Abstract
Pediatric human immunodeficiency virus (HIV) infection and malnutrition are still 2 major health issues in sub-Saharan Africa including Burkina Faso where few studies have been conducted on child malnutrition and HIV infection. This study assessed the effects of antiretroviral therapy (ART) in HIV infection and also compared the prevalence of malnutrition in terms of an inadequate diet, underweight, stunting, and wasting among HIV-infected and uninfected children less than 5 years in Bobo-Dioulasso city, Burkina Faso.
This was a case–control study matching for age and sex in 164 HIV-infected and 164 HIV-uninfected children. The sociodemographic characteristics of mothers and children, household food security, drinking water source, child feeding and care practices, and child anthropometric data such as body weight, height, and mid-upper arm circumference were collected.
The prevalence of food insecurity and inadequate diet was 58% and 92% of children less than 5 years of age, respectively. The prevalence of underweight, stunting, and wasting was 77% versus 35%, 65% versus 61%, and 63% versus 26% in HIV-infected and uninfected children less than 5 years of age, respectively. Out of 164 HIV-infected children, 59% were on ART initiation during data collection and the median of CD4 cell counts was 1078 cells/μL. HIV-infected children on ART had greater CD4 cell counts (P = .04) and higher weight-for-age Z (P = .01) and weight-for-height Z scores (P = .03) than those without ART. HIV infection was a risk factor for those who had inadequate dietary intake [adjusted odds ratio (AOR) = 2.17, 95% confidence interval (CI) 1.17–3.62, P = .04]. In addition, HIV-infected children were more likely of being underweight (AOR = 10.24, 95% CI 4.34–24.17, P < 0.001) and wasting (AOR = 5.57, 95% CI 2.49–12.46, P < 0.001) than HIV-uninfected children less than 5 years of age.
High prevalence of malnutrition was observed in HIV-infected children compared with HIV-uninfected children. Except for ART, nutritional assessment and support should be included in pediatric HIV management.
Keywords: Burkina Faso, children less than 5, HIV infection, malnutrition
1. Introduction
Pediatric HIV infection and malnutrition are 2 major health issues in sub-Saharan Africa.[1,2] In 2015, an estimated 1.8 million children under 15 years were living with HIV, and approximately 90% of these children lived in sub-Saharan Africa.[3] The majority of children were infected with HIV due to the transmission from HIV-infected mothers during pregnancy, delivery, or breastfeeding.[3] In addition to HIV infection in sub-Saharan Africa, underweight, stunting, and wasting were present among 21 million, 28 million, and 14 million children less than 5 years of age, respectively.[4]
HIV infection and malnutrition often coexist in children, and malnutrition is a major problem for HIV-infected children.[5,6] The risk for malnutrition was significantly higher in HIV-infected children than in HIV-uninfected children.[7] Malnutrition also increased the frequency and severity of infection and delayed recovery from disease.[4,8] The previous studies showed that HIV infection was associated with increased undernutrition among children.[6,9–11]
In Burkina Faso, although the Program for the Prevention of Mother-to-Child Transmission of HIV has been implemented since 2002, HIV/AIDS is still accounted for 4% of deaths in children.[12] In 2015, an estimated 7700 children aged 0 to 14 years were living with HIV.[13] Out of 7700 HIV-infected children, 2293 (30%) children were on antiretroviral therapy (ART) including 291 (4%) registered at a teaching hospital in Bobo-Dioulasso. More than half of children (167, 57%) among these 291 children were less than 5 years of age, and almost all presented moderate or severe acute malnutrition.[14] Although there is no cure for HIV infection, effective ART can control the virus and help prevent transmission. Early initiation of ART was associated with decreased opportunistic infections and HIV loads, which lead to a positive health status with prolonged life, especially in younger children.[2,7]
Several studies have been conducted on child malnutrition in Burkina Faso, but these studies have not compared the impact of malnutrition among HIV-infected children and uninfected children less than 5 years of age. Two national health and nutrition surveys were conducted in 2010 and 2015, but these 2 surveys did not include nutritional status in HIV-infected children. The Demographics Health survey (DHS) in 2010 and the national nutrition surveys in 2015 demonstrated that 26% versus 24%, 35% versus 37%, and 16% versus 10% of children less than 5 years of age suffered from underweight, stunting, and wasting, respectively, in Burkina Faso.[14,15] The previous studies have mainly focused on the prevalence or risk factors of malnutrition among children in different parts of Burkina Faso.[14–19] Only a few studies assessed the effects of HIV infection on mortality and nutritional status with or without supplement among undernourished children in Burkina Faso.[20,21] Therefore, the objective of this study investigated the effects of HIV infection on malnutrition in terms of inadequate dietary intake, underweight, stunting, and wasting among children less than 5 years of age in Bobo Dioulasso city, Burkina Faso.
