Abstract
This study aimed to provide physiologic health risk parameters by gender and age among college students enrolled in a U.S. Midwestern University to promote chronic disease prevention and ameliorate health. A total of 2615 college students between 18 and 25 years old were recruited annually using a series of cross-sectional designs during the spring semester over an 8-year period. Physiologic parameters measured included body mass index (BMI), percentage body fat (%BF), blood serum cholesterol (BSC), and systolic (SBP) and diastolic (DBP) blood pressure. These measures were compared to data from NHANES to identify differences in physiologic parameters among 18–25 year olds in the general versus college-enrolled population. A quantitative instrument assessed health behaviors related to physical activity, diet, and licit drug use. Results suggest that average physiologic parameters from 18 to 25 year olds enrolled in college were significantly different from parameters of 18–25 year olds in the general population. Generally, men reported higher percentiles for BMI, SBP, and DBP than women, but lower %BF and BSC percentiles than women at each age. SBP and DBP significantly increased with age and alcohol use. Students in the lowest (5th) and highest percentiles (95th and 75th), for most age groups, demonstrated DBP, BMI, and %BF levels potentially problematic for health and future development of chronic disease based on percentiles generated for their peer group. Newly identified physiologic parameters may be useful to practitioners serving college students 18–25 years old from similar institutions in determining whether behavior change or treatment interventions are appropriate.
Keywords: Physiologic health risk parameters, College students, Health behaviors, Chronic disease, Health promotion
1. Introduction
Developing physiological health risk parameters (here after referred to as physiologic parameters) is a scientific approach concerned with establishing typical or desirable values for behavior, education, health, or other cultural or societal aspects (VandenBos, 2007). Cut-off scores for screening characterize what is desirable or unusual in a defined population at a specific point in time (O'Connor, 1990, Porta, 2008, Vogt, 1999). Desirable scores are often part of an initial screening process and consultation with a healthcare provider to ultimately decide on more definitive and expensive testing and whether behavioral changes and/or medical treatment are indicated (Black and Johnson, 2015, Frauenknecht and Black, 2003, Porta, 2008). Examining patient health and behavioral parameters at the earliest stage of development may increase longevity by reducing mortality, morbidity, injury, and disability, and may reduce the gross national product for healthcare costs by introducing preventive interventions earlier in life (Black and Johnson, 2015).
Physiologic age- and gender-specific health parameters have been identified and examined in adults for several decades, especially regarding the development of chronic diseases such as cardiovascular, diabetes, cholesterol, and hypertension (Gilbert and Nijland, 2008, Rodgers et al., 2006). While primarily physiologic in nature, health outcomes are due to a myriad of complex factors, such as health-related behaviors, which vary by age and gender (Krieger, 2003, O'Loughlin et al., 2011). Standards based on age and gender distributions have been reported as the most reliable and valid because of being less susceptible to measurement error and bias (Black and Johnson, 2015, Porta, 2008, Tombaugh, 2004). Developing physiologic parameters for a specific homogenous segment of a population would enhance the sensitivity, specificity, and accuracy of screening measures for that population segment (Black and Johnson, 2015).
Adolescents and young adults may not necessarily have the healthiest physiologic parameters (Belsky et al., 2015, Helms et al., 2014). For example, according to the Framingham Heart Study, adolescents and young adults with reportedly average or healthy physiologic parameters demonstrated physical evidence of atherosclerosis upon premature mortality, as confirmed by autopsies (Mahmood et al., 2014). Investigators from the Pathobiological Determinants of Atherosclerosis in Youth (McMahan et al., 2006) study suggested that identifying physiologic parameter risk factors at a younger rather than an older age is a better predictor of potential chronic disease development and severity when comorbidities are present.
College students are susceptible to chronic diseases because they engage in deleterious health behaviors, such as physical inactivity and binge drinking, that deviate from those in the general adult population (Carter et al., 2010, Lenk et al., 2012, Nelson et al., 2007, Quinn and Fromme, 2011). College students are at risk for higher rates of chronic diseases, including high blood serum cholesterol, increased blood pressure, and greater body mass index (BMI) (Sparling et al., 1999, Spencer, 2002). Currently, there are no screening criteria or national surveillance data health parameters that distinguish 18–25 years olds in the general population from 18 to 25 year olds enrolled in colleges or universities. Approximately 20.4 million in 2013 or 40% of all 18–25 year olds were enrolled in an institute of higher education (National Center for Education Statistics, 2013), and this age group's representation is expected to increase in the next decade as education becomes more affordable (National Center for Education Statistics, 2016). Therefore, it is imperative for the health and economic well-being of the nation to develop health risk parameters specifically for college students that are linked to deleterious health behaviors (Henke et al., 2010, Ormond et al., 2011).
National datasets, such as the National Health and Nutrition Examination Survey (NHANES) (National Center for Health Statistics, 2017), exist to capture the physiologic, physical, and emotional health parameters of the general adult population in the US across the lifespan. These large-scale datasets include adults between the ages of 18–25 years old who have “none” or “some” college experience or are identified as having a college degree. The use of these national large-scale datasets could shed light on the physiologic parameters of 18–25 year olds with limited college experience; however, simply reporting “some college” experience does not ensure current part- or full-time enrollment at a university. In fact, some college could indicate the completion of only one semester prior to withdrawal. Through the implementation and widespread use of the American College Health Association's National College Health Assessment (ACHA/NCHA) (American College Health Association, 2014), the US has recognized the importance of assessing the physical and emotional health status and needs of students enrolled in institutions of higher education; a population consisting of diverse groups with unique health risks and needs. Currently, there is a gap in the literature examining the physiologic parameters of 18–25 year olds who identify as enrolled in an institute of higher education, and not simply receiving some college education.
This study aims to: 1) “fill the gap” by examining physiologic parameters (i.e., BMI, percentage body fat, blood serum cholesterol, systolic blood pressure, and diastolic blood pressure) among a sample of 18–25 year olds enrolled in a university; 2) segment physiologic parameters by age and gender; and 3) examine the association of “unhealthy” behavioral health practices of physical inactivity, poor diet, and overuse/abuse of licit drug use with physiologic parameters.
2. Methods
2.1. Participants
Participants were a convenience sample of 2615 college students enrolled part- or full-time in a large U.S. Midwestern University. Among the sample of 17–40 year olds, 95% were between 18 and 25 years old (M = 20.4; Mdn = 20) and 51% identified as female. Participants were Caucasian (79.3%), Black (8.3%), and “other” (12.4%).
