Abstract
Objective
Emerging studies have focused on the association between non-alcoholic fatty liver disease (NAFLD) and the risk of type 2 diabetes mellitus (T2DM). We aimed to investigate whether NAFLD diagnosed by ultrasonography could predict the risk of future T2DM in a Japanese middle-aged health check population.
Methods
We conducted a 10-year observational study in a health checkup population of middle-aged Japanese men and women at Hidaka Hospital from 2004 to 2013. We excluded cases with an alcohol intake exceeding 20 g/day and those with impaired glucose tolerance. The remaining 1,544 men and 864 women were classified into fatty liver and non-fatty liver groups based on the findings of abdominal ultrasonography. Both groups were followed for the development of diabetes. A multiple regression analysis was performed for each variable to predict the risk of future diabetes.
Results
The median age of the participants was 46.0 years at the entry, and the follow-up period was 10 years. The incidence of diabetes in the fatty liver group was 12.5% (29/232) in men and 26.3% (10/38) in women, whereas the incidence of diabetes in the non-fatty liver group was 2.5% (34/1,312) in men and 1.8% (15/826) in women. The relative risk of diabetes associated with fatty liver was 4.8 [95% confidence interval (CI) 3.0 -7.8, p<0.0001] in men and 14.5 (95% CI 7.0-30.1, p<0.0001) in women.
Conclusion
NAFLD was a significant predictor for future diabetes in a Japanese middle-aged health check population, especially in women.
Keywords: Type 2 diabetes mellitus, non-alcoholic fatty liver disease (NAFLD), health check for 10-year follow up, ultrasonography
Introduction
With the increasing prevalence of obesity, diabetes, and metabolic syndrome in the United States (US), non-alcoholic fatty liver disease (NAFLD) has become the most common disease of chronic liver damage in the US (1-3). The prevalence of NAFLD is also increasing in Japan due to the Westernization of lifestyles, such as high-fat and high-calorie diets with less physical activity (4, 5). A high prevalence of fatty liver has been reported to be associated with type 2 diabetes mellitus (T2DM) (6-8).
NAFLD is characterized by significant lipid deposition in the hepatocytes in patients without a history of excessive alcohol intake and is often associated with obesity (9) and hypertension (10). Although these abnormalities are often categorized as insulin resistance syndrome or metabolic syndrome (11), they carry a risk of cardiovascular disease. In addition, diabetes, insulin resistance, and increased plasma fatty acids are considered to increase the risk of NAFLD (12, 13), and each of these metabolic factors is also characteristic of T2DM. It has been reported that NAFLD influences the severity of hepatic insulin resistance in T2DM (14). Furthermore, NAFLD has been correlated with hepatic insulin resistance independently of obesity and intra-abdominal adiposity among non-obese men without T2DM (15).
The increased prevalence of NAFLD in relation to the development of diabetes has been reported in a cross-sectional study (16), and a close relationship between liver enzymes and diabetes has been reported in cohort studies (17-22). However, the former does not prove a causal relationship, and the latter does not directly concern NAFLD. Shibata et al. first reported an observational cohort study in male workers over 40 years old from 1997 to 2005 as a health-check study of the direct relationship between NAFLD and the incidence of diabetes (23). The causal relationship between NAFLD and diabetes is not yet clear, but NAFLD might play an important role as a confounding factor.
The present study is a retrospective study clarifying the significance of NAFLD on the risk of diabetes in an observational population study in middle-aged men and women who continuously attended health checks from 2004 to 2013 at Hidaka Hospital, which is located in a typical, middle-sized Japanese city near Tokyo, Japan.
Materials and Methods
Subjects
The study population comprised randomly selected individuals who had continuously received an annual health check at Hidaka Hospital, Takasaki, Japan, from April 2004 to October 2013. Subjects with the following were excluded: 1) alcohol intake >20 g/day (based on the frequency of drinking alcohol); 2) a recent history of acute illness; 3) taking medications known to modify lipid levels, blood pressure, or blood glucose; 4) taking medications known to induce a fatty liver; 5) being seropositive for hepatitis B or C; and 6) having any other health problem known to be associated with liver steatosis. All cases were aged 35-65 years old. Those with fatty liver in this study were confirmed to have NAFLD.
All of the patients were referred to the hepatology unit at Hidaka Hospital for ultrasound investigation of hepatic steatosis, performed as a part of routine clinical practice. Subjects were divided into those with and without a fatty liver according to the ultrasound results. The fatty liver-positive group included cases that presented with “bright liver” echo patterns according to standard criteria (i.e., evidence of a diffuse increase in the echogenicity of the liver compared with that of the kidneys). The non-fatty liver group was comprised of cases that did not exhibit any echogenic evidence of fatty liver.
Diabetes subjects were defined according to the Japan Diabetes Society (JDS) criteria: HbA1c (NGSP) ≥6.5% and fasting plasma glucose ≥126 mg/dL or the use of a prescribed anti-diabetic agent. In addition, pre-diabetes subjects [mainly those with impaired fasting glucose (IFG)] were also defined according to the JDS criteria: HbA1c (NGSP) <6.5%, fasting plasma glucose 110 to <126 mg/dL, and no prescriptions for anti-diabetic agents. “Suspected diabetes”, as a type pre-diabetes defined by JDS criteria, was not included, since this could not be determined in a single examination.
