Abstract
In this report, we describe the synthesis and characterization of 1,3-bis(hexyloxy)propan-2-yl nitrate (NDHP), a novel organic mono nitrate. Using purified xanthine oxidoreductase (XOR), chemiluminescence and electron paramagnetic resonance (EPR) spectroscopy, we found that XOR catalyzes nitric oxide (NO) generation from NDHP under anaerobic conditions, and that thiols are not involved or required in this process. Further mechanistic studies revealed that NDHP could be reduced to NO at both the FAD and the molybdenum sites of XOR, but that the FAD site required an unoccupied molybdenum site. Conversely, the molybdenum site was able to reduce NDHP independently of an active FAD site. Moreover, using isolated vessels in a myograph, we demonstrate that NDHP dilates pre-constricted mesenteric arteries from rats and mice. These effects were diminished when XOR was blocked using the selective inhibitor febuxostat. Finally, we demonstrate that NDHP, in contrast to glyceryl trinitrate (GTN), is not subject to development of tolerance in isolated mesenteric arteries.
Keywords: Nitric oxide, Organic nitrates, Xanthine oxidoreductase, Tolerance, Nitrite, Nitrate
1. Introduction
Organic nitrates are a class of drugs widely used for treatment of chronic heart failure and for symptomatic relief of ischemic heart disease [1], [2]. The prototypic organic nitrate, nitroglycerin, has been used in the clinic for over a century [3].
Nitroglycerin is enzymatically converted by mitochondrial aldehyde dehydrogenase (ALDH2) [4] to form nitric oxide (NO), which then mediates vasodilation by activation of sGC/cGMP signaling. The organic nitrates are believed to vasodilate preferentially venous vessels thereby decreasing preload. However, at higher doses, organic nitrates also dilate arteries, which may also result in unwanted side effects such as headaches and with chronic use even endothelial dysfunction [5], [6], [7]. Moreover, organic nitrates are subject to tolerance [8], [9], and therefore the development of new compounds lacking these side effects are warranted. Importantly, in addition to ALDH2, organic nitrates such as nitroglycerin and isosorbide dinitrate can also generate NO in a reaction catalyzed by xanthine oxidoreductase (XOR) [10], [11], in particular under low oxygen tensions [12]. Moreover, we and other groups have demonstrated that XOR may switch function and generate NO instead of superoxide, by using inorganic nitrite or nitrate as substrates [13], [14]. Exploiting XOR-mediated NO formation may represent an alternative for development of a novel class of NO donors for treatment of cardiovascular diseases.
In the current study, we synthesized and characterized a new organic mono nitrate 1,3-bis (hexyloxy) propan-2-yl nitrate (NDHP), and we provide experimental evidence showing that NDHP is reduced to NO by XOR and exerts vasorelaxation in mesenteric arteries from both rat and mouse, an effect that was partially blocked by the selective XOR inhibitor febuxostat.
2. Material and methods
2.1. Synthesis of NDHP (1,3-bis (hexyloxy) propan-2-yl nitrate)
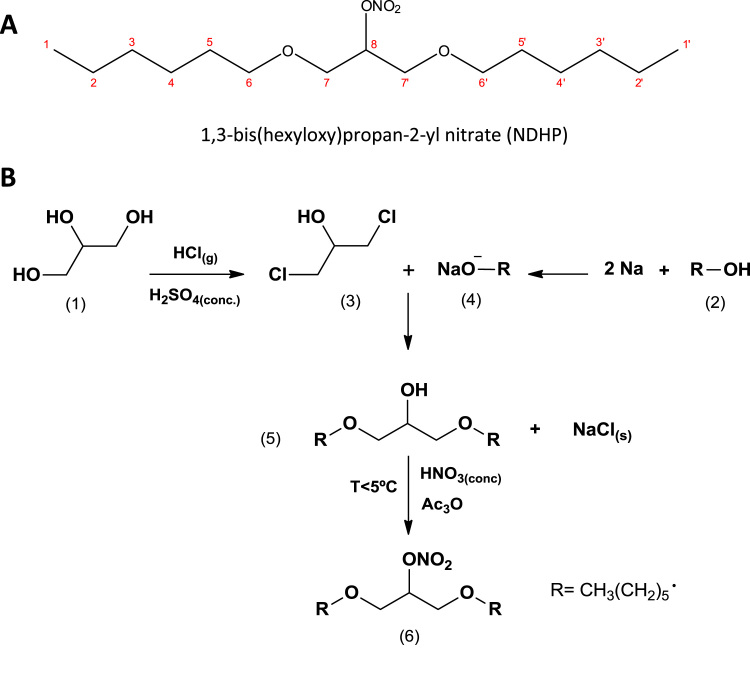
Firstly, 1,3-dichloropropan-2-ol (3) was obtained by reacting glycerol (1) with HCl (g). In brief, glycerol (200 g) was heated at 120 °C for 12 h to remove moisture and then hydrochloric acid was bubbled through a moisture-protected tubular system. Gaseous HCl was generated by dropping 100 mL of sulfuric acid (12 N) over slurry of sodium chloride (100 g) and hydrochloric acid (36.5%, 2 mol). The reaction was terminated when the absorption of HCl by glycerin was no longer observed (typically, at the end absorption the volume is increased by 25% from initial volume). Fractional distillation at 174–176 °C was used to purify the 1,3-dichloropropan-2-ol (3) obtained. Secondly, sodium alkoxide (4) was prepared by adding sodium metal (2 mol, finely cut) to a flask containing 1 mol of hexyl alcohol (2). The mixture was vigorously stirred until the full consumption of added sodium. The synthesis of oxyalcohol (5) was then carried out by reacting the sodium alkoxide (4; 2 mol) obtained with purified 1,3-dichloropropan-2-ol (3; 1 mol), added dropwise under continuous stirring for 6 h. The resulting mixture was distilled under vacuum at 185–190 °C, and then TLC and NMR were used to evaluate the purity. The reaction yield at this step is 83%. Finally, the 1,3-bis (hexyloxy) propan-2-yl nitrate (NDHP) was obtained by reacting the 0.5 mol of compound (5) with 0.6 moles of acetic anhydride. Fuming HNO3 (0.6 mol) was added dropwise to obtain the NDHP (Fig. 1A). The system was kept under constant stirring and controlled temperature 5 °C. The reaction was quenched with 100 mL of ice-cold distilled water and neutralized with sodium bicarbonate. The water was separated from the organic phase, which was solubilized in chloroform and dried with anhydrous sodium sulfate. Chloroform was subsequently removed by rotoevaporation. The purity of compound 1,3-bis (hexyloxy) propan-2-yl nitrate was assessed by TLC using hexane:ethyl acetate (9:1). The reaction yield was 83.2% and IR, 1H NMR, and 13C NMR spectroscopy were used to identify and confirm purity of compound obtained: molecular formulae: C15H31NO5; molar mass: 305,22 g/mol; C, 58.99%; H, 10.23%; N, 4.59%; O, 26.19%; 1H NMR (CDCl3, 500 MHz, δ ppm): 5,32–5,22 (m, 1H, J = 5,27, H-8), 3,61–3,59 (d, 4H, J = 5,60, H-7,7′), 3,44–3,39 (t, 4H, J = 3,42, H-6,6′), 1,61–0,82 (m, s, d, 22H, H-5,5′, H-4,4′, H-3,3′, H-2,2′, H-1,1′); 13C NMR (CDCl3, 125 MHz, δ ppm): 13,90 (C-1,1′), 22,55 (C-2,2′), 25,60 (C-3,3′), 29,40 (C-4,4′), 31,55 (C-5,5′), 67,94 (C-6,6′), 71,98 (C-7,7′), 81,22 (C-8); IR (ATR, cm-1): 2927–2850 (C–H, sp3), 1631 e 1269 (N–O), 1111 (C–O), 852 (N = O). The compound was synthetized in batches and storage in the darkness at 5 °C throughout experiments. After 45 days, the purity remains stable as confirmed by TLC and NMR spectroscopy.
