Abstract
Introduction:
Patients with incurable cancer have poor prognostic awareness. We present a detailed analysis of the dialogue between oncologists and patients in conversations with prognostic implications.
Methods:
A total of 128 audio-recorded encounters from a large multisite trial were obtained, and 64 involved scan results. We used conversation analysis, a qualitative method for studying human interaction, to analyze typical patterns and conversational devices.
Results:
Four components consistently occurred in sequential order: symptom-talk, scan-talk, treatment-talk, and logistic-talk. Six of the encounters (19%) were identified as good news, 15 (45%) as stable news, and 12 (36%) as bad news. The visit duration varied by the type of news: good, 15 minutes (07:00-29:00); stable, 17 minutes (07:00-41:00); and bad, 20 minutes (07:00-28:00). Conversational devices were common, appearing in half of recordings. Treatment-talk occupied 50% of bad-news encounters, 31% of good-news encounters, and 19% of stable-news encounters. Scan-talk occupied less than 10% of all conversations. There were only four instances of frank prognosis discussion.
Conclusion:
Oncologists and patients are complicit in constructing the typical encounter. Oncologists spend little time discussing scan results and the prognostic implications in favor of treatment-related talk. Conversational devices routinely help transition from scan-talk to detailed discussions about treatment options. We observed an opportunity to create prognosis-talk after scan-talk with a new conversational device, the question “Would you like to talk about what this means?” as the oncologist seeks permission to disclose prognostic information while ceding control to the patient.
INTRODUCTION
Patients with advanced and incurable cancer generally overestimate their probability for long-term survival and misunderstand the goals of anticancer therapy.1,2 Weeks et al3 showed that 69% of patients with metastatic lung cancer and 81% of patients with metastatic colorectal cancer incorrectly believed their chemotherapy was curative in intent; Rocque et al4 found that only 65% of hospitalized patients with advanced cancer correctly identified their cancer as incurable. In this article, we present an analysis of the nature of talk in the cancer clinic, describing why patients might misunderstand the incurable nature of their disease, and then propose a simple intervention, a question, that we anticipate will improve the quality of prognostic discussions.
Poor prognostic awareness may lead to unrealistic expectations and the pursuit of inappropriately aggressive therapy. Doctors typically convey detailed information about a serious diagnosis only in response to direct inquiries from patients.5-7 Fifty-seven percent of oncologists self-reported that they sometimes, rarely, or never give a time frame for when they think death is likely to occur.8 Barriers that hinder understanding in conversations about prognosis and end-of-life issues include the following: (1) bad news is bad and inherently difficult to disclose9-11; therefore, disclosure is often shrouded to seem more optimistic to preserve hope12-15; (2) patients may misinterpret their prognosis, even if it is explicitly stated by the oncologist3; (3) physicians and patients are often complicit in withholding or ignoring important prognostic information16-18; and (4) reporting bad news has been shown to be a dispreferred social action.9,10,19,20 Simply put, just as oncologists struggle to give bad news, patients struggle to receive it.
Patient-centered health care has gained prominence as the best way of providing modern health care.21-24 As such, shared decision making (SDM) and patient-centered communication (PCC) are seen as the key vehicles for optimal care25-28 as both moral imperatives and means to align treatment with a patient’s preferences. The incorporation of SDM and PCC into regular clinical practice, however, has been met with major impediments.29 Barriers to achieving patient-centered care, SDM, and PCC can be organized into two general categories: (1) those due to the structure of the medical health care system itself and, most important for this article, (2) those due to the interactions between medical staff and patients.22,23,29,30
Although it has been demonstrated that patients have poor illness understanding, little is known about how oncologists actually discuss prognostic information with patients and whether that discussion contributes to patients’ misperceptions. In this study, we collected a set of recordings of conversations between oncologists and patients when scan results were presented to analyze critical conversations with prognostic implications. Our main objectives were to first to observe how oncologists spend time in the room with patients and determine patterns of communication, with a specific focus on identifying explicit and implicit prognosis discussion. Next, using conversation analysis (CA) as our main methodologic approach, we assessed whether oncologists used conversational devices that shrouded prognosis. To our knowledge, we present a new conversational device that is expected to create a space for discussion of prognostic information as a result of our analysis. Furthermore, it may also help to maintain the principles of SDM and patient-centered care and has the potential to significantly improve prognostic communication.
