Abstract
Background:
Both unilateral pedicle screw fixation with posterior lumbar interbody fusion (PLIF) and bilateral pedicle screw fixation with PLIF are used to treat lumbar degenerative diseases (LDD). However, which one is a better treatment for LDD remains considerable controversy. Therefore, the focus of this meta-analysis was to assess the merits and shortcomings of efficacy of these 2 surgical procedures for LDD.
Methods:
An extensive search of literature was performed in Pubmed/MEDLINE, Embase, CNKI, and WANFANG databases on unilateral versus bilateral pedicle screw fixation with PLIF fusion for LDD, from January 2007 to January 2017 and language was restricted to Chinese or English. The following variables were extracted: blood loss, operation time, length of hospital stay, Japanese Orthopedic Association (JOA) scores, visual analog scale (VAS) and Oswestry disability index (ODI) scores, fusion rate, total complications, infection, dural injury, and nerve injury. Data analysis was conducted with RevMan 5.3 and STATA 12.0.
Results:
A total of 11 studies containing 844 patients were included in our study. The results showed that unilateral is better than bilateral pedicle screw fixation with PLIF in blood loss (P < .00001), operation time (P < .00001), the length of hospital stay (P = .003), and the final follow-up ODI scores (P = .04). However, there are no significant differences in JOA, VAS, and preoperative ODI scores. There are also no significant differences in fusion rate and complications (all P > .05).
Conclusion:
Based on our meta-analysis, our results suggest that both unilateral pedicle screw fixation with PLIF and bilateral pedicle screw fixation with PLIF for LDD have effective results in clinical outcomes. Both 2 methods may result in clinical improvement and similar outcomes of fusion rate and complications; However, compared with bilateral fixation, unilateral fixation produces more satisfactory efficacy in the blood loss and the operation time.
Keywords: bilateral fixation, lumbar degenerative diseases, meta-analysis, posterior lumbar interbody fusion, unilateral fixation
1. Introduction
Lumbar degenerative diseases (LDD) is a common disease which including prolapsed lumbar intervertebral disc, degenerative instability, spondylolisthesis of lumbar, lumbar spinal stenosis, and degenerative scoliosis. Posterior lumbar interbody fusion (PLIF) has gradually become a common and effective surgical method to treat LDD, since first reported by Dr Ralph Cloward more than 60 years ago.[1] PLIF could achieve a decompression of the dura sac and nerve roots, maintain proper disk space height, and accelerate the recovery process from spine surgery.[2–4]
Traditionally, bilateral pedicle screw fixation was widely used for managing PLIF, which could provides promote arthrodesis, prevent nonunion, and improve fusion rate.[5] However, due to the excessive rigidity of bilateral fixation, this procedure has also been suspected to result in more extensive dissection, adjacent segments degeneration, device-related osteoporosis, and higher risk of implant-related complications.[6–8] Also, it may mean more extensive dissection, more blood loss, longer duration of operation, and greater medical costs. In recent years, unilateral pedicle screw fixation in PLIF was used to decrease the stiffness of the instrumented segment, and acquired similar functional results and fusion rate compared with bilateral fixation in the management of LDD.[9–14]
Previous meta-analyses[15–17] reviewed mainly focused on the comparison between bilateral and unilateral pedicle screw fixation with transforaminal lumbar interbody fusion (TLIF) or minimally invasive surgery TLIF, with few variables or included studies. The clinical efficacy and complications of unilateral compared with bilateral screw fixation with PLIF for LDD still remain controversial. Thereby, we conduct this meta-analysis to critically assess the effectiveness and safety of these 2 techniques for the treatment of LDD.
2. Materials and methods
2.1. Ethics statement
There is no need to seek consent from patients, as in this study all the data were collected from the published data and analyzed anonymously without any potential harm to the patients; this study was approved by the Ethics Committee of our hospital.
2.2. Search strategy
An extensive search of literature was performed in PubMed, Embase, the Cochrane library, CNKI, and WANFANG databases published from January 2007 to January 2017. The search was conducted with the use of the following search terms: “unilateral pedicle screw fixation,” “bilatera pedicle screw fixation,” “posterior lumbar interbody fusion,” and “lumbar degenerative diseases,” with various combinations of the operators “AND” and “OR.” Language was restricted to Chinese and English.
2.3. Inclusion criteria
Studies were included if they met the following criteria: age between 30 and 75 years; included patients with LDD, such as degenerative lumbar disk herniation, lumbar spinal stenosis, and degenerative spondylolisthesis; included patients who underwent PLIF; and unilateral and bilateral pedicle screw fixation were compared.
2.4. Exclusion criteria
Studies were excluded if they met the following criteria: had an average follow-up time of less than 6 months; patients with spinal deformity, trauma, spinal tumor, or with previous lumbar operation; only described unilateral or bilateral screw fixation; without PLIF; involved patients with another disease, such as severe osteoporosis, active infection, cervical spondylosis, or thoracic disease; in vitro human cadaveric biomechanical studies; and earlier trials, reviews, and case-reports.
2.5. Selection of studies
All subjects, abstracts, and the full text of articles were independently reviewed by 2 reviewers. Then the eligible trials were selected according to the inclusion criteria. If they disagreed, a 3rd reviewer was consulted to resolve the differences.
2.6. Data extraction and management
Two reviewers extracted data independently. The extracted information included: author; year of publication; the country of study, study type, the sample size, the mean age of participants, gender, and duration of follow-up, blood loss, operation time, the clinical outcomes (Japanese Orthopedic Association [JOA], Oswestry disability index [ODI], visual analog scale [VAS] score, and the length of hospital stay), fusion rate, and complications.
2.7. Statistical analysis
All data analyses were performed using RevMan 5.3 and STATA 12.0. For dichotomous variables, we analyzed using odds ratio (OR), and for continuous variables, the standardized mean difference (SMD) was used. Both were reported with 95% confidence intervals, and the heterogeneity test was considered statistically significant when P < .05. We used I2 statistic to assess heterogeneity. I2 > 50% implied substantial heterogeneity among the included studies, random-effect model was used to analysis. If I2 less than or equal to 50%, which were considered to represent no significant heterogeneity, we chose fixed-effect model.
2.8. Test for risk of publication bias
Funnel plot was performed to evaluate the risk of publication bias. If the funnel plot was asymmetric, there is publication bias and symmetric indicated no publication bias. The funnel plot asymmetry was measured by Begg and Egger tests. P values less than .05 were regarded as a significance level.
3. Results
3.1. Search results
Through the application of search strategy, a total of 504 English studies in Pubmed/MEDLINE and Embase, 661 Chinese studies in CNKI and WANFANG were identified. Of these, 1053 articles after duplicates were removed; 75 articles were excluded after title and abstract screening. Twenty-six articles were excluded due to eligibility criteria. As a result, a total of 11 studies[3,9,18–26] were identified for this meta-analysis, including 2 English article and 9 Chinese articles. The flow diagram of the study search process is presented in Fig. 1.
Figure 1.