2.2. Procedures
The study design is an observational cross-sectional design in which data were collected during spring semesters over 8 consecutive years, which made it possible to evaluate reliability of data (Black and Johnson, 2015). Additionally, the study design selection was institutionally restricted to accommodate university pedagogical training demands. Participants were recruited through posters and flyers displayed across campus. Institutional Review Board (IRB) approval was obtained before data collection.
2.3. Measures for Physiologic Parameters
2.3.1. Body mass index (BMI)
BMI for each participant was calculated by body weight (lb) and height (in.) (Centers for Disease Control and Prevention, 2015a). A Detecto Mechanical Physician's Eye Level Scale (Model #339) was used to measure weight; height was measured with the scale's metric ruler.
2.3.2. Percentage body fat (%BF)
A 3-site skinfold thicknesses assessed with Lange Skinfold Calipers (patent# 3,008,239) were used to determine %BF. Based on gender, 3-sites were measured 3 times and averaged. The chest, abdomen, and thigh were measured for males (Jackson and Pollock, 1978), and the triceps, thigh, and suprailium were measured for females (Jackson et al., 1980). The Siri formulas (Siri, 1956) were used to estimate %BF (see formulas at the bottom of Table 2).
Table 2.
Regression analyses predicting physiologic chronic disease indicators.
| Healthy behaviors | BMI | %BF | Cholesterol | Systolic BP | Diastolic BP |
|---|---|---|---|---|---|
| Exercise | − 0.17⁎(0.07) | 0.28⁎⁎ (0.11) | 0.38⁎ (0.15) | − 0.08 (0.28) | 0.16 (0.20) |
| Healthy diet | − 0.33 (0.24) | 0.08 (0.30) | − 0.22 (0.43) | 0.91 (0.75) | 0.30 (0.55) |
| Alcohol use | 0.09 (0.06) | 0.13 (0.08) | 0.06 (0.12) | 0.42⁎ (0.21) | 0.36⁎ (0.15) |
| Tobacco use | 0.12 (0.15) | − 0.13 (0.22) | − 0.31 (0.30) | − 0.35 (0.57) | 0.10 (0.41) |
| Age | 0.05 (0.07) | 0.23 (0.22) | 0.02 (0.13) | 0.48⁎ (0.23) | 0.38⁎ (0.17) |
| Sex | 1.04⁎⁎⁎ (0.24) | − 13.34⁎⁎⁎ (0.34) | − 12.77⁎⁎⁎ (0.48) | 12.11⁎⁎⁎ (0.86) | 3.80⁎⁎⁎ (0.62) |
Note: Standard errors are in parentheses. Sex coded 0 for female, 1 for male. BMI = weight (lb) / [height (in)] (O'Connor, 1990) * 703 (National Center for Health Statistics, 2017).%BF = %BF for males using the Siri formulas (Jackson and Pollock, 1978) (%BF = 1.10938 − 0.0008267 * tf + 0.0000016 * tf * tf − 0.0002574 * age) and %BF for females (%BF = 1.0994921 − 0.0009929 * tf + 0.0000023 * tf * tf − 0.0001392 * age), where tf is the average across the 3 sites of the skinfold thickness measures of the chest, abdomen, and thigh for males (American College Health Association, 2014), and the triceps, thigh, and suprailium for females (Centers for Disease Control and Prevention, 2015a).
p < 0.05.
p < 0.01.
p < 0.001.
2.3.3. Blood serum cholesterol (BSC)
BSC was assessed using the finger-stick method with a Kodak DT 60, from Ortho-Clinical Diagnostics and the Boehringer Mannheim Corporation ProAct System from Roche Diagnostics. Participants self-reported whether they fasted or not before the assessment and were asked to reschedule if they had not fasted. Cronbach alpha across independent screeners was α = 0.91.
2.3.4. Systolic and diastolic blood pressure
Systolic and diastolic blood pressure (SBP and DBP, respectively) readings were assessed with a sphygmomanometer and stethoscope by following American Heart Association's recommended Korotkoff's sound technique (Pickering et al., 2005). Two evaluators used a training stethoscope, and each independently recorded readings. Training, based on criterion-referenced testing (VandenBos, 2007), continued until both the faculty member and each undergraduate student agreed 100% of the time. Internal consistency of the 3 measurements of BP was sufficient across the sample (Cronbach α = 0.95).
2.4. 2.4. Behavioral measures
Thirty-two items assessing dietary and exercise habits and licit drug use were adapted from national data collection instruments (Centers for Disease Control and Prevention (CDC) and National Center for Health Statistics (NCHS), n.d.). Item stems and response options were used from the surveys to preserve the integrity of the original items. The items were separated into 5 categories: 1) age in years; 2) gender; 3) dietary habits (i.e., daily average number of servings of soft drinks, sweets, fatty meats, fast food, fish, poultry, legumes, fruits, vegetables); 4) exercise habits (i.e., type of exercise, minutes per session of exercise, and exercise sessions per week); and 5) licit drug use (i.e., tobacco use, including cigarettes, snuff, and chew and alcohol use, and drinks per day and days per week of drinking alcohol). Each item used in a behavioral health scale was scored from 1 (best for health) to 5 (worst for health) and the items comprising each scale were then averaged to produce the scale score.
2.5. 2.5. Statistical analyses
All data were analyzed using SAS Version 9.3.1 (SAS Institute, n.d.). Analyses performed were descriptive statistics, linear regression analyses, and analysis of variance. Descriptive statistics, including means, percentiles, and graphical summaries, were computed for physiologic parameters, health behaviors, and demographic variables. Percentiles reported identify both “typical” and “extreme” levels for each physiologic parameter, and provide the opportunity to observe trends over age for each gender. Linear regression analyses were used to predict potential physiologic parameters based on healthy behavior scales and demographic variables. Analyses of variance were computed to examine reliability and external validity.