METHODS
This report is a secondary analysis of data collected from a multisite, nonblinded randomized trial testing the effectiveness of the Web-based Comprehensive Health Enhancement Support System31,32 for patients with lung cancer and caregiver dyads. Dyads were recruited from four academic cancer center hospitals in the eastern, midwestern, and southwestern United States between September 2004 and April 2007, with data collection ending in May 2009. Primary eligibility criteria were English-speaking adults with stage IIIA, IIIB, or IV non–small-cell lung cancer. A total of 518 caregiver-patient dyads were assessed for eligibility, and 144 caregiver-patient dyads received the Comprehensive Health Enhancement Support System intervention.32 Our data set included audio-recorded encounters of multiple oncologists with the dyads from all study sites. A total of 11 physician faculty members were audio recorded at these different institutions, of whom three were women and eight were men. We listened to 128 recorded conversations. After excluding any conversations that were devoid of scan results, a further reduction in data was made because of the intensive nature of CA, which brought us to 64 conversations. These 64 conversations were then transcribed and analyzed using CA conventions. Our analysis of laudable event proposals (LEP) and/or appreciation sequences (AS) comes from the 33 cases that we found in the 64 conversations we analyzed using CA. We categorized the type of news delivered in each encounter as good, stable, or bad news on the basis of the content of the recording. To describe how oncologists and patients spend their time together, we categorized the amount of time spent in each phase of conversation on the basis of the type of news delivered. The University of Wisconsin institutional review board approved this analysis.
The oncologist-patient interactional dynamic is extremely complex and requires an equally intensive analysis technique: CA. CA is an examination of what Sacks33(p211) called “naturally occurring social activities” and is a precise tool for the study of human interaction. It is an inductive, empirically driven approach that captures minute interactional features and identifies reoccurring patterns. CA focuses on the organization of an interaction—how participants recognize what the other is saying and take part in understanding one another. Analysts uncover patterns and orderly conversational devices, which are specific utterances, phrases, or sentences that provide the speaker with the ability to accomplish a social action. The result is a detailed description of the practices by which participants achieve the organization of human interactions. To give a sense of the detail involved, transcription of an audio file into a CA transcript requires approximately 10 to 100 times the length of the audio file, for example, 10 minutes of audio recording could take up to 10 hours to transcribe, including details such as prosody, microinflections, rising and falling volume and pitch, and pauses.34 CA is an established strategy to examine the fine detail in nuanced conversations.
We previously described oncologists’ routine use of two conversational devices, termed LEP and AS, as transitional phrases to help them close out and shift from reporting scan news to talking about treatment options.35 We uncovered and specifically analyzed the use of these conversational devices.35 These two devices showed up in more than half (ie, 33) of the transcripts. Panel 1 in Appendix Fig A1 (online only) demonstrates an LEP, defined as an utterance that offers a praiseworthy or favorable version of scan results. Oncologists use this technique to recruit patients to their perspective when the news is not exactly what the patient expected or wanted to hear. Panel 2 in Appendix Fig A1 demonstrates an AS, an utterance reminding patients to appreciate the fact that their health status is relatively good and that the treatment has been beneficial.
RESULTS
Oncology Encounter Structure Is Consistent
Medical interviews in primary care have an ordered structure of component activities.13,35-38 We found that oncologic visits also follow a typical phase structure. In fact, 77% of them followed the typical phase structure (49 of 64), whereas 23% (15 of 64) deviated from this structure. This phase structure comprises four central components that typically follow this order: symptom-talk, scan-talk, treatment-talk, and logistic-talk. After initial greetings, patients and caregivers report on physical and psychologic symptoms, which we call symptom-talk. Next, there is a transition to reporting the most recent imaging and laboratory results, which we call scan-talk. The conversation then shifts to treatment-talk, where oncologists and patients discuss chemotherapy, radiation, surgical, or symptom management options. Finally, logistic-talk consists of coordination and organization of care (eg, instructions for scheduling a follow-up visit).
We call the interactional phase structure typical because these four components appear often, and in sequential order, across oncology visits. In fact, as shown in Panel 3 in Appendix Fig A1, when a doctor or patient attempts to skip over one of the first three phases, the attempt is often blocked or explicitly acknowledged by the other participant, demonstrating a form of resistance. Thus, in line with CA inquiry, participants co-construct and maintain the social order of these oncology visits.
