Abstract
Background
The body dysmorphic disorder is prevalent in general population and in psychiatric, dermatological, and plastic-surgery patients, but there lacks a structure-validated, comprehensive self-report measure of body image concerns, which is established through both exploratory and confirmatory factor analyses.
Methods
We have composed a 34-item matrix targeting the body image concerns and trialed it in 328 male and 365 female Chinese university students. Answers to the matrix dealt with treatments including exploratory factor analyses, reserve of qualified items, and confirmatory factor analyses of latent structures.
Results
Six latent factors, namely the Social Avoidance, Appearance Dissatisfaction, Preoccupation with Reassurance, Perceived Distress/Discrimination, Defect Hiding, and Embarrassment in Public, were identified. The factors and their respective items have composed a 24-item questionnaire named as the Body Image Concern Scale. Each factor earned a satisfactory internal reliability, and the intercorrelations between these factors were in a median level. Women scored significantly higher than men did on the Appearance Dissatisfaction, Preoccupation with Reassurance, and Defect Hiding.
Conclusion
The Body Image Concern Scale has displayed its structure validation and gender preponderance in Chinese university students.
Keywords: body dysmorphic disorder, body image, factor analysis, questionnaire development
Introduction
The body dysmorphic disorder is characterized by the preoccupation with appearance or self-image, which causes significant distress or impairment of daily functions to an individual.1 Its weighted prevalence in community adults was about 1.9%, in adolescents 2.2%, in students 3.3%, in psychiatric outpatients 5.8%, and in psychiatric inpatients 7.4%.2 Various psychiatric problems such as depression, suicidality, social isolation, or withdrawal are comorbid with the body dysmorphic disorder.3–6 This disorder is also diagnosed in 7%–15% patients who seek treatment from dermatologists or plastic surgeons.7 Regarding gender differences, men are more likely to be preoccupied with their genitals, muscles, and hair styles,8 while women are more likely to be preoccupied with their weight, hips, breasts, legs, and body hairs, to hide perceived defects with various camouflaging techniques.9,10
Besides some questionnaires measuring other psychosomatic problems together with the body dysmorphic disorder, there are some specific inventories measuring the body image concerns in both male and female participants. However, none of these specific ones is structure-validated after both exploratory and confirmatory factor analyses, and none has covered a broader concern of body image. For instance, the Body Dysmorphic Disorder Questionnaire11 measures the preoccupation with physical appearance such as body weight and its effects on daily life; however, the questionnaire does not comprehensively assess the body dysmorphic disorder.12 Another one is the Yale-Brown Obsessive-Compulsive Scale Modified for Body Dysmorphic Disorder,13 which measures the symptom severity and its changes over time, and the adaptation to the symptoms similar to those of the obsessive-compulsive disorder. The third one is the Body Dysmorphic Disorder Examination,14 which focuses on the body dysmorphic symptoms. However, it requires a face-to-face interview by a trained interviewer, which is time-consuming. The fourth (the Dysmorphic Concern Questionnaire)15 and the fifth (the Body Dysmorphic Symptom Scale)16 ones also measure the physical appearance in a unidimensional manner only.17,18
In the current study, we would like to develop a structure-validated self-report to measure a broader range of body image concerns. Based on the previous documentation, our first hypothesis is that such an assessment should be composed of the following six aspects. The first aspect includes the negative evaluation of and preoccupation with appearance. An example statement is “I am dissatisfied with my appearance defect,” as mentioned in previous studies.11,13–16 The second aspect is the distress caused by the appearance defect. One example is “I am often upset when concentrating on my appearance,” as studied previously.11,13,14,16 The third one is the embarrassment in public, and the feeling of being scrutinized by others. One sample is “I feel uneasy or embarrassed in public situations such as city streets or restaurants where I concentrate on my appearance,” as mentioned previously.14,16 The fourth is the repetitive behaviors or mental acts relating to appearance. An example is “I often camouflage my appearance defect with clothes or makeup,” as covered in previous studies.13–16 The fifth one is the avoidance of social activities or physical contacts with others. An example is “Because of my appearance, I avoid appearing in social situations such as parties or speaking to authority figures,” as previously reported.11,13,14,16 The sixth one is the preliminary exclusion of other mental disorders. For example, “I have suffered from one or more of the following: eating disorder, obsessive-compulsive disorder, anxiety disorder, major depressive disorder, or other mental disorders,” as noted previously.14
We, therefore, have developed an item matrix, and trialed it in Chinese university students. Our second hypothesis is that women score higher than men do on the negative evaluation of and the preoccupation with appearance, and on the repetitive behaviors (or mental acts) relating to appearance. We would apply both exploratory and confirmatory factor analyses to the item matrix, look for its latent factors and their possible gender differences, and develop a questionnaire measuring these body image concerns. We have expected that the emerged factors, the internal reliability of and the gender differences on these factors, and their interfactor relationships might help to describe the structure of the questionnaire.