3. Results
3.1. Physiologic parameters
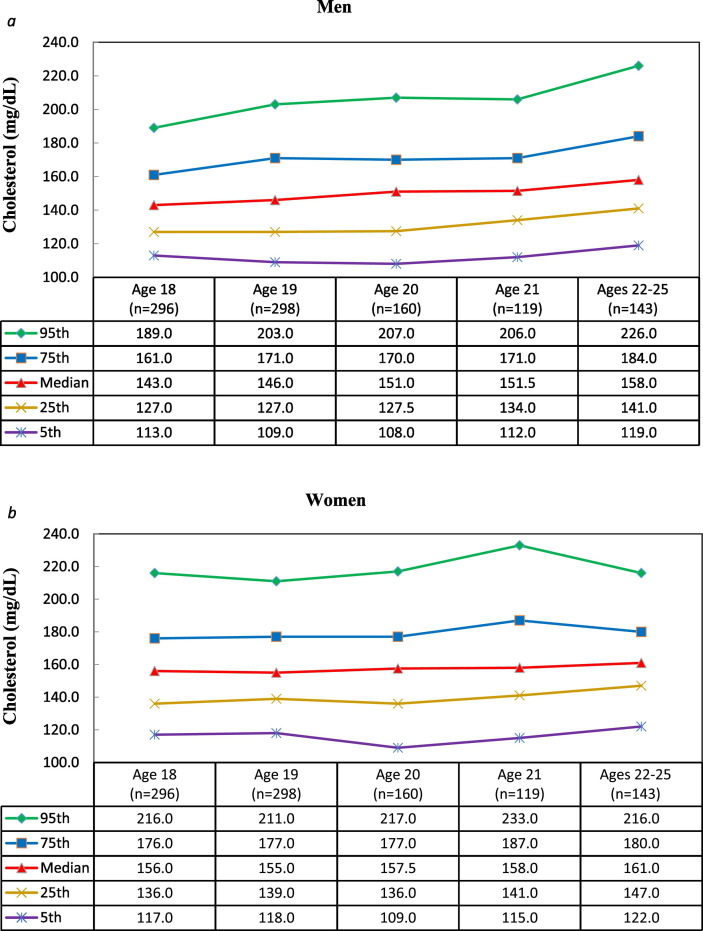
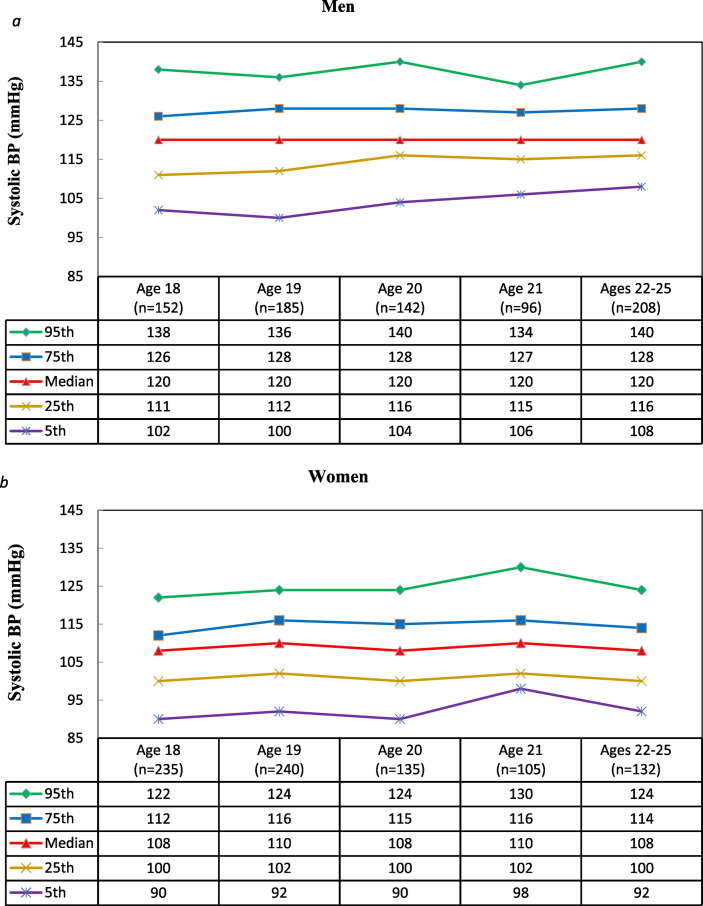
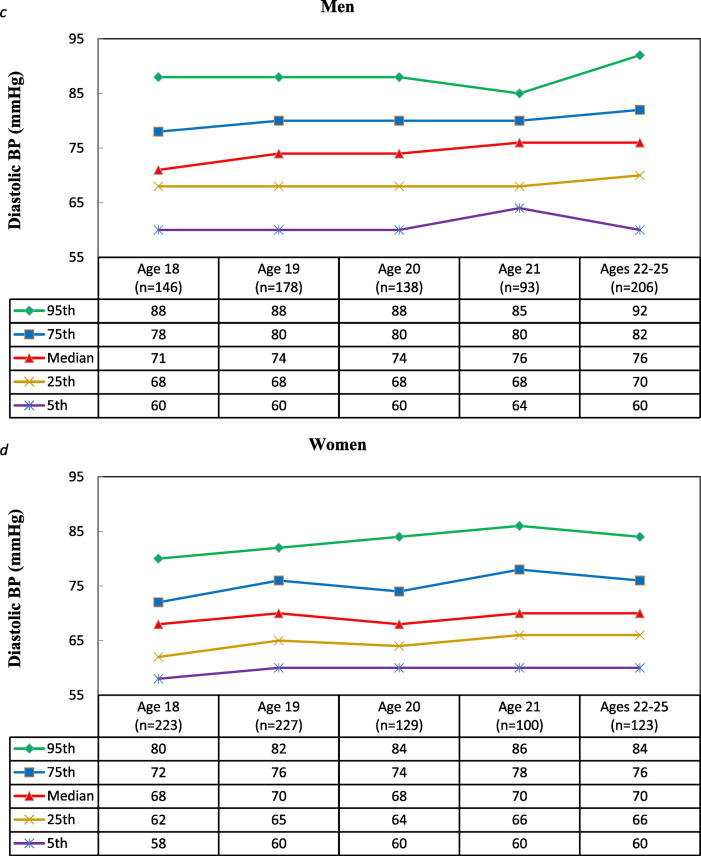
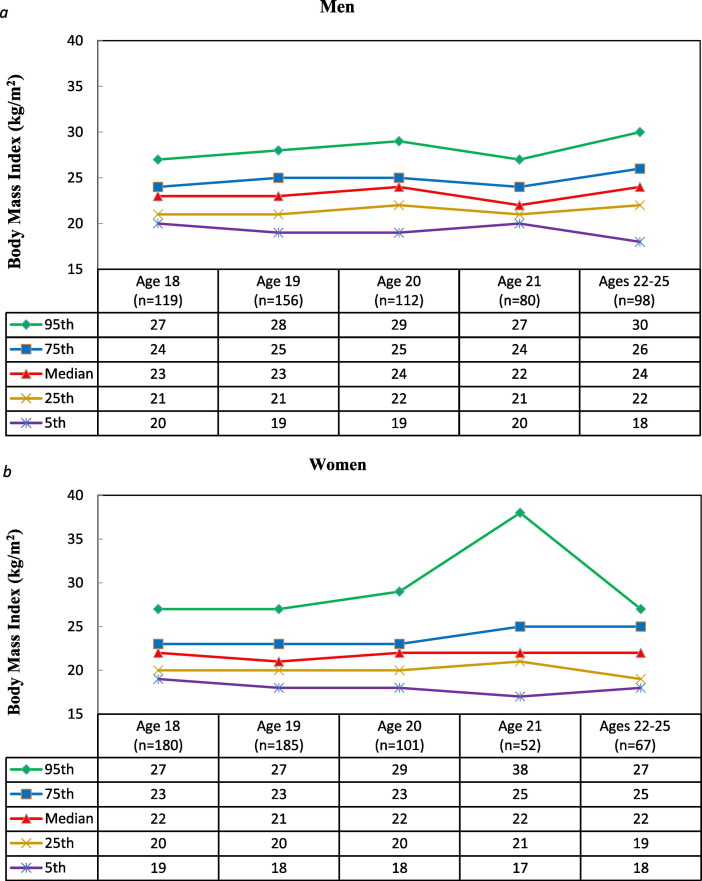
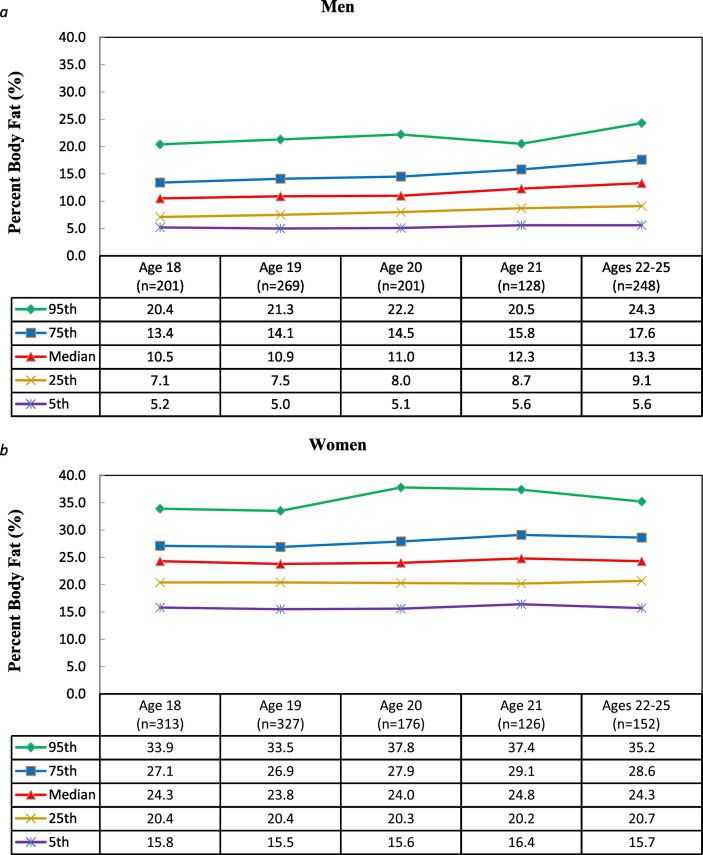
Summary descriptive data by gender and age are presented in Fig. 1, Fig. 2, Fig. 3, Fig. 4, with accompanying percentile tables for BSC (Fig. 1a and b), SBP and DBP (Figs. 2a–2d), BMI (Figs. 3a–3b), and %BF (Figs. 4a–4b), respectively. M values for each chronic disease indicator are as follows: 1) BSC (mg/dL), M = 157, SD = 31.4; 2) SBP levels (mmHg), M = 114, SD = 12.1; 3) DBP levels (mmHg), M = 72, SD = 8.2; 4) %BF, M = 18.4, SD = 8.3; and 5) BMI (kg/m2), M = 22.6, SD = 3.1.
Fig. 1.
Selected Percentiles for Cholesterol by Gender and Age.
Fig. 2.
Selected Percentiles for Systolic BP by Gender and Age.
Fig. 3.
Selected Percentiles for BMI by Gender and Age.
Fig. 4.
Selected Percentiles for percent Body Fat by Gender and Age.
Using linear regression analyses, the average BSC increased by an average of 3.65 (mg/dL) per year of age for men (P ≤ 0.001) and by an average 1.29 (mg/dL) per year of age for women (P = 0.04). Rates of M increase per year also differed significantly between men and women (P ≤ 0.01).
Average DBP increased by an average of 0.73 (mmHG) per year of age for men (P < 0.001) and 0.49 (mmHG) per year of age for women (P < 0.01). The average increase per year did not differ significantly between men and women (P = 0.32).
Average SBP increased by 0.55 (mmHG) per year for men and by an 0.11 (mmHG) per year for women, with a significant rate of increase for men (P = 0.0088), but not for women (P = 0.6635). However, the average increase/year did not differ significantly between men and women, P = 0.1517.