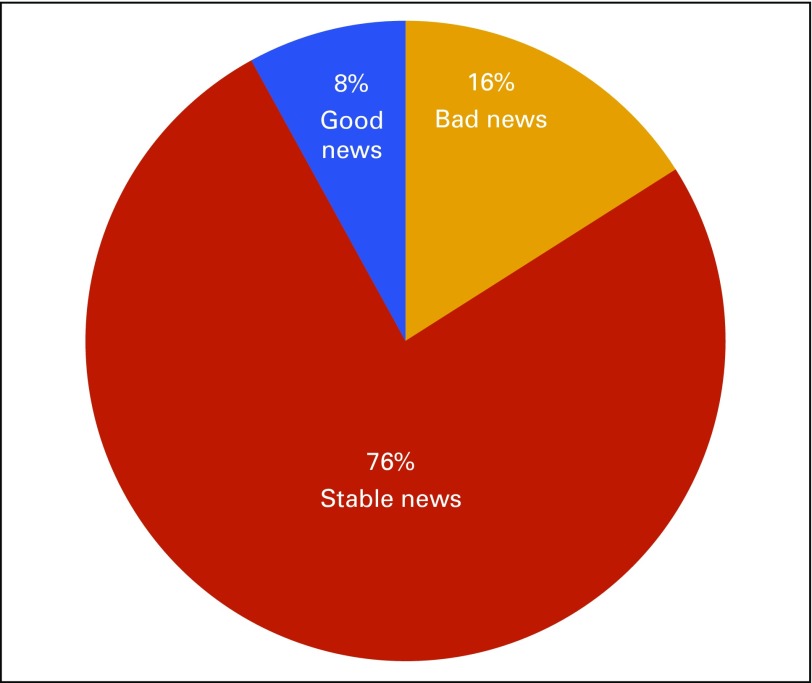
Good, Stable, or Bad News
Of the 33 analyzed conversations that had an AP or LEP, six (19%) were identified as good news delivery, 15 (45%) as stable news delivery, and 12 (36%) as bad news delivery. The average amount of time oncologists spent in the room varied in relation to the type of news delivered: for good news delivery, 15:03 minutes (range, 07:25-29:05); stable news delivery, 17:14 minutes (range, 06:50-41:19); and bad news delivery, 20:53 minutes (range, 07:1428:10).
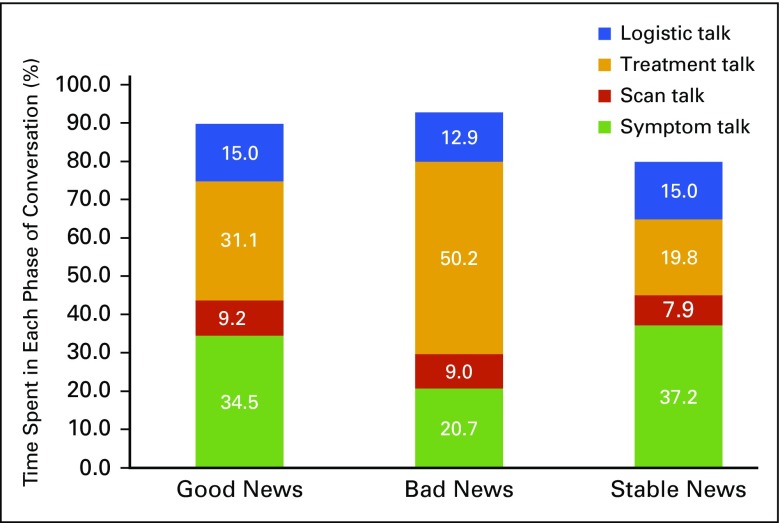
Fig 1 depicts the time spent in each phase of conversation in relation to the type of news delivered. More time was spent discussing symptoms during stable (37.2%) and good news (34.5%) delivery, whereas less time was devoted to this topic during bad news delivery. When bad news was delivered, approximately 50% of the conversation was devoted to treatment-talk, whereas with good and stable news delivery, it was 31% and 19%, respectively. Scan-talk, which is indisputably news of a prognostic nature, was always less than 10% of the entire conversation, regardless of the news type delivered. Logistic-talk made up about 15% of all conversations regardless of the type of news delivered. In all cases, the physicians spoke the vast majority of the time and demonstrated control over the direction of the discussion, particularly with regard to transitioning between different phases of the conversation. Furthermore, although we argue that these discussions are co-constructed, this does not ensure that each participant has an equal say in how conversations unfold or what topics are brought up and when they are introduced; asymmetry in clinical interactions exists.39,40 The transitions between the typical components were often quick.