Fig. 1.
Structural formulae and synthetic route for 1,3-bis (hexyloxy) propan-2-yl nitrate (NDHP). Panel A shown the structural formulae for NDHP. Panel B shows briefly the synthetic approach used to obtain NDHP. The purity of NDHP was assessed by TLC, and IR, 1H NMR, and 13C NMR spectroscopy were used to identify and confirm the purity of the compound obtained. The reaction yield was 83.2%.
2.2. Assessment of XOR-mediated NO production from NDHP
We evaluated NO formation from NDHP in the presence of purified XOR. In brief, a reactional buffer (PBS pH 7.4) containing purified XOR (0.05 U/mL, Roche, Cat. no: 10110434001), NADH (1 mM, Sigma, Cat. no: 10107735001), and NDHP (1 mM) was used. In specific experiments, NADH was replaced by xanthine (Sigma, Cat. no: X0626) or 2,3-dihydroxybenzaldehyde (DBA, sigma, Cat.no: 189839). A total of 1 mL of reactional buffer was added into a chamber of an Oxygraph-2k system (Oroboros instruments) at 37 °C. The Oxygraph chamber was connected in line to a chemiluminescence NO analyzer device (Eco Physics, Durnten, Switzerland), using nitrogen gas as carrier (400 mL/min), as described in detail before [13]. After a period of equilibration (approx. 5 min), NDHP, XOR, and electron donors NADH, xanthine, or DBA were directly injected into the chamber using Hamilton syringes. The NO production was recorded in real-time throughout the experiments by using a data acquisition system (AcqKnowledge v3.9, Biopac MP150, Goleta, CA, U.S.A.). NO production was recorded during 1 h and, in a subset of experiments, the XOR inhibitor oxypurinol (100 µM), the flavoprotein inhibitor DPI (50 µM), or L-cysteine (5 mM) was added 15 min prior to adding electron donors.
2.3. Electron paramagnetic resonance (EPR) spectroscopy
EPR studies were performed with the bench X-band spectrometer MiniScope MS400 (Magnettech, Germany) and the recordings were made at room temperature, and test samples were evaluated using capillary tubes provided by Magnettech (Germany). The instrument settings were 10 mW of microwave power, 0.6 mT of amplitude modulation, 100 kHz of modulation frequency, 12 s of sweep time, and 20 number of scans. The Fe(MGD)2 complex was freshly prepared by adding 100 µL of 1.9 mM FeSO4·7H2O, (prepared freshly by dissolving 0.8 mg in 1000 µL DPBS) and 100 µL of 18.4 mM of MGD (prepared freshly by dissolving 5.4 mg in 1000 µL DPBS) as previously described [15]. The DPBS was bubbled over one hour with nitrogen gas to avoid dissolved oxygen. The reaction buffer contained XOR (0.05 U/mL), NDHP (1 mM) and XOR substrate NADH (1 mM), xanthine (500 µM) or DBA (500 µM). The reaction buffer was kept at 37 °C under nitrogen atmosphere and slow homogenization, as described above. After 5 min of buffer equilibration, the Fe(MGD)2 complex was injected using Hamilton syringes and the reaction was allowed for 1 h. Afterwards, an aliquot was collected using capillary tubes and the spectra were carry out.
2.4. Measurement of nitrate, nitrite and S-nitrosothiols
The reaction buffer cocktail containing XOR (0.05 U/mL), NADH (1 mM), and increasing concentrations of NDHP (0.1, 1, and 10 mM) was allowed to form NO during 1 h in the presence or absence of L-cysteine (5 mM). NO production was monitored as described above and after 1 h, the mixture was collected and the concentrations of nitrite, nitrate, and nitrosothiols were evaluated. Nitrate and nitrite were assessed using a dedicated high performance liquid chromatography (HPLC) system (ENO-20; Eicom) as described in detail previously [16]. The method is based on the separation of nitrate by reverse-phase/ion exchange chromatography, followed by in-line reduction of nitrate to nitrite with cadmium and reduced copper. Derivatization of reduced nitrite was performed with Griess reagent, and the level of diazo compounds was measured at 540 nm. The samples were kept at 4 °C throughout the analyses by a cooling device in the auto sampler. The data were collected and analyzed using the PowerChrom software (V 2.7.9, eDAQ). S-nitrosothiols (RSNO) were analyzed in duplicate using an ozone-based reductive chemiluminescence assay using copper/ascorbic acid as reducing agent, as previously described [17]. In brief, 5 mL of PBS (pH 7.4) containing a large excess of ascorbic acid over CuCl2 (50 mM vs. 0.2 mM) was used and duplicate samples were injected into purge vessel. A standard curve was constructed injecting known amounts of S-nitrosoglutathione in duplicate. We used a CLD 77 NO chemiluminescence analyzer (Eco Physics, Durnten, Switzerland). The sensitivity was set in D3 with the aspirating sample tube running at 300 mL per minute. The data signal was collected using the Chromatography Data System software Azur 5.0.10 (Datalys; Le Touvet, France).
