Abstract
Mental health conditions are common, disabling, potentially life-threatening, and costly; however, they are mostly treatable with early detection and intervention. Unfortunately, mental healthcare is in significantly short supply both nationally and locally, and particularly in small, rural, and relatively isolated communities. This article provides physicians and other health practitioners with a primer on the basic rationale and principles of integrating behavioral healthcare — particularly psychiatric specialty care — in primary care settings, including effective use of teleconferencing. Referring to a local-based example, this paper describes the programmatic components (universal screening, telephone availability, mutually educational team rounds, as-needed consultations, etc) that operationalize and facilitate successful primary care integration, and illustrates how these elements are applied to population segments with differing needs for behavioral healthcare involvement. Lastly, the article discusses the potential value of primary care integration in promoting quality, accessibility, and provider retention; discusses how new developments in healthcare financing could enhance the sustainability of primary care integration models; and summarizes lessons learned.
Keywords: Primary care integration, mental health, telepsychiatry, sustainability
Introduction
In the United States (U.S.), mental health conditions — defined as those conditions that affect mood, thinking, and/or behavior — affect 20% of the general population.1 Unfortunately, because of significant mental health provider shortages and stigma, only a fraction of this 20% receives appropriate and timely care. Untreated mental health conditions tend to get worse with time, and they significantly contribute to disability and mortality. Of note, the top leading causes of death among children, adolescents, and young adults in the U.S. and Hawai‘i are unintentional injuries (accidents) and suicide.2,3 Furthermore, untreated mental health conditions (including addictions, maladaptive health behaviors, and non-adherence secondary to depression and other behavioral health conditions) contribute to approximately one third of excess cost and waste in the U.S. healthcare system.4
In Hawai‘i, even conservative, demand-based estimates of psychiatric workforce needs indicate a shortage in absolute number of psychiatrists as well as a significant mal-distribution of services, such that there are very small numbers of psychiatrists on certain neighbor islands,5 and some of the smallest islands do not have any resident psychiatrists. The prevalence of certain youth and adult mental health conditions and substance use in Hawai‘i appear to be similar to those found nationally,6 but there are ethnic and socioeconomic health and mental health disparities7 that may reflect limitations in cultural appropriateness or accessibility of care. As an example, Andrade, et al, found that Native Hawaiian youth had significantly higher rates of any psychiatric disorder (32.7%) than non-Hawaiian youth (23.7%) and that these differences were largely the result of significantly different anxiety disorder rates.7 On the other hand, Hawai‘i has been a national leader in terms of primary care accessibility via the “medical home,” which is a concept founded by Dr. Calvin Sia as early as the 1970s.8
While primary care providers may be optimally positioned to ensure early detection and care for mental health conditions, they may be either unprepared or pressured for time in their practice. It is also important to note that in the U.S., most prescriptions for psychotropic agents (such as antidepressants and anxiolytics, including benzodiazepines) are written by primary care providers. In view of the prime importance of accessible behavioral healthcare for the future of U.S. healthcare reform, agencies such as the Substance Abuse and Mental Health Services Administration (SAMHSA), and the Health Resources and Services Administration (HRSA) have strongly advocated for models of behavioral health integration in the primary care medical home.9 Such models are particularly important for island states where the only way to access appropriate care is by paying for and flying to another island.
This article aims to provide the reader with a primer on the concept of behavioral health integration (BHI) for an island state by describing one local-based example of BHI. In studying this example, certain programmatic elements may be identified that improve access to mental healthcare and that could be potentially applicable for other remote and/or sparsely populated locations
Methodology
Program Overview
The program described in this article was based in a rural neighbor island federally qualified community health center (FQHC) that served a population of approximately 1,500 patients, predominantly of Asian, Native Hawaiian, and Other Pacific Islander ancestry. In this community, there were significantly fewer than 8,400 people, which is a number cited to feasibly support a full-time psychiatrist.10 There were not any locally based psychiatrists in this community, which was remotely located and accessible only by air or sea.
