Abstract
Purpose
To compare the performance of non-contrast MRI with HASTE versus contrast-enhanced MRI/3D-MRCP for assessment of suspected choledocholithiasis in hospitalized patients.
Methods and Materials
123 contrast-enhanced abdominal MRI/MRCP scans in the hospital setting for possible choledocholithiasis were retrospectively evaluated. ERCP, intraoperative cholangiogram or documented clinical resolution served as the reference standard. Readers first evaluated the biliary tree using coronal and axial HASTE and other non-contrast sequences, and later reviewed the entire exam with post-contrast sequences and 3D-MRCP. Test performance for the image sets was compared for choledocholithiasis, acute hepatitis, cholangitis, and acute cholecystitis. Reader agreement, MRCP image quality, and confidence levels were also assessed. Clinical predictors of age and fever were tested for association with perceived need for contrast in biliary assessment.
Results
There were 27 cases of choledocholithiasis, 31 cases of acute hepatitis, 37 cases of acute cholecystitis, and 3 clinically diagnosed cases of acute cholangitis. Both the abbreviated and full contrast-enhanced/MRCP image sets resulted in high accuracy for choledocholithiasis (91.1–94.3% versus 91.9–92.7%). There was no difference in sensitivity or specificity for either reader for any diagnosis between image sets (p>0.40). 1 reader showed improved confidence (p<0.001) with inclusion of MRCP and contrast-enhanced images, but neither confidence nor MRCP quality scores were associated with diagnostic accuracy. Patient age and fever did not predict the need for contrast-enhanced images.
Conclusion
In hospitalized patients with suspected choledocholithiasis, performance of non-contrast abdominal MRI with HASTE is similar to contrast-enhanced MRI with 3D-MRCP, offering potential for decreased scanning time and improved patient tolerability.
Introduction
Gallstone disease is estimated to affect 10–15% of adults with over 6 billion dollars in associated healthcare costs each year in the U.S. alone (1–3). When gallstones are symptomatic, the presence of choledocholithiasis can affect treatment decisions and patient outcomes. The incidence of choledocholithiasis varies according to clinical presentation but has been reported to be approximately 5–15% in patients undergoing laparoscopic cholecystectomy, and 18–33% in acute biliary pancreatitis (2, 4, 5). Therefore, patients with symptomatic gallstones are often evaluated for choledocholithiasis before cholecystectomy or during treatment for pancreatitis (5, 6).
Possible choledocholithiasis may be most accurately tested using endoscopic retrograde cholangiopancreatography (ERCP), which is also therapeutic but associated with a small risk of complications, including pancreatitis, cholangitis, hemorrhage or bowel perforation (7–11). Endoscopic ultrasound (EUS) has a lower complication rate than ERCP, but provides only diagnostic evaluation for choledocholithiasis with high sensitivity (93–97%) and specificity (77–96%) (2, 12–15). Although the American Society for Gastrointestinal Endoscopy recommends direct endoscopic evaluation for individuals with pretest probability for choledocholithiasis of greater than 50%, and magnetic resonance cholangiopancreatography (MRCP) or EUS for intermediate pretest probability (10–50%), imaging is commonly favored in order to optimize selection for therapeutic ERCP, and particularly in patients who may be at higher risk of endoscopic complication (2, 4, 16, 17). Moreover, a 2015 Cochrane review found EUS and MRCP to be essentially equivalent in their ability to evaluate for the presence of CBD gallstones (18).
3D-heavily T2 weighted fast spin echo MRCP offers high signal-to-noise and contrast-to-noise ratios for delineation of the biliary tree, and near-isotropic voxels also improve postprocessing for maximum intensity projections. The signal-to-noise ratio is higher than in 2D MRCP, though thinner contiguous sections of 2D MRCP may be considered a complement to 3D MRCP. While MRCP sequences are routinely acquired in suspected cholestasis, the subset of patients in a clinical condition severe enough for hospitalization face difficulty with breathing instructions (including regular breathing for respiratory triggering) and with the length of scanning time needed for a high-quality, contrast-enhanced MRI. The half-Fourier acquisition single-shot turbo spin echo (HASTE) sequence is also routinely included in the protocol for acute cholestasis, and the technique previously provided a basis for accurate assessment of the biliary tree with MRCP, though publications have not directly compared diagnostic accuracy of the sequence with other 2D- or 3D-MRCP techniques (19). Thus, the added value of acquiring 3D-MRCP in patients with suspected choledocholithiasis has not been studied.
The need for intravenous contrast in MRI evaluation of suspected choledocholithiasis is also not well established. In patients with signs of acute biliary obstruction, the American College of Radiology recommends ultrasound as the first line study, and MRI with and without gadolinium contrast is considered “usually appropriate,” as contrast may be helpful in assessment for cholangitis, while non-contrast MRCP has a lower appropriateness rating of “may be appropriate” (20). However, ascending cholangitis is suspected in a minority of cases of symptomatic gallstone disease, is usually clinically diagnosed using Charcot’s triad of right upper quadrant pain, fever or chills, and jaundice, along with laboratory data and evidence of biliary dilatation on ultrasound; MRI findings in themselves do not establish the diagnosis (21).