Flow diagram of study selection.
3.2. Baseline characteristics and quality assessment
A total of 11 studies comprising 398 patients treated with unilateral and 446 patients treated with bilateral screw fixation with PLIF, respectively, were included in the final analysis. There were no significant differences between groups regards to age, sex, and follow-up (Table 1), presents the baseline characteristics of the 2 groups. To assess the quality of each study, we used the Newcastle Ottawa Quality Assessment Scale (NOQAS). This scale for nonrandomized case controlled studies and cohort studies had a maximum of 9 points, which included the quality of selection, comparability, exposure, and outcomes for study participants. Of these studies, 8 scored 8 points and 3 scored 7 points. Therefore, the quality of each study was relatively high (Table 2).
Table 1.
Characteristics of included studies.

Table 2.
The quality assessment according to the Newcastle Ottawa Quality Assessment Scale (NOQAS) of each study.

3.3. Blood loss and operation time
Six studies reported the intraoperative blood loss between unilateral and bilateral pedicle screw fixation with PLIF (n = 252 in the unilateral group, and 288 in the bilateral group). Meta-analysis showed unilateral group had less blood loss than bilateral group (P < .00001, SMD = −82.69 [−117.31, −48.07]; heterogeneity: P < .00001, I2 = 93%, random-effect model, Fig. 2).
Figure 2.

The standardized mean difference (SMD) estimate for blood loss.
Five studies reported the operation time (n = 168 in the unilateral group, and 186 in the bilateral group). The unilateral group showed shorter operation time compared with the bilateral group (P < .00001, SMD = −51.02 [−54.17, −47.87]; heterogeneity: P < .18, I2 = 36%, fixed-effect model, Fig. 3).
Figure 3.

