Abstract
We report the case of a 36-year old man who underwent elective posterior lumbar spinal fusion after presenting with bilateral leg pain with associated back pain. He had undergone a L5/S1 discectomy in 2001, which provided good symptomatic relief. On this admission, he underwent elective L4-S1 posterolateral fusion and bilateral L4/5 and L5/S1 decompression. Intra-operatively a pedicle screw had to be re-inserted after fluoroscopy confirmed a lateral breech. The patient had no major postoperative complications until the sixth day when the patient re-presented with acute leg pain and weakness. Following a local multidisciplinary meeting (MDT) an MRI showed a large haematoma at the right psoas muscle. CT angiogram confirmed a bleeding lumbar segmental vessel at the site of the previous misplaced screw and an emergency fluoroscopic guided embolisation of the vessel was performed. The patient recovered well post operatively and was discharged back to the community 12 days later. Haemorrhage, as in this case a psoas haematoma should be considered as one of the differentials in patients with recurrent post-operative radiculopathy following posterior lumbar spine fusion. This should be suspected particularly if there has been a misplacement of one or more screws as this can cause injury to blood vessels and be fatal for the patient.
Keywords: Post-operative complication, Case report, Haemorrhage, Pain, Spinal fusion
Highlights
-
•
Recognition of post-operative complication in minimally invasive spine surgery.
-
•
Importance of urgency in investigating in post-operative spine patients.
-
•
Misplacement of a screw in spine surgery can have serious and potentially fatal outcomes in patients.
1. Introduction
Post-operative complications are often experienced in a specialised area of surgery that requires specific care for the intervention performed. Lumbar artery haemorrhage is in most cases associated with anticoagulant therapy [1] and injuries following lumbar spine surgery have rarely been described [2], [3], [4]. Although rare, we should be aware of the significant mortality associated with haemorrhage in minimally invasive spine surgery. When suspected, urgent intervention is recommended for best patient outcome.
2. Case presentation
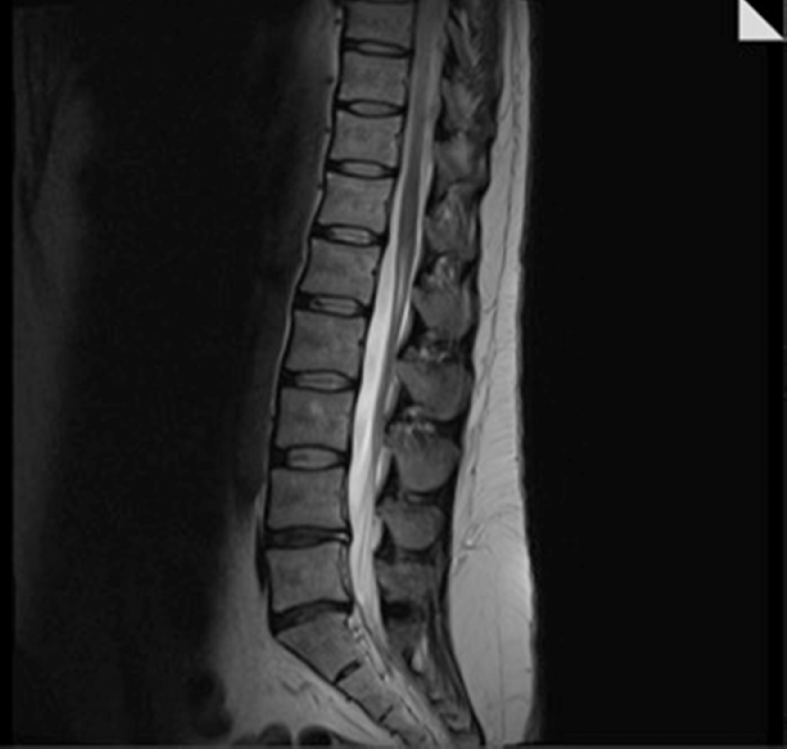
A 36-year-old gentleman underwent elective L4-S1 posterolateral fusion and bilateral L4/5 L5/S1 decompression. Fourteen years previously, he had undergone a left sided L5/S1 discectomy, which at the time had given him excellent relief of his symptoms. Subsequently, he was referred to our unit for further investigation and management. He reported a 12-month history of bilateral leg pain with associated back pain. The leg pain was consistent with bilateral L5 radiculopathy. Standing radiographs of the lumbar spine showed reduced disc heights of the L4/5 and L5/S1 levels but were otherwise unremarkable. An MRI revealed a broad based central L4/5 disc prolapse resulting in canal stenosis and bilateral nerve root compression and well as a of bilateral L5 compression from foraminal narrowing secondary to loss of disc height and circumferential osteophytic bar (See Fig. 1).