Methods
Participants
Six hundred and ninety-three university students were invited to participate in the study: 328 men (mean age: 19.86 years with 1.78 SD; age range: 17–27 years) and 365 women (mean age: 20.42±2.16; age range: 17–26). There was no significant age difference between genders (t=−1.84, 95% confidence interval = [−0.58, 0.02], P=0.07). All participants were free from somatic or psychiatric illnesses and were asked to be drug or alcohol free for at least 72 hours prior to the test. The study protocol was approved by the Ethics Committee of Zhejiang University School of Public Health (No ZGL201606-1-1), and conformed to the Helsinki Declaration concerning human rights, and followed correct procedures concerning treatment of humans in research. All participants gave their written informed consent (guardians signed written informed consent for the young adolescents) for the current study.
Measures
The item matrix regarding the body image concerns covered the following aspects: (a) nine items for the negative evaluation of and preoccupation with appearance; (b) four items for the distress caused by the appearance defect; (c) six items for the embarrassment in public, and feeling of being scrutinized by others; (d) seven items for the repetitive behaviors or mental acts relating to appearance; (e) seven items for the avoidance of social activities or physical contacts with others; (f) one item for the preliminary exclusion of other mental disorders. The initial scale offers five alternatives with five-point Likert format: 1 – very unlike me, 2 – moderately unlike me, 3 – somewhat like and unlike me, 4 – moderately like me, and 5 – very like me.
Statistical analyses
Answers to the 34-item matrix were first subjected to a principal axis factoring analysis using the SPSS, Release Version 23.0.0 (IBM Corp., Armonk, NY, USA). Components extracted were treated as latent factors; the factor loadings were then rotated orthogonally using the varimax normalized methods. Items that were loaded less heavily (<0.40) on a target factor or cross-loaded heavily (>0.35) on more than one factor were removed from subsequent analyses one by one. The procedure continued until no further item needed to be removed.
The factor model fits were evaluated by confirmatory factor analysis for structural equation modeling using the Analysis of Moment Structures version 17.0 (AMOS Development Corp., 2008, Crawfordville, FL, USA). Following Schermelleh-Engel et al,19 and Hu and Bentler,20 we used the following parameters to identify the model fit: the χ2/df (better <3.0), goodness-of-fit index (better >0.9), adjusted goodness-of-fit index (better >0.9), comparative fit index (better >0.8), Tucker–Lewis index (better >0.8), root mean square error of approximation (better <0.05), and standardized root mean square residual (better <0.08). Afterwards, the factors and their related items were defined.
Furthermore, a questionnaire was developed based on the results of these exploratory and confirmatory factor analyses. The internal reliabilities (the Cronbach alphas) of the questionnaire factors were then calculated. The scores of each factor were submitted to multivariate analysis of variance (MANOVA) in the two gender groups. A P-value of <0.05 was considered to be significant. Moreover, the inter-relationships between factors in all participants were evaluated by the Pearson correlation test. To reduce the chance of Type I error regarding correlations, a P-value of <0.01 was considered to be significant.
