Abstract
Objectives
To assess the relationship between self-reported adherence to a gluten-free diet (GFD) and the ability to determine correctly the appropriateness of particular foods in a GFD.
Research Methods & Procedures
Persons with celiac disease were recruited through clinics and support groups. Participants completed a questionnaire with items related to GFD information sources, gluten content of 17 common foods (food to avoid, food allowed, food to question), GFD adherence and demographics. Diagnosis was self-reported.
Results
The 82 respondents (88% female) had a median of 6 years GFD experience. Most (55%) reported strict adherence, 18% reported intentional gluten consumption and 21% acknowledged rare unintentional gluten consumption. Cookbooks, advocacy groups and print media were the most commonly used GFD information sources (85–92%). No participant identified correctly the gluten content of all 17 foods; only 30% identified at least 14 foods correctly. The median score on the Gluten-Free Diet Knowledge Scale (GFD-KS) was 11.5 (IQR 10–13). One in five incorrect responses put the respondent at risk of consuming gluten. GFD-KS scores did not correlate with self-reported adherence or GFD duration. Patient advocacy group members scored significantly higher on the GFD-KS than non-members (12.3 vs. 10.6; p<0.005).
Conclusions
Self-report measures which do not account for the possibility of unintentional gluten ingestion overestimate GFD adherence. Individuals who believe they are following a GFD are not readily able to correctly identify foods that are GF, which suggests ongoing gluten consumption may be occurring, even among patients who believe they are “strictly” adherent. The role of patient advocacy groups and education to improve outcomes through improved adherence to a GFD requires further research.
Keywords: Celiac Disease; diet, gluten-free; Health Knowledge, Attitudes, Practice; Health Literacy; Information seeking behavior; Patient compliance; Self-assessment; Self-Help Groups
Introduction
Celiac disease and dermatitis herpetiformis are chronic autoimmune conditions treated by elimination of all sources of dietary gluten[1,2]. Following a gluten-free diet (GFD) is challenging and although most patients self-report strict dietary adherence, a significant number have persistent mucosal damage two years after starting a GFD[3]. Even in the absence of symptoms, persistent mucosal damage is clinically significant because it is associated with greater risk of severe complications of celiac disease, including malignancy[4], as well as with increased all-cause mortality[3]. Reasons for persistent mucosal damage are likely multi-factorial. Potential reasons include occult gluten ingestion due to lack of awareness of gluten content of foods[5], contamination of allegedly gluten-free foods[6,7] and factors intrinsic to underlying celiac disease and its natural history[8,9].
Gluten ingestion due to lack of awareness of the gluten content of foods may be a significant issue for many individuals, but has the potential to be modified. Determining whether a food contains gluten is challenging. Gluten is a component of many ingredients, thus it is often not explicitly listed on product labels. Within specific food categories (e.g., potato chips), certain brands may be gluten-free while others may contain trace amounts of gluten and thus should be avoided[10]. Even within a brand, some flavors may contain gluten while others are gluten-free. The products available and the composition of particular products also changes. For example, some companies have adjusted the recipe for popular breakfast cereals to offer gluten-free versions[11]. For these reasons, following a gluten-free diet is a dynamic process that requires continuous review and reassessment.
Patients with celiac disease use many different information sources to learn about gluten-free diets[12]. These include experts (e.g., dietitians, nutritionists, and physicians), the internet, patient support groups, and print media. There is no standardized education source for individuals requiring a GFD. Whatever the source of a patient’s technical information about gluten-free diets, this knowledge must be applied to the practical daily decisions of what to eat and, equally important, what not to eat. In practice, GFD knowledge is frequently applied in the context of attention to the content of processed foods. There have been few studies that have assessed GFD knowledge or evaluated its relationship to self-reported adherence[13,14]. This has particular clinical relevance as misunderstandings regarding the gluten content of foods could account for (unrecognized) gluten exposure and persistent mucosal damage[5].
Efforts to maintain a stringent GFD are tempered by practical, cultural, and social realities. Individuals may choose to avoid any products that ‘potentially’ contain gluten, thereby eliminating many common foods from their diet. This may result in adverse effects such as social isolation[15,16] or specific nutrient insufficiencies. This contrasts with the exponential increase in availability and diversity of gluten-free foods. Consequently, individuals trying to follow a GFD must balance vigilant avoidance of gluten containing products with awareness of new gluten-free foods as well as of alternate grains (which may or may not contain gluten) which were not previously available.
In this study, we aimed to assess the relationship between self-reported GFD adherence and the ability to determine correctly the appropriateness of particular foods in a GFD among a community sample of individuals with celiac disease and/or dermatitis herpetiformis trying to follow a GFD.
Methods
From October 2011 through October 2012, adults trying to follow a GFD were recruited through the local celiac support group, specialist clinics and advertisements at retail locations specializing in gluten-free products. Interested individuals accessed an anonymous online questionnaire. This study includes adults who reported following a GFD for a medical diagnosis of celiac disease or dermatitis herpetiformis. The questionnaire included items related to personal demographics, medical history, diet, sources of information about gluten-free diets, and the gluten content of foods (see supplementary information).
