Abstract
Recently, more attention has been paid to the role of the acetabular labrum. Therefore, we designed a retrospective cohort study of patients with residual hip dysplasia (RHD) who underwent magnetic resonance imaging (MRI). The objective of this study was to investigate an association between the MRI appearance of the labrum before school age and the natural history of RHD.
We retrospectively investigated 45 hips of 40 patients who underwent MRI at about 3 and 4 years of age for RHD and were conservatively followed up with until 6 years of age or older. We evaluated the extent of eversion with a new method that measures the β angle (MRI β angle) using landmarks of the Graf method on MRI T2∗-weighted images. The outcome measure was the Severin classification at the final follow-up. We compared the radiographic and MRI parameters at approximately 3 and 4 years of age between the good and poor outcome groups. The Student t test or one-way analysis of variance was used to compare the quantitative variables between groups. The Chi-square test was used to perform a ratio comparison.
Although there was a significant difference in the center-edge (CE) angle, there was no significant difference in the acetabular index and the ratio of the presence of femoral head necrosis and the break in Shenton line between the good and poor groups. The MRI β angle was significantly greater in the poor outcome group than in the normal and good outcome groups. The cut-off value of the MRI β angle to differentiate the good and poor outcome groups was 65°, and its specificity and sensitivity were 92% and 53%, respectively.
There was labral eversion on MRI scans in patients with RHD. Acetabular development before adolescence was poorer with greater labral eversion on MRI scans. The specificity for poor acetabular development was high when the MRI β angle was 65° or more. The MRI β angle has the potential to predict acetabular development.
Keywords: acetabular development, developmental dysplasia of the hip, labrum, magnetic resonance imaging, residual hip dysplasia
1. Introduction
Residual hip dysplasia (RHD) after the initial treatment of developmental dysplasia of the hip in infancy sometimes requires Salter innominate osteotomy before school age.[1] Radiographic parameters [acetabular index > 30°, center-edge (CE) angle[2] < 5°] are frequently used to determine the indication for osteotomy in our country.[3–6] It is often difficult to make a judgment in patients whose radiographic evaluations are borderline. Corrective operations confer a risk of acetabular retroversion, as they alter the morphology of the acetabulum.[7,8] Therefore, the overutilization of corrective operation should be avoided, as a more accurate prediction of acetabular development is required at this age.
The β angle in the Graf method uses a landmark of the labrum.[9] Recent studies have shown that the labrum plays an important role in stabilization of the hip joint. The labrum provides resistance for traction by sealing the joint fluid and lubricating the articular cartilage.[10,11] Furthermore, the labrum itself disperses the load applied to the acetabular cartilage and increases the coverage of the femoral head.[12] Thus, an abnormal labrum can impair function of the acetabular cartilage, affecting acetabular development, but the labral disorder in patients with RHD before school age remains unknown.
The β angle in the Graf method indicates the extent of labral eversion and cartilaginous roofing. Greater eversion angles indicate subluxations and dislocations. The research questions of this study are as follows: is there labral eversion on magnetic resonance imaging (MRI) scans of patients with RHD? and is there a relationship between the labral eversion on MRI scans and acetabular development? To answer these clinical questions, we designed a retrospective cohort study of patients with RHD who underwent MRI. The objective of this study was to investigate an association between the MRI appearance of the labrum or radiographic indicators before school age and the natural history of RHD.
2. Methods
Ethical approval for this study was provided by the institutional review board of Nagoya City University, Nagoya, on November 18, 2014 (approval no.: 541-2). Oral informed consent was obtained from patients. The need for signing the informed consent was waived because of the retrospective nature of our study and the fact that no patient identification data were included in the analysis.