2. Methods
2.1. Study design
This was a case–control study matching for age and sex of HIV-infected and uninfected children less than 5 years of age. Independent variables including age of the child (in months), sex of the child, maternal education, religion and marital status, family income, percentage of income spent on foods, information provided to mother regarding child nutrition or care, food security, water source, child feeding practices, and child health status were investigated. Dependent variables including dietary intake score, underweight or weight-for-age (WAZ), stunting or height-for-age (HAZ), and wasting or weight-for-height (WHZ) were determined.
2.2. Study setting and participants
This study was carried out at 1 teaching hospital and 2 health districts[14] in Bobo Dioulasso city in Burkina Faso. At the end of 2014, the number of HIV-infected children less than 5 years of age was 172 at Souro Sanou Teaching Hospital. A total of 164 HIV-infected children aged 12 to 58 months as the case group were recruited at Souro Sanou Teaching Hospital from July to September 2014, and 164 HIV-uninfected children extracted form 426 HIV-uninfected children aged 12 to 59 months as the control group were recruited at 2 health districts Dafra and Do in Bobo Dioulasso City from July to September 2015. This study minimized the selection biases by using matching methods and recruiting the subjects from the same geographic area, Bobo Dioulasso City in Burkina Faso. The control group was matched 1:1 for age (±1 month) and sex with the HIV-infected children. There were 48% (n = 156) aged from 12 to 24 months and 52% (n = 172) aged from 25 to 58 months among 328 children less than 5 years of age. The participants were 52% (n = 170) female and 48% (n = 158) male.
2.3. Ethical considerations
This study used the data from 2 previous studies related to malnutrition among HIV-infected and uninfected children less than 5 years of age, which were approved by the Institutional Review Board of Burkina Faso National Ethics Committee for Health Research in 2014 (No. 2014-1794/MS/SG/DGS/DN) and 2015 (No. 2015-2400/MS/SG/DGS/DN). Written informed consent was obtained from the mothers.
2.4. Data collection and measurements
The demographic information and measurements were collected from July to September 2014 and from July to September 2015, respectively, in HIV-infected and uninfected children. The questionnaires as the research instrument developed by Sunguya et al[11] were adapted and administered in this study, and completed by the mothers. Child anthropometric data such as body weight, height, and mid-upper arm circumference (MUAC) were measured.
Dietary intake in the past month was determined by food frequency questionnaire that was completed by the mothers. In food frequency questionnaire, 7 categories of food groups were cereal grains (millet or maize, rice, and wheat products), root vegetables (Irish potato, sweet potato, and yam), legumes (beans and peanuts), vegetables (green leafy vegetables, tomato, pumpkin, carrot, and onion), fruits (orange, mango, papaya, banana, pineapple, and avocado), dairy products (milk and cream), and animal products (meat, pork, poultry, fish, and eggs). To quantify dietary intake in children, a score from 0 to 5 was given for each food item in 7 food categories according to intake frequency; 0 indicates never or less than 1 day per month, 1 indicates 1 to 3 days per month, 2 indicates 1 day per week, 3 indicates 2 to 4 days per week, 4 indicates 5 to 6 days per week, and 5 indicates 7 days per week. The total score for each food category was determined by the sum of scores of the corresponding food items. The maximum total scores for cereal grains, root vegetables, legumes, vegetables, fruits, dairy products, and animal products were 15, 15, 10, 25, 30, 10, and 25, respectively. The sum score of all 7 food categories ranged from 0 to 130, and the cutoff point was 65 in this study. A score above or below 65 was defined as adequate or inadequate dietary intake, respectively.
