Abstract
Public reporting and payment programs in the United States have embraced thirty-day readmissions as an indicator of between-hospital variation in the quality of care, despite limited evidence supporting this interval. We examined risk-standardized thirty-day risk of unplanned inpatient readmission at the hospital level for Medicare patients ages sixty-five and older in four states and for three conditions: acute myocardial infarction, heart failure, and pneumonia. The hospital-level quality signal captured in readmission risk was highest on the first day after discharge and declined rapidly until it reached a nadir at seven days, as indicated by a decreasing intracluster correlation coefficient. Similar patterns were seen across states and diagnoses. The rapid decay in the quality signal suggests that most readmissions after the seventh day postdischarge were explained by community- and household-level factors beyond hospitals’ control. Shorter intervals of seven or fewer days might improve the accuracy and equity of readmissions as a measure of hospital quality for public accountability.
Reducing the number of preventable hospital readmissions has become a national health policy priority.1 In an effort to achieve this goal, the Affordable Care Act authorized the Centers for Medicare and Medicaid Services (CMS) to penalize acute care hospitals for excessive unplanned readmissions. Through this authority, CMS created the Hospital Readmission Reduction Program (HRRP) and developed methods to measure and publicly report the hospital-wide all-cause, unplanned readmission rates occurring within thirty days of discharge for each hospital.2 The National Quality Forum has endorsed all of these measures and several other readmission measures for adults, focusing on acute myocardial infarction,3 heart failure,4 pneumonia,5 chronic obstructive pulmonary disease,6 hospital-wide readmission,7 vascular procedures,8 cardiac stent interventions,9 coronary bypass graft surgery,10 and total hip and knee replacement.11 The use of all-cause, unplanned readmission measures12 for quality measurement is being extended to accountable care organizations.13
The CMS condition-specific technical reports state: “Outcomes occurring within 30 days…can be influenced by hospital care and the early transition to the outpatient setting.”14,15 The HRRP was built on this premise that hospitals’ scope of responsibility should include postdischarge care coordination, although essentially no empirical evidence supports the use of a thirty-day readmission interval for assessing hospital-modifiable quality in all settings and clinical domains.16,17 Despite substantial economic impact on facilities, and potential impact on the care that patients receive, it is not clear whether hospitals can practicably affect care for such a long period after discharge. For this reason, many researchers remain skeptical about the use of a thirty-day readmission interval for all conditions and procedures.18,19
Hierarchical models provide a statistical method to account for patient characteristics and to separate the readmission risk component associated with hospitals from the readmission risk associated with nonhospital sources.20 The conventional parameter to quantify this relationship is the intracluster correlation coefficient (ICC), which represents the proportion of risk explained by hospitals (between-hospital variation) compared to the total risk in the population (all variation).21 If readmissions are heavily influenced by hospital practices (for example, inpatient care, discharge planning, or care coordination), then between-hospital variation should be large compared to total variation, and the ICC should be relatively large. Conversely, if patient or household characteristics (for example, educational attainment, access to primary care, family support, or community resources) are dominant drivers of readmission risk, then the ICC should be relatively small. For example, the team that developed CMS’s methods for analyzing both thirty-day mortality and readmissions reported hospital ICCs of 4.8–5.3 percent for mortality measures and 1.5–2.6 percent for readmission measures.22
Given this conceptual framework, we calculated the ICC across a range of postdischarge time intervals and conditions, while adjusting for the contribution of patient-level clinical risk factors. This analytic approach allowed us to measure how hospital-level variation in readmission risk changes over time after discharge, independent of patient characteristics. We hypothesized that hospital-level variation would rapidly decrease within ten days after discharge in a diverse population of older adults and that this decrease would occur more quickly after medical admissions than after surgical admissions, as a result of late postoperative blood clots and infections that might reflect the quality of inpatient care.
Study Data And Methods
DATA SOURCES
Using the State Inpatient Databases and State Emergency Department Databases from the Healthcare Cost and Utilization Project,16 we constructed an all-payer data set from Arizona (2005–07), California (2005–11), Florida (2005–12), and New York (2006–11).We selected these states and years because they offered large, diverse populations that accommodated longitudinal patient-level analysis and their data were relatively inexpensive to purchase. The University of California, Davis, Institutional Review Board approved the study protocol.
POPULATION
Patients discharged from any nonfederal hospital in Arizona, California, Florida, and New York during the study years were eligible for inclusion. We adapted source code developed by the Yale School of Medicine’s Center for Outcomes Research and Evaluation (CORE) for measuring risk-standardized readmission rates,3–5,7 as defined by the inpatient prospective payment system Final Rule,1 to create three encounter-based cohorts: acute myocardial infarction, heart failure, and pneumonia. Hospital encounters in these cohorts were mutually exclusive, but individual patients might cross between cohorts. Similarly, we applied CORE criteria from the hospital-wide all-cause, unplanned readmission measure to create five mutually exclusive cohorts: medicine, surgery and gynecology, cardiorespiratory, cardiovascular, and neurology.23 All encounters in the three risk-standardized readmission rate cohorts were also selected for one of the five hospital-wide all-cause, unplanned readmission cohorts.
