Abstract
Objective
To examine the influence of collectivist orientation (often called familismo when applied to the Latino sub-group in the United States) in oral health discussion networks.
Basic Research Design
Through respondent-driven sampling and face-to-face interviews, we identified respondents’ (egos) personal social network members (alters). Egos stated whom they talked with about oral health, and how often they discussed dental problems in the preceding 12 months.
Participants
An urban community of adult Mexican-American immigrants in the Midwest United States. We interviewed 332 egos (90% born in Mexico); egos named an average of 3.9 alters in their networks, 1,299 in total.
Method
We applied egocentric network methods to examine the ego, alter, and network variables that characterize health discussion networks.
Results
Kin were most often leveraged when dental problems arose; egos relied on individuals whom they perceive to have better knowledge about dental matters. However, reliance on knowledgeable alters decreased among egos with greater behavioral acculturation.
Conclusions
This paper developed a network-based conceptualization of familismo. We describe the structure of oral health networks, including kin, fictive kin, peers, and health professionals, and examine how networks and acculturation help shape oral health among these Mexican-Americans.
Keywords: network science, social network analysis, familismo, collectivism, dental health, Mexican immigrants, Mexican-American
Introduction
Disproportionate experience of oral health problems among Latinos is well established (Dye et al., 2015; Eke et al., 2015). Various explanations of these oral health disparities have pointed to biological susceptibility, structural barriers posed by health care systems and lifestyle (Maupome et al., 2015a) as possible reasons. However, the role of personal interactions within social networks is often ignored. This gap in our understanding of social factors underlying oral health disparities is worrying, as it has been established in other areas of health and disease that individuals often discuss issues within their personal social networks (Bearman and Parigi, 2004; Perry and Pescosolido, 2015). Specifically, scholars have developed the Network-Episode Model (NEM) as a response to more individualistic models for healthcare decision-making (Pescosolido, 2006). According to the NEM, episodes of illness are embedded within both formal (i.e. professional) and informal (i.e. lay) social networks. Individuals rely on these relationships to understand and address their health problems: network members can offer support, recommend, or provide services, influence health behaviors, and encourage or discourage treatment adherence. Through these processes individuals leverage their social networks and shape decisions, treatment trajectories, and health outcomes.
In the present manuscript we focus on one homogenous ethnic/nationality group of Latinos to examine if and how personal social networks – and especially family members – are activated for oral health discussion (Perry and Pescosolido, 2015). Our target group is urban-based adults of Mexican origin living in the Midwest United States (henceforth called Mexican-Americans for simplicity). Mexican-Americans are the largest Latino nationality of origin, and Latinos are the fastest growing ethnic group in the USA (Ennis et al., 2011). Because utilization of dental services by Mexican-Americans is moderated by peers (Maupome et al., 2015a), health discussion within networks may influence perception and strategies to address oral health problems; a prime example being those related to oral health issues. Our qualitative research (Maupome et al., 2015a) reported that seeking urgent dental care was encouraged by peers (parents, co-workers, etc.) (Cohen et al., 2009). Seeking preventive care was also influenced by significant others, especially a spouse or partner, which partially offsets the lack of emphasis on prevention so pervasive in Mexican culture (Borrayo and Jenkins 2003). Moreover, we found that the involvement of extended family (such as grandparents) in healthcare decisions (Hilton et al., 2007) often contributed to a fatalistic view that oral diseases are inevitable and sometimes increased anxiety associated with negative dental care experiences (Cohen et al., 2009; 2007).