The program's leadership felt that BHI was arguably the only viable option for sustainable and accessible psychiatric care. Without BHI, access to psychiatry and psychiatric sub-specialties (child, addictions, geriatric, pain medicine, etc) would be only a remote possibility for small isolated communities.
The program had, at its foundation, a grant-funded behavioral health/primary care integration project. The project's general activities included: awareness of behavioral health conditions presenting in primary care; behavioral health screening by multidisciplinary healthcare providers, who have received basic training in such protocols as Screening, Brief Intervention, and Referral to Treatment (SBIRT); trauma-informed care; promotion of healthy behaviors and adherence, and practical application of motivational interviewing approaches; and overall promotion of mental health in the community.
The program included an on-site, primary care-embedded clinical psychologist/behavioral health specialist (1.0 full time equivalent [FTE]), as well as funding for a part-time psychiatrist (0.13 FTE), physically located in an urban setting, but readily available by video-teleconferencing (VTC) or telephone. In this project, the psychiatrist's time was devoted to the following roles: guidance on screening tools for behavioral and developmental conditions throughout the lifespan; provider-to-provider consultation around selected patients, including those who screened positive; telephone availability during the working week for questions relevant to primary care management of psychiatric conditions; scheduled VTC consultations with selected patients, together with their primary care team providers; ongoing collaboration and discussion with the primary care/psychology team around selected patients; monthly participation at team conferences; and in-services as requested - particularly around high-yield topics, such as pain management and common geriatric psychiatric conditions. In-person visits from the psychiatrist were periodically scheduled (approximately semi-annually), guided by needs for on-site team-building, problem-solving, and developing familiarity and relationships with community resources.
Process of Comprehensively Describing the Pilot Program and Identifying Key Components
The authors — inclusive of all members of the FQHC's primary care, embedded clinical psychology, and psychiatry teams (collectively the BHI team) — contributed to a comprehensive description (assembled by the first author) of the BHI model as it evolved over the previous year-and-a-half since the team's formation.
The Institutional Review Board of the University of Hawai‘i at Manoa provided approval for dissemination of program information (Committee on Human Studies #24022), as did the leadership of the project's community health center. No consents were utilized given the nature of this retrospective study.
Results
Description of Program Components
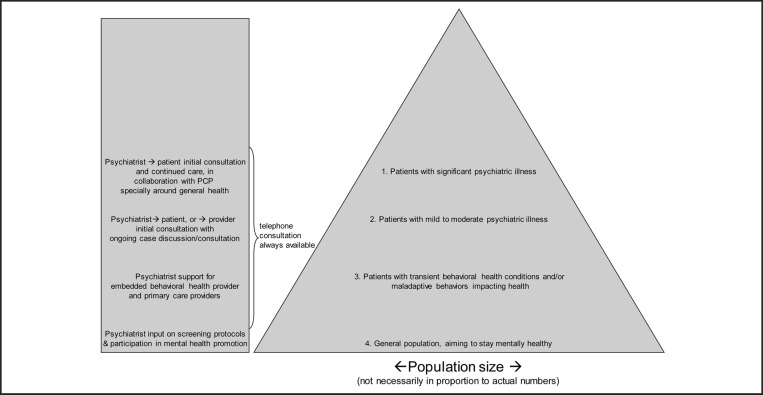
The model used for matching services to population needs is depicted in Figure 1 and Table 1 and is based on the clinic's intent to provide accessible health and preventive services for the community. The model illustrates how the aforementioned psychiatric services are integrated with the clinic's practice in providing care for patients with differing levels of need for mental healthcare. To demonstrate how the model is implemented in practice, four fictitious case vignettes are provided below. The case vignettes illustrate the important operational details of the model:
Fictitious/Hypothetical Case Vignette #1 (representing the general population aiming to stay mentally healthy): An early adolescent male patient presents for a routine school physical. The primary care clinic staff utilize a behavioral health screening tool that had previously been recommended by the BHI team and that (through training) they felt comfortable administering. They further feel confident that, should the screening be positive for depression or any other psychiatric condition, the embedded behavioral health specialist would be available on-site either to provide advice to the primary care providers or to meet the patient for additional screening and services, if appropriate. The screening is negative for any mental health concerns. Resources for mental health promotion (e.g., exercise, mindfulness, etc) are available through the community center.