The BMI average increased by 0.15 (kgm− 2) per year for men and by 0.09 (kgm− 2) per year for women, both non-significant rates of increase, P = 0.0573 for men and P = 0.3013 for women. This average increase/year, however, did not differ significantly between men and women, P = 0.5769.
The average %BF increased by 0.58%/year for men and by 0.22%/year for women, both significant rates of increase, P < 0.0001 for men and P = 0.0446 for women. Like DBP and BMI, the average increase/year did differ significantly between men and women (P = 0.0144).
3.2. Deleterious health behaviors
Table 1 provides the summary statistics and percentiles for each health behavior.
Table 1.
Summary statistics for health behaviors for the total sample of 18–25-year-old college students.
| Health behaviors | Percentile |
|||||||
|---|---|---|---|---|---|---|---|---|
| N | M | SD | 5th | 25th | 50th | 75th | 95th | |
| Healthy diet | 1888 | 2.85 | 0.45 | 2.09 | 2.55 | 2.82 | 3.18 | 3.54 |
| Exercise | 1751 | 3.66 | 0.71 | 2.33 | 3.22 | 3.67 | 4.11 | 4.56 |
| Alcohol | 1903 | 2.02 | 1.14 | 1.00 | 1.00 | 1.57 | 3.29 | 3.86 |
| Tobacco | 2227 | 1.16 | 0.49 | 1.00 | 1.00 | 1.00 | 1.00 | 2.33 |
Note: Each of “Healthy Diet,” “Exercise,” “Alcohol” and “Tobacco” was scaled from 1 (best) to 5 (worst) for health.
Dietary behaviors, a M of 2.85 (SD = 0.45) and Mdn of 2.82 can be interpreted as approaching an unhealthy diet, with 10% reporting an unhealthy diet (i.e., 90th percentile above 3.5 on the 1–5 scale used).