In keeping with the collectivist notion (Varela et al., 2004) of Latino clan structures, family and community networks have a significant influence on help-seeking in the Mexican-American population. This notion has been called familismo (McAdoo, 1999). Together with concepts such as respeto (obedience to authority, deference, and decorum in public behaviour, Marin, 1999) and simpatia (emphasis on politeness and pleasantness even in the face of stress, McAdoo, 1999), familismo is often used as a qualifier for how Latinos behave with respect to health and disease. At its most general, familismo is a multifaceted system of values that underlie norms and beliefs, as well as transgenerational solidarity (Stein et al., 2015). Familismo is often expressed as respect for authority; it encompasses acceptance that individual needs are conditioned by obligations to the clan while at the same time enjoying the benefits of unity and cohesiveness (Lugo Steidel et al., 2003). Although familismo is often quoted as a cultural value moderating Latino health behaviors and norms, calls have been made to further specify its features in distinct types of illness, various Latino sub-groups, and different historical periods (Ruiz and Ransford, 2012). A case in point is the transformation of familismo as older immigrants spend more time in the USA, are separated by geographic distance, have financial limitations, and even re-create extended family to include “fictive kin” (Ruiz and Ransford, 2012). Such fluid conceptualizations serve as a reminder that familismo is not a single entity.
Latino values such as familismo lie at the heart of differences between Latinos and other ethnic/race groups with respect to health behaviors. For example, Hispanic college students were more likely than Whites to seek support from peers and use prayer as approaches to alleviate pain compared to students from other backgrounds (Hastie et al., 2005). Additionally, Hispanics had a heightened concern and sense of responsibility for the welfare of kin when considering health behaviors such as tobacco and alcohol use (VanOss Marin et al., 1990); this trend was also exemplified by Hispanic smokers being more likely to perceive tobacco use as poor parental role models (compared to non-Hispanic White smokers), or being concerned by second hand smoking posing a risk to children (Marin et al., 1990). Finally, a considerable proportion of Hispanics who delayed seeking care for a dental problem, paradoxically, did so out of fear of negatively affecting a pregnancy (Cohen et al., 2008), lending more weight to the Hispanic-specific perceptions of health issues having impacts beyond the individual.
Building on our initial research and cited literature on familismo, we set out to examine familismo in the context of oral health by identifying health discussion within a network of people of Mexican origin. We aimed to generally improve understanding of the specific social ties underlying difficult-to-operationalize cultural processes (Jimenez et al., 2009). The present report uses data from the TalaSurvey Study, a structured survey and social network analysis investigation into a well-bounded community of Mexican-Americans in the Midwest United States. Our principle aim was to identify characteristics of individual actors and dyadic relationships that influence whom Mexican-American immigrants talk to about oral health problems, in relation to their regular discussion partners. We discuss results in the context of collectivist identity among Mexican-Americans to develop a more nuanced, network-based understanding of the link between familismo and a selected array of oral health outcomes.
Materials and Methods
Procedures were approved by an IRB at Indiana University (#1306011692). Participation included signing a letter of informed consent in Spanish or English after explanations in person in either language. The study had additional protection through a Federal Certificate of Confidentiality to allay fears by potential participants who may have been concerned about disclosing personal information. In this way we minimized self-selection of participants toward a biased group of Mexican-Americans with legal residence status in the USA.
Participants were urban-based adults of Mexican origin, first- or second-generation immigrants, recruited in the fall and winter of 2013 through announcements made via churches, community organizations flyers and posters. Participants received monetary compensation.
A questionnaire was adapted (Wright and Gayman, 2006) to include name generator questions addressing oral health domains. After iterative refinement in focus groups, Spanish-English translation and back translation was undertaken. The adapted questionnaire was discussed with community members to verify literacy level, clarity, and relevance. They did not take part in the main study. Questionnaires were administered individually in English or Spanish by trained staff.
Social network analysis (SNA) is a set of relational methods identifying connections between members of a system. SNA is a perspective using systematic approaches grounded in graph theoretic images and statistical models. One such form of SNA is egocentric analysis. Egocentric studies use information about egos (the person being interviewed) and their relationships with other people that the ego names (i.e. alters); such studies use name generator questions to identify and gather information about an ego’s network members, but they do not necessarily involve researchers contacting the alters. An example egocentric network is presented in the Supplemental Figure (this Figure and other appendices accompany the online-only version of this paper).