2.5. Mechanisms of NDHP activation
Next, mechanistic studies were performed in order to evaluate the putative XOR sites involved in the reduction of NDHP to NO. We used the same experimental setup described above, and exploited NO production mediated by different XOR substrates NADH, xanthine, and DBA, in the presence or absence of oxypurinol or DPI, a molybdenum and FAD site inhibitors, respectively, as described before [18].
2.6. Effects of NDHP on isolated mesenteric arteries
Multiwire myograph system (Model 620 M, Danish Myo Technology, Denmark) was used to evaluate the potential vascular effects of NDHP. Rat superior mesenteric artery rings were isolated, placed in Tyrode's solution, and all adhering tissue was removed in order to obtained rings (1–2 mm), which were kept gassed with carbogenic mixture (95% O2 and 5% CO2) and maintained at 37 °C and pH 7.4. Rings were mounted vertically on two Δ-shaped stainless steel wires in a myograph chamber, connected to a tension transducer (PowerLab™, ADInstruments, MA, U.S.A.), as previously described in detail [19], [20]. All rings were stabilized under 0.75 g resting tension for 1 h. Tissue viability was verified by the presence of a contraction to phenylephrine (PHE, 10 μM) added to the bath, and successful removal of the endothelium was verified by the absence of a response to acetylcholine (ACH; 10 μM), as previously described. For denuded vessels, vasorelaxation less than 90% were considered as without endothelium. The mesenteric artery rings were pre-constricted using PHE (1 µM) until the contraction plateau was reached, then NDHP (10–12–10−3 mol/L) was added to the organ bath in order to build a concentration-response curve. Similarly, second-order branch of mesenteric resistance vessels (200–250 µm in diameter) from C57BL6 mice (weight of 28–32 g) were isolated and dissected in ice-cold Krebs solution (composition in mmol/L: NaCl 119; KCl 4.7; CaCl2 1.6; KH2PO4 1.2; MgSO4·7H2O 1.2; NaHCO3 25.1; glucose 5.5; EDTA 0.026). Arterial segments (1–2 mm) were mounted on 25 µm tungsten wires in the multi-wire myograph system. After mounting, stabilization and washout protocols (as described above), 1 µM PHE was used to preconstrict the arterial rings to obtain a basal tone of approximately 50% of its diameter. When the constriction reached a steady-state plateau, NDHP (10−6–10−3 mol/L) was cumulatively added to the chambers [21]. Cumulative concentration-responses were studied with or without pretreatment (15 min) with febuxostat (500 nM). The responses are expressed as percentage of vasorelaxation in PHE pre-constricted vessels and the potency (pD2) and maximum relaxation effect (Emax) were calculated using GraphPad Prism v. 5.0. The experimental protocols were approved by Institutional Animal Care and Use Committee (IACUC) from Karolinska Institute in Stockholm, Sweden, and performed according to the National Institutes of Health guidelines for the conduct of experiments in animals.
2.7. Induction of tolerance in mesenteric artery
Mesenteric artery rings without functional endothelium were preincubated with nitroglycerin (GTN, 100 µM) or NDHP (1 mM) for 30 min; then the physiological solution was successively changed ten times for complete removal of the drugs previously used. A new stabilization period (60 min) was then performed with the exchange of the nutrient solution every 15 min. At the end of the stabilization period a new contraction was induced with phenylephrine (PHE, 1 μM), and after plateau was reached, GTN (10–12–10−3 M) or NDHP (10–12–10−3 M) was added to the bath in increasing and cumulative concentrations. The potency (pD2) and maximum relaxation effect (Emax) were calculated as described above.
2.8. Drugs and solutions
All drugs and reagents used were purchased from Sigma Chemical Co. (St Louis, MO, USA), except the spin trapping N-(Dithiocarbamoyl)-N-methyl-D-glucamine sodium (FGD), which was bought from Enzo Life Sciences (Cat.no: ALX-400-014). All drugs were dissolved immediately before use.
2.9. Statistical analysis
The results are expressed as means ± S.E.M. The comparisons between groups were assessed by t-tests or one-way analysis of variance followed by Dunnett's multiple comparison tests. Vasodilatory responses to NDHP were analyzed by two-way repeated measures ANOVA followed by Sidak post-hoc test. Statistical analyses were carried out using the software GraphPad Prism v. 5.0. A P-value < 0.05 was considered significant.