FIG 1.
Time management by type of news delivery. The graph shows the amount of time spent in each phase of conversation in relation to the type of news being delivered. The percentages do not add up to 100% because we excluded the small talk that often comes at the end of the clinic visit. Such small talk includes, for example, weekend plans.
Prognosis-Talk
There were only four instances of frank prognosis discussion in which life expectancy was discussed, and three of these instances (75%) were initiated by the patient or caregiver. We observed significant but unexplicated prognostic information most frequently shrouded in scan-talk, in which the size of a tumor was characterized either explicitly (eg, grown by 5 mm) or categorically (“getting bigger”). These interactions were too numerous to count. We also noted that patients or caregivers tried to elicit more information about the meaning of their scan results, presumably in an attempt to better decipher their underlying prognosis. These instances typically occurred at the beginning of treatment-talk, when the patient would pause the discussion about treatment and attempt to transition back to scan-talk. Some ways in which they did this included reiterating what physicians initially stated about the scan (“So the scan is stable?”), asking for specifics about the size of the malignancy and focusing on radiographic technique (eg, contrast, type of study). The physicians’ usual way of responding was to briefly reiterate what they had said previously about the scan and reattempt a transition to treatment-talk. We anticipated quantifying explicit empathetic statements, which we expected would occur during prognosis communication, but there was a notable absence of these statements.
Use of Conversation Devices
LEP and AS are common, appearing in nearly half of all recorded conversations. In 84% of these instances, they appear in association with stable or bad news (Fig 2). When it did not seem appropriate to use an LES or AS, for example, because of dire news, there were other devices physicians used, such as an optimistic projection.10,41 In one instance, the oncologist described progression in the liver after second-line docetaxel and then upgraded this news, saying, “The good news is there there’s a lot of other options here.” In this conversation, an optimistic projection was used to transition to treatment-talk and functioned to obscure the nature of the bad news (Panel 4 in Appendix Fig A1).
FIG 2.
The frequency of laudable event proposals and appreciation sequences by type of news. These devices are most commonly associated with stable news and bad news, and less often seen in good news discussions.
DISCUSSION
We intended to characterize the nature of oncologist-patient talk to better understand the observed phenomenon that patients with cancer have poor prognostic awareness. Medical interviews in primary care have an ordered structure of component activities, and a similar pattern is observed in the oncologic visit. Our analysis concludes with four primary observations.
First, oncologists spend the shortest amount of time on the discussion of scan news and its prognostic implications. Oncologists seem determined to move the conversation to treatment-talk, often using an AS or LEP as the transition mechanism. An estimate of life expectancy was provided in only four clinical encounters (6%), and three of those were at the request of patients or caregivers, suggesting that prognostic discussions will occur when invited. This is important, considering recent findings that show that patients’ illness understanding improves after continued prognosis discussions.42 We observed only rare instances of empathic statements or silence to allow processing of the serious news. The paucity of explicit prognostic communication in the encounters likely contributes to the observed poor illness understanding seen nationally.1-4 This makes it difficult to create interactional space to use the main attributes of SDM and PCC—building a consensus about the preferred treatment,43 creating a clear understanding of the information being discussed, supporting opportunities for patient autonomy, and providing emotional support as needed.44
Second, oncologists quickly transition the conversation from scan-talk to treatment-talk. We observed immediate transition to treatment-talk during the disclosures of bad news, which potentially contributes to patients’ misinterpretation of their prognosis and stifles any further discussions surrounding prognosis. We also found that patients and their caregivers rarely inquire about prognosis, suggesting this is a socially dispreferred action, much the same way an oncologists’ disclosure of a poor prognosis might be. This preexisting dynamic sets the stage for both parties to communicate in a way that avoids explicit discussion about survival. Although avoidance may seem emotionally preferable in the short term, poor-prognosis discussions negatively affect illness understanding, which can affect advance care planning, care satisfaction,3,45 and the amount of patient involvement in decision making.46
There is an opportunity after scan-talk and before treatment recommendations for an intentional pause and a question: “Would you like to talk about what this means?” By phrasing this as a question, the oncologist seeks permission to enter into a space where prognosis can be discussed while ceding control of the conversation to the patient. An affirmative response—“Yes, I would like to know”—could empower oncologists to disclose the prognostic implications of the test results. Pausing after the delivery of scan news would also create an opportunity to express empathy, an emotion that is both the imaginative reconstruction of another’s perspective and the emotional resonance this creates in the self.47 Crucially, the addition of this question does not alter the typical flow or organization of an oncologist-patient interaction and thus has the potential to improve prognostic communication without breaking its intrinsic structure.