The weight and height of each participant was measured, and the body mass index (BMI) was calculated to evaluate the presence of obesity. The retrospective study analysis in this health check population was approved by the Ethics Committee of Hidaka Hospital.
Biochemical analysis
After 12-h overnight fasting, blood samples were taken, and sera were isolated and stored at 4℃. The following analytes were measured within 48 hours of drawing blood: liver enzymes, HbA1c, total cholesterol (TC), triglycerides (TG), and direct low-density lipoprotein cholesterol (LDL-C) and high-density lipoproteins (HDL-C) as previously reported (19). The reagent used to measure LDL-C and HDL-C by the direct method was obtained from Denka Seiken (Tokyo, Japan). Liver enzymes, including aspartate aminotransferase (AST), alanine aminotransferase (ALT), gamma-glutamyltranspeptidase (GGT), and choline esterase (ChE), were used as markers of hepatic damages, and glucose, insulin, and hemoglobin A1c (HbA1c) were measured using commercial enzymatic kits on a Hitachi 917 auto-analyzer (Tokyo, Japan).
Statistical analysis
The data are presented as the median with the 25th and 75th percentile. Accordingly, the differences between groups were tested by Mann-Whitney U test, and multivariate analyses were performed after logarithmic transformation of the results for AST, ALT, GGT, TG, choline esterase, and HbA1c. A multiple regression analysis was performed for each variable with age and the presence of fatty liver (binary: 0 or 1) as the explanatory variables in order to examine the relative contribution to fatty liver. A multiple logistic regression analysis was also performed to evaluate the relative contribution of the variables in diagnosing the status of fatty liver. In addition, a factor analysis was performed to explore the commonality among the variables based on the principal component method with the varimax rotation of the factorial axes. A comparison of factor scores derived from the analysis between subjects with or without fatty liver was performed via a receiver operating characteristic (ROC) analysis. The area under the ROC curve was used as an index of accuracy in differentiating the two conditions. All of the statistical analyses were performed using the StatFlex Ver. 6 software program (Artech, Osaka, Japan). p values <0.05 were considered statistically significant.
Results
Clinical and biochemical characteristics in cases without diabetes in 2004
Table 1 shows the clinical and biochemical characteristics of the cases in this study group. The parameters of lipid metabolism, liver function, and glucose homeostasis were all significantly different between sexes (Table 1). BMI was also significantly different between sexes, as well as between the NAFLD and non-NAFLD cases. The most significant difference between sexes was in the prevalence of NAFLD, with values of 15.0% in men and 4.4% in women. These data indicated a 3.4-fold higher prevalence of NAFLD in men than in women.
Table 1.
The Clinical and Biochemical Characteristics of the Study Cases.
| Male (n=1,544) | Female (n=864) | p value | ||||||
|---|---|---|---|---|---|---|---|---|
| Median | 25th percentile | 75th percentile | Median | 25th percentile | 75th percentile | |||
| Age | 45 | 41 | 50 | 46 | 41 | 51 | NS | |
| Body weight (kg) | 67.4 | 61.7 | 73.6 | 53.2 | 48.9 | 58.2 | <0.0001 | |
| BMI | 23.4 | 21.7 | 25.2 | 21.4 | 19.9 | 23.3 | <0.0001 | |
| NAFLD (%) | 15.0 | 4.4 | <0.0001 | |||||
| Systolic Blood pressure (mmHg) | 122 | 114 | 132 | 117 | 107 | 127 | <0.0001 | |
| Diastolic Blood pressure (mmHg) | 78 | 59.0 | 78 | 71 | 65 | 78 | <0.0001 | |
| AST (IU/L) | 21 | 18 | 26 | 18 | 16 | 21 | <0.0001 | |
| ALT (IU/L) | 24 | 18 | 33 | 15 | 12 | 19 | <0.0001 | |
| GGT (IU/L) | 33 | 23 | 54 | 16 | 13 | 22 | <0.0001 | |
| ChE (IU/L) | 5,591 | 4,959 | 6,220 | 4,746 | 4,175 | 5,426 | <0.0001 | |
| UA (mg/dL) | 6.2 | 5.4 | 7.0 | 4.3 | 3.8 | 4.9 | <0.0001 | |
| FBS (mg/dL) | 101 | 96 | 106 | 95 | 91 | 100 | <0.0001 | |
| HbA1c(JDS) (%) | 5.1 | 4.9 | 5.4 | 5.1 | 4.8 | 5.3 | <0.0001 | |
| TC (mg/dL) | 197 | 176 | 217 | 197 | 174 | 218.0 | NS | |
| TG (mg/dL) | 106 | 75 | 151 | 66 | 50 | 91 | <0.0001 | |
| HDL-C (mg/dL) | 49 | 43 | 58.0 | 62 | 54 | 71 | <0.0001 | |
| LDL-C (mg/dL) | 122 | 102 | 143 | 110 | 91 | 132 | <0.0001 | |
Comparison of diagnostic parameters among cases with or without NAFLD in men and women
Table 2 compares the values between NAFLD and non-NAFLD cases for both sexes. All of the parameters were further divided into those with or without a NAFLD. We noted a stronger association of NAFLD with lipoproteins (elevated TG, low HDL-C) and markers of glucose homeostasis and liver function in those with NAFLD than in those without. HDL-C levels were significantly lower in those with NAFLD than in those without, and similar trends were noted for choline esterase (ChE) and uric acid (UA). In addition, NAFLD cases showed significantly higher levels of ALT, AST, and γ-GTP than those without, although most of these levels were still within the normal ranges.