Following CMS and CORE specifications, a hospital encounter was eligible for inclusion if the patient was discharged alive at age sixty-five or older. We excluded encounters that occurred in psychiatric, rehabilitation, long-term care, or prospective payment system–exempt cancer hospitals. Patients discharged against medical advice; patients transferred to another acute care facility; and patients admitted for a primary psychiatric diagnosis, rehabilitation, or medical treatment of cancer were also excluded. Additional methodological details are provided in on-line Appendix 1a.24
OUTCOMES
We adapted the CORE source code to determine whether a patient experienced an unplanned readmission for all risk-standardized readmission rate and hospital-wide all-cause, unplanned readmission cohorts; we repeated this determination each day, from one to ninety days after the index discharge. This range was chosen not only to contain the entire thirty-day interval used in CMS measures but also to capture later readmissions that might or might not be related to care during the prior hospitalization.25,26
STATISTICAL ANALYSIS
We calculated summary statistics for the demographic and clinical characteristics of hospital encounters in the acute myocardial infarction, heart failure, and pneumonia cohorts and a composite of all hospital-wide all-cause, unplanned readmission cohorts. As described by CMS and CORE, we estimated the base readmission measures separately using hierarchical logistic regression models. The acute myocardial infarction, heart failure, and pneumonia models were adjusted for age, sex, and clinical risk factors (see Appendices 2a, 2b, and 2c for risk-standardized readmission rate risk factor prevalence).24 Each of the hospital-wide all-cause, unplanned readmission models— medicine, surgery and gynecology, cardiorespiratory, cardiovascular, and neurology—was adjusted for age, clinical risk factors (see Appendix 2d for hospital-wide all-cause, unplanned readmission risk factor prevalence),24 and principal diagnosis.7 For each postdischarge interval, from one day to ninety days, we fitted a separate model and estimated the ICC, which represents the proportion of variation in readmission risk associated with the hospital, compared to variation associated with all other factors.27–29 Additional statistical details are reported in Appendix 1b.24
We evaluated the consistency of our findings across states for the risk-standardized readmission rate cohorts and performed a stratified analysis to calculate the ICC for seven- and thirty-day readmissions. We also determined how much a hospital’s performance changed between day seven and day thirty (measured by risk-standardized readmission rate percentile), to determine whether some hospitals appear to affect readmission over longer intervals.
ROBUSTNESS ANALYSES INCLUDING GEODEMOGRAPHIC FACTORS
To explore the robustness of our primary findings, we extended the base models to include additional factors that might affect readmission risk but are outside the hospital’s influence and not directly related to clinical care processes. These factors included fixed effects for hospital location (state), patient-level rural–urban continuum category,30 and median household income quartile for patient ZIP code.31 We fitted a geodemographic-extended model for each cohort, adjusted for these additional covariates, and then compared the ICCs from these models to the ICCs from our base models, at each interval from one to ninety days.
To evaluate the impact of hospital discharge practices (for example, short length-of-stay), we calculated the correlation (weighted by hospital volume) between median length of stay and the risk of readmission at intervals from one to ten days. Finally, to verify data validity, we used “admission source” and “point of origin” variables to assess the percentage of readmissions in our analysis that the receiving hospital reported as incoming transfers, stratified by the length of the time-to-readmission interval.
LIMITATIONS
Several limitations should be noted. Although our study population included four demographically and geographically diverse states, these states might not be representative of the United States, and most of our data predate implementation of the HRRP. Identifiers used to link unique patients across multiple encounters are state-specific; therefore, out-of-state readmissions could not be detected, potentially leading to underestimation of readmission rates. We used all-payer data to capture both fee-for-service and managed care enrollees in Medicare, given that Medicare Advantage plans have more than 35 percent of the market in these four states.32 Our findings should be confirmed using Medicare fee-for-service data and post-HRRP all-payer claims data sets.
We employed the ICC as a measure of the hospital quality signal, in accord with recommendations from the Committee of Presidents of Statistical Societies.21 Although this measure has been used in similar research,22,27,29 hospital quality is a complicated construct that might not be fully captured by any single metric. For example, low ICCs could indicate that all hospitals have similarly excellent (or poor) quality, or that all patients have similar risk of readmission (at any hospital), although the latter interpretation is less plausible.
Study Results
HOSPITAL AND PATIENT CHARACTERISTICS
Of the 66,741,340 hospital discharge records available, our study sample included 15,212,575 index hospitalizations for 6,768,057 unique patients at 910 hospitals. Considering all hospital-wide all-cause, unplanned readmission measures, the median number of encounters per hospital was 10,942 (interquartile range: 2,904 to 24,796). Patients’ median age was seventy-eight (IQR: 71–84), 56.5 percent were female, 71.7 percent were white, and 89.7 percent had Medicare as the primary expected payer (Exhibit 1) (see Appendix 3 for additional descriptive statistics).24
EXHIBIT 1.
Characteristics of hospital encounters among acute myocardial infarction, heart failure, pneumonia, and combined hospital-wide readmission cohorts
| Characteristic | Acute myocardial infarction | Heart failure | Pneumonia | Hospital-wide readmission |
|---|---|---|---|---|
| No. of patient encounters | 363,534 | 900,632 | 648,371 | 15,212,575 |
|
| ||||
| No. of hospitals | 558 | 750 | 784 | 910 |
|
| ||||
| Mean agea (years) | 78.2 | 80.2 | 79.8 | 78.0 |
|
| ||||
| Female | 47.2% | 53.4% | 53.5% | 56.5% |
|
| ||||
| Race or ethnicityb | ||||
| White | 73.3% | 68.4% | 72.8% | 71.7% |
| Hispanic | 11.7 | 13.2 | 12.4 | 12.1 |
| Black | 6.3 | 11.0 | 6.3 | 8.3 |
| Otherc | 8.7 | 7.4 | 8.4 | 7.9 |
|
| ||||
| Mean no. of comorbiditiesd | 2.8 | 3.3 | 1.9 | 1.8 |
|
| ||||
| Statee | ||||
| Arizona | 2.3% | 1.8% | 2.5% | 2.3% |
| California | 35.4 | 35.7 | 41.6 | 36.4 |
| Florida | 42.0 | 39.5 | 34.2 | 39.2 |
| New York | 20.3 | 23.0 | 21.7 | 22.2 |
|
| ||||
| Hospital typeb | ||||
| Nonprofit | 75.2% | 74.9% | 76.5% | 79.8% |
| Investor-owned | 18.7 | 19.6 | 18.4 | 18.1 |
| Missing | 6.1 | 5.5 | 5.1 | 2.1 |
SOURCE Authors’ analysis of data from the Healthcare Cost and Utilization Project, State Inpatient Database, and State Emergency Department Database: Arizona (2005–07); California (2005–11); Florida (2005–12); and New York (2006–11).