Names of alters were solicited from egos using the standard Important Matters (IM) name generator: From time to time most people discuss important matters with other people. Looking back over the past 6 months, who are the people with whom you discussed matters important to you? These can be anyone in your life: family, friends, professionals, people who live nearby or people who live far away. Who do you feel you can talk to or depend on for help if you need it? The Oral Health Matters (OHM) name generator was: Looking back over the past 12 months, who are the people with whom you discussed issues about dental health, the people in your life that you feel you can really count on for help when you have dental health problems? IM and OHM questions resulted in two lists of nominated alters for each participating ego. Egos were asked follow-up questions about each alter with defined response categories printed on cards.
The main outcome variable was frequency of discussion of oral health problems. Egos stated how often they talked about problems in the past 12 months with each alter, whether “Several times” (1) or less often (0). To predict such discussion, we analyzed variables across three conceptual levels: ego, alter, and network. At the ego level, we measured citizenship status, acculturation, education, having dental insurance, gender, and age. At the alter level, we measured how knowledgeable alter was perceived to be about dental matters, whether they resided in Indiana, frequency of contact with ego, highest level of formal education, having dental insurance, age, gender, and relationship to ego. Finally, variables at the network level aggregated characteristics of all alters who were included in the OHM network. OHM network variables included network size, average education, and average perceived dental knowledge. We used a Psychological-Behavioral Acculturation Scale (P-BAS) validated for Mexican-Americans in the Midwest United States (Maupome et al., 2015b) (Appendix A3). P-BAS incorporates distinct behavioral and psychological acculturation domains. Because the psychological domain of P-BAS had no effect on the variables investigated in this sample, it is not described in detail; a similar finding suggesting an ambivalent effect for P-BAS is discussed elsewhere (Unpublished data, Oct. 2015; manuscript under editorial review).
Following listwise deletion of observations with any missing data, the sample of egos used in analysis included 275 egos linked to 957 alters (17% of egos dropped from the analysis sample). Sensitivity analyses were conducted to compare retained cases with those omitted due to missing data. Retained egos were more likely to be older and not have a high school degree (both p<0.05, two sample two-tailed t-tests). Relative to omitted alters, the analyzed alters were more likely to be very close to the ego (p<0.05) but did not differ in other respects. Our multivariate models adjusted for demographic differences, but we emphasize the need to be cautious when generalizing results.
Because our observations are linked via network ties, normal independence assumptions for regression did not hold. To address this problem we fitted random-intercept models that nest alters (level-1) within egos (level-2) (Raudenbush and Bryk, 2002). In these models, a random intercept for each ego allows the alter observations to be conditionally independent from one another; i.e., these are mixed models that include a random intercept as well as fixed effects that are held to be the same across the level-2 units. In an unbalanced sample this approach is preferable to alternatives like clustered OLS (Raudenbush and Bryk, 2002), and it avoids the loss of information from aggregating data up to higher levels. We used Stata 13/SE (StataCorp LP, USA).
One complexity of using multilevel models arose from the TalaSurvey Study being a near-saturated sample of egocentric networks in the community: alters named by egos often overlapped and egos sometimes appeared as alters in other ego’s networks. Consequently, we conducted sensitivity analyses to assess the robustness of our approach (Appendix A1).
Results
A total of 332 immigrants (egos) participated: all indicated their parents were born in Mexico, and 90% reported being born in Mexico; 55% of egos had no education beyond elementary school; 41% reported household income <$30kpa. Only 35% of egos had dental insurance, but 43% had a dental visit in the prior 12 months. On average, egos named 3.9 alters in his/her IM+OHM personal networks, for a total of 1,299 alters. Mean number of alters in OHM networks was 2.7 (SE 1.9, range 0–9). Table 1 contains descriptive statistics for all variables.
Table 1.