3. Results and discussion
3.1. XOR catalyzes the reduction of NDHP to NO
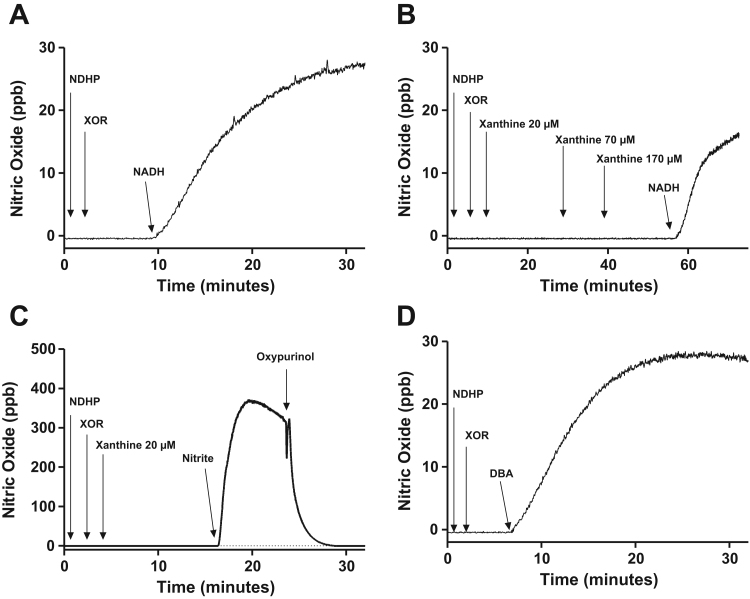
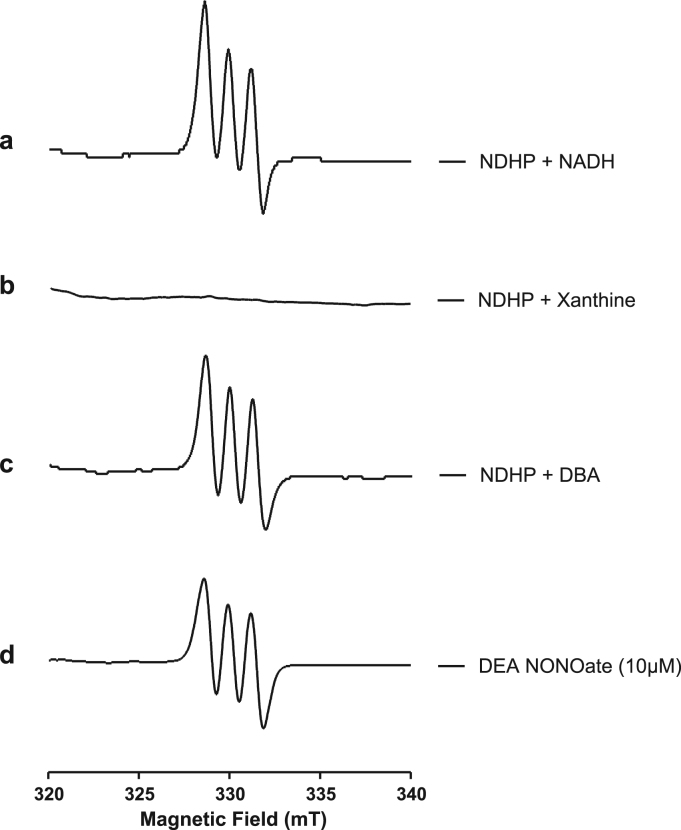
XOR has been widely implicated in the bioactivation of inorganic nitrite, nitrate, and organic nitrates, via reduction steps to form NO [10], [11], [22]. We evaluated if XOR would be able to reduce NHDP to NO using chemiluminescence detection, and exploited different XOR substrates as electron donors. NDHP alone or in association with XOR was unable to induce any NO generation (Fig. 2A). However, addition of NADH promptly induced a robust NO signal (Fig. 2A), which remained stable until it started to decay at around 1 h after NADH addition. Surprisingly, when xanthine was used as the electron donor instead of NADH, NO generation was not observed, even when high concentrations of xanthine were tested (Fig. 2B). Xanthine is a purine base that is difficult to dissolve in water, and typically alkaline solutions and ultrasound sonication are needed. In our experiments, stock solutions of xanthine were prepared in NaOH (10 mM), which could possibly affect XOR/X activity. However, even after association of NDHP, XOR and high concentration of xanthine (500 µM), an NO signal was not detected, but NADH was still able to trigger NO generation (Fig. 2B). Correspondingly, using the same experimental conditions and using xanthine concentrations as low as 20 µM, inorganic nitrite induced high levels of NO generation (Fig. 2C). These results confirm that both XOR and xanthine solutions were entirely viable in our experimental conditions, and suggest that xanthine is not an electron donor for the XOR-mediated bioactivation of NDHP. Furthermore, similarly to NADH, DBA also induced a robust NO signal (Fig. 2D). We confirmed XOR-mediated reduction of NDHP to NO by using EPR spectroscopy and Fe2+-MGD, which traps NO. Again, when NADH or DBA were used as electron donors, a characteristic triplet spectrum from NO-Fe(MGD)2 was detected (Fig. 3, spectrum a and c, respectively), but no signal was observed when xanthine was used (Fig. 3, spectrum b). Finally, the NO formation from NDHP was followed of accumulation of nitrite and nitrate in the reaction buffer (Table 1).
Fig. 2.
Assessment of NO formation from NDHP in the presence of XOR and different electron donors. NO formation was assessed in real-time using a chemiluminescence device and nitrogen gas as the NO carrier. The experimental conditions were: 1 mL reactional buffer (PBS, pH 7.4) containing XOR (0.05 U/mL), NDHP (1 mM) and the substrate A) NADH (1 mM), B) xanthine (20–500 µM), or D) 2,3-dihydroxybenzaldehyde (DBA, 500 µM). While only noise signals were detected in the presence of NDHP and XOR alone, adding NADH or DBA induced a distinct increase in nitric oxide formation. Conversely, increasing concentrations of xanthine induced no XOR-mediated NO generation from NDHP (Panel B). Similarly, the combination NDHP, XOR and xanthine (20 µM) induced no NO generation, but a later addition of nitrite (1 mM) to this mixture induced a distinct NO signal, which was inhibited by oxypurinol (Panel C). The tracings are representative of 4–6 independent experiments.
Fig. 3.
Electron paramagnetic resonance (EPR) detection of NO formation from NDHP in the presence of XOR and different electron donors. The EPR spectra (X-band) of water-soluble complex NO-Fe(MGD)2 was recorded at room temperature. A total of 1 mL reactional buffer (PBS, pH 7.4) contained NDHP (1 mM), XOR (0.05 U/mL), and NADH (1 mM, a), xanthine (500 µM, b), or 2,3-dihydroxybenzaldehyde (DBA, 500 µM, c) as electron donors. The short-lived nitric oxide donor DEA NONOate was used as positive control (d). The parameters for the EPR device (MiniScope MS400, Magnettech) were 10 mW of microwave power, 0.6 mT of amplitude modulation, 100 kHz of modulation frequency, 12 s of sweep time, and 20 number of scans. Traces are representative from 3 to 4 independent experiments.
Table 1.
Levels of nitrite and nitrate accumulated in a reaction buffer after 60 min incubation of XOR and the novel organic nitrate NDHP. The experimental conditions are as described in Fig. 2 and NADH (1 mM) was used as the electron donor. (n = 3–4 independent experiments for each NDHP concentration tested).
| NDHP | 0.1 mM | 1 mM | 10 mM |
|---|---|---|---|
| Nitrite (μM) | 7.13 ± (0.52) | 28.87 (4.65) | 53.70 (8.68) |
| Nitrate (μM) | 9.33 (0.75) | 26.42 (0.84) | 104.7 (9.96) |
Data are shown as mean ± (S.E.M.)