Standard deviation for age was 8.2 for acute myocardial infarction, 8.1 for heart failure, 8.1 for pneumonia, and 8.0 for hospital-wide all-cause unplanned readmission.
Not included in the geodemographic-extended models.
Includes Asian or Pacific Islander, Native American, other race, and missing.
Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27.
Models adjusted for ZIP code did not converge.
READMISSION MEASURES
Unplanned readmissions accounted for 90.1 percent of all-cause readmissions. The observed thirty-day unplanned readmission rate was 17.5 percent for acute myocardial infarction, 23.6 percent for heart failure, 17.6 percent for pneumonia, and 15.5 percent for hospital-wide all-cause, unplanned readmissions. Among subcategories of the latter, observed thirty-day unplanned readmission rates were 17.1 percent for medicine, 11.3 percent for surgery and gynecology, 20.6 percent for cardiorespiratory, 12.5 percent for cardiovascular, and 13.7 percent for neurology.
Patients who resided in ZIP codes in the lowest household income quartile had higher thirty-day readmission risk (odds ratio: 1.1 relative to the highest household income quartile; p < 0:001) in all cohorts (see Appendix 4 for geodemographic risk estimates).24 Similarly, patients residing in the smallest rural communities, compared to the largest urban communities, experienced at least 41 percent greater thirty-day readmission risk (for example, pneumonia odds ratio: 1.41; p = 0.01). State-level ICCs for California, Florida, and New York were similar to that of the multistate population, but Arizona’s ICCs were consistently larger in all cohorts (see Appendices 5, 6a, 6b, and 6c for state-level comparisons).24 Mean hospital volume was consistently lowest in Arizona and highest in New York.
BETWEEN-HOSPITAL VARIATION
The ICC for all three specific medical conditions dropped rapidly from 2.7 percent (acute myocardial infarction), 1.6 percent (heart failure), and 3.2 percent (pneumonia) on the first day after discharge, to less than 1.0 percent (all three cohorts) by day four, reaching a minimum of 0.8 percent or less at seven days after discharge (Exhibit 2). Across all of these measures, most of the hospital quality signal dissipated by the seventh day after discharge—for example, the ICC decreased between the first day and the seventh day by 78 percent, 49 percent, and 76 percent among patients admitted with acute myocardial infarction, heart failure, and pneumonia, respectively. Hospital-level variation in models with geodemographic adjustments followed the same trend but was lower than that in the base models (Exhibit 3; see Appendix 7 for hospital-wide all-cause, unplanned readmission models).24
EXHIBIT 2. Intracluster correlation coefficient estimates at specific readmission intervals from one to ten days, for acute myocardial infarction, heart failure, and pneumonia.
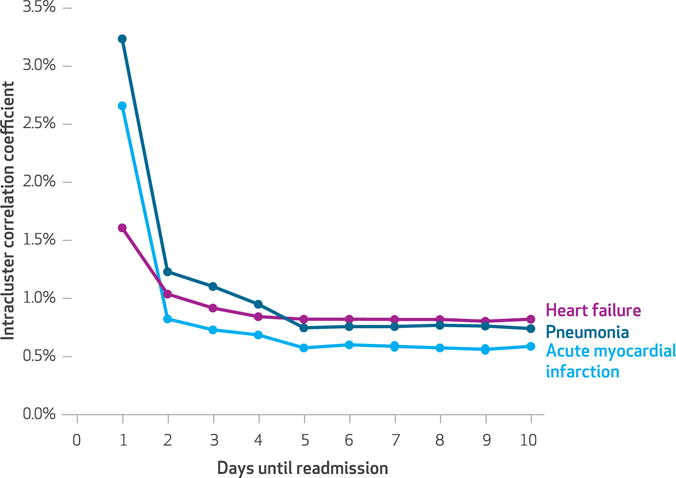
SOURCE Authors’ analysis of data from the Healthcare Cost and Utilization Project, State Inpatient Database, and State Emergency Department Database: Arizona (2005–07); California (2005–11); Florida (2005–12); and New York (2006–11).
NOTE Data represent unadjusted base models by cohort.
EXHIBIT 3. Intracluster correlation coefficient estimates at specific readmission intervals from one to ninety days for acute myocardial infarction, heart failure, and pneumonia.