The standardized mean difference (SMD) estimate for operation time.
3.4. Clinical outcomes
Six studies reported the length of hospital stay between unilateral and bilateral pedicle screw fixation with PLIF (n = 239 in the unilateral group, and 265 in the bilateral group). Meta-analysis showed unilateral group had shorter hospital stay than bilateral group. (P = .003, SMD = −1.14 [−2.45, −0.49]; heterogeneity: P < .00001, I2 = 95%, random-effect model, Fig. 4).
Figure 4.

The standardized mean difference (SMD) estimate for length of hospital stay.
Three studies reported the preoperative and the final follow-up JOA scores (n = 102 in the unilateral group, and 102 in the bilateral group). There is also no significant difference between the 2 groups in preoperative JOA scores (P = .77, SMD = −0.12 [−0.95, −0.71]; heterogeneity: P = .06, I2 = 64%, random-effect model, Fig. 5), but significant difference in the final follow-up JOA scores (P = .09, SMD = −0.39 [−0.07, 0.85]; heterogeneity: P = .08, I2 = 60%, random-effect model, Fig. 6).
Figure 5.
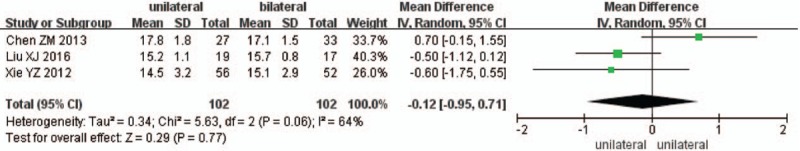
The SMD estimate for preoperative JOA scores. JOA = Japanese Orthopedic Association, SMD = standardized mean difference.
Figure 6.

The SMD estimate for the final follow-up JOA scores. JOA = Japanese Orthopedic Association, SMD = standardized mean difference.
Five studies reported the preoperative and the final follow-up ODI scores (n = 181 in the unilateral group, and 204 in the bilateral group). There is no significant difference between the 2 groups in preoperative ODI scores (P = .15, SMD = −0.43 [−1.01, 0.15]; heterogeneity: P = .64, I2 = 0%, fixed-effect model, Fig. 7), but significant difference in the final follow-up ODI scores (P = .04, SMD = −0.38 [−0.74, −0.02]; heterogeneity: P = .43, I2 = 0%, fixed-effect model, Fig. 8).
Figure 7.

The SMD estimate for preoperative ODI scores. ODI = Oswestry disability index, SMD = standardized mean difference.
Figure 8.

The SMD estimate for the final follow-up ODI scores. ODI = Oswestry disability index, SMD = standardized mean difference.
Eight studies reported preoperative and the final follow-up VAS scores (n = 286 in the unilateral group, and 328 in the bilateral group). Preoperative VAS scores were similar between the 2 groups (P = .61, SMD = −0.12 [−0.6, 0.35]; heterogeneity: P < .00001, I2 = 84%, random-effect model, Fig. 9), the final follow-up VAS scores were also similar between the 2 groups (P = .83, SMD = −0.02 [−0.21, 0.17]; heterogeneity: P < .00001, I2 = 87%, random-effect model, Fig. 10).
Figure 9.

The SMD estimate for preoperative VAS scores. SMD = standardized mean difference, VAS = visual analog scale.
Figure 10.

The SMD estimate for the final follow-up VAS scores. SMD = standardized mean difference, VAS = visual analog scale.
3.5. Fusion rate
Eleven studies reported fusion rate between unilateral and bilateral pedicle screw fixation with PLIF (n = 398 in the unilateral group, and 446 in the bilateral group). The meta-analysis showed that unilateral has a similar result of fusion rate compared with bilateral (P = .12, OR = 0.58 [0.29, 1.16]; heterogeneity: P = .98, I2 = 0%, fixed-effects model Fig. 11)
Figure 11.

The standardized mean odds ratio (OR) estimate for fusion rate.
3.6. Complications
Eleven studies reported total complications between unilateral and bilateral pedicle screw fixation with PLIF (n = 398 in the unilateral group, and 446 in the bilateral group). Total complications were similar between the 2 groups (P = .18, OR = 0.73 [0.46, 1.16]; heterogeneity: P = .86, I2 = 0%, fixed-effects model, Fig. 12).
Figure 12.

