Abstract
Objectives:
The prevalence of opioid use disorder (OUD) during pregnancy is increasing. Practical recommendations will help providers treat pregnant women with OUD and reduce potentially negative health consequences for mother, fetus, and child. This article summarizes the literature review conducted using the RAND/University of California, Los Angeles Appropriateness Method project completed by the US Department of Health and Human Services Substance Abuse and Mental Health Services Administration to obtain current evidence on treatment approaches for pregnant and parenting women with OUD and their infants and children.
Methods:
Three separate search methods were employed to identify peer-reviewed journal articles providing evidence on treatment methods for women with OUD who are pregnant or parenting, and for their children. Identified articles were reviewed for inclusion per study guidelines and relevant information was abstracted and summarized.
Results:
Of the 1697 articles identified, 75 were included in the literature review. The perinatal use of medication for addiction treatment (MAT, also known as medication-assisted treatment), either methadone or buprenorphine, within comprehensive treatment is the most accepted clinical practice, as withdrawal or detoxification risks relapse and treatment dropout. Medication increases may be needed with advancing pregnancy, and are not associated with more severe neonatal abstinence syndrome (NAS). Switching medication prenatally is usually not recommended as it can destabilize opioid abstinence. Postnatally, breastfeeding is seen as beneficial for the infant for women who are maintained on a stable dose of opioid agonist medication. Less is known about ideal pain management and postpartum dosing regimens. NAS appears generally less severe following prenatal exposure to buprenorphine versus methadone. Frontline NAS medication treatments include protocol-driven methadone and morphine dosing in the context of nonpharmacological supports.
Conclusions:
Women with OUD can be treated with methadone or buprenorphine during pregnancy. NAS is an expected and manageable condition. Although research has substantially advanced, opportunities to guide future research to improve maternal and infant outcomes are provided.
Keywords: fetus, infant, neonatal abstinence syndrome, opioid, pregnancy, substance use disorder
Opioid use disorder (OUD) is a chronic disease with potentially serious negative consequences for individuals—particularly so for pregnant and parenting women and their children—and society. (This document uses the current definition of opioid use disorder found in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders, published by the American Psychiatric Association in 2013.) Since 2002, prescription opioid use and misuse has significantly increased among men and women (pregnant and nonpregnant) (Center for Behavioral Health Statistics and Quality [CBHSQ], 2015b). In 2013–2014, the number of women aged between 15 and 44 years who reported past-month nonmedical use of psychotherapeutics, OxyContin (oxycodone) type, increased to 98,000, up 5.4% from 2011 to 2012. The number of women aged between 15 and 44 who reported past-month heroin use increased to 109,000 in 2013–2014, up 31% from 2011 to 2012 (CBHSQ, 2015a, Table 6.71A).
Infants exposed to tobacco, alcohol, prescription medications, and illicit substances may exhibit signs of physiologic withdrawal from these substances after birth. Neonatal abstinence syndrome (NAS) is a broad, nonspecific term assigned to this type of presentation in the newborn. It is widely applied both clinically and in the published literature to infants withdrawing from opioids. However, the more specific term neonatal opioid withdrawal syndrome (NOWS) is becoming more widely used. The utility of the more specific NOWS term is to capture more accurately the numbers of infants experiencing withdrawal from opioid exposure in utero. This is important because specific screening and treatment protocols can be used to promote the best outcomes for these infants, whereas infants not exposed to opioids may require different assessment and management. However, the published literature uses the more general NAS term and, in clinical practice, substance-exposed infants are typically exposed to multiple substances.
NAS incidence increased nearly 2-fold from 2009 to 2012 (Patrick et al., 2015). NOWS or NAS signs and symptoms occur 48 to 72 hours postbirth following discontinuation of prenatal opioid exposure (eg, Patrick et al., 2012; Jones and Fielder, 2015). Compared with pregnant women treated for OUD with methadone or buprenorphine, an untreated OUD group had more adverse maternal-fetal and maternal-infant health outcomes, including elevated risk of low-birth-weight newborns, intrauterine growth restriction, and placental changes (Binder and Vavrinková, 2008). Research to develop evidence-based criteria or consensus statements for the treatment of pregnant and parenting women with OUD and the concurrent care of their infants and children is largely absent. Thus, practical recommendations derived from appropriate and accepted clinical experiences are urgently needed.
An effective method for assessing the validity of clinical procedures with limited scientific evidence is the RAND Appropriateness Method (RAM), developed in the 1980s by the RAND Corporation and the University of California, Los Angeles (UCLA). A PubMed search for “RAND/UCLA Appropriateness Method” indicates the RAM has been used in 127 articles, 77 of which were published in the last 5 years, including the American Society of Addiction Medicine (ASAM) National Practice Guideline for the Use of Medications in the Treatment of Addiction Involving Opioid Use (Kampman and Jarvis, 2015) and the Practice Guidance for Buprenorphine for the Treatment of Opioid Use Disorders: Results of an Expert Panel Process (Farmer et al., 2015).
The foundation of any appropriateness study is a critical literature review. However, unlike a meta-analysis, which combines the results of different studies to allow for the use of inferential statistical methods, the RAM literature review objective is to produce a synthesis of all available evidence, including the collective judgment of expert opinions, on a particular topic. The RAM literature review is typically less strict in inclusion criteria than a Cochrane review and, where evidence is lacking, may include lower-quality evidence, such as cohort or case studies (see Fitch et al., 2001, for RAM methodology details).
The RAM literature review presented in this article was undertaken for the US Department of Health and Human Services (HHS), Substance Abuse and Mental Health Services Administration (SAMHSA). SAMHSA used the RAM to assess the appropriateness of clinical procedures to treat pregnant and parenting women with OUD and their children and to ultimately develop guidance for healthcare providers who evaluate and treat this population.
As part of the RAM, SAMHSA convened a Federal Steering Committee (Table 1) and an Expert Panel (Table 2). The Federal Steering Committee and the Expert Panel recommended and evaluated the literature (see Search Method 3).
TABLE 1.
Agencies and Offices Participating in the Federal Steering Committee
| Bureau of Prisons (BOP) |
| Centers for Disease Control and Prevention (CDC) |
| Centers for Medicare & Medicaid Services (CMS) |
| Department of Defense (DoD) |
| Department of Veterans Affairs (VA) |
| Food and Drug Administration (FDA) |
| Health Resources and Services Administration (HRSA) |
| Indian Health Service (IHS) |
| National Institute on Drug Abuse (NIDA) |
| Office of National Drug Control Policy, The White House (ONDCP) |
| Office of the Assistant Secretary for Health (OASH) |
| Office of the Assistant Secretary for Planning and Evaluation (ASPE) |
| Office on Women's Health, Department of Health and Human Services (OWH) |
| Substance Abuse and Mental Health Services Administration (SAMHSA) |
TABLE 2.
Composition of Expert Panel by Field
| Field of Expertise | Number of Expert Panelists |
| Family medicine | 1 |
| Neonatal medicine | 1 |
| Nursing | 1 |
| Obstetrics/gynecology | 3 |
| Pediatrics | 1 |
| Psychiatry | 1 |
| Psychology | 1 |
This literature review, which arose as part of the RAM process, is intended primarily for researchers and policymakers in the areas of OUD and pregnant women whose opioid exposure also exposed infants in utero. In addition, healthcare providers interested in reviewing the evidence for treating such women and their infants and children will find this review useful.
Together, this literature review and the SAMHSA RAM report provide the foundation for a critically needed guidance document (hereafter referred to as the Guide) that will include practical recommendations for assessing and treating pregnant and parenting women with OUD and their infants and children. (SAMHSA's detailed RAM process and results are described in the report entitled Advancing the Care of Pregnant and Parenting Women With Opioid Use Disorder and Their Infants: A Foundation for Clinical Guidance, available at https://www.regulations.gov/document?D=SAMHSA-2016-0002-0001) The Guide, which is intended for healthcare providers, will be published by SAMHSA after a period of public review and comment.
The current literature review has 4 aims: (1) to summarize current evidence on treatment approaches for pregnant and parenting women with OUD and their children; (2) to identify the current state of the research; (3) to identify gaps in the research evidence; and (4) to derive recommended questions to guide future research.
METHODS
The RAM process took place from May through September 2015. Given the methodology used for this analysis, the research did not meet criteria for institutional review board review. SAMHSA instructed the Federal Steering Committee and the Expert Panel to recommend articles for inclusion in the literature review that were specific to treatment of pregnant or parenting women with OUD. Thus, articles pertaining to tobacco or alcohol cessation recommendations during pregnancy were not included. Additionally, the literature review excluded topics lacking literature; for example, treatment for depression or anxiety in pregnant or parenting women with OUD, or maternal, fetal, and child safety and efficacy data in the United States regarding naltrexone use in pregnant or postpartum women with OUD. The first step of the RAM process is to conduct a literature review of historical and newly published research. The RAM literature review took place between April 2013 and April 2015.
This RAM literature review used 3 separate search methods (Fig. 1) to identify peer-reviewed journal articles providing evidence on treatment methods for pregnant or parenting women with OUD, and for their children. Excluded were (1) review articles, as the literature review focused on primary research publications; (2) commentaries; and (3) articles not focused on opioid use and misuse in pregnant women or the effects of prenatal OUD on children (both immediate and long-term effects).
FIGURE 1.