The anthropometric data including body weight, height, and MUAC were measured in kilograms (to the nearest 100 g) by using an electronic digital scale (Seca model 770; Seca, Hamburg, Germany), a stadiometer with a precision of 0.1 cm, and an anthropometric tape (to the nearest centimeter), respectively. The height of children less than 2 years of age was measured in a recumbent position.[22] Body mass index (BMI) was calculated by the formula: body weight (kg)/height2 (m2). WHO Anthro3.2.2 software[23] was used to calculate weight-for-age Z (WAZ), height-for-age Z (HAZ), and weight-for-height Z (WHZ) scores, and the prevalence of malnutrition in terms of underweight, stunting, and wasting were determined. As compared with the WHO standard, WAZ, HAZ, and WHZ scores below -1 standard deviation (SD), below -2, and below -3 SD were defined as mild, moderate, and severe underweight, stunting, and wasting, respectively. The definitions from UNICEF-WHO-World Bank only included the subjects with moderate and severe underweight, stunting, and wasting.[24] In addition, more information such as ART and the immunological marker (CD4 cell counts) were collected among HIV-infected children.
2.5. Statistical analysis
The data were analyzed by SPSS 21 version (SPSS Inc., Chicago, IL) and WHO Anthro 3.2.2 version (WHO, Geneva, Switzerland). Shapiro–Wilk test was performed for the normality of anthropometric data and dietary intake. Nonparametric tests were used to analyze the data due to the normality test with P values greater than 0.05 for all of the variables. Chi-square test was used to describe the distribution between HIV-infected and uninfected children. Mann–Whitney U test was used to compare the median between the 2 groups. Logistic regression test was performed to assess the risk factors of malnutrition. Differences were considered statistically significant at P values less than .05.
3. Results
3.1. Characteristics of the subjects
The characteristics of the children and their mothers are summarized in Table 1. Among 328 subjects, more than 60% of mothers were Muslim (68%), married (70%), educated (77%), and received information on child nutrition and care (61%). The majority of the family (69%) had monthly income less than or equal to 100,000 CFA franc (approximately USD171); however, 62% of family spent 60% to 90% of income on foods. There were 58% of family under food insecurity and 60% of family with piped drinking water. There were 27% of children still under breastfeeding during the data collection phase and 54% of children breastfed for 18 to 24 months. In terms of health status, 73% of children were under fair or poor health status, and 62% of children had vitamin A supplement in the past 6 months.
Table 1.
Characteristics of HIV-infected and uninfected children less than 5 years of age and their mothers.
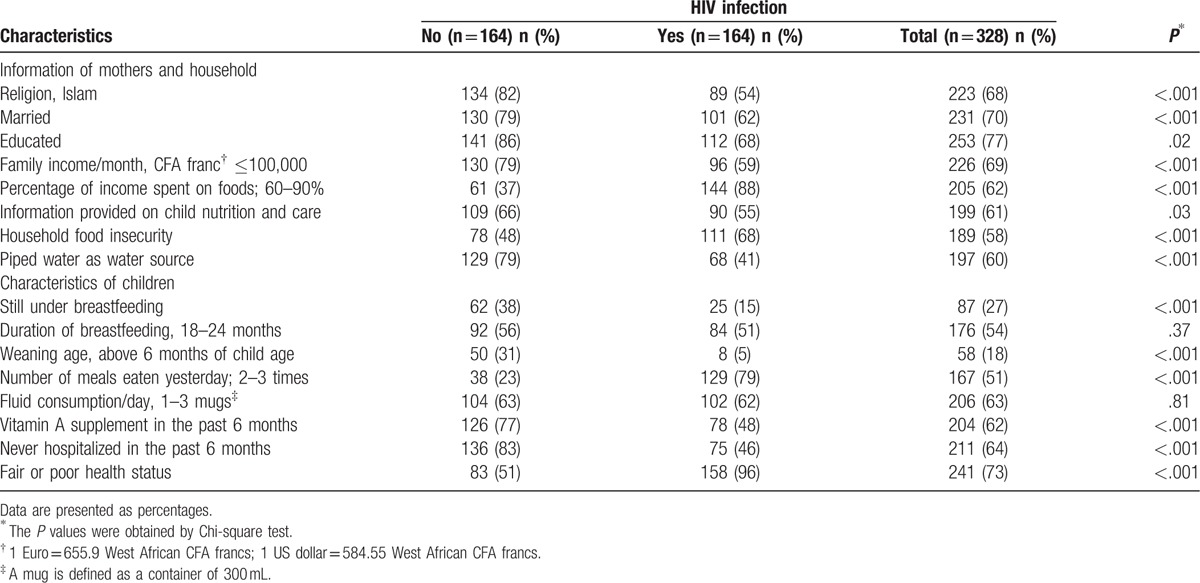
A higher proportion of HIV-infected children's mothers than uninfected children's mothers were Christian (46% vs 18%, P < .001), unmarried (38% vs 21%, P < .001), and without educated (32% vs 14%, P = .02). A higher proportion of HIV-infected children than uninfected children had family income spent on foods with 60% to 90% (88% vs 37%, P < .001). However, a lower proportion of HIV-infected children than uninfected children had food security (32% vs 52%, P < .001) and drank piped water (41% vs 79%, P < .001). A lower proportion of HIV-infected children than uninfected children were still under breastfeeding (15% vs 38%, P < .001), with weaning age at 7 to 9 months (5% vs 31%, P < .001), ate 4 to 7 meals yesterday (21% vs 77%, P < .001), and had vitamin A supplement in the past 6 months (48% vs 77%, P < .001). However, a higher proportion of HIV-infected children than uninfected children were hospitalized in the past 6 months (54% vs 17%, P < .001), and had fair or poor health status (96% vs 51%, P < .001).
