THE CASE: A 6-year-old previously healthy right-handed girl presented with a 3-day history of progressive epigastric abdominal pain, polydipsia and secondary nocturnal enuresis and a 2-week history of weight loss of 5 kg. Her initial assessment revealed tachypnea with Kussmaul's respiration, tachycardia and moderate dehydration, with an estimated fluid deficit of 6%– 9%. The girl was hyperglycemic (plasma glucose level 43.4 mmol/L) and acidotic (pH 7.13, bicarbonate level 3.8 mmol/L), with urinalysis revealing ketonuria and glucosuria. After admission, appropriate fluid resuscitation and insulin treatment were started. The patient's diabetic ketoacidosis resolved over 20 hours, at which point a diabetic diet was introduced along with subcutaneous insulin therapy.
On the morning after admission, the patient was found by the nursing staff to be irritable, lethargic and intermittently combative. Twelve hours later a right hemiparesis and aphasia became evident. A cranial CT scan showed an evolving infarct in the left basal ganglia. Transcranial Doppler ultrasonography and magnetic resonance angiography showed occlusion of the proximal left middle cerebral artery (Fig. 1). Echocardiography showed 2 thrombi, measuring 11 х 9 mm and 1 х 1 mm respectively, on the underside of the anterior mitral valve leaflet. There was no associated congenital heart disease. Because of a high risk of further thromboembolic events, heparin infusion was begun, and open thrombectomy was performed on the third day. Pathological examination revealed inflammatory cells and an organized thrombus. Blood cultures and prothrombotic studies yielded negative findings.
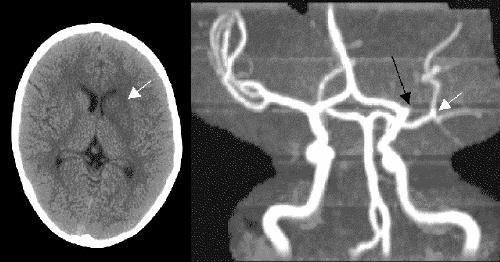
Fig. 1: Left: Initial non-contrast cranial CT scan of 6-year-old girl showing evolving infarct and focal edema of the left basal ganglia (arrow). Right: Maximal intensity projection time-of-flight magnetic resonance angiogram showing occlusion of the proximal left middle cerebral artery (black arrow); the overlying artery (white arrow) is the patent left posterior cerebral artery.
Intensive rehabilitation therapy and low-molecular-weight heparin (enoxaparin, 30 mg subcutaneously every 12 hours) were started after surgery, and the insulin treatment was continued. A year after her stroke the patient is still receiving insulin therapy as well as ASA 40 mg/d. She is functioning at an age-appropriate grade level at school and can ambulate independently.
The incidence of type 1 diabetes mellitus varies from 0.1 to 36.8 per 100 000 worldwide. Diabetic ketoacidosis (DKA) is a well-recognized complication of insulin deficiency in children and adolescents and results in hospital admission in about 10 per 100 000 children in Canada.
Optimal management of pediatric DKA requires judicious correction of dehydration and metabolic abnormalities, and administration of insulin.1 In addition, patients should have their neurological status closely monitored for at least 48 hours after presentation.
The most common cause of acute neurological deterioration in children with DKA is cerebral edema, which occurs in 3 to 10 per 1000 cases of DKA and is associated with morbidity and mortality of 35% and 24% respectively. Early signs and symptoms of cerebral edema include headache, confusion, drowsiness, or unexplained changes in heart rate, blood pressure or respiratory pattern.
Intracerebral arterial or sinus venous thrombosis may also cause acute neurological deterioration in children with DKA. Despite the known association between adult DKA and vascular thrombosis, little is known about pediatric DKA and vascular thrombosis, and the incidence of ischemic stroke in children with DKA remains undefined. Rates of death from stroke in children vary from 7% to 28%. In a recent series of 123 children with ischemic stroke, only one-third of the survivors were neurologically normal.2 Children with multiple risk factors for stroke tend to have worse outcomes.
The initial presentation of pediatric stroke can be subtle, with nonspecific changes in behaviour, new-onset seizures or altered level of consciousness. Patients suspected of having central nervous system (CNS) complications should be treated in a pediatric intensive care unit, with prompt neurological imaging studies (cranial CT or MRI, or both) to look for evidence of cerebral edema or other intracranial pathologies.
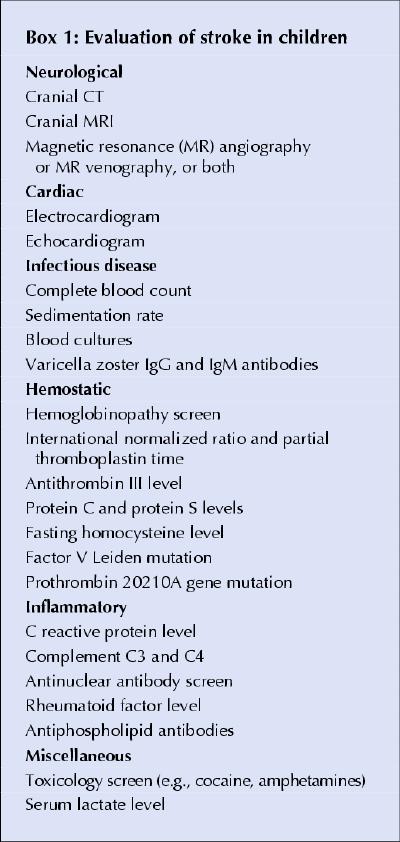
Besides metabolic abnormalities, other risk factors for ischemic stroke in children include congenital heart disease, sickle-cell anemia, coagulation disorders, vasculopathy, infection and a number of uncommon genetic disorders. Evaluation of pediatric stroke requires a systematic approach (Box 1). Careful history-taking may identify recent head or neck trauma, varicella zoster infection, drug ingestion, or a family history of hematologic or vascular disease.