Descriptive statistics for dependent and independent variables
| Variable | Mean (%) | SD | Range | Description |
|---|---|---|---|---|
| Dependent Variable | ||||
| Talk about dental problems | (0.29) | 0–1 | 1 if ego talked to alter “Several times” in past 12 months, 0 if less often. | |
| Independent Variables | ||||
| Alter characteristics1 | ||||
| Dental knowledge | 2.70 | 0.95 | 1–4 | Perceived alter dental knowledge, 1 “Nothing at all” to 4 “A lot”. |
| Local residence | (0.75) | 0–1 | 1 if alter lives in Indiana. | |
| See or talk daily | (0.55) | 0–1 | 1 if ego sees alter “Everyday”, 0 if less often. | |
| Education | (0.43) | 0–1 | 1 is high school degree or more. | |
| Age | 38.77 | 14.16 | 9–90 | Age in years. |
| Female | (0.62) | 0–1 | 1 if female. | |
| Relationship | 1–6 | Alter’s relationship to ego. | ||
| Partner/Spouse | (0.15) | |||
| Parent | (0.16) | |||
| Sibling | (0.21) | |||
| Child | (0.11) | |||
| Friend | (0.26) | |||
| Other relationship | (0.12) | |||
| Kin | (0.52) | 0–1 | 1 if alter is kin (any family relation). | |
| Ego Characteristics2 | ||||
| USA citizen | (0.23) | 0–1 | 1 if USA citizen, dual citizen, or permanent resident, 0 if Mexican citizen only. | |
| Behavioral acculturation | 2.32 | 0.90 | 1–5 | Behavioral acculturation scale. |
| Education | (0.39) | 0–1 | 1 if high school degree or more. | |
| Female | (0.61) | 0–1 | 1 if female. | |
| Age | 37.05 | 12.00 | 18–69 | Age in years. |
| Oral Health Matters Network2,3 | ||||
| Network size | 2.67 | 1.85 | 0–9 | Count of OHM network members. |
| Average alter education | 4.37 | 1.81 | 1–9 | Average education attainment on 9-level scale. |
| Average alter dental knowledge | 2.63 | 0.95 | 1–4 | Average perceived dental knowledge. |
Statistics for 957 level-1 observations.
Statistics for 275 level-2 observations.
OHM network variables were calculated using all available data for alters before other missing data adjustments.
Table 2 presents results from random-intercept logistic regression of discussion of oral health problems (1, several times; 0, else) on alter, ego, and network characteristics. The model in Panel 1 contains ego and alter characteristics. Egos had greater odds to discuss dental problems with alters who had higher ego-perceived dental knowledge (Odds Ratio, OR 3.1, p<0.001), and with those whom ego sees or talks to every day (OR 3.4, p<0.001). Interestingly, egos did not hold preferences with respect to alter education, location of residence, age, or gender. Looking at ego characteristics, female egos had marginally (p<0.10) greater odds to discuss problems with any alter, and more behaviorally acculturated egos had lower odds to discuss oral health issues with alters (OR 0.56, p<0.001).
Table 2.