Gluten-Free Eating Assessment Tool (GF-EAT)
Adherence to a gluten-free diet was self-reported. Specifically, respondents chose one of eight descriptors which best characterized their current diet. The descriptors were: 1) Unrestricted diet; 2) Unrestricted gluten but other foods restricted; 3) Gluten-free diet sometimes; 4) Gluten-free diet most of the time; 5) Trying to follow a gluten-free diet but not always sure. 6) Usually gluten-free with rare intentional gluten consumption; 7) Usually gluten-free with rare unintentional gluten consumption; 8) Strict gluten-free diet. “Strict adherers” were defined as those who self-reported strict adherence to a gluten-free diet whereas all other respondents were considered to be “gluten-exposed”.
Sources of Gluten-free Diet Information
Participants were asked about their use of ten information sources to learn about gluten-free diets. For each information source, participants either rated the quality of the information obtained using a scale ranging from 1 (poor) to 5 (excellent) or indicated that they did not use this information source.
Gluten-Free Diet Knowledge Scale (GFD-KS)
Participants completed the GFD-KS by categorizing particular foods as “allowed” (i.e., gluten-free), “foods to question” (i.e., potentially containing gluten) or “not allowed” (i.e., certainly contain gluten) in a GFD. The GFD-KS was developed by an expert panel consisting of a gastroenterologist, dietitian and persons with celiac disease. Foods were chosen to include those that may be consumed on their own and/or appear on an ingredient list as a component of another food (e.g., milk) as well as complex foods which contain many ingredients with various recipes (e.g., sausages). Oatmeal was included because oats have recently been recognized as acceptable in a GFD[17,18]. The content was further revised following pretesting for readability and face validity by three members of the Canadian Celiac Association.
Correct classification of foods as “allowed”, “not allowed” or “foods to question” was determined by a specialist dietitian with expertise in gluten-free diets (DW) and verified by reviewing product labels at grocers and shops specializing in gluten-free products. The final list contained 17 foods: 7 foods allowed, 7 foods to question and 3 foods not allowed. One point was awarded for each correct answer for a maximum total score of 17. Over-restriction was defined as questioning foods “allowed” or not allowing foods “allowed” or “foods to question”. Under-restriction was defined as questioning or allowing foods “not allowed” or always allowing “foods to question”.
Statistical Analysis
Statistical analyses were performed using SPSS (version 15.0; SPSS Inc., Chicago, IL). Confidence intervals are typically reported in survey research and they are used here to facilitate comparisons across groups and across question items. The use of confidence intervals is recommended rather than pairwise significance tests because they help the reader focus on the magnitude of differences rather than simply concluding that a difference is statistically significant[19,20]. In making comparisons between means (between groups and across different question items) the reader should keep in mind that in 1 case out of 20 confidence intervals will be non-overlapping by chance.
Odds ratios (OR) and 95% confidence intervals (CI) were calculated using the method of Cochran and Mantel-Haensel. Pearson correlations were performed to describe the relationships between GFD-KS scores and years on a GFD. All statistical tests were two-sided with a p-value less than 0.05 considered significant.
The study protocol was approved by the University of Manitoba Health Research Ethics Board. Completion of the anonymous survey constituted informed consent to participate in the research.
Results
Of the 82 participants who completed the questionnaire, 76 had celiac disease and 6 had both celiac disease and dermatitis herpetiformis (Table 1). The majority (88%) were female and most were older than 55 years of age. Median GFD duration was 6.0 years (IQR 2–10 years).
Table 1.
Participant characteristics
| Strict GFD (n = 45) | Gluten Exposure (n= 37) | |
|---|---|---|
| Age | ||
| < 35 years | 22% | 17% |
| 35–55 years | 20% | 31% |
| > 55 years | 58% | 52% |
| Gender (% female) | 91% | 81% |
| Duration of GFD [years median (IQR)] | 6 (3–13) | 5 (1–8) |
| Diagnosis (n) | ||
| CD | 43 | 33 |
| CD + DH | 2 | 2 |
| Biopsy | 92% | 81% |
| Education | ||
| High school or less | 14% | 24% |
| Trade/certificate | 41% | 32% |
| University | 45% | 44% |
| Celiac Association Member | 69% | 51% |
| Primary shopper | ||
| Self | 79% | 81% |
| Spouse/partner | 16% | 11% |
| Other | 5% | 9% |
| Dietitian consult | 84% | 76% |
| GFD-KS score (mean, 95% confidence interval) | 11.9 (11.2–12.7) | 11.3 (10.5–12.1) |
GFD-KS= Gluten-Free Diet Knowledge Scale
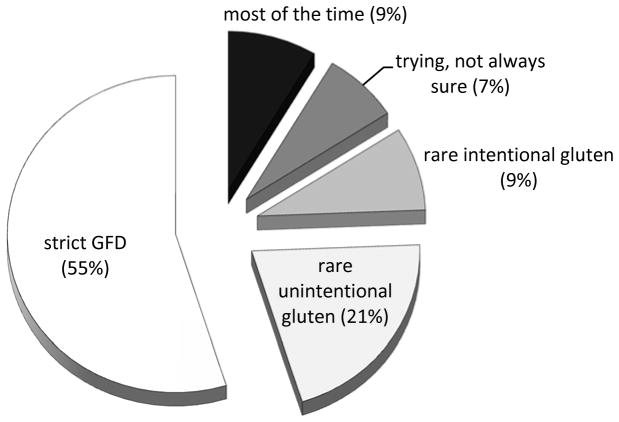
Self-reported Adherence
Based on the 8-item categorical self-assessment of dietary adherence, strict adherence was reported by 55%. Of the remainder, 9% followed a gluten-free diet “most of the time”, 9% reported rare intentional gluten consumption and 21% rare unintentional gluten consumption (Figure 1). None reported unrestricted gluten ingestion, unrestricted gluten (other foods restricted) or gluten-free diet sometimes. About one-third (37%) reported at least one additional dietary restriction, either for medical or other reasons, with dairy being the food most commonly restricted in addition to gluten. Those who reported some level of current gluten consumption were equally likely to have had a duodenal biopsy (OR 0.13, 0.016–1.14), but tended to have been following a gluten restricted diet for a shorter period of time (median 5 years, IQR 1–8 years) than those who reported strict adherence (median 6 years, IQR 3–13 years). Respondents who were members of the Canadian Celiac Association were not significantly more likely to report strict adherence than non-members (OR 2.1; 95% CI 0.85–5.2).