Results
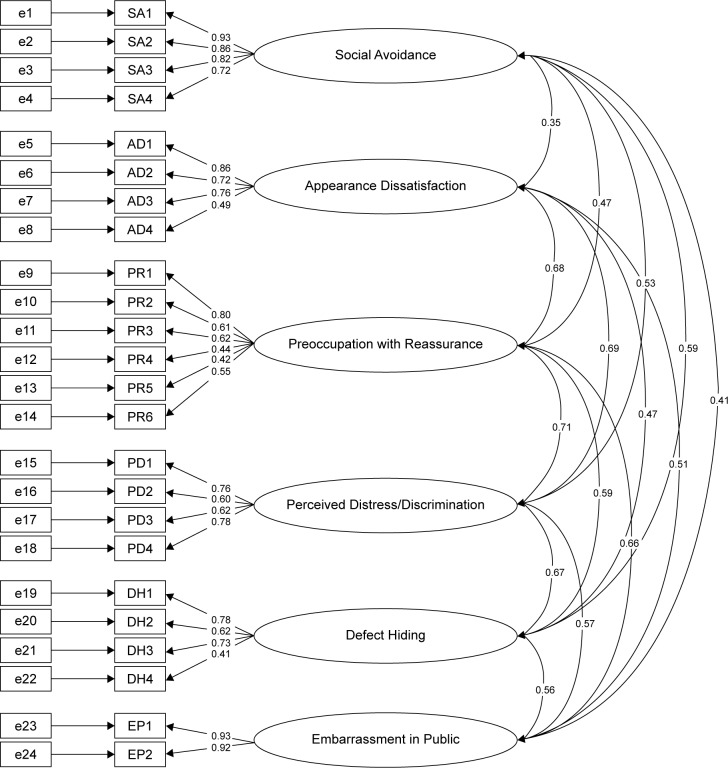
When analyzing the answers to the 34 items, after the principal axis factoring analysis, seven factors emerged with eigenvalues larger than 1.00: 31.98, 7.95, 5.04, 4.78, 3.76, 3.45, and 3.04. The visual speculation, the Minimum Average Partial test, and the Parallel Analysis suggested four- to seven-factor models; the first four, five, six, and seven factors altogether accounted for 49.74%, 53.50%, 56.96%, and 60.00%, respectively, of total variance. Items with higher target-loadings and lower cross-loadings on the respective factors were determined. According to the parameter values of the model fit (Table 1) and the item numbers for each factor, the six-factor model was the optimal one. The standardized structure of the six-factor model is illustrated in Figure 1.
Table 1.
Multiple-factor fitting models of the item matrix regarding the body image concerns in 693 participants
| Model | Item number under each factor | χ2/df | Goodness-of-fit index | Adjusted goodness-of-fit index | Tucker–Lewis index | Comparative fit index | Root mean square error of approximation | Standardized root mean square residual |
|---|---|---|---|---|---|---|---|---|
| Four-factor | 5, 5, 5, 3 | 4.14 | 0.92 | 0.90 | 0.88 | 0.90 | 0.067 | 0.062 |
| Five-factor | 7, 6, 6, 3, 2 | 4.21 | 0.89 | 0.86 | 0.88 | 0.89 | 0.068 | 0.066 |
| Six-factor | 4, 4, 6, 4, 4, 2 | 3.33 | 0.91 | 0.89 | 0.92 | 0.93 | 0.058 | 0.050 |
| Seven-factor | 4, 3, 2, 3, 4, 2, 2 | 3.14 | 0.94 | 0.91 | 0.94 | 0.95 | 0.056 | 0.046 |
Figure 1.
Standardized factor structures for a confirmatory factor analysis of the six-factor Body Image Concern Scale model.