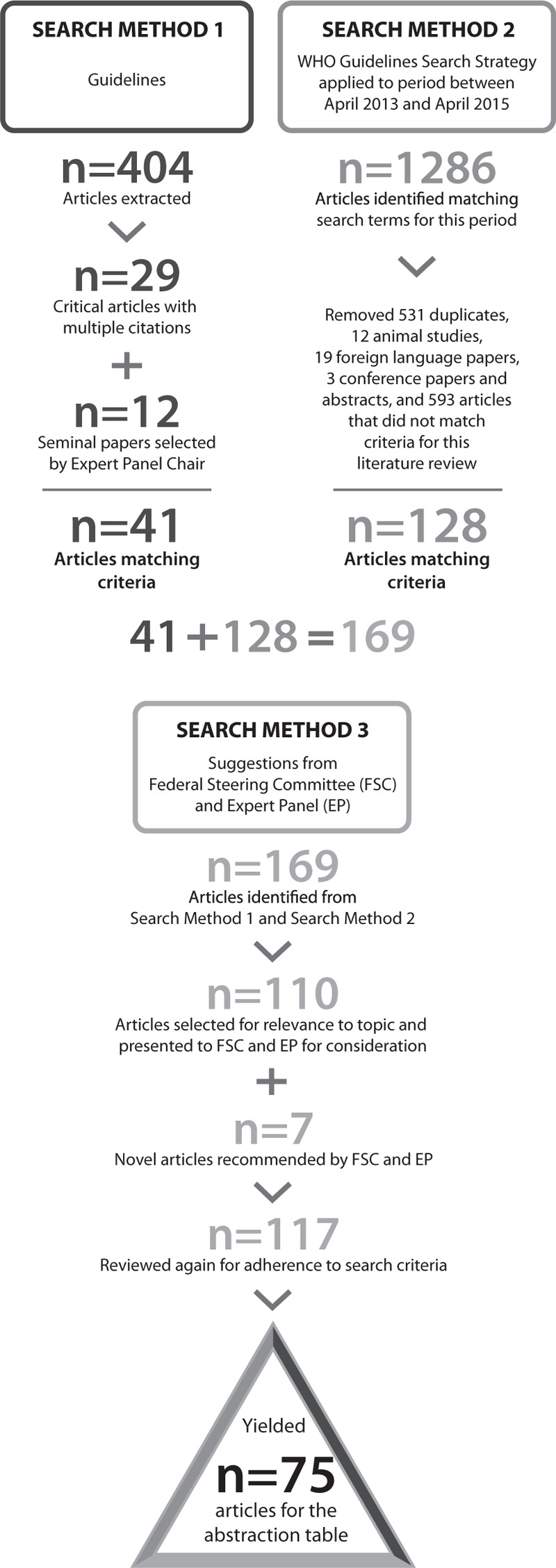
Flowchart of article identification and exclusion.
Search Method 1: Use of Bibliographies From Guidelines
For the first search method, relevant peer-reviewed primary research articles were extracted from the bibliographies of guidelines shown in Table 3, as well as recent compilations of materials devoted to substance use disorders and their treatment among pregnant or parenting women, and neonatal withdrawal from psychoactive substances.
TABLE 3.
Materials Used to Inform Search Method 1
| American College of Obstetricians and Gynecologists Committee on Health Care for Underserved Women; American Society of Addiction Medicine. Committee Opinion No. 524: Opioid Abuse, Dependence, and Addiction in Pregnancy, 2012. Available at: https://www.acog.org/-/media/Committee-Opinions/Committee-on-Health-Care-for-Underserved-Women/co524.pdf?dmc=1&ts=20160302T1440499290 |
| American Society of Addiction Medicine. National Practice Guideline for the Use of Medications in the Treatment of Addiction Involving Opioid Use. Available at: http://www.asam.org/quality-practice/guidelines-and-consensus-documents/npg |
| Hudak ML, Tan RC; Committee On Drugs, Committee On Fetus And Newborn, American Academy of Pediatrics. Clinical report: neonatal drug withdrawal. Pediatrics 2012;129:e540–e560. Available at: http://pediatrics.aappublications.org/content/129/2/e540 |
| Reece-Stremtan S, Marinelli KA; The Academy of Breastfeeding Medicine. ABM Clinical Protocol #21: guidelines for breastfeeding and substance use or substance use disorder, revised 2015. Breastfeed Med 2015;10:135–141. Available at: http://www.bfmed.org/Media/Files/Protocols/Guidelines%20for%20Breastfeeding%20and%20Substance%20Use%20or%20Use%20Disorder.pdf |
| World Health Organization. Guidelines for the Identification and Management of Substance Use and Substance Use Disorders in Pregnancy. Geneva, Switzerland: WHO Press; 2014. Available at: http://www.who.int/substance_abuse/publications/pregnancy_guidelines/en/ |
A total of 404 articles were identified in the guidelines and bibliographies. Articles that were cited more than once were considered “critical articles” and were selected for inclusion, resulting in 29 articles. These articles may have included self-citations, but this was not analyzed. Of these 29 articles, 2 were cited 5 times, 4 were cited 4 times, 3 were cited 3 times, and 20 were cited twice. The titles and abstracts of the articles cited only once were also reviewed by the Expert Panel Chair to identify additional essential articles, resulting in 12 additional articles being selected for inclusion in this literature review. This method yielded 41 articles for in-depth review.
Search Method 2: Use of World Health Organization Search Method
To identify additional articles published between April 2013 and April 2015, the second search method replicated the literature search method used in the World Health Organization's (WHO's) Guidelines for the Identification and Management of Substance Use and Substance Use Disorders in Pregnancy (WHO, 2014). The initial search produced 467 articles. A research librarian modified and added to the WHO search terms to identify additional relevant articles. Consistent with the WHO method, the librarian searched PubMed, PsycInfo, CINAHL (Cumulative Index to Nursing and Allied Health Literature), Embase, and CENTRAL (Cochrane Center Register of Controlled Trials) databases using the listed search terms (see Appendix A).
This search method yielded 819 articles. Combining the 2 strategies produced a total of 1286 articles. Of those, 1158 articles were excluded, yielding 128 articles from search method 2.
Search Method 3: Federal Steering Committee and Expert Panel Literature Review
The 169 articles from search methods 1 and 2 were then reviewed independently and in depth for a second time for relevance to the topic of OUD in pregnant and parenting women. This review reduced the article total from 169 to 110.
The Federal Steering Committee and the Expert Panel reviewed the list of 110 articles. Federal Steering Committee members recommended a review of National Institute on Drug Abuse grantee publications from April 2013 to April 2015. That review identified 74 articles, of which 46 were novel articles not identified using the first 2 search methods. The Federal Steering Committee and Expert Panel members also recommended including another 12 articles. Of these 58 articles, 7 met eligibility criteria, yielding a total of 117 articles.
A final overview of the 117 articles was conducted to remove duplicate results and articles with insufficient numbers of subjects or inappropriate use of statistical methods. Forty-two articles were dropped, leaving a final list of 75 articles (see Appendix B) selected to identify relevant evidence regarding treatment of pregnant and parenting women with OUD and their infants and children.
Creating the Abstraction Table
Three public health doctoral students with experience in conducting systematic literature reviews independently read the 75 articles. They abstracted relevant information from the eligible articles to generate a summary table presenting the key details of the study design and major findings (see Supplemental Material). To ensure fidelity to the process, the students began with a review of 3 articles. Their independent reviews resulted in complete agreement with regard to which data to extract. They then divided the remaining articles and worked collaboratively to create the abstraction table. The Expert Panel members then reviewed the abstraction table to inform their initial RAM literature review judgments.
RESULTS
All articles found through any of the search methods were included in the initial review. The earliest article was published in 1975, the latest in 2015. Included were 5 guidelines (see Table 3) that summarized the state of the field through early 2015. Of the 1697 articles identified, 75 were included in the literature review. This final list of 75 articles was selected to identify relevant evidence regarding treatment of pregnant and parenting women with OUD and their infants and children.
The current literature review covers 3 overlapping areas: (1) prenatal, (2) postnatal, and (3) neonatal. Most literature addresses methadone and buprenorphine, with limited data regarding buprenorphine + naloxone (Debelak et al., 2013; Jones et al., 2013a).
Prenatal
Medication-Assisted Withdrawal
Medication-assisted withdrawal is known to have a high relapse rate (Jones et al., 2008b). The subsequent return to use of illicit opioids subjects pregnant women and the fetus to all the risks associated with such psychoactive substance use (eg, Kaltenbach et al., 1998; Mattick et al., 2009). Despite this concern regarding opioid use relapse, a secondary data analysis reported that a few studies support the concept that a small minority of women (16%) are successful at completing medication-assisted withdrawal and remaining in drug-free treatment until delivery (eg, Lund et al., 2012).
Medication for Addiction Treatment (MAT) (also known as medication-assisted treatment) and the Fetus
Opioid agonists cross the placental barrier (Zharikova et al., 2007) in concentrations consistent with maternal dose (Concheiro et al., 2010; de Castro et al., 2011), and may adversely affect the fetus. Given the inability to measure fetal physiologic behavior directly, fetal impact from opioid agonists has focused on measures of heart and movement activity. In a secondary data analysis from the Maternal Opioid Treatment: Human Experimental Research (MOTHER) study, a large-scale trial comparing maternal and neonatal outcomes in 175 pregnant women randomly assigned to methadone or buprenorphine pharmacotherapy and provided with comprehensive care throughout their pregnancy, Jansson et al. (2011) found that compared with methadone-exposed fetuses, buprenorphine-exposed fetuses had significantly higher levels of fetal heart rate variability, more fetal heart rate accelerations, and greater coupling between fetal heart rate and fetal movement. Compared with the methadone-exposed group at 24 and 28 weeks’ gestation, the buprenorphine-exposed fetuses displayed significantly less motor activity suppression and longer duration of movements than the methadone-exposed fetuses. In another secondary analysis of MOTHER study data, Salisbury et al. (2012) reported that, at 31 and 33 weeks of gestation, compared with buprenorphine-exposed fetuses, methadone-exposed fetuses were more likely to have a nonreactive (abnormal) nonstress test, fewer fetal heart rate accelerations, and lower biophysical profile scores (hence, more negative) at peak dosing. These findings suggest more optimal fetal indicators with buprenorphine than with methadone. These indicators were equivalent in the 2 groups of fetuses before dosing, suggesting that the medication was the only critical variable.
Kakko et al. (2008) prospectively followed buprenorphine-exposed pregnancies compared with retrospective methadone-exposed pregnancies. Their data support a greater incidence of intrauterine growth restriction in the methadone-exposed than in the buprenorphine-exposed fetuses, a conclusion based on a nonsignificantly higher number of cesarean deliveries in the methadone-exposed than the buprenorphine-exposed group.
Finally, Jansson et al. (2012) reported that—in a prospective sample of women undergoing 36-week fetal monitoring—fetal heart rate, fetal heart rate variability, and fetal activity were lower in methadone-exposed fetuses relative to the nonpsychoactive-substance-exposed fetuses, measured at peak dosage levels of methadone. Moreover, fetal movement at trough (just before maternal methadone dose) measurement was significantly lower in the methadone-exposed fetuses than in the fetuses who were not exposed to psychoactive substances, which was interpreted as a methadone persistent effect.
