Abstract
Objectives
The fractional flow reserve (FFR) is an index of the severity of coronary stenosis that has been clinically validated in several studies. The instantaneous wave-free ratio (iFR) and the resting distal coronary artery pressure/aortic pressure (Pd/Pa) are nonhyperemic pressure-derived indices of the severity of stenosis. This study sought to examine the diagnostic accuracy of the iFR and resting Pd/Pa with respect to hyperemic FFR.
Methods
Following an intracoronary injection of papaverine, the iFR, resting Pd/Pa, and FFR were continuously measured in 123 lesions in 103 patients with stable coronary disease.
Results
The iFR and resting Pd/Pa values were strongly correlated with the FFR (R=0.794, p<0.001, R=0.832, p<0.0001, respectively). A receiver operator curve (ROC) analysis revealed that the optimal iFR cut-off value for predicting an FFR of <0.80 was 0.89 (AUC 0.901, sensitivity 84.1%, specificity 80.0%, positive predictive value 69.8%, negative predictive value 90.0%, diagnostic accuracy 81.3%), while the optimal resting Pd/Pa cut-off value was 0.92 (AUC 0.925, sensitivity 90.9%, specificity 78.5%, positive predictive value 70.2%, negative predictive value 93.9%, diagnostic accuracy 82.9%). The lesions with an iFR value of ≤0.89 and a Pd/Pa value of ≤0.92 were defined as double-positive lesions, while the lesions with an iFR value of >0.89 and a Pd/Pa value of >0.92 were defined as double-negative lesions. In these 109 lesions, the sensitivity, specificity, positive predictive value, negative predictive value, and diagnostic accuracy were 92.3%, 82.9%, 75.0%, 95.1%, and 86.2%, respectively.
Conclusion
This analysis demonstrated that the iFR and resting Pd/Pa were strongly correlated with the FFR and that the diagnostic accuracy of the iFR was similar to that of the resting Pd/Pa. The diagnostic accuracy can be improved with the use of both the iFR and the resting Pd/Pa.
Keywords: FFR, iFR, resting Pd/Pa
Introduction
The fundamental limitations of coronary angiography and its poor correlation with the severity of functional stenosis, in terms of blood flow, are well recognized (1). The fractional flow reserve (FFR) is an accurate invasive index that can be used in a catheterization laboratory to determine whether angiographically-equivocal stenosis is of functional significance (2). Recent randomized trials assessing the value of FFR-guided PCI have demonstrated reduced rates of major adverse cardiac events, mainly due to a decreased need for repeat revascularization (3, 4). These results have led to changes in practice guidelines. The use of the FFR is recommended for the assessment of lesions of intermediate severity (5, 6). With regard to the measurement of the FFR, some drugs are currently used for producing maximal coronary hyperemia in humans. The bolus intracoronary administration of papaverine or the intravenous infusion of adenosine or adenosine triphosphate (ATP) is capable of producing maximal coronary hyperemia (7-9).
However, it takes much more time and cost to induce pharmacological hyperemia and some patients experience chest discomfort during hyperemia. Two nonhyperemic measures of inducing pressure might be useful for assessing the severity of coronary stenosis. The resting distal coronary artery pressure/aortic pressure (Pd/Pa) is the ratio of distal coronary artery pressure to aortic pressure over the entire cardiac cycle. Conversely, the instantaneous wave-free ratio (iFR) measures coronary pressure during a specific period of diastole when the resting resistance is the lowest (10). The assessment of the severity of coronary stenosis without the induction of hyperemia is attractive because it reducing the procedural time and cost, and avoids the patient-related discomfort associated with pharmacological hyperemia. This study sought to examine the diagnostic accuracy of the iFR and resting Pd/Pa with in comparison to hyperemic FFR.
Material and Methods
Patients
One hundred three patients with mild or moderate coronary stenosis who were undergoing coronary angiography were selected for this study. The patients' characteristics are shown in Table 1. Written informed consent was obtained from all of the patients prior to coronary angiography and this study protocol was approved by the ethical committee of Tsuchiya General Hospital.
Table 1.
Patients Characteristics.
| n=103 | ||
| age (years) | 70.4±8.7 | |
| Male (%) | 77 (74.8%) | |
| Cardiac Status | ||
| Stable Angina | 92 | |
| Previous MI | 11 | |
| Risk Factors | ||
| Hypertension | 82 | |
| Dyslipidemia | 61 | |
| Diabetes | 40 | |
| Smoking | 28 | |
| Hemodialysis | 12 |
MI: myocardial infarction
Study design
Diagnostic coronary angiography was performed through a standard percutaneous radial or femoral arterial approach. After obtaining vascular access, 3,000 units of heparin were administered intravenously. A 6F guide catheter was introduced into the left or right coronary arteries. The FFR was measured with a coronary pressure guide wire (Verrata guide wire; Volcano Corporation, San Diego, CA) as follows: 1) resting Pd/Pa; 2) iFR; 3) FFR after the intracoronary injection of papaverine (12 mg in the left coronary artery or 8 mg in the right coronary artery). The FFR, electrocardiography results and arterial blood pressure were monitored until the FFR value returned to the baseline value.