Factor 1 was loaded with items relating to the avoidance of social activities, thus was named as Social Avoidance. Factor 2 with items relating to the dissatisfaction of body appearance defect was then called Appearance Dissatisfaction. Factor 3 with items describing the repetitive attempts to improve the appearance and obsessive thoughts about the defect was called Preoccupation of Reassurance. Factor 4 with items describing the excessive high attention to others’ opinions of appearance and the distress thoughts of discrimination due to appearance was called Perceived Distress/Discrimination. Factor 5 with items describing the actions to hide defect or camouflage was called Defect Hiding. Factor 6 with items describing the embarrassment in public or social situations was called Embarrassment in Public. The determined items to be left altogether formed an inventory called the Body Image Concern Scale (Table 2). In all participants (N=693), the internal reliabilities (the Cronbach alphas) of these six factors were 0.90, 0.79, 0.75, 0.78, 0.71, and 0.92, respectively, and the intercorrelations between factors were in a medium level (Table 3).
Table 2.
Item loadings on six factors in 693 participants
| Factor 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| Social Avoidance | ||||||
| Because of my appearance, I avoid appearing in social situations such as parties or speaking to authority figures | 0.84 | 0.16 | 0.08 | 0.15 | 0.18 | 0.15 |
| Because of my appearance, I avoid appearing in public situations such as restaurants, restrooms, or city streets | 0.80 | 0.10 | 0.09 | 0.14 | 0.14 | 0.14 |
| Because of my appearance, I avoid close physical contact, hugging, kissing, or sex | 0.73 | 0.20 | 0.05 | 0.15 | 0.27 | 0.12 |
| Because of my appearance, I avoid physical activities such as exercise, or outdoor recreation | 0.70 | 0.02 | 0.14 | 0.14 | 0.14 | 0.07 |
| Appearance Dissatisfaction | ||||||
| I am dissatisfied with my appearance defect | 0.07 | 0.74 | 0.29 | 0.15 | 0.11 | 0.15 |
| I believe that I have defect in my appearance | 0.03 | 0.73 | 0.14 | 0.13 | 0.07 | 0.10 |
| I am dissatisfied with my overall appearance | 0.18 | 0.61 | 0.15 | 0.32 | 0.07 | 0.16 |
| I have complained about other defects of my body, such as parasitic infection or body odor | 0.10 | 0.43 | 0.17 | 0.10 | 0.19 | 0.06 |
| Preoccupation with Reassurance | ||||||
| I am often upset when concentrating on my appearance | 0.19 | 0.30 | 0.57 | 0.18 | 0.07 | 0.33 |
| I often ask others repeatedly how they feel about my appearance for comfort | 0.20 | 0.15 | 0.52 | 0.05 | 0.08 | 0.18 |
| I often compare my appearance to that of others | 0.03 | 0.32 | 0.48 | 0.12 | 0.15 | 0.19 |
| I have tried various remedies to improve my appearance, such as plastic surgery | 0.25 | 0.11 | 0.47 | 0.16 | 0.05 | −0.10 |
| I often receive comments about my appearance from others | 0.15 | 0.02 | 0.44 | 0.22 | 0.06 | 0.10 |
| I often camouflage my appearance defect with clothes or makeup | 0.14 | 0.25 | 0.42 | 0.05 | 0.18 | 0.12 |
| Perceived Distress/Discrimination | ||||||
| I feel distressed when others comment on my appearance | 0.22 | 0.25 | 0.26 | 0.59 | 0.21 | 0.13 |
| I often feel being treated differently because of my appearance | 0.19 | 0.20 | 0.22 | 0.52 | 0.15 | 0.07 |
| I feel distressed when being treated differently because of my appearance | 0.08 | 0.29 | 0.07 | 0.45 | 0.26 | 0.11 |
| I feel distressed when others are scrutinizing my appearance defect | 0.11 | 0.34 | 0.30 | 0.40 | 0.33 | 0.25 |
| Defect Hiding | ||||||
| When I have physical contact with others, I change my movements or body posture to hide the defect, such as avoiding some parts being touched by others | 0.26 | 0.10 | 0.22 | 0.14 | 0.68 | 0.11 |
| I avoid physical contact with others | 0.25 | 0.10 | −0.04 | 0.16 | 0.62 | 0.06 |
| I often cover up my appearance defect with unnatural posture such as putting my hands in pocket | 0.27 | 0.19 | 0.34 | 0.13 | 0.46 | 0.24 |
| I avoid being looked at by others when I am unclothed | 0.01 | 0.10 | 0.08 | 0.05 | 0.46 | 0.11 |
| Embarrassment in Public | ||||||
| I feel uneasy or embarrassed in public situations such as city streets or restaurants where I concentrate on my appearance | 0.19 | 0.22 | 0.27 | 0.11 | 0.18 | 0.80 |
| I feel uneasy or embarrassed at work or in social situations where I concentrate on my appearance | 0.16 | 0.18 | 0.27 | 0.19 | 0.21 | 0.76 |
Note: Items with target loading >0.40 and cross-loading <0.35 were shown.
