Abstract
Objective: To report the first case of ciguatera-associated rheumatoid arthritis in Japan.
Patient: A 53-year-old man presented to our clinic with morning stiffness and pain in the fingers and wrists.
Results: For six months, he had suffered from chronic pain in both hands and shoulders caused by ciguatera poisoning. He was referred to a local general hospital and diagnosed with RA.
Conclusion: When synovitis becomes evident in chronic ciguatera poisoning, reevaluation is necessary, including investigation of chronic arthritis, which might be associated with the onset of RA.
Keywords: ciguatera poisoning, rheumatoid arthritis, Okinawa, Minamidaito Island
Introduction
Ciguatera poisoning is a type of food poisoning caused by ingestion of fish in subtropical and tropical regions that are contaminated by ciguatoxin. Ciguatoxin is produced by a dinoflagellate called Gambierdiscus toxicus and is concentrated through the food chain and is mainly accumulated in fish muscles1). Ciguatera poisoning causes a variety of symptoms, including acute and chronic phases. Chronic symptoms are general malaise, numbness, pruritus, and arthralgia1). Ciguatoxin may be associated with chronic systemic diseases such as polymyositis, chronic fatigue syndrome, and fibromyalgia2,3,4). It has not been previously reported that ciguatera poisoning can lead to the onset of rheumatoid arthritis (RA). To our knowledge, this is the first report from Japan of RA following ciguatera poisoning, and we believe that it will provide a new insight into the clinical course of ciguatera poisoning.
Patient
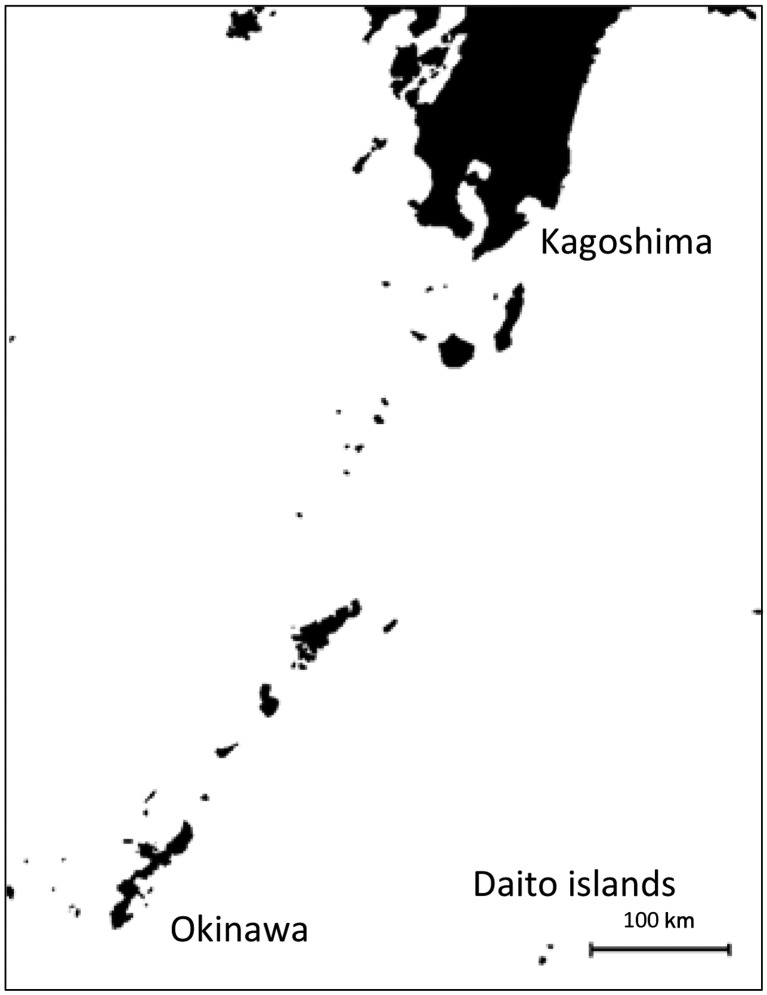
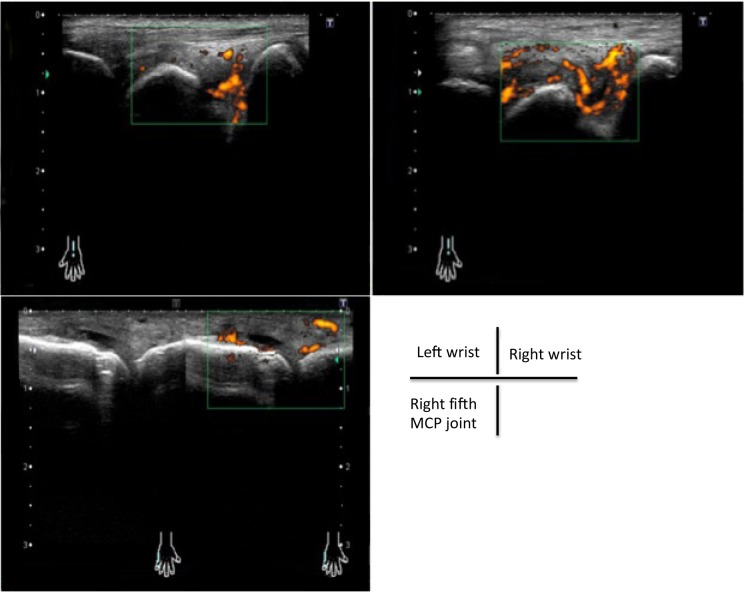
A 53-year-old man presented to our clinic on Minamidaito island (Figure 1) of Okinawa with morning stiffness and pain in the fingers and wrists of both hands. Six months previously, after eating boiled Oplegnathus punctatus (Figure 2), the patient had sought medical attention along with two family members because of numbness in both arms and the oral cavity, pain in the hands and shoulders, as well as pruritus of the whole body. His medical history included diabetes mellitus with neuropathy and retinopathy. He was taking insulin glargine 30 Units (U) and insulin aspart 6U-4U-8U. His vital signs were stable. Physical examination showed decreased sensation in both hands and feet, but there was no joint swelling or tenderness. All three individuals had similar symptoms and were diagnosed with ciguatera poisoning. The patient was prescribed diclofenac and pregabalin. One month before admission, the joint pain became so acute that the patient came back for reevaluation. On physical examination, the following were warm, swollen, and tender: left fifth metacarpophalangeal joint, right second metacarpophalangeal joint, right second proximal interphalangeal joint, right third metatarsophalangeal joint, and right fourth metatarsophalangeal joint. There was only tenderness in both shoulders without swelling. Blood tests revealed an erythrocyte sedimentation rate of 54 mm, rheumatoid factor of 70 IU / mL and an anti-CCP antibody level of 377 U /mL. Anti-SS-A / Ro antibody and antinuclear antibody were negative. Based on ACR/EULAR classification criteria, the patient was diagnosed with RA and referred to a local general hospital for further investigation. Joint ultrasound revealed an enhancement of blood flow signal in the right fifth metacarpophalangeal joint and bilateral wrists (Figure 3). No abnormalities were seen on plain radiographs of the hands and chest. His symptoms were controlled with salazosulfapyridine 1000 mg.