Third, the routine use of conversational devices to transition out of scan-talk leads the discussion to detailed talk about anticancer treatment options, which are often optimistically framed and possibly misleading. This tendency is most readily apparent during the delivery of stable and bad news, which is when we see an increased incidence of AS and LEP. This suggests that oncologists realize that delivery of stable news will be construed as bad news by patients and thus pre-emptively attempt to convince patients of their belief that, for example, stable disease is good news. Although this conversational technique might seem to ease the emotional reaction to unwanted news in the short term, it also drives the conversation away from prognostic communication and minimizes empathic opportunities.
Fourth, when oncologists discuss the impact of treatment, they rely on jargon (most commonly, response rates), rather than more tangible patient outcomes. Together, these four observed communication patterns limit patient inquiries about “what this [scan results] means to the quality or duration of my life” and runs counter to the main principles of SDM and patient-centered care. Our findings contribute to this growing body of knowledge that examines the importance of diagnostic imaging results38,48,49; the analysis of the many impediments hindering the implementation of SDM, PCC, and patient-centered care23,26,29,50,51; and the literature that documents the importance of clear prognostic discussion.3,46,52-54
There are several strengths to this study. This was a multi-institutional study reflective of practice styles from both academic and private clinics, with oncologists trained in different programs and practicing in different parts of the country, and the sample size was relatively large for a CA study. Some limitations include the fact that nonverbal cues could not be identified or commented on by only listening to audio recordings. The audio recordings analyzed were 10 years old and might not reflect current prognosis communication practices of oncologists. Although treatment options have evolved, we have no reason to believe oncologists’ communication behaviors have changed to any significant degree in the last 10 years. Our analysis is specific to oncologists and thus not necessarily reflective of the communication practices of other clinicians.
In conclusion, oncologists communicate scan results to patients with a natural and structured pattern of talk. A natural collusion to avoid the prognostic implications of the scans permeates the patient-physician relationship. There is a need to create space within the typical phase structure for prognosis communication. We propose the question “Would you like to talk about what this means?” as a communication device that can regularly incorporate occasions for prognosis-talk and SDM in the clinic encounters. It has the benefit of keeping the sequential order of the phase structure intact and maintaining the oncologist’s role as the lead architect of the discussion.
Although efforts should continue to support communication skills training, our research suggests a simple modification that requires little education or training, that is aligned with the way oncologists naturally communicate, and that could meaningfully affect the dialogue. It is our hope that, as patients answer this question honestly, oncologists, too, can engage in discussion surrounding prognosis that leads to enhanced prognostic awareness and improved illness understanding.
ACKNOWLEDGMENT
Supported by Grant No. P50 CA095817-01A1 from the National Cancer Institute through the Center for Health Enhancement Systems Studies at the University of Wisconsin, the Cambia Health Foundation’s Sojourns Scholars Leadership Program (T.C.C.), and a T32 National Research Service Award (No. AT006956) from the National Center for Complementary and Integrative Health at the National Institutes of Health (D.C.). These funding sources had no role in the design, preparation, review, or approval of the manuscript for publication. No other financial support was declared for the remaining authors. The authors thank Gabrielle Rocque and Jamie Von Roenn for their review of a previous version of this manuscript.
Appendix
FIG A1.
Examples of communication phenomena. CT, computed tomography; NSCLC, non–small-cell lung cancer.
AUTHOR CONTRIBUTIONS
Conception and design: Sarguni Singh, Dagoberto Cortez, James F. Cleary, Toby C. Campbell
Provision of study materials or patients: Lori DuBenske
Collection and assembly of data: James F. Cleary, Lori DuBenske, Toby C. Campbell
Data analysis and interpretation: Sarguni Singh, Dagoberto Cortez, Douglas Maynard, Toby C. Campbell
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Characterizing the Nature of Scan Results Discussions: Insights Into Why Patients Misunderstand Their Prognosis
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/journal/jop/site/misc/ifc.xhtml.
