2015;373(22):2103–16. 10.1056/NEJMoa1511939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shahin Y, Barnes R, Barakat H, Chetter IC. Meta-analysis of angiotensin converting enzyme inhibitors effect on walking ability and ankle brachial pressure index in patients with intermittent claudication. Atherosclerosis. 2013;231(2):283–90. 10.1016/j.atherosclerosis.2013.09.037 [DOI] [PubMed] [Google Scholar]
- 45.Ahimastos AA, Walker PJ, Askew C, Leicht A, Pappas E, Blombery P, et al. Effect of ramipril on walking times and quality of life among patients with peripheral artery disease and intermittent claudication: a randomized controlled trial. JAMA. 2013;309(5):453–60. 10.1001/jama.2012.216237 [DOI] [PubMed] [Google Scholar]
- 46.Ahimastos AA, Lawler A, Reid CM, Blombery PA, Kingwell BA. Brief communication: ramipril markedly improves walking ability in patients with peripheral arterial disease: a randomized trial. Ann Intern Med. 2006;144(9):660–4. [DOI] [PubMed] [Google Scholar]
- 47.Shahin Y, Mazari F, Chetter I. Do angiotensin converting enzyme inhibitors improve walking distance in patients with symptomatic lower limb arterial disease? A systematic review and meta-analysis of randomised controlled trials. Int j surg. 2011;9(3):209–13. 10.1016/j.ijsu.2010.12.006 [DOI] [PubMed] [Google Scholar]
- 48.Ostergren J, Sleight P, Dagenais G, Danisa K, Bosch J, Qilong Y, et al. Impact of ramipril in patients with evidence of clinical or subclinical peripheral arterial disease. Eur Heart J. 2004;25(1):17–24. [DOI] [PubMed] [Google Scholar]
- 49.Bavry AA, Anderson RD, Gong Y, Denardo SJ, Cooper-Dehoff RM, Handberg EM, et al. Outcomes Among hypertensive patients with concomitant peripheral and coronary artery disease: findings from the INternational VErapamil-SR/Trandolapril STudy. Hypertension. 2010;55(1):48–53. 10.1161/HYPERTENSIONAHA.109.142240 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
(DOC)
Results are expressed as mean ± SD. The mathematical approach taken for obtaining these data is given in S2 Table. Mean arterial pressure was defined from the following formula: MAP = [(2*DBP) + SBP] / 3. Different anti-hypertensives were used in the trials: Overlack trial—perindopril, Shahin et al.–ramipril, Zankl et al.–telmisartan, Bagger et al.–verapamil, Robert et al.–captopril, atenolol, labetolol and pindolol. Abbreviations: DBP- diastolic blood pressure, MAP—mean arterial pressure, PI—post-intervention and SBP—systolic blood pressure.
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.