Evaluation of the biliary tree in patients with acute abdominal pain for possible choledocholithiasis may potentially be accomplished using a simplified MRCP protocol to reduce scanner time and resource utilization, and expedite patient care in the hospital setting. Our purpose was to assess the performance of a potential abbreviated protocol of non-contrast MRI with abdominal HASTE images versus contrast-enhanced MRI/3D-MRCP for assessment of suspected choledocholithiasis in hospitalized patients. Secondarily, we examined the detection of other etiologies of acute cholestasis, and also described incidental findings that would warrant additional contrast-enhanced imaging when only non-contrast sequences were viewed.
Methods and Materials
Patient Population
This study was approved by our institutional review board and compliant with the Health Insurance Portability and Accountability Act. The institutional PACS system was searched for all consecutive abdominal MRI/MRCP examinations with contrast performed in inpatients and emergency department patients from January 2013–June 2014. Inclusion criteria were as follows: 1) adults aged 18 years or older, and 2) MRI indication of possible choledocholithiasis, or symptomatic gallstone disease with suspected acute biliary obstruction. Exclusion criteria were: 1) chronic abdominal pain, 2) painless jaundice, 3) known malignancy and/or metastatic disease, and 3) other medical conditions predisposing patients to jaundice (e.g. chronic hepatitis B or C, primary sclerosing cholangitis, liver disease associated with HIV or cystic fibrosis). A reference standard of ERCP or intraoperative cholangiogram was required to confirm suspected choledocholithiasis, while clinical follow-up of at least 1 month after presentation for acute biliary symptoms was used to confirm negative results for choledocholithiasis or other biliary pathology. One of the authors (LH) recorded pertinent clinical factors, including presence or absence of patient age, fever, and clinically diagnosed acute pancreatitis, ascending cholangitis, or acute hepatitis.
Imaging Technique
For symptomatic gallstone disease and acute biliary obstruction, MRI at our institution is performed with and without gadolinium contrast, at the time of the collected studies using gadopentetate dimeglumine (Magnevist, Bayer HealthCare). All examinations were performed on 1.5T clinical scanners (Avanto, Siemens, Erhlangen, Germany) using a torso phase-array coil, and sequences included: axial fat-saturated T2-weighted imaging, axial and coronal HASTE, axial T1 weighted in-phase and out-of-phase imaging, axial diffusion weighted imaging (DWI), and axial 3D T1-weighted spoiled gradient-recalled echo fat-suppressed imaging before and after dynamic contrast administration of 0.1 mmol of Magnevist per kilogram of body weight followed by 20 cc saline flush, with measures at 0, 60 and 120 seconds (Table 1). In addition, MRCP was performed using a respiratory triggered, coronal oblique 3D T2-weighted fast spin echo sequence. MRCP PACE acquisition parameters included: TR/TE 3000/620 ms, flip angle 180, number of averages 1, field of view 320 mm, matrix size of 384 × 361, bandwidth 318 Hz/pixel, slice thickness 1.2 mm, intersection gap 1.5 mm, number of averages 1, parallel imaging acceleration factor 2. MRCP thick slab parameters included TR/TE of 5000/463 ms, flip angle 180, slice thickness 50 mm, and field of view 350 mm.
Table 1.
MRI parameters in protocol for acute biliary obstruction
| Sequence | TR (ms) | TE (ms) | Flip angle | Slice thickness (mm) | Intersection gap (mm) | Matrix size | FOV (cm) |
|---|---|---|---|---|---|---|---|
| Axial HASTE | infinite | 87 | 150 | 4 | 0.7 | 256 × 256 | 420 |
| Coronal HASTE | infinite | 101 | 150 | 6 | 0.7 | 320 × 224 | 350 |
| 3D PACE MRCP* | 3000 | 620 | 180 | 1.2 | 1.5 | 384 × 361 | 320 |
| 3D MRCP Thick Slab | 5000 | 463 | 180 | 50 | -- | 384 × 384 | 350 |
| Axial T2 FSE fat-saturated | 2800 | 90 | 150 | 4 | 0.8 | 256 × 179 | 420 |
| DWI# | 6400 | 93 | -- | 8 | 1.6 | 192 × 144 | 350 |
| 3D fat-suppressed T1W GRE | 3.46 | 1.28 | 12 | 3.3 | N/A | 256 × 129 | 350 |
Coronal oblique plane
b values of 50, 500, 1000
Reader Interpretation
The abbreviated image set included HASTE, DWI, T2-weighted fat-saturated imaging, and pre-contrast T1-weighted imaging, but excluded 3D-MRCP and post-contrast images. The full sets of sequences were reviewed after a two-week washout period. Two fellowship-trained abdominal radiologists (JR,AD) with 2 years of experience independently evaluated each set of images for acute pathology of the biliary tree and liver, blinded to the results of the examination and clinical outcomes. Assessment included indication of presence or absence of choledocholithiasis, and presence of an alternative cause of acute biliary obstruction with options for specific type of abnormality including acute hepatitis and acute cholangitis. Acute hepatitis was diagnosed on noncontrast MRI on the basis of periportal edema and increased signal on T2-weighted imaging in the liver parenchyma, and gallbladder wall thickening as may be seen on multiple sequences, and heterogeneous arterial phase enhancement or delayed periportal enhancement of the liver may have contributed to diagnosis when viewing post-contrast images (22, 23). Acute cholangitis was determined present with periportal increased signal on T2-weighted imaging and biliary ductal dilatation with bile duct wall thickening on pre-contrast sequences; the addition of wall enhancement may have served as a confirmatory characteristic on post-contrast images (24).