Table 3.
The Body Image Concern Scale factor scores (mean ± SD) in two gender groups, and their internal reliabilities and intercorrelations in all participants
| Social Avoidance | Appearance Dissatisfaction | Preoccupation with Reassurance | Perceived Distress/Discrimination | Defect Hiding | Embarrassment in Public | |
|---|---|---|---|---|---|---|
| Score | ||||||
| Women (n=365) | 5.74±2.74 | 1.85±3.94 | 12.05±4.37 | 8.71±3.70 | 9.21±3.78 | 5.18±2.33 |
| Men (n=328) | 6.00±2.89 | 9.68±3.67* | 10.60±3.66* | 8.30±3.32 | 8.46±3.53* | 4.92±2.18 |
| Internal alpha (n=693) | 0.90 | 0.79 | 0.75 | 0.78 | 0.71 | 0.92 |
| Intercorrelation (n=693) | ||||||
| Social Avoidance | 0.32** | 0.41** | 0.45** | 0.45** | 0.38** | |
| Appearance Dissatisfaction | 0.53** | 0.56** | 0.36** | 0.45** | ||
| Preoccupation with Reassurance | 0.55** | 0.43** | 0.53** | |||
| Perceived Distress/Discrimination | 0.48** | 0.47** | ||||
| Defect Hiding | 0.44** | |||||
Notes:
P<0.05 vs women;
Significant correlation at P<0.01.
Moreover, MANOVA had found a significant gender difference on factor scores (Wilks’ λ=0.934, F [6, 686] =8.04, P<0.001). Specifically, women scored significantly higher on Appearance Dissatisfaction (F [1, 691] =16.41, P<0.001, mean square effect [MSE] =238.60), Preoccupation with Reassurance (F [1, 691] =22.12, P<0.001, MSE =362.57), and Defect Hiding (F [1, 691] =7.32, P=0.007, MSE =98.12) than men did (Table 3).
Discussion
Using both exploratory and confirmatory factor analyses on the 34-item matrix regarding the body image concerns, we have developed a structure-validated self-report, the 24-item Body Image Concern Scale in Chinese university students. The disclosure of six factors namely Social Avoidance, Appearance Dissatisfaction, Preoccupation with Reassurance, Perceived Distress/Discrimination, Defect Hiding, and Embarrassment in Public has partly confirmed our first hypothesis. Being distinct from each other, the six factors composed a satisfactory model, and some of them displayed a female preponderance. Each factor had a satisfactory internal reliability, and was intercorrelated with other factors in a medium level. In this case, our second hypothesis has been confirmed.
Factor 1, Social Avoidance, covered the avoidance of social situations or activities in public and the avoidance of physical contacts with others. This aspect was presented before in the Body Dysmorphic Disorder Questionnaire, the Body Dysmorphic Disorder Examination, the modified Yale-Brown Obsessive-Compulsive Scale, and the Body Dysmorphic Symptom Scale.11,13,14,16 This factor corresponds to the clinical features of body dysmorphic disorder, for instance, the appearance preoccupation causes significant secondary social anxiety and avoidance,21 and some aspects of the social anxiety contribute to the functional impairment of the disorder in return.4
Factor 2, Appearance Dissatisfaction, covered the negative evaluation of appearance, which corresponds to the core feature of body dysmorphic disorder.1 The aspect was also considered in other similar measures such as the Body Dysmorphic Disorder Questionnaire, the Body Dysmorphic Disorder Examination, the modified Yale-Brown Obsessive-Compulsive Scale, and the Body Dysmorphic Symptom Scale.11,13,14,16 Patients with body dysmorphic disorder tended to overfocus on the negative appearance attributes.22 The preoccupation with dissatisfaction also triggered the explicit symptoms of the body dysmorphic disorder, eg, the significant distress or impairment in important areas of daily functioning.23 Normally, women pay more attention to their appearance than men do,24 and the physical beauty is a central component of female concerns.25 Our female participants scored higher on Appearance Dissatisfaction, which was in line with these notions.