Fictitious/Hypothetical Case Vignette #2 (representing the population of patients with transient behavioral health conditions and/or maladaptive behaviors impacting health): A young adult female is newly diagnosed with Type II diabetes mellitus, along with obesity and elevated blood pressure. Routine mental health screening reveals sub-threshold symptoms of depression, which the primary care provider feels are important to address nonetheless to improve adherence with lifestyle changes that are necessary to manage the patient's chronic conditions. The behavioral health specialist sees the patient for a few sessions and provides suggestions to the primary care provider on how to optimize motivation and address psychosocial barriers to change. The primary care provider and behavioral health specialist are aware that they have multiple forums — including the monthly team meeting and availability — to seek input from the psychiatrist should there be any need to seek consultation regarding the development of a major depressive episode possibly requiring treatment with psychiatric medication.
Fictitious/Hypothetical Case Vignette #3 (representing the population of patients with mild to moderate psychiatric illness): An adult female patient has a history of Major Depressive Disorder and Generalized Anxiety Disorder. She has not fully responded to the various serotonin-selective reuptake inhibitors (SSRIs) prescribed by the primary care provider nor to regular psychotherapy from the behavioral health specialist. The primary care provider and behavioral health specialist arrange for a call with the psychiatrist. The psychiatrist subsequently sees the patient for a VTC consultation and recommends updated laboratory tests (including a thyroid function test) to rule out other medical causes for the psychiatric symptoms and pharmacogenomic testing, the results of which subsequently guide the selection of a new antidepressant/anxiolytic medication. The primary care provider and psychiatrist jointly see the patient for a few sessions while the medication regimen is stabilized, and subsequently, the primary care provider (with the psychiatrist readily available for re-consultation or additional advice if needed) once again resumes the medication follow-up.
Fictitious/Hypothetical Case Vignette #4 (representing the population of patients with significant psychiatric illness): An adult male, relatively new to the clinic, has a history of a Schizophrenia Spectrum Disorder with past exacerbations requiring psychiatric hospitalization. He also has chronic pain from a previous injury. His psychotropic medication regimen consists of an antipsychotic medication, an SSRI, and an anxiolytic. The psychiatrist (via VTC, or on-site if able to coincide with a periodic site visit) and primary care provider see the patient together for several sessions and take the opportunity to mutually educate each other on the care they provide. In follow-up, the primary care provider, who sees the patient more frequently than the psychiatrist does, assists the latter in identifying early warning signs of relapse, in monitoring recommended labs (eg, fasting blood glucose, lipids, etc) in a timely fashion, and in monitoring for abnormal involuntary movements using standardized assessments. Periodically, the psychiatrist also sees the patient jointly with the behavioral health specialist, who provides supportive psychotherapy and assistance with stress management (to minimize the risk of symptom exacerbations). Working collaboratively, the entire BHI team can assist the patient with other issues that are optimally addressed via a combined primary care/behavioral health approach, ie, weight loss (particularly in the context of atypical antipsychotic medications with a side effect of weight gain and associated metabolic consequences), smoking cessation, and appropriate pain management. Because the lattermost issue is a particularly challenging one for the whole team, the psychiatrist provides, during one of the monthly team meetings, an in-service on non-narcotic management of chronic non-malignant pain.
Figure 1.
Behavioral Health Integration to Match Population Groups
Table 1.