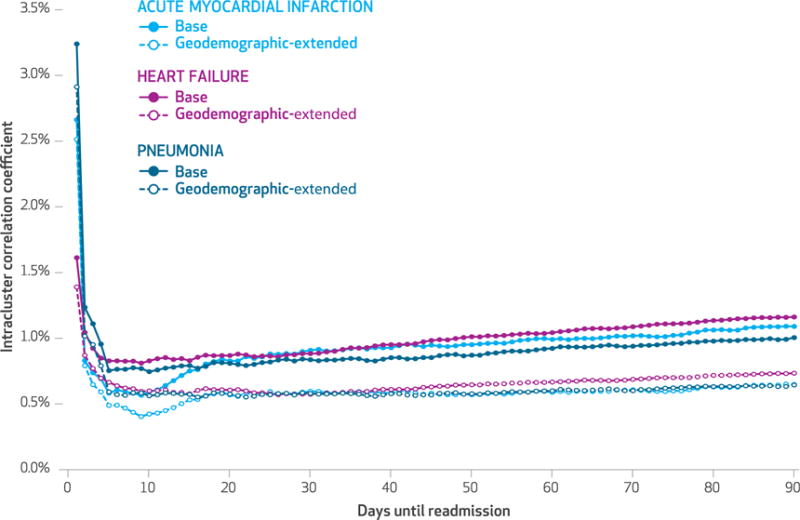
SOURCE Authors’ analysis of data from the Healthcare Cost and Utilization Project, State Inpatient Database, and State Emergency Department Database: Arizona (2005–07); California (2005–11); Florida (2005–12); and New York (2006–11).
NOTE Base and geodemographic-extended models by cohort; see text for explanation.
After the tenth day, hospital-level variation rose slightly but steadily in the base models for risk-standardized and hospital-wide readmissions to 0.84–1.10 percent at the thirtieth day and 1.01–1.23 percent at the ninetieth day after discharge (mean ICC difference between day ninety and day ten: 0.38 percent; 95% confidence interval: 0.30, 0.45). However, hospital-level variation did not rise, or rose only minimally, between the tenth and ninetieth days in the eight models extended to include geodemographic covariates (mean ICC difference between day ninety and day ten: 0.16 percent; 95% CI: 0.11, 0.20). The acute myocardial infarction cohort differed from other cohorts, with an earlier rise in hospital-level variation between the tenth and twentieth postdischarge days (Exhibit 3; see Appendix 7 for hospital-wide all-cause, unplanned readmission models).24 Among state-stratified analyses, readmissions within seven days were too rare to determine the hospital-level variation. When we compared seven-versus thirty-day readmissions, the median hospital rank change was 11.4–11.8 percent (see Appendices 8a, 8b, and 8c for ranked differences).24
ROBUSTNESS ANALYSIS
A weak correlation between the hospital-level median length of stay and readmission rate was found on the first post-discharge day in the cardiovascular cohort (r = −0.08; p = 0:026); this relationship was not significant in other cohorts (see Appendix 9 for hospital-level readmission rates versus length-of-stay).24 Among readmissions in our analysis, only 2.2–2.6 percent were reported by the receiving/admitting hospital as incoming transfers (see Appendix 10 for validation of discharge disposition),24 which suggests that this problem was rare and cannot account for observed ICC changes over time.
Discussion
Readmission rates were first introduced in 1953 to characterize risk among neuropsychiatric patients discharged from Department of Veterans Affairs (VA) hospitals33 but gained prominence in 2010 with CMS’s adoption for use in the Hospital Risk Reduction Program.2 Previous studies have reported the percentage of patients readmitted within various intervals,34 but these studies did not address the untested assumption that thirty days is the optimal interval for ascertaining hospital-level (that is, between-hospital) variation.35 To understand whether shorter or longer intervals would better identify the hospital quality signal, we implemented the hierarchical models developed by CMS3–5,7 across three reported patient cohorts and ascertainment intervals from one day to ninety days.
PRIMARY FINDINGS
Our analysis revealed four primary findings: First, hospital-level variation was low at the conventional thirty-day cutoff for all patient cohorts, ranging from 1.1 percent for surgery to 0.8 percent for pneumonia. Second, hospital-level variation was consistently and substantially higher within the first several days after discharge (with values as high as 3.2 percent for the pneumonia cohort on the first postdischarge day), reaching a nadir around seven days. Taken together, these findings suggest that a five-to-seven-day ascertainment interval would better capture hospital-attributable readmissions, particularly when compared to intervals of thirty, sixty, or ninety days.26
Third, the optimal interval for capturing hospital-level variation in the risk of readmission appears to vary across conditions. For example, the acute myocardial infarction cohort (in which 47 percent of patients had at least one major procedure) manifested the greatest increase in hospital-level variation after the tenth post-discharge day.
Fourth, CMS’s current risk-standardized readmission models (which adjust only for patient age, sex, and clinical characteristics) unexpectedly showed increasing hospital ICCs with longer ascertainment periods, from seven to ninety days. However, this effect largely disappeared after adjustment for geodemographic effects outside the hospital’s control (state, rural-urban designation, and median household income). This suggests that much of the presumed hospital quality signal at thirty days and beyond could be attributable to characteristics of the communities within which hospitals are situated.
CONTEXT AND COMPARABILITY
We used all-payer linked claims data, but our estimates of thirty-day readmission rates were consistent with estimates based on Medicare fee-for-service claims data (17 percent for acute myocardial infarction, 24 percent for heart failure, 17 percent for pneumonia, and 16 percent for hospital-wide all-cause, unplanned readmission).2,22,23,26 Similarly, our estimates of hospital-level variation were consistent with prior work on thirty-day readmissions (ICC for acute myocardial infarction, 1.5 percent; ICC for heart failure, 2.6 percent)22 and comparable to readmission models previously described for coronary artery bypass graft surgery.27 In contrast, studies of risk-adjusted mortality have generally reported hospital-level variation in the range of 4–6 percent,22 and as high as 10.1 percent for hospitals performing coronary artery bypass grafting in Italy.36 One notable exception (ICC = 0.6 percent) was a study limited to mechanically ventilated patients at VA hospitals.37 Hospital-level variation for process measures such as blood transfusions38 and use of critical care39 has been estimated as high as 30 percent.40
Consistent with findings from our geodemographic-extended models, two recent studies found patient and community characteristics affected readmission risk,41,42 and readmission rates differed when safety-net hospitals were compared to other hospitals.43 Other investigators27,42,44 have reported that facility-level variation is markedly decreased by adjusting for additional clinical and social characteristics of patients. One group sought to determine the best interval for using intensive care unit (ICU) readmission as a quality indicator, hypothesizing that variables measuring ICU circumstances (for example, percent of beds occupied) would become less strongly associated with readmission risk at longer intervals, while variables representing chronic diseases would become more strongly associated with readmission risk.44 Their analyses also supported a relatively short interval of two calendar days.