Table 2.
The Comparison of the Diagnostic Parameters among the Cases with or without Fatty Liver.
| Male (n=1544) | Female (n=864) | p value | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NAFLD (A) (n=232) | non-NAFLD (B) (n=1,312) | NAFLD (C ) (n=38) | non-NAFLD (D) (n=826) | A vs. B | C vs. D | A vs. C | B vs. D | |||||||||||||
| Median | 25th percentile | 75th percentile | Median | 25th percentile | 75th percentile | Median | 25th percentile | 75th percentile | Median | 25th percentile | 75th percentile | |||||||||
| Age | 44 | 40 | 49 | 46 | 41 | 50 | 49 | 45 | 53 | 46 | 41 | 50 | NS | <0.05 | <0.01 | NS | ||||
| Body weight (kg) | 75.0 | 69.3 | 82.0 | 66.3 | 61.0 | 72.8 | 64.7 | 55.4 | 70.7 | 53.0 | 48.9 | 57.7 | <0.01 | <0.01 | <0.01 | <0.01 | ||||
| BMI | 25.5 | 24.2 | 27.6 | 23.0 | 21.4 | 24.6 | 26.1 | 23.8 | 29.2 | 21.2 | 19.8 | 23.1 | <0.01 | <0.01 | NS | <0.01 | ||||
| Systolic Blood pressure (mmHg) | 126 | 117 | 135 | 121 | 113 | 131 | 123 | 115 | 134.0 | 117 | 107 | 127 | <0.01 | <0.05 | NS | <0.01 | ||||
| Diastolic Blood pressure (mmHg) | 80 | 73 | 86 | 77 | 70 | 84 | 75 | 69 | 80 | 71 | 64 | 78 | <0.01 | NS | NS | <0.01 | ||||
| AST (IU/L) | 25 | 21 | 33 | 21 | 18 | 24 | 22 | 18 | 29 | 18 | 16 | 20 | <0.01 | <0.01 | <0.05 | <0.01 | ||||
| ALT (IU/L) | 40 | 28 | 58 | 22 | 18 | 30 | 25 | 21 | 40 | 15 | 12 | 19 | <0.01 | <0.01 | <0.05 | <0.01 | ||||
| GGT (IU/L) | 43 | 29 | 66 | 32 | 22 | 51 | 25 | 21 | 31 | 16 | 13 | 21 | <0.01 | <0.01 | <0.01 | <0.01 | ||||
| ChE (IU/L) | 6,111 | 5,543 | 6,722 | 5,485 | 4,888 | 6,135 | 5,914 | 5,523 | 6,484 | 4,684 | 4,155 | 5,321 | <0.01 | <0.01 | NS | <0.01 | ||||
| UA (mg/dL) | 6.7 | 6.0 | 7.4 | 6.1 | 5.3 | 6.9 | 5.2 | 4.5 | 6.1 | 4.3 | 3.7 | 4.9 | <0.01 | <0.01 | <0.01 | <0.01 | ||||
| FBS (mg/dL) | 103 | 98 | 107 | 100 | 95 | 105 | 106 | 99 | 113 | 95 | 91 | 99.0 | <0.01 | <0.01 | NS | <0.01 | ||||
| HbA1c(JDS) (%) | 5.3 | 5.0 | 5.5 | 5.1 | 4.9 | 5.4 | 5.5 | 5.1 | 5.7 | 5.0 | 4.8 | 5.3 | <0.01 | <0.01 | NS | <0.01 | ||||
| TC (mg/dL) | 206 | 178 | 224 | 196 | 175 | 216 | 216 | 201 | 233 | 195 | 173 | 217 | <0.01 | <0.01 | NS | NS | ||||
| TG (mg/dL) | 142 | 102 | 201 | 100 | 71 | 143 | 126 | 77 | 165 | 64 | 50 | 87 | <0.01 | <0.01 | NS | <0.01 | ||||
| HDL-C (mg/dL) | 43 | 39 | 49.0 | 51 | 44 | 59 | 51 | 44 | 59 | 62 | 55 | 71 | <0.01 | <0.01 | <0.01 | <0.01 | ||||
| LDL-C (mg/dL) | 134 | 113 | 157 | 120 | 101 | 142 | 139 | 125 | 159 | 109 | 90 | 130 | <0.01 | <0.01 | NS | <0.01 | ||||
Incidence of diabetes over 10 years by presence of NAFLD
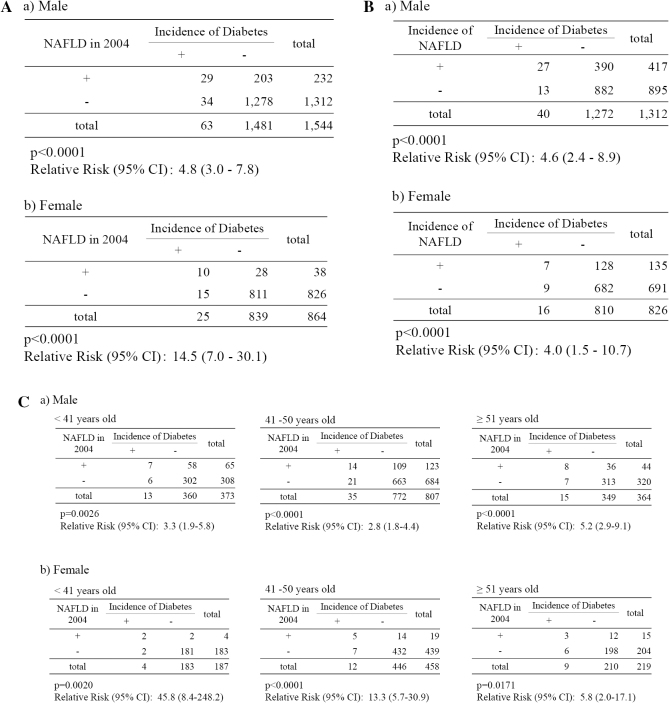
The median age of participants was 46.0 years at the start of the study period, and the follow-up period was 10 years. Table 3A shows that the incidence of diabetes in the NAFLD group was 12.5% (29/232) in men and 26.3% (10/38) in women, whereas the incidence in the non-NAFLD group was 2.6% (34/1,312) in men and 1.8% (15/826) in women. The relative risk of diabetes associated with NAFLD was 4.8 [95% confidence interval (CI) 3.0-7.8, p<0.0001] in men and 14.5 (95% CI 7.0-30.1, p<0.0001) in women. The incidence of diabetes over the 10-year period was significantly higher in women than in men, although the proportion of cases of diabetes in women with NAFLD was significantly lower than that in men with NAFLD. In addition, the incidence of diabetes in non-NAFLD cases was significantly lower than in NAFLD cases (p<0.0001).
Table 3.
