Abstract
We report surgical management of a disrupted radical prostatectomy vesicourethral anastomosis after bleeding from undiagnosed hemophilia that required re-exploration, pudendal artery embolization, and urinary diversion with nephrostomy and surgical drains. After referral, the 4.5 cm vesicourethral anastomotic defect was reconstructed with a robotic-assisted abdomino-perineal approach. Intra-abdominal robotic-assisted mobilization of the bladder and perineal mobilization of the urethra permitted a tension-free vesicourethral anastomosis while avoiding a pubectomy. Side docking of the Da Vinci Xi robot allows for simultaneous access to the perineum during pelvic minimally invasive surgery, enabling a novel approach to complex bladder neck reconstruction.
Key words: Radical prostatectomy, Bladder neck contracture, Bladder neck stricture, Anastomotic stricture, Reconstruction
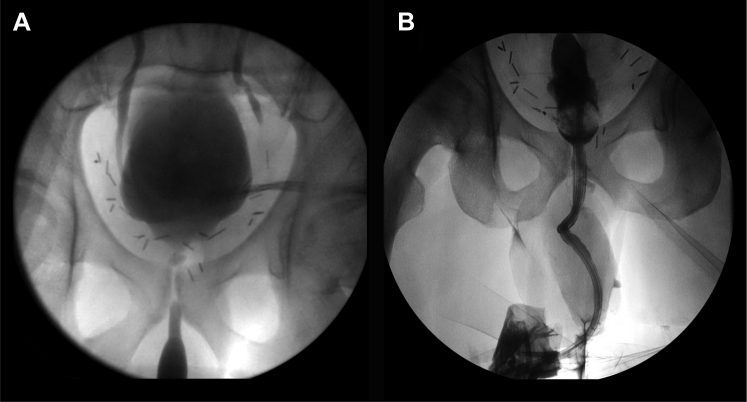
A 49 year-old with Gleason 3+4 prostate cancer underwent open radical prostatectomy complicated by hemorrhage requiring laparotomy and pudendal artery embolization. Disruption of the vesicourethral anastomosis during laparotomy was not repaired and the patient was managed with nephrostomy tubes and a Jackson-Pratt drain, prior to referral. On presentation, urethroscopy demonstrated a type 4 bulbo-membranous stricture1; synchronous cystogram and retrograde urethrogram revealed a 4.5 cm defect (see Fig. 1). Hematology consultation revealed hemophilia A, and the patient was transfused 35 units/kg of recombinant antihemophilic factor VIII, preoperatively.
Figure 1.
(A) Preoperative cystogram and retrograde urethrogram revealing a 4.5 cm vesicourethral anastomotic disruption (B) Postoperative cystogram without 4.5 cm vesicourethral anastomotic disruption.
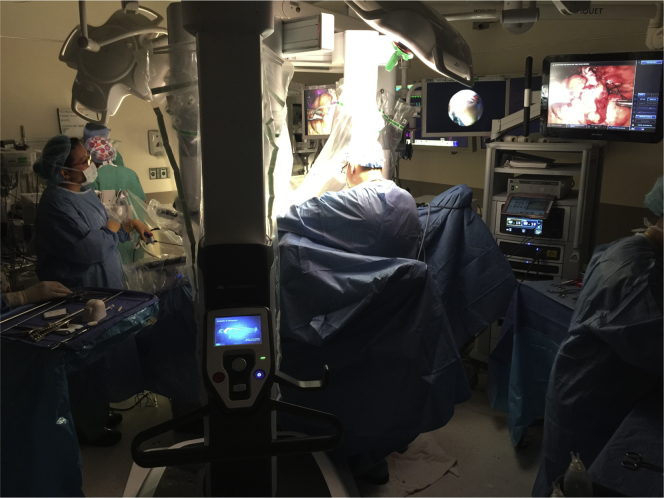
Robotic-assisted vesicourethral anastomotic reconstruction was performed 6-months post-prostatectomy in lithotomy position, docking the Da Vinci Xi robot on the patient's right and including the perineum in the surgical field (see Fig. 2). Four 8 mm trocars and one 12 mm assistant trocar were inserted in a straight line configuration across the abdomen at the level of the umbilicus. The bladder was mobilized to enter the retropubic space. After identifying the bladder on laparoscopy, concurrent cystoscopy was performed by the reconstructive specialist with insertion of a 22-gauge needle through the working channel to aid identification of the urethral stump, which was obliterated by scar tissue. Next, the reconstructive surgeon mobilized the urethra from the bulbo-spongiosus muscle and off of the corpora cavernosa. A barbed (V-Loc™) suture was then used to perform a Rocco stitch, brining the posterior bladder neck into approximation with the periurethral tissue posteriorly. A 0-silk stay suture was placed through the proximal end of the mobilized urethra, and this suture was passed into