Figure 1.
Self-reported gluten restriction
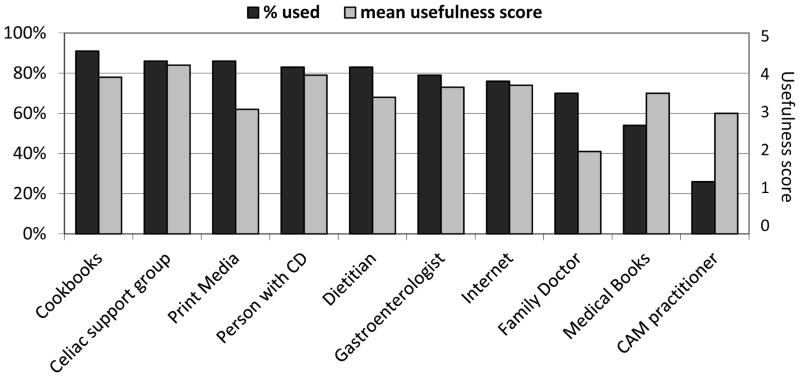
Sources of information about a gluten-free diet
Cookbooks, the internet, print media, patient advocacy groups and other persons with celiac disease were the top five most commonly used sources of information about the GFD. Each was used by greater than 80% of respondents (Figure 2). With the exception of print media, these sources were also identified as the most useful sources of information. Family physicians were the second least frequently used sources of information (70%), and had the lowest rating for usefulness (4.1).
Figure 2.
Information sources used to learn about a GFD in the past 12 months*
*For each information source which was used, participants rated the quality of the information obtained using a scale ranging from 1 (poor) to 5 (excellent).
Gluten-free food identification
None of the foods on the GFD-KS were correctly categorized by 100% of the participants (Table 2). The foods most commonly identified correctly were milk and chickpea flour, which over 95% recognized as gluten-free. Fewer respondents identified correctly products which always contain gluten. Only 73% correctly identified spelt as a gluten-containing grain. Croutons, imitation seafood and rice crisp cereal were the foods most commonly misidentified. Fewer than two-thirds of respondents correctly identified oatmeal as a “food to question”, more typically indicating “not allowed” instead. Sausages and croutons were the only potentially gluten-containing foods which all respondents recognized as not necessarily gluten-free. The gluten-free foods most commonly questioned or restricted inappropriately were modified corn starch (39%), cocoa (33%) and glutinous rice (32%).
Table 2.