Figure 1.
The Minamidaito island and Kitadaito island make up the Daito islands. The former is located in the south.
Figure 2.

Oplegnathus punctatus. The fish inhabits rocky and coral reefs in Pacific Ocean.
Figure 3.
Ultrasound of both wrists and the right fifth finger. There are enhancements of blood flow signal in both wrists and the right fifth metacarpophalangeal joint.
Discussion
The clinical implications of this case are two-fold: 1) a similarity of clinical manifestations between RA and ciguatera poisoning; and 2) the possibility of a cause-and-effect relationship between ciguatera poisoning and RA.
In ciguatera poisoning, general malaise and arthralgia occur in 60–100% and 29–86% of patients, respectively5). Similar results have been reported from other areas of Japan; these symptoms may persist for several months and become chronic1). In chronic ciguatera poisoning, the clinical presentation can be similar to that seen in connective tissue diseases, and it is possible that ciguatoxin might induce the onset of some connective tissue diseases. For example, inflammation of muscle tissues induced by ciguatoxin can lead to polymyositis6). When symptoms are prolonged and clinical features of arthritis become evident, we should reconsider the diagnosis and proceed to investigation of chronic arthritis.
It has not been previously reported that ciguatera poisoning can cause arthritis. However, in experimental models of RA established in small animals, some toxins such as lipopolysaccharide and pertussis toxin may be related to arthritis, and the pathogenesis of this arthritis model might be partially shared with that of human RA7,8,9). These results may support the proposed cause-and-effect relationship between ciguatera poisoning and RA. Furthermore, ciguatoxin was shown to up-regulate mRNA expression of proinflammatory cytokines, tumor necrosis factor-α (TNF-α), matrix metalloproteinase-9 (MMP-9), interleukin-1β and-610). TNF-α plays a dominant role in RA, and patients with RA have high levels of TNF-α, which activate inflammation and destruction of joints11). MMPs, a family of related enzymes, mediate the hydrolysis of connective tissue extracellular matrix12). MMP-9 is increased in patients with RA and shows that the disease is active13). MMP-9 may promote inflammation and cartilage degradation in patients with RA14, 15). Based on this evidence, it is suggested that the increase in TNF-α and MMP-9 may be related to the onset and progression of RA in patients with chronic ciguatera poisoning. Unfortunately, we did not measure these inflammatory mediators in our patient. However, based on the overall evidence, there is a possibility that systemic inflammation induced by ciguatera poisoning might be associated with the onset of RA.