Implications
Our finding that the hospital quality signal is higher in the first five days after discharge than at longer time periods, such as thirty days, suggests that hospitals’ practices with respect to care coordination and postdischarge follow-up could have the greatest impact within the first few days after discharge. This finding is consistent with previous observations that “stability at discharge” is a key predictor of early readmissions after medical hospitalizations45 and that early postdischarge follow-up appointments might be associated with lower readmission risk.46
Patients with acute myocardial infarction were the most likely to have had major surgical procedures during their index encounters, when compared to our heart failure and pneumonia cohorts. Therefore, the unique increase in ICC in this cohort beginning at ten days after discharge (Exhibit 3) might reflect postoperative complications following major surgery, as reported previously.47 These findings suggest that the optimal readmission interval in which to measure the strongest hospital quality signal could be related to the cohort’s clinical attributes, although additional analysis is needed to better understand this relationship.
Readmissions occurring after seven days appear to be more susceptible to geodemographic characteristics that reflect the inherent social and community-related factors in the patient’s environment after hospital discharge.48 These findings might, in part, explain why readmission rates appear to have decreased only modestly since the implementation of the HRRP penalty,49–52 and these decreases have been partially offset by increases in rates of observation stay.53 If nonhospital factors have a greater impact on readmissions after seven days, then hospitals may have limited opportunity to prevent these outcomes.
Efforts to improve hospital quality have largely focused on motivating individual facilities to reduce their readmission rates, while little attention has been paid to the role of health care providers outside the hospital setting. Although some authors have examined the association between readmission rates and facility or patient characteristics within postacute care settings,54,55 these efforts have not separated the proportion of risk attributable to multiple facilities. Therefore, the relative proportions of risk attributable to hospitals, postacute care, or non–health care factors are unknown, and additional efforts are needed to understand how different settings and types of care affect readmission rates, after adjustment for patient characteristics.
Extending our view of readmission to include risk contributed by other care providers after hospital discharge could enhance the alignment of quality improvement goals, hospital incentives, and national policy.56 Future research and policy discussions should consider shared attribution of readmissions, especially after five to seven days, among postdischarge care providers such as skilled nursing facilities, dialysis facilities, and primary care providers.
Conclusion
Thirty-day risk-standardized, all-cause, unplanned readmission rates have become widely used to measure hospitals’ performance for public reporting and to impose financial penalties on facilities with excess readmissions,2 despite little evidence that these rates reflect aspects of care that are under hospitals’ direct or indirect control. We found that the hospital quality signal, or hospital-level effect, is strongest within the first seven days after discharge. Factors outside the hospital’s control (community or household characteristics) might have a relatively large effect on readmission risk at longer intervals and reflect the cumulative quality of health care provided to patients.
If the goal of current public policy is to encourage hospitals to assume responsibility for post-discharge adherence and primary care follow-up, then penalties assessed for readmissions within thirty days or longer periods might align appropriately. However, if the goal is empowering patients and families to make health care choices informed by true differences in hospital performance, then a readmission interval of seven days or fewer might be more accurate and equitable.
Supplementary Material
Acknowledgments
An earlier version of this work was presented at the 2015 Agency for Healthcare Research and Quality (AHRQ) Research Conference, Crystal City, Virginia, October 5, 2015. David Chin was supported by Grant No. T32HS022236 from AHRQ through the Quality, Safety, and Comparative Effectiveness Research Training program. Heejung Bang is partially supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant No. UL1 TR000002. The authors thank the Yale Center for Outcomes Research and Evaluation for providing source code for all readmission measures; the Healthcare Cost and Utilization Project (HCUP), AHRQ, Social and Scientific Systems Inc., and Julie Kale for curating and providing the State Inpatient Databases and State Emergency Department Databases; and HCUP partner organizations—California Office of Statewide Health Planning and Development, Arizona Department of Health Services, Florida Agency for Health Care Administration, and New York State Department of Health—for providing these data to HCUP. The authors also thank Regan Scott-Chin for her critical contributions to drafting this manuscript and Gary Tabler for computational support.
Contributor Information
David L. Chin, Postdoctoral scholar at the Center for Healthcare Policy and Research, University of California, Davis, in Sacramento
Heejung Bang, Professor of biostatistics in the Department of Public Health Sciences, University of California, Davis.