The standardized mean odds ratio (OR) estimate for total complications.
Six studies reported the infection after surgery between unilateral and bilateral pedicle screw fixation with PLIF (n = 232 in the unilateral group, and 268 in the bilateral group). Meta-analysis showed unilateral group was similar compared with bilateral group in infection. (P = .32, OR = 0.63 [0.23, 1.62]; heterogeneity: P = .98, I2 = 0%, fixed-effect model, Fig. 13).
Figure 13.

The standardized mean odds ratio (OR) estimate for infection.
Four studies reported the nerve injury between unilateral and bilateral pedicle screw fixation with PLIF (n = 186 in the unilateral group, and 204 in the bilateral group). Meta-analysis showed unilateral group was similar compared with bilateral group in nerve injury. (P = .85, OR = 1.10 [0.42, 2.88]; heterogeneity: P = .41, I2 = 0%, fixed-effect model, Fig. 14).
Figure 14.
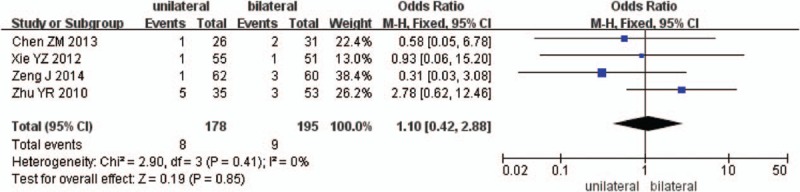
The standardized mean odds ratio (OR) estimate for nerve injury.
Six studies reported the dural injury between unilateral and bilateral pedicle screw fixation with PLIF (n = 232 in the unilateral group, and 268 in the bilateral group). Meta-analysis showed unilateral group was similar compared with bilateral group in dural injury. (P = .28, OR = 0.57 [0.21, 1.58]; heterogeneity: P = .93, I2 = 0%, fixed-effect model, Fig. 15).
Figure 15.
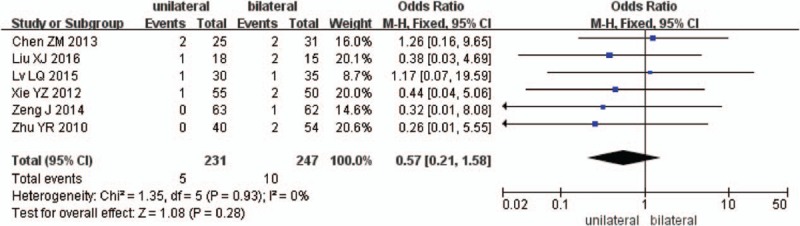
The standardized mean odds ratio (OR) estimate for dural injury.
3.7. Publication bias
Publication bias were detected by STATA 12.0, and no publication bias found for all included studies (all P > .05). The funnel plot did not indicate any publication bias in blood loss (Begg, P = .133; Egger, P = .146); operation time (Begg, P = .806; Egger, P = .69); length of hospital stay (Begg, P = .452; Egger, P = .689); JOA score before surgery (Begg, P = 1.000; Egger, P = .957); JOA score at final follow-up (Begg, P = 1.000; Egger, P = .925); ODI score before surgery (Begg, P = .221; Egger, P = .114); ODI score at final follow-up (Begg, P = .806; Egger, P = .746); VAS score before surgery (Begg, P = 1.000; Egger, P = .974); VAS score at final follow-up (Begg, P = .902; Egger, P = .875); fusion rate (Begg, P = .711; Egger, P = .947); total complications (Begg, P = .436; Egger, P = .206); infection (Begg, P = 1.000; Egger, P = .779); nerve injury (Begg, P = 1.000; Egger, P = .744); and dural injury (Begg, P = .089; Egger, P = .054).
4. Discussion
LDD is a common disease, which can lead to significant disability and severe pain. With the population aging trends and lifestyle changes of the elderly, LDD has become an important degenerative disease causing spinal dysfunction and seriously affect the work and life of patients. To achieve favorable clinical results, adequate decompression around the spinal cord and nerve roots with or without fusion is essential. Bilateral pedicle screw fixations has been regarded as the standard surgical procedure in spinal fusion surgery to provide rigid lumbar spinal fixation.[9,27,28] But this procedure has also been suspected to result in adjacent segments degeneration, device-related osteoporosis, and higher risk of implant-related complications.
Recently, unilateral pedicle screw fixation has been reported to be as effective as bilateral fixation in lumbar fusion.[14,29] Hu et al[30] conducted a systematic review comparing unilateral versus bilateral pedicle screw fixation in TLIF, Wang et al[31] conducted a meta-analysis comparing unilateral versus bilateral pedicle screw fixation of minimally invasive TLIF. But they did not compare the unilateral with bilateral pedicle screw fixation in PLIF. Zhong et al[32] performed a meta-analysis comparing unilateral and bilateral fixation with PLIF, but the JOA scores and the incidence rate of infection, nerve injury and dural injury were not analyzed. And Zhong study showed that the final follow-up VAS score was significantly different between unilateral and bilateral fixation, while in this paper, there were no statistical differences. That is probably due to the number of papers included was too small.[32] Therefore, we conducted this meta-analysis to analyze the data of the unilateral and bilateral pedicle screw fixation in PLIF.