2.1. Study design, setting, and procedure
We reviewed consecutive patients with RHD who underwent MRI from December 1999 to November 2010 after being diagnosed as having developmental dysplasia of the hip and receiving initial treatment at our hospital. We performed selective MRI on hips that met our indication for Salter innominate osteotomy at about 3 and 4 years of age. Our indication for Salter innominate osteotomy was hips with clinical signs of instability or with an acetabular index ≥30° or CE angle ≤5° on radiographs. We checked a high-signal intensity area within the weight-bearing portion of the acetabular cartilage on T2-weighted MRI scans.[13] Although we suggested corrective operation for patients who met our indication, some patients declined and received conservative treatment.
2.2. Inclusion and exclusion criteria
Our study included consecutive patients with RHD who underwent MRI before school age and were followed up with until 6 years of age or older. We excluded hips that had neurological or teratologic disorders and infections. We also excluded hips that had good acetabular development, did not undergo MRI before school age, received Salter innominate osteotomy, or had missing data. Two hundred thirty hips of 210 patients who were diagnosed as having developmental dysplasia of the hip without neurological or teratologic disorders and infections received initial treatment. After excluding 154 hips of 139 patients who had good acetabular development and did not undergo MRI before school age or had missing data, a consecutive series of 76 hips of 71 patients met our inclusion criteria. After excluding 31 hips of 31 patients who underwent Salter innominate osteotomy, the data for 45 hips of 40 patients were investigated in our analysis.
2.3. Outcome measures
The outcome measure was the Severin classification[14] at the final follow-up. We defined hips that had Severin grade I or II as the good outcome group. We defined hips that had Severin grade III or IV as the poor outcome group. We defined contralateral hips of age-matched patients who underwent MRI because of unilateral transient synovitis, Perthes disease, and traumatic hip injuries as the normal control group. The age of exposure to MRI was at approximately 3 and 4 years.
2.4. Measurement of β angle on MRI scans
To evaluate the extent of labrum eversion using MRI, we applied the landmarks of the Graf method[9] and introduced a new measurement method. We measured the β angle (MRI β angle) by drawing a baseline and cartilage roof line based on coronal slices of T2∗-weighted images through the center of the femoral head (Fig. 1). We used T2∗-weighted images because they provided the clearest sequence with which to visualize the contrast of the articular cartilage and labrum.[15,16]
Figure 1.
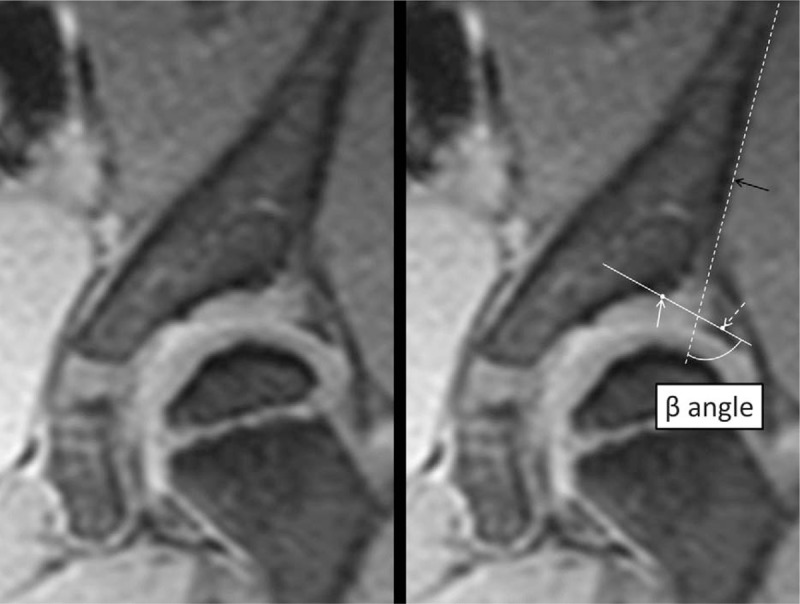
Measurement of the β angle on magnetic resonance imaging (MRI) scans. On the basis of landmarks in the Graf method, the baseline (dotted line) and cartilage roofline (white line) are drawn to measure the β angle on MRI scans. The baseline is defined as the tangent line with the lateral edge of the iliac wing (low signal area; black arrow). The cartilaginous acetabular line is defined as the line between the acetabular bony rim (low signal area; white arrow) and the center of the labrum (low signal area; dotted arrow). The acetabular bony rim is defined as the point on the lateral acetabular edge (low signal area) at which the curvature switches from concave to convex. Furthermore, the center of the labrum is defined as the center of the triangle (low signal area).