Participant responses on the Gluten-free Diet Knowledge Scale, comparing those with self-reported strict adherence to those who acknowledge some gluten exposure
| Food allowed | Food to question | Food NOT allowed | Strict GFD n=45 | Gluten exposure n=37 | |||
|---|---|---|---|---|---|---|---|
|
| |||||||
| % correct | 95% CI | % correct | 95% CI | ||||
| Foods allowed | |||||||
| Milk | 96% | 3% | 1% | 96 | 89–100 | 95 | 87–100 |
| Chickpea flour | 95% | 4% | 1% | 96 | 89–100 | 95 | 87–100 |
| Balsamic vinegar | 73% | 21% | 6% | 73 | 60–87 | 73 | 58–88 |
| Buckwheat | 70% | 17% | 13% | 73 | 60–87 | 65 | 49–81 |
| Glutinous rice | 68% | 14% | 18% | 70 | 56–83 | 66 | 50–82 |
| Cocoa | 67% | 32% | 1% | 74 | 61–87 | 58 | 41–74 |
| Modified corn starch | 60% | 35% | 5% | 60 | 45–75 | 59 | 43–76 |
| Foods to question | |||||||
| Flavored yogurt | 13% | 83% | 4% | 87 | 76–97 | 78 | 64–92 |
| Sausages | 0% | 82% | 18% | 80 | 68–92 | 84 | 71–96 |
| Soy sauce | 2% | 76% | 22% | 80 | 68–92 | 70 | 55–86 |
| Oatmeal | 8% | 61% | 31% | 62 | 47–77 | 59 | 43–76 |
| Rice crisp cereal | 11% | 59% | 30% | 62 | 47–77 | 54 | 37–71 |
| Imitation seafood | 4% | 51% | 44% | 51 | 36–66 | 51 | 34–68 |
| Croutons | 0% | 7% | 93% | 7 | 0–14 | 8 | 0–17 |
| Foods not allowed | |||||||
| Malt vinegar | 5% | 17% | 78% | 80 | 68–92 | 76 | 61–90 |
| Spelt | 16% | 11% | 73% | 76 | 63–89 | 65 | 49–81 |
| Egg noodles | 5% | 24% | 71% | 64 | 50–79 | 78 | 64–92 |
Bolded percentages indicate percent with correct response
No respondent was able to categorize all 17 foods correctly. There were 44% who correctly identified all 3 foods to avoid, 17% who correctly identified all 7 foods allowed, and none who correctly identified all 7 foods to question. Total scores ranged from 4–16 out of 17. Neither the mean score nor the percent correct for any given food or any given category differed significantly between the strictly adherent (11.9, 95% CI 11.2–12.7) and the gluten exposed group (11.3, 95% CI 10.5–12.1). In both groups, fewer than 30% were able to identify correctly the gluten-free status of at least 14 (82%) of the 17 foods (19% gluten exposed vs. 29% strict; p=0.61). Of the incorrect responses, 22% of the decisions would put the respondent at risk of consuming gluten-containing food and 78% would result in the respondent inappropriately restricting a food.
Factors associated with knowledge of gluten-free food
Duration of a GFD was not correlated with the GFD-KS scores (r=0.13; p=0.25). In univariate analysis, there were no statistically significant differences between the scores of males and females nor those who were the primary shopper versus those who relied upon somebody else to shop for them. Neither educational level nor having seen a dietitian was associated with knowledge of gluten-free foods. Respondents who were members of the Canadian Celiac Association (CCA) had a significantly higher total score (12.2, 95% CI 11.8–12.9) than non-members (10.6, 95% CI 9.6–11.6). The only individual items for which CCA members scored significantly higher than non-members were buckwheat [82% (95% CI 71–93%) vs. 50% (95% CI 32–68%)] and spelt [80% (95% CI 69–91%) vs. 56% (95% CI 38–74%)]. Imitation seafood, rice crisp cereal and flavored yogurt were the only items on which non-members of the CCA scored higher than members; however, these differences were not statistically significant. There were no significant differences between those who had friends and family who follow a GFD and those who did not.
Discussion
Individuals with celiac disease with or without dermatitis herpetiformis exhibited significant deficits in their knowledge of the gluten content of different foods. Those who reported “strict adherence” to a GFD were as likely as other respondents to misidentify the gluten content of a variety of foods. Thus, although they may be scrupulous about what they eat, “strict” adherers appear at equal risk of unwittingly consuming gluten. Indeed, a study of patients with putative “non-responsive celiac disease” found that inadvertent gluten ingestion was the cause of ongoing symptoms in the majority of cases[5]. All patients were interviewed by an “experienced dietitian with expertise in celiac disease” who did not identify any sources of trace gluten exposure. Inadvertent gluten ingestion may also be responsible for the failure of complete mucosal recovery after a prolonged period of apparent GFD adherence[3].
Overall, 24% of respondents were able to determine correctly the gluten content of at least 14 of the 17 foods. This contrasts to results of a study of members of the Canadian Celiac Association in which 81.8% of respondents correctly identified at least 6 of 7 items not allowed in a GFD[12] and an Australian randomized controlled trial of an online GFD educational tool in which participants with celiac disease had a mean score of 80.5% in identifying gluten in ingredient lists[14]. This may reflect greater GFD education among the participants in these studies. In an American study which included questions about celiac disease as well as gluten-free diets, the mean score was 55% (70% reported strict adherence to a GFD)[13]. In cross-sectional surveys of members of the Canadian Celiac Association, 85% reported difficulty determining whether foods were gluten-free some or most of the time[21] and nearly 80% expressed concern that gluten does not always appear on food labels[12].
Complex products with multiple ingredients were identified correctly at rates similar to individual ingredients. A notable exception was croutons, a food for which gluten-free versions are increasingly available, which 93% of respondents incorrectly identified as never gluten-free. Recently, uncontaminated oats have been determined to be safe for patients following a gluten-free diet[17]. Nearly two thirds of respondents correctly identified oatmeal as a food to question, and only 8% identified oatmeal as always allowed, suggesting that patients are aware of this change. Owing to the limitations of the study design, it is unknown how many could actually identify gluten-free oats on product labels. In contrast, spelt is an ancient gluten-containing wheat cultivar which has recently become more widely available. One in six respondents identified spelt as always allowed and 11% identified it as a food to question.