Exercise frequency, a M of 3.66 (SD = 0.71) and Mdn of 3.67 can be interpreted as physically inactive with more than 25% exercising once/week or less, while less than 0.31% of respondents engaged in 7 or more exercise sessions/week.
Average alcohol consumption of 2.02 (SD = 1.14) and Mdn of 1.57 can be interpreted overall as mild–moderate use. Of 1903 subjects responding to both alcohol items, 49.30% did not drink any alcohol and of those who did drink, 59.54% consumed on average 1 drink/day. Slightly less than 10% consumed 5 or more drinks/day.
Of the 2227 subjects responding to both tobacco use items, 11.03% smoked cigarettes and 2.80% used snuff or chew.
3.3. Segmentation of physiologic parameters by age and gender
Table 2 shows, after adjusting for all other effects in the fitted models, men had a significantly higher (M.) BMI, SBP, and DBP than women and a significantly lower %BF and cholesterol. Age was significantly and positively associated with increasing SBP and DSP.
3.4. Relationship of health behaviors with physiologic parameters
Table 2 provides results for predicting physiologic parameters based on health behaviors. Multiple linear regression analyses indicated that higher exercise scale scores, which corresponds to less exercise, was significantly associated with higher %BF (P = 0.008). The same was true for cholesterol (P = 0.038). Both blood pressure responses were significantly and positively associated with the alcohol usage scale (P = 0.031 and 0.023, respectively) indicating that average SBP and DBP increased with increasing quantity and/or frequency of alcohol consumption.
3.5. Reliability and external validity evidence
The following results demonstrate acceptable consistency from year-to-year based on the demographic variables of the study sample. First, the overall age for the study sample was M = 19.92 with SD = 1.77 years. The M age did not differ across study years. Second, overall 48.5% of participants were women, and the percentage of women did not differ significantly across study years. Third, race was dichotomized as Caucasian versus non-Caucasian. There was no difference in race (P = 0.2609) across study years, with 81.1% of study participants being Caucasian. These comparisons indicate that there is consistency from year-to-year.
Comparisons were made with the general population of 18–25 year olds on campus and nationally. Data from the University registrar's office showed that participants were representative of all 18–25 year olds on campus (M P level = 3276, SD = 0.46). To further assess generalizability and the uniqueness of this sub-population with 18–25 years old in the general U.S. population, comparisons were made with data from NHANES studies from years 1999–2010 that included 4812 adults 18–25 years old, but again did not attend or only attended some college (National Center for Health Statistics, 2017). The NHANES data includes estimates of physiologic parameters, except %BF.
Table 3 provides Ms. and SDs for each health parameter, by age and gender (with those 22–25 in one category to make comparisons possible), for the college students in this study and for the NHANES participants. For each age and gender, M cholesterol and BMI was significantly lower for college students than NHANES participants, with P values < 0.001 in almost all age and gender combinations. M diastolic BP was significantly higher for the college students than NHANES participants, P < 0.001 for all comparisons. SBP was higher for male college students versus NHANES participants, but not for college women. College students may be less at risk in regards to cholesterol and BMI, but at higher risk in regards to blood pressures.
Table 3.
Physiologic parameter comparisons between college-attending study participants and the general population represented by NHANES participants.
| Health Parameter |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Gender | Age | Cholesterol |
Diastolic BP |
Systolic BP |
BMI |
||||
| Students | NHANES | Students | NHANES | Students | NHANES | Students | NHANES | ||
| Men | 18 | 146 | 162⁎⁎⁎ | 72.5 | 63.1⁎⁎⁎ | 119 | 115⁎⁎⁎ | 22.8 | 25.1⁎⁎⁎ |
| 182, 24.0 | 599, 31.2 | 146, 8.3 | 599, 11.2 | 152, 10.3 | 599, 10.7 | 119, 2.7 | 599, 5.9 | ||
| 19 | 151 | 166⁎⁎⁎ | 73.2 | 64.0⁎⁎⁎ | 119 | 117⁎ | 23.1 | 25.2⁎⁎⁎ | |
| 234, 30.0 | 603, 34.6 | 178, 8.1 | 603, 11.7 | 185, 11.4 | 603, 10.1 | 156, 2.6 | 603, 5.7 | ||
| 20 | 153 | 168⁎⁎⁎ | 74.0 | 64.9⁎⁎⁎ | 122 | 116⁎⁎⁎ | 23.6 | 25.3⁎⁎ | |
| 168, 31.5 | 222, 33.0 | 138, 7.9 | 222, 11.6 | 142, 10.5 | 222, 10.7 | 112, 2.9 | 222, 5.3 | ||
| 21 | 155 | 170⁎⁎⁎ | 74.4 | 65.5⁎⁎⁎ | 120 | 118⁎ | 22.8 | 25.7⁎⁎⁎ | |
| 114, 29.1 | 242, 32.9 | 93, 7.1 | 242, 11.6 | 96, 8.8 | 242, 10.2 | 80, 2.4 | 242, 5.9 | ||
| 22–25 | 163 | 177⁎⁎⁎ | 75.9 | 67.0⁎⁎⁎ | 122 | 118⁎⁎⁎ | 23.7 | 26.4⁎⁎⁎ | |
| 221, 32.6 | 616, 38.3 | 206, 9.5 | 616, 11.5 | 208, 11.4 | 616, 10.3 | 98, 3.2 | 616, 5.7 | ||
| Women | 18 | 159 | 170⁎⁎⁎ | 68.6 | 62.9⁎⁎⁎ | 107 | 108 | 22.0 | 25.8 |
| 296, 30.7 | 607, 34.5 | 223, 7.1 | 607, 10.6 | 235, 9.7 | 607, 9.6 | 180, 2.7 | 607, 6.5 | ||
| 19 | 159 | 172⁎⁎⁎ | 70.8 | 63.1⁎⁎⁎ | 109 | 109 | 21.8 | 25.9⁎⁎⁎ | |
| 298, 31.4 | 544, 35.0 | 227, 7.2 | 544, 9.9 | 240, 10.3 | 544, 9.6 | 185, 2.9 | 544, 6.3 | ||
| 20 | 159 | 180⁎⁎⁎ | 69.8 | 63.0⁎⁎⁎ | 108 | 108 | 21.9 | 26.4 | |
| 160, 33.4 | 268, 40.1 | 129, 7.8 | 268, 10.1 | 135, 10.4 | 268, 9.9 | 101, 3.4 | 268, 7.0 | ||
| 21 | 166 | 180⁎⁎⁎ | 71.6 | 62.9⁎⁎⁎ | 111 | 109 | 23.6 | 26.3⁎⁎ | |
| 119, 38.3 | 271, 40.1 | 100, 7.9 | 271, 9.7 | 105, 10.3 | 271, 9.4 | 52, 5.2 | 271, 7.0 | ||
| 22–25 | 164 | 187⁎⁎⁎ | 71.2 | 62.9⁎⁎⁎ | 108 | 109 | 22.0 | 27.9⁎⁎⁎ | |
| 143, 27.9 | 840, 43.4 | 123, 7.1 | 840, 10.6 | 132, 9.7 | 840, 9.9 | 67, 3.3 | 840, 7.4 | ||
Note: First row of each cell presents the mean; second row presents the n size.
p < 0.05.
p < 0.01.
p < 0.001.