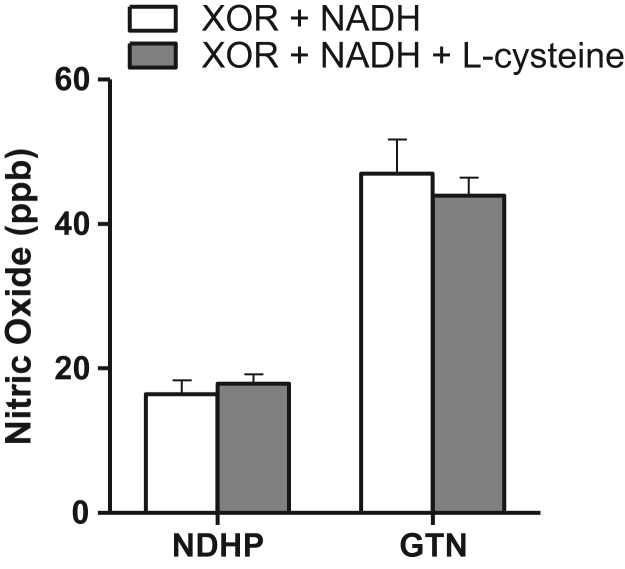
3.2. Effect of thiols on XOR-catalyzed reduction of NDHP
Thiols have been implicated in the biotransformation of organic nitrates such as glyceryl trinitrate, isosorbide dinitrate, and pentaerythritol tetranitrate [11], [23], although conflicting observations have been reported [3]. Similarly, the role of thiols in XOR-mediated NO formation from organic nitrates is still controversial. Using experimental conditions similar to ours, Millar et al. [10] reported XOR-mediated NO formation from nitroglycerin independently of thiols [10], while Li et al. [11] showed that thiols are required for XOR-dependent NO formation from both nitroglycerin and isosorbide dinitrate [11]. We tested if thiols were involved in NO generation from NDHP, and if the NO nitrosothiols would be formed. Using the same experimental settings described above with NADH as the electron donor and in the presence or absence of L-cysteine, NO generation was monitored for 60 min. At the end of experiment the reaction buffer was collected for assessment of nitrosothiol content. The presence of L-cysteine induced no change in the NO generation from NDHP (Fig. 4) suggesting that NDHP does not require sulfhydryl (SH-) to generate NO. Similar results were found for nitroglycerin in line with results from Millar et al. [10] Additionally, nitrosothiol formation was not found in the reaction buffer at the end of experiments (data not shown), suggesting that nitrosothiols are not an intermediate source of the NO formed from NDHP.
Fig. 4.
Effect of thiols on XOR-catalyzed reduction of NDHP and nitroglycerin (GTN) to NO. The presence of L-cysteine induced no changes in NO formation from either NDHP or GTN. The experimental conditions were: 1 mL reactional buffer (PBS, pH 7.4) containing XOR (0.05 U/mL), NDHP (1 mM) or GNT (1 mM), NADH (1 mM), in the presence or absence of L-cysteine (5 mM). Data are shown as mean ± S.E.M. (n = 4).
3.3. Mechanisms for NDHP activation by XOR
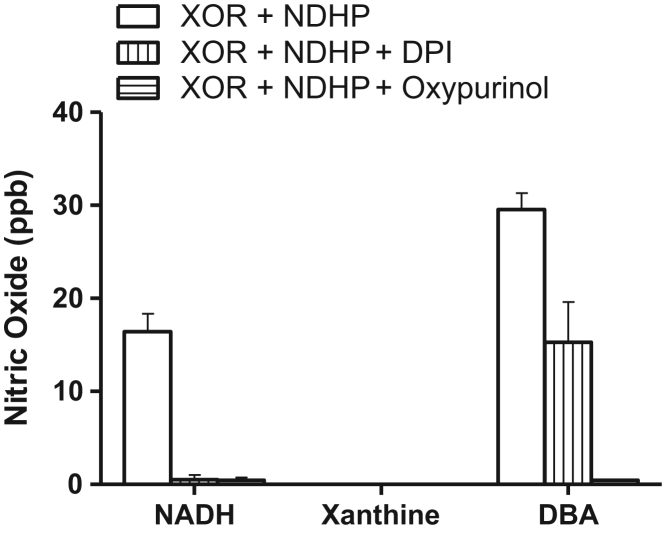
Next we evaluated the potential sites on XOR that could be involved in the reduction of NDHP to NO. XOR has two reducing sites (FAD and a molybdenum) that have been implicated in nitrite, nitrate, and organic nitrate bioactivation to NO [11]. When NADH was used as a substrate, the selective inhibitor of the FAD site DPI completely blocked NO production from NDHP (Fig. 5). Surprisingly, the molybdenum site inhibitor oxypurinol also blunted NO formation from NDHP. Whereas NADH acts as an electron donor only at the FAD site, these findings suggest that the FAD site of XOR requires an unoccupied molybdenum site for NDHP bioactivation. When DBA was used as the substrate, NO formation also was observed (Fig. 5). Pretreatment with DPI, a FAD blocker, decreased NO production by approximately 50%. Interestingly, DBA has been described as an electron donor at the molybdenum site [11] and as expected, oxypurinol completely blunted NO production (Fig. 5). These results suggest that DBA is not a selective electron donor for the molybdenum site of XOR, but donates electrons at both the FAD and molybdenum sites albeit with some preferences for the molybdenum site. Altogether, these findings suggest that NDHP may be reduced to NO at both sites of XOR, FAD and molybdenum, but the FAD site of XOR requires an unoccupied molybdenum site for NDHP bioactivation.
Fig. 5.
Mechanism of NDHP activation. When NADH was used as a substrate, the FAD inhibitor DPI completely blocked NO production from NDHP. Similarly, the molybdenum site inhibitor oxypurinol also blunted NO formation from NDHP. Xanthine does not serve as electron donor for NDHP reduction. When DBA was used as the substrate, NO formation also was observed but pretreatment with DPI decreased NO production by approximately 50% while oxypurinol completely blunted NO production. The experimental conditions used were: 1 mL reactional buffer (PBS, pH 7.4) containing XOR (0.05 U/mL), NDHP (1 mM) and the substrate NADH (1 mM), xanthine (500 µM) or DBA (500 µM). The concentration used for the inhibitors were 100 µM for DPI and 50 µM for oxypurinol. Data are shown as mean ± S.E.M. (n = 4).