In our study, only 55% believed they were following a “strict gluten-free diet”, a surprisingly low proportion for a celiac disease sample. This is lower than is generally reported in studies relying upon self-reported dietary adherence and significantly less than the 90% reported in a Canadian national survey of persons with celiac disease[22]. Given that our sample was quite similar to that in the national Canadian survey, this discrepancy may reflect the question itself rather than a true difference in dietary adherence. In the present study, participants were presented with eight possible descriptors of their diet which included “usually gluten-free diet with rare unintentional gluten consumption” and “usually gluten-free diet with rare intentional gluten consumption”. With these qualifiers, 30% acknowledged rare gluten consumption.
It is likely that many studies have failed to capture “rare” occurrences of gluten ingestion when categorizing participants. The definition of GFD adherence varies greatly among studies[23]. Usually, a range of a few inexact categorical descriptions is used. For instance, in the Canadian study cited above, participants were asked to classify their diet as “strictly gluten-free”, “partially gluten-free” or “not gluten-free”. In a follow-up study with a similar design and recruitment methods, participants were asked about gluten consumption rather than gluten restriction[12]. One in three respondents reported intentional gluten consumption in the previous year. In the present study, a similar proportion reported rare gluten consumption, but only 8% acknowledged rare intentional gluten consumption.
A reliable self-report tool for gluten-free diet adherence has proven elusive. The Celiac Diet Assessment Tool[24] is one of the few validated measures available; however, it is not widely used. It is unclear what this tool is measuring as five of seven items pertain to non-specific symptoms, self-perceptions and beliefs unrelated to gluten ingestion and perceived ability to adhere to a gluten-free diet. Interestingly, knowledge of celiac disease was the one a priori factor identified by focus groups which was not significant in the final model. One wonders whether knowledge of a gluten-free diet, which was incorporated in the dietitian assessment, may have reached statistical significance.
The extent of unintended gluten consumption is nearly impossible to quantify and likely higher than was self-reported. All respondents had difficulty determining the appropriateness of foods in a GFD and many patients may not experience clinical symptoms following gluten ingestion, especially in small quantities[25–27]. Unintentional gluten ingestion was not related to GFD knowledge. The amounts of gluten consumed were not quantified; however, ingestion of as little as 1 milligram of gluten per day may cause persistent mucosal damage[28], so accuracy of food choices for a GFD is relevant.
Changes in product availability and the definition of gluten-free foods may contribute to the observation that GFD duration was not correlated with gluten-free food knowledge. The cross-sectional design of the study precludes more detailed analysis of changes in knowledge over time. Similarly, the small number of male respondents relative to female respondents may explain the failure to replicate previous findings that women had a higher level of knowledge than men[29].
While inclusion of foods containing gluten has obvious adverse consequences, exclusion of gluten-free foods may also have deleterious effects. Persons with celiac disease are inherently at increased risk of nutritional deficiencies[30]. This is compounded by the lower levels of iron, folate, calcium, B vitamins and fiber in gluten-free products relative to their gluten-containing counterparts[31,32]. Avoidance of foods which are gluten-free decreases the variety of foods consumed, which further increases the risk of consuming a diet which is nutritionally inadequate. Unnecessary restriction of modified corn starch by 40% of respondents is especially concerning as this is frequently used in processed foods, including by specialist manufacturers of gluten-free products. Traditionally, GFD education has emphasized foods to be avoided; however, education regarding foods that are gluten-free is equally needed.
In this study, membership in the Canadian Celiac Association (CCA) was associated with greater GFD knowledge. The CCA provides information to individuals with celiac disease through a variety of media including their website, publications such as a pocket gluten-free diet dictionary, and an educational national annual general meeting. Published materials and information on the website is reviewed by a multidisciplinary professional advisory board with expertise in celiac disease. World class experts in celiac disease are invited to the national meeting which is largely attended by patients with celiac disease and their family members. In order to optimize the education of individuals trying to follow a GFD and facilitate a broader educational effort, future study is needed to determine which factors contribute to the increased gluten-free knowledge among advocacy group members.
A potential limitation of this study is that diet adherence was determined by self-report rather than assessment by a trained dietitian or analysis of intestinal biopsy specimens. Therefore, it is not possible to relate gluten-free food knowledge to mucosal recovery or persistent mucosal damage. Nevertheless, the majority of studies involving patients who are “following a gluten-free diet” do not include assessment of histology and many rely solely upon self-reported adherence. Furthermore, although diet review with a specialist dietitian trained in gluten-free diets is considered the most sensitive proxy for assessing mucosal recovery[33], it is an imperfect tool and not widely available. While not as accurate as detailed diet assessment by an expert dietitian, self-report is significantly correlated with this assessment[34]. Of note, a validated measure of gluten-free diet adherence was not used as these are not typically used in clinical practice. Moreover, the scale developed by Biagi et al.[35] has not been validated in a North American population[36] and is difficult to apply in this context where packaged foods guaranteed by a Celiac Association are not widely available. As discussed above, the CDAT[24] is limited by the majority of items being not clearly related to GFD adherence.