Raj N. Manickam, Graduate student researcher in the Graduate Group in Epidemiology, University of California, Davis
Patrick S. Romano, Professor of medicine and pediatrics in the Division of General Medicine at the University of California, Davis, School of Medicine and at the Center for Healthcare Policy and Research
NOTES
- 1.Centers for Medicare and Medicaid Services. Medicare program; hospital inpatient prospective payment systems for acute care hospitals and the long-term care hospital prospective payment system policy changes and fiscal year 2016 rates; revisions of quality reporting requirements for specific providers, including changes related to the Electronic Health Record Incentive Program; extensions of the Medicare-dependent, Small Rural Hospital Program and the low-volume payment adjustment for hospitals. Final rule; interim final rule with comment period. Fed Regist. 2015;80(158):49325–886. [PubMed] [Google Scholar]
- 2.Centers for Medicare and Medicaid Services. Readmissions Reduction Program (HRRP) [Internet] Baltimore (MD): CMS; [cited 2016 Aug 5]. Available from: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html. [Google Scholar]
- 3.National Quality Forum. Hospital 30-day all-cause risk-standardized readmission rate (RSRR) following acute myocardial infarction (AMI) hospitalization [Internet] Washington (DC): NQF; 2014. Dec 22, [cited 2016 Aug 17]. Available (after acceptance of copyright terms) from: http://www.qualityforum.org/QPS/0505. [Google Scholar]
- 4.National Quality Forum. Hospital 30-day, all-cause, risk-standardized readmission rate (RSRR) following heart failure (HF) hospitalization [Internet] Washington (DC): NQF; 2014. Nov 6, [cited 2016 Aug 17]. Available (after acceptance of copyright terms) from: http://www.qualityforum.org/QPS/0330. [Google Scholar]
- 5.National Quality Forum. Hospital 30-day, all-cause, risk-standardized readmission rate (RSRR) following pneumonia hospitalization [Inter-net] Washington (DC): NQF; 2015. Mar 5, [cited 2016 Aug 17]. Available (after acceptance of copyright terms) from: http://www.qualityforum.org/QPS/0506. [Google Scholar]
- 6.National Quality Forum. Hospital 30-day, all-cause, risk-standardized readmission rate (RSRR) following chronic obstructive pulmonary disease (COPD) hospitalization [Internet] Washington (DC): NQF; 2014. Apr 8, [cited 2016 Aug 17]. Available (after acceptance of copyright terms) from: http://www.qualityforum.org/QPS/1891. [Google Scholar]
- 7.National Quality Forum. Hospital-wide all-cause unplanned readmission measure (HWR) [Internet] Washington (DC): NQF; 2014. Nov 6, [cited 2016 Aug 17]. Available (after acceptance of copyright terms) from: http://www.qualityforum.org/QPS/1789. [Google Scholar]
- 8.National Quality Forum. Hospital 30-day all-cause risk-standardized readmission rate (RSRR) following vascular procedures [Internet] Washington (DC): NQF; 2015. Nov 3, [cited 2016 Aug 17]. Available (after acceptance of copyright terms) from: http://www.qualityforum.org/QPS/2513. [Google Scholar]
- 9.National Quality Forum. Hospital 30-day risk-standardized readmission rates following percutaneous coronary intervention (PCI) [Inter-net] Washington (DC): NQF; 2015. Nov 3, [cited 2016 Aug 17]. Available (after acceptance of copyright terms) from: http://www.qualityforum.org/QPS/0695. [Google Scholar]
- 10.National Quality Forum. Hospital 30-day, all-cause, unplanned, risk-standardized readmission rate (RSRR) following coronary artery bypass graft (CABG) surgery [Internet] Washington (DC): NQF; 2015. Nov 3, [cited 2016 Aug 17]. Available (after acceptance of copyright terms) from: http://www.qualityforum.org/QPS/2515. [Google Scholar]
- 11.National Quality Forum. Hospital-level 30-day, all-cause risk-standardized readmission rate (RSRR) following elective primary total hip arthroplasty (THA) and/or total knee arthroplasty (TKA) [Internet] Washington (DC): NQF; 2014. Nov 6, [cited 2016 Aug 17]. Available (after acceptance of copyright terms) from: http://www.qualityforum.org/QPS/1551. [Google Scholar]
- 12.National Quality Forum. All-cause admissions and readmissions measures—final report [Internet] Washington (DC): NQF; 2015. Apr, [cited 2016 Aug 17]. Available from: http://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=79368. [Google Scholar]
- 13.RTI International. Accountable care organization 2016 program quality measure narrative specifications [Internet] Baltimore (MD): Center for Medicare and Medicaid Innovation; 2016. Jan 13, [cited 2016 Aug 5]. Available from: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Downloads/2016-ACO-NarrativeMeasures-Specs.pdf. [Google Scholar]
- 14.Yale New Haven Health Services Corporation/Center for Outcomes Research and Evaluation. 2016 AMI, HF, pneumonia, COPD, and stroke readmission measures updates and specifications report [Internet] Baltimore (MD): Centers for Medicare and Medicaid Services; 2016. Mar, [cited 2016 Aug 25]. Available for download from: http://www.qualitynet.org/dcs/ContentServer?cid=1219069855841&pagename=QnetPublic%2FPage%2FQnetTier4&c=Page. [Google Scholar]
- 15.Yale New Haven Health Services Corporation/Center for Outcomes Research and Evaluation. Hospital-wide readmission measure methodology report [Internet] Baltimore (MD): Centers for Medicare and Medicaid Services; 2016. Mar, [cited 2016 Aug 17]. Available for download from: http://www.qualitynet.org/dcs/ContentServer?cid=1219069855841&pagename=QnetPublic%2FPage%2FQnetTier4&c=Page. [Google Scholar]