With regard to fetal heroin and methadone exposure, 2 studies provide conflicting results and conclusions. A meta-analysis suggests that continued use of heroin while receiving methadone counteracts the birth-weight advantage gained from methadone alone (Hulse et al., 1997). In contrast, a cohort study suggests that methadone remains advantageous for the maternal-fetal dyad regardless of continued heroin use (Buckley et al., 2013). In a surveillance study, methadone alone has also not been shown to increase fetal or infant mortality (Kelly et al., 2012).
Postnatal
Methadone and Buprenorphine: Pain Medication During Pregnancy, Delivery, and Postpartum
Individuals with long-term exposure to opioids experience tolerance (reduced analgesia) and hyperalgesia (increased sensitivity to pain) (Savage, 1996). Therefore, pregnant and postpartum women using MAT or with a history of long-term exposure to opioids will likely need higher doses of opioid agonist medication during labor, delivery, and the postpartum period (Alford et al., 2006; Meyer et al., 2007, 2010). Furthermore, opioid agonist-antagonist medications (eg, nalbuphine or butorphanol) should be avoided owing to the risk of precipitated withdrawal in women receiving opioid agonists (eg, methadone or buprenorphine) (Savage, 1996; Cassidy and Cyna, 2004; Jones et al., 2014b). Jones et al. (2009) examined postpartum pain management in women with severe OUD in the Pregnant and the Reduction of Opiates: Medication Intervention Safety and Efficacy (PROMISE) study, a small-scale trial comparing maternal and neonatal outcomes in 30 pregnant women randomly assigned to methadone or buprenorphine pharmacotherapy. On average, buprenorphine-receiving women decreased their daily ibuprofen dose, whereas methadone-receiving women increased their daily ibuprofen dose.
Methadone and Buprenorphine: Postpartum Dosing
It is well established that women need increases in methadone dose with advancing gestation (eg, Jones et al., 2005). A similar yet less conclusive pattern is seen with buprenorphine (eg, Jones et al., 2005). Dividing the dose of methadone in half (split dosing) is an approved protocol for women in the third trimester of pregnancy because of the shorter half-life and larger clearances of medications during pregnancy (eg, Bogen et al., 2013). There is mixed evidence supporting the need to lower methadone or buprenorphine doses after delivery (Jones et al., 2008a; Bogen et al., 2013; Pace et al., 2014; Bastian et al., 2016).
Methadone and Buprenorphine: Breast Milk
Limited research has focused on concentrations of opioid agonist medication in breast milk; firm conclusions are difficult given the generally small sample sizes. However, assays clearly suggest that concentrations of both buprenorphine (eg, Ilett et al., 2012) and methadone (eg, Jansson et al., 2008b) in human breast milk are quite low, and pose little risk for neonates.
Methadone and Buprenorphine: Breastfeeding
Women maintained on a stable dose of methadone or buprenorphine should be encouraged to breastfeed (WHO, 2014) unless specifically contraindicated (eg, maternal human immunodeficiency virus positive [HIV+]). Few studies of opioid agonist pharmacotherapy for pregnant women with OUD have focused on breastfeeding as an outcome (notably, Johnson et al., 2001; Abdel-Latif et al., 2006; Abrahams et al., 2010; Debelak et al., 2013). The US literature typically shows low rates of breastfeeding among postpartum women with OUD (eg, Jansson et al., 2008a; Jones et al., 2010b; Pritham et al., 2012).
Impact of Breastfeeding
A study of neonates prenatally exposed to methadone or buprenorphine for a minimum of 30 days found that breastfed neonates had significantly shorter lengths of hospital stay and need for pharmacotherapy for NAS (Wachman et al., 2013). Abdel-Latif et al. (2006) examined the impact of breastfeeding in a retrospective chart review of women with opioid dependence (not all of whom were maintained on methadone; none were maintained on buprenorphine), who either breastfed or formula fed their neonates on day 5 of life. The breastfed neonatal group had lower withdrawal scores for the first 9 days postpartum, a lower rate of need for pharmacotherapy for withdrawal, a longer median time to such pharmacotherapy, and shorter hospital stays. Although relevant research is inconclusive, breastfed neonates may be exposed to small amounts of either buprenorphine or methadone, thereby avoiding the withdrawal symptoms that might be caused by an abrupt cessation of opioid exposure (Malpas and Darlow, 1999). It has also been postulated that NAS severity is mitigated by the act of breastfeeding rather than the amount of medication in breast milk (eg, WHO, 2014).
Methadone and Buprenorphine: NAS Measurement and Treatment Incidence
Widely different NAS prevalence rates are reported in the research, which largely consists of retrospective cohort studies (see Jones et al., 2012, for a comprehensive buprenorphine review). These discrepancies are likely due to 4 factors. First, the studies have different inclusion criteria (eg, including women who were using benzodiazepines), and inclusion and/or exclusion criteria for nonrandomized studies were often not reported (Jones et al., 2012). Second, there is wide variability in the measurement of NAS. For example, many scoring systems, such as the modified Finnegan, allow clinicians to assess the severity of NAS. However, as with all behavioral measures, such Finnegan scores are fallible; moreover, interrater reliability has often been reported to be poor or substandard. Although the Finnegan scoring system is used to assess opioid and nonopioid withdrawal, shortened or simplified versions of this scoring system have not been widely adopted (Kocherlakota, 2014). Third, examiners’ skills vary. For example, the Finnegan scoring system requires considerable training for reliable use, yet even trained raters have difficulty accurately judging some items, such as the difference between “mild” and “marked” tremors (Jones and Fielder, 2015). Fourth, there are differences in NAS treatment initiation and weaning protocols, because the healthcare provider needs to customize each infant's treatment to reflect withdrawal intensity and gestational period (Kocherlakota, 2014). Additionally, initiation of treatment and weaning of medications will differ depending on the standardized scoring system used and the protocol used (Teague et al., 2015). The current consensus is that the NAS incidence is similar for buprenorphine and methadone, at approximately 50%. Moreover, research indicates that compared with methadone-exposed neonates, buprenorphine-exposed neonates require less morphine to treat NAS, spend less time in the hospital medicated for NAS, and have a shorter hospital stay (Jones et al., 2005, 2010b, 2012).
Methadone and Buprenorphine: Maternal Dose-response Relationships to Neonatal Outcomes
Retrospective studies examining the relationship between methadone dose (and, to a lesser extent, buprenorphine dose) and neonatal outcomes have yielded inconsistent findings (see Jones et al., 2013c, 2014a, for reviews of these 2 lines of research). The need to examine whether there was a relationship between dose and neonatal outcomes was stimulated by the concern that higher methadone doses might harm the fetus and result in more severe NAS. Jones et al. (2013c, 2014a) used MOTHER data and found no relationship between either methadone or buprenorphine dose and peak NAS score, total amount of morphine needed to treat NAS, duration of neonatal hospital stay, duration of pharmacotherapy for NAS, estimated gestational age at delivery, Apgar score at 5 minutes, and neonatal head circumference, length, and weight at birth. These findings on the lack of a link between methadone or buprenorphine dose and NAS extend the results of a meta-analysis (Cleary et al., 2010) that found that the severity of NAS was unrelated to methadone dose, and strongly suggest that the practice of reducing maternal opioid agonist medication to protect the fetus is unwarranted.
Weight-Based Versus Symptom-Based Pharmacotherapy for NAS
Beginning with Finnegan et al.'s (1975) guidance regarding weight-based pharmacotherapy for NAS, treatment for NAS has been weight based with few exceptions (notably the Jones et al., 2010b, MOTHER study). However, pharmacotherapeutic dosing for NAS based on symptom severity may be more efficacious than pharmacotherapeutic dose based on neonatal weight (Jansson et al., 2009). At present, the dosing regimen is thought to be complex, and dependent on both initial assessment of NAS severity and response to treatment.
Methadone and Buprenorphine: NAS Signs and Time Course
Gaalema et al. (2012) compared the NAS signs of methadone-exposed and buprenorphine-exposed infants in the MOTHER study, who had been assessed for 10 days following delivery using the study's modified Finnegan scale (MOTHER NAS Scale [MNS]; Jones et al., 2010b). The authors found that undisturbed tremors and hyperactive Moro reflex occurred significantly more often in the methadone-exposed neonatal group, and nasal stuffiness, sneezing, and loose stools occurred significantly more often in the buprenorphine-exposed neonatal group. The methadone-exposed group had higher mean MNS scores than did the buprenorphine-exposed neonatal group, marked by higher scores on disturbed and undisturbed tremors, hyperactive Moro reflex, excessive irritability, and failure to thrive; sneezing was significantly higher among buprenorphine-exposed neonates. Gaalema et al. (2013) also found that in a secondary data analysis the mean time (hours:minutes, interquartile range) to initiation of pharmacotherapy for buprenorphine-exposed neonates was significantly longer compared with methadone-exposed neonates (71:02, 44:21–96:27 vs 34:12, 21:00–55:41, respectively, P < 0.001), a finding consistent with the MOTHER study and a previous smaller trial (Fischer et al., 2006). The American Academy of Pediatrics recommendation that both groups of neonates be monitored for NAS for a minimum of 5–7 days (120–168 hours) was crafted to ensure that no infant is sent home too early to determine whether NAS treatment is needed (Hudak and Tan, 2012).
Other Factors Affecting NAS
A number of studies have focused on elucidating the factors that exacerbate or minimize NAS. The extent of nicotine use has been found to be a robust factor in increasing NAS expression (eg, Jones et al., 2013b). Furthermore, the presence of selective serotonin reuptake inhibitors and/or benzodiazepines may also exacerbate NAS expression (Kaltenbach et al., 2012).
Rooming-in to Reduce NAS
Recent research suggests that the first-line approach to managing neonates prenatally exposed to 1 or more classes of opioids may be a rooming-in model that minimizes stimulation from outside sources (eg, by using low lighting), maximizes maternal-infant contact, and encourages breastfeeding (eg, Abrahams et al., 2010).