Another potential limitation relates to the population studied, which included patients receiving regular follow-up for their celiac disease and/or members of the Canadian Celiac Association. Given that these involvements afford an opportunity to receive ongoing information regarding gluten-free living, this bias may have resulted in a greater GFD knowledge. Also, the study cohort included patients that had been adherent to a GFD for a prolonged period of time which may not be representative of the GFD knowledge among an unselected group of celiac patients.
Overall, the results of this study suggest an important role for a reliable, up to date, and comprehensive education resource to improve GFD adherence. This aspect of long-term management is neither well-studied nor emphasized in practice guidelines for celiac disease management. A guideline developed by the National Institutes of Health (NIH) emphasizes the needs for education about the disease and reinforcement of the importance of treatment adherence, but mentions only briefly the need for education about implementing and maintaining the treatment for the disease, i.e., a gluten-free diet[37]. Guidelines developed by the American Gastroenterological Association describe ongoing GFD education in more detail; however, these recommendations are on the basis of expert opinion and have not been verified in research studies[38,39]. A randomized-controlled study involving an online GFD education intervention showed that education was associated with increased adherence[14], which was assessed using a self-report tool[24]. The recently published American College of Gastroenterology guidelines recommend regular follow-up of individuals with celiac disease to determine GFD adherence, but do not make any specific recommendations regarding on-going education[40].
Conclusions
While it is generally recognized that it can be difficult to determine if food is gluten-free, it is equally challenging for the health care professional to determine whether an individual’s diet is gluten-free. Traditionally, the most common approaches have been patient self-report and assessment by a skilled dietitian with training in gluten-free diets. Both of these methods rely upon the patient’s own knowledge of a GFD. In this study, we demonstrated that patients with celiac disease trying to follow a GFD have imperfect knowledge of the gluten content of common foods which they may encounter. Furthermore, self-reported GFD adherence did not correlate with scores on the Gluten-free Diet Knowledge Scale. This may partially explain the observation that many patients with celiac disease who are on a strict GFD do not experience complete mucosal recovery. As well, nearly one-third of participants reported “rare” exposure to gluten. This was primarily unintentional, which further suggests that inaccurate understanding of foods allowed in a GFD may be contributing to persistent mucosal damage in some patients. It also underscores the importance of asking patients about gluten-consumption as well as gluten-restriction. Membership in a patient advocacy groups was associated with significantly higher scores on the GFD-KS. Further research is needed to determine how this association is mediated as well as educational approaches to improve rates of successful patient adherence to a GFD. In addition, future studies should address the role of deficits in GFD knowledge in predicting incomplete mucosal recovery in patients with celiac disease.
Supplementary Material
Acknowledgments
The authors thank the people with celiac disease who generously gave their time to complete the questionnaire. This study would not have been possible without their support.
Financial support: This study was supported by the Canadian Celiac Association JA Campbell Award. JS received post-doctoral fellowships from the Canadian Institutes of Health Research and the Manitoba Health Research Council. These sponsors did not have any role in study design; the collection, analysis and interpretation of data; the writing of the report; or in the decision to submit the article for publication.
Footnotes
Specific author contributions: All authors contributed to the conception and design of the study; generation, collection, assembly, analysis and/or interpretation of data; and drafting or revision of the manuscript. All authors reviewed and approved the final submitted manuscript.
Potential competing interests: None.
References
- 1.See J, Murray JA. Gluten-free diet: the medical and nutrition management of celiac disease. Nutr Clin Pract. 2006;21:1–15. doi: 10.1177/011542650602100101. [DOI] [PubMed] [Google Scholar]
- 2.Kárpáti S. Dermatitis herpetiformis. Clin Dermatol. 2012;30:56–9. doi: 10.1016/j.clindermatol.2011.03.010. [DOI] [PubMed] [Google Scholar]