Fig. 1.
Sagittal slice of MRI showing disc dessication at L4/5 and L5/S1 levels.
Bilateral L5 nerve root blocks were performed which gave the patient three weeks of complete relief of his symptoms; after which his leg pain slowly returned to previous levels. Hence the patient was offered and consented to L4/5 decompression and discectomy, L5/S1 decompression with L4-S1 posterolateral fusion. The aim of this was to decompress all neural elements, in particular the L5 nerve roots.
The patient underwent the above elective procedure under general anaesthetic and neural monitoring. Pedicle tracks were established using free-hand technique, standard anatomic landmarks and two-person probing. After palpation of bone in all five walls, a marker was placed. Fluoroscopic images, AP and lateral were obtained to further confirm accurate tracks. This was then followed by a thorough decompression of both levels.
Pedicle screws were then inserted into the tracks, sequentially replacing the markers. All screws had excellent hold apart from the right L4 screw. Fluoroscopy confirmed that this screw had not followed the original track and had breached laterally. The screw was hence removed, the correct track retraced and the screw reinserted. Repeat fluoroscopy showed good position of all screws. The rest of the procedure went without complication and no significant bleeding was encountered at anytime.
Immediately after the operation, the patient complained of numbness in the right thigh (L2 distribution). This was accompanied by weakness of hip flexion, 4 out of 5 on the Medical Research Council Scale for Muscle Strength [5]. However these symptoms resolved over the course of 12 hours and was put down to the epidural analgesia that had been administered intra-operatively.
On the first post-operative day, his Haemoglobin (Hb) was 104 g/L, the neurology was normal and the patient was mobilised with routine physiotherapy. Three days after surgery a check x-ray of his lumbar spine was performed and this showed good spinal alignment and satisfactory position of fixation. The patient was discharged home on the fifth post-operative day.
The patient returned to the Emergency Department 24 hours later, with pins and needles in the right thigh, pain in the right groin and reduced power in his right hip. His bladder and bowel functions were normal and the surgical wound site showed no signs of infection. Femoral nerve stretch was strongly positive on the right. Repeat radiographs of the lumbar spine were identical to those taken prior to discharge but an MRI scan revealed a massively enlarged right psoas muscle and the appearance suggested the presence of a large haematoma and secondary inflammation (See Fig. 2).
Fig. 2.
Post-op MRI showing large haematoma in the right psoas.
Although the patient was haemodynamically stable, blood investigations revealed a Hb of 84 g/L which fell to 72 g/L six hours later. After discussion with the radiologist on duty, we decided to proceed with a CT angiogram. This revealed a pseudoaneurysm arising from the right L4 lumbar artery, which was considered to not only be the source for the psoas haematoma but also to be actively bleeding.
An emergency fluoroscopic guided embolisation of the vessel under local anaesthetic was performed and there were no immediate procedural complications.
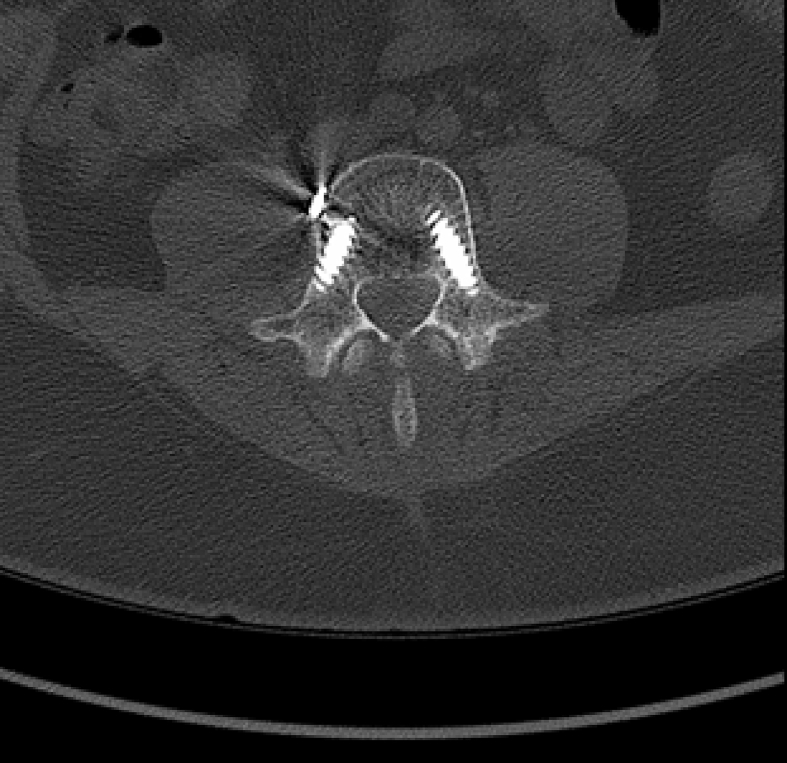
Over the following 48 hours, his groin pain improved as did the power in his right lower-limb. He was mobilised with physiotherapy and was discharged home several days later. On review in the clinic about 6 months later, he still complained of mild pain to his back and right leg. However, he had returned to work and has been having ongoing physiotherapy in the community. An MRI was arranged and the results were satisfactory (See Fig. 3). He was referred back to the physiotherapist to continue his recovery.