Measurement of NAS
Several studies have attempted to develop alternative measures to the Finnegan scoring system, also referred to as the Neonatal Abstinence Scoring System (NASS). Moreover, many of the measures in clinical use are modifications of the NASS, making comparisons among cohort studies difficult if not impossible. The psychometric properties of both the NASS and the MNS certainly seem deficient (Jones et al., 2016c), suggesting a need to develop new NAS measures. (See Jones and Fielder, 2015, for a review of these measures and the issues in the measurement of NAS.) Research aimed at developing short forms of the NASS and the MNS that are easier to administer consistently has shown promise (eg, Jones et al., 2010a, 2016b).
NAS Medication Treatment Protocol
Paregoric was originally the treatment of choice for NAS; it is found in the initial treatment protocol presented by Finnegan et al. (1975). Diluted tincture of opium was also once popular, but concerns about its high alcohol content and the possibility of its confusion with deodorized tincture of opium (both are commonly abbreviated DTO) led to calls for use of oral morphine sulfate instead. Oral morphine sulfate was found to be as efficacious as diluted tincture of opium in a randomized controlled trial (Langenfeld et al., 2005). Oral morphine use has been complicated by a retrospective review suggesting that methadone may be just as efficacious (Lainwala et al., 2005). Buprenorphine holds promise as a first-line NAS treatment (eg, Kraft et al., 2008, 2011).
Although research indicates that clonidine or phenobarbital may be used as second-line medications for infants with more severe NAS not completely controlled with morphine or methadone (eg, Coyle et al., 2002; Agthe et al., 2009), ongoing research is still trying to determine the safety and efficacy of clonidine (Bada et al., 2015).
Future Research Topics
This RAM literature review highlights the complexity of issues and practices affecting the treatment of pregnant and parenting women for OUD and the concurrent care of their infants and children. Ongoing research on the prenatal, postnatal, and neonatal periods is needed. To that end, the chair of the Expert Panel, Hendrée E. Jones, PhD, a senior author of this article, in collaboration with SAMHSA staff drew up a list of future research topics, presented in Table 4. The selected topics have been the subject of promising but not yet definitive research. Although not exhaustive, the table highlights important areas for future study that might lead to meaningful advances in the care and outcomes of mothers who have OUD and their children.
TABLE 4.
Questions for Future Research
| Domain | Future Research Questions |
| MATERNAL (across all 4 trimesters) | |
| Substance use disorders | What level of substance use is harmful to the mother, fetus, and child (eg, Wright et al., 2016)? |
| What are the potential pretreatment and/or treatment, fetal, neonatal, and child outcomes between women with OUD who misuse prescription opioids and become pregnant compared with women with OUD who use illicit opioids and become pregnant? | |
| What are the best methods for detecting emerging trends in substance use and prenatal exposure to substances (eg, Martin et al., 2015)? | |
| To what extent is genomics testing helpful as a component of OUD identification? If found to be helpful, how should it be used? | |
| What are the best methods for supporting women with OUD who are seeking treatment? | |
| How can structural barriers that inhibit women from seeking, entering, and/or engaging in treatment be overcome? | |
| What are the best ways to treat women for OUD in rural settings across all 4 trimesters (eg, Jumah et al., 2015; Meyer and Phillips, 2015)? | |
| What are the best ways to prevent OUD? What are the unique factors and effective program elements for women? | |
| Which methods of contraception work best for which women with OUD (considering the likelihood of trauma history) and how can they be made more accessible (eg, Terplan et al., 2015)? | |
| Which behavioral interventions (such as contingency management) are most effective for pregnant and parenting women with OUD? What internal and external factors explain differences in effectiveness (eg, type of pharmacotherapy, other maternal variables)? | |
| To what extent can contingency management be implemented in clinical settings to help women across all 4 trimesters improve outcomes (eg, Forray, 2016)? | |
| What are the most cost-effective ways to provide care for women with OUD that will lead to optimal maternal and child outcomes? | |
| What are the best reimbursement structures for promoting engagement of and access, treatment, and optimal outcomes for women with OUD and their children? | |
| For co-occurring health and social issues | What are the best methods to ensure universal hepatitis C and HIV screening and treatment for pregnant women with OUD (eg, Krans et al., 2016a, 2016b)? |
| What are the best methods to identify and address social determinants of health in pregnant and parenting women with OUD? | |
| To what extent does tobacco influence outcomes for mother, fetus, and child in women receiving MAT across all 4 trimesters (eg, Akerman et al., 2015)? | |
| What are the best ways to treat comorbid conditions, including alcohol, benzodiazepine, stimulant, and marijuana use disorders, as well as tobacco use, depression, anxiety, posttraumatic stress disorder, HIV, hepatitis C, and sexually transmitted infections in pregnant women with OUD (eg, Coleman et al., 2015; Caputo et al., 2016; Chisolm and Payne, 2016; Huang et al., 2016; O’Connor et al., 2016)? | |
| What is the relative contribution of multiple risk factors to adverse outcomes? What are the resilience factors most likely to improve these outcomes (eg, Kramlich and Kronk, 2015)? | |
| Screenings | What are the optimal screening tools and procedures to identify other types of SUDs in pregnant women with OUD (eg, Ondersma et al., 2015; Wright et al., 2016)? |
| What are the best ways to treat women of different ages with SUD, and women who become pregnant while being treated with opioids for pain? | |
| What are the most effective tools and procedures for screening for OUD and other health and social issues in integrated care (eg, Goodman, 2015)? | |
| Medication selection, induction, and dose adjustments | |
| How should the optimal opioid agonist therapy be selected for pregnant and parenting women? What patient variables (eg, age, socioeconomic status, race, ethnicity) and community variables (eg, urban, suburban, rural, incarcerated) should be considered? | |
| Which opioid treatment regimen works best for pregnant patients using prescription opioids or heroin (eg, Martin and Finlayson, 2015; Krans et al., 2016a; Noormohammadi et al., 2016)? | |
| What are the best methods for induction onto buprenorphine during pregnancy (eg, Meyer and Phillips, 2015; Jones et al., 2016a)? | |
| What are the best methods for induction onto an optimal dose of methadone during pregnancy (eg, McCarthy et al., 2015)? | |
| To what extent does fetal stress during MAT induction occur and what are the implications of such stress for the child? | |
| What are the best strategies for maintaining a safe, effective dose of MAT over the course of a patient's pregnancy, postpartum period, and breastfeeding period? | |
| To what extent is naltrexone safe and effective for OUD for the maternal-fetal and/or maternal-infant dyad? | |
| Under what circumstances would transition from one form of MAT to another be beneficial to the mother-fetal, mother-infant dyad? | |
| What is the relative safety and efficacy of buprenorphine + naloxone vs buprenorphine or methadone during pregnancy? What is the risk/benefit of transferring a woman from buprenorphine + naloxone to another opioid agonist because of pregnancy? How should such a transition be accomplished (eg, Meyer et al., 2015; Nørgaard et al., 2015; Wiegand et al., 2015; Dooley et al., 2016; Zedler et al., 2016)? | |
| PRENATAL | |
| Medically assisted withdrawal | |
| Under what circumstances is medically assisted withdrawal appropriate for pregnant women and what medication should be used (eg, Dooley et al., 2015; Welle-Strand et al., 2015; Bell et al., 2016)? What accompanying services are required to ensure an optimal outcome for both mother and child? | |
| What are the best methods for identifying women who are most likely to successfully complete medication-assisted withdrawal and maintain abstinence? | |
| Pain relief | |
| What are the optimal pharmacological and nonpharmacological approaches to providing pain relief during pregnancy, labor, delivery, and the postpartum period for women receiving MAT? | |
| Which pain management protocols are most effective for reducing pain for which women with OUD during labor, delivery, and the postpartum period? | |
| NEONATAL | |
| Screening for the presence of prenatal exposure to substances | What are the best biological matrices and analytical methods for accurately determining neonatal exposure to opioids and other substances (eg, Joya et al., 2015; Kyle et al., 2015)? |
| What are the best protocols to support the mother-child dyad and ensure the safety of child and mother? | |
| What are the best strategies to help women navigate legal issues and ensure that appropriate consent occurs? | |
| What are the extent and impact of polysubstance use on opioid exposure in pregnancy and NAS? In particular, what are the long-term effects of prenatal exposure to opioids, as compared with exposure to other substances or pharmaceuticals? Such research needs to be carefully controlled for social, familial, and environmental risk and protective factors encountered during childhood. | |
| Screening and assessment of NAS | What are the most psychometrically sound screening and assessment measures of NAS for premature, term, and older infants (Jones and Fielder, 2015)? |
| What are the best methods and tools for identifying, assessing, and treating possible comorbid withdrawal from other substances such as benzodiazepines, nicotine, or alcohol? | |
| What degree (amount and timing) of exposure to prescription opioids for pain should be considered a risk for NAS (eg, Desai et al., 2015)? | |
| How efficient, valid, and reliable are the new short forms of the MNS (eg, Jones et al., 2010a; Jones et al., 2016b)? Further research is needed. | |
| Treatment of infants for NAS | What is the safest, most effective protocol for using nonpharmacological NAS treatments that will also minimize the ongoing medication exposure of infants with NAS (eg, Patrick et al., 2016)? |
| What are the best items to include in the most accurate and sensitive measures of NAS (eg, Jones et al., 2010a; Jones et al., 2016b)? | |
| Which medications should be used as first-line therapy or considered second-line options for the treatment of NAS, and for which infants (eg, Nayeri et al., 2015; Young et al., 2015)? | |
| What are the best protocols for dosing and weaning neonates from NAS medications (eg, Hall et al., 2015b; Jones and Fielder, 2015; Patrick et al., 2016)? | |
| What are the pharmacokinetics and dynamics of NAS medications? How do they differ by medication and age of infant (Hall et al., 2015a; Ng et al., 2015; Wiles et al., 2015; Johnson et al., 2016)? | |
| What are the effects of co-occurring exposures to substances such as alcohol and other stressors on NAS severity (eg, Kreitinger et al., 2016; Popova et al., 2016)? | |
| To what extent do maternal or infant factors alone or in combination exacerbate and mitigate NAS and its severity (such as tobacco use, prematurity. and genetics) (eg, Ruwanpathirana et al., 2015; Stover and Davis, 2015)? | |
| What medication might be more efficacious for long-acting vs short-acting opioids when treating infants for NAS? | |
| Would neonates of mothers maintained on an opioid agonist medication respond better to that same medication, or would oral morphine or another medication be a better choice? | |
| What are optimal pharmacotherapeutic dosings for NAS based on symptom severity? | |
| What are the most cost-effective ways to produce the best outcomes and care for infants with NAS (eg, Brandt et al., 2015)? | |
| POSTNATAL | |
| Relapses | What are the factors and predictors for transitioning to another medication a new mother who was stable on MAT and relapses (Forray et al., 2015)? |
| Breastfeeding | How should breastfeeding amount (eg, exclusivity or supplemented with formula) and duration be differentiated by OUD treatment medication (Tsai and Doan, 2016)? |
| What are the best parameters and optimal duration for breastfeeding (eg, expressed, supplemented with formula, standard) based on OUD treatment medication (Tsai and Doan, 2016)? | |
| To what extent is breastfeeding safe while the mother is using marijuana and/or other substances (eg, Chomchai et al., 2016)? | |
| How can the representation of pregnant and breastfeeding women best be increased in clinical trials (Scaffidi et al., 2016)? | |
| What are the most efficacious interventions to successfully introduce, and then maintain, breastfeeding in opioid-agonist-maintained new mothers? | |
| Mother-child dyad | |
| What parenting and recovery supports are most beneficial to the maternal-child dyad (eg, Giles et al., 2016)? What family, maternal, child, or community variables need to be considered? What is the optimal frequency and duration of delivery for such services? What is the optimal role of peer-support services? | |
| What are the modifiable maternal variables that can mitigate the risk of NAS for infants of women who, for medical reasons, require opioid therapy during pregnancy? Such variables include tobacco cessation and in-home support services. | |
| Which dyads will benefit from rooming in? Which dyads will benefit from outpatient treatment with medication for NAS (eg, Holmes et al., 2016)? | |
| What in-home early interventions or developmental assessments provide the greatest benefit to the infant? What family, maternal, child, or community variables need to be considered? What is the optimal frequency and duration of delivery for such services? | |
| What is the safest and most effective strategy for providing ongoing NAS medication posthospital discharge? | |
| How can sudden infant death syndrome (SIDS) and other causes of infant mortality be reduced in infants prenatally exposed to substances (Cohen et al., 2015; Ali et al., 2016)? | |
| To what extent does a prenatal opioid exposure environment lead to changes in fetal development and later developmental consequences (eg, Beckwith and Burke, 2015; Kivistö et al., 2015; Konijnenberg and Melinder, 2015; Pearson et al., 2015; Whitham et al., 2015; Jones et al., 2016a)? |
MAT, medication for addiction treatment; MNS, NASS or the MOTHER NAS Scale; NAS, neonatal abstinence syndrome; OUD, opioid use disorder; SUD, substance use disorder.