MRI scans were obtained under sedation using triclofos sodium (80 mg/kg of body weight). Patients were placed in a supine position with the hip in a neutral position. The 1.5-T Gyroscan ACSII MRI scanner (Philips, Best, The Netherlands) was used, and coronal T2∗-weighted images were obtained using the gradient echo method. We used the following scanning parameters: repetition time = 380 msec, time to echo = 13 msec, flip angle 20°, field of view = 250 mm, thickness = 3 to 5 mm, and matrix size 256 × 192.
2.5. Data collection
We compared the acetabular index and CE angle and the presence of avascular necrosis or break in Shenton line on radiographs at the time of MRI. We evaluated the presence of avascular necrosis using the Kalamchi and MacEwen classification.[17] To investigate the relationship between labral eversion and acetabular development, we compared the MRI β angle between the normal control, good, and poor outcome groups. We evaluated the cut-off value for the poor outcome group. We selected 20 of 45 hips and evaluated the interobserver and intraobserver reliability of the MRI β angle. The angles on radiographs and MRI scans were measured using the Picture Archiving and Communication System (PSP Corp., Tokyo, Japan).
2.6. Statistical analysis
The Student t test was used to compare the quantitative variables between 2 groups. The Chi-square test was used to perform a ratio comparison. One-way analysis of variance was used to compare the quantitative variables among the 3 groups. The cut-off value was determined by identifying the point on the receiver operating characteristic curve (ROC curve) at which the specificity was greater.[18] Intraobserver and interobserver reliabilities of the MRI β angle were investigated using the interclass correlation coefficient (ICC). Statistical analyses were performed using SPSS software, version 23 (SPSS Inc., Chicago, IL), and the statistical significance value was P < .05.
3. Results
There were 26 hips (58%) in the good outcome group (Severin I, n = 19; Severin II, n = 7) and 19 hips (42%) in the poor outcome group (Severin III, n = 18; Severin IV, n = 1). Diagnoses and the initial treatment of patients are summarized in Table 1. There were 18 hips in the normal control group. Baseline characteristics of the 2 groups are summarized in Table 2. There was no significant difference between the 2 groups in terms of the age at reduction, MRI evaluation, and the final follow-up; ratio of left to right; dislocation to subluxation and acetabular dysplasia; open reduction versus other treatments, or the female-to-male ratio.
Table 1.
Diagnoses and initial treatment of patients.

Table 2.
Baseline characteristics of the good outcome group and poor outcome group.

3.1. Comparison of the radiographic parameters between the good and poor outcome groups
Results of the radiographic parameters at the time of the MRI examination between the 2 groups are summarized in Table 3. Although there was a significant difference in the CE angle, there was no significant difference in the acetabular index and the ratio of the presence of femoral head necrosis or break in Shenton line between the 2 groups.
Table 3.
Comparison of radiographic parameters between the good outcome group and poor outcome group.

3.2. MRI β angle in the normal control, good, and poor outcome groups and the cut-off value
We were able to identify the labrum in all patients as a low signal area on coronal T2∗-weighted images. MRI β angles in the normal control, good outcome, and poor outcome groups are shown in Fig. 2. The average MRI β angles were 41.8 ± 14.5°, 52.5 ± 11.3°, and 65.8 ± 9.9° for the normal control, good outcome, and poor outcome groups, respectively. The MRI β angle was increasingly large in the normal control, good outcome, and poor outcome groups, and there were significant differences among all 3 groups. The ROC curve between the good and poor outcome groups is shown in Fig. 3. The cut-off value of the MRI β angle to differentiate between the good and poor outcome groups was 65°, and its specificity and sensitivity were 92% and 53%, respectively. The area under the curve was 0.81.