Fig. 3.
MRI showing embolisation coils in situ, good alignment of screws and no haematoma.
3. Discussion
Cadaveric studies have shown that the first four lumbar arteries originate directly from the aorta, while the fifth lumbar artery can branch from the iliolumbar artery or the median sacral artery. The lumbar artery continues between two vertebral bodies in the intervertebral neural foramen. It then divides into four branches; ganglionic, transverse, ascending, and descending. The last three branches extend their feeding branches to the transverse process, the facet joint, and paraspinal muscles. The close anatomic relationship between the spine and this artery may place it at risk of injury during spinal surgery [6].
Segmental artery injury during posterior spinal surgery has been described several times in literature, including during pedicle screw insertion [2], [3], [4]. To our knowledge, they have all led to acute intra-operative bleeding, some of which have been extremely difficult to control and led to haemodynamic collapse. In our case, there was no overt bleeding at the time of surgery and the patient remained haemodynamically stable throughout.
We suspect that the segmental vessel was injured during screw misplacement, causing a false aneurysm secondary to intimal dissection. This would explain the initial intermittent radiculopathy. The aneurysm went on to spontaneously rupture some seven days after surgery and the patient returned with pain secondary to a haematoma in the right psoas muscle. This theory would also explain the drop in haemoglobin on secondary admission.
Endovascular embolisation of the segmental artery has been described and advocated by several authors and has been used effectively to control the haemodynamic status of patients [2], [7], [8], [9], [10]. For this patient, embolisation of the bleeding vessel served in improving the radiculopathy secondary to the psoas haematoma compressing the lumbar plexus.
Psoas haematoma is a rare but well described complication of anti-coagulation and haemorrhagic disorders, abdominal trauma and angiography [11], [12] To our knowledge, psoas haematoma following posterior spinal surgery leading to lumbar plexus compression has been described twice before. Sarwat et al. describe a case where the patient underwent dynamic lumbar stabilisation but three days post-operatively the patient developed radiculopathy. A CT was performed and this confirmed a haematoma that was subsequently drained percutaneously [13].
In the second similar case, Lakkol et al. describe a patient who returned with recurrence of radiculopathy four days after posterior lumbar fusion [14]. They opted to manage the patient conservatively with observation and analgesia to good effect.
Given that our patient had a CT angiogram confirming active bleeding accompanied with worsening pain and radiculopathy, we decided on endovascular embolisation. We opted not to surgically drain the haematoma itself as the patient's clinical picture improved over a few days both in terms of pain and motor power.
4. Conclusion
Psoas haematoma developing from lumbar artery injury should be considered as one of the differential diagnosis in patients with recurrent postoperative radiculopathy, particularly if intra-operatively there has been some difficulty cannulating the pedicles or a screw is misplaced. The clinical course of the patient could have been a lot worse and even fatal if he had not been able to remain haemodynamically stable. This shows the importance of urgent investigation in patients to detect an arterial bleed. In this case, the arterial bleed was detected on the sixth post-operative day and he was consequently treated. Although surgical drainage of the haematoma is not mandatory, an actively bleeding vessel can be successfully treated by endovascular embolisation.
Consent of patient
The consent of the patient has been obtained.
SCARE criteria
This case has been reported in line with the SCARE Criteria [15].
Ethical approval
Ethical approval not required.