3.4. Vasorelaxation effects of NDHP in mesenteric arteries and role of XOR
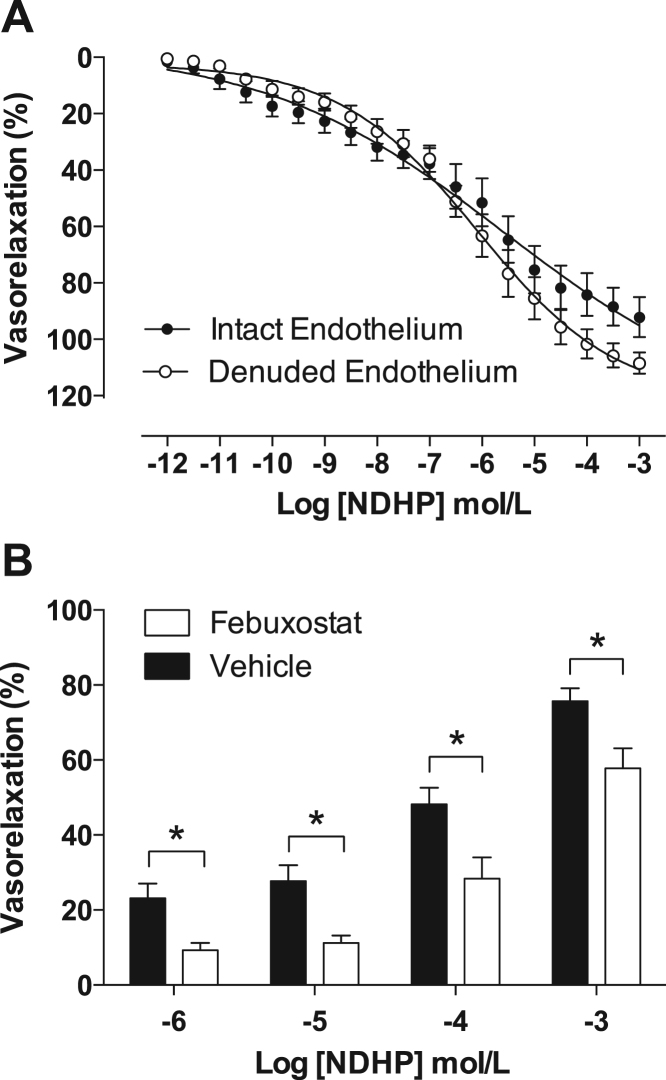
Functional studies revealed that NDHP induces vasorelaxation of mesenteric resistance arteries from rats in a concentration-dependent manner (Fig. 6A). The presence or absence of an endothelium had no impact on the vasodilatory responses to NDHP (pD2 = 6.3 ± 0.10 and Emax = 92 ± 7% for intact endothelium; pD2 = 6.6 ± 0.07 and Emax = 109 ± 4% for denuded endothelium, P > 0.05), demonstrating endothelium-independent vasorelaxation. Further, we evaluated NDHP-mediated vasorelaxation in resistance mesenteric arteries from mice. Similarly, NDHP induced vasorelaxation in a concentration-dependent manner, and these properties were significantly attenuated when the vessels were pre- incubated with febuxostat (P < 0.05, Fig. 6B). Together, these results show that NDHP is a vasodilator that acts independently of the endothelium, and that a part of its vasorelaxation properties is mediated by XOR.
Fig. 6.
NDHP-mediated vasorelaxation and the role of XOR. Panel A shows concentration-response curves of NDHP (10–12–10−3 mol/L) in superior mesenteric arteries from rats. NDHP induced a concentration-dependent vasorelaxation in both intact and denuded-endothelium vessel segments (n = 6 and 10, respectively). Panel B shows the effect of the selective XOR inhibitor febuxostat on vasorelaxation effects of NDHP in 3nd order branch mesenteric arteries from mice. Intact-endothelium vessels were pre-incubated with vehicle or febuxostat (500 nM, n = 6 and 10, respectively) for 15 min before the concentration-response to NDHP (10−6–10−3 mol/L). The responses are expressed as percentage of vasorelaxation in phenylephrine pre-constricted vessels in both sets of experiments. No significant differences were found when comparing intact versus denuded-endothelium (P > 0.05, A) *P < 0.05 versus Vehicle (B). Data are shown as mean ± S.E.M.
Oxidative stress and NO deficiency are considered to contribute to the development or progression of cardiovascular disorders, including coronary heart disease, cerebrovascular disease, peripheral arterial disease [24]. Increased XOR-mediated superoxide and hydrogen peroxide generation may contribute to endothelial dysfunction, metabolic and functional impairment, inflammatory activation, and other features of cardiovascular pathophysiology [25]. In this regard, we have been developing novel organic nitrates with the aim of finding compounds that lack tolerance development and can be reduced to NO by XOR, thus reducing oxidative stress that is associated with altered XOR function in the vasculature [19], [26]. The novel organic nitrate NDHP may have dual benefits by switching the function of XOR from generating superoxide to instead produce NO.