Figure 2.

Comparison of β angles on magnetic resonance imaging (MRI) scans among the normal control, good outcome, and poor outcome groups. Error bars indicate the average and standard deviation.
Figure 3.

Receiver operating characteristic (ROC) curve based on each value of β angles on magnetic resonance imaging (MRI) scans. Left: We consider the data point of 65° (arrow) on the ROC curve as the cut-off value to differentiate the good and poor outcome groups. Right: The scatter plots show the data for each group. The line indicates the cut-off line.
3.3. Reliability of the MRI β angle.
Intraobserver and interobserver reliabilities of the MRI β angle are summarized in Table 4. The ICCs indicate high intraobserver and interobserver reliabilities.
Table 4.
Intraobserver and interobserver reliability of ß angle on MRI scans.

4. Discussion
Omeroğlu et al[19] reported that accurately determining indications for corrective operations based solely on radiographs is difficult for even experienced pediatric orthopedic surgeons, and they tend to opt for nonoperative management. Our study's results showed that 19 of 45 hips (42%) conservatively treated for RHD had a poor outcome at the time of the final follow-up, supporting the results of study by Omeroğlu et al.[19] Furthermore, we did not find significant differences in the acetabular index and the ratio of the presence of femoral head necrosis or the break in Shenton line between the good and poor outcome groups at about 3 and 4 years of age in patients with RHD. This finding suggests that there is a limitation to predicting the acetabular development before school age based only on the osseous radiographic appearance, indicating the need for evaluations of soft tissue. Graf reported that the labrum is important for evaluating acetabular development.[20] Thus, we evaluated the labrum using MRI in this study.
Pauwels et al[21] described the biomechanics of the hip joint, particularly that the progression of acetabular dysplasia allows loading forces to push the femoral head upward and laterally. Klaue et al[22] reported that instability of the femoral head in these directions increases stress on the labrum in patients with acetabular dysplasia. Kim et al[23] also evaluated the labrum using MRI, and they reported that eversion of the labrum in patients with RHD was greater than that in those with normal hips. The MRI β angle in our study reflects eversion of the labrum, including the acetabular cartilage, and we found a significant difference in the CE angle and MRI β angle between the good and poor outcome groups. These results indicate that lateral shifting contributes to hip instability by placing excessive stress on the labrum from the femoral head, resulting in the eversion of the labrum and an increase in the MRI β angle.
Bittersohl et al[24] explained that stress concentration occurs at the lateral acetabulum in acetabular dysplasia, and Siffert[25] reported that this stress concentration prevents acetabular development. Thus, stress concentration at the lateral edge of the acetabulum may be related to poor acetabular developmental in patients with RHD. In an animal model study, Kim [26] showed that artificial eversion of the labrum evoked acetabular dysplasia and subluxation, causing degeneration of the acetabular cartilage. Therefore, labral disorders can cause developmental degeneration in the acetabular cartilage. Our study's results also showed that the MRI β angle in the poor outcome group was greater than that in the normal control and good outcome groups for patients with RHD. Existing knowledge and our finding suggest that a greater MRI β angle reflects greater shear forces in the labrum, which can cause impairment in the labrum and stress concentration at the adjacent acetabular cartilage, leading to inhibition of the acetabular development.
The strength of this study was that we evaluated hip biomechanics in patients with RHD before school age with a focus on the extent of labrum eversion on MRI scan, and we investigated its relationship with acetabular development. According to our study's results, the specificity for a poor outcome was 92% with an MRI β angle of 65° or more. This means that 92% of patients with RHD with good acetabular development before adolescence did not have an MRI β angle of 65° or more at approximately 3 years old. This finding can be generalized as an adjuvant indicator to predict acetabular development when determining the indication for corrective operation before school age. Furthermore, we may be able to measure the MRI β angle in patients with RHD with less invasive ultrasonography. The MRI β angle can be measured with ultrasonography from a lateral approach in patients after the femoral head ossific nucleus appears. Considering the possible application of ultrasonography, we measured the MRI β angle using ultrasonographic landmarks.