Sources of funding
No source of funding.
Conflicts of interest
No conflicts if interest.
Contributor Information
R. Daureeawoo, Email: rd9922@my.bristol.ac.uk.
S. Baliga, Email: santoshbaliga@doctors.org.uk.
W. Mohahmed, Email: Wafaa.mohahmed@uhns.nhs.uk.
E.B. Ahmed, Email: Elnasri.ahmed@uhns.nhs.uk.
References
- 1.Fortina M., Carta S., Del Vecchio E.O., Crainz E., Urgelli S., Ferrata P. Retroperitoneal hematoma due to spontaneous lumbar artery rupture durino fondaparinux treatment. Case report and review of the literature. Acta Biomed. 2007;78(1):46–50. [PubMed] [Google Scholar]
- 2.Sandri A., Regis D., Marino M.A., Puppini G., Bartolozzi P. Lumbar artery injury following posterior spinal instrumentation for scoliosis. Orthopedics. 2011 Apr 11;34(4) doi: 10.3928/01477447-20110228-24. [DOI] [PubMed] [Google Scholar]
- 3.Karaikovic E.E., Rattner Z., Bilimoria M.M. Coil embolization of a lumbar artery to control vascular injury during intradiscal surgery. Spine (Phila Pa 1976) 2010;35(5):E163–E166. doi: 10.1097/BRS.0b013e3181bdc2f7. [DOI] [PubMed] [Google Scholar]
- 4.Sugimoto Y.1, Tanaka M., Gobara H., Misawa H., Kunisada T., Ozaki T. Management of lumbar artery injury related to pedicle screw insertion. Acta Med. Okayama. 2013;67(2):113. doi: 10.18926/AMO/49670. [DOI] [PubMed] [Google Scholar]
- 5.Medical Research Council . Her Majesty's Stationery Office; London: 1981. Aids to the Examination of the Peripheral Nervous System, Memorandum No. 45. [Google Scholar]
- 6.Caglar S., Dolgun H., Ugur H.C. Extraforaminal lumbar arterial anatomy. Surg. Neurol. 2004;61(1):29–33. doi: 10.1016/s0090-3019(03)00541-x. [DOI] [PubMed] [Google Scholar]
- 7.Chemelli A.P., Thauerer M., Wiedermann F. Transcatheter arterial embolization for the management of iatrogenic and blunt traumatic intercostal artery injuries. J. Vasc. Surg. 2009 Jun;49(6):1505–1513. doi: 10.1016/j.jvs.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 8.Nemoto C., Ikegami Y., Suzuki T. Repeated embolization of intercostal arteries after blunt chest injury. Gen. Thorac. Cardiovasc Surg. 2014 Nov;62(11):696–699. doi: 10.1007/s11748-013-0269-6. Epub 2013 Jun 1. [DOI] [PubMed] [Google Scholar]
- 9.Janík V., Martínek V., Pádr R. Embolization of lumbar artery due to retroperitonal bleeding following renal biopsy. Nephrol. Dial. Transpl. 2005;20(4):820–822. doi: 10.1093/ndt/gfh685. [DOI] [PubMed] [Google Scholar]
- 10.Tisnado1 J., Amendola M.A., Amendola C. Lumbar artery embolization: a rarely performed but lifesaving procedure. Eur. Soc. Radiol. ECR. 2012 Poster No C-001. [Google Scholar]
- 11.Fernandez-Palazzi F., Hernandez S.R., De Bosch N.B., De Saez A.R. Hematomas within the iliopsoas muscles in hemophilic patients: the Latin American experience. Clin. Orthop. 1996;328:19–24. doi: 10.1097/00003086-199607000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Akata T., Nakayama T., Kandabashi T., Kodama K., Takahashi S. Massive retroperitoneal hemorrhage associated with femoral vein cannulation. J. Clin. Anesth. 1998;10(4):321–326. doi: 10.1016/s0952-8180(98)00036-1. [DOI] [PubMed] [Google Scholar]
- 13.Sarwat A.M., Sutcliffe J.C. Haematoma of the psoas muscle after posterior spinal instrumentation and Enoxaparin prophylaxis. Grand. Rounds. 2003;3:35–37. [Google Scholar]
- 14.Lakkol S., Sarda P., Karpe P., Krishna M. Conservative management of psoas haematoma following complex lumbar surgery. Indian J. Orthop. 2014;48(1):107–110. doi: 10.4103/0019-5413.125534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., for the SCARE Group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]