- 16.Burgess JF, Hockenberry JM. Can all cause readmission policy improve quality or lower expenditures? A historical perspective on current initiatives. Health Econ Policy Law. 2014;9(2):193–213. doi: 10.1017/S1744133113000340. [DOI] [PubMed] [Google Scholar]
- 17.Leppin AL, Gionfriddo MR, Kessler M, Brito JP, Mair FS, Gallacher K, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med. 2014;174(7):1095–107. doi: 10.1001/jamainternmed.2014.1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Joynt KE, Jha AK. A path forward on Medicare readmissions. N Engl J Med. 2013;368(13):1175–7. doi: 10.1056/NEJMp1300122. [DOI] [PubMed] [Google Scholar]
- 19.Vaduganathan M, Bonow RO, Gheorghiade M. Thirty-day read-missions: the clock is ticking. JAMA. 2013;309(4):345–6. doi: 10.1001/jama.2012.205110. [DOI] [PubMed] [Google Scholar]
- 20.Houchens R, Chu B, Steiner C. Hierarchical modeling using HCUP data [Internet] Rockville (MD): Agency for Healthcare Research and Quality; 2007. Jan 10, [cited 2016 Aug 6]. Available from: http://www.hcup-us.ahrq.gov/reports/methods/2007_01.pdf. [Google Scholar]
- 21.Ash AS, Fienberg SE, Louis TA, Normand S-LT, Stukel TA, Utts J. Statistical issues in assessing hospital performance [Internet] Baltimore (MD): Centers for Medicare and Medicaid Services; 2011. Nov 28, [updated 2012 Jan 27; cited 2016 Aug 5]. Available from: http://cms.hhs.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Downloads/Statistical-Issues-in-Assessing-Hospital-Performance.pdf. [Google Scholar]
- 22.Krumholz HM, Merrill AR, Schone EM, Schreiner GC, Chen J, Bradley EH, et al. Patterns of hospital performance in acute myocardial infarction and heart failure 30-day mortality and readmission. Circ Cardiovasc Qual Outcomes. 2009;2(5):407–13. doi: 10.1161/CIRCOUTCOMES.109.883256. [DOI] [PubMed] [Google Scholar]
- 23.Horwitz LI, Partovian C, Lin Z, Grady JN, Herrin J, Conover M, et al. Development and use of an administrative claims measure for profiling hospital-wide performance on 30-day unplanned readmission. Ann Intern Med. 2014;161(10 Suppl):S66–75. doi: 10.7326/M13-3000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 25.Gore JM, Peterson E, Amin A, Anderson FA, Jr, Dasta JF, Levy PD, et al. Predictors of 90-day readmission among patients with acute severe hypertension. The cross-sectional observational Studying the Treatment of Acute hyperTension (STAT) study. Am Heart J. 2010;160(3):521–7.e1. doi: 10.1016/j.ahj.2010.06.032. [DOI] [PubMed] [Google Scholar]
- 26.Epstein AM, Jha AK, Orav EJ. The relationship between hospital admission rates and rehospitalizations. N Engl J Med. 2011;365(24):2287–95. doi: 10.1056/NEJMsa1101942. [DOI] [PubMed] [Google Scholar]
- 27.Li Z, Armstrong EJ, Parker JP, Danielsen B, Romano PS. Hospital variation in readmission after coronary artery bypass surgery in California. Circ Cardiovasc Qual Outcomes. 2012;5(5):729–37. doi: 10.1161/CIRCOUTCOMES.112.966945. [DOI] [PubMed] [Google Scholar]
- 28.Wynants L, Timmerman D, Bourne T, Van Huffel S, Van Calster B. Screening for data clustering in multicenter studies: the residual intraclass correlation. BMC Med Res Methodol. 2013;13:128. doi: 10.1186/1471-2288-13-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tangri N, Tighiouart H, Meyer KB, Miskulin DC. Both patient and facility contribute to achieving the Centers for Medicare and Medicaid Services’ pay-for-performance target for dialysis adequacy. J Am Soc Nephrol. 2011;22(12):2296–302. doi: 10.1681/ASN.2010111137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Department of Agriculture. Ruralurban continuum codes [Internet] Washington (DC): USDA; 2003. [cited 2016 Aug 5]. Available from: http://www.ers.usda.gov/data-products/rural-urban-continuum-codes/documentation.aspx. [Google Scholar]
- 31.Healthcare Cost and Utilization Project. MEDINCSTQ—median household income state quartile for patient ZIP code [Internet] Rockville (MD): Agency for Healthcare Research and Quality; [cited 2016 Aug 5]. Available from: http://www.hcup-us.ahrq.gov/db/vars/siddistnote.jsp?var=medincstq. [Google Scholar]
- 32.Jacobson G, Damico A, Neuman T, Gold M. Medicare Advantage 2015 spotlight: enrollment market update [Internet] Menlo Park (CA): Henry J. Kaiser Family Foundation; 2015. Jun 30, [cited 2016 Aug 5]. Available from: http://kff.org/medicare/issue-brief/medicare-advantage-2015-spotlight-enrollment-market-update/ [Google Scholar]
- 33.Jenkins RL, Bemiss EL, Jr, Lorr M. Duration of hospitalization, readmission rate and stability of diagnoses in veterans hospitalized with neuropsychiatric diagnoses. Psychiatr Q. 1953;27(1):59–72. doi: 10.1007/BF01562475. [DOI] [PubMed] [Google Scholar]
- 34.Dharmarajan K, Hsieh AF, Lin Z, Bueno H, Ross JS, Horwitz LI, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355–63. doi: 10.1001/jama.2012.216476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fischer C, Lingsma HF, Marang-van de Mheen PJ, Kringos DS, Klazinga NS, Steyerberg EW. Is the readmission rate a valid quality indicator? A review of the evidence. PLoS One. 2014;9(11):e112282. doi: 10.1371/journal.pone.0112282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.D’Errigo P, Tosti ME, Fusco D, Perucci CA, Seccareccia F. Use of hierarchical models to evaluate performance of cardiac surgery centres in the Italian CABG outcome study. BMC Med Res Methodol. 2007;7:29. doi: 10.1186/1471-2288-7-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cooke CR, Kennedy EH, Wiitala WL, Almenoff PL, Sales AE, Iwashyna TJ. Despite variation in volume, Veterans Affairs hospitals show consistent outcomes among patients with non-postoperative mechanical ventilation. Crit Care Med. 2012;40(9):2569–75. doi: 10.1097/CCM.0b013e3182591eee. [DOI] [PubMed] [Google Scholar]