(A) Relative Risk of NAFLD for the Prediction of Diabetes. (B) Relative Risk of the Incidence of NAFLD in 2013 for the Prediction of Diabetes. (C) Age-stratified Relative Risks of NAFLD in 2004 for the Prediction of Diabetes.
Table 3B shows that the relative risk of diabetes associated with the incidence of NAFLD during the 10-year observational period was 4.6 (95% CI 2.4-8.9, p<0.0001) in men and 4.0 (95% CI 1.5-10.7, p<0.01) in women. Although the relative risk of incidence of diabetes associated with NAFLD was significantly higher in women than in men (Table 3A), the relative risk of incidence of diabetes associated with the incidence of NAFLD was almost the same between sexes.
In addition, the samples were stratified into 3 groups by age: <41 years old, 41 to 50 years old, and ≥51 years old. Table 3C shows that the age-stratified relative risk of diabetes associated with NAFLD in 2004 was 3.3 (95% CI 1.9-5.8, p<0.01), 2.8 (95% CI 1.5-2.8, p<0.0001), and 5.2 (95% CI 2.9-9.1, p<0.0001) in men, and 45.8 (95% CI 8.4-248.2, p<0.01), 13.3 (95% CI 5.7-30.9, p<0.0001), and 5.8 (95% CI 2.0-17.1, p<0.05) in women for <41 years old, 41 to 50 years old, and ≥51 years old, respectively.
Multiple logistic regression analysis of diagnostic markers suggestive of diabetes risk in 2013
Table 4 shows the results of the multiple regression analysis with age, gender, NAFLD, HbA1c, lipids, and lipoproteins set as the target variables. The values in Table 4 (A and B) represent the standardized regression coefficients that correspond to the partial (or adjusted) correlation coefficient between the target variables of diabetes and each explanatory variable.
Table 4.
(A) Multiple Regression Analysis of the Diagnostic Parameters Associated with the Prediction of Diabetes. (B) Multiple Regression Analysis of Diagnostic Parameters without HbA1c Associated with the Prediction of Diabetes.
A Incidence of Diabetes in 2013
| Parameter | β | SE (β) | z value | p value | |
|---|---|---|---|---|---|
| HbA1c | 3.673 | 0.399 | 9.202 | <0.0001 | |
| NAFLD | 1.014 | 0.258 | 3.939 | 0.0001 | |
| HDL-C | -0.043 | 0.013 | 3.357 | 0.0008 | |
| Gender (female) | 0.790 | 0.296 | 2.673 | 0.0075 | |
| Age | -0.040 | 0.018 | 2.225 | 0.0261 | |
| Systolic Blood Pressure | 0.015 | 0.008 | 1.846 | 0.0649 | |
| β= partial regression coefficient, SE (β)=standard error of β, z value =β/SE (β) AUC = 0.865 | |||||
| B Incidence of Diabetes in 2013 | |||||
| β | SE (β) | z value | p value | ||
| NAFLD | 1.446 | 0.247 | 5.854 | <0.0001 | |
| HDL-C | -0.039 | 0.012 | 3.178 | 0.0015 | |
| Gender (female) | 0.621 | 0.279 | 2.228 | 0.0259 | |
| LDL Choresterol | 0.007 | 0.003 | 2.130 | 0.0332 | |
| Systolic Blood Pressure | 0.014 | 0.007 | 1.967 | 0.0492 | |
| TG | 0.003 | 0.001 | 1.966 | 0.0493 | |
β= partial regression coefficient, SE (β)=standard error of β, z value =β/SE (β) AUC = 0.865
To identify variables effective in predicting diabetes from the diagnostic markers (age, gender, ALT, AST, ChE, UA, HDL-C, LDL-C, and HbA1c), a multiple logistic regression analysis was performed by the backward elimination procedure. Table 4A shows the variables selected through the best regression model. The predictors of diabetes (from most to least important) were HbA1c, NAFLD, HDL-C, gender (female), and age. The accuracy of prediction by the model was evaluated by an ROC analysis, with the area under the curve (AUC) at a high level of 0.865. After removing the strongest predictor HbA1c (Table 4B), NAFLD was effective in predicting the diabetes, with an accuracy of AUC=0.788.