CONCLUSIONS
The number of women aged between 15 and 44 who reported past-month nonmedical use of psychotherapeutics, OxyContin (oxycodone) type, and the number of women aged between 15 and 44 who reported past-month heroin use increased from 2011–2012 to 2013–2014 (CBHSQ, 2015a, Table 6.71A). In addition, the prevalence of OUD during pregnancy more than doubled between 1998 and 2011, to 4 per 1000 deliveries (Maeda et al., 2014). Given that women with OUD have a higher frequency of additional risk factors for adverse pregnancy outcomes than do pregnant women who do not use opioids, evidence-based clinical guidance on the treatment of these women and their children is needed. The present article, developed as part of a RAM process, serves as the basis for a series of recommendations for researchers and policymakers in the areas of OUD and pregnant women whose opioid exposure also exposed infants in utero. Healthcare providers interested in reviewing the evidence for treating such women and their infants and children may also find this review useful. This work supports and extends the ASAM National Practice Guideline for the Use of Medications in the Treatment of Addiction Involving Opioid Use, which includes guidance on treating pregnant women (Kampman and Jarvis, 2015).
Several recent reviews have similarly discussed use of prescription opioids during pregnancy and birth outcomes. Zedler et al. (2016) found evidence that buprenorphine treatment for OUD during pregnancy demonstrates lower risk of preterm birth, greater birth weight, and larger head circumference compared with methadone treatment. Yazdy et al. (2015) found evidence that head circumference and birth length have no association with opioid use. (The present status of research does not indicate that opioid agonist pharmacotherapy during pregnancy exposes the fetus to greater teratological risk than found in the non-opioid-exposed fetus; however, to date, no research has been reported indicating that MAT during pregnancy is associated with birth defects.) This RAM literature review is broader in scope than these recent reviews and makes a significant contribution to the literature by providing substantial recommendations for future research.
The present article summarized the results from 75 studies that focused on prenatal and postnatal OUD treatment of women and their prenatally opioid-exposed infants and children. The collective literature review points to several conclusions:
Although withdrawal from opioids to an opioid-free state is possible during pregnancy, relapse rates are high and repeated cycles of intoxication and withdrawal are associated with possible adverse effects.
The accepted treatment for OUD during pregnancy is long-acting opioid agonist MAT that includes methadone or buprenorphine provided within the context of a comprehensive program of obstetrical care and behavioral intervention.
For the fetus, steady states of buprenorphine appear to have a less sedating effect than single daily dosing of methadone. Split dosing of methadone in the third trimester may also have a less suppressive effect on the fetus. At this time, the postnatal and longer-term effects of suppression of fetal parameters remain unknown.
As gestation increases, higher doses of methadone and possibly buprenorphine appear to be needed.
Postpartum women with OUD may need greater amounts of pain relief medication compared with women without such opioid experience.
Breastfeeding among women not using other substances and maintained on methadone or buprenorphine can encourage and promote maternal-infant bonding, and likely have mitigating effects on NAS severity.
NAS severity may be less with buprenorphine than with methadone; however, other factors such as maternal tobacco use, maternal benzodiazepine use, dyad genetics, NAS medication regimens, and hospital protocols determining where infants reside (eg, neonatal intensive care unit or rooming-in) may alter this relationship.
Although NAS has been an issue of focus, it is an identifiable and treatable condition that is only one aspect of the complete risk/benefit ratio decision for any patient and her provider to make during pregnancy. For a sustained recovery, the maternal-fetus/maternal-infant dyad must be considered as a whole and in the context of the dyad's risk and protective life factors.
The summary of research found in the present article must be considered within the context of its limitations. These include the fact that different literature search methods may find different articles and possibly lead to different conclusions. Several studies may have limited generalizability to the US population, in large part because of cultural and health system differences. Furthermore, the descriptive and correlational designs of some studies may have resulted in several biases (eg, selection bias weakens the study results, confounding psychosocial factors).
Although this literature review identified evidence from recent clinical research studies providing support for the Guide, substantial questions for future research, as noted in Table 4, still remain. Further research that focuses on those questions is likely to have an impact on the treatment of pregnant and parenting women and their infants and children.
In conclusion, both methadone and buprenorphine provide effective treatment for OUD before, during, and after pregnancy; however, neither medication is a “cure.” For the mother, both medications offer benefits to support behavioral change. For the fetus, buprenorphine appears less sedating than methadone. For the neonate, collective randomized controlled trials, and prospective and retrospective data, show a less severe NAS for buprenorphine than methadone exposure in utero. However, NAS is only one aspect of the complete risk/benefit ratio decision that must be made. Any MAT plan for OUD must be developed in the context of a comprehensive care program that is supportive of and responsive to women and the maternal-fetus/maternal-infant dyad.
Supplementary Material
Supplementary Material
Supplementary Material
Acknowledgments
CDR Sidney Hairston, MSN, RN, Public Health Advisor, Division of Pharmacologic Therapies, CSAT, SAMHSA, HHS, and LCDR Brandon T. Johnson, MBA, Regulatory Compliance Officer, DPT, CSAT, SAMHSA, HHS, served as the Contracting Officer's Representatives.
The authors are grateful to the Federal Steering Committee and Expert Panel members for their input on articles to include.
Federal Steering Committee members: Alexis Geier-Horan, MPP (Assistant Secretary for Planning and Evaluation); Maureen Buell (Tenure—May 2015), Alison Leukefeld, PhD (Tenure—May 2015); and Alix McLearen, PhD (Bureau of Prisons); Andreea Creanga, MD, PhD, and Peggy Honein, PhD, MPH (Centers for Disease Control and Prevention); Meena Abraham, DrPH, MPH (Centers for Medicare & Medicaid Services); Major Robert Bush, MD (Department of Defense); Pamela Horn, MD, and Leyla Sahin, MD, FACOG (Food and Drug Administration); Laurie Zephyrin, MD, MPH, MBA, FACOG (Department of Veterans Affairs); Beth Collins-Sharp, PhD, RN, FAAN (Tenure—June 2015), and Jessica Tytel, MPH (Health and Human Services Office on Women's Health); Hani Atrash, MD, MPH, and John McGovern, MGA (Health Resources and Services Administration); Beverly Cotton, MSN, SANE-A, SANE-P (Indian Health Service); Cheryl Boyce, PhD, and Wilson Compton, MD, MPE (National Institute on Drug Abuse); Christine Cichetti (Office of the Assistant Secretary for Health); Cecelia Spitznas, PhD (The White House Office of National Drug Control Policy).
Expert Panel members: Shahid Ali, MD, MBBS (Meharry Medical College Rainbow Program); Diana Coffa, MD (Department of Family and Community Medicine, University of California, San Francisco School of Medicine); Deborah Finnell, DNS, PMHNP-BC, CARN-AP, FAAN (Department of Acute and Chronic Care, Johns Hopkins University School of Nursing); Lauren Jansson, MD (Center for Addiction and Pregnancy, Johns Hopkins Bayview Medical Center and Pediatrics, Johns Hopkins University School of Medicine); Hendrée E. Jones, PhD (Chair, University of North Carolina at Chapel Hill School of Medicine Horizons Program and Department of Obstetrics and Gynecology, University of North Carolina); Marjorie Meyer, MD, FACOG (Maternal-Fetal Medicine Division, University of Vermont College of Medicine); Stephen Patrick, MD, MPH, MS (Department of Pediatrics, Vanderbilt University School of Medicine); Charles Schauberger, MD, MS, FACOG, CPE (Gundersen Health System, La Crosse, Wisconsin); Mishka Terplan, MD, MPH, FACOG (Behavioral Health System Baltimore and Department of Epidemiology and Public Health, University of Maryland School of Medicine).