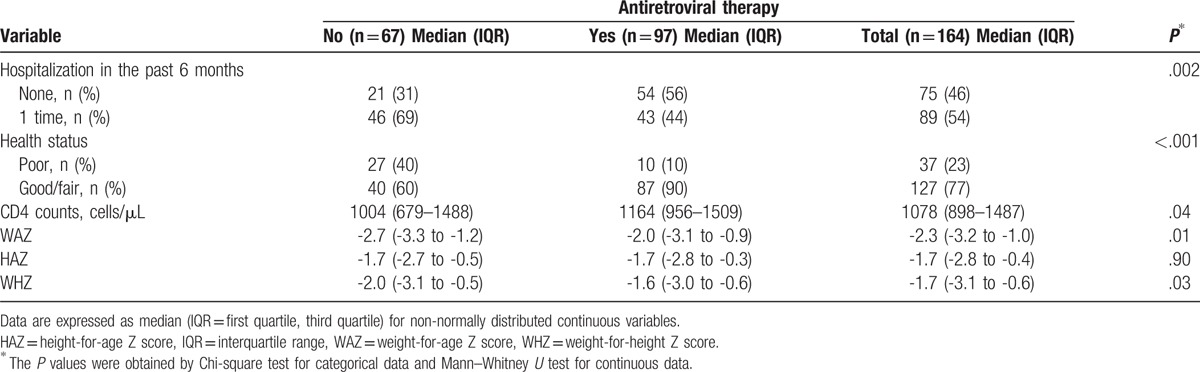
Among 164 HIV-Infected children less than 5 years of age, 59% were on ART initiation during data collection (Table 2). More children on ART were never hospitalized in the past 6 months compared with those without ART (56% vs 31%, P = .002). Similarly, more children on ART had fair or good health status compared with those without ART (90% vs 60%, P < .001). In addition, the children on ART had greater CD4 cell counts (1164 vs 1004 cells/μL, P = .04) and higher WAZ (-2.0 vs -2.7, P = .01) and WHZ scores (-1.6 vs -2.0, P = .03) than those without ART.
Table 2.
Antiretroviral therapy assessment in 164 HIV-infected children less than 5 years of age.
