Abstract
Neuroendocrine tumors (NETs) of the extrahepatic bile duct are extremely rare and reported infrequently in the literature. These tumors are difficult to diagnose preoperatively, and the prognosis is variable, often determined by extent of disease, tumor grade and resectability. This case report presents a 45-year-old male with history of biliary obstruction relieved by endobiliary stents with common hepatic duct stricture just above the cystic duct, thought to be a Klatskin’s cholangiocarcinoma. Final pathological examination was consistent with primary extrahepatic NET.
INTRODUCTION
While neuroendocrine tumors (NETs) are most commonly found in the digestive system, NETs originating from the bile duct are incredibly rare. The World Health Organization (WHO) classifies neoplasms with neuroendocrine characteristics as NETs. The WHO classification system divides these tumors into NET Grade 1, NET Grade 2 and neuroendocrine carcinoma (NEC) [1]. NECs were previously classified as small-cell carcinomas (SCCs), large cell neuroendocrine carcinomas or poorly differentiated neuroendocrine carcinomas [2]. Here we present the clinical course and surgical management of a patient with NET Grade 2 of the common hepatic duct and common bile duct.
CASE REPORT
The patient is a 45-year-old African American male, previously healthy, but was examined at an outside facility for abdominal pain, jaundice, and abnormal liver function tests (LFTs) with hyperbilirubinemia. An esophagogastroduodenoscopy and endoscopic ultrasound was performed suggesting a dilated common hepatic duct to 1.4 cm with tapering of the duct at the ampulla to 6 mm, otherwise normal. Endoscopic retrograde cholangiopancreatography showed dilated intrahepatic right and left hepatic ducts with a tight hilar stricture, Bismuth Type I, with a 3 cm stricture encompassing the cystic and common bile ducts. Endoscopic brushings of the bile ducts showed benign glandular stromal tissue, non-diagnostic for malignancy. An MRI with contrast of the abdomen showed a non-cirrhotic liver with periductal thickening of the right and left central hepatic ducts with restricted diffusion and severe stenosis suggesting a Klatskin-type hilar cholangiocarcinoma, without evidence of extrahepatic disease (Figs 1 and 2). Imaging of the chest was negative for tumor. The laboratory workup showed normal liver function following endoscopic stenting, normal alpha-fetoprotein level, CA 19-9 and CEA. Colonoscopy was also negative for malignancy.
Figure 1:
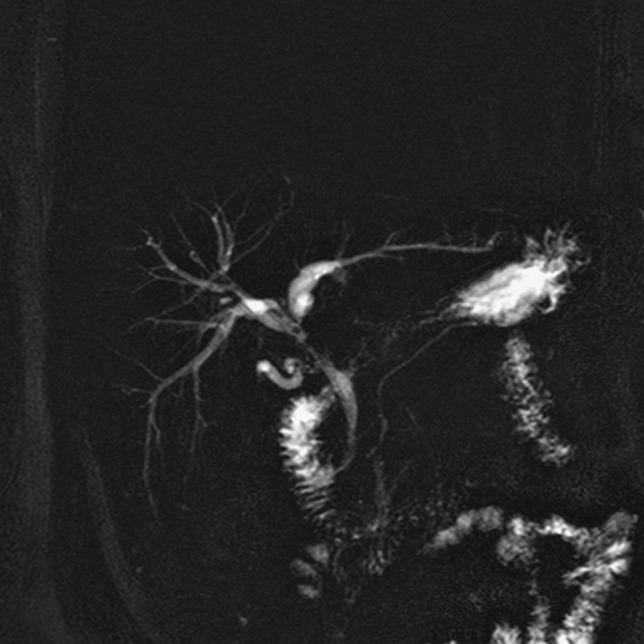
Preoperative MRI/MRCP with Bismuth Type I stricture of the common hepatic duct.
Figure 2:
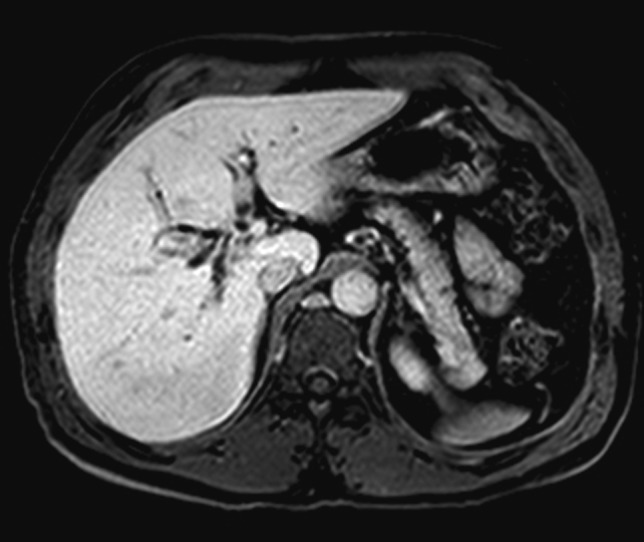
Preoperative axial T1 MRI with dilated right and left intrahepatic bile ducts.
The patient was scheduled for exploratory laparotomy with bile duct resection and possible extended hepatectomy. At exploration, there was no evidence of carcinomatosis. A complete celiac and portal lymphadenectomy was performed, completely skeletonizing the common, proper, left and right hepatic arteries, portal vein and extrahepatic bile duct. The gallbladder and entire extrahepatic biliary tree were excised en-bloc. The distal common bile duct margin was negative for malignancy on frozen examination. In addition, the right and left hepatic duct margins were negative for malignancy on frozen section. The hepatic ducts were opened, identifying the 3 cm occlusive stricture encompassing the cystic duct, common hepatic duct, and common bile duct. Biliary continuing was re-established using a Roux-N-Y intrahepatic hepaticojejunostomy with spatulation of the right and left hepatic ducts into a common channel for a single biliary anastomosis. Estimated blood loss was <100 ml. The patient had an unremarkable postoperative course and was discharged home on post-op Day 3.