Random-intercept logistic regression predicting having talked about dental problems with alter at least several times in the past 12 months using ego, alter, and network characteristics
| (1) Ego and Alter Characteristics | (2) Relationship Type | (3) Network Characteristics | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Odds ratio | Std. Error | Odds ratio | Std. Error | Odds Ratio | Std. Error | |
| Level-1 Variables | ||||||
| Alter Characteristics | ||||||
| Dental knowledge1 | 3.116 *** | (0.77) | 3.419 *** | (0.91) | 3.241 *** | (1.00) |
| Lives in Indiana | 1.123 | (0.49) | 1.737 | (0.91) | 2.015 | (0.94) |
| See or talk daily | 3.401 *** | (1.20) | 2.669 ** | (1.01) | ||
| Education | 0.813 | (0.24) | 0.917 | (0.27) | ||
| Age1 | 1.001 | (0.01) | ||||
| Female | 0.981 | (0.25) | ||||
| Relationship (ref=Partner/Spouse) | ||||||
| Parent | 0.474 | (0.24) | ||||
| Child | 0.380 + | (0.21) | ||||
| Sibling | 0145 *** | (0.07) | ||||
| Friend | 0.040 *** | (0.02) | ||||
| Other relationship | 0.058 *** | (0.03) | ||||
| Kin | 4.010 *** | (1.33) | ||||
| Ego Characteristics | ||||||
| Female | 2.101 + | (0.90) | 2.903 * | (1.49) | 2.135+ | (0.97) |
| Age | 1.017 | (0.02) | 1.025 | (0.02) | 1.024 | (0.02) |
| Education | 1.005 | (0.47) | 1.041 | (0.56) | 0.973 | (0.50) |
| Behavioral acculturation | 0.562 * | (0.16) | 0.521* | (0.17) | 0.457 ** | (0.13) |
| USA citizen | 0.446 | (0.24) | 0.320 + | (0.20) | 0.486 | (0.27) |
| Oral Health Matters Network | ||||||
| Network size | 1.315 * | (0.16) | ||||
| Average alter education | 1.034 | (0.15) | ||||
| Average alter dental knowledge | 0.869 | (0.30) | ||||
| Constant | 0.103 | (0.13) | 0.403 | (0.62) | 0.0212 | (0.03) |
|
| ||||||
| Wald χ2 | 48.81 *** | 67.03 *** | 65.42 *** | |||
| N | 957 | 957 | 957 | |||
p<0.10,
p<0.05,
p<0.01,
p<0.001 (two-tailed tests).
Level-1 continuous variables centered at grand mean. Notes: Random effects not shown; cluster robust standard errors in parentheses.
Panel 2 of Table 2 introduces dummy variables representing alters’ relationship with ego. These results are presented graphically in Figure 1. Relative to other relationships, egos tended to turn to spouses, parents, and children for discussion of dental problems. These alters had significantly greater probability to be leveraged in the OHM network than siblings, friends, or other relationships (all tests of differences p<0.05), with the exception of children versus siblings (p>0.05). These results underscore that discussion of oral health is primarily a kin-focused activity rather than one based around friends, dental professionals, or other relationships. Current results corroborate prior analyses in this dataset (Unpublished data, Aug. 2015; manuscript under editorial review).
Figure 1.
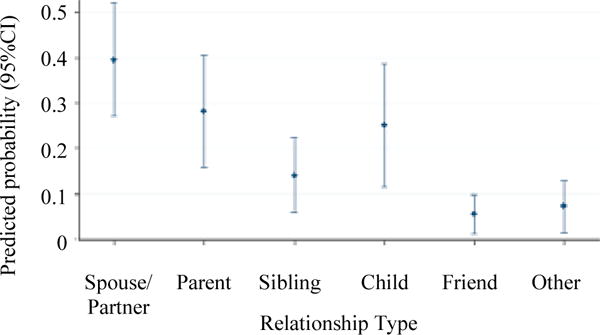
Predicted probabilities to talk about dental problems at least several times in the last 12 months (calculated from panel 2 of Table 2)
Panel 3 of Table 2 examines the impact of OHM network contextual variables on ego’s discussion of dental problems. Although average alter education and perceived dental knowledge had no effect, egos with larger OHM networks had significantly greater odds to have access to alters with whom they discuss dental problems (OR 1.3, p<0.05). Other effects in this panel are consistent with previous models. Most notably, we see that kin have a 15% greater predicted probability to be leveraged than non-kin (test of difference p<0.001).