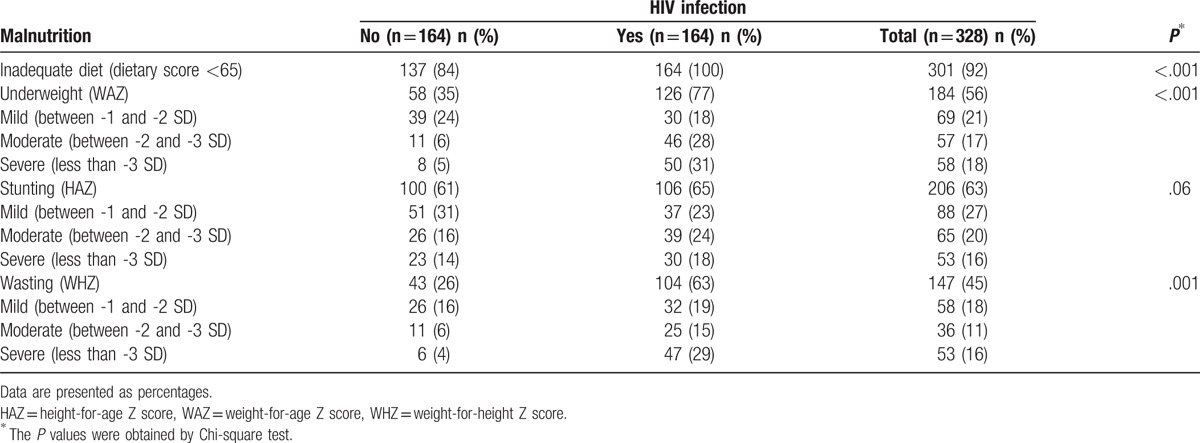
3.2. Prevalence of malnutrition
The prevalence of inadequate diet, underweight, stunting, and wasting was 92%, 56%, 63%, and 45%, respectively, among 328 children (Table 3). A higher proportion of HIV-infected children than uninfected children had an inadequate diet (100% vs 84%, P < .001), were underweight (77% vs 35%, P < .001) and wasting (63% vs 26%, P = .001). Nearly one-third HIV-infected children had severe underweight (31%) or severe wasting (29%); however, no more than 5% of HIV-uninfected children had severe underweight (5%) or severe wasting (4%).
Table 3.
Prevalence of malnutrition in HIV-infected and uninfected children less than 5 years of age in terms of inadequate dietary intake, underweight, stunting, and wasting.
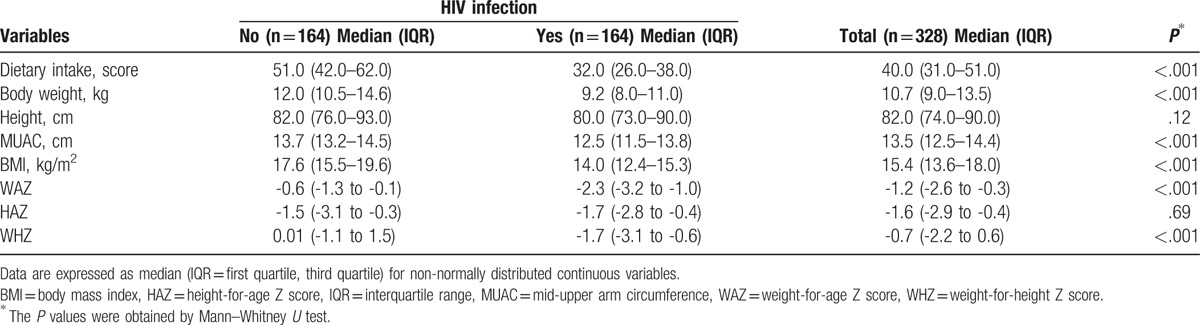
3.3. Comparison of dietary intake and anthropometric measures
Compared with HIV-uninfected children, HIV-infected children less than 5 years of age had lower median dietary intake score (51.0 vs 32.0, P < .001), body weight (12.0 vs 9.2 kg, P < .001), MUAC (13.7 vs 12.5 cm, P < .001), BMI (17.6 vs 14.0 kg/m2, P < .001), WAZ (-0.6 vs -2.3, P < .001), and HAZ (0.01 vs -1.72, P < .001) (Table 4).
Table 4.
Comparison of dietary intake and anthropometric measures between HIV-infected and uninfected children less than 5 years of age.
3.4. Association between HIV infection and nutritional status
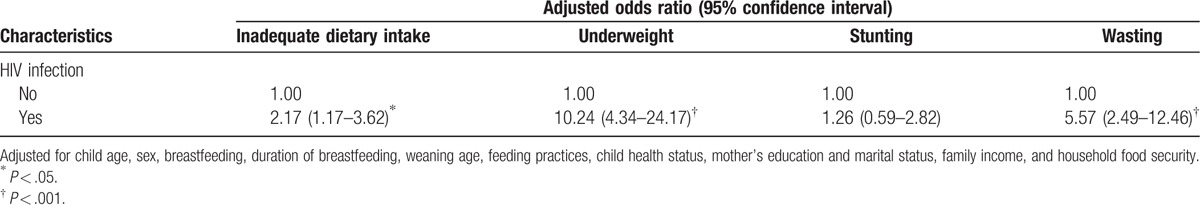
The adjusted odds ratios (AORs) of inadequate dietary intake, underweight, stunting, and wasting in HIV-infected children are summarized in Table 5. Compared with HIV-uninfected children, HIV-infected children had a higher risk for having inadequate dietary intake [AOR = 2.17, 95% confidence intervals (95% CIs) 1.17–3.62, P = .04]. In terms of anthropometric indicators, HIV-infected children were more likely of being underweight (AOR = 10.24, 95% CI 4.34–24.17, P < .001) and wasting (AOR = 5.57, 95% CI 2.49–12.46, P < .001) than HIV-uninfected children. However, stunting was not significantly associated with HIV infection (AOR = 1.26, 95% CI 0.59–2.82, P = .51).