Hypothetical and Fictitious Examples of Patients in Each Population Group
| Population group | Hypothetical/fictitious clinical example, with description of services provided (please see text for further examples and further elaboration) |
| 1. Patients with significant psychiatric illness | Adult or adolescent needing treatment with atypical antipsychotic medication and needing ongoing psychiatric follow-up and metabolic side effect monitoring from the primary care provider |
| 2. Patients with mild to moderate psychiatric illness | Adult with major depression, amenable to and responsive to standard medication (eg, serotonin-selective reuptake inhibitor) |
| 3. Patients with transient behavioral health conditions and/or maladaptive behaviors impacting health | Adult with diabetes or other chronic illness needing assistance with improving health behaviors and/or adjusting to illness |
| 4. General population, aiming to stay mentally healthy | Adolescent or parent of a new baby, presenting for health maintenance care and receiving depression screening |
Preliminary Findings and Impressions
Over the course of the project, regular check-ins were made with staff to review the model and the implementation, and to make necessary adjustments. Overall, the BHI team maintained a very positive view of the project, and while describing the project's model, they spontaneously identified several perceived strengths. They felt that most of their patients were served well and even optimally — because of enhanced continuity — by the primary care team, with readily available backup from the consulting psychiatrist. The psychiatrists' telephone availability allowed for timely feedback and advice when uncommon, but potential medication side effects were encountered in primary care. In addition, the team felt that mutual education and collaboration allowed psychiatry, psychology, and primary care team members to become partners in assuring that patients were on-time for recommended blood draws and other screens. The BHI team also felt that, particularly for patients with chronic psychiatric conditions needing periodic psychiatric (and not just primary care) visits, it was extremely beneficial to have regular team dialogue and collaboration around weight management, smoking cessation, and coexisting medical conditions (see Case Vignette #4). The on-site primary care providers and behavioral health specialist felt that it was very helpful and essential to the project's success to have all psychiatric documentation (in this case, via notes faxed soon after the psychiatric consultations) available in their health records.
The BHI team recalled various scenarios where they, by necessity, developed experience in stabilizing acute symptoms that, if not treated early, could potentially have led to emergency room visits or off-island acute hospitalizations that (besides being unsustainably costly) could further have fragmented the care.
The BHI team did not recall any encounters where VTC was either not accepted by patients or families, or technologically unfeasible. The BHI team authors observed that VTC consultations allowed for more accessibility and scheduling flexibility than is usually experienced in a comparable urban (non-VTC) practice. The team's experience was consistent with literature reviews supporting VTC's reliability and favorable outcomes.11
Thus far, lessons learned are as follows. In anticipation of long-term sustainability, it would have been ideal to have, from the beginning, a more detailed tracking of all professional activities and communications, including those pertaining to patients in the 3rd and 4th tiers of the pyramid and those not currently attached to billing codes (but potentially attached to billing codes in the future). Also, in retrospect, it would have been ideal to involve psychiatric or primary care physician trainees in the process of establishing and maintaining a behavioral health integration program, which could very well be an important component of future practice that would address workforce issues.
An additional lesson is one that is probably already well known; however, it bears repeating: Collaborating closely to provide coordinated care to patients is efficient and results in high-quality care. Especially in a remote, rural area, these types of specialty services and coordination are often non-existent — yet this program provided both to this rural community. It was very important to have, from the beginning, a team approach to care fostered at the FQHC and a strong commitment from primary care and clinical psychology to expand existing practices (such as SBIRT) and to positively engage psychiatry into planning and work-flow. It was also very important to have a reliable user-friendly VTC platform that could ensure buy-in from staff, consultants, and patients. The FQHC had an existing license for Zoom version 4.0.2258.0125, 9 (San Jose, CA) which is a cloud-based, Health Insurance Portability and Accountability Act (HIPAA)-compliant VTC/telehealth application that made scheduling and connecting easy by any member of the FQHC team.