Factor 3, Preoccupation with Reassurance, covered the excessive self-evaluation of appearance, which led to the frequently physical camouflaging, body checking, and reassurance seeking from others. The factor corresponds well to the repetitive behaviors and mental acts in clinics1 and in previous report.26 On the other hand, patients with body dysmorphic disorder selectively attend to their appearance flaws and mostly ignore the rest of their body,27 which is similar to those patients with obsessive-compulsive disorder.28,29 Women scored higher on this factor, which was also consistent with the previous report8 where women performed more increased mirror-checking and cloth-changing behaviors than men did.
Factor 4, Perceived Distress/Discrimination, covered the preoccupation with negative appearance evaluation from others and the perceived discrimination from others leading to distress. This factor was described in previous measurements of the body dysmorphic disorder.14,16 In clinics, however, some patients with body dysmorphic disorder present ideas or delusions of reference.1 To relieve distress, patients tended to accept plastic surgery for both social and personal reasons.30 The factor also helps to understand the comorbidity between body dysmorphic disorder and social anxiety disorder.31
Factor 5, Defect Hiding, covered avoidance of physical contacts with others and camouflaging appearance with body posture, which corresponds to the clinical description of body dysmorphic disorder,1 and these patients frequently show rituals to correct, fix, or hide body parts.14–16,26 The higher score in women was in accordance with the previous investigation that women more often altered their body position to hide their perceived defect.8
Factor 6, Embarrassment in Public, covered self-consciousness, embarrassment, and feeling of being scrutinized in public or social situations, which also corresponds to the clinical manifestation of body dysmorphic disorder.1 Previous measurements of this kind, such as the Body Dysmorphic Disorder Examination and the Body Dysmorphic Symptom Scale, have described the embarrassment due to appearance defect.14,16 In addition, these patients presented feelings of inferiority,32 which corresponds with shame being a defensive response to threats and social attractiveness losses.33
One should also bear in mind the limitations of the current study design. First, our participants were young university students; thus, results obtained in this age group might not be generalized to a broader age population. Second, our results were based on the healthy participants, and whether they would be valid in psychiatric conditions such as the obsessive-compulsive disorder and eating disorder remains to be seen. Third, personality traits might influence the body imaging report, but that merits further investigation. Future studies might be designed to address the validation of the scale, such as sensitivity, discriminant validity, and test–retest reliability, and convergent validity with other instruments assessing body dysmorphic disorder symptoms. Nevertheless, the questionnaire we developed was a structure-validated one, which might help a precise description of body dysmorphic disorder and related problems in clinics. The earlier detection would ensure an earlier psychotherapy applying to the disorder; for instance, the cognitive-behavioral therapy has proven to be effective in these patients by relieving symptoms and improving self-esteem and quality of life.34
Acknowledgments
The study was supported by grants from the Natural Science Foundation of China (No 81571336) to the corresponding author (Dr W Wang). WH, QMZ, and YJ had contributed equally to the current study.
Footnotes
Disclosure
All authors report no conflicts of interest in this work.