- 3.Rubio-Tapia A, Rahim MW, See JA, Lahr BD, Wu T-T, Murray JA. Mucosal recovery and mortality in adults with celiac disease after treatment with a gluten-free diet. Am J Gastroenterol. 2010;105:1412–20. doi: 10.1038/ajg.2010.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lebwohl B, Granath F, Ekbom A, Smedby KE, Murray JA, Neugut AI, et al. Mucosal healing and risk for lymphoproliferative malignancy in celiac disease: a population-based cohort study. Ann Intern Med. 2013;159:169–75. doi: 10.7326/0003-4819-159-3-201308060-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abdulkarim AS, Burgart LJ, See J, Murray JA. Etiology of nonresponsive celiac disease: results of a systematic approach. Am J Gastroenterol. 2002;97:2016–21. doi: 10.1111/j.1572-0241.2002.05917.x. [DOI] [PubMed] [Google Scholar]
- 6.Thompson T, Lee AR, Grace T. Gluten contamination of grains, seeds, and flours in the United States: a pilot study. J Am Diet Assoc. 2010;110:937–40. doi: 10.1016/j.jada.2010.03.014. [DOI] [PubMed] [Google Scholar]
- 7.Hollon JR, Cureton PA, Martin ML, Leonard Puppa EL, Fasano A. Trace gluten contamination may play a role in mucosal and clinical recovery in a subgroup of diet-adherent non-responsive celiac disease patients. BMC Gastroenterol. 2013;13:40. doi: 10.1186/1471-230X-13-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lanzini A, Lanzarotto F, Villanacci V, Mora A, Bertolazzi S, Turini D, et al. Complete recovery of intestinal mucosa occurs very rarely in adult coeliac patients despite adherence to gluten-free diet. Aliment Pharmacol Ther. 2009;29:1299–308. doi: 10.1111/j.1365-2036.2009.03992.x. [DOI] [PubMed] [Google Scholar]
- 9.Tuire I, Marja-Leena L, Teea S, Katri H, Jukka P, Päivi S, et al. Persistent duodenal intraepithelial lymphocytosis despite a long-term strict gluten-free diet in celiac disease. Am J Gastroenterol. 2012;107:1563–9. doi: 10.1038/ajg.2012.220. [DOI] [PubMed] [Google Scholar]
- 10.Case S. Gluten-Free Diet: a comprehensive resource guide. 8. Regina, SK: Case Nutrition Consulting Inc; 2008. [Google Scholar]
- 11.General Mills. General Mills 2015 Annual Report: Making food people love. Minneapolis, MN: 2015. [Google Scholar]
- 12.Zarkadas M, Dubois S, Macisaac K, Cantin I, Rashid M, Roberts KC, et al. Living with coeliac disease and a gluten-free diet: a Canadian perspective. J Hum Nutr Diet. 2013;26:10–23. doi: 10.1111/j.1365-277X.2012.01288.x. [DOI] [PubMed] [Google Scholar]
- 13.Leffler DA, Edwards-George J, Dennis M, Schuppan D, Cook F, Franko DL, et al. Factors that influence adherence to a gluten-free diet in adults with celiac disease. Dig Dis Sci. 2008;53:1573–81. doi: 10.1007/s10620-007-0055-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sainsbury K, Mullan B, Sharpe L. A Randomized Controlled Trial of an Online Intervention to Improve Gluten-Free Diet Adherence in Celiac Disease. Am J Gastroenterol. 2013:1–7. doi: 10.1038/ajg.2013.47. [DOI] [PubMed] [Google Scholar]
- 15.Sverker A, Hensing G, Hallert C. “Controlled by food”-lived experiences of coeliac disease. J Hum Nutr Diet. 2005;18:171–80. doi: 10.1111/j.1365-277X.2005.00591.x. [DOI] [PubMed] [Google Scholar]
- 16.Sverker A, Ostlund G, Hallert C, Hensing G. Sharing life with a gluten-intolerant person--the perspective of close relatives. J Hum Nutr Diet. 2007;20:412–22. doi: 10.1111/j.1365-277X.2007.00815.x. [DOI] [PubMed] [Google Scholar]
- 17.Rashid M, Butzner D, Burrows V, Zarkadas M, Case S, Molloy M, et al. Consumption of pure oats by individuals with celiac disease: a position statement by the Canadian Celiac Association. Can J Gastroenterol. 2007;21:649–51. doi: 10.1155/2007/340591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pulido OM, Gillespie Z, Zarkadas M, Dubois S, Vavasour E, Rashid M, et al. Introduction of oats in the diet of individuals with celiac disease: a systematic review. Adv Food Nutr Res. 2009;57:235–85. doi: 10.1016/S1043-4526(09)57006-4. [DOI] [PubMed] [Google Scholar]
- 19.Gardner MJ, Altman DG. Confidence intervals rather than P values: estimation rather than hypothesis testing. Br Med J (Clin Res Ed) 1986;292:746–50. doi: 10.1136/bmj.292.6522.746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cummings P, Koepsell TD. P values vs estimates of association with confidence intervals. Arch Pediatr Adolesc Med. 2010;164:193–6. doi: 10.1001/archpediatrics.2009.266. [DOI] [PubMed] [Google Scholar]
- 21.Zarkadas M, Cranney A, Case S, Molloy M, Switzer C, Graham ID, et al. The impact of a gluten-free diet on adults with coeliac disease: results of a national survey. J Hum Nutr Diet. 2006;19:41–9. doi: 10.1111/j.1365-277X.2006.00659.x. [DOI] [PubMed] [Google Scholar]