Scientific Advisors: Sonia Hernandez-Diaz, MD, DrPH (Department of Epidemiology, and Pharmacoepidemiology Program, Harvard School of Public Health); Karol Kaltenbach, PhD (Emeritus Professor of Pediatrics, Sidney Kimmel Medical College, Thomas Jefferson University); and Walter Ling, MD (Psychiatry and Biobehavioral Sciences, and Integrated Substance Abuse Program, UCLA David Geffen School of Medicine).
Kea Turner, MPH, MA, and McLean Pollock, PhD, MSW, LCSW, of the University of North Carolina at Chapel Hill contributed to the production of the Abstraction Table.
Footnotes
This article was prepared for the Center for Substance Abuse Treatment (CSAT), Substance Abuse and Mental Health Services Administration (SAMHSA), US Department of Health and Human Services (HHS), by JBS International, Inc., under contract numbers HHSS283200700003I/HHSS28342007T and HHSS283201200002I/HHSS28342009T.
The authors report no conflicts of interest.
REFERENCES
- Abdel-Latif ME, Pinner J, Clews S, et al. Effects of breast milk on the severity and outcome of neonatal abstinence syndrome among infants of drug-dependent mothers. Pediatrics 2006; 117:e1163–e1169. [DOI] [PubMed] [Google Scholar]
- Abrahams RR, MacKay-Dunn MH, Nevmerjitskaia V, et al. An evaluation of rooming-in among substance-exposed newborns in British Columbia. J Obstet Gynaecol Can 2010; 32:866–871. [DOI] [PubMed] [Google Scholar]
- Agthe AG, Kim GR, Mathias KB, et al. Clonidine as an adjunct therapy to opioids for neonatal abstinence syndrome: a randomized, controlled trial. Pediatrics 2009; 123:e849–e856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akerman SC, Brunette MF, Green AI, et al. Treating tobacco use disorder in pregnant women in medication-assisted treatment for an opioid use disorder: a systematic review. J Subst Abuse Treat 2015; 52:40–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alford DP, Compton P, Samet JH. Acute pain management for patients receiving maintenance methadone or buprenorphine therapy. Ann Intern Med 2006; 144:127–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali K, Rossor T, Bhat R, et al. Antenatal substance misuse and smoking and newborn hypoxic challenge response. Arch Dis Child Fetal Neonatal Ed 2016; 101:F143–F148. [DOI] [PubMed] [Google Scholar]
- Bada HS, Sithisarn T, Gibson J, et al. Morphine versus clonidine for neonatal abstinence syndrome. Pediatrics 2015; 135:e383–e391. [DOI] [PubMed] [Google Scholar]
- Bastian JR, Chen H, Zhang H, et al. Dose-adjusted plasma concentrations of sublingual buprenorphine are lower during than after pregnancy. Am J Obstet Gynecol 2016; 216:64.e1–64.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beckwith AM, Burke SA. Identification of early developmental deficits in infants with prenatal heroin, methadone, and other opioid exposure. Clin Pediatr (Phila) 2015; 54:328–335. [DOI] [PubMed] [Google Scholar]
- Bell J, Towers CV, Hennessy MD, et al. Detoxification from opiate drugs during pregnancy. Am J Obstet Gynecol 2016; 215:374e1–374e6. [DOI] [PubMed] [Google Scholar]
- Binder T, Vavrinková B. Prospective randomised comparative study of the effect of buprenorphine, methadone and heroin on the course of pregnancy, birthweight of newborns, early postpartum adaptation and course of the neonatal abstinence syndrome (NAS) in women followed up in the outpatient department. Neuro Endocrinol Lett 2008; 29:80–86. [PubMed] [Google Scholar]
- Bogen DL, Perel JM, Helsel JC, et al. Pharmacologic evidence to support clinical decision making for peripartum methadone treatment. Psychopharmacology (Berl) 2013; 225:441–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandt L, Fischberger S, Unger A, et al. Neonatal abstinence syndrome after intrauterine opioid exposure: standards, cost-effectiveness of treatment and maternal rights. Heroin Addict Relat Clin Problems 2015; 17:35–44. [Google Scholar]
- Buckley V, Razaghi A, Haber P. Predictors of neonatal outcomes amongst a methadone- and/or heroin-dependent population referred to a multidisciplinary Perinatal and Family Drug Health Service. Aust N Z J Obstet Gynaecol 2013; 53:464–470. [DOI] [PubMed] [Google Scholar]
- Caputo C, Wood E, Jabbour L. Impact of fetal alcohol exposure on body systems: a systematic review. Birth Defects Res C Embryo Today 2016; 108:174–180. [DOI] [PubMed] [Google Scholar]
- Cassidy B, Cyna AM. Challenges that opioid-dependent women present to the obstetric anaesthetist. Anaesth Intensive Care 2004; 32:494–501. [DOI] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. 2014 National Survey on Drug Use and Health: detailed tables. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2015. a. Available at: http://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs2014/NSDUH-DetTabs2014.pdf Accessed October 28, 2016. [Google Scholar]
- Center for Behavioral Health Statistics and Quality. Behavioral Health Trends in the United States: Results From the 2014 National Survey on Drug Use and Health. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2015b. HHS Publication No. (SMA) 15-4927, NSDUH Series H-50; Available at: http://www.samhsa.gov/data/sites/default/files/NSDUH-FRR1-2014/NSDUH-FRR1-2014.pdf Accessed October 28, 2016. [Google Scholar]
- Chisolm MS, Payne JL. Management of psychotropic drugs during pregnancy. BMJ 2016; 532:h5918. [DOI] [PubMed] [Google Scholar]
- Chomchai C, Chomchai S, Kitsommart R. Transfer of methamphetamine (MA) into breast milk and urine of postpartum women who smoked MA tablets during pregnancy: implications for initiation of breastfeeding. J Hum Lact 2016; 32:333–339. [DOI] [PubMed] [Google Scholar]
- Cleary BJ, Donnelly J, Strawbridge J, et al. Methadone dose and neonatal abstinence syndrome—systematic review and meta-analysis. Addiction 2010; 105:2071–2084. [DOI] [PubMed] [Google Scholar]
- Cohen MC, Morley SR, Coombs RC. Maternal use of methadone and risk of sudden neonatal death. Acta Paediatr 2015; 104:883–887. [DOI] [PubMed] [Google Scholar]
- Coleman T, Chamberlain C, Davey M-A, et al. Pharmacological interventions for promoting smoking cessation during pregnancy. Cochrane Database Syst Rev 2015. CD010078. [DOI] [PubMed] [Google Scholar]
- Concheiro M, Jones HE, Johnson RE, et al. Maternal buprenorphine dose, placenta buprenorphine, and metabolite concentrations and neonatal outcomes. Ther Drug Monit 2010; 32:206–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyle MG, Ferguson A, Lagasse L, et al. Diluted tincture of opium (DTO) and phenobarbital versus DTO alone for neonatal opiate withdrawal in term infants. J Pediatr 2002; 140:561–564. [DOI] [PubMed] [Google Scholar]
- de Castro A, Jones HE, Johnson RE, et al. Maternal methadone dose, placental methadone concentrations, and neonatal outcomes. Clin Chem 2011; 57:449–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Debelak K, Morrone WR, O’Grady KE, et al. Buprenorphine + naloxone in the treatment of opioid dependence during pregnancy—initial patient care and outcome data. Am J Addict 2013; 22:252–254. [DOI] [PubMed] [Google Scholar]
- Desai RJ, Huybrechts KF, Hernandez-Diaz S, et al. Exposure to prescription opioid analgesics in utero and risk of neonatal abstinence syndrome: population based cohort study. BMJ 2015; 350:h2102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dooley R, Dooley J, Antone I, et al. Narcotic tapering in pregnancy using long-acting morphine: an 18-month prospective cohort study in northwestern Ontario. Can Fam Physician 2015; 61:e88–e95. [PMC free article] [PubMed] [Google Scholar]
- Dooley J, Gerber-Finn L, Antone I, et al. Buprenorphine-naloxone use in pregnancy for treatment of opioid dependence: retrospective cohort study of 30 patients. Can Fam Physician 2016; 62:e194–e200. [Google Scholar]
- Farmer CM, Lindsay D, Williams J, et al. Practice guidance for buprenorphine for the treatment of opioid use disorders: results of an expert panel process. Subst Abus 2015; 36:209–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finnegan LP, Connaughton JF, Jr, Kron RE, et al. Neonatal abstinence syndrome: assessment and management. Addict Dis 1975; 2:141–158. [PubMed] [Google Scholar]
- Fischer G, Ortner R, Rohrmeister K, et al. Methadone versus buprenorphine in pregnant addicts: a double-blind, double-dummy comparison study. Addiction 2006; 101:275–281. [DOI] [PubMed] [Google Scholar]
- Fitch K, Bernstein SJ, Aguilar MD, et al. The RAND/UCLA Appropriateness Method User's Manual. Santa Monica, CA: RAND Corporation; 2001. [Google Scholar]
- Forray A. Substance use during pregnancy. F1000Research 2016; 5:887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forray A, Merry B, Lin H, et al. Perinatal substance use: a prospective evaluation of abstinence and relapse. Drug Alcohol Depend 2015; 150:147–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaalema DE, Heil SH, Badger GJ, et al. Time to initiation of treatment for neonatal abstinence syndrome in neonates exposed in utero to buprenorphine or methadone. Drug Alcohol Depend 2013; 133:266–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaalema DE, Scott TL, Heil SH, et al. Differences in the profile of neonatal abstinence syndrome signs in methadone-versus buprenorphine-exposed neonates. Addiction 2012; 107 suppl 1:53–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giles AC, Ren D, Founds S. Development, implementation, and evaluation of a pilot parenting educational intervention in a pregnancy buprenorphine clinic. Nurs Womens Health 2016; 20:258–267. [DOI] [PubMed] [Google Scholar]
- Goodman D. Improving access to maternity care for women with opioid use disorders: colocation of midwifery services at an addiction treatment program. J Midwifery Womens Health 2015; 60:706–712. [DOI] [PubMed] [Google Scholar]