Readers submitted confidence scores for assessment of the biliary tree on a 5-point scale: 1 = very low degree of confidence (<25%), 2 = low degree of confidence (25–49%), 3= moderate (50–75% confident), 4 = high (75–95%), 5=highest (>95% certainty). Quality scores for 3D-MRCP were submitted on a 5-point scale: 1 = non-diagnostic, 2 = minimal information provided (e.g. common bile duct dilated versus non-dilated and otherwise no information), 3= evaluation of some of the biliary tree, 4 = good visualization of entire biliary tree, and 5 = excellent visualization of entire biliary tree (Fig. 1, 2). Readers also indicated whether or not contrast-enhanced imaging would have been needed to aid the evaluation of a cause of acute cholestasis on abbreviated imaging sets, exclusive of cases where acute pancreatitis was the only finding needing contrast-enhanced evaluation as the diagnosis is most often clinically suspected and would result in contrast-enhanced MRI regardless of the possibility of choledocholithiasis or cholecystitis. Separately, incidental findings the readers perceived as requiring contrast-enhanced evaluation for further characterization were also noted during use of the abbreviated image set to examine the potential consequence of additional imaging tests.
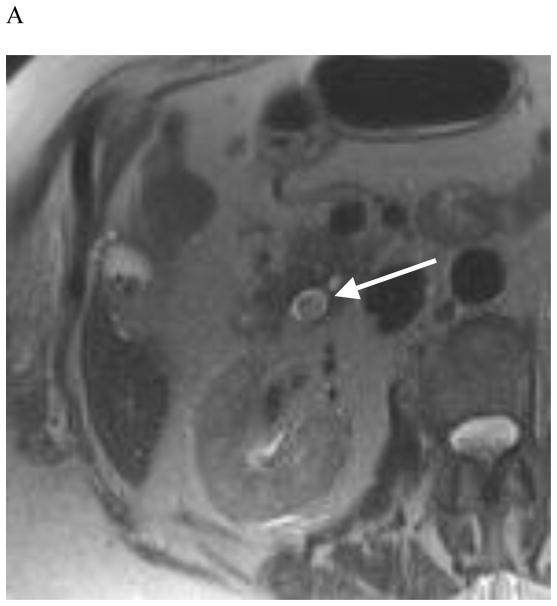
Fig. 1.


A 90-year-old woman with right abdominal pain for one day and history of gallstones. Axial HASTE (A, arrow) and axial T2-fat saturated (B, arrow) sequences show a gallstone at the level of the ampulla in the presence of common bile duct dilatation. Both readers assigned the MRCP, including MRCP PACE (C), with a quality score of 5, indicating excellent visualization of entire biliary tree including choledocholithiasis in this case (arrow). The diagnosis was correctly made by both readers using abbreviated as well as the full image set
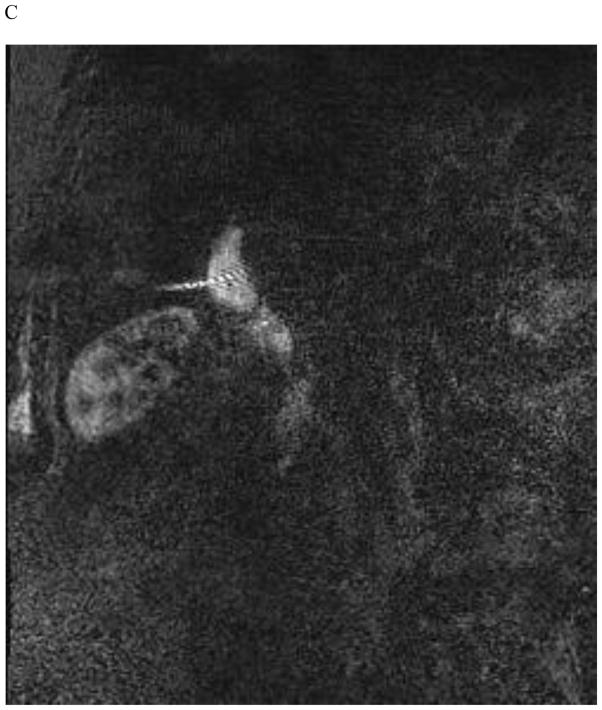
Fig. 2.
A 72-year-old man with severe right upper quadrant pain for one day and abnormal liver function tests. Axial HASTE (A, arrow) and axial T2-fat saturated (B, arrow) sequences show a gallstone in the distal common bile duct with dilatation of the bile duct, as correctly interpreted by both readers using the abbreviated image set. Both readers assigned the MRCP, including MRCP PACE (C), with a low quality score of 2, indicating minimal information provided as the images depicted a dilated common bile duct but otherwise poor visualization of the biliary tree secondary to breathing motion
Data Analysis
Inter-reader agreement was assessed using simple kappa coefficients and in terms of the percentage of times the readers provided concordant opinions for choledocholithiasis and for alternative diagnoses when evaluating the non-contrast imaging sets for the same case. Kappa (K) was interpreted as an indication of poor agreement when less than zero, as slight agreement when 0≤K≤0.2, as fair agreement when 0.2<K≤0.4, as moderate agreement when 0.4<K≤0.6 and as substantial agreement when K>0.6.