Complete datasets from the NCHA/ACHA (American College Health Association, 2014) are not publicly accessible; therefore, data from college students in the Monitoring the Future Study (Monitoring the Future, 2017), an initiative from the University of Michigan, were used to provide evidence of external validity for behavioral correlates. For respondents 19–30 years old, this study had 11.3% with a daily use of cigarettes versus 11.2% from the Monitoring the Future Study, and these percentages did not differ significantly (z = 0.11, P = 0.9088). Similarly, this study had 2.8% using smokeless tobacco (chew, snuff) versus a Monitoring the Future Study value of 2.5% and these values did not differ significantly, z = 0.86, P = 0.3900. There is similarity with the rates for daily use of alcohol, 5.4% for the Monitoring the Future Study and 5.1% for this study (z = 0.53, P = 0.5990). Based on all these comparisons, external validity seems satisfactory.
4. Discussion
This study establishes specific physiologic parameters within a college student population, and provides initial data for peer-to-peer comparisons for chronic disease risk reduction and health promotion. Findings suggest that 18–25 year olds enrolled in college have more favorable physiologic risk health parameters in some instances than 18–25 year olds in the general population, who are comprised of adults who have never attended or attended some college or may have discontinued college (National Center for Health Statistics, 2017). However, among adults enrolled in college scoring in higher percentiles, physiologic parameters were significantly associated with deleterious health behaviors that increase the risk of potential future chronic diseases. Among universities with similar demographic characteristics as the study sample, the proposed parameter scores, segmented by gender and age, are preferred and should be considered in place of those developed for the general U.S. adult population across the life span.
Increasing age was significantly associated with increasing diastolic and systolic blood pressure levels, where a peak in diastolic and systolic blood pressure was seen at age 21 for women, while a decrease was noted for men at age 21. This result needs further investigation because the present findings offer no plausible explanation and none was found in the extant literature. Regarding body mass index, women's levels remained stable with a rising exception at age 21, and the status for men steadily increased with a lowering exception at age 21. Although mean body mass index did not significantly vary by age, percentage body fat did. This trend of poor physiologic parameters with increasing age provides further justification for prevention efforts and intervening earlier.
A significant relationship existed between health behaviors and physiologic parameters. A greater number of exercise sessions per week were significantly predictive of a lower BMI levels, lower percentage body fat, and a lower cholesterol level. This is consistent with reports that exercise has a positive impact on chronic disease indicators (Durstine et al., 2013). Although physical activity recommendations are in place to provide guidelines for adequate weekly sessions and time requirements (Centers for Disease Control and Prevention, 2015b), results suggest that even one exercise session each week has a positive impact on percentage body fat (Jamurtas et al., 2004). Additionally, along with age, a higher number of daily alcohol servings per week was significantly associated with higher systolic and diastolic blood pressure. These findings also are consistent with reports suggesting that regular alcohol consumption is predictive of increased systolic and diastolic blood pressure levels (Puddey and Beilin, 2006) and that blood pressure increases with age (Landahl et al., 1986).
4.1. Practical implications
Acknowledging that data from a cross-sectional study versus other study designs may have less clinical value (Black and Johnson, 2015), the results may still have clinical utility, if the demographics of clients at another institution are like the study sample and the universities are comparable in academic standing. Age trends in this study over the 6-year age range show that, on average, men's BSC increased by about 22 mg/DL. Such an increase for an average male is concerning and if the trend continued beyond the college years would be alarming. The age-trend for those at or above the 95th percentile was even greater (see Fig. 1a). Similarly, average %BF for men increased by about 3.5% over the age range of this study and was similar for those at the 95th percentile (see Fig. 4a). This is suggestive of tertiary prevention for those scoring in the 95th percentile or above. Those at the 5th percentile may deserve medical attention too. Justification for those at the lowest extreme for medical and behavioral examinations and interventions includes well documented medical problems and accompanying behavioral issues related to low body weight and bodyfat (Brunet, 2005). The 75th percentile may offer opportunity to intervene earlier prior to future health repercussions and possibly when individuals may be more amenable to change because the amount required and the magnitude of change is less (Hardcastle et al., 2015). Those at the median should be encouraged to maintain their healthy lifestyle behaviors.
Research has suggested that personalized feedback interventions based on health parameters can lead to a so called “boomerang effect” to motivate behavior change or maintenance (Schultz et al., 2007) and fits within the long established intervention of John Snow (Black and Johnson, 2015) and Occam's Razor (parsimony) (Porta, 2008), which also is known as minimal intervention (Abood et al., 2002, Black and Cameron, 2002). This phenomenon occurs when, after personalized feedback is delivered (comparison of individual data to the health parameter percentiles), an individual's performance shifts closer to the established parameter, regardless of whether performance status was initially above or below the percentile (Rimal and Real, 2005). Personalized data among the college-age population based on standardized criteria has been effective for minimal interventions, such as decreasing binge drinking (Burger et al., 2011), gambling (Larimer and Neighbors, 2003), and increasing physical activity and healthy eating (Ball et al., 2010, Burger et al., 2010).
4.2. Limitations/future research
The method of measuring physiologic parameters may influence outcome. For example, people who are more muscular will have a higher body mass index because muscle weighs more than fat (Rothman, 2008). This may have accounted for some variations. Participants may have underestimated their caloric intake or exaggerated the amount of exercise based on response bias (Lichtman et al., 1992, Schuna et al., 2013). More precise, yet less convenient and more expensive, measurements of physiologic parameters exist and may provide data with less systematic error; however, by how much and to what degree is unknown. Cost versus benefit should be weighed and considered. Along with this priority for future research and due to a dearth of data, another priority would be to include questions in national secondary datasets to inquire about college-student enrollment and undergraduate participants represent all 4 years of college. Alternative research designs (i.e., experimental and observation) might be used to determine if outcomes differ or are comparable to study results.