Table 5.
HIV infection associated with malnutrition in terms of inadequate dietary intake, underweight, stunting, and wasting in children less than 5 years of age.
4. Discussion
To our knowledge, this is the first study that has used dietary intake and anthropometric indicators to assess the nutritional status among HIV-infected and uninfected children in Burkina Faso. This study revealed a higher prevalence of malnutrition in terms of underweight and wasting in HIV-infected children and brought more evidence about the relationship between malnutrition and HIV infection. Consistently, the previous study reported that HIV-infected children were under poorer nutritional status in terms of anthropometric measures compared with age- and sex-matched HIV-uninfected children in Nigeria.[25] This study showed that anthropometric measures such as body weight, MUAC, and BMI were significantly lower in HIV-infected children than in HIV-uninfected children, suggesting that HIV-infected children need greater nutritional support.[7,26] This study also found poor dietary intake in HIV-infected children, which may be associated with a higher proportion of being underweight and wasting in HIV-infected children than in HIV-uninfected children. Similarly, the previous studies revealed that malnutrition was more prevalent in HIV-infected children than HIV-uninfected children.[27–31] A previous study confirmed that growth retardation and the deterioration of nutritional status in children were associated with HIV infection.[32] The previous studies in South Africa and Tanzania demonstrated that HIV infection was associated with an increased burden of child underweight and wasting,[33] even among ART-treated children.[11] Infection with HIV causes immune impairment and further leads to malnutrition that could contribute to increased mortality in children.[5,34]
In this study, 59% of HIV-infected children were on ART, which were higher than the rate of 24% in the world in 2014.[2] The possible reasons for the remaining 41% not on ART could be newly diagnosis of HIV infection, shortage of ART, and inadequate or lack of medical human resources to provide ART to HIV-infected children. The findings of this study also showed that HIV-infected children on ART had greater CD4 counts and were less likely of being underweight and wasted, which contributing to better health status and less hospitalization. Consistent with the previous studies, ART exerted a favorable effect on growth [2,6,32] and immune functions.[35]
HIV infection and malnutrition may interact in complex ways that result in high vulnerability to infection and worse health status. The previous studies reported that food insecurity in HIV-positive households, greater nutritional needs, and coinfections such as gastroenteritis or pneumonia were the major contributing factors of malnutrition in children.[7,28,36] Although this study did not perform clinical assessment, most of the HIV-infected children experienced malnutrition and poor health status, which were consistent with the results of the frequency of hospitalization in HIV-infected children. This situation could be solved by early diagnosis, treatment, and care with nutritional support to improve the nutritional status of HIV-infected children.[1,28]
Dietary intake and anthropometric data were simultaneously used to assess nutritional status in this study instead of using only anthropometric measures that are often practiced in many developing countries. In addition, WHO Anthro3.2.2 was used to analyze anthropometric data and this study determined the prevalence of malnutrition by using WAZ, HAZ, and WHZ scores below -1, -2, or -3 SD to define mild, moderate, or severe underweight, stunting, and wasting, respectively. Whereas the previous studies investigated malnutrition in children by only covering moderate and severe underweight, stunting, and wasting using UNICEF-WHO-World Bank report and National Nutrition survey in Burkina Faso.[6,11,17,24] Child nutrition assessment usually includes anthropometric, biochemical, clinical, and dietary assessment. However, this study did not include biochemical data and clinical examination to compare malnutrition between HIV-infected and uninfected children.
The findings of this study confirm that malnutrition is more common in HIV-infected children than in HIV-uninfected children. HIV-infected children have significantly higher risk of having inadequate dietary intake, being underweight and wasting. However, ART was associated with improved outcomes in HIV-infected children. The early screening of malnutrition and more nutrition intervention should be involved for pediatric HIV management.