Conclusion
We need to recognize that reevaluation is of great importance when synovitis becomes evident in patients with chronic ciguatera poisoning, and ciguatera poisoning can be associated with onset of RA, although a cause-and-effect relationship is not yet definitively established.
References
- 1.Lehane L, Lewis RJ. Ciguatera: recent advances but the risk remains. Int J Food Microbiol 2000; 61: 91–125. doi: 10.1016/S0168-1605(00)00382-2 [DOI] [PubMed] [Google Scholar]
- 2.Shoemaker RC, House D, Ryan JC. Defining the neurotoxin derived illness chronic ciguatera using markers of chronic systemic inflammatory disturbances: a case/control study. Neurotoxicol Teratol 2010; 32: 633–639. doi: 10.1016/j.ntt.2010.05.007 [DOI] [PubMed] [Google Scholar]
- 3.Hokama Y, Campora CE, Hara C. Anticardiolipin antibodies in the sera of patients with diagnosed chronic fatigue syndrome. J Clin Lab Anal 2009; 23: 210–212. doi: 10.1002/jcla.20325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Erv B, Hajnšek S, Kello N. Neurotoxin-induced fibromyalgia or fibromyalgia after ciguatera (tilapia fish) poisoning. Neurol Croat 2014; 63: 1–2. [Google Scholar]
- 5.Friedman MA, Fleming LE, Fernandez M. Ciguatera fish poisoning: treatment, prevention and management. Mar Drugs 2008; 6: 456–479. doi: 10.3390/md6030456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stommel EW, Parsonnet J, Jenkyn LR. Polymyositis after ciguatera toxin exposure. Arch Neurol 1991; 48: 874–877. doi: 10.1001/archneur.1991.00530200116031 [DOI] [PubMed] [Google Scholar]
- 7.Terato K, Harper DS, Griffiths MM. Collagen-induced arthritis in mice: synergistic effect of E. coli lipopolysaccharide bypasses epitope specificity in the induction of arthritis with monoclonal antibodies to type II collagen. Autoimmunity 1995; 22: 137–147. doi: 10.3109/08916939508995311 [DOI] [PubMed] [Google Scholar]
- 8.Thornton S, Duwel LE, Boivin GP. Association of the course of collagen-induced arthritis with distinct patterns of cytokine and chemokine messenger RNA expression. Arthritis Rheum 1999; 42: 1109–1118. doi: [DOI] [PubMed] [Google Scholar]
- 9.Choy EH, Panayi GS. Cytokine pathways and joint inflammation in rheumatoid arthritis. N Engl J Med 2001; 344: 907–916. doi: 10.1056/NEJM200103223441207 [DOI] [PubMed] [Google Scholar]
- 10.Matsui M, Kumar-Roiné S, Darius HT. Pacific ciguatoxin 1B-induced modulation of inflammatory mediators in a murine macrophage cell line. Toxicon 2010; 56: 776–784. doi: 10.1016/j.toxicon.2009.05.039 [DOI] [PubMed] [Google Scholar]
- 11.Vasanthi P, Nalini G, Rajasekhar G. Role of tumor necrosis factor-alpha in rheumatoid arthritis: a review. APLAR J Rheumatol 2007; 10: 270–274. doi: 10.1111/j.1479-8077.2007.00305.x [DOI] [Google Scholar]
- 12.Stone AV, Loeser RF, Vanderman KS. Pro-inflammatory stimulation of meniscus cells increases production of matrix metalloproteinases and additional catabolic factors involved in osteoarthritis pathogenesis. Osteoarthritis Cartilage 2014; 22: 264–274. doi: 10.1016/j.joca.2013.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tchetverikov I, Lard LR, DeGroot J. Matrix metalloproteinases-3, -8, -9 as markers of disease activity and joint damage progression in early rheumatoid arthritis. Ann Rheum Dis 2003; 62: 1094–1099. doi: 10.1136/ard.62.11.1094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ahrens D, Koch AE, Pope RM. Expression of matrix metalloproteinase 9 (96-kd gelatinase B) in human rheumatoid arthritis. Arthritis Rheum 1996; 39: 1576–1587. doi: 10.1002/art.1780390919 [DOI] [PubMed] [Google Scholar]
- 15.Xue M, McKelvey K, Shen K. Endogenous MMP-9 and not MMP-2 promotes rheumatoid synovial fibroblast survival, inflammation and cartilage degradation. Rheumatology (Oxford) 2014; 53: 2270–2279. doi: 10.1093/rheumatology/keu254 [DOI] [PubMed] [Google Scholar]