Although no randomized controlled trials (RCTs) included in this meta-analysis, we considered the included studies suitable for meta-analysis because of the high quality of those included studies according to the NOQAS, and the baseline variables were similar. Surgical trauma (including blood loss and operation time), clinical outcomes (including JOA, ODI, VAS score, and the length of hospital stay), fusion rate, and complications (including total complications, infection, dural injury, and nerve injury) were analyzed in this study.
Surgical trauma were always assessed by operation time and blood loss.[33] This meta-analysis showed that unilateral pedicle screw fixation has better results in both the blood loss and the operation time, indicated that the surgical trauma is smaller in unilateral pedicle screw fixation compared with bilateral. This results may be attribute to only one side of muscle was dissected and unilateral pedicle screw placed.[34,35]
The clinical outcomes after lumber surgery were often evaluated using JOA, VAS, ODI scores, and the length of hospital stay. The pooled data showed that there were no significant difference in preoperative and final follow-up JOA scores, preoperative and final follow-up VAS scores, and preoperative ODI scores. But statistically significant in final follow-up ODI scores and the length of hospital stay. Both 2 methods could achieved sufficient improvement in JOA, VAS, ODI scores, hence, both methods were effective in decompression of spinal cord and nerve improvement. But unilateral fixation may superior to bilateral in spinal function recovery regarding the final follow-up ODI scores and the length of hospital stay.
We selected total complications, infection, nerve injury, and dural injury to evaluate postoperative complications. Both side of muscle dissection and bilateral pedicle screw placement in bilateral group, resulting in the increased chances of a surgical infection and nerve injury.[18] However, the pooled data showed no significant difference in the total complications, infection, dural injury, and nerve injury between 2 groups.
We also analyzed the fusion rate between unilateral and bilateral pedicle screw fixation. This study found that there was no significant difference between the 2 groups in fusion rate. Fusion could greatly improve the stiffness of internal fixation.[36] Fusion is important for unilateral pedicle screw fixation particularly, so the completely resection of intervertebral disc and the correctly scraping of cartilage endplates are significant in surgery.
There are several limitations of this study. First, there was no RCTs included this study, we need RCTs for further study. Second, adjacent level degeneration after lumbar interbody fusion is an important radiographic evaluation of surgical outcome, this result was not analyzed. Third, the sample sizes of these studies might not be large enough to show significant differences between the 2 groups, more studies should be included to improve the power of the findings. Fourth, the length of follow-up varied among the included studies, and thus may influence our results. Finally, we only included the studies in English and Chinese, and some relevant studies reported in other languages were not included due to a language limitation.
5. Conclusions
In summary, the findings of this meta-analysis suggest that both unilateral pedicle screw fixation with PLIF and bilateral pedicle screw fixation with PLIF for LDD have effective results in clinical outcomes. Both 2 methods may result in similar outcomes of fusion rate and complications. However, unilateral group produced more satisfactory efficacy in the blood loss and the operation time. Further studies with high methodological quality and long-term follow-up periods are needed to evaluate the 2 procedures for LDD treatment.
Footnotes