3.5. NDHP does not induce tolerance in mesenteric arteries
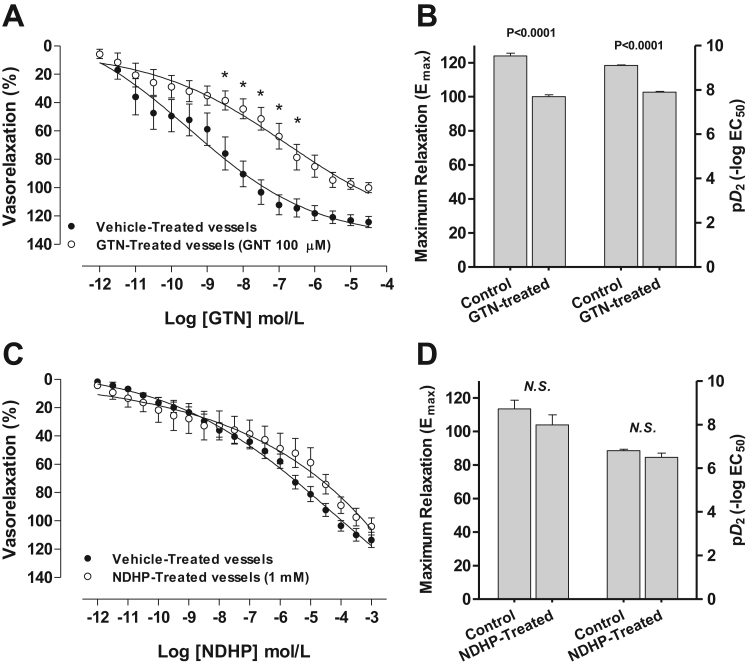
Organic nitrates are subjected to development of tolerance [8], [9]. In this regard, we evaluated the ability of NDHP to induce tolerance in mesenteric arteries and used nitroglycerin (GTN) as standard. As expected, GTN induced a concentration-dependent vasorelaxation (Fig. 7A). However, pre-incubation of mesenteric rings for 30 min in GTN (100 µM) induced a significant shift to the right of vasorelaxation curves (Fig. 7A and B; pD2 = 9.1 ± 0.10 versus pD2 = 7.9 ± 0.10, for vehicle- and GTN-treated vessels, respectively; P < 0.001). In addition, GTN pretreatment also decreased the maximum relaxation values (Fig. 7B; Emax = 124 ± 4% and Emax = 100 ± 3% for vehicle- and GTN-treated vessels, respectively; P < 0.001). Conversely, NDHP pretreatment induced no significant changes on pD2 (Fig. 7D; pD2 = 6.8 ± 0.08 and 6.5 ± 0.20, for vehicle- and NDHP-treated vessels, respectively; P > 0.05) or Emax (Fig. 7D; Emax = 124 ± 4% and Emax = 100 ± 3% for vehicle- and NDHP-treated vessels, respectively; P > 0.05). Altogether, these data suggest that in opposition to GTN, NDHP does not induce tolerance in mesenteric arteries. However, GTN still exhibit higher potency than NDHP, which is compatible with the number of nitrate groups each molecule, three for GTN versus one in NDHP.
Fig. 7.
NDHP does not induce tolerance in mesenteric arteries. Panels A and C show concentration-response curves for GTN and NDHP (10–12–10−3 mol/L), respectively, in endothelium-denuded superior mesenteric arteries from rats. GTN induced a concentration-dependent vasorelaxation in arterial rings (A). When the ring vessels were pre-treated for 30 min in GTN (100 µM), the potency (pD2) and maximum relaxation effects (Emax) were significantly reduced (B). Conversely, NDHP pretreatment induced no significant changes either pD2 or Emax (D) suggesting that in opposition to GTN, NDHP is not subjected to development of tolerance in mesenteric arteries. N = 6–7 per group. N.S. = non-significant. Data are shown as mean ± S.E.M.
In summary, this study describes the synthesis and characterization of a novel organic nitrate NDHP, which can be reduced to NO by XOR and induces vasorelaxation of mesenteric arteries from rats and mice. In addition, our in vitro findings suggests that NDHP does not induce tolerance as is the case with the prototypic nitrovasodilator GTN. Further studies in vivo will reveal the therapeutic value of NDHP in models of cardiovascular disease, by investigating tolerance formation, endothelial function and blood pressure lowering effects following chronic treatment, as well as its effects on XOR-mediated oxidative stress.
Sources of funding
This study was supported by grants from the William Harvey Research Institute Academy (Project 608765 M.F.M.), the Swedish Medical Research Council (Project 2016-01381 M.C.), the Swedish Heart and Lung Foundation (Projects: 20140673 J.O.L. & 20140448 M.C.), Karolinska Institutet KID Grant (Project: 2‐3707/2013 M.C.), CAPES/STINT (Projects: 1499/2014 V.A.B. & BR2013-5512 M.C.).
Acknowledgements
We thank Annika Olsson and Carina Nihlén (Dept. of Physiology and Pharmacology, Karolinska Institutet) for their specialized technical contribution. Special thanks to Magnettech GmbH (Berlin, Germany) for offering us the bench X-band spectrometer MiniScope MS400, which was used in the present study.
References
- 1.Wilson J.F. In the clinic. Stable ischemic heart disease. Ann. Intern. Med. 2014;160(1) doi: 10.7326/0003-4819-160-1-201401070-01001. (ITC1-1-16; quiz ITC1-16) [DOI] [PubMed] [Google Scholar]
- 2.Mebazaa A., Yilmaz M.B., Levy P., Ponikowski P., Peacock W.F., Laribi S., Ristic A.D., Lambrinou E., Masip J., Riley J.P., McDonagh T., Mueller C., deFilippi C., Harjola V.P., Thiele H., Piepoli M.F., Metra M., Maggioni A., McMurray J., Dickstein K., Damman K., Seferovic P.M., Ruschitzka F., Leite-Moreira A.F., Bellou A., Anker S.D., Filippatos G. Recommendations on pre-hospital & early hospital management of acute heart failure: a consensus paper from the Heart Failure Association of the European Society of Cardiology, the European Society of Emergency Medicine and the Society of Academic Emergency Medicine. Eur. J. Heart Fail. 2015;17(6):544–558. doi: 10.1002/ejhf.289. [DOI] [PubMed] [Google Scholar]
- 3.Ignarro L.J. After 130 years, the molecular mechanism of action of nitroglycerin is revealed. Proc. Natl. Acad. Sci. USA. 2002;99(12):7816–7817. doi: 10.1073/pnas.132271799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen Z., Zhang J., Stamler J.S. Identification of the enzymatic mechanism of nitroglycerin bioactivation. Proc. Natl. Acad. Sci. USA. 2002;99(12):8306–8311. doi: 10.1073/pnas.122225199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tfelt-Hansen P.C., Tfelt-Hansen J. Nitroglycerin headache and nitroglycerin-induced primary headaches from 1846 and onwards: a historical overview and an update. Headache. 2009;49(3):445–456. doi: 10.1111/j.1526-4610.2009.01342.x. [DOI] [PubMed] [Google Scholar]
- 6.Munzel T., Steven S., Daiber A. Organic nitrates: update on mechanisms underlying vasodilation, tolerance and endothelial dysfunction. Vasc. Pharmacol. 2014;63(3):105–113. doi: 10.1016/j.vph.2014.09.002. [DOI] [PubMed] [Google Scholar]
- 7.Munzel T., Daiber A., Gori T. More answers to the still unresolved question of nitrate tolerance. Eur. Heart J. 2013;34(34):2666–2673. doi: 10.1093/eurheartj/eht249. [DOI] [PubMed] [Google Scholar]