Sarguni Singh
No relationship to disclose
Dagoberto Cortez
No relationship to disclose
Douglas Maynard
No relationship to disclose
James F. Cleary
No relationship to disclose
Lori DuBenske
No relationship to disclose
Toby C. Campbell
No relationship to disclose
REFERENCES
- 1.Pronzato P, Bertelli G, Losardo P, et al. What do advanced cancer patients know of their disease? A report from Italy. Support Care Cancer. 1994;2:242–244. doi: 10.1007/BF00365729. [DOI] [PubMed] [Google Scholar]
- 2.Weeks JC, Cook EF, O’Day SJ, et al. Relationship between cancer patients’ predictions of prognosis and their treatment preferences. JAMA. 1998;279:1709–1714. doi: 10.1001/jama.279.21.1709. [DOI] [PubMed] [Google Scholar]
- 3.Weeks JC, Catalano PJ, Cronin A, et al. Patients’ expectations about effects of chemotherapy for advanced cancer. N Engl J Med. 2012;367:1616–1625. doi: 10.1056/NEJMoa1204410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rocque GB, Campbell TC, Johnson SK, et al. A quantitative study of triggered palliative care consultation for hospitalized patients with advanced cancer. J Pain Symptom Manage. 2015;50:462–469. doi: 10.1016/j.jpainsymman.2015.04.022. [DOI] [PubMed] [Google Scholar]
- 5.Christakis NA. Prognostication and bioethics. Daedalus. 1999;128:197–214. [PubMed] [Google Scholar]
- 6.Helft PR. Necessary collusion: Prognostic communication with advanced cancer patients. J Clin Oncol. 2005;23:3146–3150. doi: 10.1200/JCO.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 7.Schaepe KS: Affective Communication: Management of Bad News Following Cancer Diagnosis & Stem Cell Transplant. Madison, WI, University of Wisconsin–Madison, 2013 [Google Scholar]
- 8.Daugherty CK, Hlubocky FJ. What are terminally ill cancer patients told about their expected deaths? A study of cancer physicians’ self-reports of prognosis disclosure. J Clin Oncol. 2008;26:5988–5993. doi: 10.1200/JCO.2008.17.2221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dosanjh S, Barnes J, Bhandari M. Barriers to breaking bad news among medical and surgical residents. Med Educ. 2001;35:197–205. doi: 10.1046/j.1365-2923.2001.00766.x. [DOI] [PubMed] [Google Scholar]
- 10.Maynard DW: Bad News, Good News: Conversational Order in Everyday Talk and Clinical Settings. Chicago, IL, University of Chicago Press, 2003 [Google Scholar]
- 11.Taylor KM. “Telling bad news”: Physicians and the disclosure of undesirable information. Sociol Health Illn. 1988;10:109–132. doi: 10.1111/j.1467-9566.1988.tb00001.x. [DOI] [PubMed] [Google Scholar]
- 12.Peräkylä A, Sorjonen M-L: Emotion in interaction. Oxford, United Kingdom, Oxford University Press, 2012 [Google Scholar]
- 13.Heritage J, Maynard DW (eds): Communication in Medical Care: Interaction Between Primary Care Physicians and Patients. Cambridge, United Kingdom, Cambridge University Press, 2006 [Google Scholar]
- 14.Holt E: The structure of death announcements: Looking on the bright side of death. Int J Stud Discourse 13:189-212, 1993
- 15.Maynard DW, Freese J: Good news, bad news, and affect: Practical and temporal “emotion work” in everyday life, in Peräkylä A, Sorjonen M-L (eds): Emotion in Interaction. Oxford, United Kingdom, Oxford University Press, 2012, pp 92-112 [Google Scholar]
- 16.Leydon GM, Boulton M, Moynihan C, et al. Cancer patients’ information needs and information seeking behaviour: In depth interview study. BMJ. 2000;320:909–913. doi: 10.1136/bmj.320.7239.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.The AM, Hak T, Koëter G, et al. Collusion in doctor-patient communication about imminent death: An ethnographic study. BMJ. 2000;321:1376–1381. doi: 10.1136/bmj.321.7273.1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vos MS, Berendsen HH: 'Doctor, I don’t want to know’: An investigation of denial in lung cancer patients, in Vos MS (ed): Denial and Quality of Life in Lung Cancer Patients. Amsterdam, Netherlands, Amsterdam University Press, 2009, pp 15-24 [Google Scholar]