The biggest disadvantage of MRI in childhood is that it requires sedation, which carries the risk of cardiorespiratory disorders. However, a recent study demonstrated the use of Ultrafast MRI without sedation in infants by using a special sequence and equipment.[27] We believe that selective MRI and our MRI finding add value with the increased use of safe MRI without sedation.
Our study has several limitations. First, the follow-up period was short. A longer follow-up until bone maturity is required. However, Weinstein et al[28] reported that 8 years is the watershed age for acetabular development, as most of the acetabulum is formed by that age. We believe that most acetabular morphologies developed in our follow-up period. Second, there is a possibility of measurement error with the MRI β angle because of pelvic tilt and hip position, although we carefully conducted MRI scans in the same hip position. To more accurately evaluate the labrum, imaging methods that eliminate pelvic tilt, such as radial-sequence MRI, are necessary.[15,16] Thus, further investigations are needed in the future.
In conclusion, there was labral eversion on MRI scans of patients with RHD. The acetabular development before adolescence was poorer with greater labral eversion. The specificity for poor acetabular development was high when the MRI β angle was 65° or more. The MRI β angle has the potential to predict acetabular development.
Footnotes
Abbreviations: CE angle = center-edge angle, ICC = interclass correlation coefficient, MRI β angle = β angle on magnetic resonance imaging scans, MRI = magnetic resonance imaging, RHD = residual hip dysplasia, ROC = receiver operating characteristic curve.
The authors have no conflicts of interest to disclose.
References
- [1].Salter RB. The classic. Innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip. J Bone Joint Surg Br 1961;43:518–39. [Google Scholar]
- [2].Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint. Acta Chir Scand 1939;83:1. [Google Scholar]
- [3].Albinana J, Dolan LA, Spratt KF, et al. Acetabular dysplasia after treatment for developmental dysplasia of the hip. Implications for secondary procedures. J Bone Joint Surg Br 2004;86:876–86. [DOI] [PubMed] [Google Scholar]
- [4].Hattori T, Ono Y, Kitakoji T, et al. Soft-tissue interposition after closed reduction in developmental dysplasia of the hip. The long-term effect on acetabular development and avascular necrosis. J Bone Joint Surg Br 1999;81:385–91. [DOI] [PubMed] [Google Scholar]
- [5].Kitoh H, Kitakoji T, Katoh M, et al. Prediction of acetabular development after closed reduction by overhead traction in developmental dysplasia of the hip. J Orthop Sci 2006;11:473–7. [DOI] [PubMed] [Google Scholar]
- [6].Nakamura J, Kamegaya M, Saisu T, et al. Treatment for developmental dysplasia of the hip. J Bone Joint Surg Br 2007;89:230–5. [DOI] [PubMed] [Google Scholar]
- [7].Dora C, Mascard E, Mladenov K, et al. Retroversion of the acetabular dome after Salter and triple pelvic osteotomy for congenital dislocation of the hip. J Pediatr Orthop B 2002;11:34–40. [DOI] [PubMed] [Google Scholar]
- [8].Robb CA, Datta A, Nayeemuddin M, et al. Assessment of acetabular retroversion following long term review of Salter's osteotomy. Hip Int 2009;19:8–12. [DOI] [PubMed] [Google Scholar]
- [9].Graf R. Classification of hip joint dysplasia by means of sonography. Arch Orthop Trauma Surg 1984;102:248–55. [DOI] [PubMed] [Google Scholar]