5. Conclusion
Physiologic parameters for college students 18–25 years old are presented and may be useful to practitioners in similar institutions to the study sample in demographics and academic standing and for recommending health behavior changes and/or medical treatments. Health parameters for a specific subset of the population are preferred and should be considered in place of those parameters for the general population. Practitioners and college students alike should become conversant about health parameter standards for their age group and special circumstances. Awareness, provider feedback, brief instructions, and/or referral for additional screening and follow-up could increase the chances of earlier intervention as well as a boomerang effect, which could promote healthy behavior change with the ultimate objective to ameliorate longevity and decrease healthcare expenditures.
Funding statement
This research did not receive any specific grant funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
None.
Acknowledgments
The authors thank Yvonne Brooks and Donna Kachuk for transcribing raw data, and Bill Whitson for the alignment and verification behavioral assessment data that varied in order of variables across the 8 years of data collection. We are grateful to Judy K. and Jacquelyn K. Black, and Christopher Brooks for providing technical support.
References
- Abood D.A., Coster D.C., Mullis A.K., Black D.R. Evaluation of a “loss framed” minimal intervention to increase mammography utilization among medically un- and under-insured women. Cancer Detect. Prev. 2002;26(5):394–400. doi: 10.1016/s0361-090x(02)00120-4. [DOI] [PubMed] [Google Scholar]
- American College Health Association National College Health Assessment. 2014. http://www.acha-ncha.org/pubs_rpts.html Available at:
- Ball K., Jeffery R.W., Abbott G., McNaughton S.A., Crawford D. Is healthy behavior contagious: associations of social norms with physical activity and healthy eating. Int. J. Behav. Nutr. Phys. Act. 2010;7:86. doi: 10.1186/1479-5868-7-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belsky D.W., Caspi A., Houts R. Quantification of biological aging in young adults. PNAS. 2015;112(30):E4104–E4110. doi: 10.1073/pnas.1506264112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black D.R., Cameron R. Self-administered interventions: a health education strategy for improving population health. Health Ed. Res. 2002;26:394–400. doi: 10.1093/her/12.4.531. [DOI] [PubMed] [Google Scholar]
- Black D.R., Johnson M.A. second ed. Creative Solutions Press; West Lafayette, IN: 2015. Handbook for Principles of Epidemiology for Nursing Practice and Research. [Google Scholar]
- Brunet M. Female athlete triad. Clin. Sports Med. 2005;24(3):623–636. doi: 10.1016/j.csm.2005.03.009. [DOI] [PubMed] [Google Scholar]
- Burger J.M., Bell H., Harvey K. Nutritious or delicious? The effect of descriptive norm information on food choice. J. Soc. Clin. Psychol. 2010;29(2):228–242. [Google Scholar]
- Burger J.M., LaSalvia C.T., Hendricks L.A., Mehdipour T., Neudeck E.M. Partying before the party gets started: the effects of descriptive norms on pregaming behavior. Basic Appl. Soc. Psychol. 2011;33(3):220–227. [Google Scholar]
- Carter A.C., Obremski Brandon K., Goldman M.S. The college and noncollege experience: a review of the factors that influence drinking behavior in young adulthood. J. Stud. Alcohol Drugs. 2010;71(5):742–750. doi: 10.15288/jsad.2010.71.742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention About Adult BMI. 2015. https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html Available at: (Accessed July 21, 2016)
- Centers for Disease Control and Prevention. How Much Physical Activity Do Adults Need? 2015b. Available at: https://www.cdc.gov/physicalactivity/basics/adults/. (Accessed July 21), 2016.
- Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey Data. Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 1999–2010, http://www/cdc/gov/nchs/nhanes.
- Durstine J.L., Gordon B., Wang Z., Luo X. Chronic disease and the link to physical activity. J. Sport Health Sci. 2013;2(1):3–11. [Google Scholar]
- Frauenknecht M., Black D.R. Creative Solutions Press, LLC; Oshtemo, MI: 2003. The Social Problem-Solving Inventory for Adolescents (SPSI-A): A Manual for Application, Interpretation, and Psychometric Evaluation. [Google Scholar]
- Gilbert J.S., Nijland M.J. Sex differences in the developmental origins of hypertension and cardiorenal disease. Am. J. Phys. 2008;295(6):R1941–R1952. doi: 10.1152/ajpregu.90724.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardcastle S.J., Hancox J., Hattar A., Maxwell-Smith C., Thogersen-Ntoumani C., Hagger M.S. Motivating the unmotivated: how can health behavior be changed in those unwilling to change? Front. Psychol. 2015;6:835. doi: 10.3389/fpsyg.2015.00835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helms S.W., Choukas-Bradley S., Widan L., Giletta M., Cohen G.L., Prinstein M.J. Adolescents misperceive and are influenced by high-status peers' health risk, deviant, and adaptive behavior. Dev. Psychol. 2014;50(12):2697–2714. doi: 10.1037/a0038178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henke R.M., Carls G.S., Short M.E. The relationship between health risks and health and productivity costs among employees at Pepsi bottling group. J. Occup. Environ. Med. 2010;52(5):519–527. doi: 10.1097/JOM.0b013e3181dce655. [DOI] [PubMed] [Google Scholar]
- Jackson A.S., Pollock M.L. Generalized equations for predicting body density of men. Br. J. Nutr. 1978;40(3):497–504. doi: 10.1079/bjn19780152. [DOI] [PubMed] [Google Scholar]
- Jackson A.S., Pollock M.L., Ward A. Generalized equations for predicting body density of women. Med. Sci. Sports Exerc. 1980;12(3):175–181. [PubMed] [Google Scholar]
- Jamurtas A.Z., Koutesakis Y., Paschalis V. The effects of a single bout of exercise on resting energy expenditure and respiratory exchange ratio. Eur. J. Appl. Physiol. 2004;92(4–5):393–398. doi: 10.1007/s00421-004-1156-8. [DOI] [PubMed] [Google Scholar]
- Krieger N. Genders, sexes, and health: what are the connections – and why does it matter? Int. J. Epidemiol. 2003;32(4) doi: 10.1093/ije/dyg156. (652–657) [DOI] [PubMed] [Google Scholar]