The strong negative effect of increased behavioral acculturation on discussion in the OHM was unanticipated. A reasonable interpretation is that egos who have adjusted more to USA cultural norms may experience fewer dental problems, have acquired more relevant knowledge, and rely less on the knowledge and advice of peers. To examine this possibility, we estimated an additional model including an interaction term between behavioral acculturation and alter dental knowledge (Figure 2). Among egos with low behavioral acculturation, increasing alter dental knowledge by 1 point predicted a 0.18 difference in the probability that they were leveraged by ego to discuss dental problems, on average (p<0.01). In contrast, among egos scoring high in behavioral acculturation, increasing alter dental knowledge resulted in only a 0.04 difference in probability that egos leveraged them (p>0.05). In other words, egos with lower behavioral acculturation exhibited greater reliance on knowledgeable peers for discussion of dental problems, whereas more acculturated egos were less likely to leverage those alters.
Figure 2.
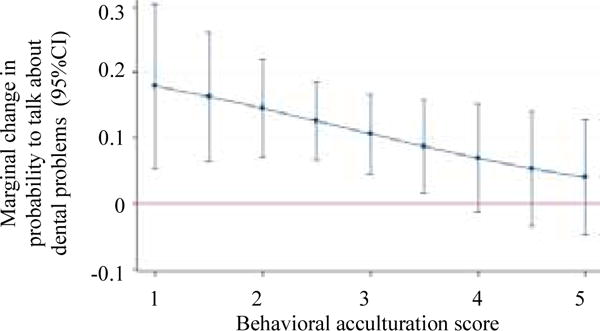
Effect of Alter dental knowledge over levels of acculturation
Note: The y-axis shows the average marginal effect of a 1-unit increase in alter perceived dental knowledge on the probability that ego talked to alter at least several times about dental problems. This marginal effect is calculated for each level of behavioral acculturation (x-axis). Model includes all controls from Table 2 plus an interaction term between acculturation and alter dental knowledge.
Appendix A2 describes testing alternative model specifications to assess stability of findings and robustness checks.
Discussion
The present study provides empirical evidence using social network methodology for the role of familismo in oral health outcomes among Mexican-Americans. It also addresses the lack of knowledge about how often Mexican-Americans interact with network members around oral health matters, and whether these patterns of interaction are consistent with familismo. Moreover, this paper adds to the current familismo literature a nuanced description of the individual, dyadic, and network-level factors influencing exchanges of information, advice, and attitudes within and outside of families.
Our results underscore that discussion of oral health issues is primarily a kin-focused activity rather than one based around friends, oral health professionals, or other relationships, as reported for other Hispanics (Cohen et al., 2009). Other research suggested (Unpublished data, Aug. 2015; manuscript under editorial review) that alters having greater knowledge about dental matters were more likely to exert social control over egos regarding oral hygiene and dental issues. Likewise, in the present analysis, we found that having alters with more dental knowledge was associated with increased discussion of oral health issues in the preceding 12 months. In the hierarchy of health discussants, a kin/non-kin divide operates when discussion of oral health issues takes place: spouses, children, and parents are more likely to be sought as health discussants than others, corroborating a preference for discussion with family members, and especially close family (Cohen et al., 2009).
Our findings on acculturation provide additional evidence for the role of familismo in oral health discussion. Specifically, net of education, health insurance status, citizenship status, and other potential confounding factors, behavioral acculturation was associated with lower odds of discussing oral health issues. Moreover, interaction models revealed that the influence of alter knowledge of dental issues was moderated by acculturation. Less acculturated Mexican-Americans displayed a strong preference for talking to knowledgeable peers about dental issues, while alter knowledge had no impact among the highly acculturated. This suggests that familism and reliance on community is likely to be especially important for less acculturated Mexican-American immigrants. It remains unclear whether this effect is a matter of more acculturated egos holding better personal information about resources to address oral health issues, being able to navigate health systems efficiently, or having resources or skills outside the OHM network that are activated when oral health issues occur. Notably, having dental insurance or not did not affect discussion patterns (Appendix A2). Together with the lack of effects for USA citizenship and level of formal schooling in ego, these results suggest the scenario cannot be simply attributed to proxy measures of higher income. Examples of non-linear effects for socio-economic position among Mexican-Americans has been found previously in relation to tooth loss (Sabbah et al., 2009) and other dental outcomes (Jimenez et al., 2009). In brief, early in the immigration process, kin and other community members serve as bridges to otherwise hard-to-reach knowledge and resources around oral health. This has implications for points of early intervention in Mexican-American immigrant communities to reduce oral health disparities.