References
- 1.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5®) Arlington: American Psychiatric Pub; 2013. [Google Scholar]
- 2.Veale D, Gledhill LJ, Christodoulou P, Hodsoll J. Body dysmorphic disorder in different settings: A systematic review and estimated weighted prevalence. Body Image. 2016;18:168–186. doi: 10.1016/j.bodyim.2016.07.003. [DOI] [PubMed] [Google Scholar]
- 3.Fang A, Hofmann SG. Relationship between social anxiety disorder and body dysmorphic disorder. Clin Psychol Rev. 2010;30(8):1040–1048. doi: 10.1016/j.cpr.2010.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kelly MM, Walters C, Phillips KA. Social anxiety and its relationship to functional impairment in body dysmorphic disorder. Behav Ther. 2010;41(2):143–153. doi: 10.1016/j.beth.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 5.Fang A, Asnaani A, Gutner C, Cook C, Wilhelm S, Hofmann SG. Rejection sensitivity mediates the relationship between social anxiety and body dysmorphic concerns. J Anxiety Disord. 2011;25(7):946–949. doi: 10.1016/j.janxdis.2011.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Angelakis I, Gooding PA, Panagioti M. Suicidality in body dysmorphic disorder (BDD): a systematic review with meta-analysis. Clin Psychol Rev. 2016;49:55–66. doi: 10.1016/j.cpr.2016.08.002. [DOI] [PubMed] [Google Scholar]
- 7.Jakubietz M, Jakubietz RJ, Kloss DF, Gruenert JJ. Body dysmorphic disorder: diagnosis and approach. Plast Reconstr Surg. 2007;119(6):1924–1930. doi: 10.1097/01.prs.0000259205.01300.8b. [DOI] [PubMed] [Google Scholar]
- 8.Phillips KA, Menard W, Fay C. Gender similarities and differences in 200 individuals with body dysmorphic disorder. Compr Psychiatry. 2006;47(2):77–87. doi: 10.1016/j.comppsych.2005.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Perugi G, Akiskal HS, Giannotti D, Frare F, Di Vaio S, Cassano GB. Gender-related differences in body dysmorphic disorder (dysmorphophobia) J Nerv Ment Dis. 1997;185(9):578–582. doi: 10.1097/00005053-199709000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Phillips KA, Diaz SF. Gender differences in body dysmorphic disorder. J Nerv Ment Dis. 1997;185(9):570–577. doi: 10.1097/00005053-199709000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Phillips KA. The broken mirror: understanding and treating body dysmorphic disorder. Oxford University Press; USA: 1996. [Google Scholar]
- 12.Littleton HL, Axsom D, Pury CL. Development of the body image concern inventory. Behav Res Ther. 2005;43(2):229–241. doi: 10.1016/j.brat.2003.12.006. [DOI] [PubMed] [Google Scholar]
- 13.Phillips KA, Hollander E, Rasmussen SA, Aronowitz BR. A severity rating scale for body dysmorphic disorder: development, reliability, and validity of a modified version of the Yale-Brown Obsessive Compulsive Scale. Psychopharmacol Bull. 1997;33(1):17–22. [PubMed] [Google Scholar]
- 14.Rosen JC, Reiter J. Development of the body dysmorphic disorder examination. Behav Res Ther. 1996;34(9):755–766. doi: 10.1016/0005-7967(96)00024-1. [DOI] [PubMed] [Google Scholar]
- 15.Oosthuizen P, Lambert T, Castle DJ. Dysmorphic concern: prevalence and associations with clinical variables. Aust NZ J Psychiatry. 1998;32(1):129–132. doi: 10.3109/00048679809062719. [DOI] [PubMed] [Google Scholar]
- 16.Kaymak Y, Taner E, Şimşek I. Body dysmorphic disorder in university students with skin diseases compared with healthy controls. Acta Derm Venereol. 2009;89(3):281–284. doi: 10.2340/00015555-0638. [DOI] [PubMed] [Google Scholar]
- 17.Mancuso SG, Knoesen NP, Castle DJ. The dysmorphic concern questionnaire: a screening measure for body dysmorphic disorder. Aust NZ J Psychiatry. 2010;44(6):535–542. doi: 10.3109/00048671003596055. [DOI] [PubMed] [Google Scholar]