the pelvis. At this time it was evident that the anastomosis would still be under tension, and so the corpora cavernosa were separated. This maneuver gained an additional centimeter of urethral length, and the silk stay suture was used to once again pass the proximal end of the urethra through the pelvic floor. The anastomosis was then completed using six interrupted 3-0 barbed sutures. Finally, a Foley catheter was inserted and the bladder was irrigated to confirm a watertight reconstruction.
Figure 2.
Da Vinci Xi robot docked on the patient's right side with perineum included on the surgical field.
This innovative approach permits concurrent abdominal bladder and perineal urethral mobilization for a tension-free robotic-assisted anastomosis without requiring pubectomy. Voiding cystogram 2-weeks postoperatively did not reveal contrast extravasation, and the catheter was removed. At 12-months postoperatively, the patient was noted to have 1 pad/day incontinence and an open bladder neck on cystoscopy.
Traditional approaches for posterior urethral reconstruction involve urethral mobilization with or without corporal splitting, pubectomy, urethral rerouting and excision of fibrous scar with an open abdomino-perineal approach for more extensive defects.2, 3, 4, 5 A robotic abdominal approach permits a less invasive mobilization of the bladder for larger urethral defects. In this case, the need for a pubectomy was averted while maintaining acceptable continence outcomes in light of undiagnosed bleeding diatheses and the major complication encountered during retropubic radical prostatectomy.
Conflict of interest
All authors declare they have no conflicts of interest.
References
- 1.Purohit R., Blaivis J., Weinberger J. A new staging system for anterior urethral strictures. Urol Pract. 2014;1(1):35–39. doi: 10.1016/j.urpr.2014.02.001. [DOI] [PubMed] [Google Scholar]
- 2.Kizer W.S., Armenakas N.A., Brandes S.B. Simplified reconstruction of posterior urethral disruption defects: limited role of supracrural rerouting. J Urol. 2007;177(4):1378–1381. doi: 10.1016/j.juro.2006.11.036. discussion 1381–1382. [DOI] [PubMed] [Google Scholar]
- 3.Pratap A., Agrawal C.S., Tiwari A. Complex posterior urethral disruptions: management by combined abdominal transpubic perineal urethroplasty. J Urol. 2006;175(5):1751–1754. doi: 10.1016/S0022-5347(05)00974-2. discussion 1754. [DOI] [PubMed] [Google Scholar]
- 4.Nikolavsky D., Blakely S.A., Hadley D.A. Open reconstruction of recurrent vesicourethral anastomotic stricture after radical prostatectomy. Int Urol Nephrol. 2014;46(11):2147–2152. doi: 10.1007/s11255-014-0816-9. [DOI] [PubMed] [Google Scholar]
- 5.Reiss C.P., Pfalzgraf D., Kluth L.A. Transperineal reanastomosis for the treatment for highly recurrent anastomotic strictures as a last option before urinary diversion. World J Urol. 2014;32(5):1185–1190. doi: 10.1007/s00345-013-1180-6. [DOI] [PubMed] [Google Scholar]