Methodological limitations are presented in Appendix A4. Briefly, we have used a non-random sample of urban MAs in the Midwest United States, thereby being highly focused on one nationality of origin/ethnic group. Our cross-sectional design precludes solid suggestions about causality. The current study reveals the personal network level interactions underlying familismo in one group of Mexican-Americans. Our results demonstrated there is a strong preference for discussing oral health matters among close kin, and especially those who are perceived as knowledgeable. Similar to other studies on Latino immigration our findings reflect a loosening of Mexican-American norms and values traditionally perceived to embody familismo.
Supplementary Material
Acknowledgments
Funded by NIDCR grant DE022096-01A1, and by Project Development Team studies UL1TR001108 and RR025761, Indiana Clinical and Translational Sciences Institute.
References
- Bearman PS, Parigi P. Cloning headless frogs and other important matters: Conversation topics and network structure. Social Forces. 2004;83:535–557. [Google Scholar]
- Borrayo EA, Jenkins SR. feeling frugal: socioeconomic status, acculturation, and cultural health beliefs among women of Mexican descent. Cultural Diversity & Ethnic Minority Psychology. 2003;9:197–206. doi: 10.1037/1099-9809.9.2.197. [DOI] [PubMed] [Google Scholar]
- Cohen LA, Bonito AJ, Adkin DR, Manski RJ, Macek MD, Edwards RR, Cornelius LJ. Toothache pain: a comparison of visits to physicians, emergency departments, and dentists. Journal of the American Dental Association. 2008;139:1205–1216. doi: 10.14219/jada.archive.2008.0336. [DOI] [PubMed] [Google Scholar]
- Cohen LA, Bonito AJ, Adkin DR, Manski RJ, Macek MD, Edwards RR, Cornelius LJ. Toothache pain: Behavioral impact and self-care strategies. Special Care in Dentistry. 2009;29:85–95. doi: 10.1111/j.1754-4505.2008.00068.x. [DOI] [PubMed] [Google Scholar]
- Cohen LA, Harris SL, Bonito AJ, Manski RJ, Macek MD, Edwards RR, Cornelius LJ. Coping with toothache pain: a qualitative study of low income persons and minorities. Journal of Public Health Dentistry. 2007;67:28–35. doi: 10.1111/j.1752-7325.2007.00005.x. [DOI] [PubMed] [Google Scholar]
- Dye B, Thornton-Evans G, Li X, Iafolla T. Dental caries and tooth loss in adults in the United States, 2011–2012. Hyattsville (MD): National Center for Health Statistics; 2015. [PubMed] [Google Scholar]
- Eke PI, Dye BA, Wei L, Slade GD, Thornton-Evans GO, Taylor GW, Page RC, Beck JD, Genco RJ. Update on prevalence of periodontitis in adults in the United States: NHANES 2009 to 2012. Journal of Periodontology. 2015;86:611–622. doi: 10.1902/jop.2015.140520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ennis SR, Rios-Vargas M, Albert NG. (2010 Census Briefs).The Hispanic Population: 2010. 2011 c2010BR-04. https://www.census.gov/prod/cen2010/briefs/c2010br-04.pdf.