Final pathology demonstrated a well-differentiated NET, intermediate grade, infiltrating the entire length of the hepatic duct and common bile duct, ~4 cm in length. One of four periductal lymph nodes was also positive for metastatic NET, while the celiac, hepatic artery and portal lymph nodes were negative for tumor. The pathological stage was pT2,N1. Ki-67 immunostaining revealed a proliferative index of 4%. Given the unexpected final pathology, an octreotide scan was performed postoperatively showing no evidence of hepatic or extrahepatic disease, and chromogranin A and serotonin were within normal limits (Fig. 3). Follow-up MRI at 6 months post-op showed no evidence of recurrent or residual disease, and the patient is currently asymptomatic and doing well. The unexpected pathology was discussed in our interdisciplinary liver tumor board. No further adjuvant therapy, such as somatostatin, was recommended given the completely resected tumor and lack of symptoms with normal serotonin and chromogranin A levels and absence of extrahepatic disease.
Figure 3:
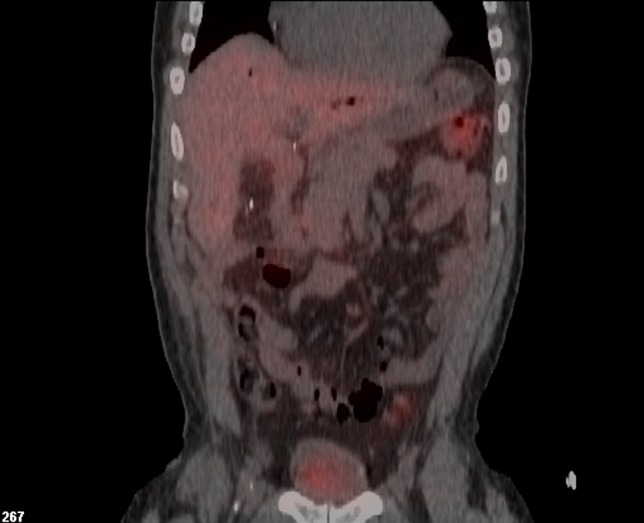
Postoperative In-111 octreotide scan showing no evidence of persistent or recurrent disease following biliary resection and hepaticojejunostomy reconstruction.
DISCUSSION
NETs arising from the biliary tract are extremely rare. Only 0.19% of tumors arising from the extrahepatic bile duct (EHBD) are NECs [3], and only 0.32% are NETs [4]. Of the extrahepatic biliary NETs reported, most are found in the common hepatic duct and distal common bile duct (19.2%), followed by the middle of the common bile duct (17.9%), cystic duct (16.7%) and proximal common bile duct (11.5%) [5]. A prior literature review including biliary NEC cases between 1985 and 2015 found only 24 reported cases of NEC found in the extrahepatic biliary ducts, excluding the intrahepatic bile duct, the gallbladder and the ampulla of Vater [5].
As seen in this case, a preoperative diagnosis of NET can be difficult to make, and the differential diagnosis is widely variable including cholangiocarcinoma, secondary metastatic tumor and lymphoma. In addition, NETs and NECs arising from the biliary tract have variable malignant potential and may be associated with poor prognosis [6]. The optimal treatment for patients with NET or NEC is controversial as most of the current literature available comes from case reports and small case series, without comparable control groups [7]. Options for the management of localized versus metastatic biliary NETs include complete surgical resection, systemic therapy and multivisceral transplant.
REFERENCES
- 1. Bosman FT, Carneiro F, Hruban RH, Theise ND. WHO Classification of Tumors of the Digestive System. 4th edn Lyon, France: IARC Press, 2010;274–6. [Google Scholar]
- 2. Kihara Y, Yokomizo H, Urata T, Nagamine M, Hirata T. A case report of primary neuroendocrine carcinoma of the perihilar bile duct. BMC Surg 2015;15:125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Albores-Saavedra J, Batich K, Hossain S, Henson DE, Schwartz AM. Carcinoid tumors and small-cell carcinomas of the gallbladder and extrahepatic bile ducts: a comparative study based on 221 cases from the Surveillance, Epidemiology and End Results Program. Ann Diagn Pathol 2009;13:378–83. [DOI] [PubMed] [Google Scholar]
- 4. Hosoda K, Kobayashi A, Shimizu A, Kitagawa N, Ito T, Yamada A, et al. Neuroendocrine tumor of the common bile duct. Surgery 2016;160:525–6. [DOI] [PubMed] [Google Scholar]
- 5. Michalopoulos N, Papavramidis TS, Karayannopoulou G, Pliakos I, Papvramidis ST, Kanellos I. Neuroendocrine tumors of the extrahepatic biliary tract. Pathol Oncol Res 2014;20:765–75. [DOI] [PubMed] [Google Scholar]
- 6. Oshiro Y, Gen R, Hashimoto S, Oda T, Sato T, Ohkohchi N. Neuroendocrine carcinoma of the extrahepatic bile duct: a case report. World J Gastroenterol 2016;22:6960–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gaujoux S, Sauvanet A, Belghiti J. Place of surgical resection in the treatment strategy of gastrointestinal neuroendocrine tumors. Target Oncol 2012;7:153. [DOI] [PubMed] [Google Scholar]