- 18.Picavet V, Gabriëls L, Jorissen M, Hellings PW. Screening tools for body dysmorphic disorder in a cosmetic surgery setting. Laryngoscope. 2011;121(12):2535–2541. doi: 10.1002/lary.21728. [DOI] [PubMed] [Google Scholar]
- 19.Schermelleh-Engel K, Moosbrugger H, Müller H. Evaluating the fit of structural equation models: Tests of significance and descriptive goodness-of-fit measures. Methods of psychological research online. 2003;8(2):23–74. [Google Scholar]
- 20.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. [Google Scholar]
- 21.Pinto A, Phillips KA. Social anxiety in body dysmorphic disorder. Body Image. 2005;2(4):401–405. doi: 10.1016/j.bodyim.2005.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Greenberg JL, Reuman L, Hartmann AS, Kasarskis I, Wilhelm S. Visual hot spots: An eye tracking study of attention bias in body dysmorphic disorder. J Psychiatric Res. 2014;57:125–132. doi: 10.1016/j.jpsychires.2014.06.015. [DOI] [PubMed] [Google Scholar]
- 23.Buhlmann U, Etcoff NL, Wilhelm S. Facial attractiveness ratings and perfectionism in body dysmorphic disorder and obsessive-compulsive disorder. J Anxiety Disord. 2008;22(3):540–547. doi: 10.1016/j.janxdis.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 24.Bergner M, Remer P, Whetsell C. Transforming women’s body image: a feminist counseling approach. Women Ther. 1985;4(3):25–38. [Google Scholar]
- 25.Striegel-Moore RH, Franko DL. Body image issues among girls and women. In: Cash TF, Pruzinsky T, editors. Body image: A handbook of theory, research, and clinical practice. New York: Guilford; 2002. pp. 183–191. [Google Scholar]
- 26.Fang A, Wilhelm S. Clinical features, cognitive biases, and treatment of body dysmorphic disorder. Annu Rev Clin Psycho. 2015;11:187–212. doi: 10.1146/annurev-clinpsy-032814-112849. [DOI] [PubMed] [Google Scholar]
- 27.Deckersbach T, Savage CR, Phillips KA, et al. Characteristics of memory dysfunction in body dysmorphic disorder. J Intern Neuropsychol Soc. 2000;6(06):673–681. doi: 10.1017/s1355617700666055. [DOI] [PubMed] [Google Scholar]
- 28.Rachman S. A cognitive theory of obsessions. Behav Res Ther. 1997;35(9):793–802. doi: 10.1016/s0005-7967(97)00040-5. [DOI] [PubMed] [Google Scholar]
- 29.Savage CR, Baer L, Keuthen NJ, Brown HD, Rauch SL, Jenike MA. Organizational strategies mediate nonverbal memory impairment in obsessive–compulsive disorder. Biol Psychiatry. 1999;45(7):905–916. doi: 10.1016/s0006-3223(98)00278-9. [DOI] [PubMed] [Google Scholar]
- 30.Park LE, Calogero RM, Young AF, Diraddo AM. Appearance-based rejection sensitivity predicts body dysmorphic disorder symptoms and cosmetic surgery acceptance. J Soc Clin Psychol. 2010;29(5):489–509. [Google Scholar]
- 31.Buhlmann U, McNally RJ, Wilhelm S, Florin I. Selective processing of emotional information in body dysmorphic disorder. J Anxiety Disord. 2002;16(3):289–298. doi: 10.1016/s0887-6185(02)00100-7. [DOI] [PubMed] [Google Scholar]
- 32.Veale D, Riley S. Mirror, mirror on the wall, who is the ugliest of them all? The psychopathology of mirror gazing in body dysmorphic disorder. Behav Res Ther. 2001;39(12):1381–1393. doi: 10.1016/s0005-7967(00)00102-9. [DOI] [PubMed] [Google Scholar]
- 33.Gilbert P, Miles J. Body shame: Conceptualisation, research and treatment. New York, NY: Brunner–Routledge; 2014. pp. 267–282. [Google Scholar]
- 34.Greenberg JL, Markowitz S, Petronko MR, Taylor CE, Wilhelm S, Wilson GT. Cognitive-behavioral therapy for adolescent body dysmorphic disorder. Cogn Behav Pract. 2010;17(3):248–258. [Google Scholar]