Quantitative coronary angiography analysis (QCA)
The results from the single most severe view were recorded. The lesion length, minimum lumen diameter (MLD), reference vessel diameter (RVD) and percent diameter stenosis (%DS) were analyzed using a computerized, automated, edge detection algorithm (Philips Medical System, Best, The Netherlands), as previously described (11).
Statistical analysis
Continuous variables were expressed as the mean±SD and compared using the paired t-test. The performance of the iFR and the resting Pd/Pa in predicting a positive FFR (<0.80) was assessed in terms of the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and diagnostic accuracy, together with their 95% confidence interval (CI). A receiver operating characteristic (ROC) curve was created to measure the accuracy of the test (area under the ROC curve: AUC) and identify iFR and the optimal resting Pd/Pa cut-off value that corresponded to an FFR of <0.80.
Results
The characteristics of the patients and lesions
The patients' characteristics are summarized in Table 1. Eleven patients had a past history of myocardial infarction. Twelve patients had end-stage renal dysfunction with hemodialysis.
The characteristics of the lesion are summarized in Table 2. The locations of the lesions were as follows: left anterior descending coronary artery (LAD) (n=90), left circumflex coronary artery (LCx) (n=4), and right coronary artery (RCA) (n=29). The mean % stenosis was 49.1±16.1%.
Table 2.
Lesions’ Characteritics.
| Lesion Location | n=123 | ||
| LAD | 90 | ||
| LCx | 4 | ||
| RCA | 29 | ||
| QCA data | |||
| Lesion Length (mm) | 9.6±5.4 | ||
| RVD (mm) | 2.67±0.65 | ||
| MLD (mm) | 1.36±0.50 | ||
| % stenosis | 49.1±16.1 | ||
LAD: left anterior descending artery
LCx: left circumflex artery, RCA: right coronary artery
RVD: reference vessel diameter
MLD: minimum lesion diameter
The correlations between the iFR and FFR values and between the resting Pd/Pa and FFR values
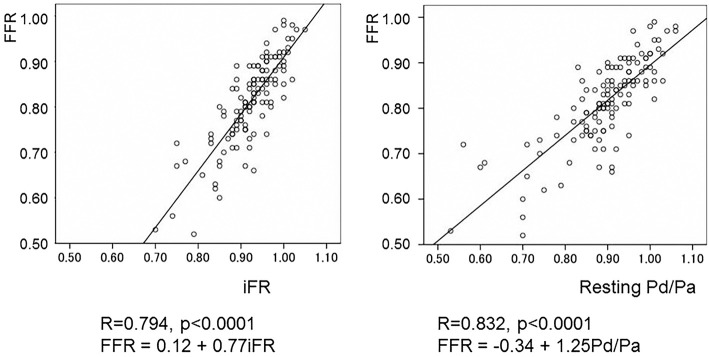
Both the iFR and resting Pd/Pa were strongly correlated with the FFR. The correlation between the iFR and the FFR was R=0.794 (p<0.0001, FFR=0.12+0.77iFR). The correlation between the resting Pd/Pa and the FFR was R=0.832 (p<0.0001, FFR=-0.34+1.25Pd/Pa) (Fig. 1). The receiver operator curve (ROC) analysis revealed that the optimal iFR cut-off value for predicting an FFR value of <0.80 was 0.89 (AUC 0.901, sensitivity 84.1%, specificity 80.0%, positive predictive value 69.8%, negative predictive value 90.0%, diagnostic accuracy 81.3%), while the optimal resting Pd/Pa cut-off value was 0.92 (AUC 0.925, sensitivity 90.9%, specificity 78.5%, positive predictive value 70.2%, negative predictive value 93.9%, diagnostic accuracy 82.9%) (Fig. 2). The lesions with an iFR value of ≤0.89 and a Pd/Pa value of ≤0.92 were defined as double-positive, while those with an iFR value of >0.89 and a Pd/Pa value of >0.92 were defined as double-negative lesions. These lesions were summarized in Table 3. In these 109 lesions, the sensitivity, specificity, positive predictive value, negative predictive value and diagnostic accuracy were 92.3%, 82.9%, 75.0%, 95.1%, 86.2%, respectively.