- [10].Crawford MJ, Dy CJ, Alexander JW, et al. The 2007 Frank Stinchfield Award. The biomechanics of the hip labrum and the stability of the hip. Clin Orthop Relat Res 2007;465:16–22. [DOI] [PubMed] [Google Scholar]
- [11].Song Y, Ito H, Kourtis L, et al. Articular cartilage friction increases in hip joints after the removal of acetabular labrum. J Biomech 2012;45:524–30. [DOI] [PubMed] [Google Scholar]
- [12].Ferguson SJ, Bryant JT, Ganz R, et al. An in vitro investigation of the acetabular labral seal in hip joint mechanics. J Biomech 2003;36:171–8. [DOI] [PubMed] [Google Scholar]
- [13].Wakabayashi K, Wada I, Horiuchi O, et al. MRI findings in residual hip dysplasia. J Pediatr Orthop 2011;31:381–7. [DOI] [PubMed] [Google Scholar]
- [14].Severin E. Contribution to the knowledge of congenital dislocation of the hip joint. Acta Chir Scand 1941;84:1–42. [Google Scholar]
- [15].Kubo T, Horii M, Harada Y, et al. Radial-sequence magnetic resonance imaging in evaluation of acetabular labrum. J Orthop Sci 1999;4:328–32. [DOI] [PubMed] [Google Scholar]
- [16].Horii M, Kubo T, Hachiya Y, et al. Development of the acetabulum and the acetabular labrum in the normal child: analysis with radial-sequence magnetic resonance imaging. J Pediatr Orthop 2002;22:222–7. [PubMed] [Google Scholar]
- [17].Kalamchi A, MacEwen GD. Avascular necrosis following treatment of congenital dislocation of the hip. J Bone Joint Surg Am 1980;62:876–88. [PubMed] [Google Scholar]
- [18].Zou KH, O’Malley AJ, Mauri L. Receiver-operating characteristic analysis for evaluating diagnostic tests and predictive models. Circulation 2007;115:654–7. [DOI] [PubMed] [Google Scholar]
- [19].Omeroğlu H, Ağuş H, Biçimoğlu A, et al. Evaluation of experienced surgeons’ decisions regarding the need for secondary surgery in developmental dysplasia of the hip. J Pediatr Orthop 2012;32:58–63. [DOI] [PubMed] [Google Scholar]
- [20].Graf R. The acetabular labrum in infants. Orthopade 1998;27:670–4. [PubMed] [Google Scholar]
- [21].Pauwels F, Furlong RJ, Maquet P. Biomechanics of the Normal and Diseased Hip: Theoretical Foundation, Technique and Results of Treatment: an Atlas. New York: Springer; 1976. [Google Scholar]
- [22].Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. J Bone Joint Surg Br 1991;73:423–9. [DOI] [PubMed] [Google Scholar]
- [23].Kim HT, Kim IB, Lee JS. MR-based parameters as a supplement to radiographs in managing developmental hip dysplasia. Clin Orthop Surg 2011;3:202–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Bittersohl B, Hosalkar HS, Wenger DR. Surgical treatment of hip dysplasia in children and adolescents. Orthop Clin North Am 2012;43:301–15. [DOI] [PubMed] [Google Scholar]
- [25].Siffert RS. Patterns of deformity of the developing hip. Clin Orthop Relat Res 1981. 14–29. [PubMed] [Google Scholar]
- [26].Kim YH. Acetabular dysplasia and osteoarthritis developed by an eversion of the acetabular labrum. Clin Orthop Relat Res 1987. 289–95. [PubMed] [Google Scholar]
- [27].Fukuda A, Fukiage K, Futami T, et al. 1.0 s Ultrafast MRI in non-sedated infants after reduction with spica casting for developmental dysplasia of the hip: a feasibility study. J Child Orthop 2016;10:193–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Weinstein SL, Mubarak SJ, Wenger DR. Fundamental concepts of developmental dysplasia of the hip. Instr Course Lect 2014;63:299–305. [PubMed] [Google Scholar]