- 19.Lutfey KE, Maynard DW. Bad news in oncology: How physician and patient talk about death and dying without using those words. Soc Psychol Q. 1998;61:321–341. [Google Scholar]
- 20.Ptacek JT, McIntosh EG. Physician challenges in communicating bad news. J Behav Med. 2009;32:380–387. doi: 10.1007/s10865-009-9213-8. [DOI] [PubMed] [Google Scholar]
- 21.Institute of Medicine Committee on Quality of Health Care in America: Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC, National Academies Press, 2001 [Google Scholar]
- 22.Epstein RM, Franks P, Fiscella K, et al: Measuring patient-centered communication in patient-physician consultations: Theoretical and practical issues. Soc Sci Med 61:1516-1528, 2005 [DOI] [PubMed]
- 23.Mead N, Bower P: Patient-centredness: A conceptual framework and review of the empirical literature. Soc Sci Med 51:1087-1110, 2000 [DOI] [PubMed]
- 24.Stewart M, Brown JB, Donner A, et al. The impact of patient-centered care on outcomes. J Fam Pract. 2000;49:796–804. [PubMed] [Google Scholar]
- 25.Barry MJ, Edgman-Levitan S. Shared decision making--pinnacle of patient-centered care. N Engl J Med. 2012;366:780–781. doi: 10.1056/NEJMp1109283. [DOI] [PubMed] [Google Scholar]
- 26.Légaré F, Ratté S, Gravel K, et al. Barriers and facilitators to implementing shared decision-making in clinical practice: Update of a systematic review of health professionals’ perceptions. Patient Educ Couns. 2008;73:526–535. doi: 10.1016/j.pec.2008.07.018. [DOI] [PubMed] [Google Scholar]
- 27.Légaré F, Stacey D, Turcotte S, et al. Interventions for improving the adoption of shared decision making by healthcare professionals. Cochrane Database Syst Rev. 2014;9:CD006732. doi: 10.1002/14651858.CD006732.pub3. [DOI] [PubMed] [Google Scholar]
- 28.Weston WW: Informed and shared decision-making: The crux of patient-centered care. CMAJ 165:438-439, 2001 [PMC free article] [PubMed]
- 29.Joseph-Williams N, Elwyn G, Edwards A. Knowledge is not power for patients: A systematic review and thematic synthesis of patient-reported barriers and facilitators to shared decision making. Patient Educ Couns. 2014;94:291–309. doi: 10.1016/j.pec.2013.10.031. [DOI] [PubMed] [Google Scholar]
- 30.Ishikawa H, Hashimoto H, Kiuchi T. The evolving concept of “patient-centeredness” in patient-physician communication research. Soc Sci Med. 2013;96:147–153. doi: 10.1016/j.socscimed.2013.07.026. [DOI] [PubMed] [Google Scholar]
- 31.Gustafson DH, DuBenske LL, Namkoong K, et al. An eHealth system supporting palliative care for patients with non-small cell lung cancer: A randomized trial. Cancer. 2013;119:1744–1751. doi: 10.1002/cncr.27939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.DuBenske LL, Gustafson DH, Namkoong K, et al: CHESS improves cancer caregivers' burden and mood: Results of an eHealth RCT. Health Psychol 33:1261-1272, 2014 [DOI] [PMC free article] [PubMed]
- 33.Sacks H. Harvey Sacks lectures 1964-1965. Hum Stud. 1989;12:211–215. [Google Scholar]
- 34.Chatwin J. Conversation analysis. Complement Ther Med. 2004;12:131–135. doi: 10.1016/j.ctim.2004.07.042. [DOI] [PubMed] [Google Scholar]
- 35.Maynard DW, Cortez D, Campbell TC. “End of life” conversations, appreciation sequences, and the interaction order in cancer clinics. Patient Educ Couns. 2016;99:92–100. doi: 10.1016/j.pec.2015.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Byrne PS, Long BEL: Doctors Talking to Patients: A Study of the Verbal Behavior of General Practitioners Consulting in Their Surgeries. London, United Kingdom, Her Majesty’s Stationary Office, 1976 [Google Scholar]
- 37.Robinson JD. An interactional structure of medical activities during acute visits and its implications for patients’ participation. Health Commun. 2003;15:27–57. doi: 10.1207/S15327027HC1501_2. [DOI] [PubMed] [Google Scholar]