For each reader and diagnosis, the abbreviated and contrast-enhanced data sets were compared in terms of sensitivity, specificity and overall diagnostic accuracy using McNemar tests. Since patients identified as test positive or negative for a given condition were not identical for the two image sets, logistic regression for correlated data was used in place of the McNemar test to compare the image sets in terms of positive and negative predictive values. Specifically, generalized estimating equations (GEE) based on binary logistic regression was used to model the indicator of a correct diagnosis relative to the reference standard as a function of image set (abbreviated versus contrast-enhanced).
Image quality of 3D-MRCP and reader confidence were recorded using 5-point Likert scales; the Mann-Whitney test was used in both cases to compare the mean quality and confidence scores in cases in which the reader incorrectly and correctly diagnosed choledocholithiasis.
Clinical predictors of patient age and fever were assessed for their association with perceived need for contrast-enhanced imaging of the biliary tree when readers were limited to the non-contrast study. For fever, Fisher’s exact test was used to compare patients with and without each finding in terms of the percentage needing contrast for assessment of the biliary tree, while for age the Mann-Whitney test was used to compare cases the reader felt did and did not need contrast. All statistical tests were conducted at the two-sided 5% significance level using SAS 9.3 software (SAS Institute, Cary, NC).
Results
Summary of Cohort and Test Performance
123 MRI scans for 123 patients with thin-section MRCP were included in retrospective analysis, including 65 women and 58 men, with mean age 56.4 +/− 21.7 years (range 18–96 years). There were 98 cases of diagnosed acute hepatobiliary pathology among the 123 patients, including 27 confirmed instances of choledocholithiasis, 31 clinically confirmed cases of acute hepatitis, 37 cases of acute cholecystitis at surgical pathology, and 3 clinically diagnosed cases of acute cholangitis. Nearly all (119/123) patients had a preceding ultrasound of the abdomen recorded in PACS, while the remainder had an abdominal CT or no prior imaging in PACS.
There was no difference between the performance of the abbreviated and full contrast-enhanced MRCP image sets for detection of choledocholithiasis, acute hepatitis or acute cholecystitis (presented in Table 2). The accuracy of the abbreviated set for choledocholithiasis was 91.1–94.3%, while the full study yielded an accuracy of 91.9–92.7% (p=0.80–1.00). Sensitivity for choledocholithiasis was 70.0–85.2% for the abbreviated image set versus 70.4–81.5% for the full study (p=1.0), with specificity of 96.9–97.9% for the abbreviated set versus 95.8–97.9% for the full study (p=1.0). For determination of alternative acute hepatobiliary diagnoses, performance was also similarly accurate (82.8–82.9% and 78.0–83.6% for abbreviated and full image sets, respectively; p= 0.42–1.00). There was no difference in test performance for detection of acute hepatitis (Fig. 3), with sensitivity of 16.1–19.4% and specificity of 95.7–100% for both image sets; acute cholecystitis was detected with overall accuracy of 83.5–85.3% for both image sets. Acute cholangitis was also detected with similar accuracy (96.7–98.4%) across both image sets although the total number of cases was small.
Table 2.
Performance characteristics of non-contrast MRI images with HASTE versus contrast-enhanced MRI/3D-MRCP in patients with suspected acute cholestasis. P values are from McNemar tests to compare image sets in terms of accuracy, sensitivity and specificity or from GEE to compare the sets in terms of predictive values.
| Abbreviated Image Set | Contrast-MRI/MRCP | P Value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Outcome | Component | Reader | % Correct | # Correct | N | % Correct | # Correct | N | |
| Choledocholithiasis | Accuracy | 1 | 94.3% | 116 | 123 | 92.7% | 114 | 123 | 0.797 |
| Accuracy | 2 | 91.1% | 112 | 123 | 91.9% | 113 | 123 | 1.000 | |
| NPV | 1 | 95.9% | 93 | 97 | 94.8% | 92 | 97 | 1.000 | |
| NPV | 2 | 91.3% | 94 | 103 | 92.2% | 94 | 102 | 1.000 | |
| PPV | 1 | 88.5% | 23 | 26 | 84.6% | 22 | 26 | 1.000 | |
| PPV | 2 | 90.0% | 18 | 20 | 90.5% | 19 | 21 | 1.000 | |
| Sensitivity | 1 | 85.2% | 23 | 27 | 81.5% | 22 | 27 | 1.000 | |
| Sensitivity | 2 | 70.0% | 18 | 27 | 70.4% | 19 | 27 | 1.000 | |
| Specificity | 1 | 96.9% | 93 | 96 | 95.8% | 92 | 96 | 1.000 | |
| Specificity | 2 | 97.9% | 94 | 96 | 97.9% | 94 | 96 | 1.000 | |
| Alternative Diagnosis in Biliary Tree | Accuracy | 1 | 82.9% | 102 | 123 | 78.0% | 96 | 123 | 0.421 |
| Accuracy | 2 | 82.8% | 101 | 122 | 83.6% | 102 | 122 | 1.000 | |
| NPV | 1 | 86.9% | 93 | 107 | 84.8% | 89 | 105 | 0.697 | |
| NPV | 2 | 85.5% | 94 | 110 | 86.2% | 94 | 109 | 1.000 | |