Figure 1.
The correlations between the iFR, Pd/Pa and FFR.
Figure 2.
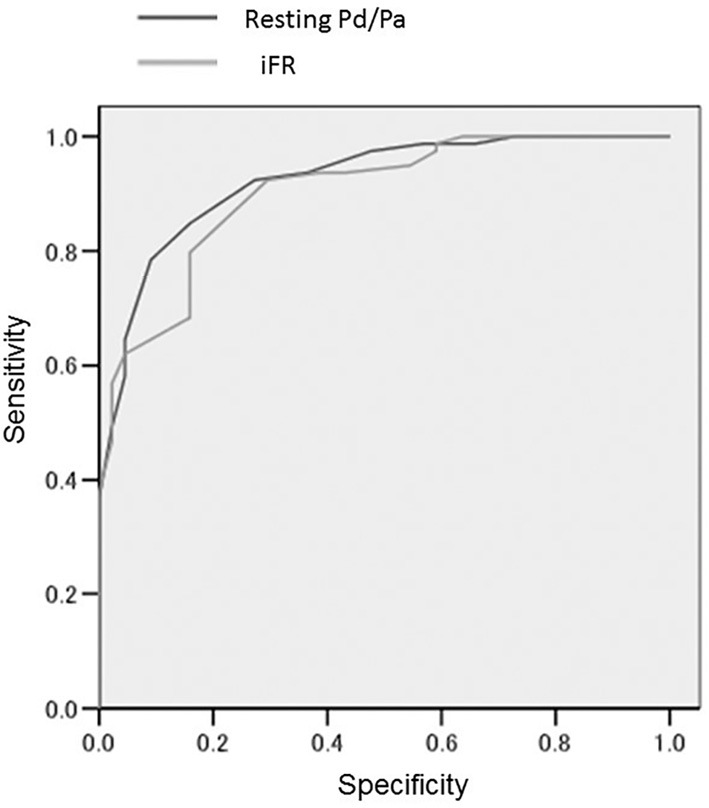
The results of the receiver operator curve (ROC) analysis. The optimal iFR and Pd/Pa cut-off values for predicting an FFR of <0.80 were 0.89 (AUC 0.901) and 0.92 (AUC 0.925), respectively.
Table 3.
Double Positive and Double Negative Lesions.
| FFR<0.80 | FFR≥0.80 | ||
| iFR≤0.89 and Pd/Pa≤0.92 | 36 | 12 | |
| iFR>0.89 and Pd/Pa>0.92 | 3 | 56 |
Deviated lesions
The lesions in which the actual measured iFR and resting Pd/Pa values differed from the predicted iFR and resting Pd/Pa values by >10% (as calculated using the formula: FFR=0.12+0.77 iFR, FFR=-0.34+1.25 Pd/Pa) were defined as deviated lesions. The lesions in which the difference between the actual measured iFR and the resting Pd/Pa values and the predicted values were <10% were defined as non-deviated lesions. The lesions in which the actual measured iFR and the resting Pd/Pa was >10% higher (iFR, n=11; resting Pd/Pa, n=11) or >10% lower (iFR, n=6; resting Pd/Pa, n=4) than the predicted iFR and resting Pd/Pa values were defined as underestimated lesions and overestimated lesions, respectively. We compared the QCA data of the deviated lesions with those of the non-deviated lesions. In the lesions underestimated by iFR, the lesion length was significantly longer and both the RVD and MLD were significantly smaller in comparison to the non-deviated lesions (Table 4). In the lesions that were underestimated by the resting Pd/Pa, the lesion length was significantly longer, both the RVD and MLD were significantly smaller and the % stenosis was more severe in comparison to the non-deviated lesions (Table 5). Thus, in small vessels with long, severe stenosis, both the iFR and the resting Pd/Pa tended to be larger than the values predicted from the FFR.
Table 4.
Deviated Lesions in iFR.
| Underestimated Lesions | Overestimated Lesions | Non-Deviated Lesions | |
|---|---|---|---|
| n | 11 | 6 | 106 |
| Lesion Length (mm) | 12.9±9.0* | 8.3±5.9 | 9.3±4.8 |
| RVD (mm) | 2.32±0.59* | 2.37±0.42 | 2.73±0.65 |
| MLD (mm) | 0.96±0.45** | 1.31±0.44 | 1.40±0.65 |
| %stenosis | 58.1±19.7 | 44.1±17.6 | 48.5±15.5 |
RVD: reference vessel diameter, MLD: minimum lesion diameter
*p<0.05, **p<0.01 vs. Corrected Estimated Lesions
Table 5.