Discussion and Future Directions
An important limitation of this paper was the absence of any quantitative or semi-quantitative data to measure outcomes. Notwithstanding this limitation, we believe that the impact on quality of behavioral health care was significant and recognized by all of those directly involved. On any given month, the primary care team has five to ten active patients with direct psychiatric intervention. The ability to provide medication management, particularly for patients with severe mental illness, dramatically improved with BHI, The primary care providers are currently safely using a much broader spectrum of psychotropic medication, monitoring for side effects, appropriately titrating and adjusting doses, and at times using combinations of medication. For several patients, the addition of psychiatric services has aided in establishing correct diagnoses for such conditions as adult Attention-Deficit Hyperactivity Disorder (ADHD), Autism Spectrum Disorder, Schizophrenia Spectrum and Other Psychotic Disorders, and Personality Disorders. With the obvious improved quality in our care delivery system, we felt that it would be helpful for local and regional healthcare providers to learn about the authors' experiences with behavioral health/primary care integration. To our knowledge, this was the first published paper (data-driven or descriptive) focused on a Hawai‘i-based program's experience with behavioral health/primary care integration.
Professional isolation is a constant challenge in rural settings. It often leads to significant stress in doing the right thing for complex patients and eventually to provider burn out. Based on our experience with this project, the authors believe that vertical integration with multi-specialty psychiatric support and backup has had a positive impact on both primary care and behavioral health providers in the rural setting. The BHI model dramatically expanded the care team and has subjectively improved the structured treatment plan and quality of medication management. Furthermore, we believe that, by reducing isolation in rural communities, BHI has the potential to improve provider job satisfaction and retention, which is a constant struggle in many rural communities and a significant stress for providers, patients, and communities alike.
To date, resources for the project have relied upon grant funding plus a small component of professional billing. Unfortunately, up to this point, many of the services that are core to primary care integration are not reimbursable in traditional fee-for-service models. This situation may change with the introduction of new Medicare codes and funding allocations, specifically to support BHI, which leads to both quality and cost-effective care.12 Likewise, accountable care organizations have already begun to recognize, via incentive reimbursements, the value of primary care-based behavioral health screening and intervention.
Overall, the authors hope that this paper will stimulate further dissemination and discussion of local experiences and ideas around this important model in healthcare's future. We further hope that this description of programmatic components felt by the team to be beneficial can help the specialty to define what may be promising or best practices for primary care/behavioral health integration.
As more models are implemented in larger organizations and in larger populations, we recommend that quantitative studies be done to measure improvements in behavioral healthcare quality, accessibility, and cost-effectiveness (eg, earlier age of first diagnosis of certain conditions, higher percentage of patients receiving indicated behavioral healthcare, decreased wait times between initial diagnosis and initiation of treatment, reduced rates of suicide and violence in communities served, reduced rates of psychiatric and other medical hospitalizations, and emergency visits, etc). Furthermore, we recommend that longitudinal studies be done to answer the important question of whether primary care/behavioral health integration can improve long-term workforce recruitment and retention in rural communities that are isolated by being on relatively small islands or by some other geographic barrier.
Acknowledgements
This project was funded by a FY 2014 Grant Award for Mental Health Service Expansion - Behavioral Health Integration from the U.S. Department of Health and Human Services, Health Resources Services Administration. Cori Takesue, Jared Medeiros, Aileen Duran, Joseph Humphry, and Diana Shaw are employees of the community health center that received the grant. Anthony Guerrero, Michael Fukuda, and Earl Hishinuma are employed by the Department of Psychiatry, University of Hawai‘i at Manoa; and during the project implementation, Ryan Lunsford was also employed by the Department of Psychiatry, University of Hawai‘i at Manoa. The community health center contracted the Department of Psychiatry to partner and provide mental health consultation and services.
Conflict of Interest
None of the authors identity any conflicts of iterest.