To investigate the relationship between NAFLD and the diabetes incidence and cardiovascular risk markers in 2013, we carried out a multiple regression analysis using NAFLD as the target variable and diabetes incidence and cardiovascular risk markers in 2013 as the explanatory variables (Table 5). NAFLD was more strongly associated with diabetes incidence than cardiovascular risk markers in 2013.
Table 5.
Multiple Regression Analysis of NAFLD Associated with the Diabetes Incidence and Cardiovascular Risk Markers in 2013.
NAFLD
| z value | p value | |
|---|---|---|
| Age | 2.118 | 0.034 |
| Gender | 1.071 | 0.284 |
| BMI | 0.313 | 0.754 |
| Systric Blood pressure | 1.449 | 0.148 |
| Diastolic Blood pressure | 1.697 | 0.090 |
| HDL-C | 2.009 | 0.045 |
| TG | 0.274 | 0.274 |
| LDL-C | 0.990 | 0.990 |
| Incidence of Diabetes | 3.442 | 0.001 |
Factor analysis for evaluation of commonality among the diagnostic parameters
The test results of 10 mutually related diagnostic parameters were subjected to an exploratory factor analysis to investigate the commonality among them. Using the principal component method with varimax rotation of the factorial axes, we obtained five factors as shown in Table 6. The values in the table correspond to factor loadings, which represent the correlation coefficient between the identified common factor and each of the original variables. From the pattern of factor loadings, Factor 1 was highly positively correlated with gender, BMI, TG, and HDL-C. Therefore, the factor was interpreted as reflecting the serum lipid level and accumulation of visceral fat, and Factor 1 was referred to as “visceral fat”. Factor 2 was interpreted as representing blood pressure. Factor 3 showed HbA1c and age. Therefore, Factor 3 was interpreted as representing the status of diabetes. Factor 4 was found to be highly positively correlated with HbA1c and NAFLD. Therefore, Factor 4 was interpreted as representing the incidence of diabetes. Factor 5 was highly correlated with BMI and LDL-C, representing obesity. The scores of each factor were computed for each individual. The accuracy of each score in differentiating the status of fatty liver was evaluated by an ROC analysis. The area under the ROC curves for Factors 1, 2, 3, 4, and 5 were 0.726, 0.608, 0.825, 0.841, and 0.690, respectively, confirming a higher specificity of Factor 4 to the incidence of diabetes than other Factors.
Table 6.
Factor Analysis for the Evaluation of Commonality among the Diagnostic Parameters.
| Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 5 | |
|---|---|---|---|---|---|
| Age | -0.0120 | 0.0585 | 0.6433 | -0.2164 | 0.0478 |
| Gender | 0.5059 | -0.799 | -0.0205 | -0.0707 | -0.2176 |
| BMI | -0.3508 | 0.1282 | 0.0356 | 0.0668 | 0.6031 |
| Diastolic blood pressure | 0.0876 | 0.8823 | 0.0729 | 0.0306 | -0.0006 |
| Systoloc blood pressure | -0.1417 | 0.8683 | -0.0287 | 0.0567 | -0.0075 |
| HDL-Chorestrerol | 0.7185 | 0.0795 | -0.0504 | -0.1105 | -0.2277 |
| TG | -0.4762 | 0.0355 | -0.0177 | 0.366 | -0.0199 |
| LDL-Choresterol | -0.0882 | -0.0864 | 0.1616 | 0.0700 | 0.3102 |
| NAFLD | -0.1323 | 0.0435 | -0.0133 | 0.4166 | 0.0848 |
| HbA1c | -0.0266 | -0.0121 | 0.6009 | 0.3200 | 0.2019 |
| Contribution of Factor | 0.709 | 0.560 | 0.829 | 0.854 | 0.665 |
Discussion
In the present health check study, we demonstrated that NAFLD is a strong risk factor for developing diabetes in middle-aged healthy Japanese men and especially in women. Specifically, the results indicated that women with NAFLD have a significantly higher incidence of diabetes than men with NAFLD, although the number of cases of NAFLD among women was significantly lower than among men. This study had several strengths, including the use of a population-based sample, sufficient ascertainment of a diabetes diagnosis, exclusion of individuals with prediabetes and diabetes at baseline, and adjustment for a number of potential confounding factors based on the criteria defined by the JDS.