| PPV | 1 | 56.3% | 9 | 16 | 38.9% | 7 | 18 | 0.492 | |
| PPV | 2 | 58.3% | 7 | 12 | 61.5% | 8 | 13 | 1.000 | |
| Sensitivity | 1 | 39.1% | 9 | 23 | 30.4% | 7 | 23 | 0.758 | |
| Sensitivity | 2 | 30.4% | 7 | 23 | 34.8% | 8 | 23 | 1.000 | |
| Specificity | 1 | 93.0% | 93 | 100 | 89.0% | 89 | 100 | 0.459 | |
| Specificity | 2 | 94.9% | 94 | 99 | 94.9% | 94 | 99 | 1.000 | |
| Acute Hepatitis | Accuracy | 1 | 76.4% | 94 | 123 | 76.4% | 94 | 123 | 1.000 |
| Accuracy | 2 | 78.9% | 97 | 123 | 78.0% | 96 | 123 | 1.000 | |
| NPV | 1 | 77.4% | 89 | 115 | 77.9% | 88 | 113 | 1.000 | |
| NPV | 2 | 78.0% | 92 | 118 | 77.8% | 91 | 117 | 1.000 | |
| PPV | 1 | 62.5% | 5 | 8 | 60.0% | 6 | 10 | 1.000 | |
| PPV | 2 | 100% | 5 | 5 | 83.3% | 5 | 6 | 1.000 | |
| Sensitivity | 1 | 16.1% | 5 | 31 | 19.4% | 6 | 31 | 1.000 | |
| Sensitivity | 2 | 16.1% | 5 | 31 | 16.1% | 5 | 31 | 1.000 | |
| Specificity | 1 | 96.7% | 89 | 92 | 95.7% | 88 | 92 | 1.000 | |
| Specificity | 2 | 100% | 92 | 92 | 98.9% | 91 | 92 | 1.000 | |
| Ascending Cholangitis | Accuracy | 1 | 96.7% | 119 | 123 | 97.6% | 120 | 123 | 1.000 |
| Accuracy | 2 | 98.4% | 121 | 123 | 98.4% | 121 | 123 | 1.000 | |
| NPV | 1 | 98.3% | 118 | 120 | 99.2% | 118 | 119 | 1.000 | |
| NPV | 2 | 98.4% | 120 | 122 | 99.2% | 119 | 120 | 1.000 | |
| PPV | 1 | 33.3% | 1 | 3 | 50.0% | 2 | 4 | 1.000 | |
| PPV | 2 | 100% | 1 | 1 | 66.7% | 2 | 3 | 1.000 | |
| Sensitivity | 1 | 33.3% | 1 | 3 | 66.7% | 2 | 3 | 1.000 | |
| Sensitivity | 2 | 33.3% | 1 | 3 | 66.7% | 2 | 3 | 1.000 | |
| Specificity | 1 | 98.3% | 118 | 120 | 98.3% | 118 | 120 | 1.000 | |
| Specificity | 2 | 100% | 120 | 120 | 99.2% | 119 | 120 | 1.000 | |
Fig. 3.
A 25-year-old woman with severe right upper quadrant pain, gallstones and elevated bilirubin. Coronal HASTE image shows marked gallbladder edema (arrow) and periportal edema (arrowhead) (A), with mildly elevated T2 signal intensity of the liver parenchyma (B) leading to the diagnosis of acute hepatitis on noncontrast MRI by both readers using the abbreviated image set, also confirmed clinically. There was also heterogeneous arterial-phase enhancement on axial fat-suppressed 3D GRE T1-weighted image after injection of gadopentetate dimeglumine (C, arrow)
For both tasks of evaluating for choledocholithiasis and presence of alternative diagnoses on both imaging sets of abbreviated MRI and full MRI/MRCP protocols, the kappa values indicated substantial agreement. For choledocholithiasis, kappa values were 0.84 and 0.87 for the non-contrast abbreviated and full contrast-enhanced imaging sets, respectively. For presence of an alternative biliary diagnosis, kappa values were 0.76 and 0.67 for the non-contrast abbreviated and full contrast-enhanced imaging sets, respectively.
Need for Contrast-enhanced Images
For assessment of the biliary tree for a cause of acute biliary obstruction, the readers varied in reported need for contrast-enhanced imaging from 4.9–21.1%, with agreement for 3 cases in which thickening of the common bile duct wall was suspected but equivocal, a common bile duct with abrupt cutoff at the pancreatic head with questioned mass, and 2 cases with indeterminate liver lesions possibly representing metastases or abscesses. Findings for which one reader perceived need for contrast included necrotic periportal lymph nodes versus peripancreatic collection, 3 additional cases of questioned common bile duct thickening, questioned mass-like thickening of a gallbladder, and 5 cases of acute versus chronic cholecystitis. Patient age and fever were tested for association with perceived need for contrast when evaluating the biliary tree and liver; when either reader indicated need for contrast-enhanced images, there was no association with presence of fever (p=0.41, 0.22) nor patient age (p=0.26, 0.73).
In terms of incidental findings requiring contrast-enhanced imaging, 18.7% (23/123) of the scans included such findings as determined by both readers. Renal and liver lesions each accounted for 34.8% (8/23) of findings, while pancreatic lesions accounted for 26.1% (6/23) of findings, and lesions in other organs accounted for the remaining 4.4% (1/23).
Association of Reader Confidence and 3D-MRCP Quality with Diagnostic Accuracy for Choledocholithiasis
The confidence scores differed for 1 of 2 readers, where the mean confidence score for evaluation of the biliary tree and liver was higher with inclusion of contrast-enhanced and 3D-MRCP images (4.03 versus 4.48, p<0.001) while the other reader showed no difference (4.17 versus 4.20, p=0.31). However, no difference was seen in confidence scores between correctly versus incorrectly diagnosed instances of choledocholithiasis for either reader, in either imaging set (p=0.09, 0.91). There was also no difference in the MRCP quality scores between correctly and incorrectly diagnosed choledocholithiasis for either reader (shown in Table 3, p>0.1).