Box 1.
Ischemic stroke is potentially treatable in children. Safe and successful acute thrombolysis in children has been reported with the use of the recombinant tissue plasminogen activator (rtPA) alteplase within 3 hours after the onset of symptoms.3,4 The use of local or systematic thrombolytic agents, including urokinase, streptokinase and rtPA, in children was associated with bleeding complications in 10% to 20% of cases and intracranial hemorrhage in 1% to 2%.5 The risk of intracerebral hemorrhage associated with the use of alteplase in pediatric stroke is currently unknown. In adults, thrombolysis for acute stroke has a 6% risk of symptomatic hemorrhagic transformation.
Without published randomized clinical trials, the treatment of pediatric stroke will remain controversial. Thrombolysis has become the standard of care for acute treatment of adult ischemic stroke in North America. Rapid diagnosis and treatment within 3 hours after the onset of symptoms is required for optimal thrombolytic therapy in adults. However, this 3-hour window is difficult to achieve in adults and may be even more difficult to achieve in children. In one report, less than one-quarter of cases of ischemic stroke in children were diagnosed within 3 hours after symptom onset.6 On the other hand, there may be indications for thrombolysis in pediatric stroke beyond the first few hours after onset. Recently 2 cases were reported in which children with vertebrobasilar thrombosis benefited from rtPA therapy up to 36 hours after symptom onset.7,8 Despite the high risk of complications, the poor natural history of basilar artery occlusion in both cases justified the aggressive treatment approach.
In summary, several key clinical issues should be emphasized. First, children with DKA should be managed according to pediatric protocols for the treatment of fluid and metabolic abnormalities. Second, close monitoring of their neurological status is required for at least 48 hours after presentation. Third, although neurological deterioration in children with DKA is more likely to be due to cerebral edema, clinicians must consider stroke in the differential diagnosis because of the prothrombotic tendency in these children. Finally, a high index of suspicion and early recognition of CNS complications in DKA is required for prompt initiation of therapy and optimization of outcome. Children with ischemic stroke may be candidates for acute thrombolytic therapy if the stroke can be diagnosed early.
Josephine Ho Danièle Pacaud Division of Endocrinology Department of Pediatrics Michael D. Hill Departments of Clinical Neurosciences, Medicine and Community Health Sciences Catherine Ross Division of Pediatric Critical Care Department of Pediatrics Lorie Hamiwka Jean K. Mah Division of Neurology Department of Pediatrics Faculty of Medicine University of Calgary Calgary, Alta.
References
- 1.Dunger DB, Sperling MA, Acerini CL, Bohn DJ, Daneman D, Danne TP, et al. European Society for Paediatric Endocrinology/Lawson Wilkins Pediatric Endocrine Society consensus statement on diabetic ketoacidosis in children and adolescents. Pediatrics 2004; 113:e133-e140. [DOI] [PubMed]
- 2.DeVeber GA, MacGregor D, Curtis R, Mayank S. Neurologic outcome in survivors of childhood arterial ischemic stroke and sinovenous thrombosis. J Child Neurol 2000;15:316-24. [DOI] [PubMed]
- 3.Gruber A, Nasel C, Lang W, Kitzmuller E, Bavinzski G, Czech T. Intra-arterial thrombolysis for the treatment of perioperative childhood cardioembolic stroke. Neurology 2000; 54: 1684-6. [DOI] [PubMed]
- 4.Carlson MD, Leber S, Deveikis J, Silverstein FS. Successful use of rt-tPA in pediatric stroke. Neurology 2001; 57: 102-4. [DOI] [PubMed]
- 5.Monagle P, Michelson AD, Bovill E, Andrew M. Antithrombotic therapy in children. Chest 2001;119(1 Suppl): 344S- 370S. [DOI] [PubMed]
- 6.Gabis LV, Yangala R, Lenn NJ. Time lag to diagnosis of stroke in children. Pediatrics 2002;110:924-8. [DOI] [PubMed]
- 7.Cognard C, Weill A, Lindgren S, Piotin M, Castaings L, Moret J. Basilar artery occlusion in a child: “clot angioplasty” followed by thrombolysis. Childs Nerv Syst 2000;16:496-500. [DOI] [PubMed]
- 8.Kirton A, Wong JH, Mah J, Ross BC, Kennedy J, Bell K, et al. Successful endovascular therapy for acute basilar thrombosis in an adolescent. Pediatrics 2003;112:e248-e251. [DOI] [PubMed]