- Hall ES, Meinzen-Derr J, Wexelblatt SL. Cohort analysis of a pharmacokinetic-modeled methadone weaning optimization for neonatal abstinence syndrome. J Pediatr 2015; 167:1221.e1–1225.e1. [DOI] [PubMed] [Google Scholar]
- Hall ES, Wexelblatt SL, Crowley M, et al. Implementation of a neonatal abstinence syndrome weaning protocol: a multicenter cohort study. Pediatrics 2015; 136:e803–e810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes AV, Atwood EC, Whalen B, et al. Rooming-in to treat neonatal abstinence syndrome: improved family-centered care at lower cost. Pediatrics 2016; 137:e1–e9. [DOI] [PubMed] [Google Scholar]
- Huang J, Zhu T, Qu Y, et al. Prenatal, perinatal and neonatal risk factors for intellectual disability: a systemic review and meta-analysis. PLoS One 2016; 11:e0153655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudak ML, Tan RC. Committee on Drugs, Committee on Fetus and Newborn. American Academy of Pediatrics. Clinical report: neonatal drug withdrawal. Pediatrics 2012; 129:e540–e560. [DOI] [PubMed] [Google Scholar]
- Hulse GK, Milne E, English DR, et al. The relationship between maternal use of heroin and methadone and infant birth weight. Addiction 1997; 92:1571–1579. [PubMed] [Google Scholar]
- Ilett KF, Hackett LP, Gower S, et al. Estimated dose exposure of the neonate to buprenorphine and its metabolite norbuprenorphine via breastmilk during maternal buprenorphine substitution treatment. Breastfeed Med 2012; 7:269–274. [DOI] [PubMed] [Google Scholar]
- Jansson LM, Choo R, Velez ML, et al. Methadone maintenance and breastfeeding in the neonatal period. Pediatrics 2008; 121:106–114. [DOI] [PubMed] [Google Scholar]
- Jansson LM, Choo R, Velez ML, et al. Methadone maintenance and long-term lactation. Breastfeed Med 2008; 3:34–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jansson LM, DiPietro JA, Elko A, et al. Pregnancies exposed to methadone, methadone and other illicit substances, and poly-drugs without methadone: a comparison of fetal neurobehaviors and infant outcomes. Drug Alcohol Depend 2012; 122:213–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jansson LM, DiPietro JA, Velez M, et al. Fetal neurobehavioral effects of exposure to methadone or buprenorphine. Neurotoxicol Teratol 2011; 33:240–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jansson LM, Velez M, Harrow C. The opioid-exposed newborn: assessment and pharmacologic management. J Opioid Manag 2009; 5:47–55. [PMC free article] [PubMed] [Google Scholar]
- Johnson RE, Jones HE, Jasinski DR, et al. Buprenorphine treatment of pregnant opioid-dependent women: maternal and neonatal outcomes. Drug Alcohol Depend 2001; 63:97–103. [DOI] [PubMed] [Google Scholar]
- Johnson TN, Jamei M, Rowland-Yeo K. How does the in vivo biliary elimination of drugs change with age? Evidence from in vitro and clinical data using a systems pharmacology approach. Drug Metab Dispos 2016; 44:1090–1098. [DOI] [PubMed] [Google Scholar]
- Jones HE, Chisolm MS, Jansson LM, et al. Naltrexone in the treatment of opioid-dependent pregnant women: common ground. Addiction 2013; 108:255–256. [DOI] [PubMed] [Google Scholar]
- Jones HE, Dengler E, Garrison A, et al. Neonatal outcomes and their relationship to maternal buprenorphine dose during pregnancy. Drug Alcohol Depend 2014; 134:414–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones HE, Deppen K, Hudak ML, et al. Clinical care for opioid-using pregnant and postpartum women: the role of obstetric providers. Am J Obstet Gynecol 2014; 210:302–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones HE, Fielder A. Neonatal abstinence syndrome: historical perspective, current focus, future directions. Prev Med (Baltim) 2015; 80:12–17. [DOI] [PubMed] [Google Scholar]
- Jones HE, Harrow C, O’Grady KE, et al. Neonatal abstinence scores in opioid-exposed and nonexposed neonates: a blinded comparison. J Opioid Manag 2010; 6:409–413. [DOI] [PubMed] [Google Scholar]
- Jones HE, Heil SH, Baewert A, et al. Buprenorphine treatment of opioid-dependent pregnant women: a comprehensive review. Addiction 2012; 107 suppl 1:5–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones HE, Heil SH, Tuten M, et al. Cigarette smoking in opioid-dependent pregnant women: neonatal and maternal outcomes. Drug Alcohol Depend 2013; 131:271–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones HE, Johnson RE, Jasinski DR, et al. Buprenorphine versus methadone in the treatment of pregnant opioid-dependent patients: effects on the neonatal abstinence syndrome. Drug Alcohol Depend 2005; 79:1–10. [DOI] [PubMed] [Google Scholar]
- Jones HE, Jansson LM, O’Grady KE, et al. The relationship between maternal methadone dose at delivery and neonatal outcome: methodological and design considerations. Neurotoxicol Teratol 2013; 39:110–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones HE, Johnson RE, O’Grady KE, Milio L, et al. Dosing adjustments in postpartum patients maintained on buprenorphine or methadone. J Addict Med 2008; 2:103–107. [DOI] [PubMed] [Google Scholar]
- Jones HE, Kaltenbach K, Heil SH, et al. Neonatal abstinence syndrome after methadone or buprenorphine exposure. N Engl J Med 2010; 363:2320–2331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones HE, Kaltenbach K, Johnson E, et al. Neonatal abstinence syndrome: presentation and treatment considerations. J Addict Med 2016; 10:224–228. [DOI] [PubMed] [Google Scholar]
- Jones HE, O’Grady K, Dahne J, et al. Management of acute postpartum pain in patients maintained on methadone or buprenorphine during pregnancy. Am J Drug Alcohol Abus 2009; 35:151–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones HE, O’Grady KE, Malfi D, et al. Methadone maintenance vs. methadone taper during pregnancy: maternal and neonatal outcomes. Am J Addict 2008; 17:372–386. [DOI] [PubMed] [Google Scholar]
- Jones HE, Seashore C, Johnson E, et al. Psychometric assessment of the Neonatal Abstinence Scoring System and the MOTHER NAS Scale. Am J Addict 2016; 25:370–373. [DOI] [PubMed] [Google Scholar]
- Jones HE, Seashore C, Johnson E, et al. Measurement of neonatal abstinence syndrome: evaluation of short forms. J Opioid Manag 2016; 12:19–23. [DOI] [PubMed] [Google Scholar]
- Joya X, Pacifici R, Salat-Batlle J, et al. Maternal and neonatal hair and breast milk in the assessment of perinatal exposure to drugs of abuse. Bioanalysis 2015; 7:1273–1297. [DOI] [PubMed] [Google Scholar]
- Jumah NA, Graves L, Kahan M. The management of opioid dependence during pregnancy in rural and remote settings. CMAJ 2015; 187:E41–E46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kakko J, Heilig M, Sarman I. Buprenorphine and methadone treatment of opiate dependence during pregnancy: comparison of fetal growth and neonatal outcomes in two consecutive case series. Drug Alcohol Depend 2008; 96:69–78. [DOI] [PubMed] [Google Scholar]
- Kaltenbach K, Berghella V, Finnegan L. Opioid dependence during pregnancy: effects and management. Obstet Gynecol Clin North Am 1998; 25:139–151. [DOI] [PubMed] [Google Scholar]
- Kaltenbach K, Holbrook AM, Coyle MG, et al. Predicting treatment for neonatal abstinence syndrome in infants born to women maintained on opioid agonist medication. Addiction 2012; 107 suppl 1:45–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kampman K, Jarvis M. American Society of Addiction Medicine (ASAM) national Practice Guideline for the use of medications in the treatment of addiction involving opioid use. J Addict Med 2015; 9:358–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly LE, Rieder MJ, Bridgman-Acker K, et al. Are infants exposed to methadone in utero at an increased risk for mortality? J Popul Ther Clin Pharmacol 2012; 19:e160–e165. [PubMed] [Google Scholar]
- Kivistö K, Tupola S, Kivitie-Kallio S. Prenatally buprenorphine-exposed children: health to 3 years of age. Eur J Pediatr 2015; 174:1525–1533. [DOI] [PubMed] [Google Scholar]
- Kocherlakota P. Neonatal abstinence syndrome. Pediatrics 2014; 134:e547–e561. [DOI] [PubMed] [Google Scholar]
- Konijnenberg C, Melinder A. Visual selective attention is impaired in children prenatally exposed to opioid agonist medication. Eur Addict Res 2015; 21:63–70. [DOI] [PubMed] [Google Scholar]
- Kraft WK, Dysart K, Greenspan JS, et al. Revised dose schema of sublingual buprenorphine in the treatment of the neonatal opioid abstinence syndrome. Addiction 2011; 106:574–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraft WK, Gibson E, Dysart K, et al. Sublingual buprenorphine for treatment of neonatal abstinence syndrome: a randomized trial. Pediatrics 2008; 122:e601–e607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramlich D, Kronk R. Relational care for perinatal substance use: a systematic review. MCN Am J Matern Child Nurs 2015; 40:320–326. [DOI] [PubMed] [Google Scholar]
- Krans EE, Bogen D, Richardson G, et al. Factors associated with buprenorphine versus methadone use in pregnancy. Subst Abus 2016; 37:550–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krans EE, Zickmund SL, Rustgi VK, et al. Screening and evaluation of hepatitis C virus infection in pregnant women on opioid maintenance therapy: a retrospective cohort study. Subst Abus 2016; 37:88–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreitinger C, Gutierrez H, Hamidovic A, et al. The effect of prenatal alcohol co-exposure on neonatal abstinence syndrome in infants born to mothers in opioid maintenance treatment. J Matern Fetal Neonatal Med 2016; 29:783–788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kyle AR, Carmical J, Shah D, et al. UHPLC-MS/MS quantification of buprenorphine, norbuprenorphine, methadone, and glucuronide conjugates in umbilical cord plasma. Biomed Chromatogr 2015; 29:1567–1574. [DOI] [PubMed] [Google Scholar]