Table 3.
The mean, standard deviation (SD), median and inter-quartile range (IQR) of the confidence scores and 3D-MRCP quality scores from each reader among cases the reader felt did and did not have a correct diagnosis of choledocholithiasis. P values are calculated from the exact Mann-Whitney tests used to compare cases the reader felt did and did have a correct finding of common bile duct stones in terms of scores.
| Reader | Image Type | CBD Stone Diagnosis Incorrect | CBD Stone Diagnosis Correct | P Value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Median | IQR | Mean | SD | Median | IQR | |||
| Confidence Scores | ||||||||||
| 1 | Non-contrast | 3.86 | 0.69 | 4.0 | 1.0 | 4.04 | 0.92 | 4.0 | 2.0 | 0.471 |
| 1 | MRCP/Contrast | 4.11 | 0.78 | 4.0 | 1.5 | 4.51 | 0.69 | 5.0 | 1.0 | 0.089 |
| 2 | Non-Contrast | 3.82 | 1.25 | 4.0 | 2.0 | 4.21 | 0.94 | 4.5 | 1.0 | 0.345 |
| 2 | MRCP/Contrast | 4.30 | 0.95 | 5.0 | 2.0 | 4.23 | 1.07 | 5.0 | 1.0 | 0.906 |
|
3D-MRCP Quality Scores | ||||||||||
| 1 | MRCP/Contrast | 3.11 | 1.27 | 3.0 | 2.0 | 3.78 | 1.23 | 4.0 | 2.0 | 0.107 |
| 2 | MRCP/Contrast | 2.80 | 1.40 | 3.0 | 3.0 | 3.19 | 1.05 | 3.0 | 1.5 | 0.278 |
Discussion
For patients in the hospital setting, an abbreviated non-contrast MRI with HASTE has the potential to provide more rapid evaluation with similar performance to a full contrast enhanced MRI with 3D-MRCP in detection of choledocholithiasis, with our results suggesting no compromise in diagnostic test performance. Diagnosis of acute hepatitis, acute cholecystitis, and cholangitis also did not improve with contrast, as sensitivity and specificity did not differ from that of the simulated abbreviated protocol. We note an overall low sensitivity overall for detecting acute hepatitis compared with clinical criteria. Importantly, our analysis excluded evaluation of pancreatitis, as contrast-enhanced imaging remains indicated for evaluation of the pancreas in clinically diagnosed acute pancreatitis or for complications of gallstone pancreatitis.
Breathing motion may impact the quality of thin-section MRCP in the acutely ill patient population. However, MRCP quality scores showed no association with diagnostic performance. Furthermore, the overall sensitivity and specificity of MRI/MRCP for choledocholithiasis in our study was comparable to previous reports of performance at similar rates of disease prevalence (18, 25). Despite the thicker sections used in HASTE imaging than in thin-section MRCP, we found no difference in detection of choledocholithiasis. HASTE remains a routinely acquired sequence in abdominal MRI, and provides rapid and clear imaging of the biliary tree and gallbladder, as well as other abdominal organs, with minimal susceptibility to patient motion (26, 27). Readers may therefore rely upon HASTE and other pre-contrast T1 and T2-weighted sequences to assess for choledocholithiasis without negative impact on diagnostic performance for this particular task and assessment of other common causes of acute cholestasis, and the value of acquiring 3D-MRCP is questioned in acutely ill patients who are less likely to be able to cooperate with breathing instructions. These findings are most relevant to inpatient and emergency department patients, in whom answering the most urgent and clinically relevant questions may be favorable over a comprehensive examination.
We also analyzed incidental findings to assess the potential impact of a non-contrast study on recommendations for additional imaging. More than 50% of these lesions perceived as needing contrast-enhanced imaging were pancreatic cystic lesions and small renal cystic lesions with some degree of complexity. Such findings may lead to recommendation for additional tests but are overall considered low risk for patient harm, and would therefore be unlikely to warrant characterization during a period of hospitalization. Ding et al encouraged analysis of incidental findings in establishing the value of imaging tests, and in our study there appears to be a tradeoff of approximately 19% of studies that would have potentially resulted in recommended additional imaging for more complete characterization of incidental findings (28). It remains debatable whether this rate is acceptable in the context of imaging performed for acute illness, and the tradeoff of rapid imaging for a chance of incompletely characterized incidental findings. The benefits/harms scenario may be comparable to recommendations for additional imaging of incidental findings on emergency room abdominal CT scans that most commonly have a single contrast-enhanced phase.