Acknowledgments
We would like to acknowledge the Pediatrics Department at Souro Sanou Teaching Hospital, the health staffs from the 2 districts in Bobo-Dioulasso city, the staffs at the HIV/AIDS Association Center for their support and assistance, and all HIV-infected children and uninfected children with their mothers who participated in this study. We also express our gratitude to Taipei Medical University for offering a scholarship to the first author for his research toward a PhD degree.
Footnotes
Abbreviations: AOR = adjusted odds ratios, CI = confidence interval, HIV = human immunodeficiency virus.
Authorship: GGP, CYH, and JCJC conceptualized the study and were responsible for the statistical analysis. CYH and JCJCJ revised all parts of the manuscript. All authors approved the final version of the manuscript.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Jesson J, Koumakpaï S, Diagne NR, et al. Effect of age at antiretroviral therapy initiation on catch-up growth within the first 24 months among HIV-infected children in the IeDEA West African Pediatric Cohort. Pediatr Infect Dis J 2015;34:e159–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Jesson J, Leroy V. Challenges of malnutrition care among HIV-infected children on antiretroviral treatment in Africa. Med Mal Infect 2015;45:149–56. [DOI] [PubMed] [Google Scholar]
- [3].UNICEF 2016. HIV/AIDS Global and Regional Trends. Available at: http://data.unicef.org/hiv-aids/global-trends.html. Accessed September 14, 2016. [Google Scholar]
- [4].UNICEF 2016. Malnutrition: Current Status and Progress. Available at: http://data.unicef.org/nutrition/malnutrition.html. Accessed September 14, 2016. [Google Scholar]
- [5].Duggal S, Chugh TD, Duggal AK. HIV and malnutrition: effects on immune system. Clin Dev Immunol 2012;2012:784740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Jesson J, Masson D, Adonon A, et al. Prevalence of malnutrition among HIV-infected children in Central and West-African HIV-care programmes supported by the Growing Up Programme in 2011: a cross-sectional study. BMC Infect Dis 2015;15:216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Rose AM, Hall CS, Martinez-Alier N. Aetiology and management of malnutrition in HIV-positive children. Arch Dis Child 2014;99:546–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Lodha R, Kabra SK. Health & nutritional status of HIV infected children. Indian J Med Res 2015;141:10–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Feucht UD, Van Bruwaene L, Becker PJ, et al. Growth in HIV-infected children on long-term antiretroviral therapy. Trop Med Int Health 2016;21:619–29. [DOI] [PubMed] [Google Scholar]
- [10].Swetha GK, Hemalatha R, Prasad UV, et al. Health & nutritional status of HIV infected children in Hyderabad, India. Indian J Med Res 2015;141:46–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Sunguya BF, Poudel KC, Otsuka K, et al. Undernutrition among HIV-positive children in Dar es Salaam, Tanzania: antiretroviral therapy alone is not enough. BMC Public Health 2011;11:869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Burkina Faso Ministry of Health. National Health Development Plan 2011-2020. Ministry of Health, Burkina Faso: Ouagadougou; 2011. [Google Scholar]
- [13].UNAIDS. Burkina-Faso HIV and AIDS Estimates, 2015. Available at: http://www.unaids.org/en/regionscountries/countries/burkinafaso. Accessed December 6, 2016. [Google Scholar]
- [14].Burkina Faso Ministry of Health. 2015 Statistical Yearbook of the Ministry of Health. Ouagadougou: Ministry of Health, Burkina Faso; 2016. [Google Scholar]
- [15].Burkina Faso National Institute of Statistics and Demography (INSD). ICF International Demographic and Health Survey and Multiple Indicator of Burkina Faso 2010. Calverton: INSD and ICF International; 2012. [Google Scholar]
- [16].Beiersmann C, Bermejo Lorenzo J, Bountogo M, et al. Malnutrition determinants in young children from Burkina Faso. J Trop Pediatr 2013;59:372–9. [DOI] [PubMed] [Google Scholar]
- [17].Burkina Faso Ministry of Health. National Nutrition Survey. Ouagadougou: Ministry of Health, Burkina Faso; 2012. [Google Scholar]