Table 3 shows that the relative risk of developing diabetes was 4.8 (95% CI: 3.0-7.8, p<0.0001) in men and 14.5 (95% CI 7.0-30.1, p<0.0001) in women among subjects with NAFLD, which was higher than in almost all previous cohort studies (23-33). A systematic review and meta-analysis indicated that the pooled odds ratio for cohort studies was 2.42 (95% CI: 1.78-3.29). Most studies diagnosed T2DM only by fasting blood glucose level or by fasting blood glucose plus HbA1c level (with/without taking antidiabetic drugs). Only one nested case-control study in men made the diagnosis based on the 75 g OGTT with an odds ratio of 5.5 (95% CI 3.6-8.5, p<0.001) (23). Making a diagnosis not based on the 2-h postprandial glucose levels may ignore a proportion of potential diabetic patients. Since patients with NAFLD were more likely to have a risk of diabetes than those without NAFLD, incident diabetes would more likely be unnoticed in the NAFLD group, indicating that the risk of T2DM associated with NAFLD might be underestimated in these studies. Future large population studies are required to confirm that the risk of T2DM associated with NAFLD might be underestimated without performing OGTTs.
Table 3A shows that, although the prevalence of NAFLD in men was higher than in women, women with NAFLD had a significantly higher incidence of diabetes than men. However, interestingly, Table 3B shows that the incidence of NAFLD and the relative risk of incidence of diabetes in women found during the observational period was almost the same as in men. In this study, it is possible that most female subjects entered menopause during the 10-year study period, as the median of age for female subjects was 46 in 2004, although we did not investigate the status of menstruation in female subjects. To clarify the effect of postmenopausal status on our findings, we stratified all of the subjects into three groups by age: <41 years old, 41-50 years old, and ≥51 years old, and calculated the age-stratified relative risks. Table 3C shows that the age-adjusted relative risk of incidence in women <41 years old was the highest among women, and the relative risk in women ≥51 years old, where most were likely postmenopausal, was almost the same as that of men. Because estrogen, which has a protective effect against NAFLD (34) and diabetes (35) in women, decreases in postmenopausal women, the prevalence of NAFLD and relative risk of incidence of diabetes with NAFLD in women was higher than in men. The effects of estrogen may therefore have influenced the results obtained over the 10-year course of our study.
Table 4 shows that HbA1c and NAFLD were stronger diagnostic markers of incidence of diabetes than others by multiple regression analyses (36). HDL-C, gender, and age were also strong markers of the incidence of diabetes. The accuracy of the prediction by the model was evaluated by an ROC analysis, and the AUC was extremely high (0.865). After removing the strongest predictor (HbA1c), NAFLD proved to still be effective in that order for predicting diabetes with an accuracy of AUC=0.788.
A multiple logistic regression analysis (Table 5) revealed that fatty liver and incident diabetes were significantly correlated. Although diabetes and visceral fat are known to be strongly correlated, fatty liver is independent from the visceral adipose tissue when predicted by plasma adiponectin levels as a specific fatty liver biomarker (36), as previously reported in the Framingham Study (37).
As an additional investigation, we obtained five factors by exploratory factor analysis, as shown in Table 6. These five factors were interpreted as reflecting or representing visceral fat (Factor 1), blood pressure (Factor 2), status of diabetes (Factor 3), incidence of diabetes (Factor 4), and obesity (Factor 5). Factor 4 showed moderate positive correlation with NAFLD and HbA1c. Therefore, Factor 4 was interpreted as representing the incidence of diabetes. Factors such as age, NAFLD, and HbA1c primarily represent the status and incidence of diabetes, while the others are primarily visceral fat, obesity, and blood pressure factors. Although HDL-C and gender (female) were shown to be more significantly associated with the incidence of diabetes than with age in Table 3A and B, only slight correlations were found with Factor 3 and 4 by the factor analysis. The individual scores of Factor 4 (DM score) were computed, and the diagnostic utility of the DM score in diagnosing the presence of incidence of diabetes was examined. The AUC representing the accuracy of the diagnosis was 0.841, while that of HbA1c was 0.802 (data not shown). The use of Factor 4 markers, which are most commonly ordered in routine clinical practice at hospital laboratories, could improve the accuracy of predicting the incidence of diabetes when a diagnosis of NAFLD is added.
Several limitations associated with the present study warrant mention. First, despite our best efforts, we had a relatively low follow-up rate over the 10-year study period, which was similar with most previous reports (30-32, 38). It is challenging for a population-based cohort study (health check at the same hospital) to maintain an adequate rate of follow-up nowadays. The individuals that participated in the follow-up study, compared with those who did not, were elderly, had more fatty liver, and had higher BMI and metabolic parameters (blood pressure and lipids). However, no marked differences were observed in gender, lifestyle factors, and blood glucose levels between the followed-up and non-followed-up groups. Second, our study sample was not large enough to conduct subgroup analyses to explore the association between degree of NAFLD and the development of T2DM. Third, ultrasound was the preferred choice in our study because of its low cost, safety profile, and availability, although liver biopsy remains the current gold standard for the diagnosis of NAFLD (39). Nevertheless, ultrasound becomes less sensitive when the liver fat content is below 33% or with an increase in abdominal obesity (39-41), which might bias the results to some extent.