- 38.Frankel RM: Talking in interviews: A dispreference for patient-initiated questions in physician-patient encounters, in Psathas G: Interactional Competence. Washington, DC.: International Institue for Ethnomethodology and Conversation Analysis & University Press of America, 1990, pp 231- 262 [Google Scholar]
- 39.Maynard D. Interaction and asymmetry in clinical discourse. Am J Sociol. 1991;97:448–495. [Google Scholar]
- 40.Pilnick A, Dingwall R: On the remarkable persistence of asymmetry in doctor/patient interaction: A critical review. Soc Sci Med 72:1374-1382, 2011 [DOI] [PubMed]
- 41.Jefferson G. On the sequential organization of troubles-talk in ordinary conversation. Soc Probl. 1988;35:418–441. [Google Scholar]
- 42.Epstein AS, Prigerson HG, O’Reilly EM, et al. Discussions of life expectancy and changes in illness understanding in patients with advanced cancer. J Clin Oncol. 2016;34:2398–2403. doi: 10.1200/JCO.2015.63.6696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Charles C, Gafni A, Whelan T: Decision-making in the physician-patient encounter: Revisiting the shared treatment decision-making model. Soc Sci Med 49:651-661, 1999 [DOI] [PubMed]
- 44.Committee on Improving the Quality of Cancer Care: Patient-centered communication and shared decision making, in Levit L, Balogh E, Nass S, Ganz PA (eds): Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. Washington, DC, National Academies Press, 2013, pp 91-152 [PubMed] [Google Scholar]
- 45.Jagosh J, Donald Boudreau J, Steinert Y, et al. The importance of physician listening from the patients’ perspective: Enhancing diagnosis, healing, and the doctor-patient relationship. Patient Educ Couns. 2011;85:369–374. doi: 10.1016/j.pec.2011.01.028. [DOI] [PubMed] [Google Scholar]
- 46.Murtagh GM, Furber L, Thomas AL. Patient-initiated questions: How can doctors encourage them and improve the consultation process? A qualitative study. BMJ Open. 2013;3:e003112. doi: 10.1136/bmjopen-2013-003112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zelenski AB: Theatre-Based Empathy Training in Medicine: Exploring the Spaces in Between. Madison, WI, University of Wisconsin-Madison, 2015 [Google Scholar]
- 48.Maynard DW: Notes on the delivery and reception of diagnostic news regarding mental disabilities, in Helm DT, Anderson WT, Meehan AJ, et al: The Interactional Order: New Directions in the Study of Social Order. New York, NY, Irvington, 1989, pp 54-67
- 49.Peräkylä A. Authority and accountability: The delivery of diagnosis in primary health care. Soc Psychol Q. 1998;61:301–320. [Google Scholar]
- 50.Frosch DL, Singer KJ, Timmermans S: Conducting implementation research in community-based primary care: A qualitative study on integrating patient decision support interventions for cancer screening into routine practice. Health Expect 14:73-84, 2011 (suppl 1) [DOI] [PMC free article] [PubMed]
- 51.Pollard S, Bansback N, Bryan S. Physician attitudes toward shared decision making: A systematic review. Patient Educ Couns. 2015;98:1046–1057. doi: 10.1016/j.pec.2015.05.004. [DOI] [PubMed] [Google Scholar]
- 52.Hagerty RG, Butow PN, Ellis PA, et al. Cancer patient preferences for communication of prognosis in the metastatic setting. J Clin Oncol. 2004;22:1721–1730. doi: 10.1200/JCO.2004.04.095. [DOI] [PubMed] [Google Scholar]
- 53.Mack JW, Smith TJ. Reasons why physicians do not have discussions about poor prognosis, why it matters, and what can be improved. J Clin Oncol. 2012;30:2715–2717. doi: 10.1200/JCO.2012.42.4564. [DOI] [PubMed] [Google Scholar]
- 54.Enzinger AC, Zhang B, Schrag D, et al. Outcomes of prognostic disclosure: Associations with prognostic understanding, distress, and relationship with physician among patients with advanced cancer. J Clin Oncol. 2015;33:3809–3816. doi: 10.1200/JCO.2015.61.9239. [DOI] [PMC free article] [PubMed] [Google Scholar]