Abbreviations: JOA = Japanese Orthopedic Association, LDD = lumbar degenerative diseases, ODI = Oswestry disability index, OR = odds ratio, PLIF = posterior lumbar interbody fusion, SMD = standardized mean difference, TLIF = transforaminal lumbar interbody fusion, VAS = visual analog scale.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Cloward RB. The treatment of ruptured lumbar intervertebral discs by vertebral body fusion. I. Indications, operative technique, after care. J Neurosurg 1953;10:154–68. [DOI] [PubMed] [Google Scholar]
- [2].Fogel GR, Toohey JS, Neidre A, et al. Is one cage enough in posterior lumbar interbody fusion: a comparison of unilateral single cage interbody fusion to bilateral cages. J Spinal Disord Tech 2007;20:60–5. [DOI] [PubMed] [Google Scholar]
- [3].Xie Y, Ma H, Li H, et al. Comparative study of unilateral and bilateral pedicle screw fixation in posterior lumbar interbody fusion. Orthopedics 2012;35:e1517–23. [DOI] [PubMed] [Google Scholar]
- [4].Bagby GW. Arthrodesis by the distractioncompression method using a stainless steel implant. Orthopedics 1988;11:931–4. [DOI] [PubMed] [Google Scholar]
- [5].Lin B, Xu Y, He Y, et al. Minimally invasive unilateral pedicle screw fixation and lumbar interbody fusion for the treatment of lumbar degenerative disease. Orthopedics 2013;36:e1071–6. [DOI] [PubMed] [Google Scholar]
- [6].Park P, Garton HJ, Gala VC, et al. Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine (Phila Pa 1976) 2004;29:1938–44. [DOI] [PubMed] [Google Scholar]
- [7].Mao L, Chen GD, Xu XM, et al. Comparison of lumbar interbody fusion performed with unilateral or bilateral pedicle screw. Orthopedics 2013;36:e489–93. [DOI] [PubMed] [Google Scholar]
- [8].Xiao SW, Jiang H, Yang LJ, et al. Comparison of unilateral versus bilateral pedicle screw fixation with cage fusion in degenerative lumbar diseases: a meta-analysis. Eur Spine J 2015;24:764–74. [DOI] [PubMed] [Google Scholar]
- [9].Fernández- Fairen M, Sala P, Ramírez H, et al. A prospective randomized study of unilateral versus bilateral instrumented posterolateral lumbar fusion in degenerative spondylolisthesis. Spine (Phila Pa 1976) 2007;32:395–401. [DOI] [PubMed] [Google Scholar]
- [10].Zhao J, Zhang F, Chen X, et al. Posterior interbody fusion using a diagonal cage with unilateral transpedicular screw fixation for lumbar stenosis. J Clin Neurosci 2011;18:324–8. [DOI] [PubMed] [Google Scholar]
- [11].Feng ZZ, Cao YW, Jiang C, et al. Short-term outcome of bilateral decompression via a unilateral paramedian approach for transforaminal lumbar interbody fusion with unilateral pedicle screw fixation. Orthopedics 2011;34:364. [DOI] [PubMed] [Google Scholar]
- [12].Jang JS, Lee SH. Minimally invasive transforaminal lumbar interbody fusion with ipsilateral pedicle screw and contralateral facet screw fixation. J Neurosurg Spine 2005;3:218–23. [DOI] [PubMed] [Google Scholar]
- [13].Li H, Yang WJ, Tian JP, et al. Clinical efficiency of unilateral vs bilateral pedicle screws system combined with TLIF for lumbar degenerative disease in elderly patients. Chin J Geriatr Orthop Rehabil (Electronic Edition) 2016;2:205–10. [Google Scholar]
- [14].Suk KS, Lee HM, Kim NH, et al. Unilateral versus bilateral pedicle screw fixation in lumbar spinal fusion. Spine (Phila Pa 1976) 2000;25:1843–7. [DOI] [PubMed] [Google Scholar]
- [15].Xin Z, Li W. Unilateral versus bilateral pedicle screw fixation in short-segment lumbar spinal fusion: a meta-analysis of randomised controlled trials. Int Orthop 2016;40:355–64. [DOI] [PubMed] [Google Scholar]
- [16].Xiao SW, Jiang H, Yang LJ, et al. Comparison of unilateral versus bilateral pedicle screw fixation with cage fusion in degenerative lumbar diseases: a meta-analysis. Eur Spine J 2015;24:764–74. [DOI] [PubMed] [Google Scholar]
- [17].Han YC, Liu ZQ, Wang SJ, et al. Comparison of unilateral versus bilateral pedicle screw fixation in degenerative lumbar diseases: a meta-analysis. Eur Spine J 2014;23:974–84. [DOI] [PubMed] [Google Scholar]
- [18].Chen ZM, Ma HS, Wang XP, et al. Unilateral versus bilateral pedicle screw fixation with a single cage in treating lumbar degenerative diseases. Chin J Bone Joint Surg 2013;6:126–30. [Google Scholar]