- Landahl S., Bengtsson C., Sigurdsson J.A., Svanborg A., Svardsudd K. Age-related changes in blood pressure. Hypertension. 1986;8:1044–1049. doi: 10.1161/01.hyp.8.11.1044. [DOI] [PubMed] [Google Scholar]
- Larimer M.E., Neighbors C. Normative misperception and the impact of descriptive and injunctive norms on college student gambling. Psychol. Addict. Behav. 2003;17(3):235–243. doi: 10.1037/0893-164X.17.3.235. [DOI] [PubMed] [Google Scholar]
- Lenk K., Rode P., Fabian L., Bernat D., Klein E., Forster J. Cigarette use among young adults: comparison between two-year college students, four-year college students, and those not in college. J. Am. Coll. Heal. 2012;60(4):303–308. doi: 10.1080/07448481.2011.607481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichtman S.W., Pisarska K., Berman E.R. Discrepancy between self-reported and actual caloric intake and exercise in obese subjects. N. Engl. J. Med. 1992;327(27):1893–1898. doi: 10.1056/NEJM199212313272701. [DOI] [PubMed] [Google Scholar]
- Mahmood S.S., Levy D., Vasan R.S., Wang T.J. The Framingham heart study and the epidemiology of cardiovascular diseases: a historical perspective. Lancet. 2014;383(9921):999–1008. doi: 10.1016/S0140-6736(13)61752-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMahan C.A., Gidding S.S., Malcom G.T., Tracy R.E., Strong J.P., McGill H.C., Jr. Pathobiological determinants of atherosclerosis in youth research group. Pathobiological determinants of atherosclerosis in youth risk scores are associated with early and advanced atherosclerosis. Pediatrics. 2006;118(4):1447–1455. doi: 10.1542/peds.2006-0970. [DOI] [PubMed] [Google Scholar]
- Monitoring the Future A Continuing Study of American Youth. 2017. http://www.monitoringthefuture.org Available at:
- National Center for Education Statistics Percentage of 18- to 24-year-olds Enrolled in Degree-granting Institutions, by Level of Institution and Race/Ethnicity of Student: 1967–2012. 2013. https://nces.ed.gov/programs/digest/d13/tables/dt13_302.60.asp Available at:
- National Center for Education Statistics Undergraduate Enrollment. 2016. http://nces.ed.gov/programs/coe/indicator_cha.asp Available at:
- National Center for Health Statistics National health and nutrition examination survey. 2017. https://www.cdc.gov/nchs/nhanes/ Available at:
- Nelson T.F., Gortmaker S.L., Subramanian S.V., Wechsler H. Vigorous physical activity among college students in the United States. J. Phys. Act. Health. 2007;4(4):495–508. [PubMed] [Google Scholar]
- O'Connor P.J. Normative data: their definition, interpretation, and importance for primary care physicians. Fam. Med. 1990;22(4):307–311. [PubMed] [Google Scholar]
- O'Loughlin R.E., Duberstein P.R., Veazie P.J., Bell R.A., Rochlen A.B. Fernandez y Garcia E, Kravitz RL. Role of the gender-linked norm of toughness in the decision to engage in treatment for depression. Psychiatr. Serv. 2011;62(7):740–746. doi: 10.1176/appi.ps.62.7.740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ormond B.A., Spillman B.C., Waidmann T.A., Caswell K.J., Tereschchenko B. Potential national and state medical care savings from primary disease prevention. Am. J. Public Health. 2011;101(1):157–164. doi: 10.2105/AJPH.2009.182287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickering T.G., Hall J.E., Appel L.J. Recommendations for blood pressure measurement in humans and experimental animals. Hypertension. 2005;45:142–161. doi: 10.1161/01.HYP.0000150859.47929.8e. [DOI] [PubMed] [Google Scholar]
- Porta M. Oxford Press; New York, NY: 2008. A Dictionary of Epidemiology (5th Ed) [Google Scholar]
- Puddey I.B., Beilin L.J. Alcohol is bad for blood pressure. Clin. Exp. Pharmacol. Physiol. 2006;33(9):847–852. doi: 10.1111/j.1440-1681.2006.04452.x. [DOI] [PubMed] [Google Scholar]
- Quinn P., Fromme K. Alcohol use and related problems among college students and their non-college peers: the competing roles of personality and peer influence. J. Stud. Alcohol Drugs. 2011;72(4):622–632. doi: 10.15288/jsad.2011.72.622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rimal R.N., Real K. How behaviors are influenced by perceived norms: a test of the theory of normative social behavior. Commun. Res. 2005;32(3):389–414. [Google Scholar]
- Rodgers A., Lawes C.M.M., Gaziano T., Vos T. The growing burden of risk from high blood pressure, cholesterol, and bodyweight. In: Jamison D.T., Measham A.R., editors. Disease Control Priorities in Developing Countries. second ed. Oxford University Press; New York, NY: 2006. [Google Scholar]
- Rothman K.J. BMI-related errors in the measurement of obesity. Int. J. Obes. 2008;32:S56–S59. doi: 10.1038/ijo.2008.87. [DOI] [PubMed] [Google Scholar]
- SAS Institute SAS 9.3 Software. http://support.sas.com/software/93/ Available at: (Accessed July 19, 2016)
- Schultz P.W., Nolan J.M., Cialdini R.B., Goldstein R.N., Griskevicius V. The constructive, destructive, and reconstructive power of social norms. Psychol. Sci. 2007;18(5):429–434. doi: 10.1111/j.1467-9280.2007.01917.x. [DOI] [PubMed] [Google Scholar]
- Schuna J.M., Johnson W.D., Tudor-Locke C. Adult self-reported and objectively monitored physical activity and sedentary behavior: NHANES 2005-2006. Int. J. Behav. Nutr. Phys. Act. 2013;10:126. doi: 10.1186/1479-5868-10-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siri W.E. The gross composition of the body. Adv. Biol. Med. Phys. 1956;4:239–280. doi: 10.1016/b978-1-4832-3110-5.50011-x. [DOI] [PubMed] [Google Scholar]
- Sparling P.B., Snow T.K., Beavers B.D. Serum cholesterol levels in college students: opportunities for education and intervention. J. Am. Coll. Heal. 1999;48(3):123–127. doi: 10.1080/07448489909595683. [DOI] [PubMed] [Google Scholar]
- Spencer L. Results of a heart disease risk-factor screening among traditional college students. J. Am. Coll. Heal. 2002;50(6):291–296. doi: 10.1080/07448480209603447. [DOI] [PubMed] [Google Scholar]
- Tombaugh T.N. Trail making test a and b: normative data stratified by age and education. Arch. Clin. Neuropsychol. 2004;19(2):203–214. doi: 10.1016/S0887-6177(03)00039-8. [DOI] [PubMed] [Google Scholar]
- VandenBos G.R. American Psychological Association APA Dictionary of Psychology; Washington, DC: 2007. APA Dictionary of Psychology. [Google Scholar]
- Vogt W.P. second ed. Sage; Thousand Oaks, CA: 1999. Dictionary of Statistics and Methodology: A Nontechnical Guide for the Social Sciences. [Google Scholar]