- [18].Beiersmann C, Bountogo M, Tiendrébeogo J, et al. Malnutrition in young children of rural Burkina Faso: comparison of survey data from 1999 with 2009. Trop Med Int Health 2012;17:715–21. [DOI] [PubMed] [Google Scholar]
- [19].Douamba Z, Martinetto M, Pietra V, et al. Effects of a cereal and soy dietary formula on rehabilitation of undernourished children at Ouagadougou, in Burkina Faso. J Nutr Metab 2012;2012:764504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Savadogo LGB, Donnen P, Kouéta F, et al. Impact of HIV/AIDS on mortality and nutritional recovery among hospitalized severely malnourished children before starting antiretroviral treatment. Open J Pediatr 2013;3:340–5. [Google Scholar]
- [21].Simpore J, Zongo F, Kabore F, et al. Nutrition rehabilitation of HIV-infected and HIV-negative undernourished children utilizing spirulina. Ann Nutr Metab 2005;49:373–80. [DOI] [PubMed] [Google Scholar]
- [22].World Health Organization. WHO Child Growth Standards: Training Course on Child Growth Assessment. Geneva: WHO; 2008. [Google Scholar]
- [23].World Health Organization. WHO Anthro Version 3.2.2 and Macros. Geneva: WHO; 2011. Available at: http://softadvice.informer.com/ext/www.who.int/childgrowth%2Fsoftware%2Fen. Accessed 18 December, 2015. [Google Scholar]
- [24].United Nations Children's Fund, World Health Organization, The World Bank. UNICEFWHO-World Bank Joint Child Malnutrition Estimates. New York: UNICEF, Geneva: WHO, Washington, DC: The World Bank; 2012. [Google Scholar]
- [25].Akintan PE, Akinsulie AO, Temiye E, et al. Anthropometric measurements of HIV-infected children aged one to five years in a tertiary hospital in Lagos Nigeria. Niger J Paed 2016;43:26–9. [Google Scholar]
- [26].World Health Organization. Guidelines for an Integrated Approach to the Nutritional Care of HIV-Infected Children (6 months-14 years): Handbook, Chart booklet and Guideline for Country Adaptation. Geneva: WHO; 2009. [PubMed] [Google Scholar]
- [27].Anyabolu HC, Adejuyigbe EA, Adeodu OO. Undernutrition and anaemia among HAART-naïve HIV infected children in Ile-Ife, Nigeria: a case-controlled, hospital based study. Pan Afr Med J 2014;18:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Asafo-Agyei SB, Antwi S, Nguah SB. HIV infection in severely malnourished children in Kumasi, Ghana: a cross-sectional prospective study. BMC Pediatr 2013;13:181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Fergusson P, Chinkhumba J, Grijalva-Eternod C, et al. Nutritional recovery in HIV-infected and HIV-uninfected children with severe acute malnutrition. Arch Dis Child 2009;94:512–6. [DOI] [PubMed] [Google Scholar]
- [30].Bachou H, Tylleskär T, Downing R, et al. Severe malnutrition with and without HIV-1 infection in hospitalised children in Kampala, Uganda: differences in clinical features, haematological findings and CD4+ cell counts. Nutr J 2006;5:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Angami K, Reddy SV, Singh KhI, et al. Prevalence of HIV infection and AIDS symptomatology in malnourished children: a hospital based study. J Commun Dis 2004;36:45–52. [PubMed] [Google Scholar]
- [32].Gómez GEM, Maldonado CME, Rojas LM, et al. Association between intracellular zinc levels and nutritional status in HIV-infected and uninfected children exposed to the virus. Rev Chil Pediatr 2015;86:103–11. [DOI] [PubMed] [Google Scholar]
- [33].Schaaf HS, Cilliers K, Willemse M, et al. Nutritional status and its response to treatment of children, with and without HIV infection, hospitalized for the management of tuberculosis. Paediatr Int Child Health 2012;32:74–81. [DOI] [PubMed] [Google Scholar]
- [34].Rytter MJ, Kolte L, Briend A, et al. The immune system in children with malnutrition: a systematic review. PLoS One 2014;9:e105017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Wolf ER, Beste S, Barr E, et al. Health outcomes of international HIV-infected adoptees in the US. Pediatr Infect Dis J 2016;35:422–7. [DOI] [PubMed] [Google Scholar]
- [36].Chisti MJ, Ahmed T, Pietroni MA, et al. Pulmonary tuberculosis in severely-malnourished or HIV-infected children with pneumonia: a review. J Health Popul Nutr 2013;31:308–13. [DOI] [PMC free article] [PubMed] [Google Scholar]