In conclusion, we found that NAFLD was a significant predictor for future diabetes in middle-aged Japanese men and especially in women. Although the prevalence of NAFLD was significantly lower in women than in men, the causal relationship between NAFLD and diabetes in women seemed to be stronger than in men in our 10-year observational study.
The authors state that they have no Conflict of Interest (COI).
References
- 1. Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Am J Gastroenterol 107: 811-826, 2012. [DOI] [PubMed] [Google Scholar]
- 2. Bellentani S, Scaglioni F, Marino M, Bedogni G. Epidemiology of non-alcoholic fatty liver disease. Dig Dis 28: 155-161, 2010. [DOI] [PubMed] [Google Scholar]
- 3. Browning JD, Szczepaniak LS, Dobbins R, et al. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology 40: 1387-1395, 2004. [DOI] [PubMed] [Google Scholar]
- 4. Eguchi Y, Hyogo H, Ono M, et al. Prevalence and associated metabolic factors of nonalcoholic fatty liver disease in the general population from 2009 to 2010 in Japan: a multicenter large retrospective study. J Gastroenterol 47: 586-595, 2012. [DOI] [PubMed] [Google Scholar]
- 5. Farrell GC. Non-alcoholic steatohepatitis: what is it, and why is it important in the Asia-Pacific region? J Gastroenterol Hepatol 18: 124-138, 2003. [DOI] [PubMed] [Google Scholar]
- 6. Clark J, Diehl A. Hepatic steatosis and type 2 diabetes mellitus. Curr Diab Rep 2: 210-215, 2002. [DOI] [PubMed] [Google Scholar]
- 7. Bellentani S, Saccoccio G, Masutti F, et al. Prevalence of and risk factors for hepatic steatosis in Northern Italy. Ann Intern Med 132: 112-117, 2000. [DOI] [PubMed] [Google Scholar]
- 8. Akbar DH, Kawther AH. Nonalcoholic fatty liver disease in Saudi type 2 diabetic subjects attending a medical outpatient clinic, prevalence and general characteristics. Diabetes Care 26: 3351-3352, 2003. [DOI] [PubMed] [Google Scholar]
- 9. Gupte P, Amarapurkar D, Agal S, et al. Non-alcoholic steatohepatitis in type 2 diabetes mellitus. J Gastroenterol Hepatol 19: 854-858, 2004. [DOI] [PubMed] [Google Scholar]
- 10. Assy N, Kaita K, Mymin D, Levy C, Rosser B, Minuk G. Fatty infiltration of liver in hyperlipidemic patients. Dig Dis Sci 45: 1929-1934, 2000. [DOI] [PubMed] [Google Scholar]
- 11. Donati G, Stagni B, Piscaglia F, et al. Increased prevalence of fatty liver in arterial hypertensive patients with normal liver enzymes: role of insulin resistance. Gut 53: 1020-1023, 2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Reaven GM. Banting lecture 1988: Role of insulin resistance in human disease. Diabetes 37: 1595-1607, 1988. [DOI] [PubMed] [Google Scholar]
- 13. Day C, Saksena S. Nonalcoholic steatohepatitis: definitions and pathogenesis. J Gastroenterol Hepatol 17: S377-S384, 2002. [DOI] [PubMed] [Google Scholar]
- 14. Ryysy L, Hakkinen AM, Goto T, et al. Hepatic fat content and insulin action on free fatty acids and glucose metabolism rather than insulin absorption are associated with insulin requirement during therapy in type 2 diabetic patients. Diabetes 49: 749-758, 2000. [DOI] [PubMed] [Google Scholar]
- 15. Seppala-Lindroos A, Vehkavaara S, Hakkinen AM, et al. Fat accumulation in the liver is associated with defects in insulin suppression of glucose production and serum fatty acids independent of obesity in normal men. J Clin Endocrinol Metab 87: 3023-3028, 2002. [DOI] [PubMed] [Google Scholar]
- 16. Jimba S, Nakagami T, Takahashi M, et al. Prevalence of non-alcoholic fatty liver disease and its association with impaired glucose metabolism in Japanese adults. Diabet Med 22: 1141-1145, 2005. [DOI] [PubMed] [Google Scholar]
- 17. Hanley AJ, Williams K, Festa A, et al. Elevations in markers of liver injury and risk of type 2: the insulin resistance atherosclerosis study. Diabetes 53: 2623-2632, 2004. [DOI] [PubMed] [Google Scholar]
- 18. Perry IJ, Wannamethee SG, Shaper AG. Prospective study of serum γ-glutamyltransferase and risk of NIDDM. Diabetes Care 21: 732-737, 1998. [DOI] [PubMed] [Google Scholar]
- 19. Nakanishi N, Nishina K, Li W, Sato M, Suzuki K, Tatara K. Serum γ-glutamyltransferase and development of impaired fasting glucose or type 2 diabetes in middle-aged Japanese men. J Intern Med 254: 287-295, 2003. [DOI] [PubMed] [Google Scholar]
- 20. Lee DH, Jacobs DR Jr, Gross M, et al. γ-glutamyltransferase is a predictor of incident diabetes and hypertension: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Clin Chem 49: 1358-1366, 2003. [DOI] [PubMed] [Google Scholar]