Our study limitations include retrospective design rather than a prospective comparison study of diagnostic test accuracy, and relatively small size. The findings apply to the inpatient and emergency department patient population, and may not be generalizable to patients capable of cooperating with breathing instructions and a full exam. We also evaluated a set of patients meeting criteria for signs of acute biliary obstruction, and results do not extend to patients with uncertainty regarding longer term obstructive symptoms with a potential malignancy, or the subset of patients with a high degree of suspicion for an abscess or infection acting as the primary cause of symptoms; contrast administration is indicated when these diagnoses are considered more likely than choledocholithiasis. Although we found no association of the MRCP image quality with the diagnostic performance, it is possible that the overall quality of outpatient scans may differ enough to provide an advantage in detection of choledocholithiasis. The small number of cases of acute cholangitis precluded a sub-analysis of MRI performance in diagnosis of this secondary process, and referrer-directed use of contrast-enhanced studies is warranted when imaging findings would help establish a clinically equivocal case of cholangitis. We also did not analyze whether small gallstones specifically may be less well detected with an abbreviated image set using HASTE. Our protocol also included both axial and coronal HASTE imaging but protocols may vary by institution, and we did not assess the contribution of each imaging plane or compare their diagnostic accuracy.
In conclusion, patients in the hospital setting may be evaluated with similar performance using non-contrast-enhanced MRI with axial and coronal HASTE instead of a full, contrast-enhanced technique with 3D-MRCP for suspected choledocholithiasis or other common causes of acute cholestasis. No difference in accuracy is seen in terms of choledocholithiasis or acute cholecystitis, or the alternative diagnosis of acute hepatitis. With exception of MRI indications to evaluate for complications of acute gallstone pancreatitis or elevated pretest probability of other infectious or neoplastic etiologies of cholestasis, acutely ill patients with suspicion for symptomatic gallstone disease may benefit from shortened, non-contrast examinations without compromise in diagnostic accuracy.
Acknowledgments
Dr. Kang has received research funding from the National Institutes of Health (K07CA197134) and the Association of University Radiologists (sponsored by GE Healthcare).
Funding: Dr. Kang and this investigation were funded in part by an Association of University Radiologists-GE Radiology Research Academic Fellowship Award.
Footnotes
Dr. Heacock declares that she has no conflict of interest. Drs. Doshi, Sun, Ream, and Babb declare no conflict of interest.
Compliance with Ethical Standards
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed Consent was waived by the institutional review board for this study.
References
- 1.Stinton LM, Shaffer EA. Epidemiology of gallbladder disease: cholelithiasis and cancer. Gut and liver. 2012;6(2):172–87. doi: 10.5009/gnl.2012.6.2.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Committee ASoP. Maple JT, Ben-Menachem T, Anderson MA, Appalaneni V, Banerjee S, et al. The role of endoscopy in the evaluation of suspected choledocholithiasis. Gastrointestinal endoscopy. 2010;71(1):1–9. doi: 10.1016/j.gie.2009.09.041. [DOI] [PubMed] [Google Scholar]
- 3.Shaffer EA. Epidemiology and risk factors for gallstone disease: has the paradigm changed in the 21st century? Current gastroenterology reports. 2005;7(2):132–40. doi: 10.1007/s11894-005-0051-8. [DOI] [PubMed] [Google Scholar]
- 4.Kaltenthaler EC, Walters SJ, Chilcott J, Blakeborough A, Vergel YB, Thomas S. MRCP compared to diagnostic ERCP for diagnosis when biliary obstruction is suspected: a systematic review. BMC medical imaging. 2006;6:9. doi: 10.1186/1471-2342-6-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Topal B, Van de Moortel M, Fieuws S, Vanbeckevoort D, Van Steenbergen W, Aerts R, et al. The value of magnetic resonance cholangiopancreatography in predicting common bile duct stones in patients with gallstone disease. The British journal of surgery. 2003;90(1):42–7. doi: 10.1002/bjs.4025. [DOI] [PubMed] [Google Scholar]
- 6.Petrov MS, Savides TJ. Systematic review of endoscopic ultrasonography versus endoscopic retrograde cholangiopancreatography for suspected choledocholithiasis. The British journal of surgery. 2009;96(9):967–74. doi: 10.1002/bjs.6667. [DOI] [PubMed] [Google Scholar]
- 7.Loperfido S, Angelini G, Benedetti G, Chilovi F, Costan F, De Berardinis F, et al. Major early complications from diagnostic and therapeutic ERCP: a prospective multicenter study. Gastrointestinal endoscopy. 1998;48(1):1–10. doi: 10.1016/s0016-5107(98)70121-x. [DOI] [PubMed] [Google Scholar]
- 8.Christensen M, Matzen P, Schulze S, Rosenberg J. Complications of ERCP: a prospective study. Gastrointestinal endoscopy. 2004;60(5):721–31. doi: 10.1016/s0016-5107(04)02169-8. [DOI] [PubMed] [Google Scholar]