- Hastie BA, Riley JL, Fillingim RB. Ethnic differences and responses to pain in healthy young adults. Pain Medicine. 2005;6:61–71. doi: 10.1111/j.1526-4637.2005.05009.x. [DOI] [PubMed] [Google Scholar]
- Hilton IV, Stephen S, Barker JC, Weintraub JA. Cultural factors and children’s oral health care: A qualitative study of carers of young children. Community Dentistry and Oral Epidemiology. 2007;35:429–438. doi: 10.1111/j.1600-0528.2006.00356.x. [DOI] [PubMed] [Google Scholar]
- Jimenez M, Dietrich T, Shih MC, Li Y, Joshipura KJ. Radical/ethnic variations in associations between socioeconomic factors and tooth loss. Community Dentistry and Oral Epidemiology. 2009;37:267–275. doi: 10.1111/j.1600-0528.2009.00466.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lugo Steidel AGL, Contreras JM. A new familism scale for use with Latino populations. Hispanic Journal of Behavioral Sciences. 2003;25:312–330. [Google Scholar]
- Marin G, VanOss Marin B, Perez-Stable EJ, Sabogal F, Otero-Sabogal R. Cultural differences in attitudes and experiences in attitudes and expectancies between Hispanic and non-Hispanic white smokers. Hispanic Journal of Behavioral Sciences. 1990;12:422–436. [Google Scholar]
- Maupome G, Aguirre-Zero O, Westerhold C. Qualitative description of dental hygiene practices within oral health and dental care perspectives of Mexican-American adults and teenagers. Journal of Public Health Dentistry. 2015a;75:93–100. doi: 10.1111/jphd.12076. [DOI] [PubMed] [Google Scholar]
- Maupome G, Marino R, Aguirre-Zero O, Ohmit A, Dai S. Adaptation of the Psychological-Behavioral Acculturation Scale to a community of urban-based Mexican Americans in the United States. Ethnicity and Disease. 2015b;25:469–478. doi: 10.18865/ed.25.4.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAdoo HP. Family ethnicity: strength in diversity. Thousand Oaks (CA): Sage Publications; 1999. [Google Scholar]
- Perry BL, Pescosolido BA. Social network activation: the role of health discussion partners in recovery from mental illness. Social Science and Medicine. 2015;125:116–128. doi: 10.1016/j.socscimed.2013.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pescosolido BA. Of pride and prejudice: the role of sociology and social networks in integrating the health sciences. Journal of Health and Social Behavior. 2006;47:189–208. doi: 10.1177/002214650604700301. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. Vol. 1. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- Ruiz ME, Ransford HE. Latino Elders reframing Familismo: Implications for health and caregiving support. Journal of Cultural Diversity. 2012;19:50–57. [PubMed] [Google Scholar]
- Sabbah W, Tsakos G, Sheiham A, Watt RG. The effects of income and education on ethnic differences in oral health: a study in US adults. Journal of Epidemiology and Community Health. 2009;63:516–520. doi: 10.1136/jech.2008.082313. [DOI] [PubMed] [Google Scholar]
- Stein LG, Gonzalez LM, Cupito AM, Kiang L, Supple AJ. The protective role of familism in the lives of Latino Adolescents. Journal of Family Issues. 2015;36:1255–1273. [Google Scholar]
- VanOss Marin B, Marin G, Perez-Stable EJ, Otero-Sabogal R, Sabogal F. Cultural differences in attitude toward smoking: Developing messages using the theory of reasoned action. Journal of Applied Social Psychology. 1990;20:478–493. [Google Scholar]
- Varela RE, Vernberg EM, Sanchez-Sosa JJ, Riveros A, Mitchell M, Mashunkashey J. Anxiety reporting and culturally associated interpretation biases and cognitive schemas: a comparison of Mexican, Mexican American, and European American families. Journal of Clinical Child & Adolescent Psychology. 2004;33:237–247. doi: 10.1207/s15374424jccp3302_4. [DOI] [PubMed] [Google Scholar]
- Wright ER, Gayman MD. Sexual networks and HIV risk of people with severe mental illness in institutional and community-based care. AIDS and Behavior. 2015;9:341–353. doi: 10.1007/s10461-005-9008-z. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