- 22.Cranney A, Zarkadas M, Graham ID, Butzner JD, Rashid M, Warren R, et al. The Canadian Celiac Health Survey. Dig Dis Sci. 2007;52:1087–95. doi: 10.1007/s10620-006-9258-2. [DOI] [PubMed] [Google Scholar]
- 23.Hall NJ, Rubin G, Charnock A. Systematic review: adherence to a gluten-free diet in adult patients with coeliac disease. Aliment Pharmacol Ther. 2009;30:315–30. doi: 10.1111/j.1365-2036.2009.04053.x. [DOI] [PubMed] [Google Scholar]
- 24.Leffler DA, Dennis M, Edwards George JB, Jamma S, Magge S, Cook EF, et al. A simple validated gluten-free diet adherence survey for adults with celiac disease. Clin Gastroenterol Hepatol. 2009;7:530–6. 536.e1–2. doi: 10.1016/j.cgh.2008.12.032. [DOI] [PubMed] [Google Scholar]
- 25.Kaukinen K, Peräaho M, Lindfors K, Partanen J, Woolley N, Pikkarainen P, et al. Persistent small bowel mucosal villous atrophy without symptoms in coeliac disease. Aliment Pharmacol Ther. 2007;25:1237–45. doi: 10.1111/j.1365-2036.2007.03311.x. [DOI] [PubMed] [Google Scholar]
- 26.Collin P, Mäki M, Kaukinen K. Safe gluten threshold for patients with celiac disease: some patients are more tolerant than others. Am J Clin Nutr. 2007;86:260. doi: 10.1093/ajcn/86.1.260. author reply 260–1. [DOI] [PubMed] [Google Scholar]
- 27.Catassi C, Fabiani E, Iacono G, D’Agate C, Francavilla R, Biagi F, et al. A prospective, double-blind, placebo-controlled trial to establish a safe gluten threshold for patients with celiac disease. Am J Clin Nutr. 2007;85:160–6. doi: 10.1093/ajcn/85.1.160. [DOI] [PubMed] [Google Scholar]
- 28.Biagi F, Campanella J, Martucci S, Pezzimenti D, Ciclitira PJ, Ellis HJ, et al. A milligram of gluten a day keeps the mucosal recovery away: a case report. Nutr Rev. 2004;62:360–3. doi: 10.1301/nr.2004.sept.360. [DOI] [PubMed] [Google Scholar]
- 29.Rashid M, Cranney A, Zarkadas M, Graham ID, Switzer C, Case S, et al. Celiac disease: evaluation of the diagnosis and dietary compliance in Canadian children. Pediatrics. 2005;116:e754–9. doi: 10.1542/peds.2005-0904. [DOI] [PubMed] [Google Scholar]
- 30.Shepherd SJ, Gibson PR. Nutritional inadequacies of the gluten-free diet in both recently-diagnosed and long-term patients with coeliac disease. J Hum Nutr Diet. 2012 doi: 10.1111/jhn.12018. [DOI] [PubMed] [Google Scholar]
- 31.Thompson T. Thiamin, riboflavin, and niacin contents of the gluten-free diet: is there cause for concern? J Am Diet Assoc. 1999;99:858–62. doi: 10.1016/S0002-8223(99)00205-9. [DOI] [PubMed] [Google Scholar]
- 32.Thompson T. Folate, iron, and dietary fiber contents of the gluten-free diet. J Am Diet Assoc. 2000;100:1389–96. doi: 10.1016/S0002-8223(00)00386-2. [DOI] [PubMed] [Google Scholar]
- 33.Ciacci C, Cirillo M, Cavallaro R, Mazzacca G. Long-Term Follow-Up of Celiac Adults on Gluten-Free Diet: Prevalence and Correlates of Intestinal Damage. Digestion. 2002;66:178–85. doi: 10.1159/000066757. [DOI] [PubMed] [Google Scholar]
- 34.Leffler DA, Edwards George JB, Dennis M, Cook EF, Schuppan D, Kelly CP. A prospective comparative study of five measures of gluten-free diet adherence in adults with coeliac disease. Aliment Pharmacol Ther. 2007;26:1227–35. doi: 10.1111/j.1365-2036.2007.03501.x. [DOI] [PubMed] [Google Scholar]
- 35.Biagi F, Andrealli A, Bianchi PI, Marchese A, Klersy C, Corazza GR. A gluten-free diet score to evaluate dietary compliance in patients with coeliac disease. Br J Nutr. 2009;102:882–7. doi: 10.1017/S0007114509301579. [DOI] [PubMed] [Google Scholar]
- 36.Biagi F, Bianchi PI, Marchese A, Trotta L, Vattiato C, Balduzzi D, et al. A score that verifies adherence to a gluten-free diet: a cross-sectional, multicentre validation in real clinical life. Br J Nutr. 2012;108:1884–8. doi: 10.1017/S0007114511007367. [DOI] [PubMed] [Google Scholar]
- 37.Suchy FJ, Brannon PM, Carpenter TO, Fernandez JR, Gilsanz V, Gould JB, et al. National Institutes of Health Consensus Development Conference Statement on Celiac Disease, June 28–30, 2004. Gastroenterology. 2005;128:S1–9. doi: 10.1059/0003-4819-152-12-201006150-00248. [DOI] [PubMed] [Google Scholar]
- 38.Kagnoff MF. AGA Institute Medical Position Statement on the Diagnosis and Management of Celiac Disease. Gastroenterology. 2006;131:1977–80. doi: 10.1053/j.gastro.2006.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rostom A, Murray JA, Kagnoff MF. American Gastroenterological Association (AGA) Institute technical review on the diagnosis and management of celiac disease. Gastroenterology. 2006;131:1981–2002. doi: 10.1053/j.gastro.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 40.Rubio-Tapia A, Hill ID, Kelly CP, Calderwood AH, Murray JA. ACG clinical guidelines: diagnosis and management of celiac disease. Am J Gastroenterol. 2013;108:656–76. doi: 10.1038/ajg.2013.79. quiz 677. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.