- Lainwala S, Brown ER, Weinschenk NP, et al. A retrospective study of length of hospital stay in infants treated for neonatal abstinence syndrome with methadone versus oral morphine preparations. Adv Neonatal Care 2005; 5:265–272. [DOI] [PubMed] [Google Scholar]
- Langenfeld S, Birkenfeld L, Herkenrath P, et al. Therapy of the neonatal abstinence syndrome with tincture of opium or morphine drops. Drug Alcohol Depend 2005; 77:31–36. [DOI] [PubMed] [Google Scholar]
- Lund IO, Fitzsimons H, Tuten M, et al. Comparing methadone and buprenorphine maintenance with methadone-assisted withdrawal for the treatment of opioid dependence during pregnancy: maternal and neonatal outcomes. Subst Abuse Rehabil 2012; 3 suppl 1:17–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maeda A, Bateman BT, Clancy CR, et al. Opioid abuse and dependence during pregnancy: temporal trends and obstetrical outcomes. Anesthesiology 2014; 121:1158–1165. [DOI] [PubMed] [Google Scholar]
- Malpas TJ, Darlow BA. Neonatal abstinence syndrome following abrupt cessation of breastfeeding. N Z Med J 1080; 112:12–13. [PubMed] [Google Scholar]
- Martin CE, Mak C, Miller C, et al. Trends in drug-exposed deliveries from 2002 to 2009. Addict Disord Their Treat 2015; 14:61–69. [Google Scholar]
- Martin PR, Finlayson AJR. Opioid use disorder during pregnancy in Tennessee: expediency vs. science. Am J Drug Alcohol Abuse 2015; 41:367–370. [DOI] [PubMed] [Google Scholar]
- Mattick RP, Breen C, Kimber J, et al. Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database Syst Rev 2009. CD002209. [DOI] [PubMed] [Google Scholar]
- McCarthy JJ, Leamon MH, Willits NH, et al. The effect of methadone dose regimen on neonatal abstinence syndrome. J Addict Med 2015; 9:105–110. [DOI] [PubMed] [Google Scholar]
- Meyer MC, Johnston AM, Crocker AM, et al. Methadone and buprenorphine for opioid dependence during pregnancy: a retrospective cohort study. J Addict Med 2015; 9:81–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer M, Paranya G, Norris AK, et al. Intrapartum and postpartum analgesia for women maintained on buprenorphine during pregnancy. Eur J Pain 2010; 14:939–943. [DOI] [PubMed] [Google Scholar]
- Meyer M, Phillips J. Caring for pregnant opioid abusers in Vermont: a potential model for non-urban areas. Prev Med (Baltim) 2015; 80:18–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer M, Wagner K, Benvenuto A, et al. Intrapartum and postpartum analgesia for women maintained on methadone during pregnancy. Obstet Gynecol 2007; 110 (2 pt 1):261–266. [DOI] [PubMed] [Google Scholar]
- Nayeri F, Sheikh M, Kalani M, et al. Phenobarbital versus morphine in the management of neonatal abstinence syndrome, a randomized control trial. BMC Pediatr 2015; 15:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng CM, Dombrowsky E, Lin H, et al. Population pharmacokinetic model of sublingual buprenorphine in neonatal abstinence syndrome. Pharmacotherapy 2015; 35:670–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noormohammadi A, Forinash A, Yancey A, et al. Buprenorphine versus methadone for opioid dependence in pregnancy. Ann Pharmacother 2016; 50:666–672. [DOI] [PubMed] [Google Scholar]
- Nørgaard M, Nielsson MS, Heide-Jørgensen U. Birth and neonatal outcomes following opioid use in pregnancy: a Danish population-based study. Subst Abuse 2015; 9 suppl 2:5–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor AB, O’Brien L, Alto WA, et al. Does concurrent in utero exposure to buprenorphine and antidepressant medications influence the course of neonatal abstinence syndrome? J Matern Fetal Neonatal Med 2016; 29:112–114. [DOI] [PubMed] [Google Scholar]
- Ondersma SJ, Beatty JR, Svikis DS, et al. Computer-delivered screening and brief intervention for alcohol use in pregnancy: a pilot randomized trial. Alcohol Clin Exp Res 2015; 39:1219–1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pace CA, Kaminetzky LB, Winter M, et al. Postpartum changes in methadone maintenance dose. J Subst Abuse Treat 2014; 47:229–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick SW, Davis MM, Lehmann CU, et al. Increasing incidence and geographic distribution of neonatal abstinence syndrome: United States 2009 to 2012. J Perinatol 2015; 35:650–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick SW, Schumacher RE, Benneyworth BD, et al. Neonatal abstinence syndrome and associated health care expenditures: United States, 2000–2009. JAMA 2012; 307:1934–1940. [DOI] [PubMed] [Google Scholar]
- Patrick SW, Schumacher RE, Horbar JD, et al. Improving care for neonatal abstinence syndrome. Pediatrics 2016; 137:e20153835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson J, Tarabulsy GM, Bussières E-L. Foetal programming and cortisol secretion in early childhood: a meta-analysis of different programming variables. Infant Behav Dev 2015; 40:204–215. [DOI] [PubMed] [Google Scholar]
- Popova S, Lange S, Shield K, et al. Comorbidity of fetal alcohol spectrum disorder: a systematic review and meta-analysis. Lancet 2016; 387:978–987. [DOI] [PubMed] [Google Scholar]
- Pritham UA, Paul JA, Hayes MJ. Opioid dependency in pregnancy and length of stay for neonatal abstinence syndrome. J Obstet Gynecol Neonatal Nurs 2012; 41:180–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reece-Stremtan S, Marinelli KA. The Academy of Breastfeeding Medicine. ABM Clinical Protocol #21: guidelines for breastfeeding and substance use or substance use disorder, revised 2015. Breastfeed Med 2015; 10:135–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruwanpathirana R, Abdel-Latif ME, Burns L, et al. Prematurity reduces the severity and need for treatment of neonatal abstinence syndrome. Acta Paediatr 2015; 104:e188–e194. [DOI] [PubMed] [Google Scholar]
- Salisbury AL, Coyle MG, O’Grady KE, et al. Fetal assessment before and after dosing with buprenorphine or methadone. Addiction 2012; 107 suppl 1:36–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savage SR. Long-term opioid therapy: assessment of consequences and risks. J Pain Symptom Manage 1996; 11:274–286. [DOI] [PubMed] [Google Scholar]
- Scaffidi J, Mol BW, Keelan JA. The pregnant women as a drug orphan: a global survey of registered clinical trials of pharmacological interventions in pregnancy. BJOG 2016; 124:132–140. [DOI] [PubMed] [Google Scholar]
- Stover MW, Davis JM. Opioids in pregnancy and neonatal abstinence syndrome. Semin Perinatol 2015; 39:561–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teague AH, Jnah AJ, Newberry D. Intraprofessional excellence in nursing: collaborative strategies for neonatal abstinence syndrome. Neonatal Netw 2015; 34:320–328. [DOI] [PubMed] [Google Scholar]
- Terplan M, Hand DJ, Hutchinson M, et al. Contraceptive use and method choice among women with opioid and other substance use disorders: a systematic review. Prev Med (Baltim) 2015; 80:23–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai LC, Doan TJ. Breastfeeding among mothers on opioid maintenance treatment: a literature review. J Hum Lact 2016; 32:521–529. [DOI] [PubMed] [Google Scholar]
- Wachman EM, Hayes MJ, Brown MS, et al. Association of OPRM1 and COMT single-nucleotide polymorphisms with hospital length of stay and treatment of neonatal abstinence syndrome. JAMA 2013; 309:1821–1827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welle-Strand GK, Skurtveit S, Tanum L, et al. Tapering from methadone or buprenorphine during pregnancy: maternal and neonatal outcomes in Norway 1996–2009. Eur Addict Res 2015; 21:253–261. [DOI] [PubMed] [Google Scholar]
- Whitham JN, Spurrier NJ, Baghurst PA, et al. Visual evoked potential latencies of three-year-old children prenatally exposed to buprenorphine or methadone compared with non-opioid exposed children: the results of a longitudinal study. Neurotoxicol Teratol 2015; 52 (pt A):17–24. [DOI] [PubMed] [Google Scholar]
- Wiegand SL, Stringer EM, Stuebe AM, et al. Buprenorphine and naloxone compared with methadone treatment in pregnancy. Obstet Gynecol 2015; 125:363–368. [DOI] [PubMed] [Google Scholar]
- Wiles JR, Isemann B, Mizuno T, et al. Pharmacokinetics of oral methadone in the treatment of neonatal abstinence syndrome: a pilot study. J Pediatr 2015; 167:1214.e3–1220.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Guidelines for the Identification and Management of Substance Use and Substance Use Disorders in Pregnancy. Geneva, Switzerland: World Health Organization Press; 2014. [PubMed] [Google Scholar]
- Wright TE, Terplan M, Ondersma SJ, et al. The role of screening, brief intervention and referral to treatment in the perinatal period. Am J Obstet Gynecol 2016; 215:539–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yazdy MM, Desai RJ, Brogly SB. Prescription opioids in pregnancy and birth outcomes: a review of the literature. J Pediatr Genet 2015; 4:56–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young ME, Hager SJ, Spurlock D., Jr Retrospective chart review comparing morphine and methadone in neonates treated for neonatal abstinence syndrome. Am J Health Syst Pharm 2015; 72 (23 suppl 3):S162–S167. [DOI] [PubMed] [Google Scholar]
- Zedler BK, Mann AL, Kim MM, et al. Buprenorphine compared with methadone to treat pregnant women with opioid use disorder: a systematic review and meta-analysis of safety in the mother, fetus and child. Addiction 2016; 111:2115–2128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zharikova OL, Deshmukh SV, Kumar M, et al. The effect of opiates on the activity of human placental aromatase/CYP19. Biochem Pharmacol 2007; 73:279–286. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