- 21. Lee DH, Ha MH, Kim JH, et al. Gamma-glutamyltransferase and diabetes: a 4 year follow-up study. Diabetologia 46: 359-364, 2003. [DOI] [PubMed] [Google Scholar]
- 22. Vozarova B, Stefan N, Lindsay RS, et al. High alanine aminotransferase is associated with decreased hepatic insulin sensitivity and predicts the development of type 2 diabetes. Diabetes 51: 1889-1895, 2002. [DOI] [PubMed] [Google Scholar]
- 23. Shibata M, Kihara Y, Taguchi M, Tashiro M, Otsuki M. Nonalcoholic fatty liver disease is a risk factor for type 2 diabetes in middle-aged Japanese men. Diabetes Care 30: 2940-2944, 2007. [DOI] [PubMed] [Google Scholar]
- 24. Zelber-Sagi S, Lotan R, Shibolet O, et al. Non-alcoholic fatty liver disease independently predicts prediabetes during a 7-year prospective follow-up. Liver Int 33: 1406-1412, 2013. [DOI] [PubMed] [Google Scholar]
- 25. Yamada T, Fukatsu M, Suzuki S, Wada T, Yoshida T, Joh T. Fatty liver predicts impaired fasting glucose and type 2 diabetes mellitus in Japanese undergoing a health checkup. J Gastroenterol Hepatol 25: 352-356, 2010. [DOI] [PubMed] [Google Scholar]
- 26. Sung KC, Kim SH. Interrelationship between fatty liver and insulin resistance in the development of type 2 diabetes. J Clin Endocrinol Metab 96: 1093-1097, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sung KC, Jeong WS, Wild SH, Byrne CD. Combined influence of insulin resistance, overweight/obesity, and fatty liver as risk factors for type 2 diabetes. Diabetes Care 35: 717-722, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Park SK, Seo MH, Shin HC, Ryoo JH. Clinical availability of nonalcoholic fatty liver disease as an early predictor of type 2 diabetes mellitus in Korean men: 5-year prospective cohort study. Hepatology 57: 1378-1383, 2013. [DOI] [PubMed] [Google Scholar]
- 29. Okamoto M, Takeda Y, Yoda Y, Kobayashi K, Fujino MA, Yamagata Z. The association of fatty liver and diabetes risk. J Epidemiol 13: 15-21, 2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kotronen A, Laaksonen MA, Heliövaara M, et al. Fatty liver score and 15-year incidence of type 2 diabetes. Hepatol Int 7: 610-621, 2013. [DOI] [PubMed] [Google Scholar]
- 31. Kim CH, Park JY, Lee KU, Kim JH, Kim HK. Fatty liver is an independent risk factor for the development of type 2 diabetes in Korean adults. Diabet Med 25: 476-481, 2008. [DOI] [PubMed] [Google Scholar]
- 32. Heianza Y, Arase Y, Tsuji H, et al. Metabolically healthy obesity, presence or absence of fatty liver, and risk of type 2 diabetes in Japanese individuals: Toranomon Hospital Health Management Center Study 20 (TOPICS 20). J Clin Endocrinol Metab 99: 2952-2960, 2014. [DOI] [PubMed] [Google Scholar]
- 33. Fan JG, Li F, Cai XB, Peng YD, Ao QH, Gao Y. Effects of nonalcoholic fatty liver disease on the development of metabolic disorders. J Gastroenterol Hepatol 22: 1086-1091, 2007. [DOI] [PubMed] [Google Scholar]
- 34. Gutierrez-Grobe Y, Ponciano-Rodríguez G, Ramos MH, Uribe M, Méndez-Sánchez N. Prevalence of non alcoholic fatty liver disease in premenopausal, posmenopausal and polycystic ovary syndrome women. The role of estrogens. Ann Hepatol 9: 402-409, 2010. [PubMed] [Google Scholar]
- 35. Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 27: 1047-1053, 2004. [DOI] [PubMed] [Google Scholar]
- 36. Yatsuzuka S, Shimomura Y, Akuzawa M, et al. Plasma adiponectin is a more specific marker of fatty liver than a marker of metabolic syndrome in Japanese men. Ann Clin Biochem 51: 68-79, 2014. [DOI] [PubMed] [Google Scholar]
- 37. Speliotes EK, Massaro JM, Hoffmann U, et al. Liver fat is reproducibly measured using computed tomography in the Framingham Heart Study. J Gastroenterol Hepatol 23: 894-899, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Sung KC, Kim SH. Interrelationship between fatty liver and insulin resistance in the development of type 2 diabetes. J Clin Endocrinol Metab 96: 1093-1097, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Holford TR, White C, Kelsey JL. Multivariate analysis for matched case-control studies. Am J Epidemiol 107: 245-256, 1978. [DOI] [PubMed] [Google Scholar]
- 40. Ohlson LO, Larsson B, Björntorp P, et al. Risk factors for type 2 (non-insulin-dependent) diabetes mellitus: thirteen and one-half years of follow-up of the participants in a study of Swedish men born in 1913. Diabetologia 31: 798-805, 1988. [DOI] [PubMed] [Google Scholar]
- 41. Marchesini G, Brizi M, Bianchi G, et al. Nonalcoholic fatty liver disease: a feature of the metabolic syndrome. Diabetes 50: 1844-1850, 2001. [DOI] [PubMed] [Google Scholar]