References
- 1.U.S. Department of Health and Human Services, author. Mental Health: A Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, National Institutes of Health, National Institute of Mental Health; 1999. [August 2, 2016]. https://profiles.nlm.nih.gov/ps/access/NNBBHS.pdf. [Google Scholar]
- 2.Osterman MJ, Kochanek KD, MacDorman MF, Strobino DM, Guyer B. Annual summary of vital statistics: 2012–2013. [September 24, 2016];Pediatrics. 2015 Jun;135(6):1115–1125. doi: 10.1542/peds.2015-0434. http://pediatrics.aappublications.org/content/pediatrics/early/2015/04/28/peds.2015-0434.full.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hawai‘i Health Data Warehouse, Hawai‘i State Department of Health, author. Leading Causes of Death in Hawai‘i by Age. 2016. [August 2, 2016]. http://hhdw.org/wp-content/uploads/Vital-Statistics_Leading-Causes-of-Deaths_IND_000232.pdf.
- 4.Pricewaterhouse Coopers' Health Research Institute, author. The Price of Excess: Identifying Waste in Healthcare Spending. 2006. [August 2, 2016]. http://www.pwc.com/us/en/healthcare/publications/the-price-of-excess.html.
- 5.Withy K. Report on Findings from the Hawai‘i Physician Workforce Assessment Project. 2015. [August 2, 2016]. https://www.hawaii.edu/offices/eaur/govrel/reports/2015/act18-sslh2009_2015_physician-workforce_report.pdf.
- 6.Substance Abuse and Mental Health Services Administration, author. Behavioral Health Barometer: Hawai‘i, 2014. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2015. [11/19/2016]. HHS Publication No. SMA-15-4895HI. http://www.samhsa.gov/data/sites/default/files/State_BHBarometers_2014_1/BHBarometer-HI.pdf. [Google Scholar]
- 7.Andrade NN, Hishinuma ES, McDermott JF, Jr, Johnson RC, Goebert DA, Makini GK, Jr, Nahulu LB, Yuen NYC, McArdle JJ, Bell CK, Carlton BS, Miyamoto RH, Nishimura ST, Else IRN, Guerrero APS, Darmal A, Yates A, Waldron JA. The National Center on Indigenous Hawaiian Behavioral Health study of prevalence of psychiatric disorders in native Hawaiian adolescents. J Am Acad Child Adolesc Psychiatry. 2006;45(1):26–36. doi: 10.1097/01.chi.0000184933.71917.f4. [DOI] [PubMed] [Google Scholar]
- 8.Sia C, Tonniges TF, Osterhus E, Taba S. History of the medical home concept. Pediatrics. 2004;113(5 Suppl):1473–1478. [PubMed] [Google Scholar]
- 9.Substance Abuse and Mental Health Services Administration, author. SAMHSA-HRSA Center for Integrated Health Solutions. [February 22, 2017]. http://www.integration.samhsa.gov/
- 10.Sargeant JK, Adey T, McGregor F, Pearce P, Quinn D, Milev R, Renaud S, Skakum K, Dada N. Psychiatric human resources planning in Canada. [September 24, 2016];Can J Psychiatry. 2010 55(9):1–20. http://www.wpanet.org/uploads/News-Zonal-Representatives/wpa-policy-papers-from-zone1/Zone-1-Psych-Human-Resources-Planning-in-Canada.pdf. [PubMed] [Google Scholar]
- 11.Hubley S, Lynch SB, Schneck C, Thomas M, Shore J. Review of key telepsychiatry outcomes. World J Psychiatry. 2016;6(2):269–282. doi: 10.5498/wjp.v6.i2.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Medicare and Medicaid Services, author. Medicare Proposes Substantial Improvements to Paying for Care Coordination and Planning, Primary Care, and Mental Health in Doctor Payment Rule. [September 24, 2016]. https://www.cms.gov/Newsroom/MediaReleaseDatabase/Press-releases/2016-Press-releases-items/2016-07-07.html.