- [19].Zhu YR, Ye XJ, Jiang YQ, et al. Modified posterior lumbar interbody fusion using unilateral pedicle screw fixation in lumber interbody fusion. Acad J Second Mil Med Univ 2010;31:1095–9. [Google Scholar]
- [20].Mao L, Yang HL, Wang GL, et al. Unilateral versus bilateral pedicle screw fixation with lumbar interbody fusion in treating lumbar degenerative disease. Chin J Clin (Electronic Edition) 2012;6:328–32. [Google Scholar]
- [21].Shi J, Hu L, Zhou J, et al. Clinical efficacy of internal fixation with unilateral versus bilateral transpedicle screws combined with intervertebral fusion in lumbar degenerative diseases. Orthop J China 2013;21:651–7. [Google Scholar]
- [22].Lv LQ, Wei XD, Meng SY, et al. Comparison of unilateral versus bilateral pedicle screw fixation in treating degenerative lumbar diseases. J Pract Orthop 2015;21:536–40. [Google Scholar]
- [23].Liu XJ, Yao FD, Wang XH, et al. Comparative study of unilateral and bilateral pedicle screws fixation in therapy of far lateral lumbar disc herniation. The Journal of Cervicodynia and Lumbodynia 2016;37:223–7. [Google Scholar]
- [24].Zeng J, Yao H, Dai M, et al. Clinical application of unilateral pedicle screw for lumbar intervertebral disc protrusion. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2014;28:74–8. [PubMed] [Google Scholar]
- [25].Xia CW, Wang SJ, Li XL, et al. Early clinical effects of internal fixation with unilateral versus bilateral transpedicle screws combined with intervertebral fusion in lumbar disc herniation. J Spinal Surg 2011;9:65–8. [Google Scholar]
- [26].Li XJ, Zhang ZL, Gao HX. Clinical research on treating 71 cases of lumbar degenerative diseases by internal fixation with unilateral versus bilateral transpedicle screws plus single cage. Clin J Chin Med 2016;8:109–12. [Google Scholar]
- [27].Beringer WF, Mobasser JP. Unilateral pedicle screw instrumentation for minimally invasive transforaminal lumbar interbody fusion. Neurosurg Focus 2006;20:E4. [PubMed] [Google Scholar]
- [28].Mao L, Zhao J, Dai KR, et al. Bilateral decompression using a unilateral pedicle construct for lumbar stenosis. Int Orthop 2014;38:573–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Kabins MB, Weinstein JN, Spratt KF, et al. Isolated L4-L5 fusions using the variable screw placement system: unilateral versus bilateral. J Spinal Disord 1992;5:39–49. [DOI] [PubMed] [Google Scholar]
- [30].Hu XQ, Wu XL, Xu C, et al. A systematic review and meta-analysis of unilateral versus bilateral pedicle screw fixation in transforaminal lumbar interbody fusion. PLoS One 2014;9:e87501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Wang L, Wang Y, Li Z, et al. Unilateral versus bilateral pedicle screw fixation of minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF): a meta-analysis of randomized controlled trials. BMC Surg 2014;14:87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Zhong YM, Fu SH, Li ZF, et al. System evaluation of unilateral and bilateral pedicle screw fixation and posterior lumbar interbody fusion in the repair of lumbar degenerative diseases. Chin J Tissue Eng Res 2016;20:1353–60. [Google Scholar]
- [33].Hu K. Comparison of effectiveness with laminoplasty versus laminectomy and fusion for cervical stenosis. J Clin Res 2011;28:541–3. [Google Scholar]
- [34].Iwatsuki K, Yoshimine T, Aoki M. Bilateral interlaminar fenestration and unroofing for the decompression of nerve roots by using a unilateral approach in lumbar canal stenosis. Surg Neurol 2007;68:487–92. [DOI] [PubMed] [Google Scholar]
- [35].Kotil K, Ali Akçetin M, Savaş Y. Clinical and radiologic outcomes of TLIF applications with or without pedicle screw: a double center prospective pilot comparative study. J Spinal Disord Tech 2013;26:359–66. [DOI] [PubMed] [Google Scholar]
- [36].Polly DW, Jr, Klemme WR, Cunningham BW, et al. The biomechanical significance of anterior column support in a simulated single-level spinal fusion. J Spinal Disord 2000;13:58–62. [DOI] [PubMed] [Google Scholar]