Deviated Lesions in Resting Pd/Pa.
| Underestimated Lesions | Overestimated Lesions | Non-Deviated Lesions | |
|---|---|---|---|
| n | 11 | 4 | 108 |
| Lesion Length (mm) | 12.6±8.5* | 11.1±5.3 | 9.3±4.9 |
| RVD (mm) | 2.40±0.53 | 2.48±0.45 | 2.71±0.66 |
| MLD (mm) | 0.94±0.35** | 1.20±0.17 | 1.40±0.50 |
| %stenosis | 61.0±13.5* | 50.7±9.6 | 47.8±16.1 |
RVD: reference vessel diameter, MLD: minimum lesion diameter
*p<0.05, **p<0.01 vs. Corrected Estimated Lesions
Hemodynamics
The patients' systolic and diastolic blood pressure values significantly decreased after the injection of papaverine, while their heart rates significantly increased (Table 6).
Table 6.
Hemodynamic Change.
| iFR | Pd/Pa | papaverine | |
| sys BP (mmHg) | 130±21 | 131±22 | 120±19* |
| dia BP (mmHg) | 67±10 | 67±10 | 61±9* |
| HR (beats/min) | 70±11 | 71±11 | 75±12* |
sys BP: systolic blood pressure, dia BP: diastolic blood pressure
HR: heart rate, *p<0.01 vs. iFR and Pd/Pa
Discussion
Two nonhyperemic measures of pressure might be useful for assessing the severity of coronary stenosis. Pd/Pa is the ratio of distal coronary artery pressure to aortic pressure over the entire cardiac cycle. Conversely, the iFR measures coronary pressure during a specific period of diastole when resting resistance is the lowest. In this study the overall linear correlation between both iFR and resting Pd/Pa and FFR was moderate, and both of the nonhyperemic indices showed moderate overall diagnostic accuracy. However, in prior reports, the diagnostic accuracy of the iFR (in comparison to the FFR) ranged widely, from 60% to 91% (10, 12-14), and its relative accuracy in comparison to the resting Pd/Pa has been debated.
In the present study, in small vessels with severe, long stenosis both the iFR and the resting Pd/Pa values tended to be higher than the predicted value that was calculated from the actual measured FFR value. In other words, the degree of functional stenosis tended to be underestimated in small vessels with severe, long stenosis. It would be better to carefully evaluate small vessels with long and severe stenosis using both iFR and resting Pd/Pa.
The diagnostic accuracy of iFR alone or resting Pd/Pa alone was moderate. However, if the lesions with an iFR ≤0.89 and a resting Pd/Pa of ≤0.92 were defined as double-positive and those with an iFR of >0.89 and a resting Pd/Pa of >0.92 were defined as double-negative, the diagnostic accuracy improved. Although the iFR and the resting Pd/Pa are imperfect surrogates of the FFR when they are close to the clinically used cutoff value of 0.80, the diagnostic accuracy can be improved by using both indices together. Only 14 lesions (11.4%) were neither double-positive nor double-negative. Thus, in clinical practice, the lesions can be deferred if they are found to be double-negative by both iFR and resting Pd/Pa.
Only the lesions that were neither double-positive nor double-negative should be evaluated by FFR with drug-induced hyperemia.
Several investigators have reported the relationship between conventional FFR and the non-hyperemic indices of the severity of stenosis (13-15). In the RESOLVE study, the overall linear correlation between both the iFR and the Pd/Pa and the FFR was strong (R value 0.81 and 0.83, respectively), and the optimal cut points for predicting an FFR of <0.80 were 0.90 and 0.92 respectively. The diagnostic accuracy was 80.4% and 81.5% respectively. These results were similar to those of our own study. Based on the level of accuracy, it seems to be insufficient to separately use either of the parameters for procedural guidance in all cases because approximately 20% of the therapeutic decisions would be discordant from the FFR. However, we are of the opinion that the combined use both the iFR and the resting Pd/Pa may have the potential to improve the diagnostic accuracy in clinical practice.
The present study is associated with several limitations. Although the data were collected prospectively with the application of a strict study methodology in patients with intermediate stenosis in the clinical setting, the present study was performed in a single center study and involved a relatively small number of patients. The analyses of the angiograms, ECGs, and pressure waveforms were performed at an in-hospital lab in a blinded fashion, but not by a core laboratory. The RESOLVE study is the first coronary physiology study to have used a core laboratory for the analysis of the diagnostic accuracy of hyperemic and resting pressure-derived indices of the severity of stenosis. In the RESOLVE study, 19.3% of measurements were found to be suboptimal and were excluded from the analysis (15). Future clinical studies should consider including a core laboratory analysis.