- 38.Rogers MA, Blumberg N, Saint S, Langa KM, Nallamothu BK. Hospital variation in transfusion and infection after cardiac surgery: a cohort study. BMC Med. 2009;7:37. doi: 10.1186/1741-7015-7-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gershengorn HB, Iwashyna TJ, Cooke CR, Scales DC, Kahn JM, Wunsch H. Variation in use of intensive care for adults with diabetic ketoacidosis. Crit Care Med. 2012;40(7):2009–15. doi: 10.1097/CCM.0b013e31824e9eae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gulliford MC, Adams G, Ukoumunne OC, Latinovic R, Chinn S, Campbell MJ. Intraclass correlation coefficient and outcome prevalence are associated in clustered binary data. J Clin Epidemiol. 2005;58(3):246–51. doi: 10.1016/j.jclinepi.2004.08.012. [DOI] [PubMed] [Google Scholar]
- 41.Barnett ML, Hsu J, McWilliams JM. Patient characteristics and differences in hospital readmission rates. JAMA Intern Med. 2015;175(11):1803–12. doi: 10.1001/jamainternmed.2015.4660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Singh S, Lin YL, Kuo YF, Nattinger AB, Goodwin JS. Variation in the risk of readmission among hospitals: the relative contribution of patient, hospital and inpatient provider characteristics. J Gen Intern Med. 2014;29(4):572–8. doi: 10.1007/s11606-013-2723-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sheingold SH, Zuckerman R, Shartzer A. Understanding Medicare hospital readmission rates and differing penalties between safety-net and other hospitals. Health Aff (Millwood) 2016;35(1):124–31. doi: 10.1377/hlthaff.2015.0534. [DOI] [PubMed] [Google Scholar]
- 44.Brown SE, Ratcliffe SJ, Halpern SD. An empirical derivation of the optimal time interval for defining ICU readmissions. Med Care. 2013;51(8):706–14. doi: 10.1097/MLR.0b013e318293c2fa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tang VL, Halm EA, Fine MJ, Johnson CS, Anzueto A, Mortensen EM. Predictors of rehospitalization after admission for pneumonia in the Veterans Affairs healthcare system. J Hosp Med. 2014;9(6):379–83. doi: 10.1002/jhm.2184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. J Am Coll Cardiol. 2013;62(16):e147–239. doi: 10.1016/j.jacc.2013.05.019. [DOI] [PubMed] [Google Scholar]
- 47.Thompson JS, Baxter BT, Allison JG, Johnson FE, Lee KK, Park WY. Temporal patterns of postoperative complications. Arch Surg. 2003;138(6):596–602. doi: 10.1001/archsurg.138.6.596. discussion 602–3. [DOI] [PubMed] [Google Scholar]
- 48.Herrin J, St Andre J, Kenward K, Joshi MS, Audet AM, Hines SC. Community factors and hospital readmission rates. Health Serv Res. 2015;50(1):20–39. doi: 10.1111/1475-6773.12177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Centers for Medicare and Medicaid Services. Outcome measures: hospital performance reports: chartbook series 2014 [Internet] Baltimore (MD): CMS; 2014. [cited 2016 Aug 5]. Available for download from: https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/hospitalqualityinits/outcomemeasures.html. [Google Scholar]
- 50.Bergethon KE, Ju C, DeVore AD, Hardy NC, Fonarow GC, Yancy CW, et al. Lack of improvement in 30-day readmission rates for patients hospitalized with heart failure: data from Get With the Guidelines—Heart Failure Registry. J Card Fail. 2015;21(8):s10. doi: 10.1161/CIRCHEARTFAILURE.115.002594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Carey K, Lin MY. Readmissions to New York hospitals fell for three target conditions from 2008 to 2012, consistent with Medicare goals. Health Aff (Millwood) 2015;34(6):978–85. doi: 10.1377/hlthaff.2014.1408. [DOI] [PubMed] [Google Scholar]
- 52.Kohn L, Simerl W, Boon Z, Friday K, Holderness C, Peterson E, et al. Hospital value-based purchasing: initial results show modest effects on Medicare payments and no apparent change in quality-of-care trends [Internet] Washington (DC): Government Accountability Office; 2015. Oct, [cited 2016 Aug 5]. Available from: http://www.gao.gov/assets/680/672899.pdf. [Google Scholar]
- 53.Feng Z, Wright B, Mor V. Sharp rise in Medicare enrollees being held in hospitals for observation raises concerns about causes and consequences. Health Aff (Millwood) 2012;31(6):1251–9. doi: 10.1377/hlthaff.2012.0129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Neuman MD, Wirtalla C, Werner RM. Association between skilled nursing facility quality indicators and hospital readmissions. JAMA. 2014;312(15):1542–51. doi: 10.1001/jama.2014.13513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ottenbacher KJ, Karmarkar A, Graham JE, Kuo YF, Deutsch A, Reistetter TA, et al. Thirty-day hospital readmission following discharge from postacute rehabilitation in fee-for-service Medicare patients. JAMA. 2014;311(6):604–14. doi: 10.1001/jama.2014.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fisher ES, Staiger DO, Bynum JP, Gottlieb DJ. Creating accountable care organizations: the extended hospital medical staff. Health Aff (Millwood) 2007;26(1):w44–57. doi: 10.1377/hlthaff.26.1.w44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