- 9.Ong TZ, Khor JL, Selamat DS, Yeoh KG, Ho KY. Complications of endoscopic retrograde cholangiography in the post-MRCP era: a tertiary center experience. World journal of gastroenterology: WJG. 2005;11(33):5209–12. doi: 10.3748/wjg.v11.i33.5209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Andriulli A, Loperfido S, Napolitano G, Niro G, Valvano MR, Spirito F, et al. Incidence rates of post-ERCP complications: a systematic survey of prospective studies. The American journal of gastroenterology. 2007;102(8):1781–8. doi: 10.1111/j.1572-0241.2007.01279.x. [DOI] [PubMed] [Google Scholar]
- 11.Baillie J. Predicting and preventing post-ERCP pancreatitis. Current gastroenterology reports. 2002;4(2):112–9. doi: 10.1007/s11894-002-0047-6. [DOI] [PubMed] [Google Scholar]
- 12.Garrow D, Miller S, Sinha D, Conway J, Hoffman BJ, Hawes RH, et al. Endoscopic ultrasound: a meta-analysis of test performance in suspected biliary obstruction. Clinical gastroenterology and hepatology: the official clinical practice journal of the American Gastroenterological Association. 2007;5(5):616–23. doi: 10.1016/j.cgh.2007.02.027. [DOI] [PubMed] [Google Scholar]
- 13.Kohut M, Nowakowska-Dulawa E, Marek T, Kaczor R, Nowak A. Accuracy of linear endoscopic ultrasonography in the evaluation of patients with suspected common bile duct stones. Endoscopy. 2002;34(4):299–303. doi: 10.1055/s-2002-23641. [DOI] [PubMed] [Google Scholar]
- 14.Tse F, Liu L, Barkun AN, Armstrong D, Moayyedi P. EUS: a meta-analysis of test performance in suspected choledocholithiasis. Gastrointestinal endoscopy. 2008;67(2):235–44. doi: 10.1016/j.gie.2007.09.047. [DOI] [PubMed] [Google Scholar]
- 15.Lachter J, Rubin A, Shiller M, Lavy A, Yasin K, Suissa A, et al. Linear EUS for bile duct stones. Gastrointestinal endoscopy. 2000;51(1):51–4. doi: 10.1016/s0016-5107(00)70387-7. [DOI] [PubMed] [Google Scholar]
- 16.Verma D, Kapadia A, Eisen GM, Adler DG. EUS vs MRCP for detection of choledocholithiasis. Gastrointestinal endoscopy. 2006;64(2):248–54. doi: 10.1016/j.gie.2005.12.038. [DOI] [PubMed] [Google Scholar]
- 17.Mandelia A, Gupta AK, Verma DK, Sharma S. The Value of Magnetic Resonance Cholangio-Pancreatography (MRCP) in the Detection of Choledocholithiasis. Journal of clinical and diagnostic research: JCDR. 2013;7(9):1941–5. doi: 10.7860/JCDR/2013/6158.3365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Giljaca V, Gurusamy KS, Takwoingi Y, Higgie D, Poropat G, Stimac D, et al. Endoscopic ultrasound versus magnetic resonance cholangiopancreatography for common bile duct stones. The Cochrane database of systematic reviews. 2015;2:CD011549. doi: 10.1002/14651858.CD011549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miyazaki T, Yamashita Y, Tsuchigame T, Yamamoto H, Urata J, Takahashi M. MR cholangiopancreatography using HASTE (half-Fourier acquisition single-shot turbo spin-echo) sequences. AJR American journal of roentgenology. 1996;166(6):1297–303. doi: 10.2214/ajr.166.6.8633435. [DOI] [PubMed] [Google Scholar]
- 20.Lalani T, Couto CA, Rosen MP, Baker ME, Blake MA, Cash BD, et al. ACR appropriateness criteria jaundice. Journal of the American College of Radiology: JACR. 2013;10(6):402–9. doi: 10.1016/j.jacr.2013.02.020. [DOI] [PubMed] [Google Scholar]
- 21.Wada K, Takada T, Kawarada Y, Nimura Y, Miura F, Yoshida M, et al. Diagnostic criteria and severity assessment of acute cholangitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg. 2007;14(1):52–8. doi: 10.1007/s00534-006-1156-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Martin DR, Seibert D, Yang M, Salman K, Frick MP. Reversible heterogeneous arterial phase liver perfusion associated with transient acute hepatitis: findings on gadolinium-enhanced MRI. J Magn Reson Imaging. 2004;20(5):838–42. doi: 10.1002/jmri.20192. [DOI] [PubMed] [Google Scholar]
- 23.Matsui O, Kadoya M, Takashima T, Kameyama T, Yoshikawa J, Tamura S. Intrahepatic periportal abnormal intensity on MR images: an indication of various hepatobiliary diseases. Radiology. 1989;171(2):335–8. doi: 10.1148/radiology.171.2.2704798. [DOI] [PubMed] [Google Scholar]
- 24.Bader TR, Braga L, Beavers KL, Semelka RC. MR imaging findings of infectious cholangitis. Magn Reson Imaging. 2001;19(6):781–8. doi: 10.1016/s0730-725x(01)00401-5. [DOI] [PubMed] [Google Scholar]
- 25.Kaltenthaler E, Vergel YB, Chilcott J, Thomas S, Blakeborough T, Walters SJ, et al. A systematic review and economic evaluation of magnetic resonance cholangiopancreatography compared with diagnostic endoscopic retrograde cholangiopancreatography. Health technology assessment. 2004;8(10):iii, 1–89. doi: 10.3310/hta8100. [DOI] [PubMed] [Google Scholar]
- 26.Byott S, Harris I. Rapid acquisition axial and coronal T2 HASTE MR in the evaluation of acute abdominal pain. Eur J Radiol. 2016;85(1):286–90. doi: 10.1016/j.ejrad.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 27.Bannas P, Pickhardt PJ. MR Evaluation of the Nontraumatic Acute Abdomen with CT Correlation. Radiol Clin North Am. 2015;53(6):1327–39. doi: 10.1016/j.rcl.2015.06.014. [DOI] [PubMed] [Google Scholar]
- 28.Ding A, Eisenberg JD, Pandharipande PV. The economic burden of incidentally detected findings. Radiologic clinics of North America. 2011;49(2):257–65. doi: 10.1016/j.rcl.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]