Conclusion
Both the iFR and resting Pd/Pa were strongly correlated with the FFR and the diagnostic accuracy of the iFR (81.3%) was similar to that of the resting Pd/Pa (82.9%). In small vessels with severe, long stenosis the degree of functional stenosis tended to be underestimated by both indices. The diagnostic accuracy could be improved by the combined use of both the iFR and the resting Pd/Pa.
The authors state that they have no Conflict of Interest (COI).
References
- 1. White CW, Wright CB, Doty DB, et al. Does visual interpretation of the coronary arteriogram predict the physiologic importance of a coronary stenosis? N Engl J Med 310: 819-824, 1984. [DOI] [PubMed] [Google Scholar]
- 2. Pijls NH, De Bruyne B, Peels K, et al. Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. N Engl J Med 334: 1703-1708, 1996. [DOI] [PubMed] [Google Scholar]
- 3. Tonino PA, De Bruyne B, Pijls NH, et al. ; FAME Study Investigators ; FAME Study Investigators Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med 360: 213-224, 2009. [DOI] [PubMed] [Google Scholar]
- 4. De Bruyne B, Pijls NH, Kalesan B, et al. ; FAME 2 Trial Investigators Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med 367: 991-1001, 2012. [DOI] [PubMed] [Google Scholar]
- 5. Task Force Members , Montalescot G, Sechtem U, Achenbach S, et al. 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J 34: 2949-3003, 2013. [DOI] [PubMed] [Google Scholar]
- 6. Patel MR, Dehmer GJ, Hirshfeld JW, et al. ACCF/SCAI/STS/AATS/AHA/ASNC/HFSA/SCCT 2012 appropriate use criteria for coronary revascularization focused update: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, Society for Cardiovascular Angiography and Interventions, Society of Thoracic Surgeons, American Association for Thoracic Surgery, American Heart Association, American Society of Nuclear Cardiology, and the Society of Cardiovascular Computed Tomography. J Am Coll Cardiol 59: 857-881, 2012. [DOI] [PubMed] [Google Scholar]
- 7. Wilson RF, White CW. Serious ventricular dysrhythmias after intracoronary papaverine. Am J Cardiol 62: 1301-1302, 1988. [DOI] [PubMed] [Google Scholar]
- 8. Wilson RF, Wyche K, Christensen BV, Zimmer S, Laxson DD. Effects of adenosine on human coronary arterial circulation. Circulation 82: 1595-1606, 1990. [DOI] [PubMed] [Google Scholar]
- 9. Shiode N, Kato M, Nakayama K, et al. Effect of adenosine triphosphate on human coronary circulation. Intern Med 37: 818-825, 1998. [DOI] [PubMed] [Google Scholar]
- 10. Berry C, van't Veer M, Witt N, et al. VERIFY (VERification of Instantaneous Wave-Free Ratio and Fractional Flow Reserve for the Assessment of Coronary Artery Stenosis Severity in EverydaY Practice): a multicenter study in consecutive patients. J Am Coll Cardiol 61: 1421-1427, 2013. [DOI] [PubMed] [Google Scholar]
- 11. van der Zwet PM, Pinto IM, Serruys PW, Reiber JH. A new approach for the automated definition of path lines in digitized coronary angiograms. Int J Card Imaging 5: 75-83, 1990. [DOI] [PubMed] [Google Scholar]
- 12. Sen S, Escaned J, Malik IS, et al. Development and validation of a new adenosine-independent index of stenosis severity from coronary wave intensity analysis: results of the ADVISE (ADenosine Vasodilator Independent Stenosis Evaluation) study. J Am Coll Cardiol 59: 1392-1402, 2012. [DOI] [PubMed] [Google Scholar]
- 13. Johnson NP, Kirkeeide RL, Asrress KN, et al. Does the instantaneous wave-free ratio approximate the fractional flow reserve? J Am Coll Cardiol 61: 1428-1435, 2013. [DOI] [PubMed] [Google Scholar]
- 14. Petraco R, Escaned J, Sen S, et al. Classification performance of instantaneous wave-free ratio (iFR) and fractional flow reserve in a clinical population of intermediate coronary stenoses: results of the ADVISE registry. EuroIntervention 9: 91-101, 2013. [DOI] [PubMed] [Google Scholar]
- 15. Jeremias A, Maehara A, Généreux P, et al. Multicenter core laboratory comparison of the instantaneous wave-free ratio and resting Pd/Pa with fractional flow reserve: the RESOLVE study. J Am Coll Cardiol 63: 1253-1261, 2014. [DOI] [PubMed] [Google Scholar]