- 8.Munzel T., Daiber A., Mulsch A. Explaining the phenomenon of nitrate tolerance. Circ. Res. 2005;97(7):618–628. doi: 10.1161/01.RES.0000184694.03262.6d. [DOI] [PubMed] [Google Scholar]
- 9.Omar S.A., Artime E., Webb A.J. A comparison of organic and inorganic nitrates/nitrites. Nitric Oxide. 2012;26(4):229–240. doi: 10.1016/j.niox.2012.03.008. [DOI] [PubMed] [Google Scholar]
- 10.Millar T.M., Stevens C.R., Benjamin N., Eisenthal R., Harrison R., Blake D.R. Xanthine oxidoreductase catalyses the reduction of nitrates and nitrite to nitric oxide under hypoxic conditions. FEBS Lett. 1998;427(2):225–228. doi: 10.1016/s0014-5793(98)00430-x. [DOI] [PubMed] [Google Scholar]
- 11.Li H., Cui H., Liu X., Zweier J.L. Xanthine oxidase catalyzes anaerobic transformation of organic nitrates to nitric oxide and nitrosothiols: characterization of this mechanism and the link between organic nitrate and guanylyl cyclase activation. J. Biol. Chem. 2005;280(17):16594–16600. doi: 10.1074/jbc.M411905200. [DOI] [PubMed] [Google Scholar]
- 12.Cantu-Medellin N., Kelley E.E. Xanthine oxidoreductase-catalyzed reduction of nitrite to nitric oxide: insights regarding where, when and how. Nitric Oxide. 2013;34:19–26. doi: 10.1016/j.niox.2013.02.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Peleli M., Zollbrecht C., Montenegro M.F., Hezel M., Zhong J., Persson E.G., Holmdahl R., Weitzberg E., Lundberg J.O., Carlstrom M. Enhanced XOR activity in eNOS-deficient mice: effects on the nitrate-nitrite-NO pathway and ROS homeostasis. Free Radic. Biol. Med. 2016;99:472–484. doi: 10.1016/j.freeradbiomed.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 14.Lundberg J.O., Gladwin M.T., Weitzberg E. Strategies to increase nitric oxide signalling in cardiovascular disease. Nat. Rev. Drug Discov. 2015;14(9):623–641. doi: 10.1038/nrd4623. [DOI] [PubMed] [Google Scholar]
- 15.Gopalakrishnan B., Nash K.M., Velayutham M., Villamena F.A. Detection of nitric oxide and superoxide radical anion by electron paramagnetic resonance spectroscopy from cells using spin traps. J. Vis. Exp. 2012;66:e2810. doi: 10.3791/2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Montenegro M.F., Sundqvist M.L., Nihlen C., Hezel M., Carlstrom M., Weitzberg E., Lundberg J.O. Profound differences between humans and rodents in the ability to concentrate salivary nitrate: implications for translational research. Redox Biol. 2016;10:206–210. doi: 10.1016/j.redox.2016.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sengupta R., Billiar T.R., Stoyanovsky D.A. Studies toward the analysis of S-nitrosoproteins. Org. Biomol. Chem. 2009;7(2):232–234. doi: 10.1039/b817981f. [DOI] [PubMed] [Google Scholar]
- 18.Li H., Samouilov A., Liu X., Zweier J.L. Characterization of the effects of oxygen on xanthine oxidase-mediated nitric oxide formation. J. Biol. Chem. 2004;279(17):16939–16946. doi: 10.1074/jbc.M314336200. [DOI] [PubMed] [Google Scholar]
- 19.Porpino S.K., Zollbrecht C., Peleli M., Montenegro M.F., Brandao M.C., Athayde-Filho P.F., Franca-Silva M.S., Larsson E., Lundberg J.O., Weitzberg E., Persson E.G., Braga V.A., Carlstrom M. Nitric oxide generation by the organic nitrate NDBP attenuates oxidative stress and angiotensin II-mediated hypertension. Br. J. Pharmacol. 2016;173(14):2290–2302. doi: 10.1111/bph.13511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu M., Zollbrecht C., Peleli M., Lundberg J.O., Weitzberg E., Carlstrom M. Nitrite-mediated renal vasodilatation is increased during ischemic conditions via cGMP-independent signaling. Free Radic. Biol. Med. 2015;84:154–160. doi: 10.1016/j.freeradbiomed.2015.03.025. [DOI] [PubMed] [Google Scholar]
- 21.Montenegro M.F., Sundqvist M.L., Larsen F.J., Zhuge Z., Carlstrom M., Weitzberg E., Lundberg J.O. Blood pressure-lowering effect of orally ingested nitrite is abolished by a proton pump inhibitor. Hypertension. 2017;69(1):23–31. doi: 10.1161/HYPERTENSIONAHA.116.08081. [DOI] [PubMed] [Google Scholar]
- 22.Li H., Samouilov A., Liu X., Zweier J.L. Characterization of the magnitude and kinetics of xanthine oxidase-catalyzed nitrate reduction: evaluation of its role in nitrite and nitric oxide generation in anoxic tissues. Biochemistry. 2003;42(4):1150–1159. doi: 10.1021/bi026385a. [DOI] [PubMed] [Google Scholar]
- 23.Kojda G., Hacker A., Noack E. Effects of nonintermittent treatment of rabbits with pentaerythritol tetranitrate on vascular reactivity and superoxide production. Eur. J. Pharmacol. 1998;355(1):23–31. doi: 10.1016/s0014-2999(98)00460-9. [DOI] [PubMed] [Google Scholar]
- 24.Elahi M.M., Kong Y.X., Matata B.M. Oxidative stress as a mediator of cardiovascular disease. Oxid. Med. Cell. Longev. 2009;2(5):259–269. doi: 10.4161/oxim.2.5.9441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Doehner W., Landmesser U. Xanthine oxidase and uric acid in cardiovascular disease: clinical impact and therapeutic options. Semin. Nephrol. 2011;31(5):433–440. doi: 10.1016/j.semnephrol.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 26.Franca-Silva M.S., Luciano M.N., Ribeiro T.P., Silva J.S., Santos A.F., Franca K.C., Nakao L.S., Athayde-Filho P.F., Braga V.A., Medeiros I.A. The 2-nitrate-1,3-dibuthoxypropan, a new nitric oxide donor, induces vasorelaxation in mesenteric arteries of the rat. Eur. J. Pharmacol. 2012;690(1–3):170–175. doi: 10.1016/j.ejphar.2012.06.043. [DOI] [PubMed] [Google Scholar]